Cerebral palsy CP Osama Sharaf Eldin Learning Objectives
Cerebral palsy (CP) Osama Sharaf Eldin
Learning Objectives • To, define, classify the causes, and describe the diagnostic approaches of cerebral palsy • To know the different methods of management of complications of cerebral palsy and the importance of rehabilitation • To understand the importance of social, medical and psychological support for the patient with cerebral palsy and his family
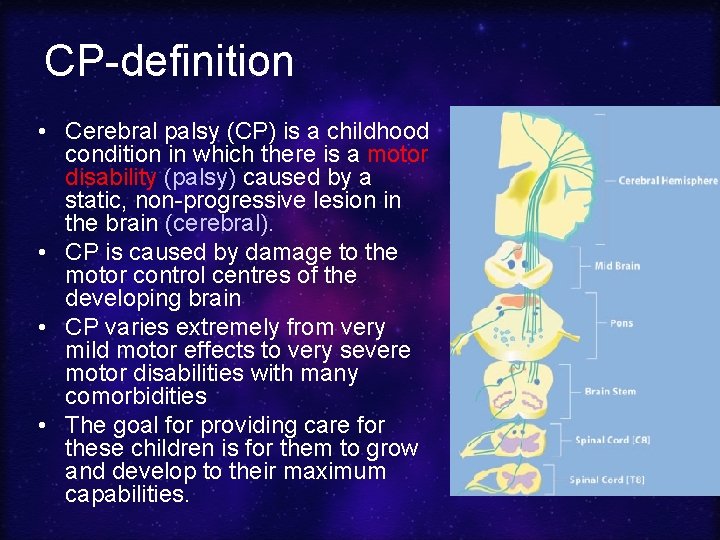
CP-definition • Cerebral palsy (CP) is a childhood condition in which there is a motor disability (palsy) caused by a static, non-progressive lesion in the brain (cerebral). • CP is caused by damage to the motor control centres of the developing brain • CP varies extremely from very mild motor effects to very severe motor disabilities with many comorbidities • The goal for providing care for these children is for them to grow and develop to their maximum capabilities.
Remember that although CP is a nonprogressive lesion in the brain, the complications and physical disabilities are progressive
Economic toll of CP The economic cost for CP patients in the US is $1000, 000 per case, including lost income
Epidemiology • 2 -3 /1000 children • Males> females (1. 5: 1) • CP occurs in early childhood, usually < 2 years of age • Timing: – During pregnancy: 75% of cases (CONGENITAL) – During childbirth: 10% (NEONATAL) – After birth (up to 2 ys): 15% (POST-NATAL)
Risk Factors – High risk in survivors of neonatal intensive care units (ICU). – Multiple births. The reported prevalence rate of CP per pregnancy for singles is 0. 2%, for twins 1. 5%, for triplets 8. 0%, and for quadruplets 43%. • Adequate prenatal care did not decrease the incidence of CP. This is attributed to medical advances in care of premature babies (which results in a greater survival rate). Those babies are at high risk of CP
