Centers for Medicare Medicaid Services CMS PROGRAM INTEGRITY




- Slides: 34
Centers for Medicare & Medicaid Services CMS PROGRAM INTEGRITY EFFORTS 2003 By: Jim Bryant CMS, Boston Regional Office Division of Financial Management
Upcoming CMS Program Integrity Changes Increasing Focus on Medical Review Hiring more clinical staff Increased outreach to providers Increased use of data analysis to tailor program integrity efforts
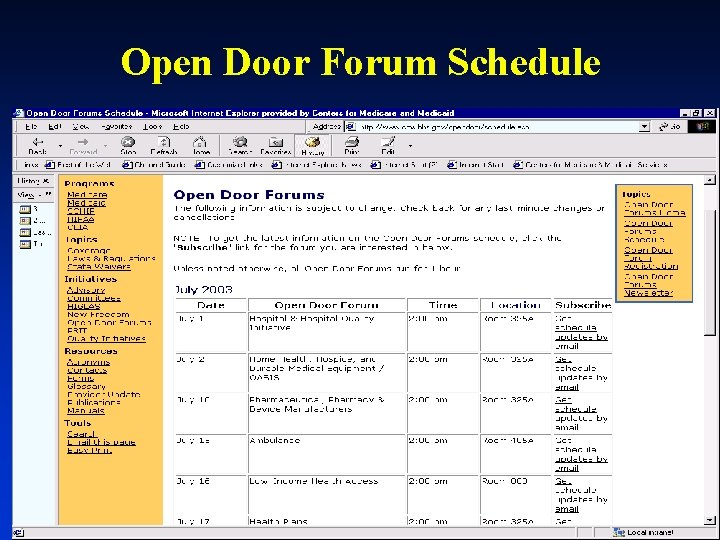
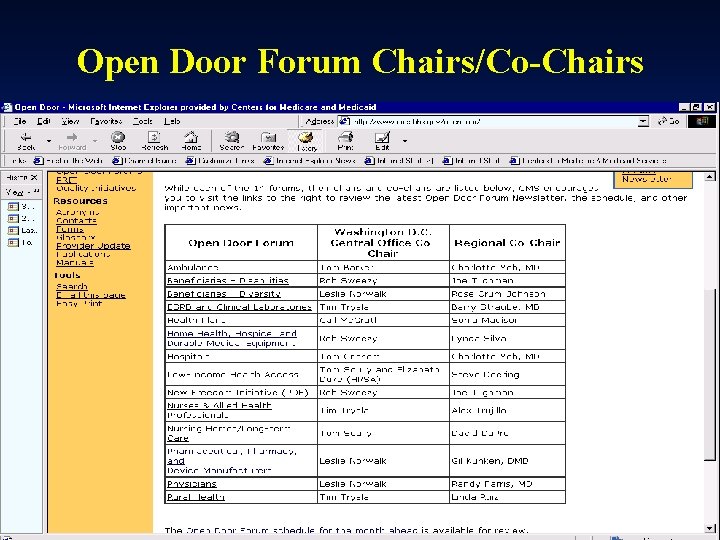
Open Door Forum Schedule
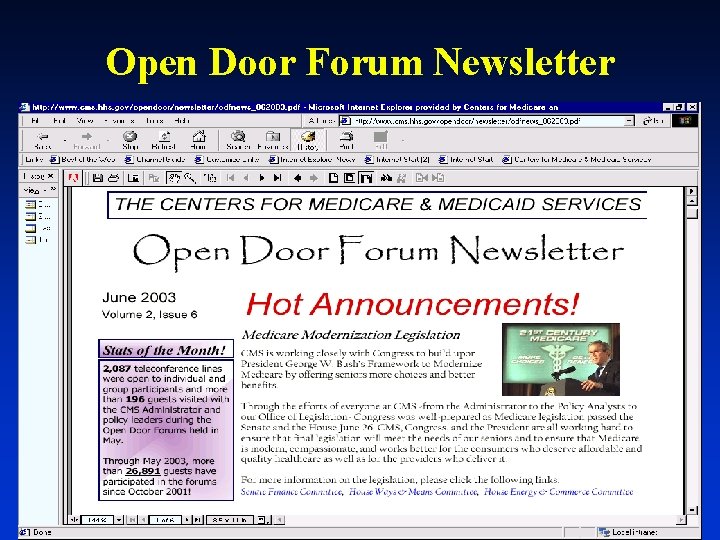
Open Door Forum Newsletter
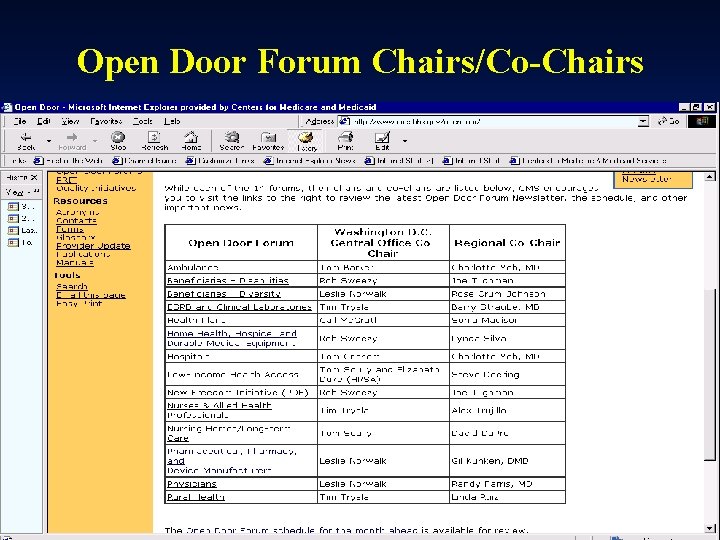
Open Door Forum Chairs/Co-Chairs
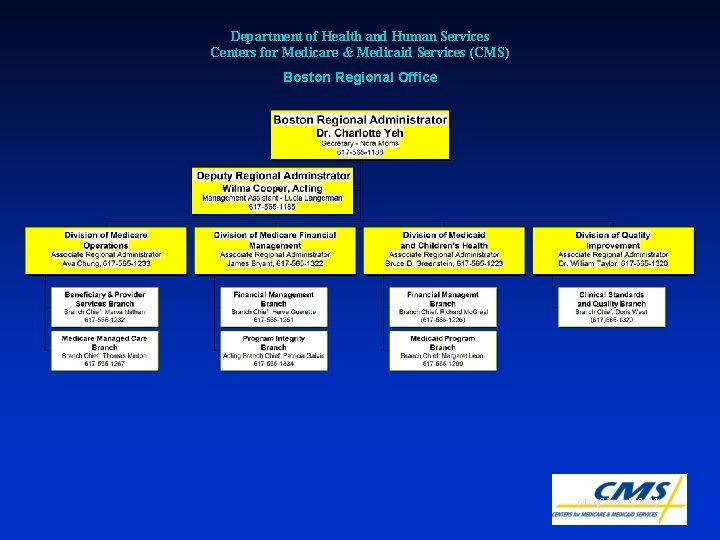
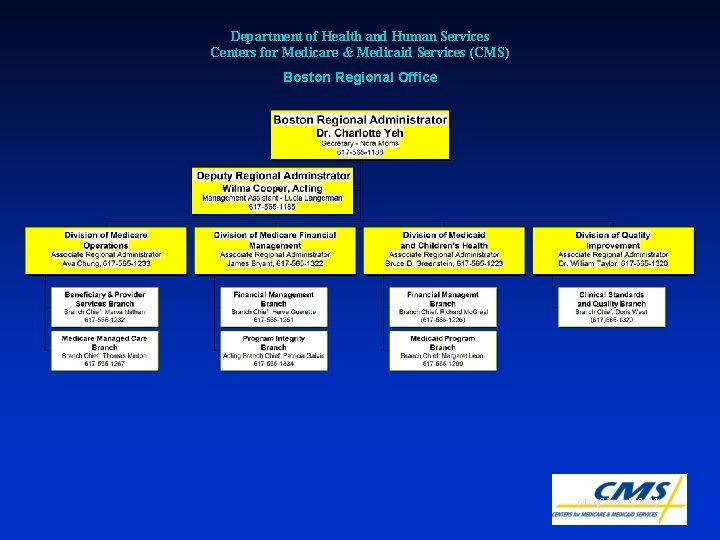
Department of Health and Human Services Centers for Medicare & Medicaid Services (CMS) Boston Regional Office (As of June 8, 2003)

