CDI and Coder Collaboration Maximizing Documentation Quality and
CDI and Coder Collaboration – Maximizing Documentation Quality and Revenues Bonnie Cassidy, MPA, RHIA, FAHIMA, FHIMSS & Approved AHIMA ICD-10 Trainer August 19 th, 2016 © 2016 n. Thrive, Inc. All rights reserved. RV 06212016
• Program Overview – CDI Program objectives – Importance of quality documentation – Coding role in accurate and quality reporting • Regulatory Impact to CDI – Coder collaboration – Explanation of the APR-DRG system – Risk adjustment – Impact on CDI, coding, and quality measures • Case studies – Demonstrate the value of improved collaboration to maximize quality and optimize revenue • Importance of the ongoing evolution in the relationship among CDI, Coding, and quality staffs. AGENDA
What is CDI? • Reference : Guidance for Clinical Documentation Improvement Programs – http: //library. ahima. org/xpedio/groups/public/documents/ahima/bok 1_ 047343. hcsp? d. Doc. Name=bok 1_047343 • CDI Professionals are responsible for: • Provider Documentation • Completeness and specificity • Knowledge of clinical documentation requirements: • Clinical indicators for common inpatient diagnoses/comorbidities • ICD-10 -CM and ICD-10 -PCS coding guidelines • MS-DRG assignment and other reimbursement methodologies • Present On Admission (POA) documentation for medical/surgical complications and other hospital-acquired conditions • Education • Providers and medical leadership regarding documentation guidelines