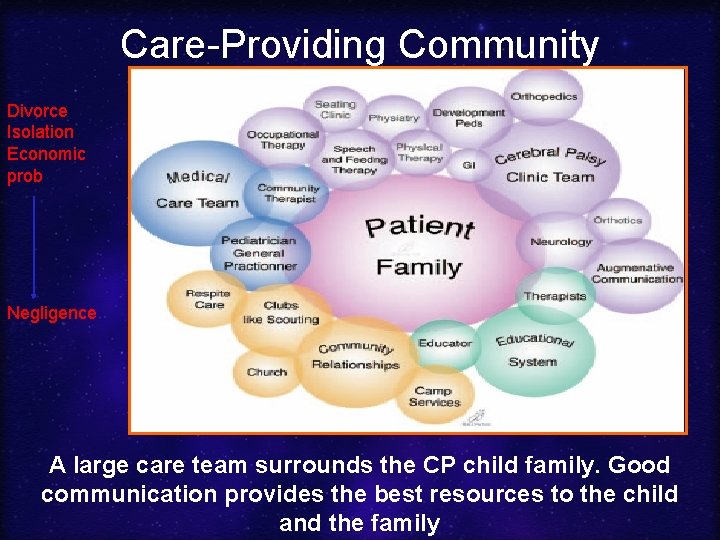
Care-Providing Community Divorce Isolation Economic prob Negligence A large care team surrounds the CP child family. Good communication provides the best resources to the child and the family
Aetiology of Cerebral Palsy Aetiology Congenital causes Neonatal causes Postnatal causes
Congenital Causes Most congenital causes lead to hypotonia +/- quadriplegia Congenital causes include: • Neural tube defects: e. g. , encephalocele • Hydrocepalus (increased cerebrospinal fluid pressure and volume) compress brain tissue • Microencepahly
Neonatal Causes that occur during or immediately after birth include: • Prematurity and intracerebral haemorrhages • Hypoxic birth injuries leads to hypoxic ischemic encephalopathy (HIE). The causes of this hypoxia include obstetric dystocias and decreased foetal cerebral blood flow
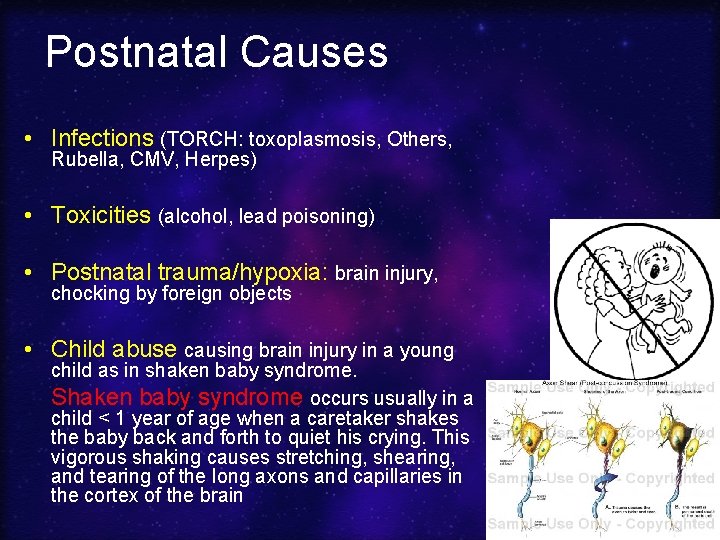
Postnatal Causes • Infections (TORCH: toxoplasmosis, Others, Rubella, CMV, Herpes) • Toxicities (alcohol, lead poisoning) • Postnatal trauma/hypoxia: brain injury, chocking by foreign objects • Child abuse causing brain injury in a young child as in shaken baby syndrome. Shaken baby syndrome occurs usually in a child < 1 year of age when a caretaker shakes the baby back and forth to quiet his crying. This vigorous shaking causes stretching, shearing, and tearing of the long axons and capillaries in the cortex of the brain
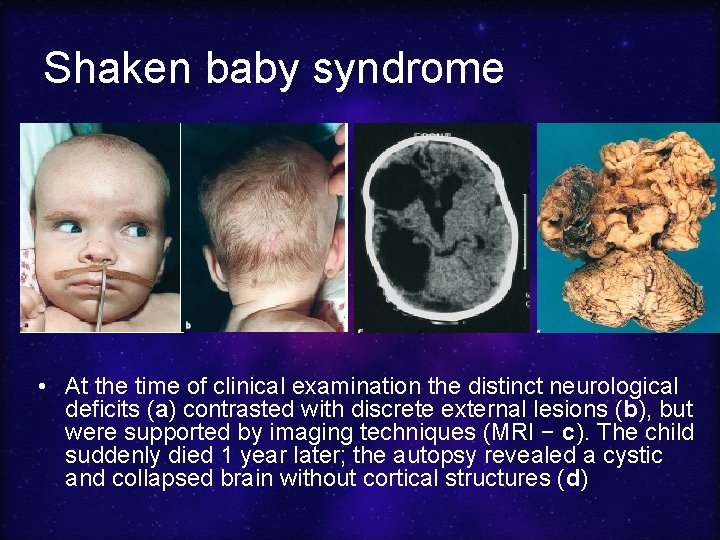