Regional Office Contacts l Jim Bryant, ARA for Medicare Financial Management ä l Reimbursement/Cost Report Lead - Jim Menza ä l jmenza@cms. hhs. gov 617. 565. 1219 mwidmer@cms. hhs. gov LTC PPS - Diana Giacalone ä l 617. 565. 1278 OPPS - Marcia Widmer ä l 617. 565. 1331 jbryant 1@cms. hhs. gov 617. 565. 1205 dgiacalone@cms. hhs. gov Psych PPS - Gil Mason ä 617. 565. 1238 gmason@cms. hhs. gov
Progressive Corrective Action l To identify and target problem providers l Hallmarks: u all decisions are data driven u emphasis on education u allow for varying review levels
Progressive Corrective Action (continued) l Determining Appropriate Actions u Primary Consideration ä Error Rate Calculation u Secondary Considerations ä Mitigating Circumstances ä Aggravating Circumstances u Review Level Increases as Level of Concern Increases
Progressive Corrective Action (continued) l Mitigating Circumstances u Favorable Self Audits u Voluntary Disclosures u Voluntary Compliance Plan u Favorable Appeals Decisions
Progressive Corrective Action (continued) l Aggravating Circumstances u High percentage of claims with errors u History of prior billing problems u Adverse findings from other reviews u Significant number of beneficiary complaints
