CAUTI Prevention A Quality Improvement Project Kayla Abrahamson
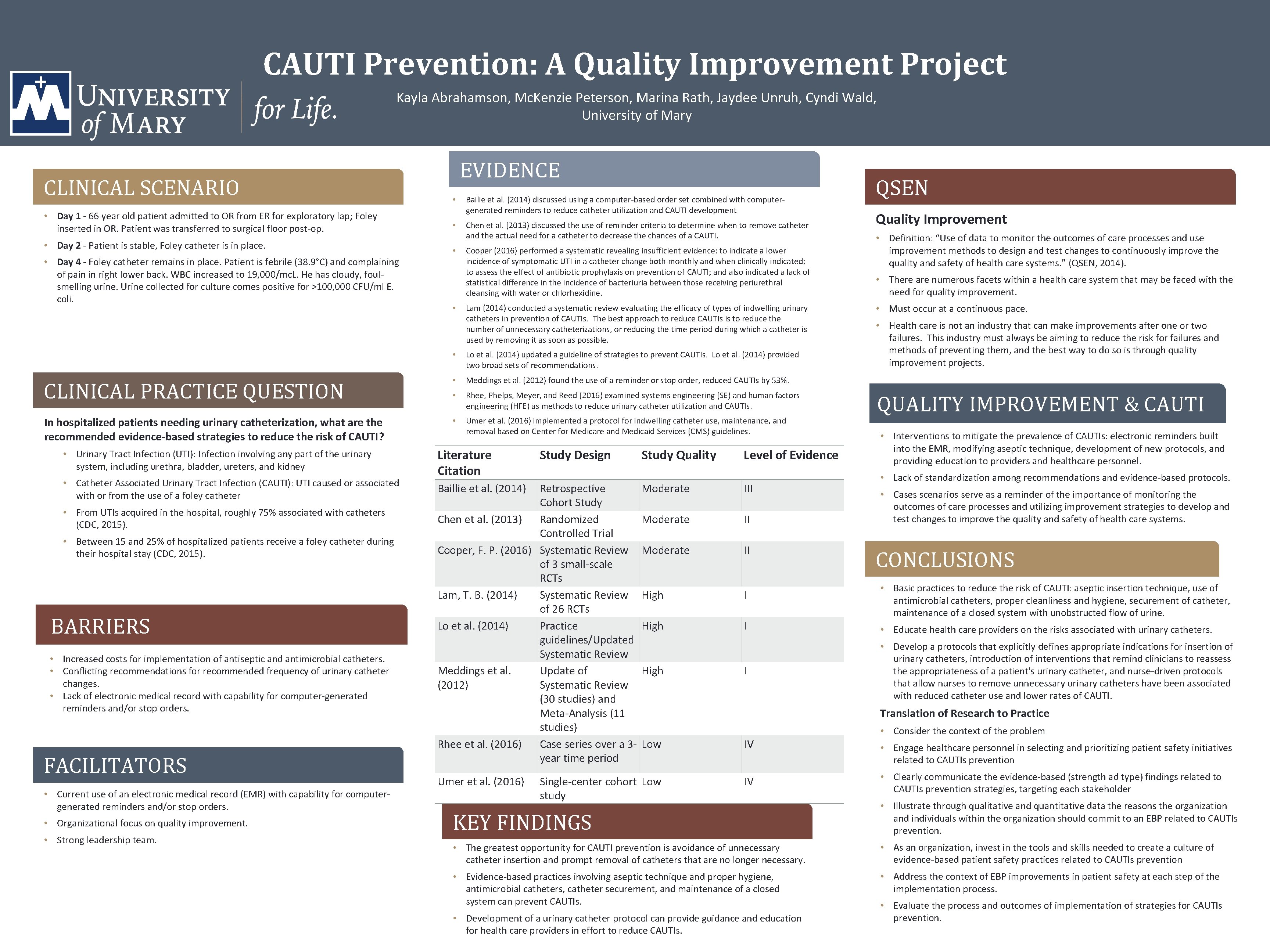
CAUTI Prevention: A Quality Improvement Project Kayla Abrahamson, Mc. Kenzie Peterson, Marina Rath, Jaydee Unruh, Cyndi Wald, University of Mary CLINICAL SCENARIO • Day 1 - 66 year old patient admitted to OR from ER for exploratory lap; Foley inserted in OR. Patient was transferred to surgical floor post-op. • Day 2 - Patient is stable, Foley catheter is in place. • Day 4 - Foley catheter remains in place. Patient is febrile (38. 9°C) and complaining of pain in right lower back. WBC increased to 19, 000/mc. L. He has cloudy, foulsmelling urine. Urine collected for culture comes positive for >100, 000 CFU/ml E. coli. EVIDENCE • Bailie et al. (2014) discussed using a computer-based order set combined with computergenerated reminders to reduce catheter utilization and CAUTI development • Chen et al. (2013) discussed the use of reminder criteria to determine when to remove catheter and the actual need for a catheter to decrease the chances of a CAUTI. • • Cooper (2016) performed a systematic revealing insufficient evidence: to indicate a lower incidence of symptomatic UTI in a catheter change both monthly and when clinically indicated; to assess the effect of antibiotic prophylaxis on prevention of CAUTI; and also indicated a lack of statistical difference in the incidence of bacteriuria between those receiving periurethral cleansing with water or chlorhexidine. Lam (2014) conducted a systematic review evaluating the efficacy of types of indwelling urinary catheters in prevention of CAUTIs. The best approach to reduce CAUTIs is to reduce the number of unnecessary catheterizations, or reducing the time period during which a catheter is used by removing it as soon as possible. • Lo et al. (2014) updated a guideline of strategies to prevent CAUTIs. Lo et al. (2014) provided two broad sets of recommendations. CLINICAL PRACTICE QUESTION • Meddings et al. (2012) found the use of a reminder or stop order, reduced CAUTIs by 53%. • Rhee, Phelps, Meyer, and Reed (2016) examined systems engineering (SE) and human factors engineering (HFE) as methods to reduce urinary catheter utilization and CAUTIs. In hospitalized patients needing urinary catheterization, what are the recommended evidence-based strategies to reduce the risk of CAUTI? • Umer et al. (2016) implemented a protocol for indwelling catheter use, maintenance, and removal based on Center for Medicare and Medicaid Services (CMS) guidelines. • Urinary Tract Infection (UTI): Infection involving any part of the urinary system, including urethra, bladder, ureters, and kidney • Catheter Associated Urinary Tract Infection (CAUTI): UTI caused or associated with or from the use of a foley catheter • From UTIs acquired in the hospital, roughly 75% associated with catheters (CDC, 2015). • Between 15 and 25% of hospitalized patients receive a foley catheter during their hospital stay (CDC, 2015). BARRIERS • Increased costs for implementation of antiseptic and antimicrobial catheters. • Conflicting recommendations for recommended frequency of urinary catheter changes. • Lack of electronic medical record with capability for computer-generated reminders and/or stop orders. FACILITATORS • Current use of an electronic medical record (EMR) with capability for computergenerated reminders and/or stop orders. • Organizational focus on quality improvement. • Strong leadership team. Literature Citation Study Design Baillie et al. (2014) Retrospective Cohort Study Chen et al. (2013) Randomized