Causes of death in patients with STEMI treated

- Slides: 43
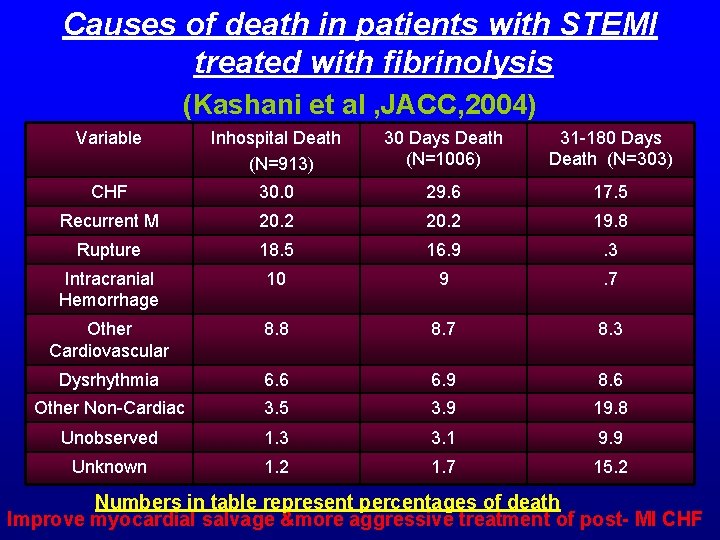
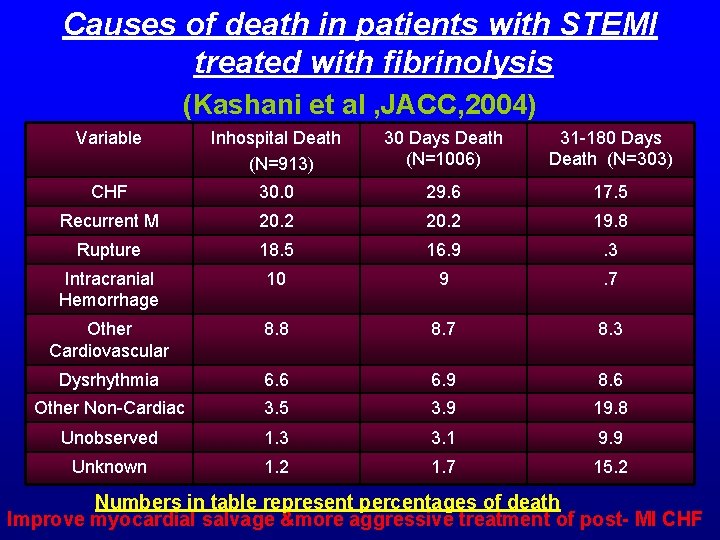
Causes of death in patients with STEMI treated with fibrinolysis (Kashani et al , JACC, 2004) Variable Inhospital Death (N=913) 30 Days Death (N=1006) 31 -180 Days Death (N=303) CHF 30. 0 29. 6 17. 5 Recurrent M 20. 2 19. 8 Rupture 18. 5 16. 9 . 3 Intracranial Hemorrhage 10 9 . 7 Other Cardiovascular 8. 8 8. 7 8. 3 Dysrhythmia 6. 6 6. 9 8. 6 Other Non-Cardiac 3. 5 3. 9 19. 8 Unobserved 1. 3 3. 1 9. 9 Unknown 1. 2 1. 7 15. 2 Numbers in table represent percentages of death Improve myocardial salvage &more aggressive treatment of post- MI CHF
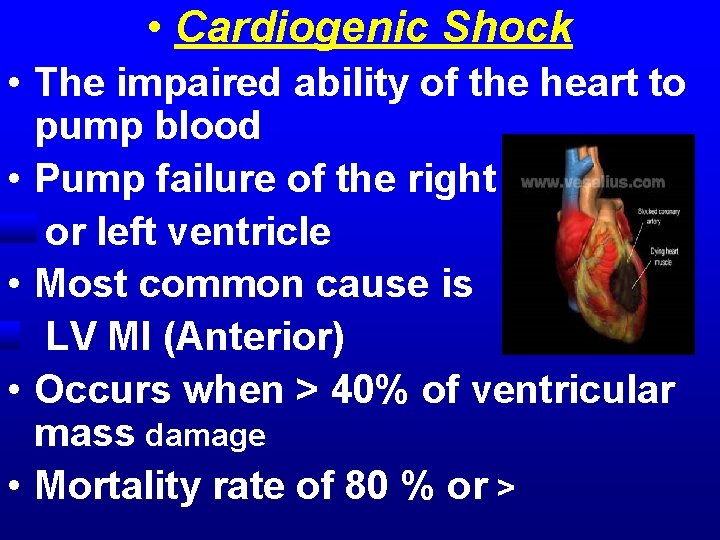
• Cardiogenic Shock • The impaired ability of the heart to pump blood • Pump failure of the right • or left ventricle • Most common cause is • LV MI (Anterior) • Occurs when > 40% of ventricular mass damage • Mortality rate of 80 % or >
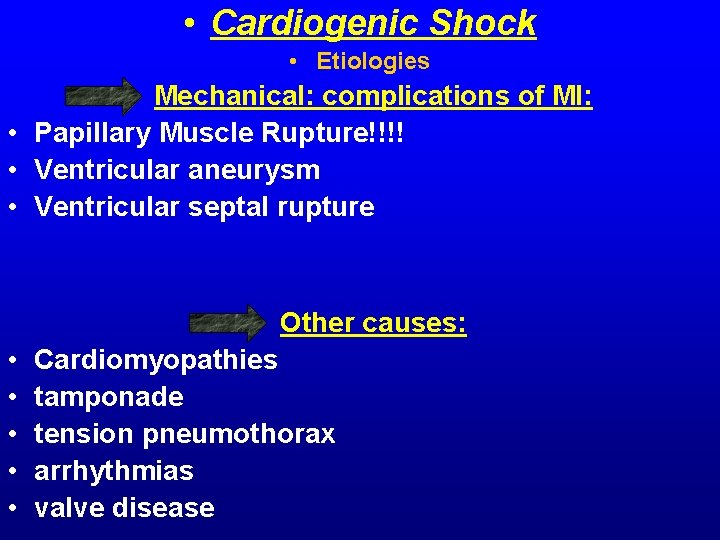
• Cardiogenic Shock • Etiologies • Mechanical: complications of MI: • Papillary Muscle Rupture!!!! • Ventricular aneurysm • Ventricular septal rupture • • • Other causes: Cardiomyopathies tamponade tension pneumothorax arrhythmias valve disease
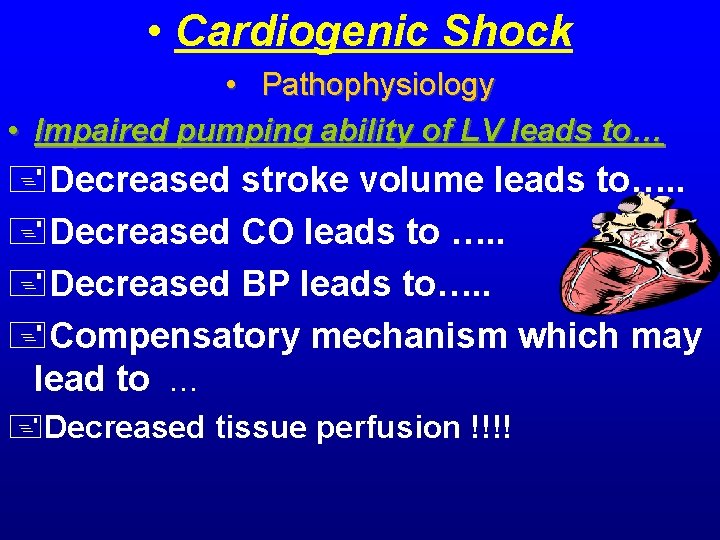
• Cardiogenic Shock • Pathophysiology • Impaired pumping ability of LV leads to… +Decreased stroke volume leads to…. . +Decreased CO leads to …. . +Decreased BP leads to…. . +Compensatory mechanism which may lead to … +Decreased tissue perfusion !!!!
