CENTRAL VENOUS CATHETERS ARTERIAL LINES ABG SAMPLING Anatomy
CENTRAL VENOUS CATHETERS, ARTERIAL LINES & ABG SAMPLING
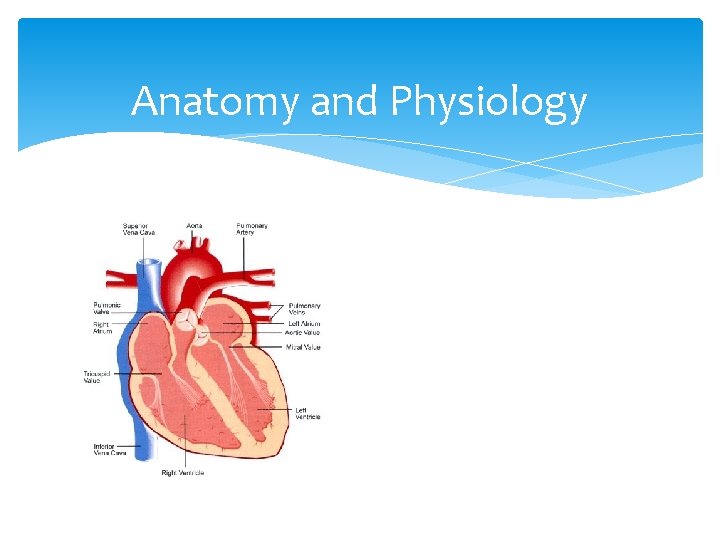
Anatomy and Physiology
Central Venous Catheter/Central Line is: A catheter inserted into a large vein of the body the tip of which lies in or very near to the right atrium
Inserted for: Venous access Infusion of peripherally irritant substances e. g. ? Administration of TPN To measure central venous pressure (preload)
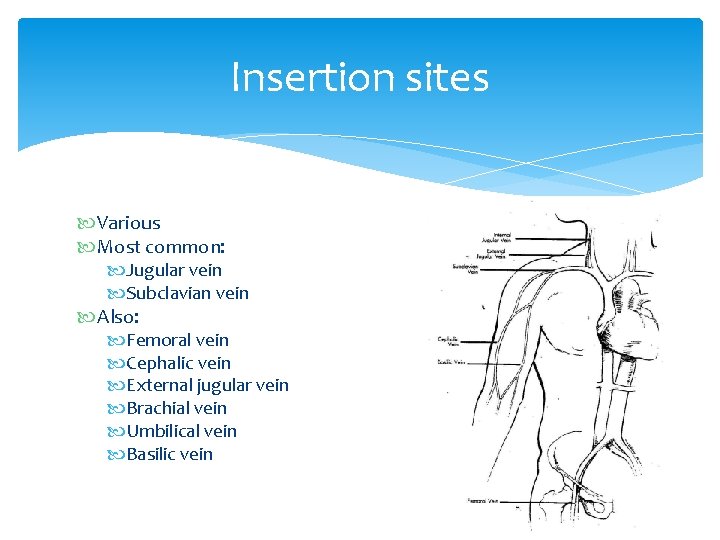
Insertion sites Various Most common: Jugular vein Subclavian vein Also: Femoral vein Cephalic vein External jugular vein Brachial vein Umbilical vein Basilic vein
Insertion Sites Internal jugular vein Right side usually used, lower risk of thrombus formation (due to rapid blood flow rates), arterial involvement & pneumothorax. Risk of air embolism, damage to carotid artery, trachea.