Shaken baby syndrome • At the time of clinical examination the distinct neurological deficits (a) contrasted with discrete external lesions (b), but were supported by imaging techniques (MRI − c). The child suddenly died 1 year later; the autopsy revealed a cystic and collapsed brain without cortical structures (d)
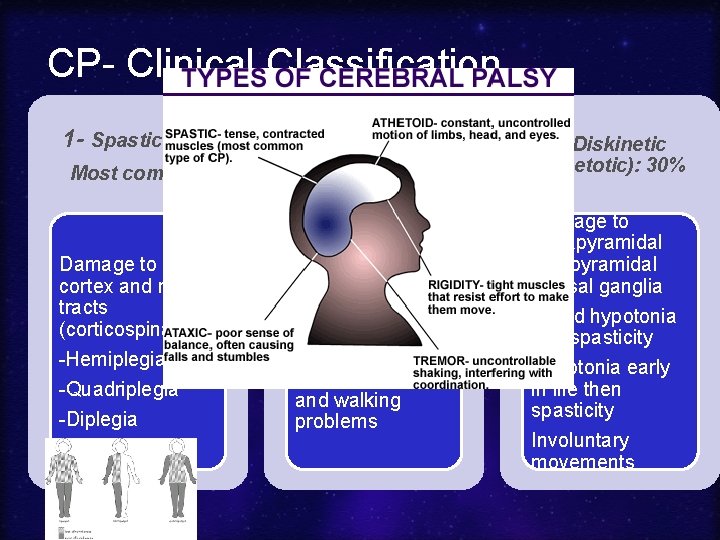
CP- Clinical Classification 1 - Spastic: 60% Most common Damage to motor cortex and motor tracts (corticospinal) -Hemiplegia -Quadriplegia -Diplegia 2 -Ataxic): 10% Cerebellar damage Hypotonia is the main problem. Loss of skilled fine movements and walking problems 3 -Diskinetic (Athetotic): 30% Damage to extrapyramidal and pyramidal +Basal ganglia Mixed hypotonia and spasticity Hypotonia early in life then spasticity Involuntary movements
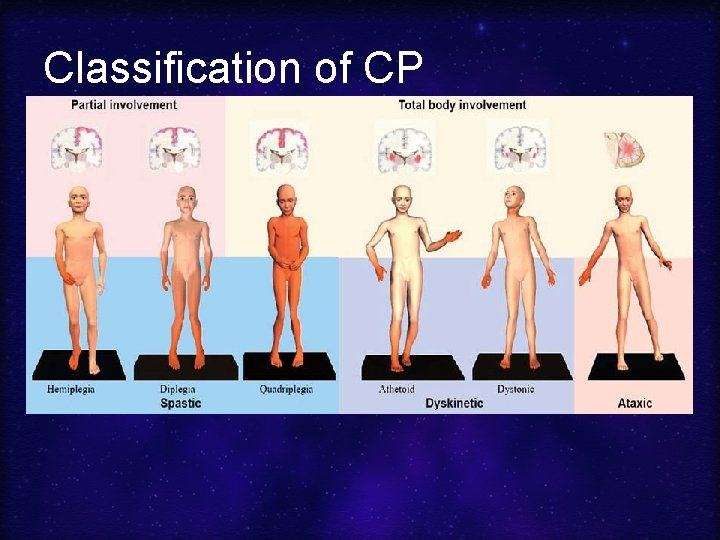
Classification of CP
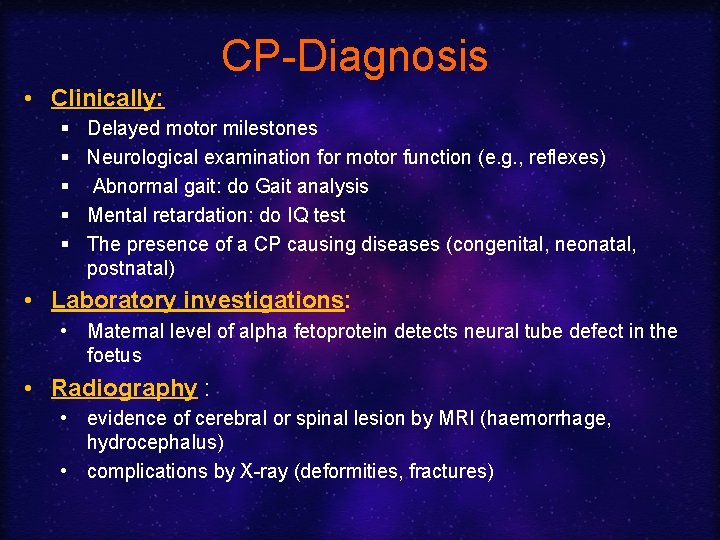
CP-Diagnosis • Clinically: § § § Delayed motor milestones Neurological examination for motor function (e. g. , reflexes) Abnormal gait: do Gait analysis Mental retardation: do IQ test The presence of a CP causing diseases (congenital, neonatal, postnatal) • Laboratory investigations: • Maternal level of alpha fetoprotein detects neural tube defect in the foetus • Radiography : • evidence of cerebral or spinal lesion by MRI (haemorrhage, hydrocephalus) • complications by X-ray (deformities, fractures)
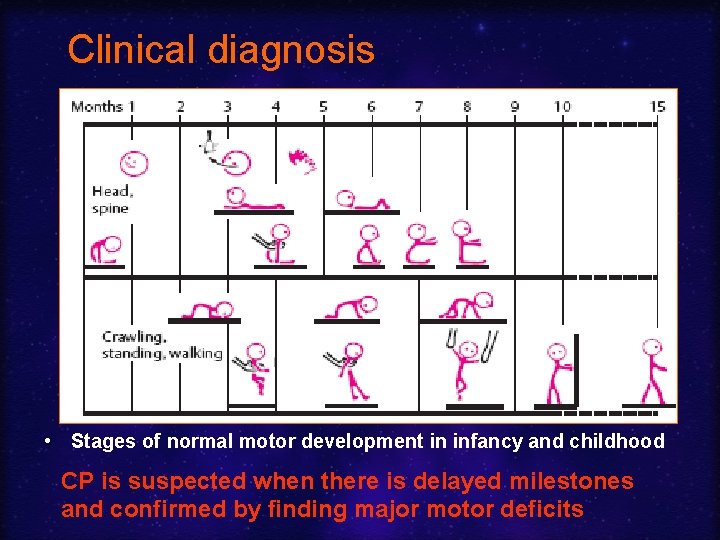
Clinical diagnosis • Stages of normal motor development in infancy and childhood CP is suspected when there is delayed milestones and confirmed by finding major motor deficits
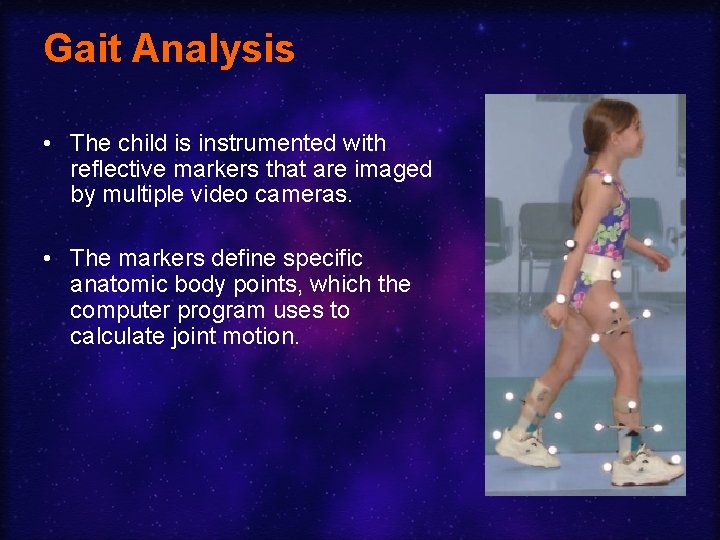
Gait Analysis • The child is instrumented with reflective markers that are imaged by multiple video cameras. • The markers define specific anatomic body points, which the computer program uses to calculate joint motion.
