Central nervous system infections 3 quick cases Case







- Slides: 64
Central nervous system infections
3 quick cases….
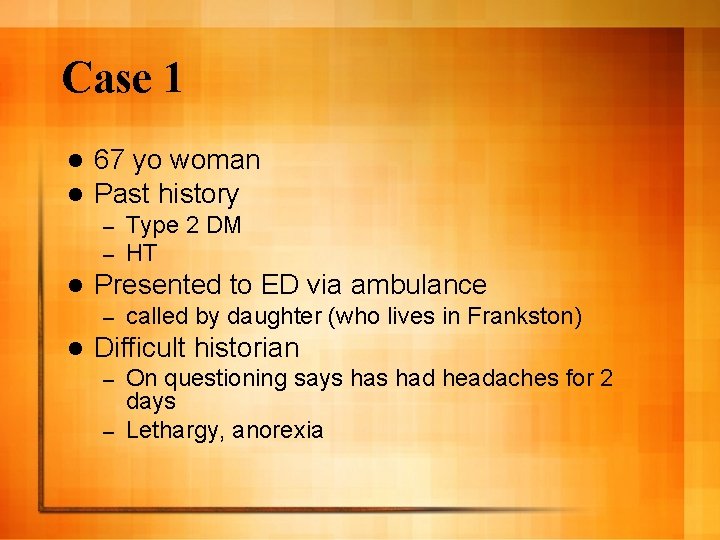
Case 1 l l 67 yo woman Past history – – l Presented to ED via ambulance – l Type 2 DM HT called by daughter (who lives in Frankston) Difficult historian On questioning says had headaches for 2 days – Lethargy, anorexia –
Case 1 l On – – – examination Drowsy but eye opens to voice Disoriented to time but not place Febrile T 37. 8 Chest clear FWT leucocyte, nitrite positive
Case 1 l Differential diagnosis?
Case 1 l Daughter noticed patient to be ‘vague’ and saying strange things over the phone last 4 days l Didn’t mention to daughter about headache l Telephoned her at 3. 30 am that morning asking her where her cat was
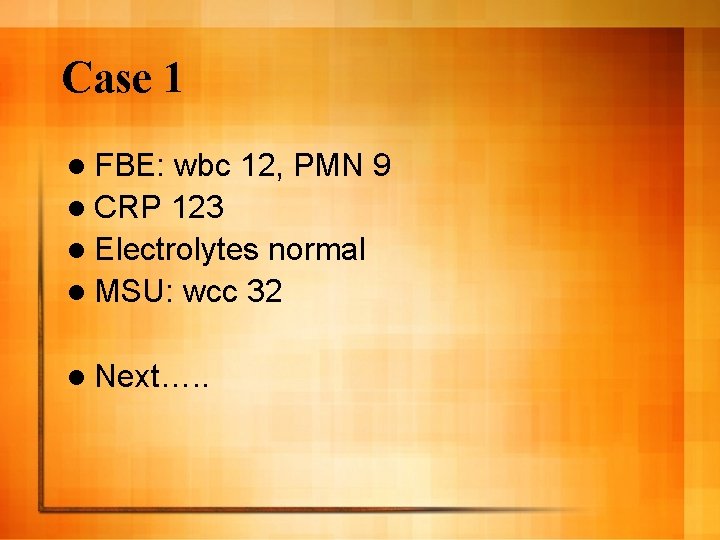
Case 1 l FBE: wbc 12, PMN 9 l CRP 123 l Electrolytes normal l MSU: wcc 32 l Next…. .
Case 1 l CT brain normal l LP: wcc 15, 100% lymphocytes – rcc 3 – Protein 0. 35 g/l – Glucose normal –
Case 1 l Diagnosis?

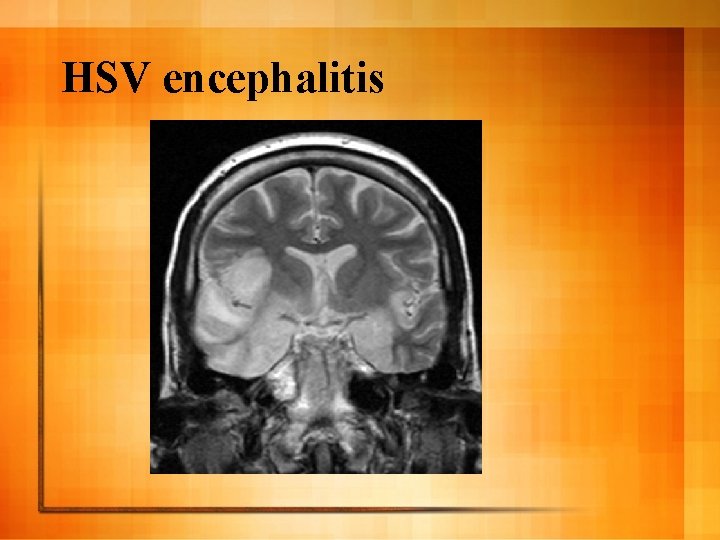
Case 1 l After d/w ID started on iv aciclovir and benzylpenicillin l 2 days later HSV PCR on CSF positive l MRI brain:
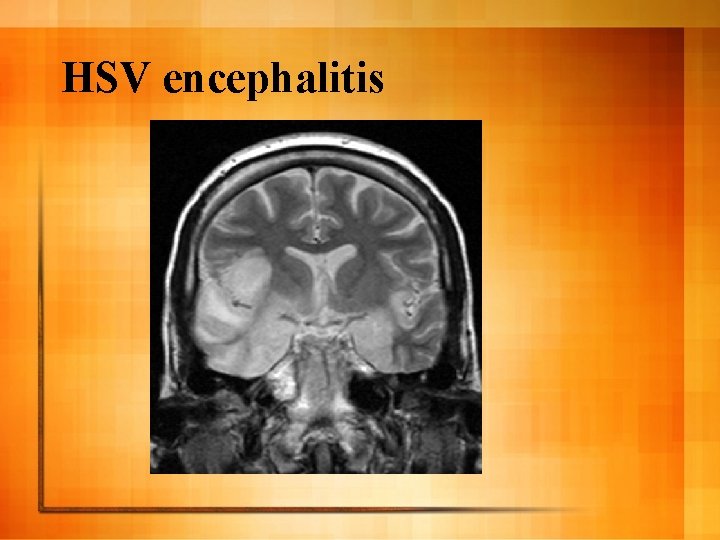
HSV encephalitis
Case 2 27 yo female l Brought in to ED 10 pm Saturday night by boyfriend l Complaining of severe headache, present 2 days. Supposed to go to Sydney for the weekend but cancelled Friday because ‘felt like crap’. Assoc nausea, lethargy. l Feeling hot and flushed l
Case 2 l Examination – – – Lying curled up in dark cubicle Not opening her eyes when talking to you but able to answer all questions Got up to go to toilet just after seen T 36. 8 Pulse 88, BP 115/80 Warm, well perfused
Case 2 l Differential diagnosis? l What next?