Subclavian vein Lower infection rates, patient comfort, lower risk of thrombus formation (due to rapid blood flow rates), displacement of catheter less likely. Risk of pneumothorax, puncture of subclavian artery, air embolism,
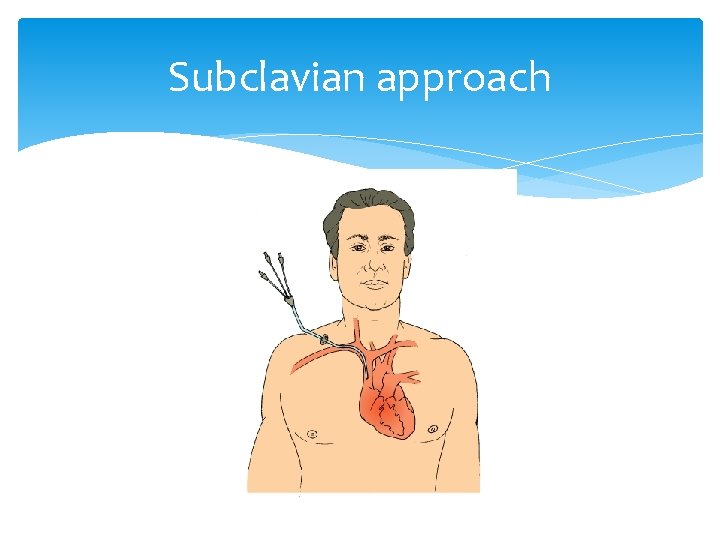
Subclavian approach
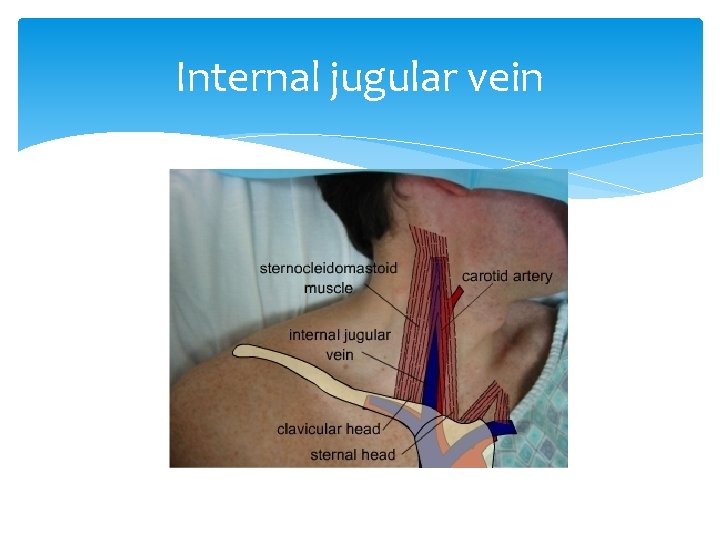
Internal jugular vein
Insertion Aseptic insertion Seldinger technique Trendelenburg position Ultrasound guidance NICE 2002 Chest x-ray Infection risk Multiple lumen catheters versus single lumen catheters - CVP via distal port
Ports & lumens • 3 or 5 lumen. • To monitor CVP, always connect monitoring line to distal port. • Other ports can be used for fluid / drug administration. • N. B. it takes @ 1 ml of fluid to prime the line. • Use bionectors, label & date lines.
