Cerebrovascular diseases Definitions Stroke it is acute onset
Cerebrovascular diseases
Definitions: -Stroke : it is acute onset of neurological deficit that persist for at least 24 h. -Minor stroke : it is deficits that last for longer than 24 h but resolve completely. -stroke in evolution: actively progressing as a direct consequence of the underlying vascular disorder. -TIA : neurological deficit that resolve completely within 24 h. Stroke either due to ischemia 85% or hemorrhage 15%.
Pathophysiology : acute occlusion of an intracranial vessel causes reduction in blood flow, fall in CBF to zero lead to death of tissue within 4 -10 min. tissue surrounding the core region of infarction is ischemic but reversibly dysfunction and referred to ischemic penumbra. Saving the ischemic penumbra is the goal of thrombolytic therapy.

Risk factors : -nonmodifiable: -Age -Sex -Race ethnicity -Hereditary modifiable -Hypertension -D. M -Smoking -Alcohol Intake -Obesity -Drugs abuse -Food intake
Causes : -common causes: -Thrombosis : lacunars stroke -large vessel stroke -dehydration -Embolic occlusion: -artery to artery like carotid bifurcation and aortic arch. Cardioembolic : AF, mural thrombus, MI, dilated cardiomyopathy,
Uncommon causes: -hypercoagulable diseases. -venous sinus thrombosis. -fibromuscular dysplagia. -vasculitis. -Cardiogenic -drugs. -moya disease. -eclampsia.
Clinical manifestations : -1 -Middle cerebral art. Stroke: it is the commonest art. Involved by imbolic rather than thrombosis. -A- superior division stroke: -contralateral hemiparesis. -contralateral hemisensory loss. -no homonymous hemianopia. -expressive aphasia if dominant. -B-inferior division stroke: -contralateral homonymous hemianopia. -agraphesthasia &asteriognosis. -anosognosia. -neglect contralateral space &limb. -wernicke aphasia if dominant. -acute confusion. -C- stem of MCA: -contralateral hemiplegia & sensory loss affecting face, arm &leg. -global aphasia.
-2 - ACA stroke: -contralateral paralysis & sensory loss affecting the leg. -impaired maturation center. -contralateral grasp reflex & sucking R. -abulia. -3 -internal carotid art. Stroke: -one fifth of ischemic stroke. -may be asymptomatic. -symptomatic similar to that of MCA stroke. -4 -PCA syndrome: -homonymous hemianopia with or without macular sparing. -anomic aphasia. -alexia without agraphia. -Visual agnosia. -Cortical blindness. -memory impairment. -prosognosia.
-5 - Basilar art. Syndrome : -brief anatomy. -hemiplegia or quadriplegia. -coma is common. -unilateral or bilateral 6 th N. palsy. -locked in syndrome. -unilateral or bilateral 3 th N. palsy. - Paralysis upward or downward gaze. -6 -PICA syndrome : -epsilateral cerebellar ataxia. -facial sensory loss. -nystagmus -contralateral loss pain &tempru. -excessive salivation. -7 - Associated symptome : -seizures. -headache. -horner syndrome. -nausea & vomiting. -vertigo. -dysphasia & dysartheria
Small vessel stroke: -lipohyalinotic or atherothrobotic occlusion of small art. -Hypertention & age. -20% of all stroke. -1 -pure motor hemiparesis: -2 -pure sensory stroke: -3 -ataxic hemiparesis: -4 -dysarthria-clumsy hand syndrome: -5 -pure motor hemiparesis & brocas aphasia:
Investigative studies : -A- blood tests : 1 -blood count. 2 -ESR. 3 -serology for syphilis. 4 -RBS. 5 -serum lipids. -B-ECG. -C-echo study. -D-CT or MRI: -E-carotid Doppler. -F-LP. -G-Angiography. -H-EEG.
DDx: 1 -vascular disorders: -ICH -SAH -subdural or epidural hematoma. -saggital sius thrombosis. 2 -structural brain lesion: -tumors. -abscess. 3 -metabolic: -hypoglycemia. -hyperosmolar nonketotic hyperglycemia.