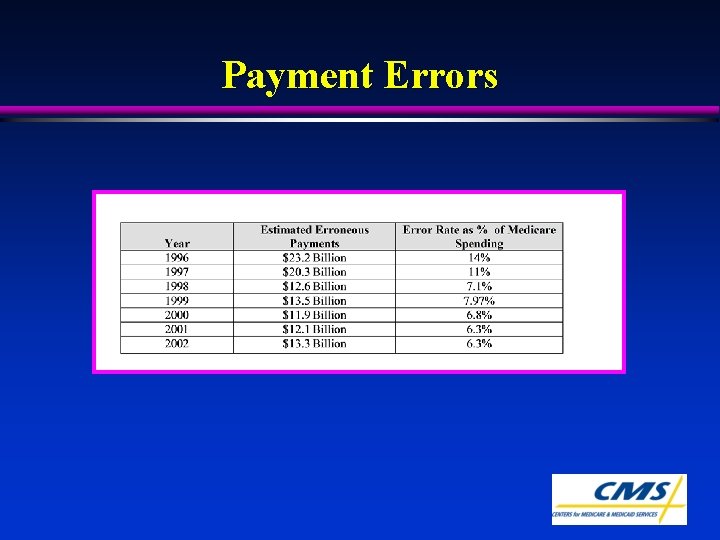
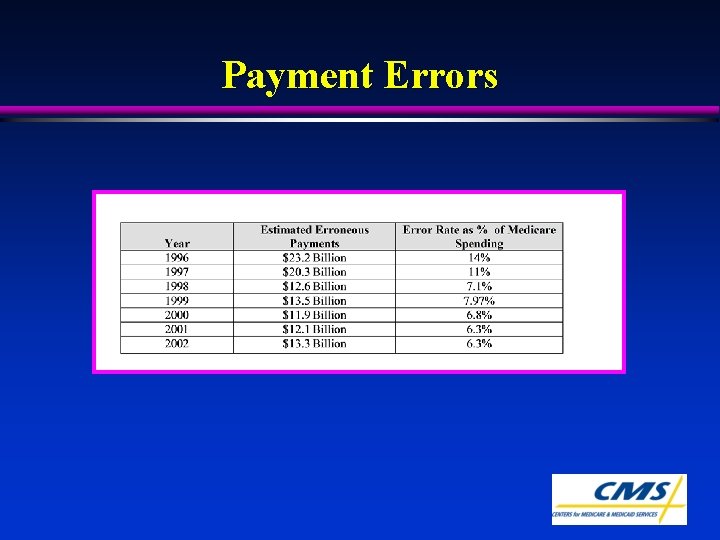
Payment Errors
Comprehensive Error Rate Testing (CERT) Program l CMS has entered into a contract with Advance. Med under its MIP contracting authority. l The purpose of the contract is to: u produce a national contractor specific and benefit category specific paid claim error rate
CERT Program (cont. ) l Independent reviewers will review statistically valid samples of claims as they are processed l Results: u National paid claims error rate u Error rate for Medicare contractors nationwide
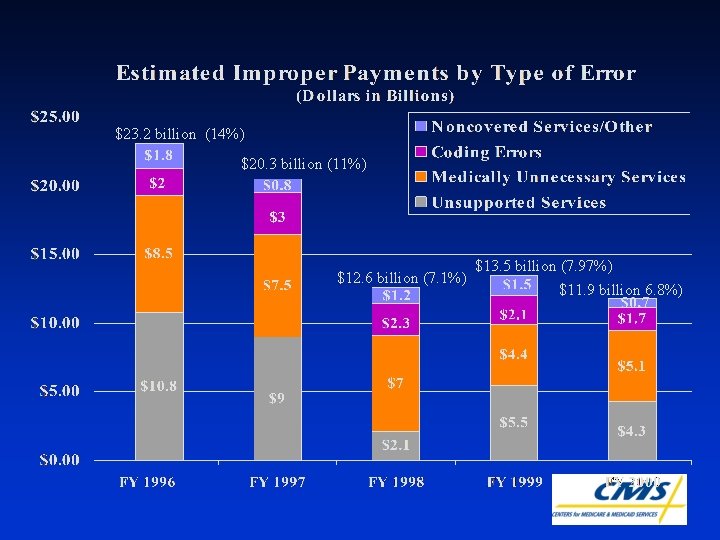
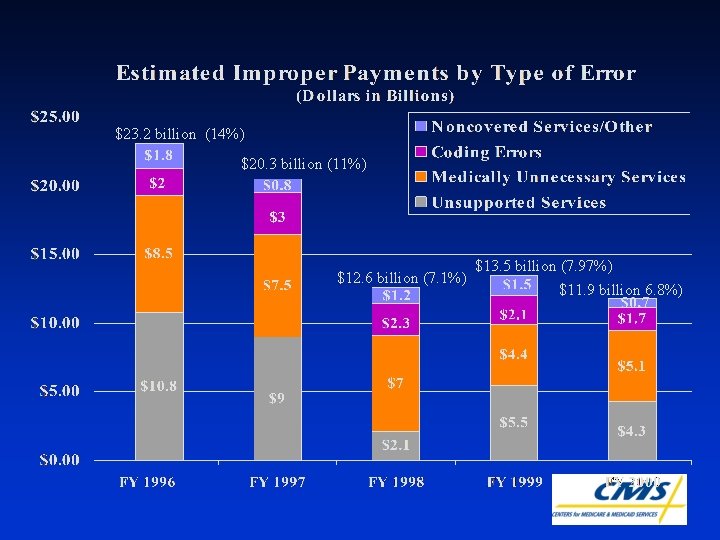
$23. 2 billion (14%) $20. 3 billion (11%) $12. 6 billion (7. 1%) $13. 5 billion (7. 97%) $11. 9 billion 6. 8%)
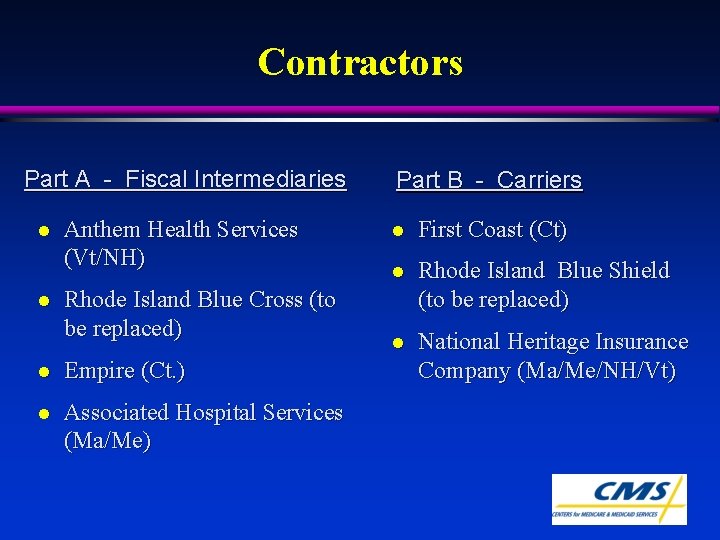
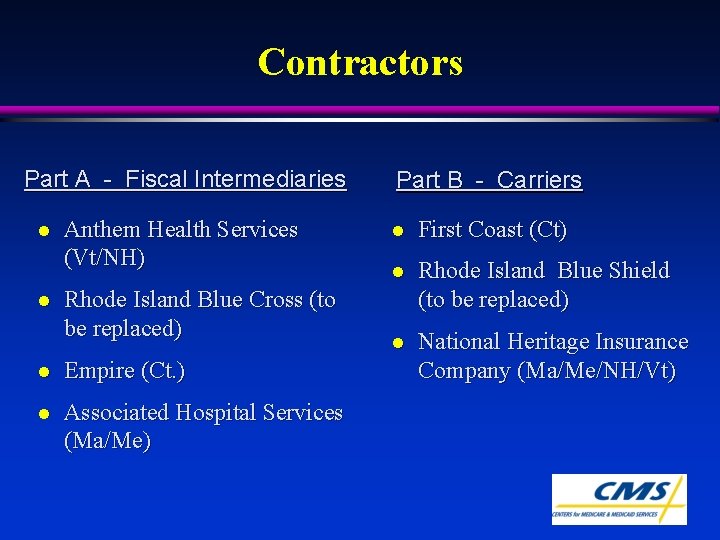