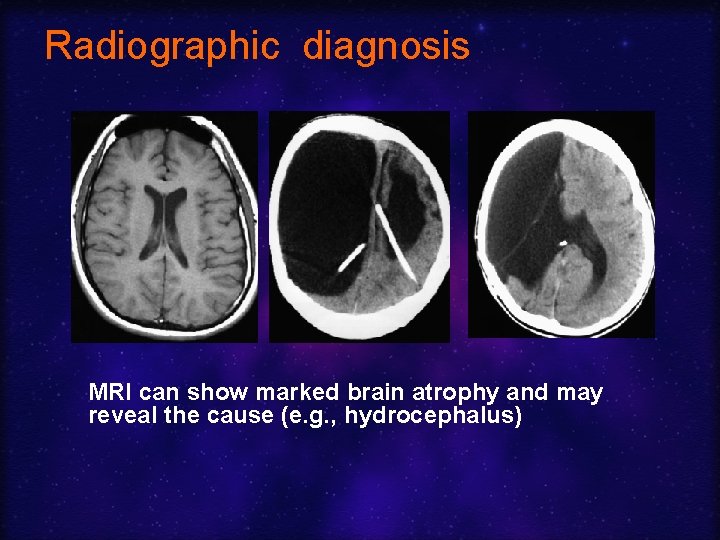
Radiographic diagnosis MRI can show marked brain atrophy and may reveal the cause (e. g. , hydrocephalus)
Main Problems of CP • • Spasticity Hypotonia Osteoporosis, arthritis and fractures Mental retardation (IQ < 50): 30% Active seizures: 20% Total paralysis: 20% Abnormal gait: Scissor walking (where the knees come in and cross) and toe walking (marionette-like) • Blindness: 10% • All complications of immobility (see complications of immobility lecture)
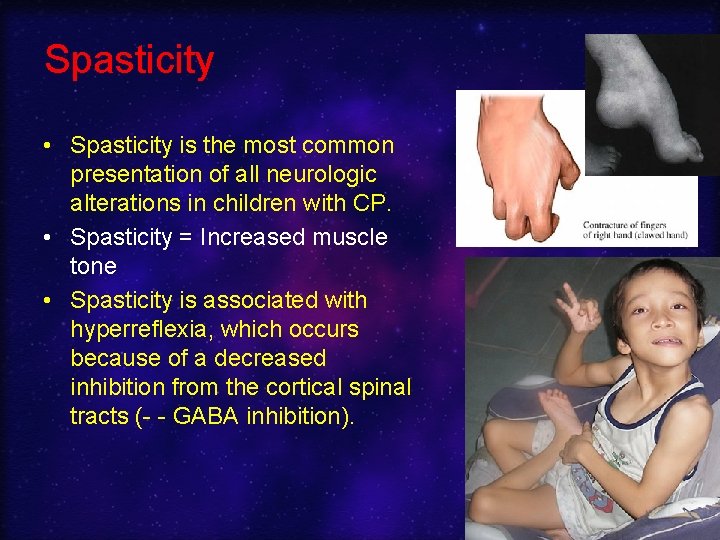
Spasticity • Spasticity is the most common presentation of all neurologic alterations in children with CP. • Spasticity = Increased muscle tone • Spasticity is associated with hyperreflexia, which occurs because of a decreased inhibition from the cortical spinal tracts (- - GABA inhibition).