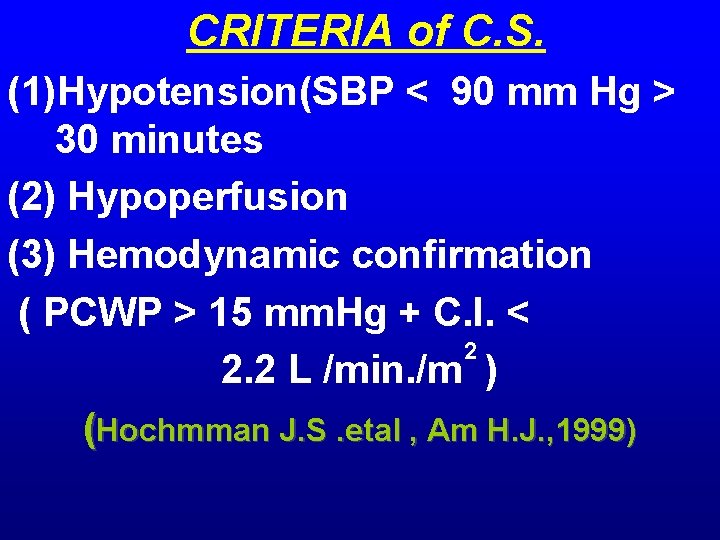
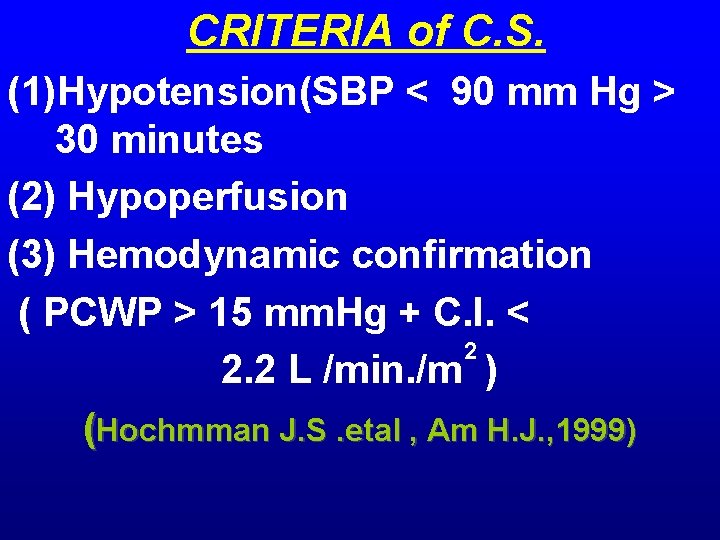
CRITERIA of C. S. (1)Hypotension(SBP < 90 mm Hg > 30 minutes (2) Hypoperfusion (3) Hemodynamic confirmation ( PCWP > 15 mm. Hg + C. I. < 2 2. 2 L /min. /m ) (Hochmman J. S. etal , Am H. J. , 1999)
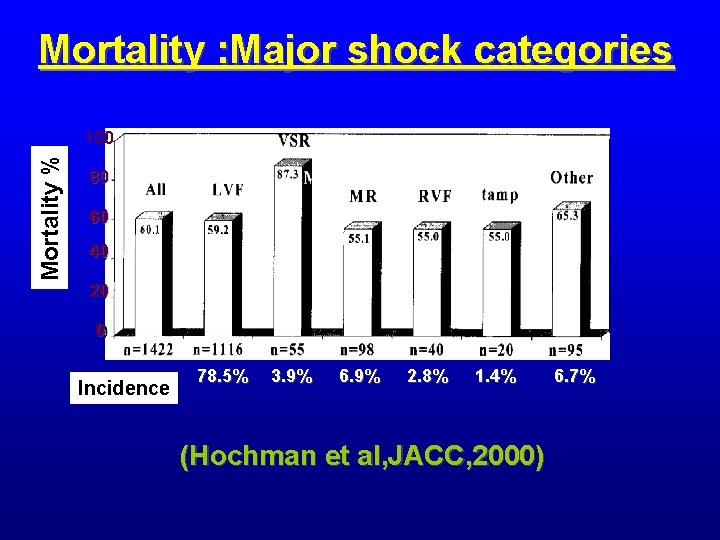
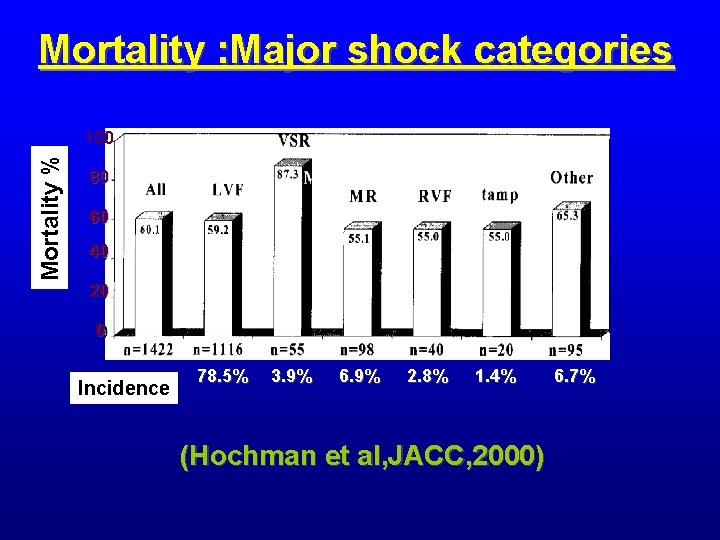
Mortality : Major shock categories Mortality % 100 80 60 40 20 0 Incidence 78. 5% 3. 9% 6. 9% 2. 8% 1. 4% (Hochman et al, JACC, 2000) 6. 7%
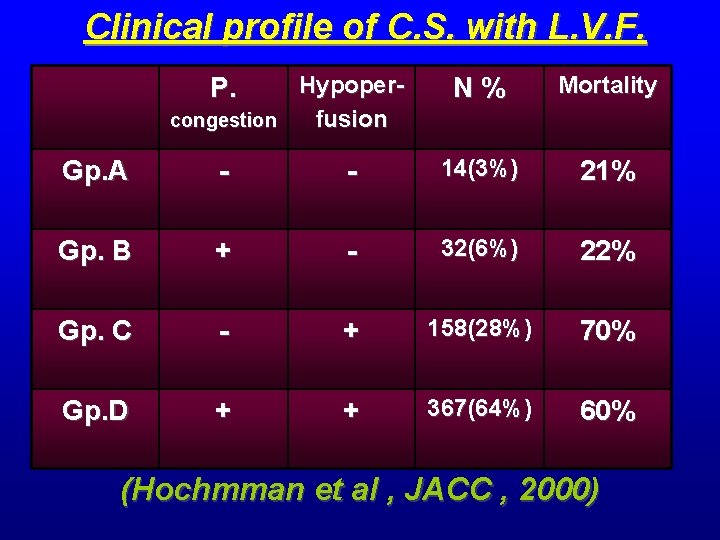
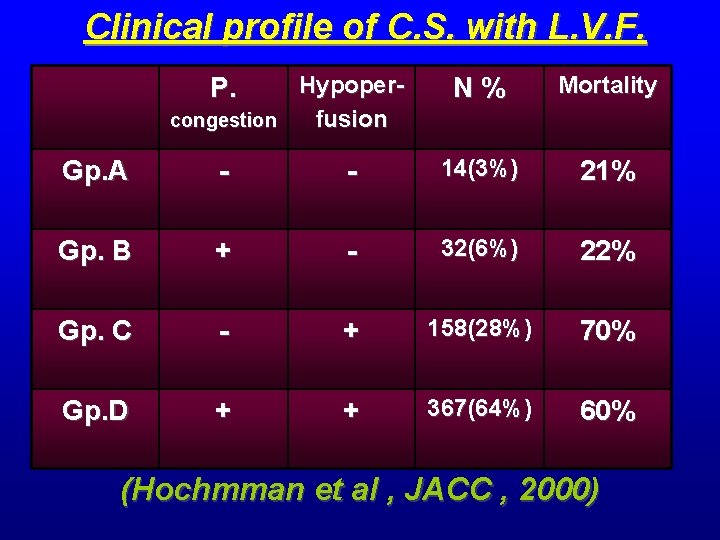
Clinical profile of C. S. with L. V. F. Hypopercongestion fusion P. N% Mortality Gp. A - - 14(3%) 21% Gp. B + - 32(6%) 22% Gp. C - + 158(28%) 70% Gp. D + + 367(64%) 60% (Hochmman et al , JACC , 2000)