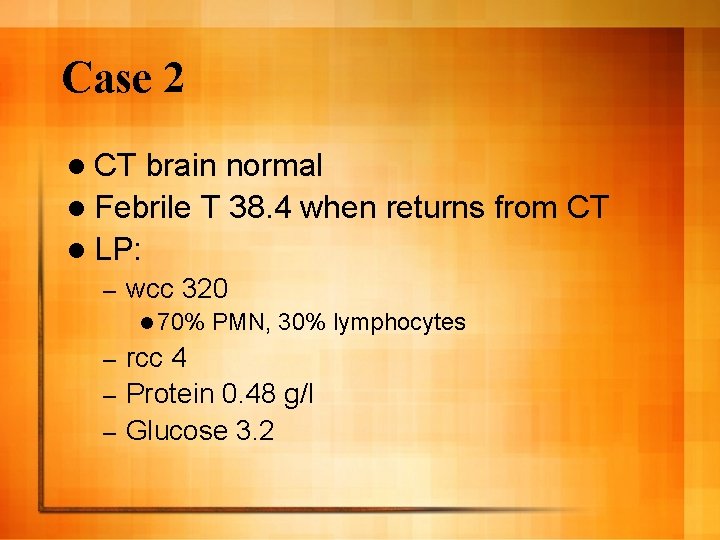
Case 2 l CT brain normal l Febrile T 38. 4 when returns from CT l LP: – wcc 320 l 70% PMN, 30% lymphocytes rcc 4 – Protein 0. 48 g/l – Glucose 3. 2 –
Case 2 l Diagnosis?
Case 2 l No antibiotics given l Admitted for analgesia, hydration l Recovered quickly, home Monday morning l Enterovirus PCR negative
Case 3 l 16 yo boy l Presents with 5 day history of headaches, fevers l ‘Bad’ headaches. Some relief with paracetamol but getting worse so presented to ED l URTI week prior but this resolved mostly
Case 3 l On examination alert and oriented, no neck stiffness. No neuro signs. Febrile T 38. 1 l FBE: wbc 11, PMN 8 l LFT, U+E normal l CRP 300
Case 3 l Differential diagnosis? l What next?
Case 3 l Sent home with analgesia, GP letter l 36 hrs later bld cultures flagged positive for GPC l What to do?
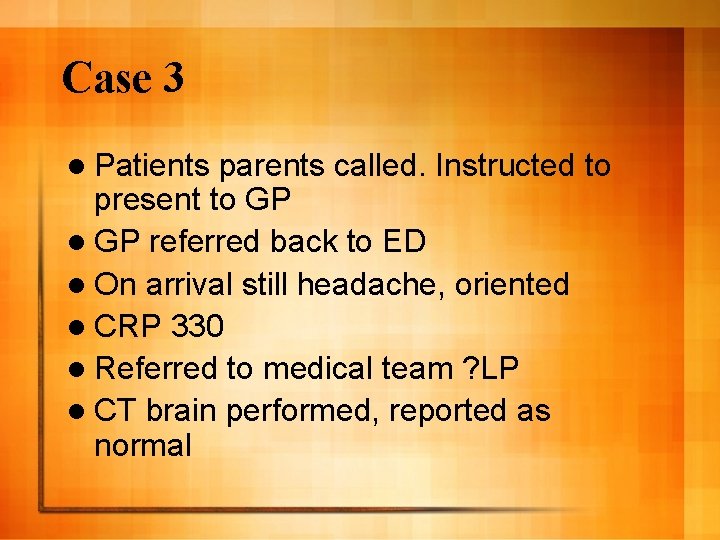
Case 3 l Patients parents called. Instructed to present to GP l GP referred back to ED l On arrival still headache, oriented l CRP 330 l Referred to medical team ? LP l CT brain performed, reported as normal
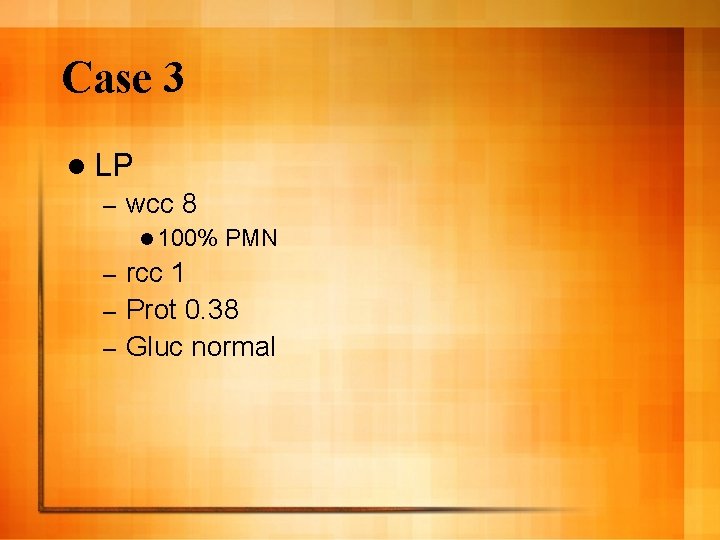
Case 3 l LP – wcc 8 l 100% PMN rcc 1 – Prot 0. 38 – Gluc normal –
Case 3 l Significance of this result?