Current State • Clearly defined CDI program and goals - not so much • • Many facilities have no clearly defined CDI goals No formal CDI program CDI objectives vary from one facility to another. ACDIS roadmap: • Pre-Implementation • • http: //www. hcpro. com/acdis/cdi_roadmap_phase 1. cfm http: //www. hcpro. com/acdis/cdi_roadmap_phase 2. cfm Clinical documentation impacts the work of many hospital departments.
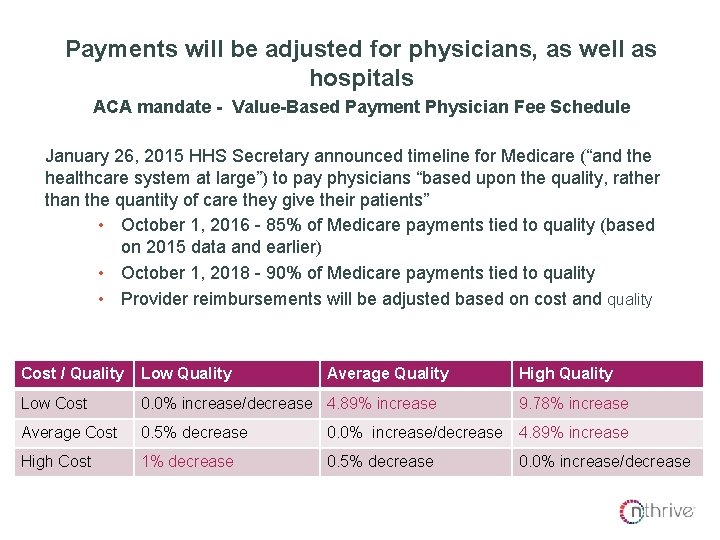
Why is this important? Payments will be adjusted for physicians, as well as hospitals ACA mandate - Value-Based Payment Physician Fee Schedule January 26, 2015 HHS Secretary announced timeline for Medicare (“and the healthcare system at large”) to pay physicians “based upon the quality, rather than the quantity of care they give their patients” • October 1, 2016 - 85% of Medicare payments tied to quality (based on 2015 data and earlier) • October 1, 2018 - 90% of Medicare payments tied to quality • Provider reimbursements will be adjusted based on cost and quality Cost / Quality Low Quality Average Quality High Quality Low Cost 0. 0% increase/decrease 4. 89% increase Average Cost 0. 5% decrease 0. 0% increase/decrease 4. 89% increase High Cost 1% decrease 0. 5% decrease 9. 78% increase 0. 0% increase/decrease

APR-DRGS AND RISK ADJUSTMENT
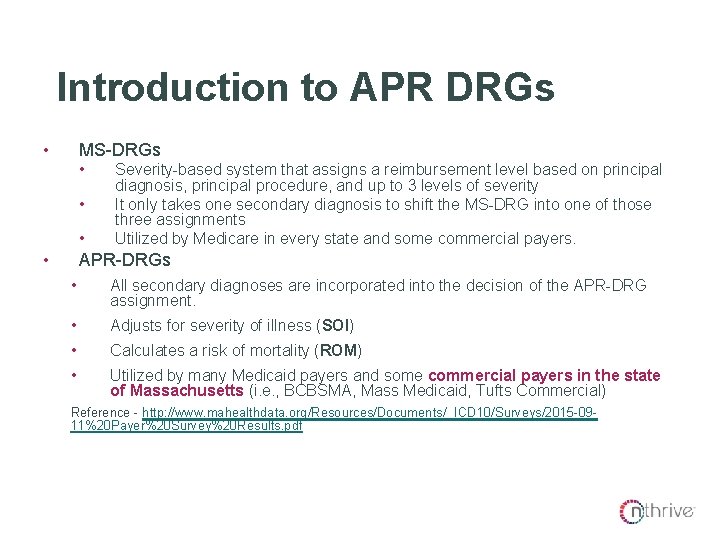
Introduction to APR DRGs • MS-DRGs • • Severity-based system that assigns a reimbursement level based on principal diagnosis, principal procedure, and up to 3 levels of severity It only takes one secondary diagnosis to shift the MS-DRG into one of those three assignments Utilized by Medicare in every state