Contractors Part A - Fiscal Intermediaries l l Anthem Health Services (Vt/NH) Rhode Island Blue Cross (to be replaced) l Empire (Ct. ) l Associated Hospital Services (Ma/Me) Part B - Carriers l First Coast (Ct) l Rhode Island Blue Shield (to be replaced) l National Heritage Insurance Company (Ma/Me/NH/Vt)
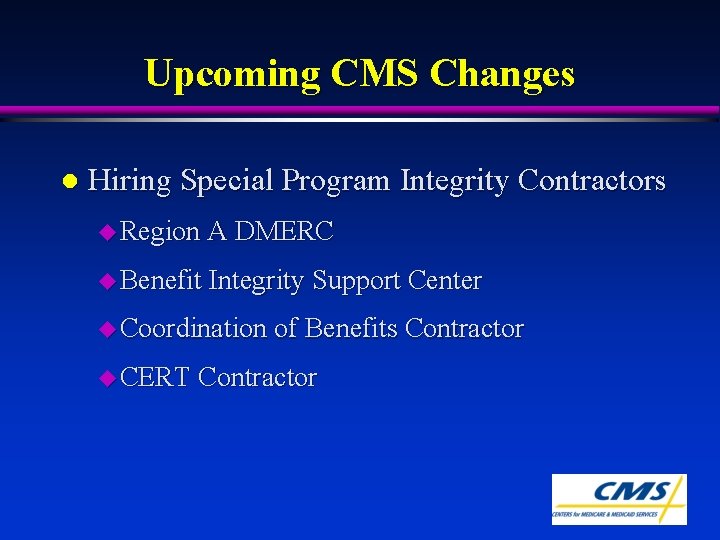
Upcoming CMS Changes l Hiring Special Program Integrity Contractors u Region A DMERC u Benefit Integrity Support Center u Coordination of Benefits Contractor u CERT Contractor
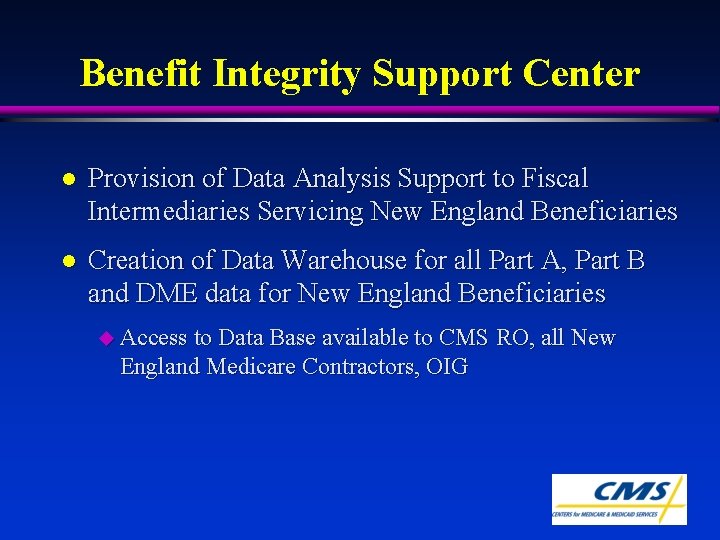
Benefit Integrity Support Center l Provision of Data Analysis Support to Fiscal Intermediaries Servicing New England Beneficiaries l Creation of Data Warehouse for all Part A, Part B and DME data for New England Beneficiaries u Access to Data Base available to CMS RO, all New England Medicare Contractors, OIG
Region A DMERC l Responsible for Fraud and Medical Review functions of DME claims for Region A (the Northeast) u Will increase data analysis capabilities