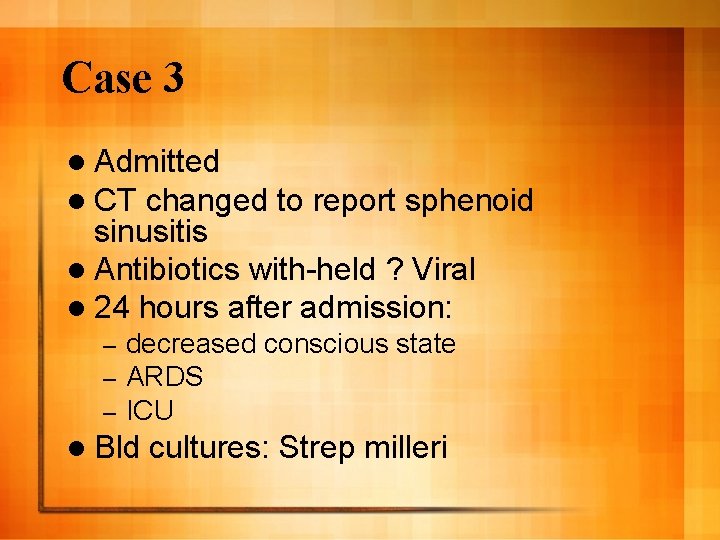
Case 3 l Admitted l CT changed to report sphenoid sinusitis l Antibiotics with-held ? Viral l 24 hours after admission: – – – decreased conscious state ARDS ICU l Bld cultures: Strep milleri
Case 3 l Despite broad-spectrum antibiotics and ENT surgery pt deteriorated

CNS infections l Headache Meningitis – Para-meningeal infection – l Confusion/seizure/focal signs Encephalitis – Brain abscess – l **History of symptoms at beginning of illness and duration crucial in differential diagnosis
Meningitis l Acute meningitis Bacterial – Viral – l ‘Chronic’ meningitis Tuberculosis – Fungal (Cryptococcal) – Non-infectious (malignant, sarcoid) –
Acute bacterial meningitis
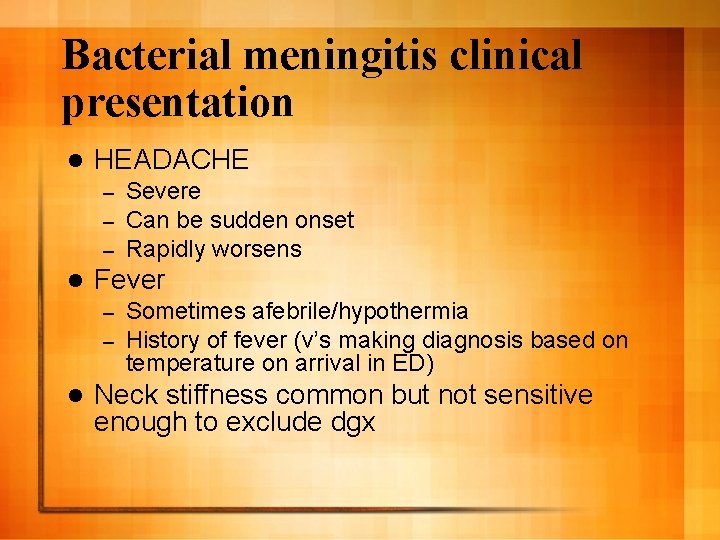
Bacterial meningitis clinical presentation l HEADACHE – – – l Fever – – l Severe Can be sudden onset Rapidly worsens Sometimes afebrile/hypothermia History of fever (v’s making diagnosis based on temperature on arrival in ED) Neck stiffness common but not sensitive enough to exclude dgx
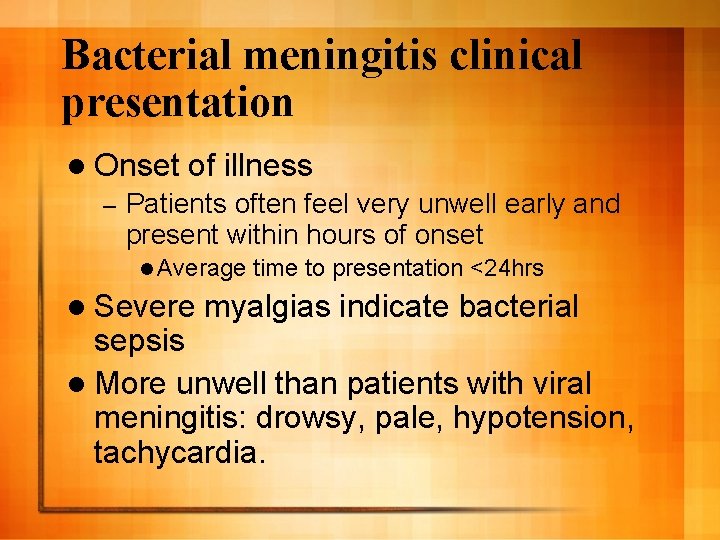
Bacterial meningitis clinical presentation l Onset – of illness Patients often feel very unwell early and present within hours of onset l Average l Severe time to presentation <24 hrs myalgias indicate bacterial sepsis l More unwell than patients with viral meningitis: drowsy, pale, hypotension, tachycardia.