and some commercial payers. APR-DRGs • All secondary diagnoses are incorporated into the decision of the APR-DRG assignment. • Adjusts for severity of illness (SOI) • Calculates a risk of mortality (ROM) • Utilized by many Medicaid payers and some commercial payers in the state of Massachusetts (i. e. , BCBSMA, Mass Medicaid, Tufts Commercial) Reference - http: //www. mahealthdata. org/Resources/Documents/_ICD 10/Surveys/2015 -0911%20 Payer%20 Survey%20 Results. pdf
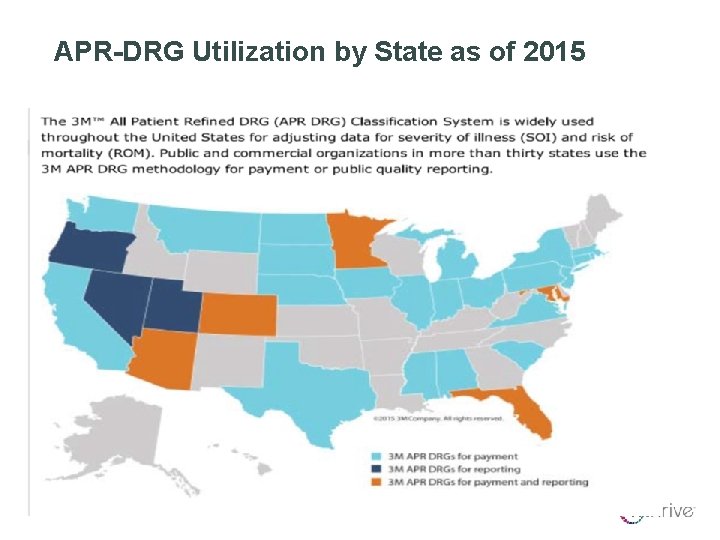
APR-DRG Utilization by State as of 2015
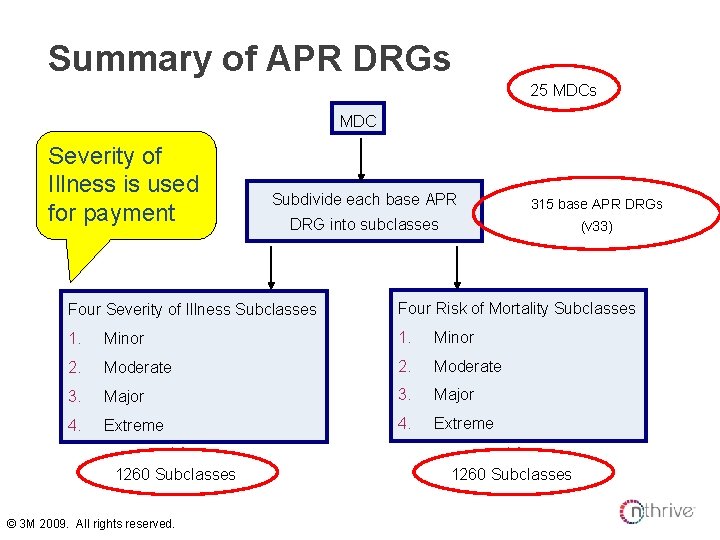
Summary of APR DRGs 25 MDCs MDC Severity of Illness is used for payment Subdivide each base APR 315 base APR DRGs DRG into subclasses (v 33) Four Severity of Illness Subclasses Four Risk of Mortality Subclasses 1. Minor 2. Moderate 3. Major 4. Extreme 1260 Subclasses © 3 M 2009. All rights reserved. 1260 Subclasses
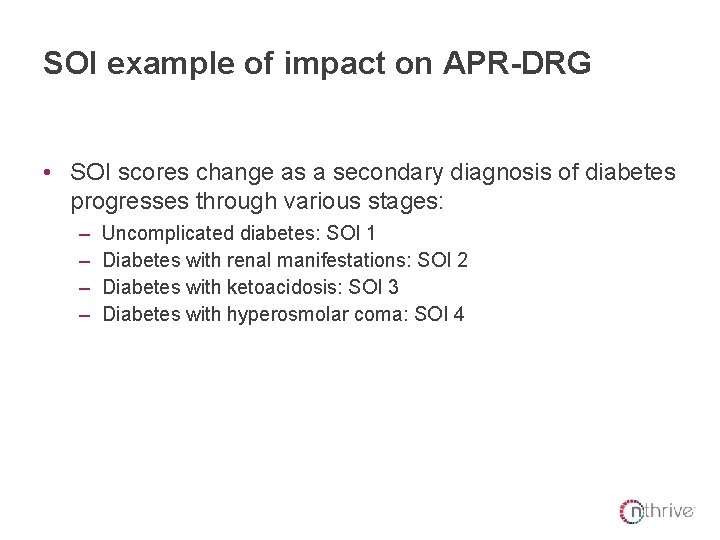
SOI example of impact on APR-DRG • SOI scores change as a secondary diagnosis of diabetes progresses through various stages: – – Uncomplicated diabetes: SOI 1 Diabetes with renal manifestations: SOI 2 Diabetes with ketoacidosis: SOI 3 Diabetes with hyperosmolar coma: SOI 4
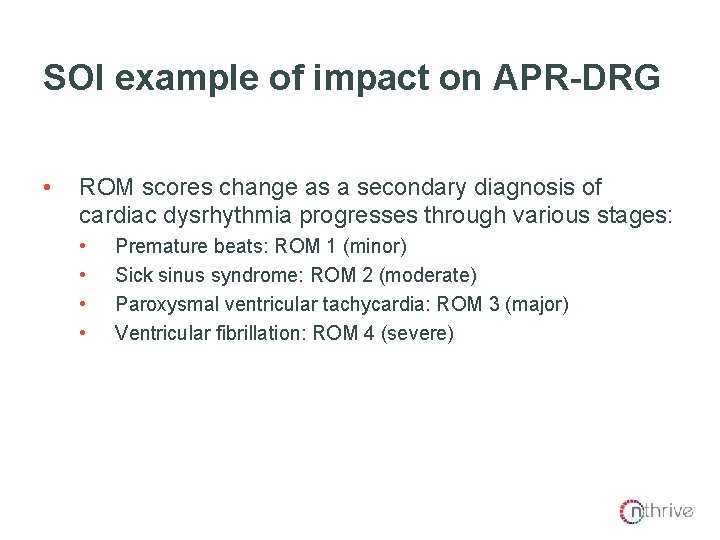
ROM example of impact on APR-DRG SOI example of impact on APR-DRG • ROM scores change as a secondary diagnosis of cardiac dysrhythmia progresses through various stages: • • Premature beats: ROM 1 (minor) Sick sinus syndrome: ROM 2 (moderate) Paroxysmal ventricular tachycardia: ROM 3 (major) Ventricular fibrillation: ROM 4 (severe)