Coordination of Benefits Contractor l CMS hired GHI as a contractor to identify health insurance coverage of Medicare beneficiaries and to coordinate the payment process centrally. l GHI investigates coverage and maintains a data base on this l GHI then assigns contractors as “leads” to respond to MSP case requests
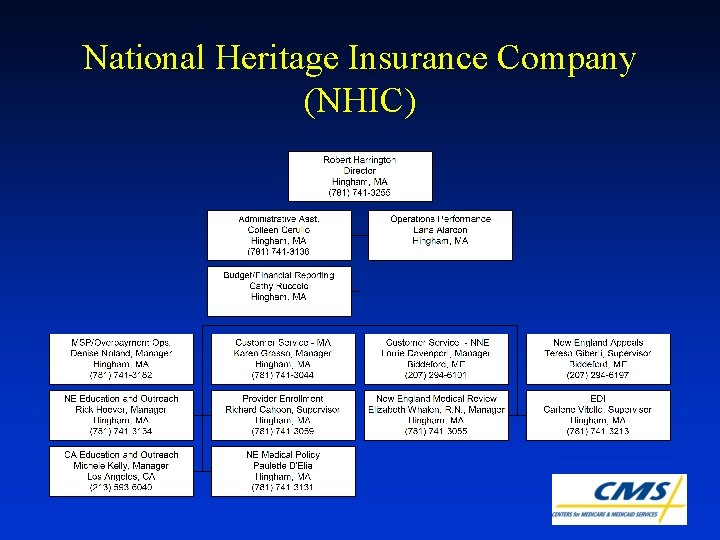
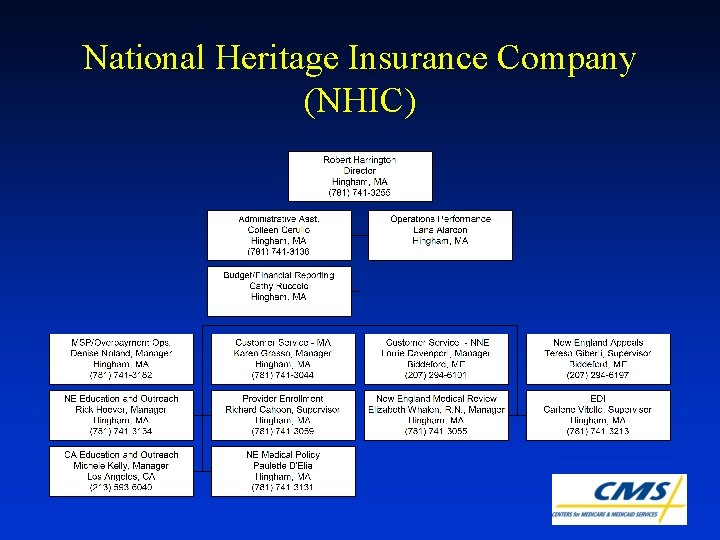
National Heritage Insurance Company (NHIC)

National Heritage Insurance Company NHIC General Provider Inquiries (877) 567 -3130 NHIC Website: medicarenhic. com

National Heritage Insurance Company Provider Education and Outreach Rick Hoover, Manager Maine Brenda Bedard (207) 294 -6104 brenda. bedard@eds. com (781) 741 -3134 New Hampshire rick. hoover@eds. com Jane Ann Fuller Medical Review (603) 228 -6552 janeann. fuller@eds. com Betty Whalen, Manager Vermont (781) 741 -3055 Robin Coletta betty. whalen@eds. com (802) 878 -3873
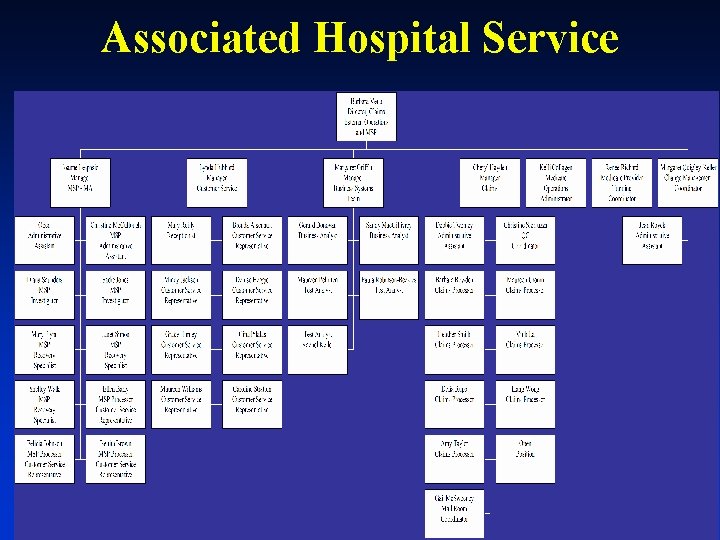
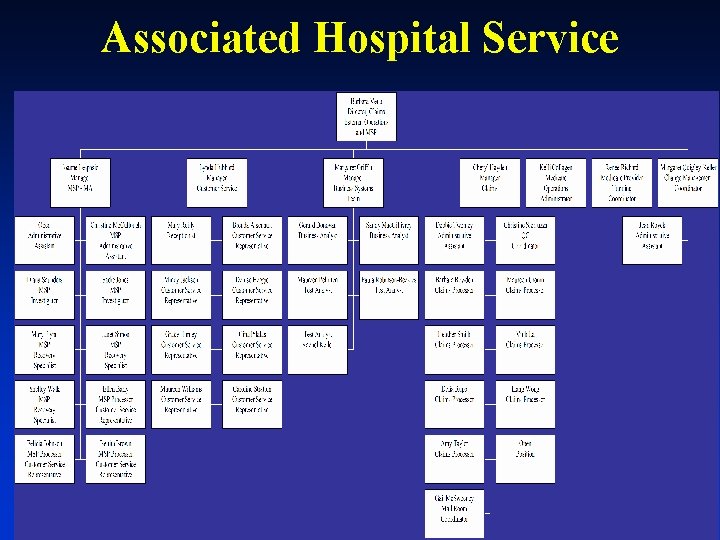
Associated Hospital Service

Other Contact Information Program Safeguard Contractor New England Benefit Integrity Service Center (BISC) Eileen Guiney, UMBI (781) 741 -3207 eileen. guiney@eds. com COB Contractor (800) 999 -1188