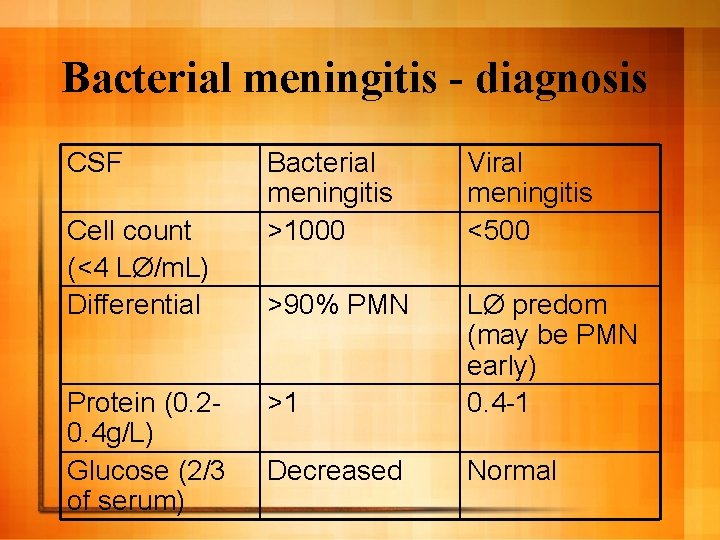
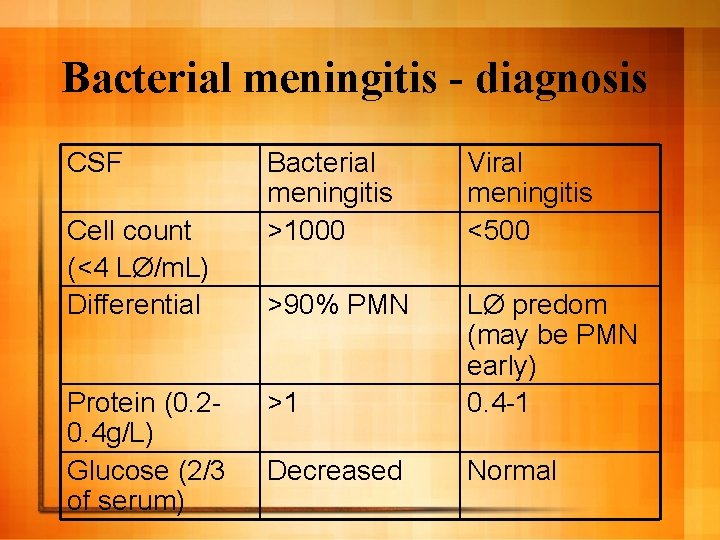
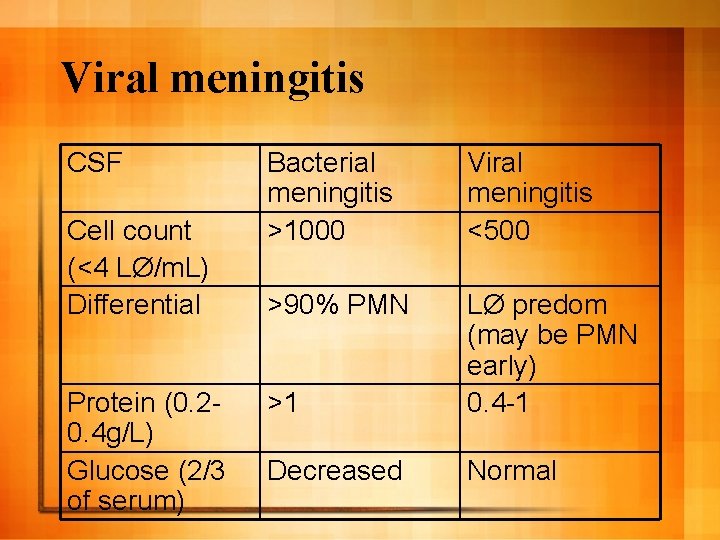
Bacterial meningitis - diagnosis CSF Cell count (<4 LØ/m. L) Differential Protein (0. 20. 4 g/L) Glucose (2/3 of serum) Bacterial meningitis >1000 Viral meningitis <500 >90% PMN >1 LØ predom (may be PMN early) 0. 4 -1 Decreased Normal
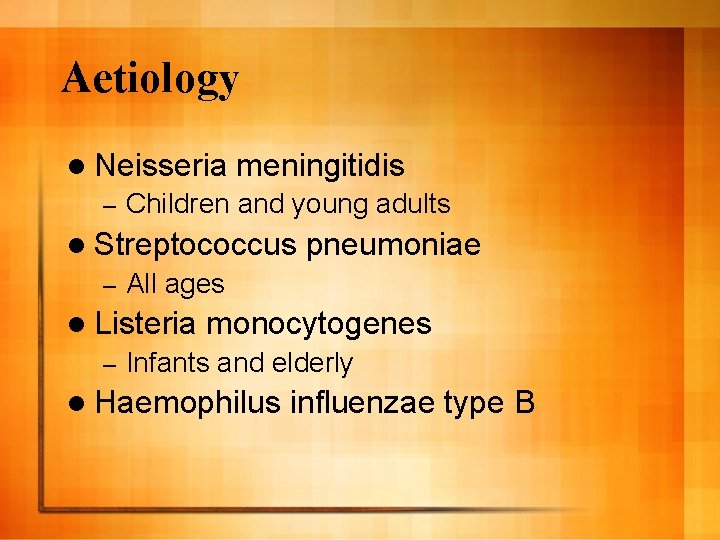
Aetiology l Neisseria – meningitidis Children and young adults l Streptococcus – All ages l Listeria – pneumoniae monocytogenes Infants and elderly l Haemophilus influenzae type B
N. meningitidis

N. meningitidis
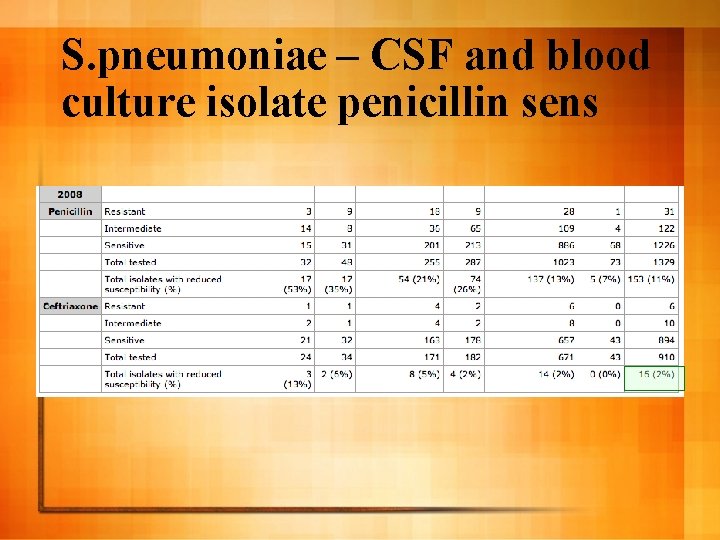
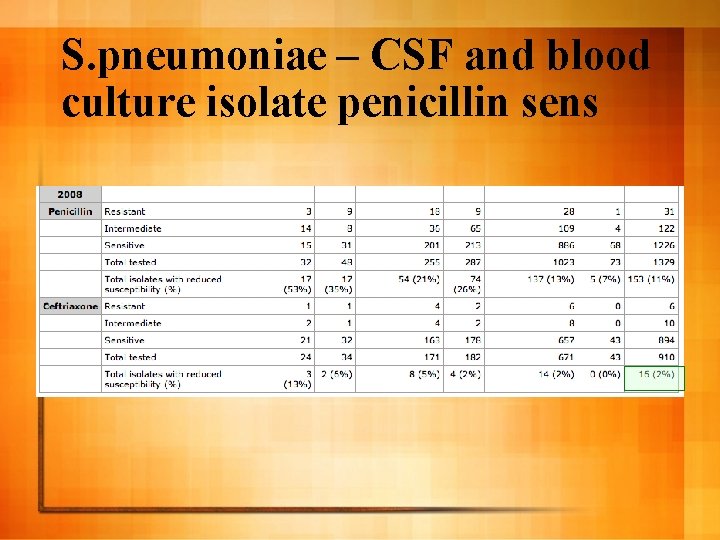
S. pneumoniae – CSF and blood culture isolate penicillin sens
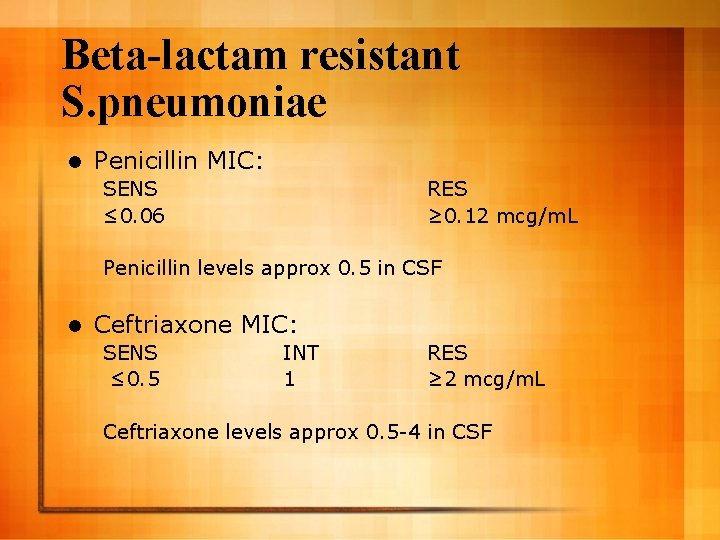
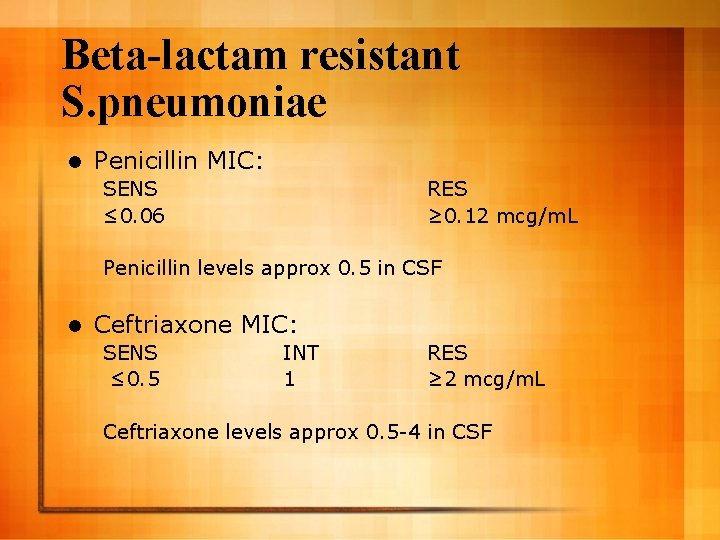
Beta-lactam resistant S. pneumoniae l Penicillin MIC: SENS ≤ 0. 06 RES ≥ 0. 12 mcg/m. L Penicillin levels approx 0. 5 in CSF l Ceftriaxone MIC: SENS ≤ 0. 5 INT 1 RES ≥ 2 mcg/m. L Ceftriaxone levels approx 0. 5 -4 in CSF