Potential complications Infection Bleeding Vascular erosion Pneumothorax Arrhythmias Embolism (air or clot) Perforation of RA Cardiac tamponade
CVAD Bundle Insertion Infection control Review & escalation process Care plan
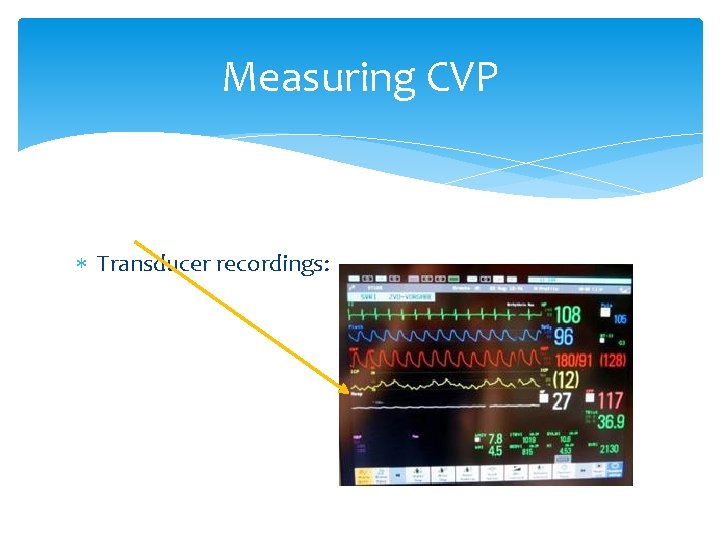
Measuring CVP Transducer recordings:
Central Venous Pressure is: Pressure exerted by the blood within the right atrium Used to measure right atrial filling pressure Guide to fluid loading and fluid replacement……. . but Also influenced by right ventricular function, transthoracic pressure and venous tone. PRELOAD
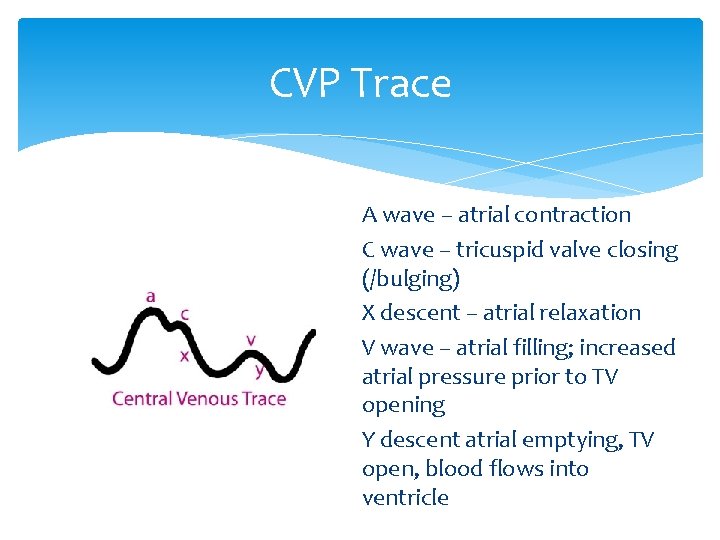
CVP Trace A wave – atrial contraction C wave – tricuspid valve closing (/bulging) X descent – atrial relaxation V wave – atrial filling; increased atrial pressure prior to TV opening Y descent atrial emptying, TV open, blood flows into ventricle
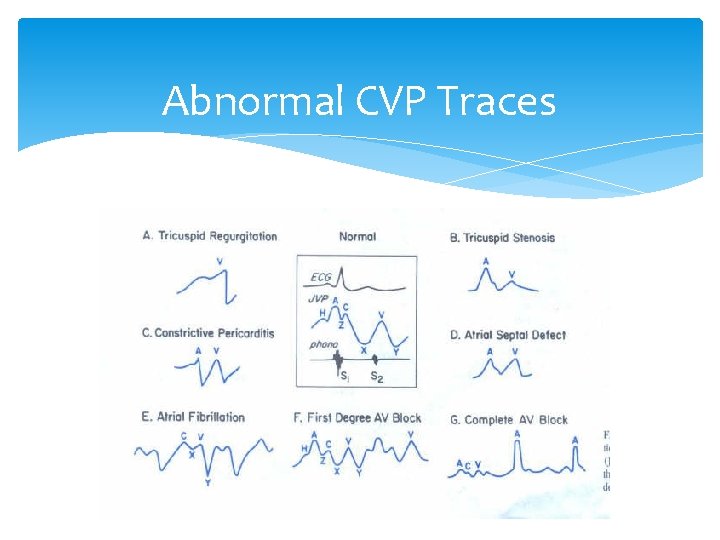
Abnormal CVP Traces
Transducer recorded CVP Central line attached to a fluid filled transducer system Transducer converts physiological pressure into an electronic waveform Readings in mm. Hg, continuous and real time
“Normal Values” 7 -14 mm. Hg (but remember influencing factors) Readings should be taken from phlebostatic axis.