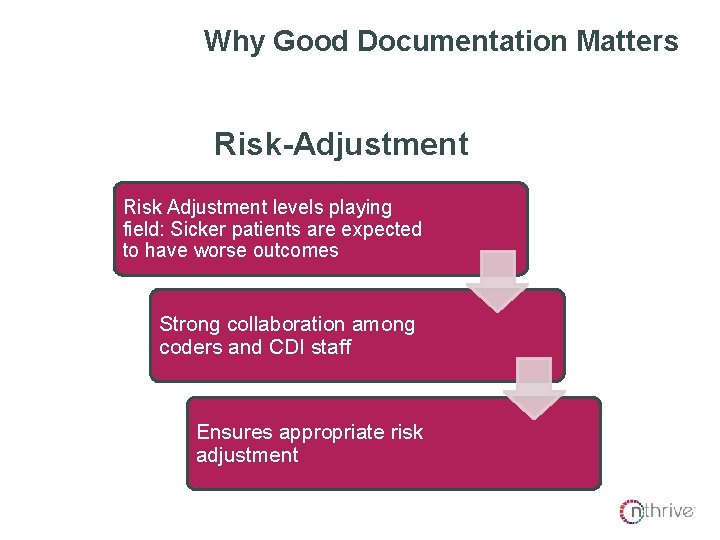
Why Good Documentation Matters Risk-Adjustment Risk Adjustment levels playing field: Sicker patients are expected to have worse outcomes Strong collaboration among coders and CDI staff Ensures appropriate risk adjustment
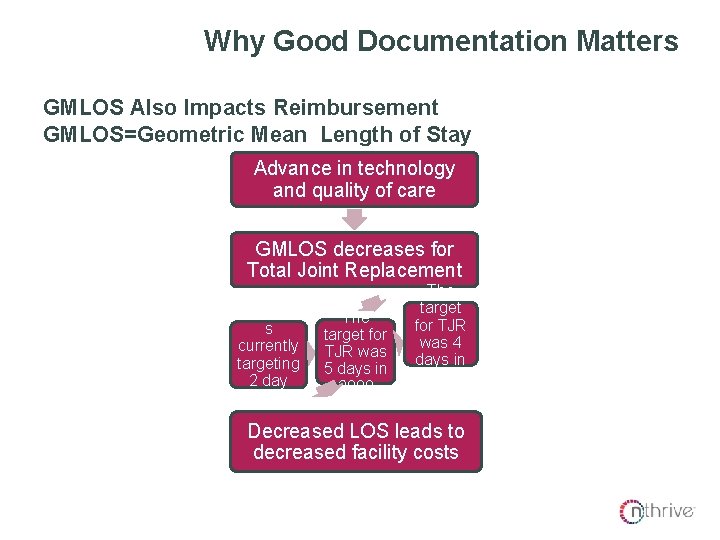
Why Good Documentation Matters GMLOS Also Impacts Reimbursement GMLOS=Geometric Mean Length of Stay Advance in technology and quality of care GMLOS decreases for Total Joint Replacement Many hospital s currently targeting 2 day LOS for TJR The target for TJR was 5 days in 2000 The target for TJR was 4 days in 2010 Decreased LOS leads to decreased facility costs

CASE STUDIES
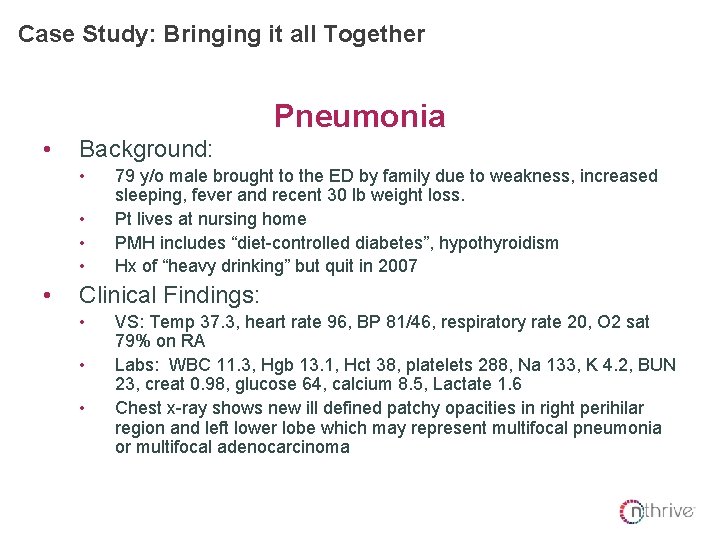
Case Study: Bringing it all Together Pneumonia • Background: • • • 79 y/o male brought to the ED by family due to weakness, increased sleeping, fever and recent 30 lb weight loss. Pt lives at nursing home PMH includes “diet-controlled diabetes”, hypothyroidism Hx of “heavy drinking” but quit in 2007 Clinical Findings: • • • VS: Temp 37. 3, heart rate 96, BP 81/46, respiratory rate 20, O 2 sat 79% on RA Labs: WBC 11. 3, Hgb 13. 1, Hct 38, platelets 288, Na 133, K 4. 2, BUN 23, creat 0. 98, glucose 64, calcium 8. 5, Lactate 1. 6 Chest x-ray shows new ill defined patchy opacities in right perihilar region and left lower lobe which may represent multifocal pneumonia or multifocal adenocarcinoma
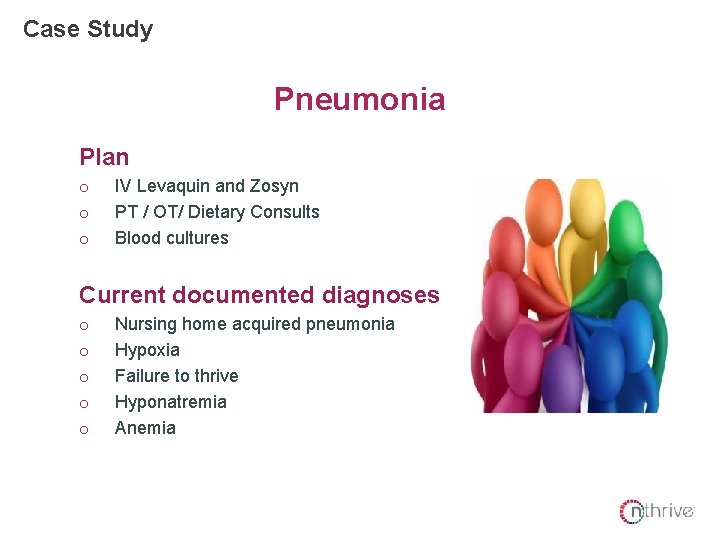