Treatment: 1 -medical support: the immediate goal is to optimize cerebral perfusion in the surrounding ischemic penumbra. 1 -Blood pressure: 2 -Glucose: 3 -Fever. 4 -Prevent complicaion: 5 -Antiedema drugs: 2 -Thrombolysis: -Indications: -C/I: 3 -Anticoagulation: when 220/120 mmhg ? ? <11. 1 mml/L (200 mg/dl). - r. TPA.
4 -Antiplatelets: -aspirin. -ticlopidine &clopidogrel. -compination. 5 -surgical therapy: -A-symptomatic carotid stenosis. -B-asymptomatic carorid stenosis. 6 -Rehabilitation: 1 -early physical therapy. 2 -speech therapy. 3 -education of pat. &family. 4 -prevente complication of immobility.
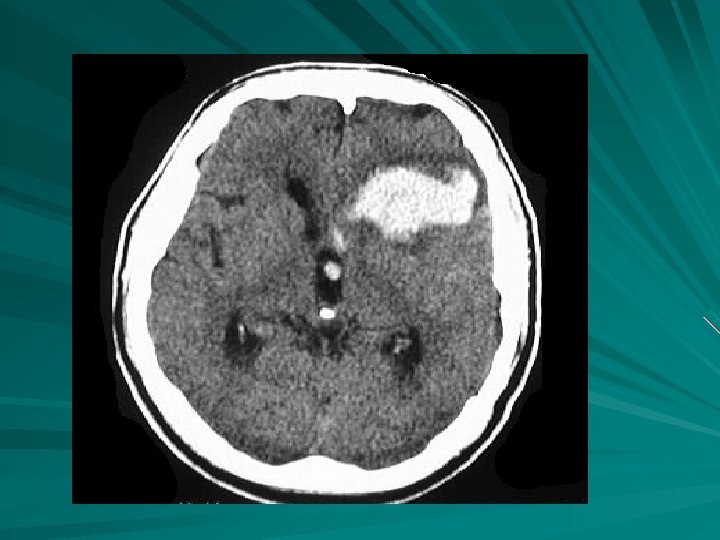
Intracranial hemorrhage: -it is classified by their location & the underlying vascular pathology. -it is incidence 15% of CVA. Causes: 1 -head trauma. 2 -hypertensive H. 3 -transformation of prior stroke. 4 -metastatic brain tumor. 5 -coagulopathy. 6 -drugs. 7 -AVM. 8 -aneurysm. 9 -amyliod angiopathy. 10 -vasculitis. 11 -vasculopathy. 12 -cavernous angioma.
Risk factors: -age. higher in young subjects. -male gender. -hypertension. -DM. -smoking. -high alcohol intake. -very low cholesterol <160 mg/dl.
Pathophysiology: ICH has 3 main phases. -arterial rupture & hematoma formation. -haematoma enlargement. -peri-hematoma oedema. -ICH result from rupture of small penetrating art. -early oedema is due to the vasogenic oedema. peak 4 -5 days. -delayed oedema is both vasogenic &cytotoxic. Last 2 -4 weeks.
Diagnosis : 1 -Imaging noncontrast CT. 2 -Routine investigation. -CBP & ESR. -Electrolyte. -PT & PTT. -U/S. - B. urea. & creatinine. -S. cholesterol. -ECG. 3 -If young patients. Send to the following. -ANA & antidouble strand DNA. -Antiphospholipid ABS. -VDRL. 4 - EEG.
Treatment: 1 -admition to stroke unit. 2 -reducing ICH. -Mannitol. -Steriod. 3 -hdrocephalus. 4 -cerebellar hematoma. >3 cm. 5 -large lobar hematoma. 6 -hypertension. BP >180/105 mmhg. 7 -seizures. 8 -prevention of aspiration. Nasogastic tube. 9 -prevention of complication. 10 -hematoma growth.
Hypertensive hemorrhage: -brief pathophysiolgy. -common sites in order. Putamen, thalamus, deep ceebellum & pons. -almost occurs when the patients are awake &stressed. -develop over 30 -90 min. -abrupt onset of focal neurological deficits. Thalamic hemorrhage : -contralateral hemipligia &hemisensory loss. -horner syndrome. -homonymous field defect. -Paralysis of vertical gaze. -absent of light R. -absence of convergence.