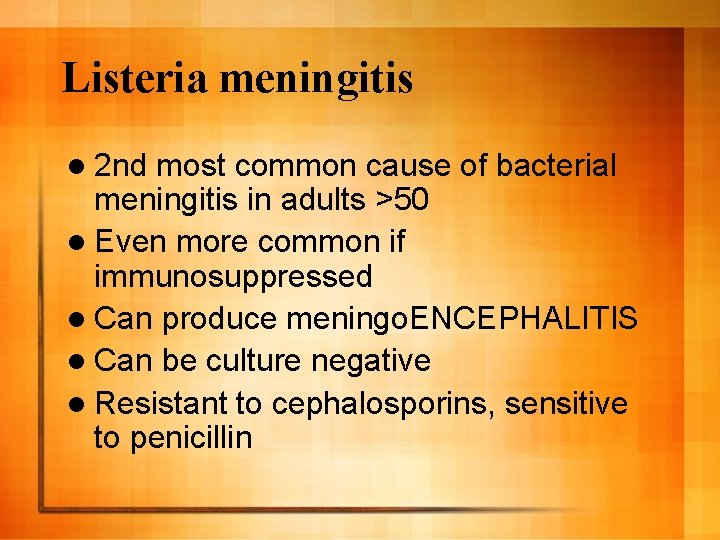
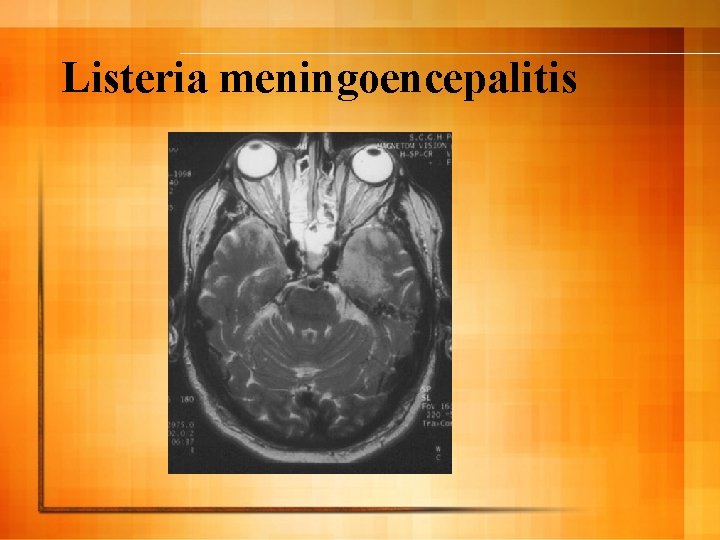
Listeria meningitis l 2 nd most common cause of bacterial meningitis in adults >50 l Even more common if immunosuppressed l Can produce meningo. ENCEPHALITIS l Can be culture negative l Resistant to cephalosporins, sensitive to penicillin
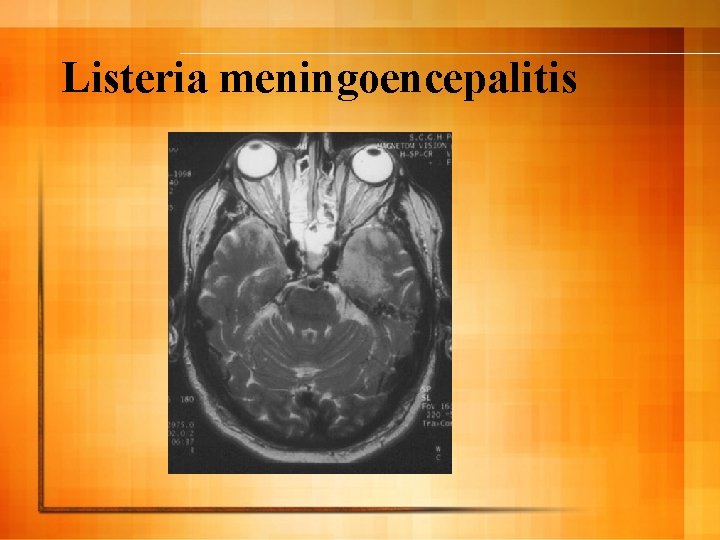
Listeria meningoencepalitis
Management of possible bacterial meningitis l Focus is ensuring rapid administration of treatment whilst attempting diagnosis Lumbar puncture – Antibiotics – Corticosteroids – CT brain –

Management of possible bacterial meningitis l Delay in antibiotics leads to greater mortality and worse neurological outcome – Delay >3 hrs from time of arrival: mortality OR 14 (Auburtin et al, Crit Care Med. 2006)
Management of possible bacterial meningitis l Factors associated with delay in antibiotics Afebrile at presentation – Triage to physician time – Time from LP to abx – CT brain!! – l Sequence of CT then LP then abx