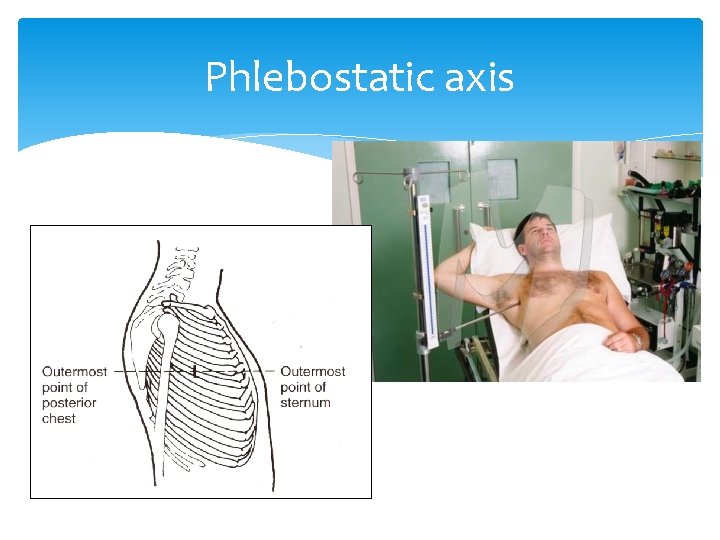
Phlebostatic axis
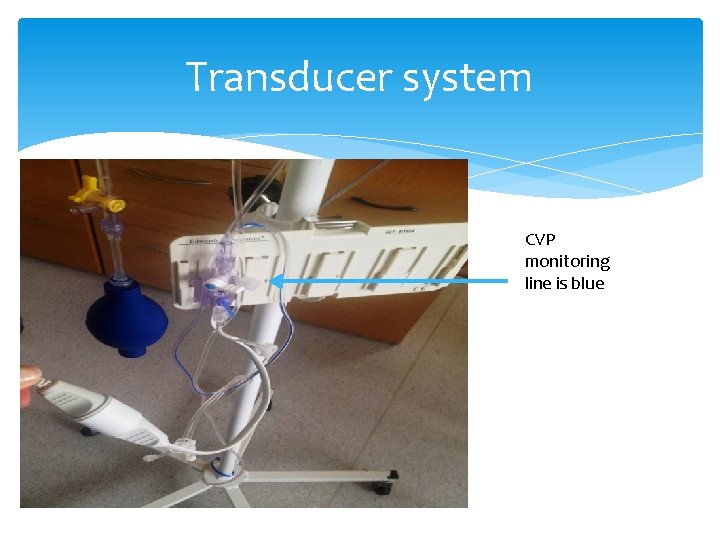
Transducer system CVP monitoring line is blue
“Zeroing” Readings have to be taken from the correct point otherwise they will be inaccurate Correct point is the source of the pressure level of the right atrium External anatomical landmark for right atrium is the phlebostatic axis
Effects of incorrect positioning • If the transducer is too low, this will give us a falsely high CVP reading. • Likewise, if the transducer is too high, this will give us a falsely low reading
Central venous pressure monitoring: limitations Cardiovascular abnormalities: Systemic venoconstriction (elevates CVP, so hypovolaemia may go unnoticed). RV compliance: if RV is constricted, hypertrophied or ischaemic, then CVP may be falsely high. Tricuspid valve disease: CVP will be elevated. Intracardiac shunts (VSD) make clinical interpretation of CVP difficult.
Central venous pressure monitoring: limitations • Increased intrathoracic pressure: PEEP, positive pressure ventilation elevate CVP • LV function: CVP and LV filling pressures correlate in health people, but in LV failure & pulmonary disease, CVP will tell you nothing about LV function
Fluid Challenges Small bolus doses of fluid given Impact on CVP noted CVP increases and stays increased – fluid loaded CVP increases initially then falls – more fluid required
Removal of Line Infection risk – remove as soon as possible Aeseptic procedure Air embolus – head down/flat, valsalva manoevre, air occlusive dressing (24 hours), tip culture and sensitivity.