Case Study Pneumonia Plan o o o IV Levaquin and Zosyn PT / OT/ Dietary Consults Blood cultures Current documented diagnoses o o o Nursing home acquired pneumonia Hypoxia Failure to thrive Hyponatremia Anemia
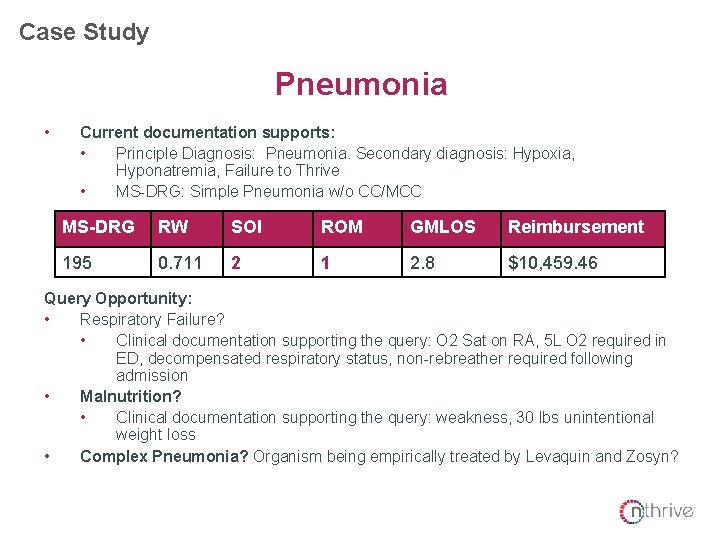
Case Study Pneumonia • Current documentation supports: • Principle Diagnosis: Pneumonia. Secondary diagnosis: Hypoxia, Hyponatremia, Failure to Thrive • MS-DRG: Simple Pneumonia w/o CC/MCC MS-DRG RW SOI ROM GMLOS Reimbursement 195 0. 711 2 1 2. 8 $10, 459. 46 Query Opportunity: • Respiratory Failure? • Clinical documentation supporting the query: O 2 Sat on RA, 5 L O 2 required in ED, decompensated respiratory status, non-rebreather required following admission • Malnutrition? • Clinical documentation supporting the query: weakness, 30 lbs unintentional weight loss • Complex Pneumonia? Organism being empirically treated by Levaquin and Zosyn?
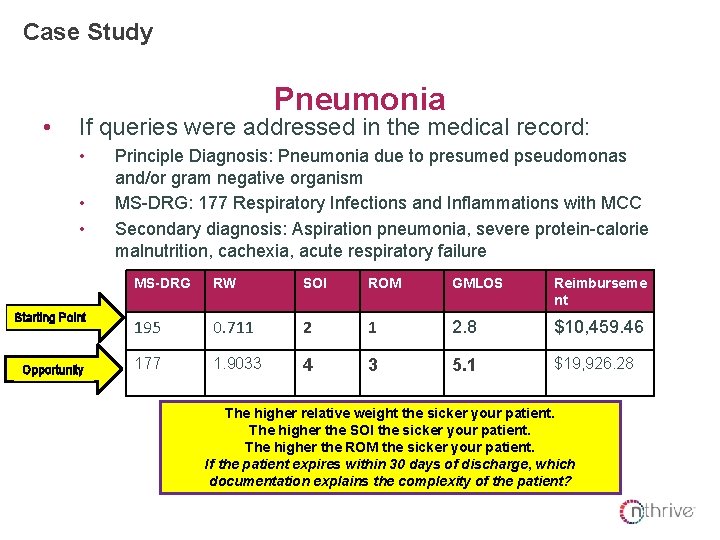
Case Study • Pneumonia If queries were addressed in the medical record: • • • Starting Point Opportunity Principle Diagnosis: Pneumonia due to presumed pseudomonas and/or gram negative organism MS-DRG: 177 Respiratory Infections and Inflammations with MCC Secondary diagnosis: Aspiration pneumonia, severe protein-calorie malnutrition, cachexia, acute respiratory failure MS-DRG RW SOI ROM GMLOS Reimburseme nt 195 0. 711 2 1 2. 8 $10, 459. 46 177 1. 9033 4 3 5. 1 $19, 926. 28 The higher relative weight the sicker your patient. The higher the SOI the sicker your patient. The higher the ROM the sicker your patient. If the patient expires within 30 days of discharge, which documentation explains the complexity of the patient?