Management of possible bacterial meningitis l Is a CT brain required before LP in adults with suspected meningitis? – – 5% of patients will have mass effect All of those with significant mass effect: l Immunosuppressed l Age >60 l Focal neuro/seizures/decreased consciousness/papilloedema – In the absence of these features safe to perform LP without CT brain (Hasbun NEJM 2001)
Management of possible bacterial meningitis l Sequence l 1. of management either: LP then abx OR l 2. Abx then CT then LP l NOT CT then LP then abx
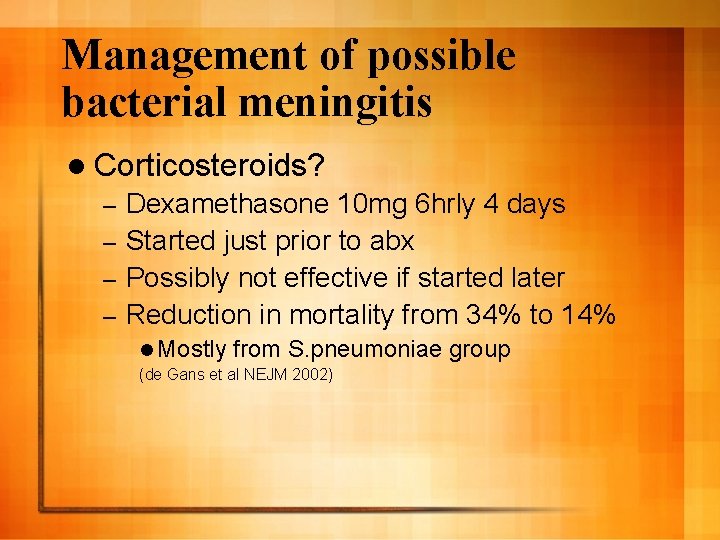
Management of possible bacterial meningitis l Corticosteroids? Dexamethasone 10 mg 6 hrly 4 days – Started just prior to abx – Possibly not effective if started later – Reduction in mortality from 34% to 14% – l Mostly from S. pneumoniae group (de Gans et al NEJM 2002)
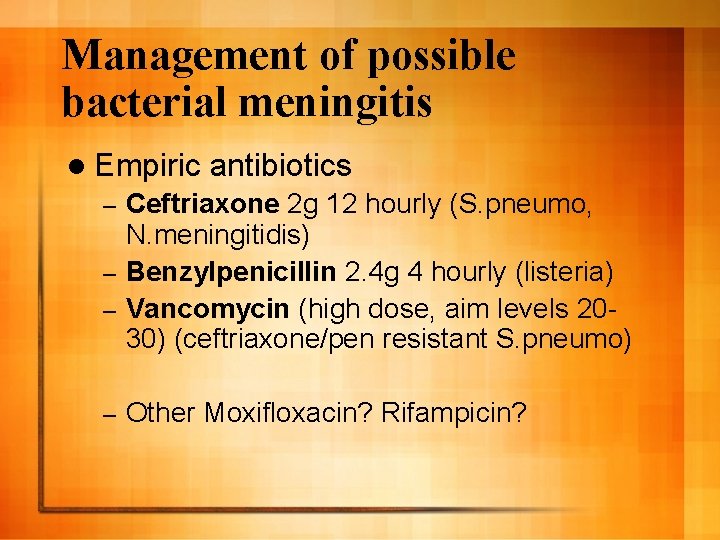
Management of possible bacterial meningitis l Empiric antibiotics Ceftriaxone 2 g 12 hourly (S. pneumo, N. meningitidis) – Benzylpenicillin 2. 4 g 4 hourly (listeria) – Vancomycin (high dose, aim levels 2030) (ceftriaxone/pen resistant S. pneumo) – – Other Moxifloxacin? Rifampicin?