Arterial Lines and Arterial Blood Gas Sampling
Reasons for arterial sampling Limitations of pulse oximetry Blood gases provide information about: p. H PCO 2 PO 2 Saturation of Hb HCO 3
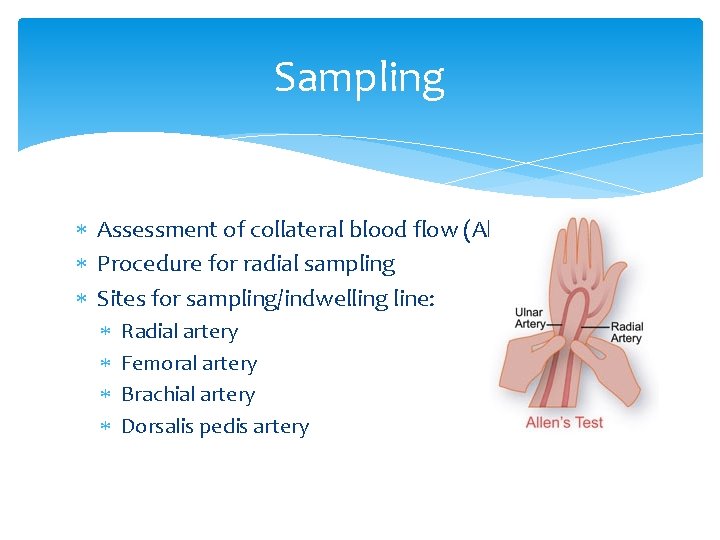
Sampling Assessment of collateral blood flow (Allen Test) Procedure for radial sampling Sites for sampling/indwelling line: Radial artery Femoral artery Brachial artery Dorsalis pedis artery
Allens Test Measuring the flow of arterial blood to the hands. Patient clenches fist for 1 minute Pressure is applied over radial arteries Patient opens fingers of both hands rapidly and colour is examined. Initial pallor should be quickly replaced by rubor (flushed) This may then be repeated using the ulnar artery
Sample management Blood gas sampling syringe Pack in ice if it cannot be analysed immediately (5 mins) Capped Pressure on puncture site Consider indwelling arterial line