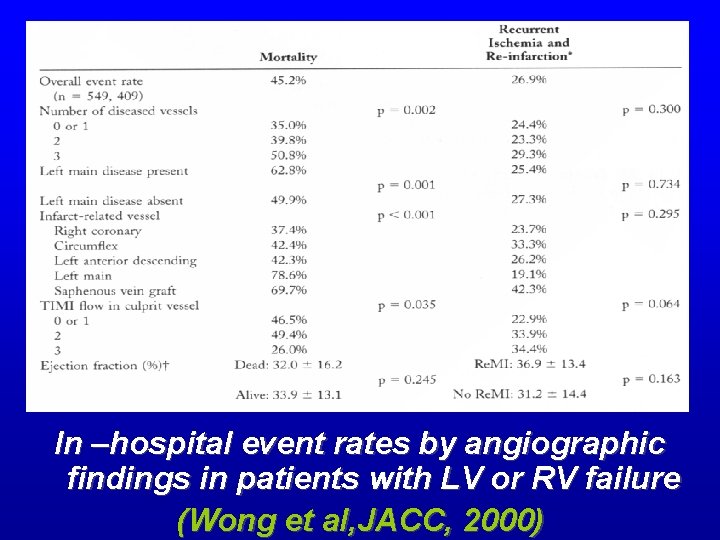
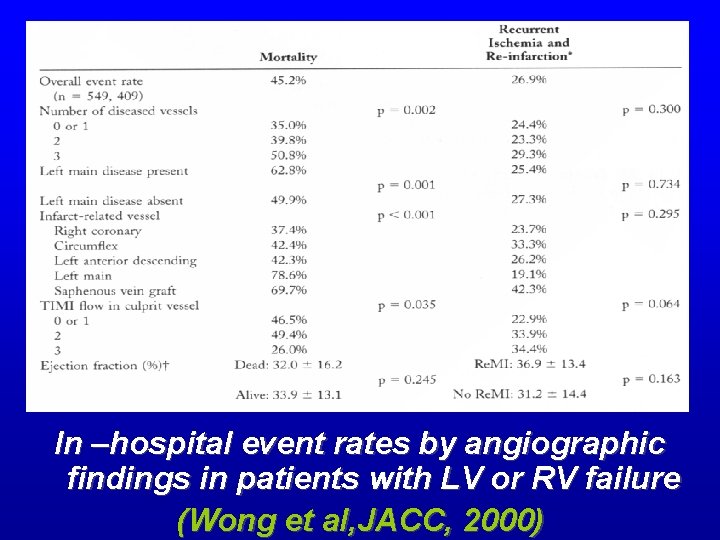
In –hospital event rates by angiographic findings in patients with LV or RV failure (Wong et al, JACC, 2000)
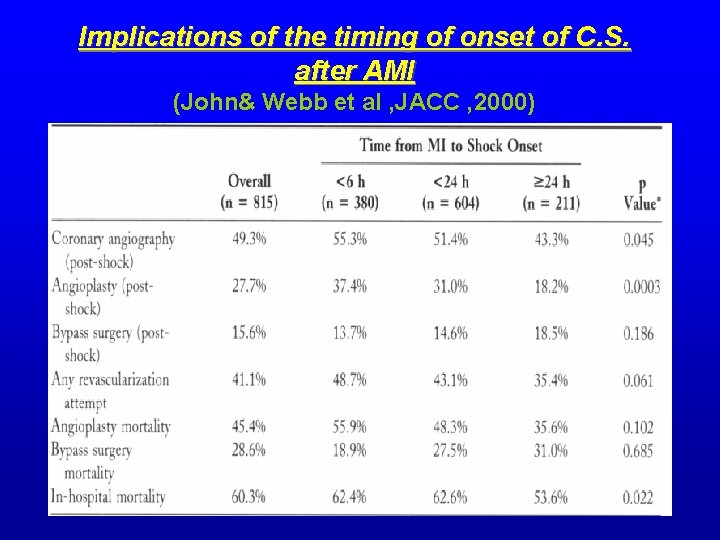
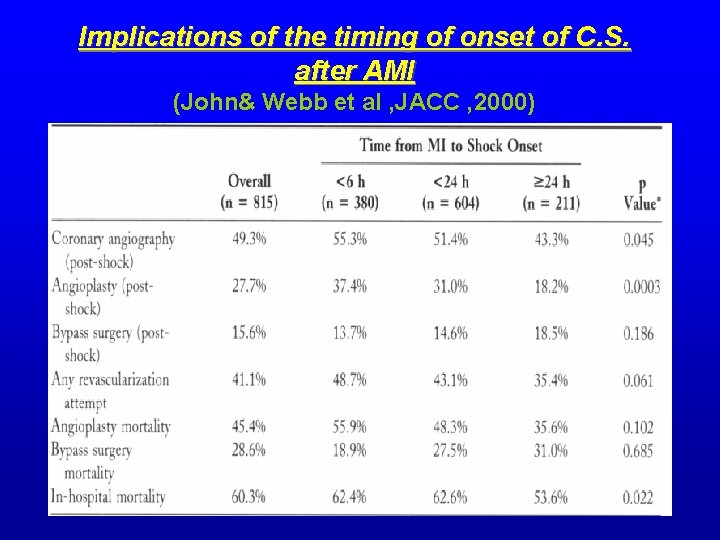
Implications of the timing of onset of C. S. after AMI (John& Webb et al , JACC , 2000)
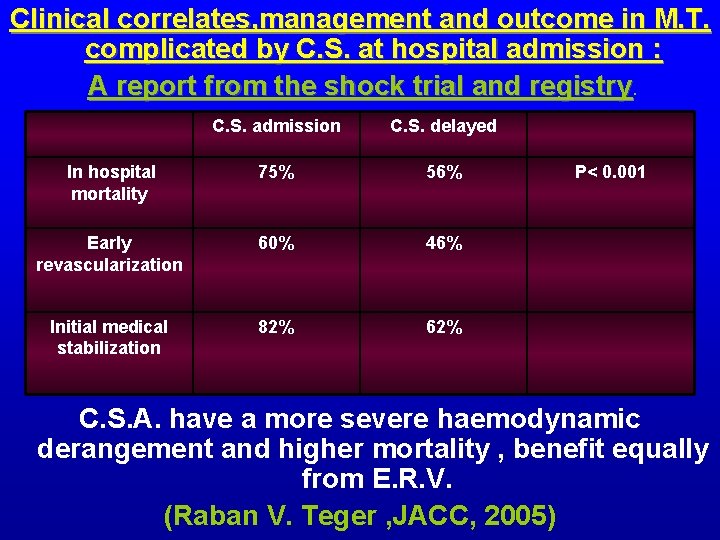
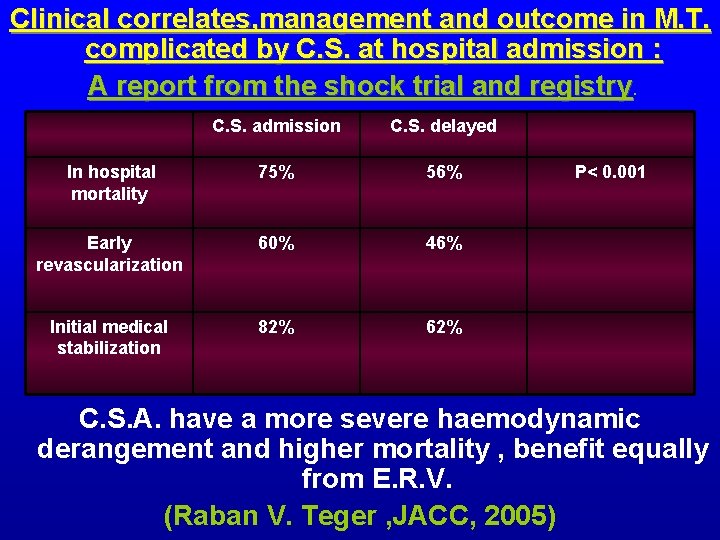
Clinical correlates, management and outcome in M. T. complicated by C. S. at hospital admission : A report from the shock trial and registry C. S. admission