Pontine hemorrhage: -occurs over min. -deep coma. -quadriplegia. -pin-piont pupils. -hyperpyrexia. -severe hypertension. -hyperpnea & hyperhydrosis. -impiarment of dolls maneuver. Cerebellar hemorrhage: -usually develop over h. -occipital headache &vomiting. -dizziness &vertigo. -ataxia of giat. Impaired of gaze. -dysartheria & dysphagia.
SAH: -excluding head trauma the most common cause of SAH is rupture of aneurysm. -saccular aneurysm occurs in 2% of adults. -the most common location are terminal ICA, MCA bifurcation, & top of basilar art. -mycotic aneurysm. Clinical manifestations: -most unruptured aneurysm are completely asymptomatic. -the hallmark feutures. -sudden onset loss of coniousness. -neck stiffness &vomiting. -cranial N. palsy. -subhyliod hemorrhage. -hemiparesis, aphasia &abulia.
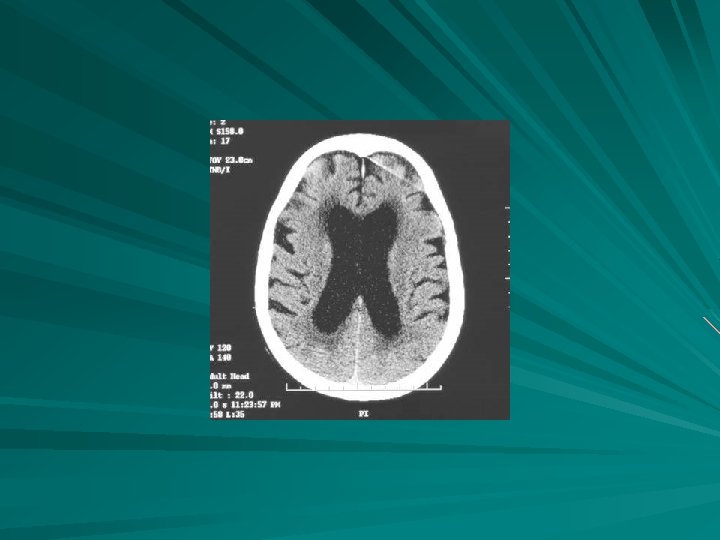
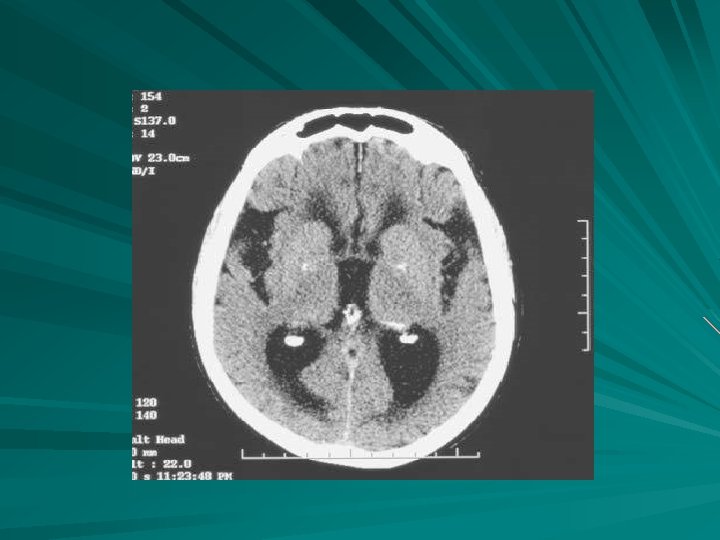
Delayed neurological deficits: 1 -Rerupture: 2 -Hydrocephalus: 3 -Vasospasm: 4 -Hyponatremia: Laboratory evaluation & Imaging: -the hallmark is blood in the CSF. -noncontrast CT of brain. -if CT fail , LP done. -what are the finding of CSF. -four vessel angiography. -ECG finding. -monitoring of electrolytes.
Tretment: -Early aneurysm repair prevent rerupture. -protecting the airway. -managing BP. -treat vasospasm. -decrease raised ICP. -bed rest in quiet room & given stool softeners. -treat seizures. -managing hyponatremia. -prevent of complication. -neurosurgical consultation.
- Slides: 27