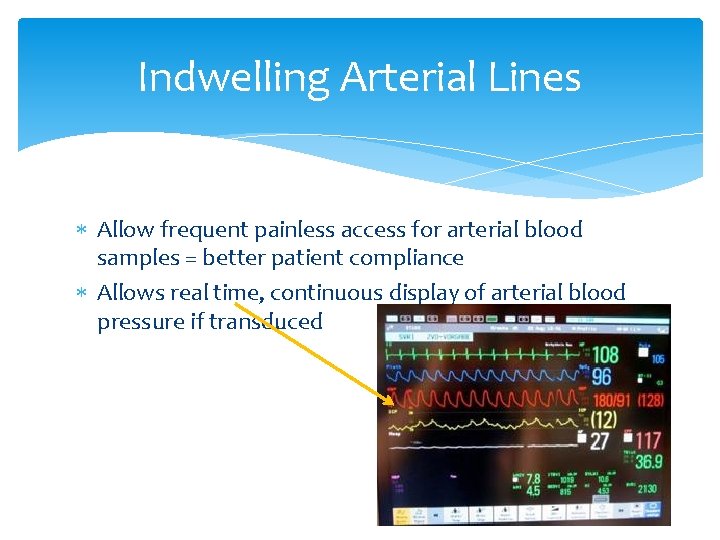
Indwelling Arterial Lines Allow frequent painless access for arterial blood samples = better patient compliance Allows real time, continuous display of arterial blood pressure if transduced
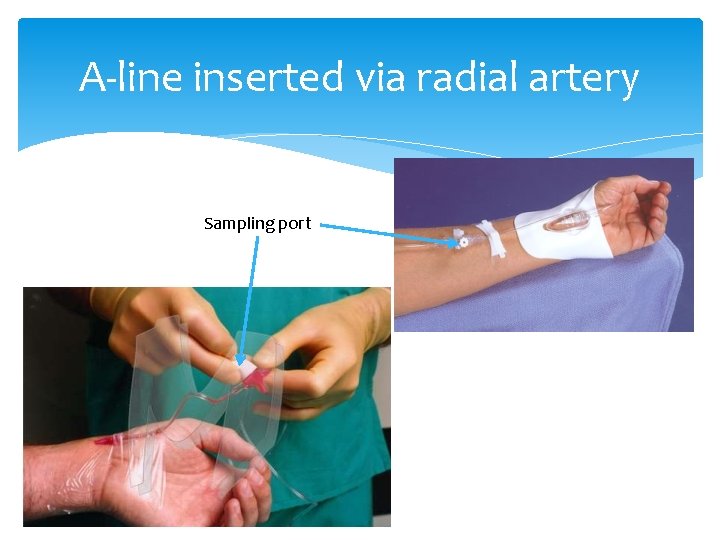
A-line inserted via radial artery Sampling port
Reasons for continuous A-line monitoring Critically ill patients e. g: sepsis, post-arrest, major trauma Patients undergoing major surgery Patients who require serial ABG sampling Acute renal failure Mechanical ventilation
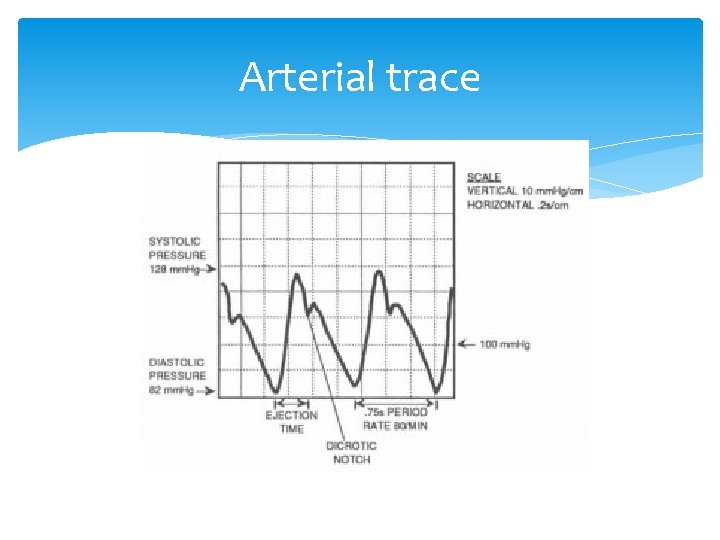
Arterial trace
Fluid filled monitoring systems It is important to keep the flush bag primed to 300 mm. Hg This delivers 3 mls/hr of flush solution & keeps the vessel patent Remember to turn the 3 way tap on the pressure bag off to the pressure bag so that it doesn’t deflate