C. S. delayed In hospital mortality 75% 56% Early revascularization 60% 46% Initial medical stabilization 82% 62% P< 0. 001 C. S. A. have a more severe haemodynamic derangement and higher mortality , benefit equally from E. R. V. (Raban V. Teger , JACC, 2005)
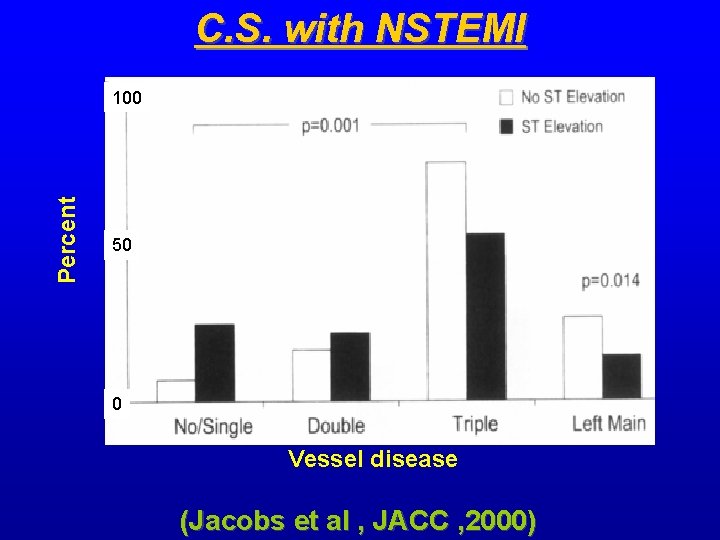
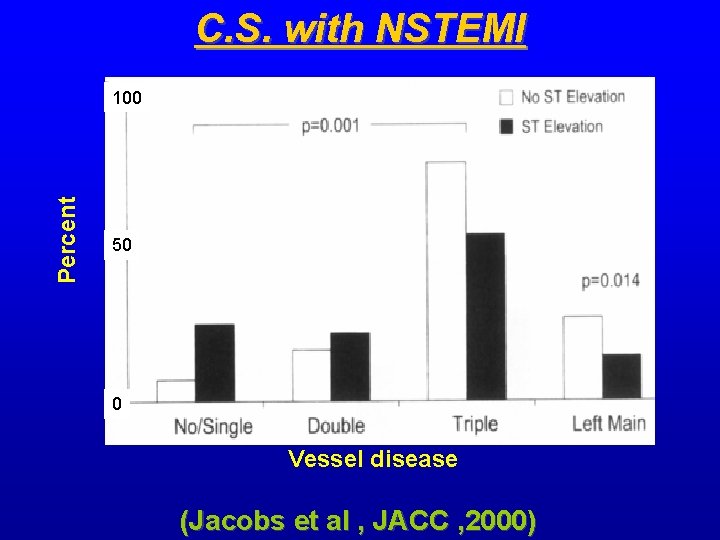
C. S. with NSTEMI Percent 100 50 0 Vessel disease (Jacobs et al , JACC , 2000)
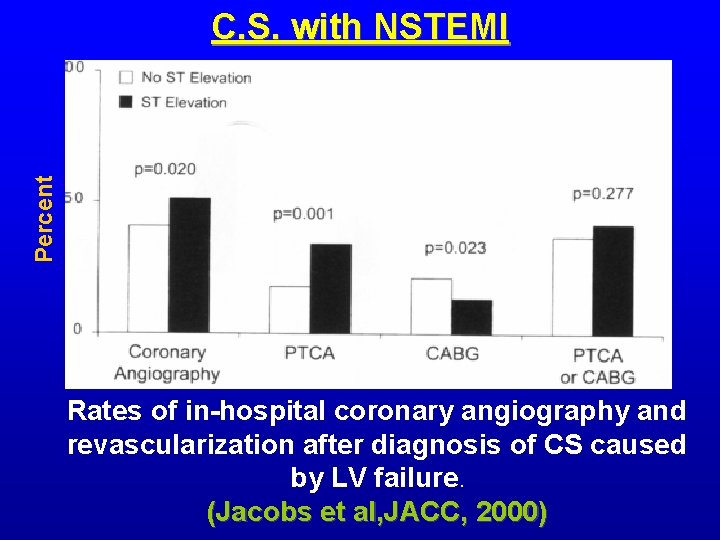
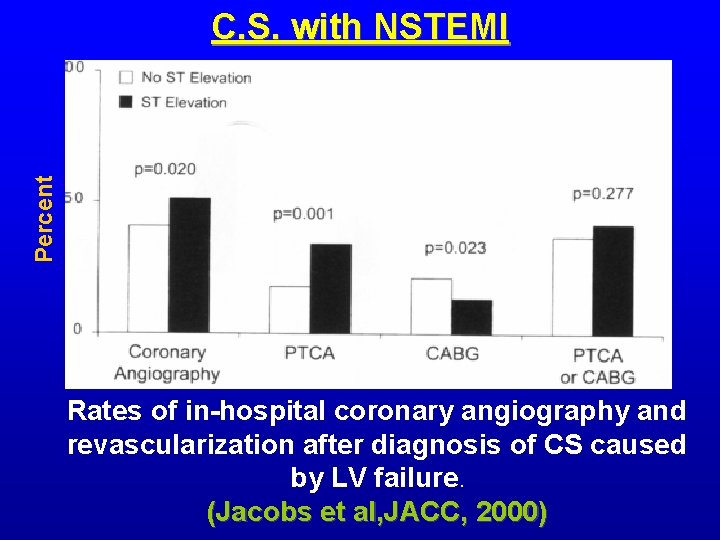
Percent C. S. with NSTEMI Rates of in-hospital coronary angiography and revascularization after diagnosis of CS caused by LV failure. (Jacobs et al, JACC, 2000)
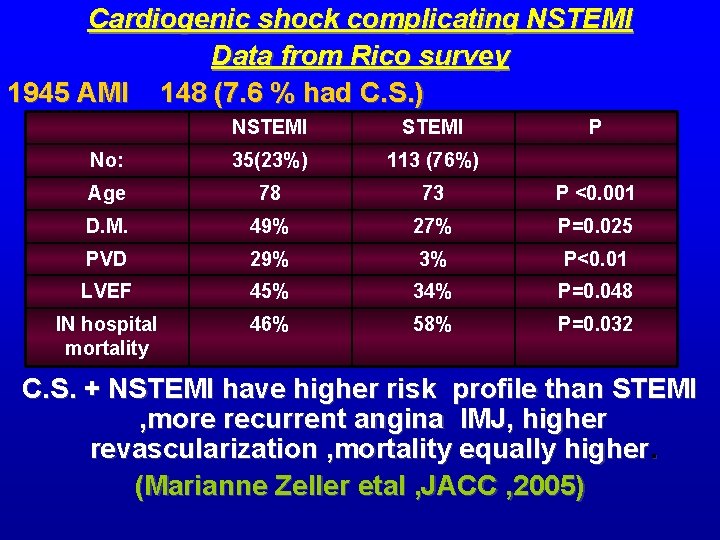