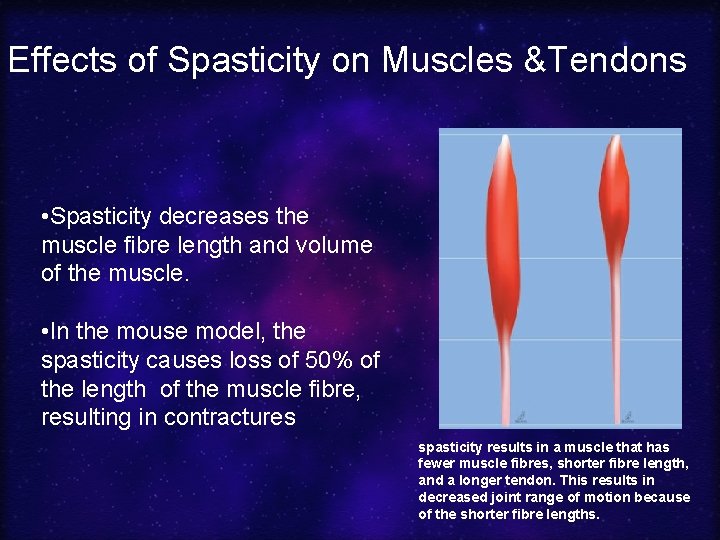
Effects of Spasticity on Muscles &Tendons • Spasticity decreases the muscle fibre length and volume of the muscle. • In the mouse model, the spasticity causes loss of 50% of the length of the muscle fibre, resulting in contractures spasticity results in a muscle that has fewer muscle fibres, shorter fibre length, and a longer tendon. This results in decreased joint range of motion because of the shorter fibre lengths.
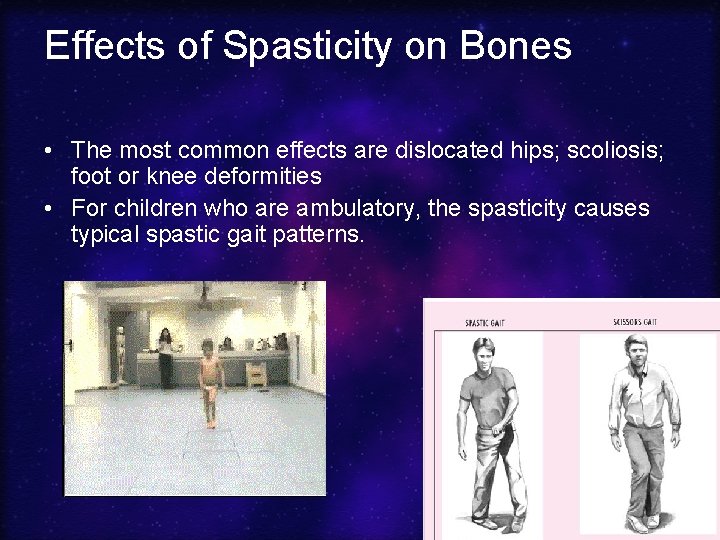
Effects of Spasticity on Bones • The most common effects are dislocated hips; scoliosis; foot or knee deformities • For children who are ambulatory, the spasticity causes typical spastic gait patterns.
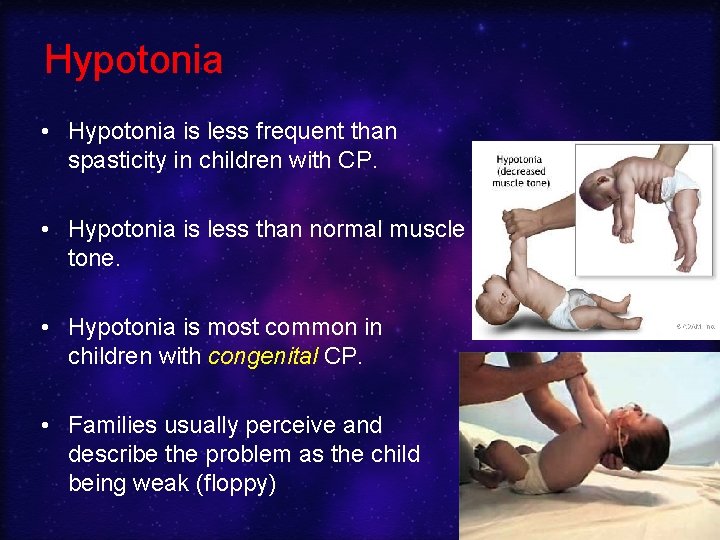
Hypotonia • Hypotonia is less frequent than spasticity in children with CP. • Hypotonia is less than normal muscle tone. • Hypotonia is most common in children with congenital CP. • Families usually perceive and describe the problem as the child being weak (floppy)
Effects of hypotonia • The muscles tend to be weak, excessively long, and very thin when examined. • Long thin (gracile) bones with enlarged metaphysis (ballooning) + osteoporosis. • Joint hypermobility.