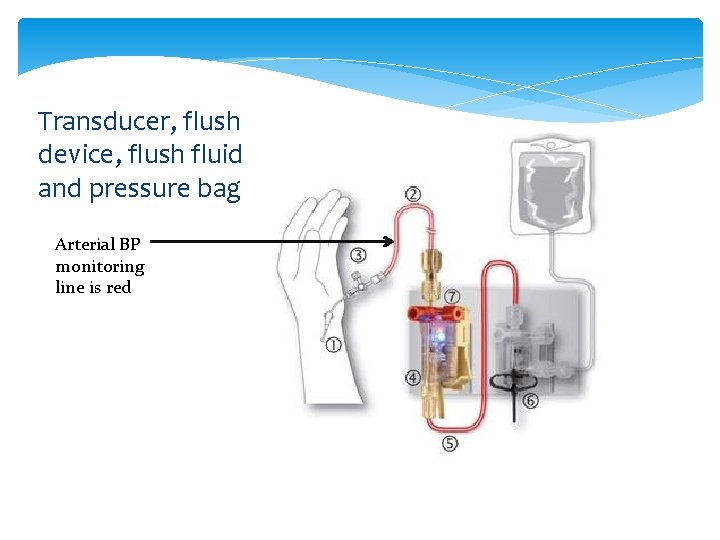
Transducer, flush device, flush fluid and pressure bag Arterial BP monitoring line is red
Zeroing As with CVP, transducer must be level with Rt atrium (@4 th intercostal space [phlebostatic axis]) If transducer is positioned to low, ABP will read falsely high If transducer is positioned incorrectly high, then ABP will read falsely low
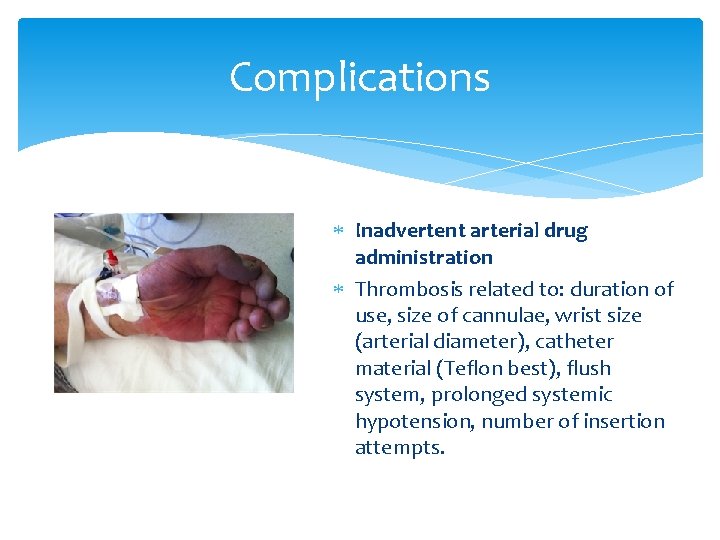
Complications Inadvertent arterial drug administration Thrombosis related to: duration of use, size of cannulae, wrist size (arterial diameter), catheter material (Teflon best), flush system, prolonged systemic hypotension, number of insertion attempts.
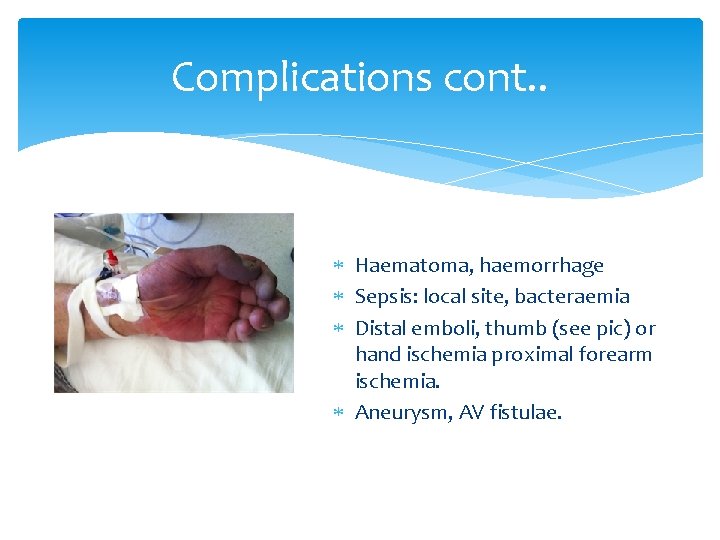
Complications cont. . Haematoma, haemorrhage Sepsis: local site, bacteraemia Distal emboli, thumb (see pic) or hand ischemia proximal forearm ischemia. Aneurysm, AV fistulae.