Why Good Documentation Matters Public Reporting Programs Rely on Coded Data Why Goodcannot Documentation • Coders code what is not. Matters documented by the provider • CMS uses MEDPAR data to calculate an actual/expected ratio for the following programs • 30 -Day Readmission Program • MCARE reduces hospitals base operating DRG payments to account for excess readmissions in the following DRGs – AMI, CHF and Pneumonia, COPD, and Total Joint Replacements • Added for 2017: CABG (data collection started in 2015) • 30 -Day Mortality Measures: • Acute myocardial infraction (AMI) • Heart failure (HF) • Pneumonia (PN) • THA/TKA • COPD • Medicare spending per beneficiary (MSPB) - started 2015 and risk adjusted. All of the programs are adjusted and calculated as ratio of actual versus expected (MEDPAR data)

DOCUMENTATION, CODING, AND QUALITY INDICATORS
Documentation and PSI • • Definition of PSI (Patient Safety Indicators) Common documentation and coding issues: • • For example, clarifying if pressure ulcer was POA when the H&P indicates the skin is intact Clarifying if case of blood stream infection is due to a device or procedure vs. multifactorial in nature
Where to Start? • PSI 90 is referred to as a composite measure because eight different PSIs are rolled up to provide an overview of hospital performance. The eight PSIs included in the CMS PSI 90 composite measure include: – PSI 03, pressure ulcer – PSI 06, iatrogenic pneumothorax – PSI 07, central venous catheter-related bloodstream infections – PSI 08, postoperative hip fracture – PSI 12, postoperative pulmonary embolism or deep venous thrombosis – PSI 13, postoperative sepsis – PSI 14, postoperative wound dehiscence – PSI 15, accidental puncture or laceration
PSI 15 – Accidental Laceration • CMS defines accidental puncture or laceration (PSI 15) as a complication; a condition, that when present, leads to substantially increased hospital resource use. This includes intensive monitoring, expensive and technically complex services and extensive care requiring a greater number of caregivers. • The most common vulnerabilities identified in PSI 15 audits include: • Incorrect reporting of dx 998. 2 (mapped to many ICD-10 codes) in situations where use of this code is excluded (e. g. , incidental durotomy) • Incorrect reporting of E codes (now Y codes in ICD-10) • Over-reporting dx 998. 2 in situations where the puncture or laceration was not accidental and/or was unavoidable due to the patient's anatomy and/or other circumstances (e. g. , dense adhesions) • Under-reporting dx 998. 2 when physicians incorrectly guide the coder not to assign a perforation or laceration as a complication
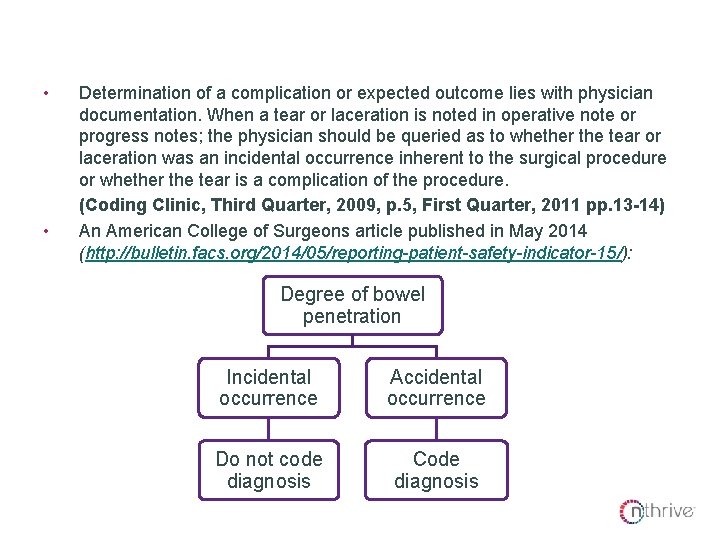