Problems of hypotonia • Poor trunk and head control. • The joint laxity and poor strength leads to a high rate of joint dislocations at the hip and feet with the development of scoliosis. • Long fragile bones (+ osteoporosis) recurrent fractures
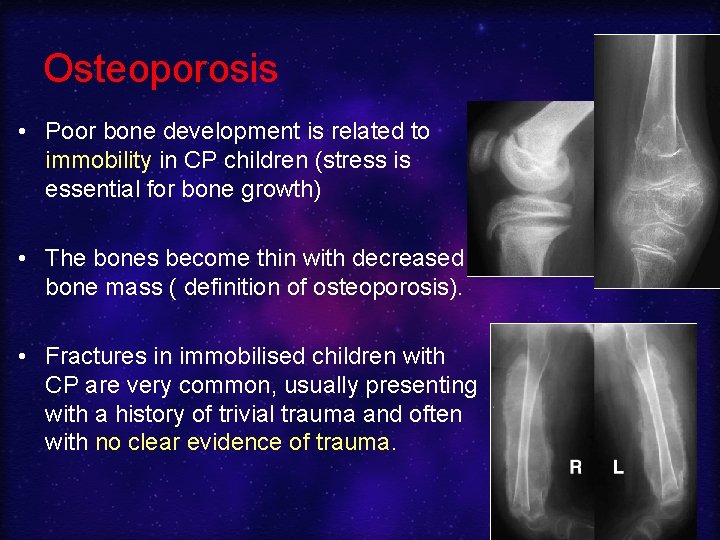
Osteoporosis • Poor bone development is related to immobility in CP children (stress is essential for bone growth) • The bones become thin with decreased bone mass ( definition of osteoporosis). • Fractures in immobilised children with CP are very common, usually presenting with a history of trivial trauma and often with no clear evidence of trauma.
CP- Medical Management • There is no known cure for CP. • Medical intervention is limited to the treatment and prevention of complications arising from CP's effects
CP- Medical Management • • Treating feeding and growth problems Spasticity treatment Hypotonia treatment Orthotics Walking aids Surgery Education “The Education for All Handicapped Children Act” facilitates involvement of CP children within the community • Physical therapy: including Electrical stimulation, Tone reducing casts, and Muscle strengthening • Otherapies
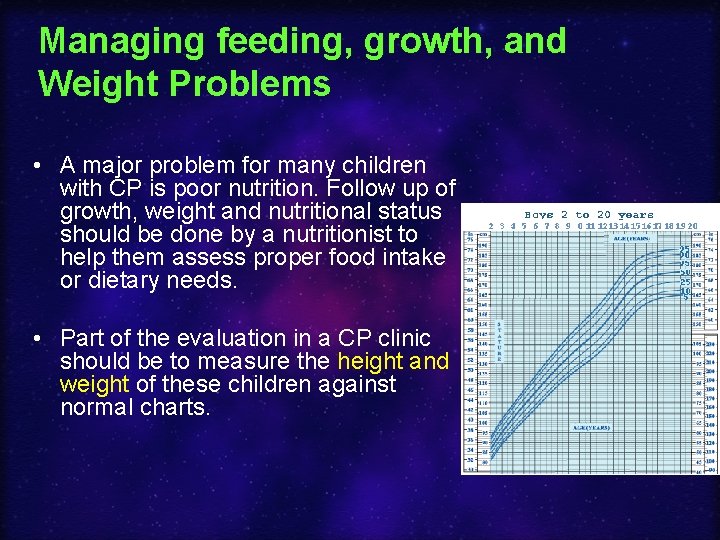
Managing feeding, growth, and Weight Problems • A major problem for many children with CP is poor nutrition. Follow up of growth, weight and nutritional status should be done by a nutritionist to help them assess proper food intake or dietary needs. • Part of the evaluation in a CP clinic should be to measure the height and weight of these children against normal charts.
Spasticity treatments • The ideal treatment of spasticity is to decrease the tone at the anatomic area of spasticity • Options: – Medical treatment – Botox – Rhizotomy
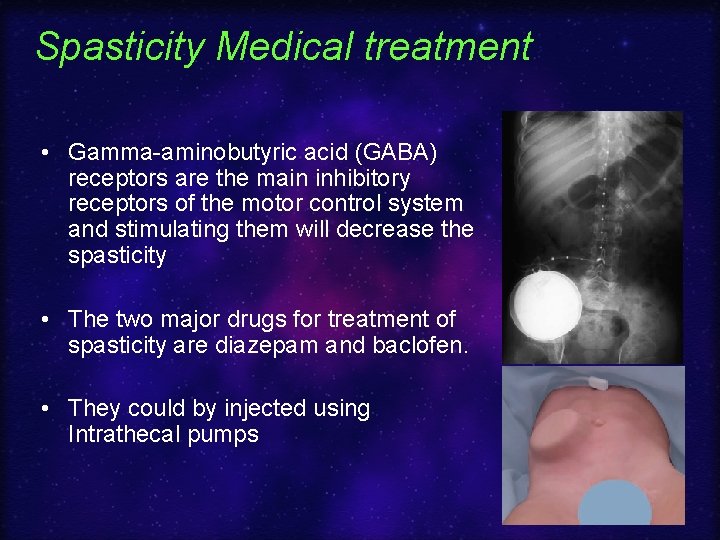