General troubleshooting • Problem: No waveform Artifact Waveform drifting Unable to flush line Reading too high Reading too low Overdamped waveform
Is the ABP trace accurate? Why does this matter (When in doubt, NIBP)
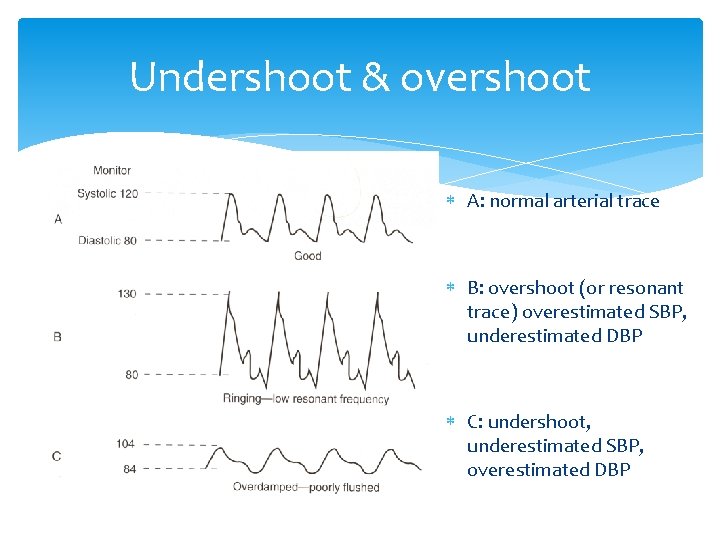
Undershoot & overshoot A: normal arterial trace B: overshoot (or resonant trace) overestimated SBP, underestimated DBP C: undershoot, underestimated SBP, overestimated DBP
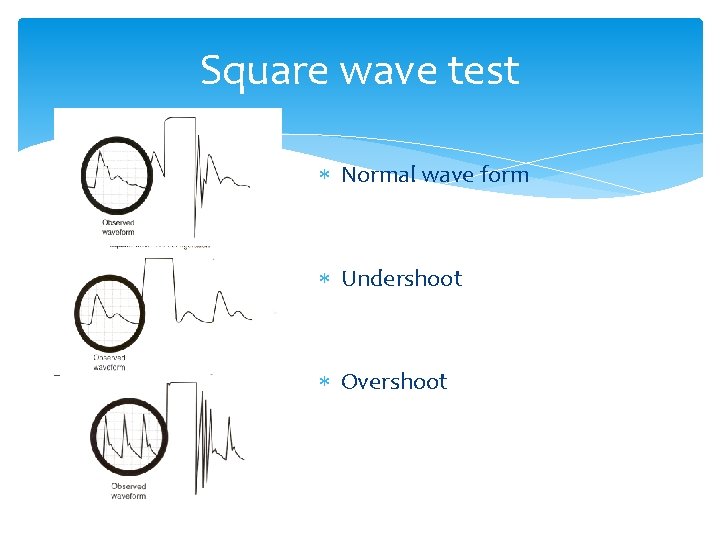
Square wave test Normal wave form Undershoot Overshoot
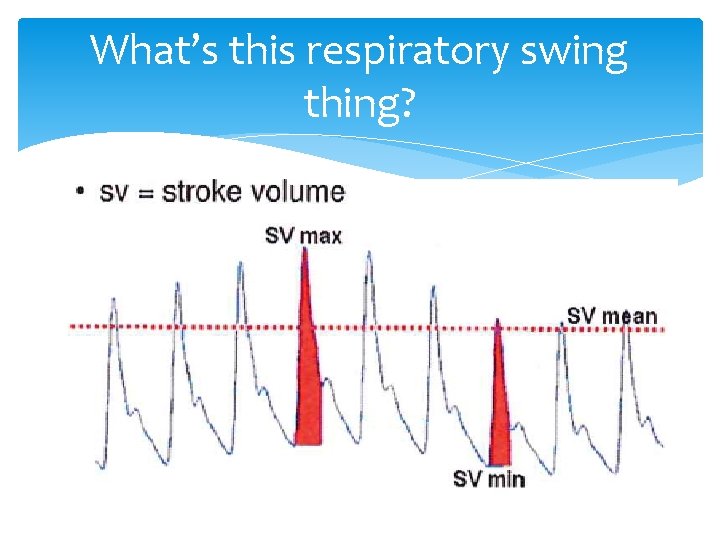
What’s this respiratory swing thing?
Removal of Art line • Wash hands, put on gloves, gather equipment. • Remove dressing and sutures (if present). • Apply firm pressure to insertion site, pull out line gently. • Apply manual pressure (this may take up to 10 mins or longer), elevate limb if desired to aid haemostasis. • Apply small occlusive dressing, continue to observe for leakage periodically.
- Slides: 47