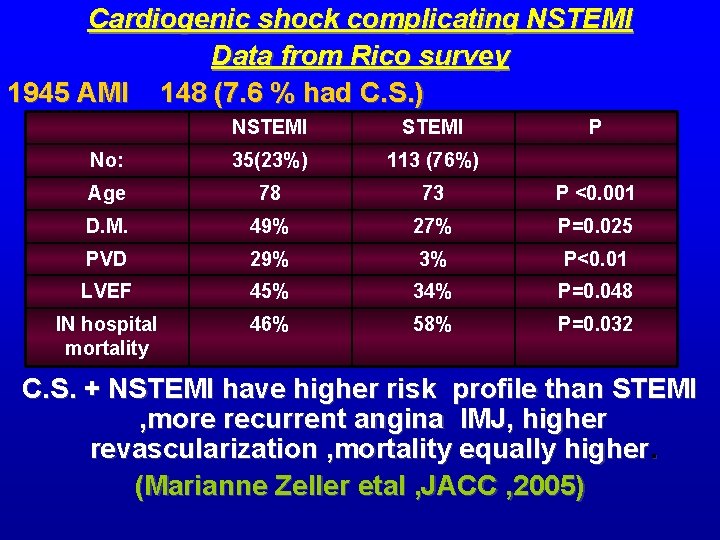
Cardiogenic shock complicating NSTEMI Data from Rico survey 1945 AMI 148 (7. 6 % had C. S. ) NSTEMI P No: 35(23%) 113 (76%) Age 78 73 P <0. 001 D. M. 49% 27% P=0. 025 PVD 29% 3% P<0. 01 LVEF 45% 34% P=0. 048 IN hospital mortality 46% 58% P=0. 032 C. S. + NSTEMI have higher risk profile than STEMI , more recurrent angina IMJ, higher revascularization , mortality equally higher. (Marianne Zeller etal , JACC , 2005)
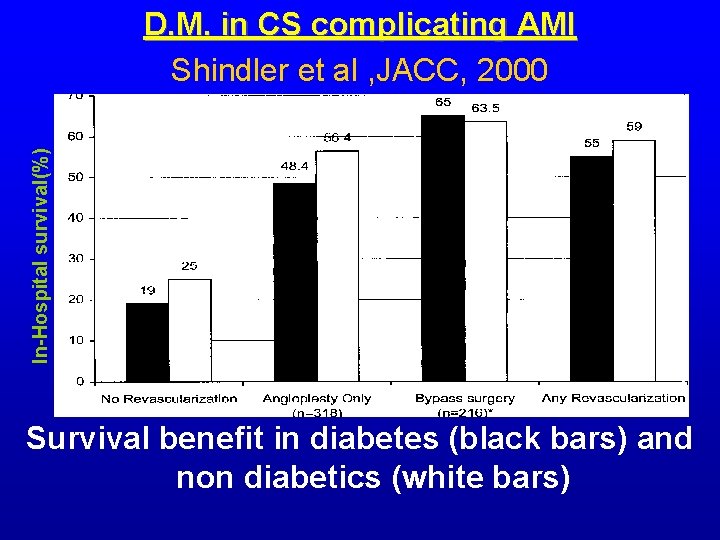
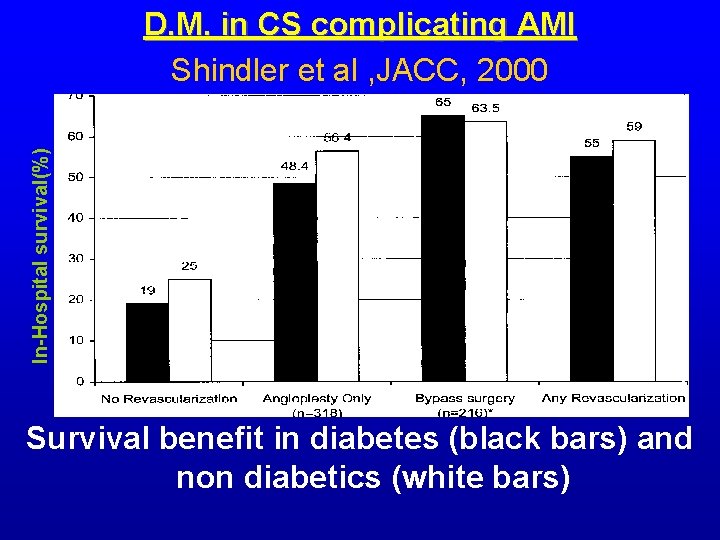
In-Hospital survival(%) D. M. in CS complicating AMI Shindler et al , JACC, 2000 Survival benefit in diabetes (black bars) and non diabetics (white bars)