Spasticity Medical treatment • Gamma-aminobutyric acid (GABA) receptors are the main inhibitory receptors of the motor control system and stimulating them will decrease the spasticity • The two major drugs for treatment of spasticity are diazepam and baclofen. • They could by injected using Intrathecal pumps
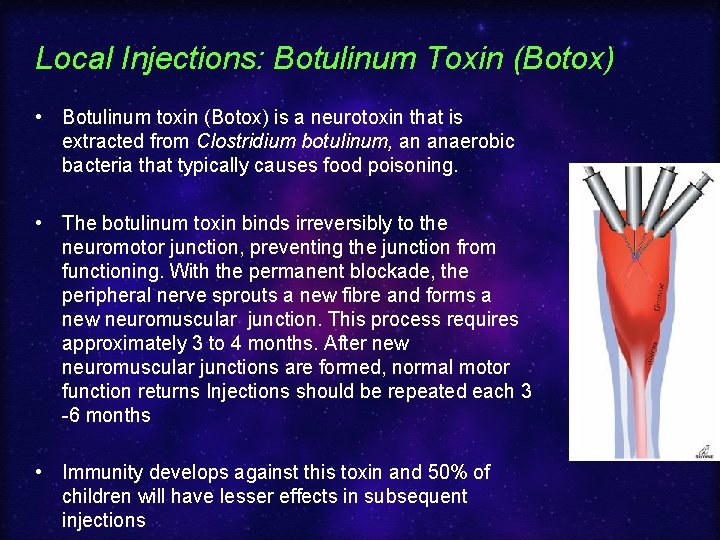
Local Injections: Botulinum Toxin (Botox) • Botulinum toxin (Botox) is a neurotoxin that is extracted from Clostridium botulinum, an anaerobic bacteria that typically causes food poisoning. • The botulinum toxin binds irreversibly to the neuromotor junction, preventing the junction from functioning. With the permanent blockade, the peripheral nerve sprouts a new fibre and forms a new neuromuscular junction. This process requires approximately 3 to 4 months. After new neuromuscular junctions are formed, normal motor function returns Injections should be repeated each 3 -6 months • Immunity develops against this toxin and 50% of children will have lesser effects in subsequent injections
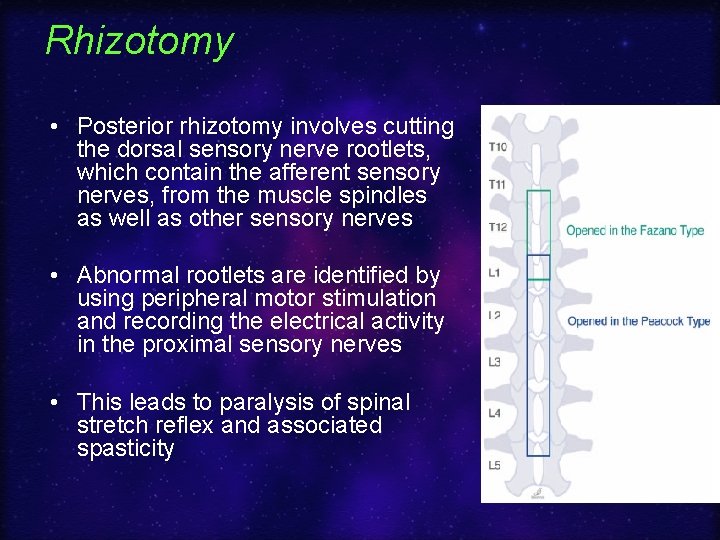
Rhizotomy • Posterior rhizotomy involves cutting the dorsal sensory nerve rootlets, which contain the afferent sensory nerves, from the muscle spindles as well as other sensory nerves • Abnormal rootlets are identified by using peripheral motor stimulation and recording the electrical activity in the proximal sensory nerves • This leads to paralysis of spinal stretch reflex and associated spasticity
Hypotonia treatment • As opposed to spasticity, the treatment options for hypotonia are very limited because hypotonia is a situation where there is not enough tone.
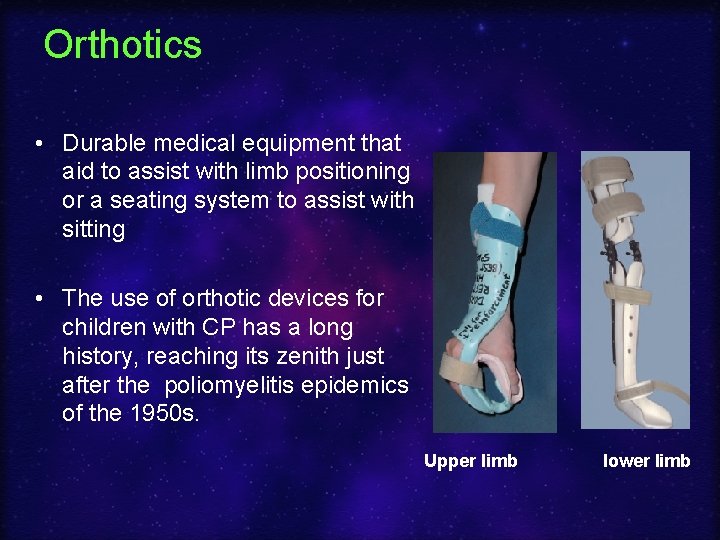