Compliance Programs • “Compliance” means following insurance billing, claims submission, and documentation rules. • 1984 Federal Sentencing Guidelines. • “A comprehensive and formal program designed to prevent, detect, and respond to violations of the law by an organization’s employees. ”
Compliance Programs • Office of Inspector General has been developing “Compliance Program Guidances” since 1997 and there are now 9 Guidances. • “The OIG of the DHHS continues in its efforts to promote voluntarily developed and implemented compliance programs for the health care industry. ”
Nine OIG Compliance Guidances • Laboratories (February, 1997) • Hospitals (February, 1998) • Home Health Agencies (August, 1998) • Third-Party Medical Billing Companies (November, 1998) • DMEPOS Industry (June, 1999) • Hospices (November, 1999) • Medicare+Choice Organizations (January, 2000) • Skilled Nursing Facilities (March, 2000) • Individual and Small Group Physician Practices (September, 2000)
Upcoming OIG Guidances • Draft OIG Compliance Program Guidance for Pharmaceutical Manufacturers, October 1, 2002. • Draft OIG Compliance Program Guidance for Ambulance Suppliers, June 6, 2002. • Hospital Guidance Revision: Solicitation of Comments in June 18, 2002 Federal Register to address “OPPS implementation and other significant changes in the hospital industry. ”
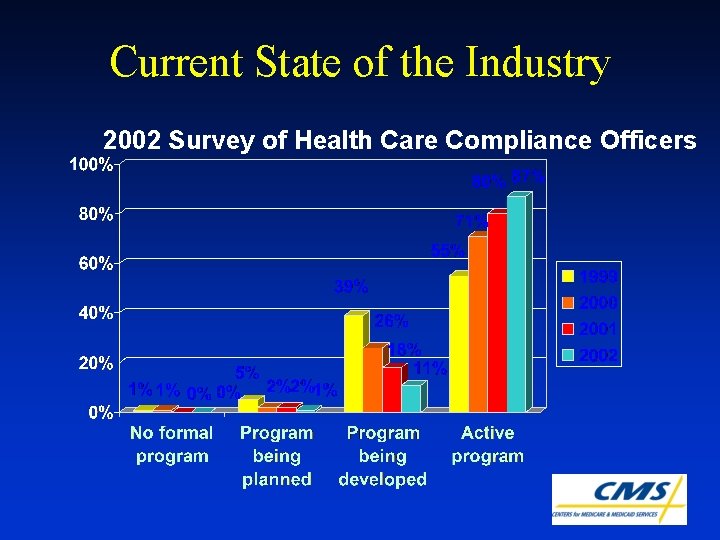
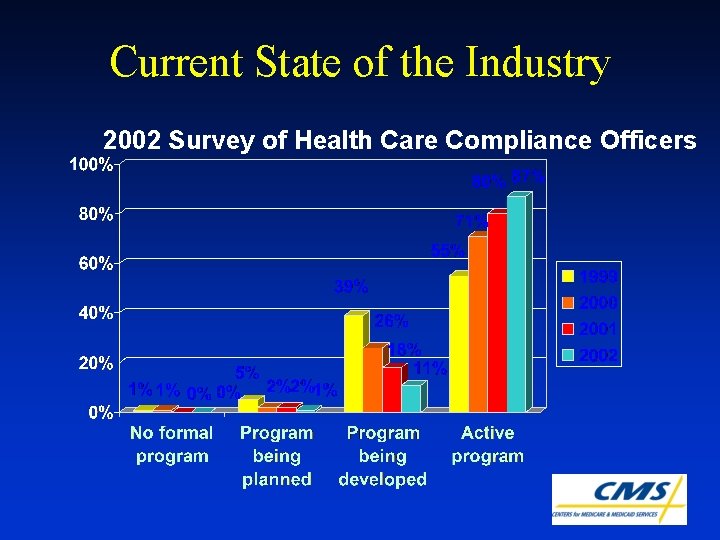
Current State of the Industry 2002 Survey of Health Care Compliance Officers
Seven Standards of Compliance • Code of Conduct • Compliance Officer • Background Checks • Training and Education • Reporting Mechanisms, Monitoring and Auditing • Enforcement and Discipline • Investigations and Response
Compliance Program Effectiveness • HCCA Reference Guide on “Evaluating and Improving A Compliance Program” • Adopts the seven standards, Federal Sentencing Guidelines and OIG Guidance as its foundation. • Two basic components of a compliance program: structural (process oriented) and substantive (results).
Compliance Program Effectiveness l To the extent that healthcare providers can demonstrate a program that results in accurately coded, and appropriately documented claims, CMS wishes to recognize in a tangible way the importance of this effort to the solvency and integrity of the Medicare trust fund. We seek to figure how to: u (1) identify the measurable results of an effective compliance program in terms of accurately coded claims, appropriately documented claims and detected inappropriate claims; and u (2) identify ways that CMS can incent the adoption of effective compliance programs by providers.
Compliance Program Effectiveness l Leslie Norwalk - Chief Operation Officer of CMS l Tim Hill - CFO of CMS • CMS Leads • Kim Brandt - (on detail from OIG Office of the General Counsel • Lisa Zone - Benefit Integrity and Law Enforcement Liaison Dir. • Jim Bryant - Boston RO jbryant 1@cms. hhs. gov 617. 565. 1331 • Lew Morris, OIG • Lori Pellicioni • David Orbach