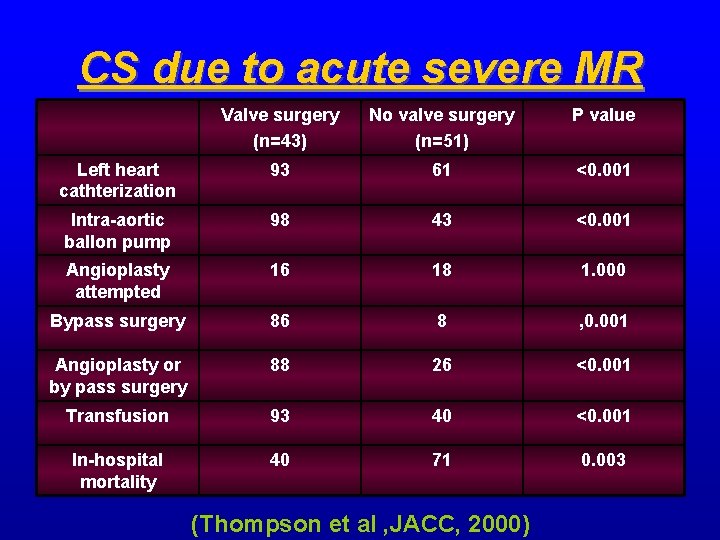
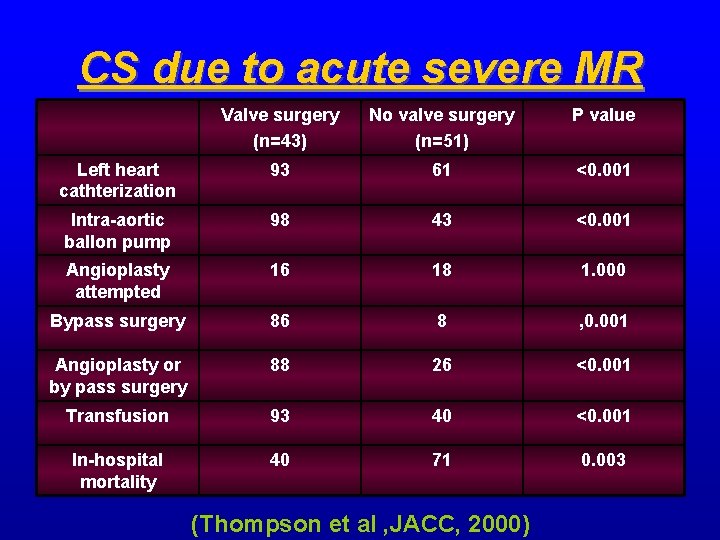
CS due to acute severe MR Valve surgery (n=43) No valve surgery (n=51) P value Left heart cathterization 93 61 <0. 001 Intra-aortic ballon pump 98 43 <0. 001 Angioplasty attempted 16 18 1. 000 Bypass surgery 86 8 , 0. 001 Angioplasty or by pass surgery 88 26 <0. 001 Transfusion 93 40 <0. 001 In-hospital mortality 40 71 0. 003 (Thompson et al , JACC, 2000)
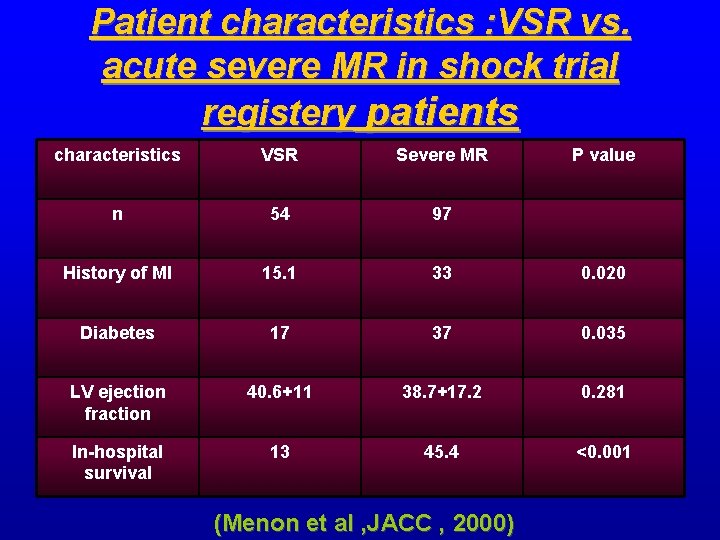
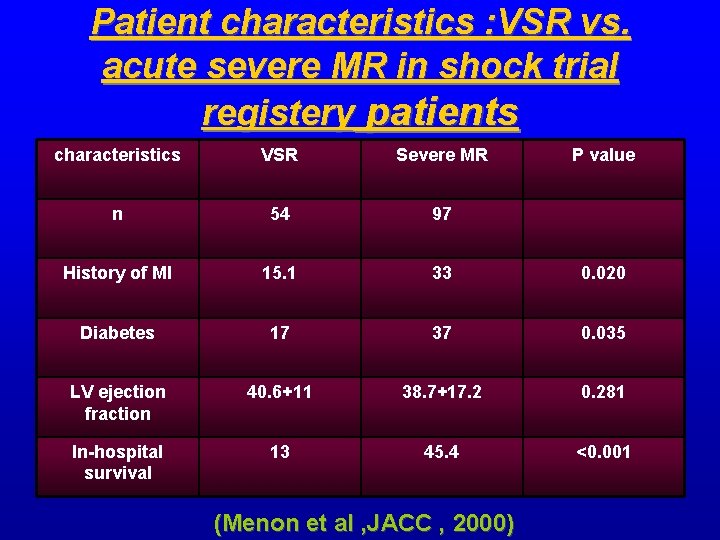
Patient characteristics : VSR vs. acute severe MR in shock trial registery patients characteristics VSR Severe MR n 54 97 History of MI 15. 1 33 0. 