Viral meningitis
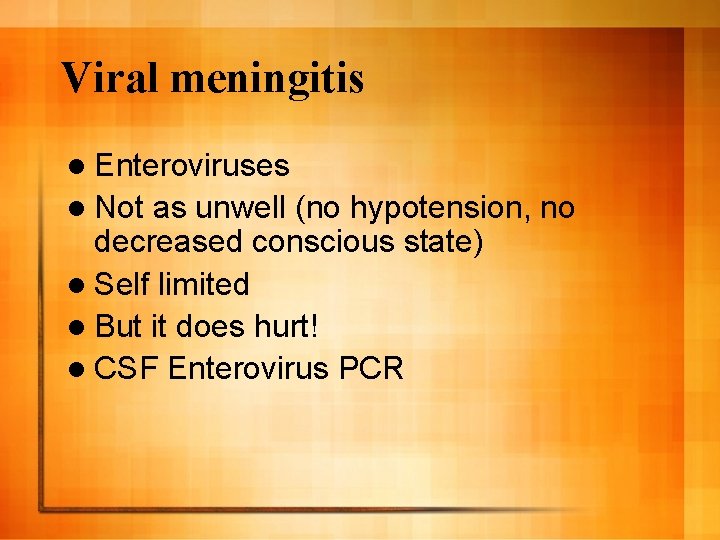
Viral meningitis l Enteroviruses l Not as unwell (no hypotension, no decreased conscious state) l Self limited l But it does hurt! l CSF Enterovirus PCR
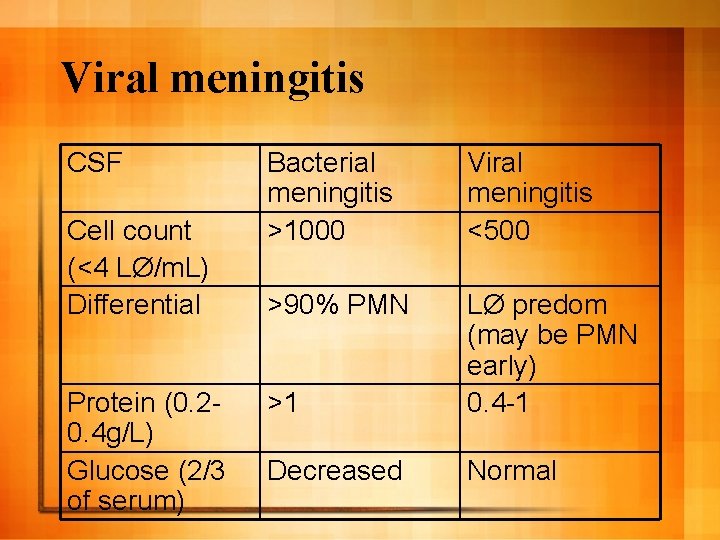
Viral meningitis CSF Cell count (<4 LØ/m. L) Differential Protein (0. 20. 4 g/L) Glucose (2/3 of serum) Bacterial meningitis >1000 Viral meningitis <500 >90% PMN >1 LØ predom (may be PMN early) 0. 4 -1 Decreased Normal
Viral meningitis l There is a differential diagnosis of ‘sterile’ meningitis with acute presentation Tb, cryptococcal – Parameningeal infections – HIV, mumps, rat-lungworm – l Measure pressure and get plenty of CSF (most people can tolerate 10 -20 ml). Lots of tests to do!
Cranial parameningeal infections
Cranial parameningeal infections l Result from sinusitis Mastoid, frontal most common – Sphenoid and ethmoid more difficult to diagnose – l Osteomyelitis -> epidural -> subdural -> brain abscess l Suspect when history of sinus symptoms then worsening headache
Cranial parameningeal infections l Diagnose – with imaging Need MRI for ethmoid/sphenoid sinuses l CSF variable. Increased wcc 15 - to >1000 l Management: Broad spectrum abx covering S. aureus, Strep, anaerobes – Urgent surgical referral –
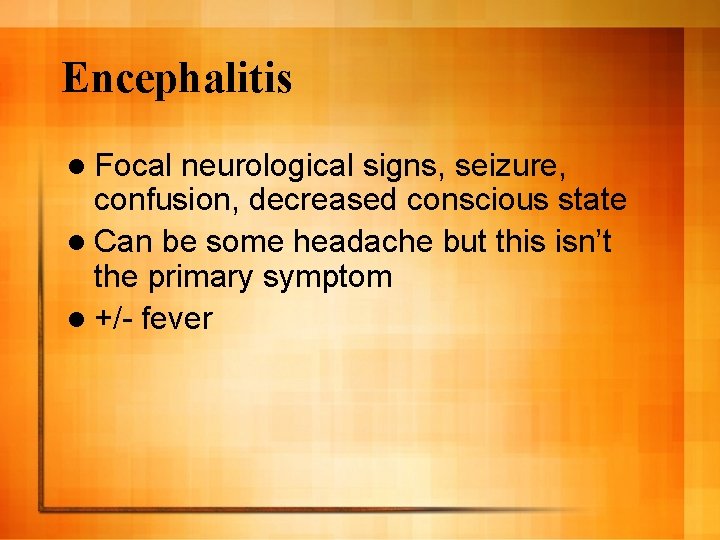
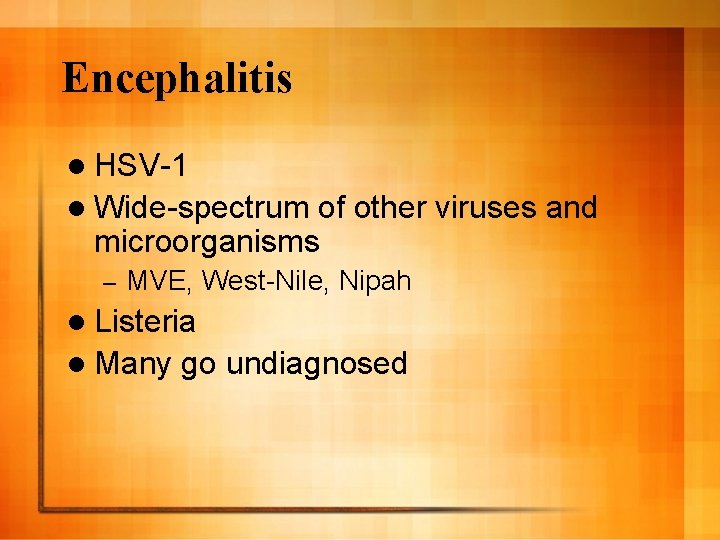
Encephalitis
Encephalitis l Focal neurological signs, seizure, confusion, decreased conscious state l Can be some headache but this isn’t the primary symptom l +/- fever
Encephalitis l HSV-1 l Wide-spectrum of other viruses and microorganisms – MVE, West-Nile, Nipah l Listeria l Many go undiagnosed