Controlled Trial Cooper, F. P. (2016) Systematic Review of 3 small-scale RCTs Lam, T. B. (2014) Systematic Review of 26 RCTs Lo et al. (2014) Practice guidelines/Updated Systematic Review Meddings et al. Update of (2012) Systematic Review (30 studies) and Meta-Analysis (11 studies) Rhee et al. (2016) Case series over a 3 year time period Umer et al. (2016) Study Quality Level of Evidence Moderate III Moderate II High I QSEN Quality Improvement • Definition: “Use of data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems. ” (QSEN, 2014). • There are numerous facets within a health care system that may be faced with the need for quality improvement. • Must occur at a continuous pace. • Health care is not an industry that can make improvements after one or two failures. This industry must always be aiming to reduce the risk for failures and methods of preventing them, and the best way to do so is through quality improvement projects. QUALITY IMPROVEMENT & CAUTI • Interventions to mitigate the prevalence of CAUTIs: electronic reminders built into the EMR, modifying aseptic technique, development of new protocols, and providing education to providers and healthcare personnel. • Lack of standardization among recommendations and evidence-based protocols. • Cases scenarios serve as a reminder of the importance of monitoring the outcomes of care processes and utilizing improvement strategies to develop and test changes to improve the quality and safety of health care systems. CONCLUSIONS • Basic practices to reduce the risk of CAUTI: aseptic insertion technique, use of antimicrobial catheters, proper cleanliness and hygiene, securement of catheter, maintenance of a closed system with unobstructed flow of urine. • Educate health care providers on the risks associated with urinary catheters. • Develop a protocols that explicitly defines appropriate indications for insertion of urinary catheters, introduction of interventions that remind clinicians to reassess the appropriateness of a patient's urinary catheter, and nurse-driven protocols that allow nurses to remove unnecessary urinary catheters have been associated with reduced catheter use and lower rates of CAUTI. Translation of Research to Practice Low Single-center cohort Low study IV IV • Consider the context of the problem • Engage healthcare personnel in selecting and prioritizing patient safety initiatives related to CAUTIs prevention • Clearly communicate the evidence-based (strength ad type) findings related to CAUTIs prevention strategies, targeting each stakeholder KEY FINDINGS • Illustrate through qualitative and quantitative data the reasons the organization and individuals within the organization should commit to an EBP related to CAUTIs prevention. • The greatest opportunity for CAUTI prevention is avoidance of unnecessary catheter insertion and prompt removal of catheters that are no longer necessary. • As an organization, invest in the tools and skills needed to create a culture of evidence-based patient safety practices related to CAUTIs prevention • Evidence-based practices involving aseptic technique and proper hygiene, antimicrobial catheters, catheter securement, and maintenance of a closed system can prevent CAUTIs. • Address the context of EBP improvements in patient safety at each step of the implementation process. • Development of a urinary catheter protocol can provide guidance and education for health care providers in effort to reduce CAUTIs. • Evaluate the process and outcomes of implementation of strategies for CAUTIs prevention.
- Slides: 1