PSI 15 – Accidental Laceration • • Determination of a complication or expected outcome lies with physician documentation. When a tear or laceration is noted in operative note or progress notes; the physician should be queried as to whether the tear or laceration was an incidental occurrence inherent to the surgical procedure or whether the tear is a complication of the procedure. (Coding Clinic, Third Quarter, 2009, p. 5, First Quarter, 2011 pp. 13 -14) An American College of Surgeons article published in May 2014 (http: //bulletin. facs. org/2014/05/reporting-patient-safety-indicator-15/): Degree of bowel penetration Incidental occurrence Accidental occurrence Do not code diagnosis Code diagnosis
KNOCKING DOWN THE SILOS
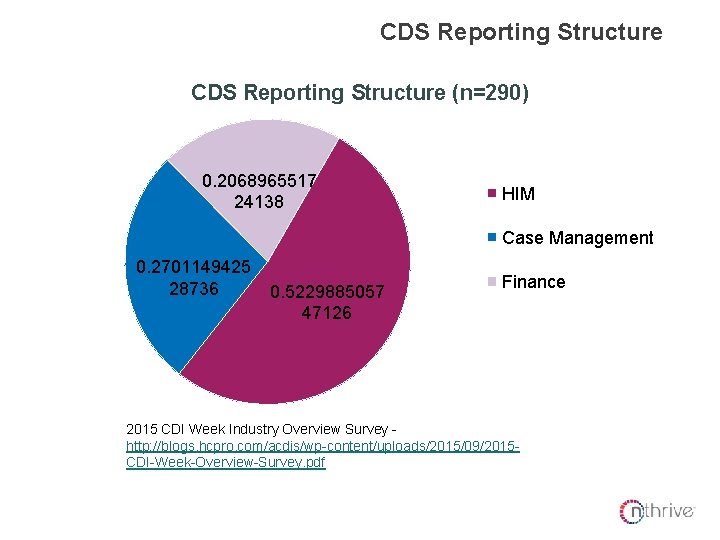
CDS Reporting Structure (n=290) 0. 2068965517 24138 HIM Case Management 0. 2701149425 28736 0. 5229885057 47126 Finance 2015 CDI Week Industry Overview Survey http: //blogs. hcpro. com/acdis/wp-content/uploads/2015/09/2015 CDI-Week-Overview-Survey. pdf
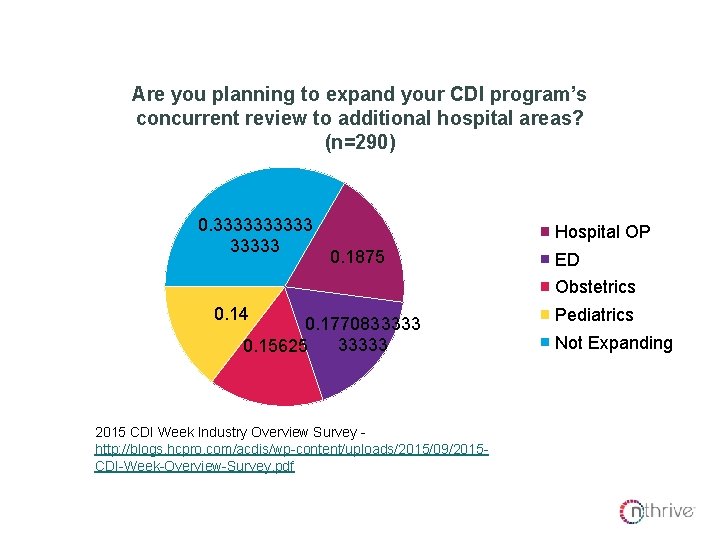
Areas of CDI Expansion Are you planning to expand your CDI program’s concurrent review to additional hospital areas? (n=290) 0. 33333 Hospital OP 0. 1875 ED Obstetrics 0. 14 0. 1770833333 0. 15625 2015 CDI Week Industry Overview Survey http: //blogs. hcpro. com/acdis/wp-content/uploads/2015/09/2015 CDI-Week-Overview-Survey. pdf Pediatrics Not Expanding

CDI/Coder/Quality Collaboration Coding Managers and CDI Directors should work together to implement the following processes • • • Ongoing ICD-10 education is available for coders and CDS staff. DRG discrepancies are reviewed with the coder/CDS on an individual basis and common DRG discrepancies are reviewed with the two teams Coder/CDI queries are modified to meet ICD-10 compliance – about 15 -20% of the ICD-10 -CM guidelines affecting when and how a code is assigned were revised and PCS requires much more specificity (approach, device, body part, etc. )
CDI/Coder/Quality Collaboration • • All HACs are reviewed pre-bill collaboratively by the Coding Manager/CDI Director to ensure the appropriateness of HAC reporting. All DRG denials accepted by the facility are reviewed with the individual coder/CDS who coded the account and reviewed with the coder/CDS teams
ICD-10 Coder/CDI/Quality Meetings • • • Review any trend in DRG or APR-DRG discrepancy between the coding team and the CDS staff. Discuss clinical indicators of commonly targeted CCs/MCCs by RACs (ex. encephalopathy, postoperative respiratory failure, acute cor pulmonale, etc. ) Review any recently reported HACs with the coding team, CDS staff, and quality leadership so the facility is in agreement with when a HAC is to be reported.