Orthotics • Durable medical equipment that aid to assist with limb positioning or a seating system to assist with sitting • The use of orthotic devices for children with CP has a long history, reaching its zenith just after the poliomyelitis epidemics of the 1950 s. Upper limb lower limb
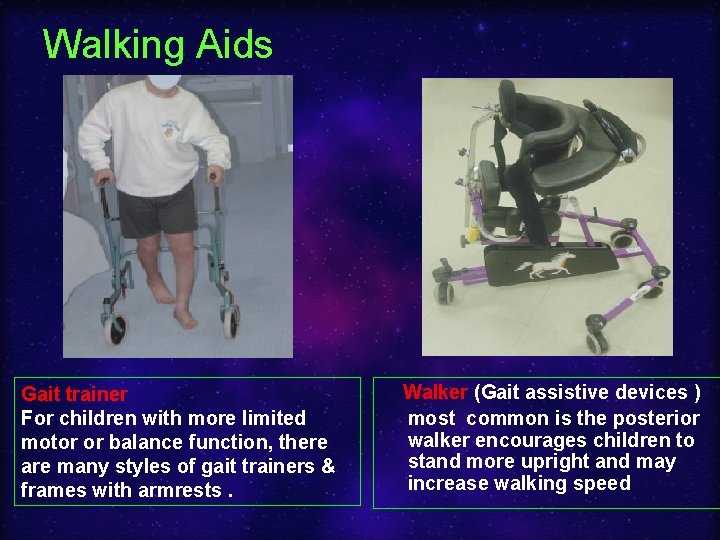
Walking Aids Gait trainer For children with more limited motor or balance function, there are many styles of gait trainers & frames with armrests. Walker (Gait assistive devices ) most common is the posterior walker encourages children to stand more upright and may increase walking speed
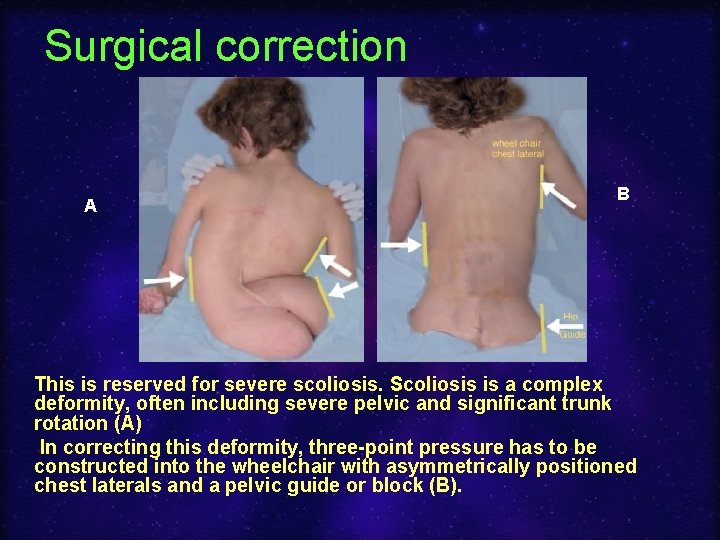
Surgical correction A B This is reserved for severe scoliosis. Scoliosis is a complex deformity, often including severe pelvic and significant trunk rotation (A) In correcting this deformity, three-point pressure has to be constructed into the wheelchair with asymmetrically positioned chest laterals and a pelvic guide or block (B).

Before After

Otherapies • • • Adaptive equipments Acupuncture Hydrotherapy: swimming Sports Hyperbaric oxygen
Finally Cerebral palsy is a lifelong condition that affects the individual & family. Therefore, the goal is to allow CP patient to live life with the least disability
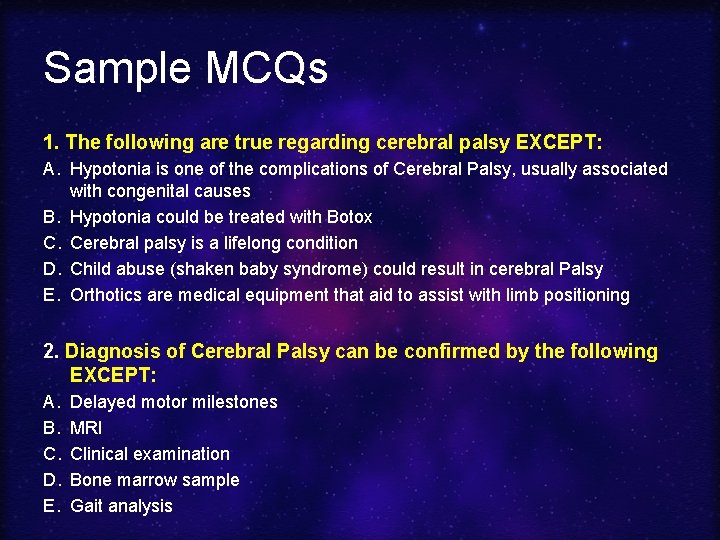
Sample MCQs 1. The following are true regarding cerebral palsy EXCEPT: A. Hypotonia is one of the complications of Cerebral Palsy, usually associated with congenital causes B. Hypotonia could be treated with Botox C. Cerebral palsy is a lifelong condition D. Child abuse (shaken baby syndrome) could result in cerebral Palsy E. Orthotics are medical equipment that aid to assist with limb positioning 2. Diagnosis of Cerebral Palsy can be confirmed by the following EXCEPT: A. B. C. D. E. Delayed motor milestones MRI Clinical examination Bone marrow sample Gait analysis
- Slides: 42