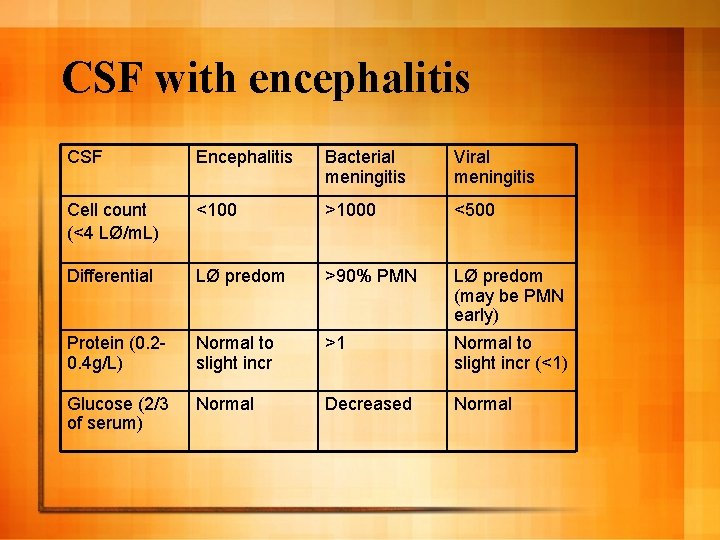
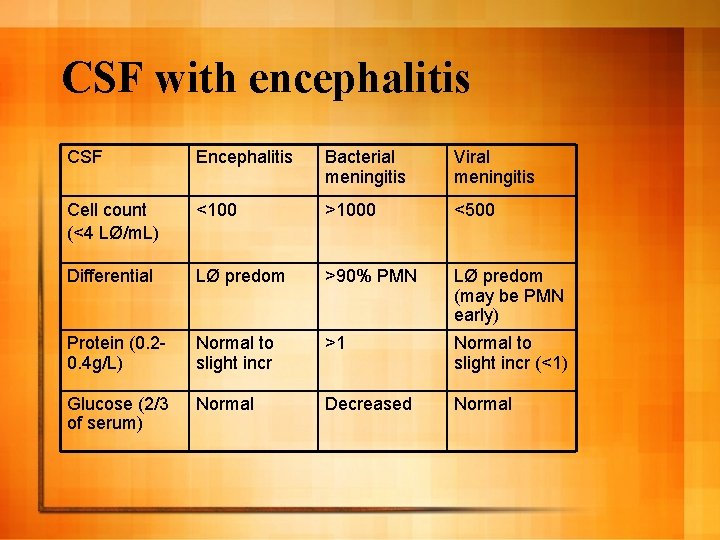
CSF with encephalitis CSF Encephalitis Bacterial meningitis Viral meningitis Cell count (<4 LØ/m. L) <100 >1000 <500 Differential LØ predom >90% PMN LØ predom (may be PMN early) Protein (0. 20. 4 g/L) Normal to slight incr >1 Normal to slight incr (<1) Glucose (2/3 of serum) Normal Decreased Normal
HSV Encephalitis l HSV PCR very sensitive and specific. Can be negative early in course of disease
HSV encephalitis l iv aciclovir l Prognosis depends on degree of impairment at presentation
Brain abscess Focal signs, fever and headache l Presentation often more prolonged l Days to weeks – But can present with eg seizure in previously well person – l Source Contiguous – Haematogenous: lung abscess, dental – l l Strep milleri group, S. aureus Management: surgery and prolonged abx
Central nervous system infections Precise history essential to diagnosis l CSF findings very helpful in confirming diagnosis l Medical (or surgical) emergency l Prioritise patients and act quickly – When suspect bacterial meningitis don’t let imaging delay therapy – Don’t forget steroids and vanc for bacterial meningitis l Call ID team!! l

Ms IN
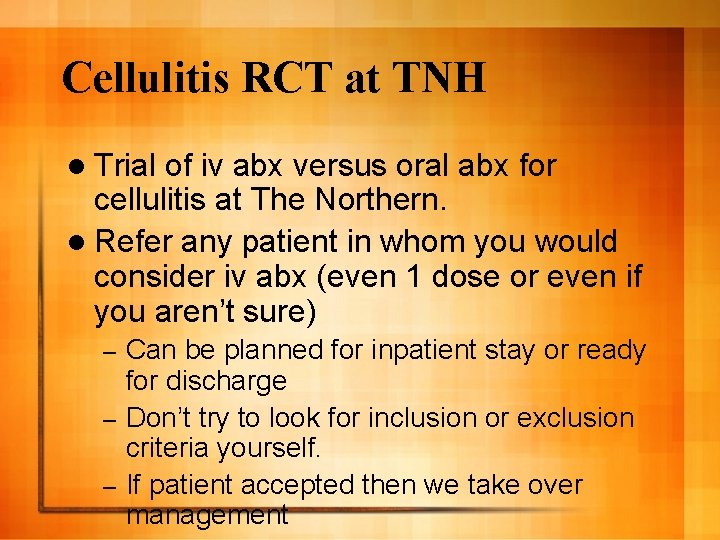
Cellulitis RCT at TNH l Trial of iv abx versus oral abx for cellulitis at The Northern. l Refer any patient in whom you would consider iv abx (even 1 dose or even if you aren’t sure) Can be planned for inpatient stay or ready for discharge – Don’t try to look for inclusion or exclusion criteria yourself. – If patient accepted then we take over management –