Why Good Documentation Matters • • As of October 1, 2015, 65 percent of value-based purchasing (VBP) scores, 25% of the new hospitalacquired conditions (HAC) payment reduction program and 100% of the readmission reduction program scores will be derived from coded data. The composite PSI-90 is of particular importance for VBP and HAC reduction program initiatives. • • A good starting place: educate CDI and coders on the PSI 90 composite. The Agency for Healthcare Research and Quality lists ICD-10 CM/PCS equivalent codes for Patient Safety Indicators (PSI) at its website- http: //www. qualityindicators. ahrq. gov/icd 10
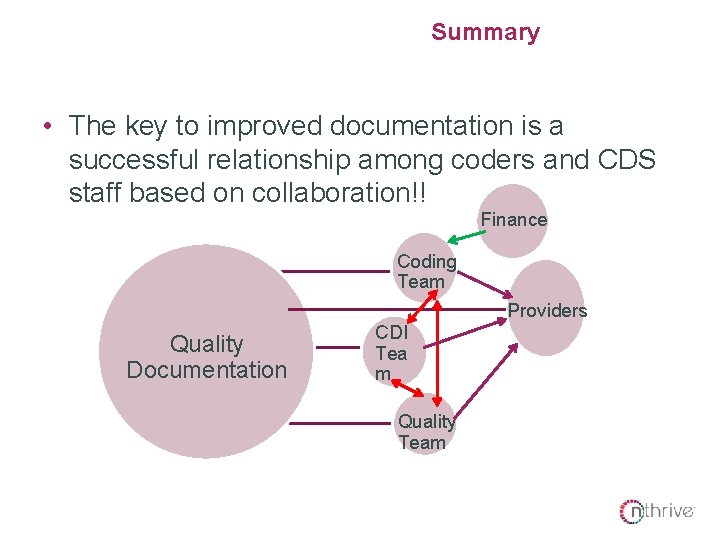
Summary • The key to improved documentation is a successful relationship among coders and CDS staff based on collaboration!! Finance Coding Team Providers Quality Documentation CDI Tea m Quality Team
Takeaways • Work together (Coding, CDI, and Quality) to educate providers on quality documentation to meet ICD-10 -CM and ICD-10 -PCS coding guidelines. Explain to providers how SOI and ROM will impact their bottom line. • Review reported HACs and PSIs on a regular basis as a team. • Educate coding and CDI teams on all DRG denials accepted by the facility. Andy Tolep, CCS, CCDS, CPC Precyse Senior HIM Consultant atolep@precyse. com
Q&A

It is up to you which option to use. SECTION DIVIDER SLIDE 1
It is up to you which option to use. SECTION DIVIDER SLIDE 2
It is up to you which option to use. SECTION DIVIDER SLIDE 3

It is up to you which option to use. SECTION DIVIDER SLIDE 4

It is up to you which option to use. SECTION DIVIDER SLIDE 5
It is up to you which option to use. SECTION DIVIDER SLIDE 6
(Printer friendly option) It is up to you which option to use. SECTION DIVIDER SLIDE 7
Introduction Overview Content Group Discussion Next Steps
Your Name Your Title (NOTE: Hit “Increase Indent” button once for formatting) Your Name Your Title Your Name Your Title ATTENDEES
Your Name Your Title (NOTE: Hit “Increase Indent” button once formatting) P: (234) 567 -8901(NOTE: Hit “Increase Indent” button twice formatting) C: (234) 567 -8901 name@nthrive. com
Sample Chart 90 80 70 60 Series 1 50 Series 2 40 Series 3 30 Series 4 20 10 0 Category 1 Category 2 Category 3
Sample Chart Title Category 1 Category 2 Category 3
Sample Table Header Content Content Content
Two Column Content Slide • Column 1 • Column 2
Two Column with Header Content Slide Column 1 Header Column 2 Header • Column 1 • Column 2
Title Only
BLANK SLIDE WITH LOGO
BLANK SLIDE

QUESTIONS

- Slides: 54