020 Diabetes 17 37 0. 035 LV ejection fraction 40. 6+11 38. 7+17. 2 0. 281 In-hospital survival 13 45. 4 <0. 001 (Menon et al , JACC , 2000) P value
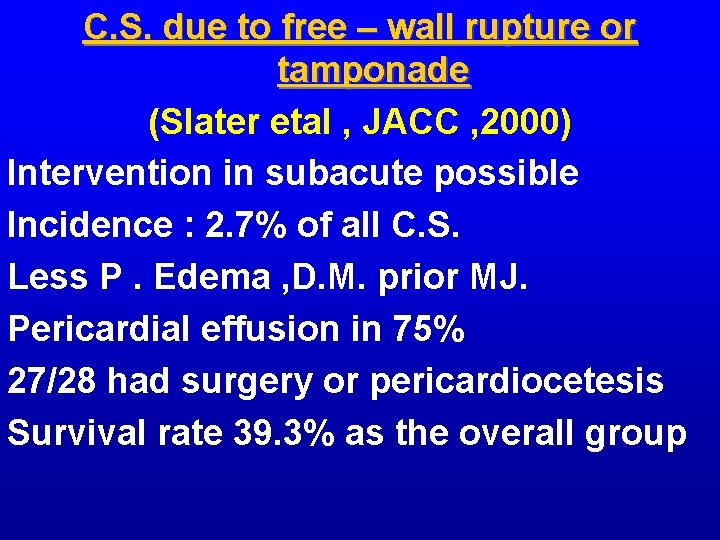
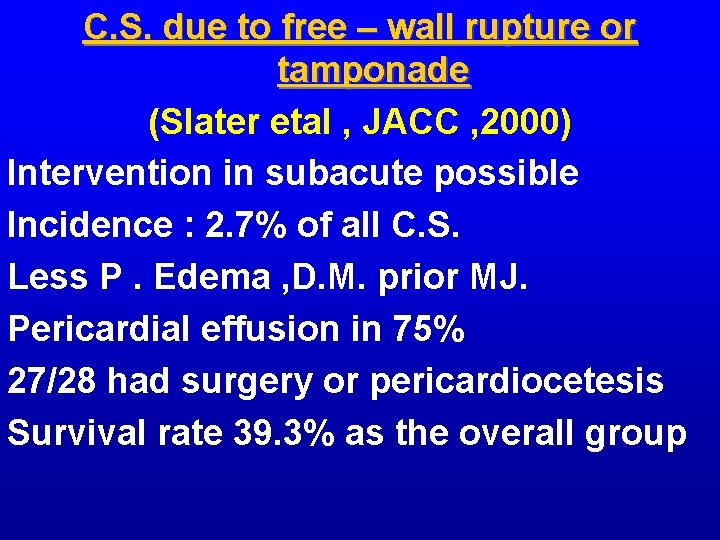
C. S. due to free – wall rupture or tamponade (Slater etal , JACC , 2000) Intervention in subacute possible Incidence : 2. 7% of all C. S. Less P. Edema , D. M. prior MJ. Pericardial effusion in 75% 27/28 had surgery or pericardiocetesis Survival rate 39. 3% as the overall group
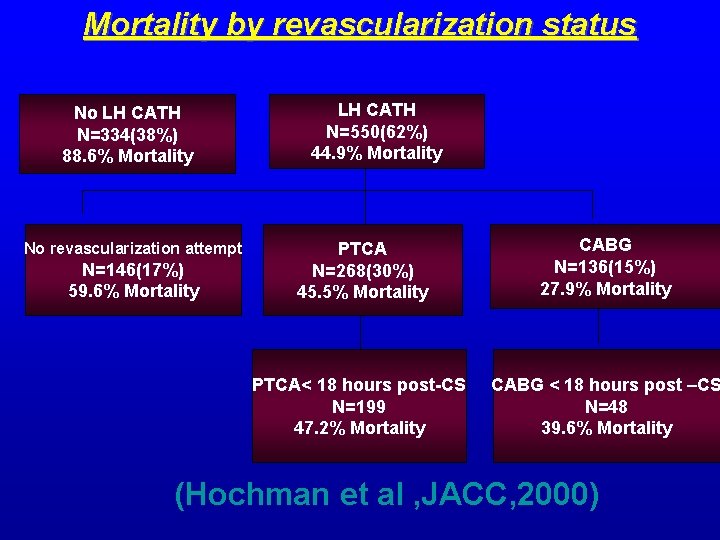
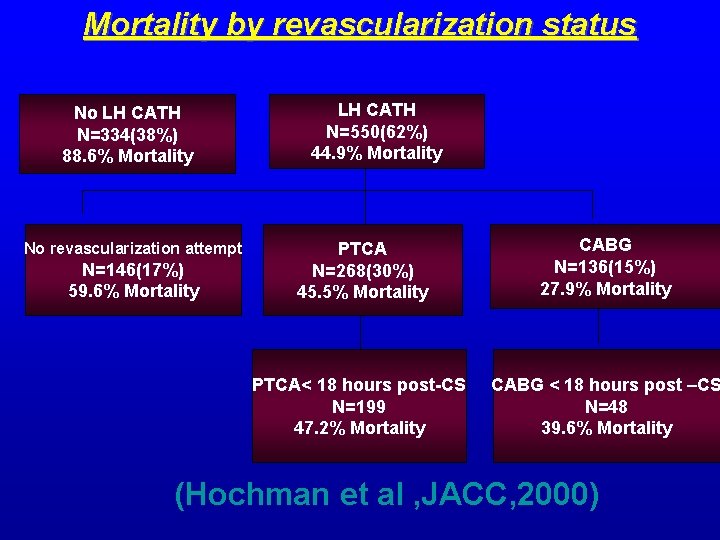
