Cells of Bone Osteoblasts Osteocytes Osteoclasts Calcium Homeostasis


Cells of Bone Osteoblasts Osteocytes Osteoclasts
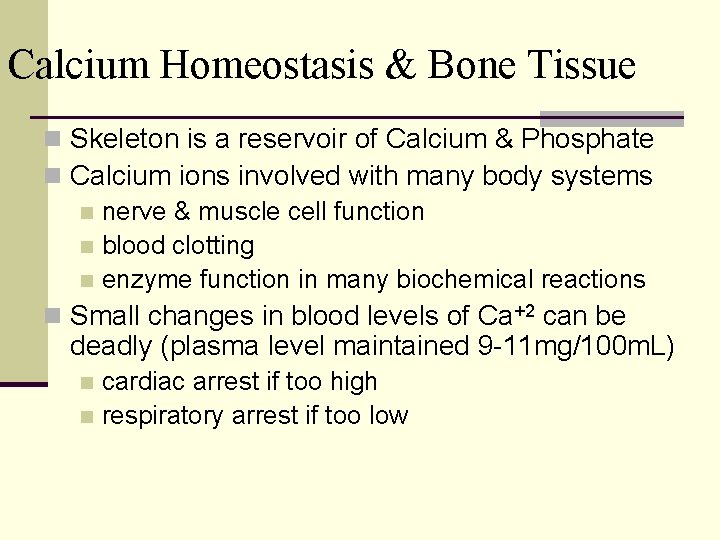
Calcium Homeostasis & Bone Tissue n Skeleton is a reservoir of Calcium & Phosphate n Calcium ions involved with many body systems n nerve & muscle cell function n blood clotting n enzyme function in many biochemical reactions n Small changes in blood levels of Ca+2 can be deadly (plasma level maintained 9 -11 mg/100 m. L) cardiac arrest if too high n respiratory arrest if too low n
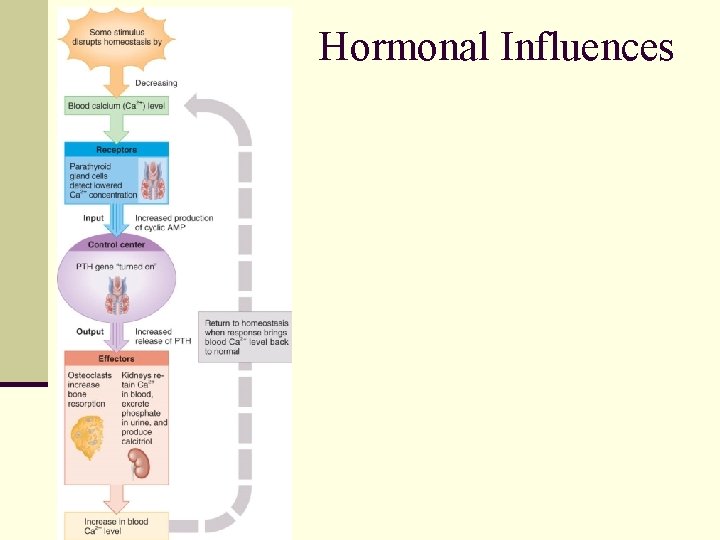
Hormonal Influences

Calcium and Bone Physiology • Serum Ca+2 derived from: – diet (active transport in intestine) – active transport in renal tubules – breakdown of bony matrix • Ca+2 homeostasis maintained by: – Parathyroid hormone – Calcitonin – Vitamin D
Physiological roles of PTH • Receptors present in kidney, gut, bone, other tissues • Activ. of receptors on osteoblasts = release of cytokines = stim. of osteoclast activity • Demineralization of bones leads to elevated Ca+2 in blood • Vit D required for PTH effects on bone – Recruiter of osteoblasts?
Physiological effects of PTH, cont’d. • Increases renal tubular reabsorption of Ca+2 • Enhances vitamin D synthesis in kidney • Enhances intestinal uptake of Ca+2 (indirect effects thru vitamin D? )

Calcitonin • Produced by thyroid gland: • Release stimulated by elevation of blood Ca+2 levels (hypercalcemia) • Other factors (e. g. , gastrin) stimulate its release • Calcitonin levels rise in response to feeding

Calcitonin • Activ of receptors by calcium stimulates calcitonin secretion (opposite of what occurs w/PTH) • Receptors present on skeletal tissue, kidney, and Leydig cells • At level of bone, calcitonin acts directly on osteoclasts to inhibit their activity
Think, pair, share • How will calcitonin and PTH secretion change in response to the injection of EDTA (a calcium chelator)? – A chelator is a substance that binds particular ions, removing them from solution, e. g. , EDTA is a chelator of divalent cations such as Mg+2. • Draw a schematic illustration the demonstrates the mechanism of regulation by calcium of hormone secretion at the cellular level.
Other roles of calcitonin • May serve as satiety factor – Inject calcitonin into rats, monkeys > inhibit food intake – Inject calcitonin into humans > reduce body weight within 24 -36 hours
Vitamin D • Can be made from dietary or endogenous (part of the internal environment of an organism) substances • Precursor of steroidlike hormones that activate nuclear receptors • Renal enzyme production stimulated by PTH
Physiological roles of Vitamin D • Facilitates Ca+2 absorption from intestines; “recruits” osteoblasts • Vitamin D actions are necessary for proper bone growth (evidence: rickets) • Mechanisms of action: – Can promote mineralization(stimulates osteoblasts to do their work) – Can enhance PTH actions • Stimulates reabsorption of Ca+2 in kidney
Osteomalacia (rickets) • Failure of normal bone mineralization • Retards growth in children • Causes skeletal abnormalities in adults
Paget’s disease • Abnormal osteoclast and osteoblast activity • Excessively rapid and uncoordinated turnover of bone • Detected due to elevated alkaline phosphatase levels in blood (the work of Vit D) • Pain, skull enlargement, scoliosis (http: //www. orthop. washington. edu/arthritis/types/ pagets/01 ) • Can lead to dementia, deafness, blindness
Estrogen effects on bone • Inhibits cytokine release (interleukins) from osteoblasts (result: less bone resorption) • Reduces osteoclast lifespan • Lengthens osteoblast lifespan • Reduces rate of activation of new bone remodeling sites
Bone Remodeling n Remodeling is the ongoing replacement of old bone tissue by new bone tissue. Old bone is constantly destroyed by osteoclasts, whereas new bone is constructed by osteoblasts. n In orthodontics teeth are moved by braces. This places stress on bone in the sockets causing osteoclasts and osteoblasts to remodel the sockets so that the teeth can be properly aligned n
EXERCISE AND BONE TISSUE n Within limits, bone has the ability to alter its strength in response to mechanical stress by increasing deposition of mineral salts and production of collagen fibers. n Removal of mechanical stress leads to weakening of bone through demineralization (loss of bone minerals) and collagen reduction. n reduced activity while in a cast n astronauts in weightless environment n bedridden person n Weight-bearing activities, such as walking or moderate weightlifting, help build and retain bone mass.
AGING AND BONE TISSUE n Of two principal effects of aging on bone, the first is the loss of calcium and other minerals from bone matrix (demineralization), which may result in osteoporosis. n very rapid in women 40 -45 as estrogens levels decrease n in males, begins after age 60 n The second principal effect of aging on the skeletal system is a decreased rate of protein synthesis n decrease in collagen production which gives bone its tensile strength n decrease in growth hormone n bone becomes brittle & susceptible to fracture
- Slides: 25