Mortality by revascularization status No LH CATH N=334(38%) 88. 6% Mortality No revascularization attempt N=146(17%) 59. 6% Mortality LH CATH N=550(62%) 44. 9% Mortality PTCA N=268(30%) 45. 5% Mortality CABG N=136(15%) 27. 9% Mortality PTCA< 18 hours post-CS N=199 47. 2% Mortality CABG < 18 hours post –CS N=48 39. 6% Mortality (Hochman et al , JACC, 2000)
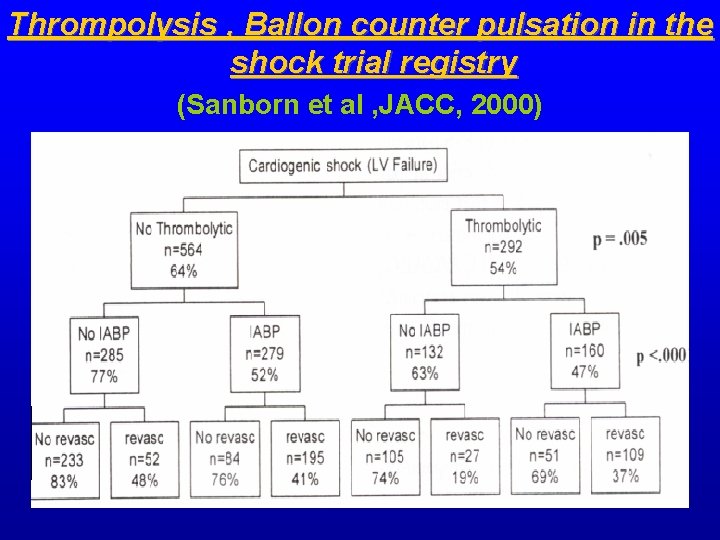
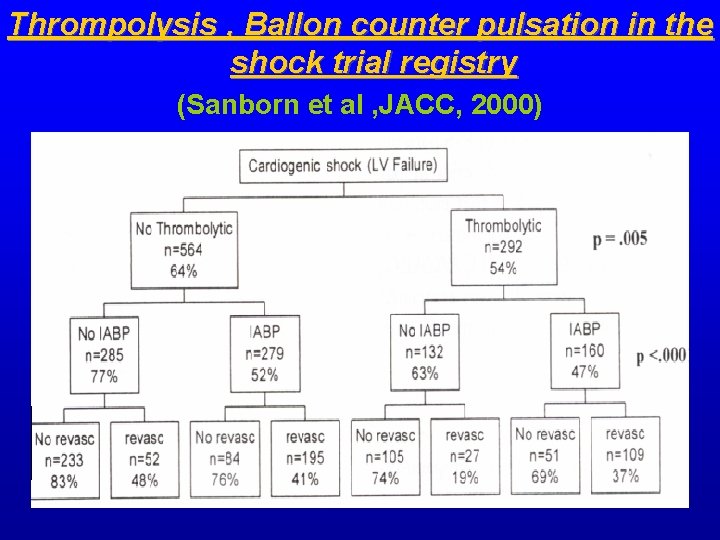
Thrompolysis , Ballon counter pulsation in the shock trial registry (Sanborn et al , JACC, 2000)
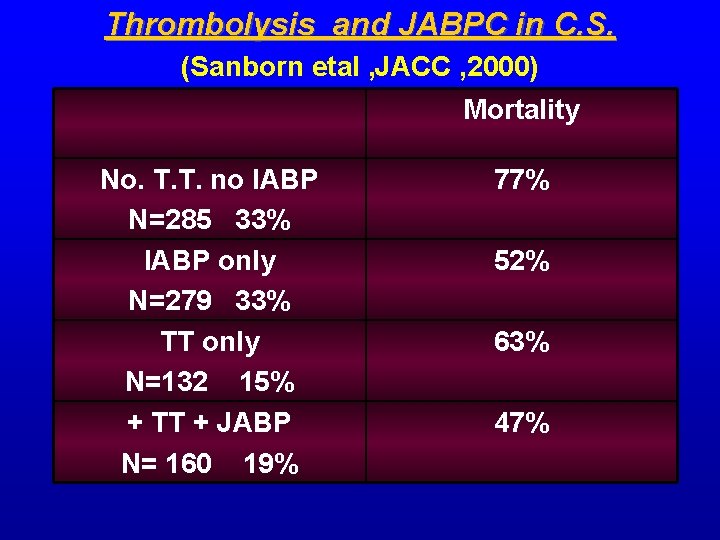
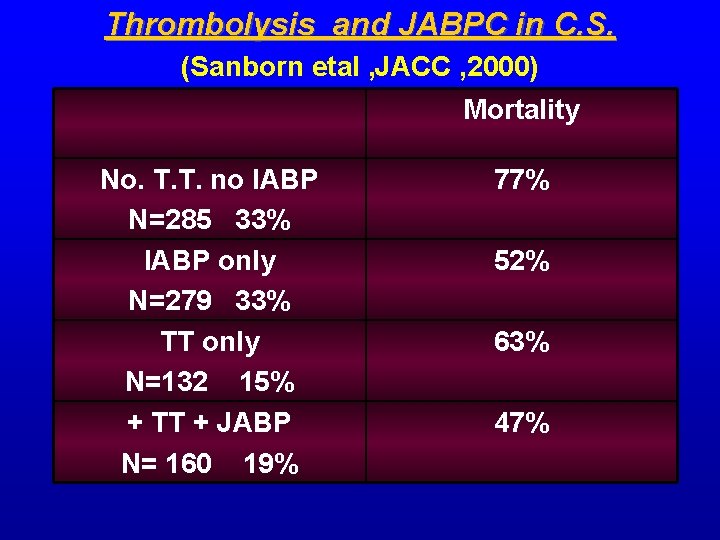
Thrombolysis and JABPC in C. S. (Sanborn etal , JACC , 2000) Mortality No. T. T. no IABP N=285 33% IABP only N=279 33% TT only N=132 15% + TT + JABP N= 160 19% 77% 52% 63% 47%
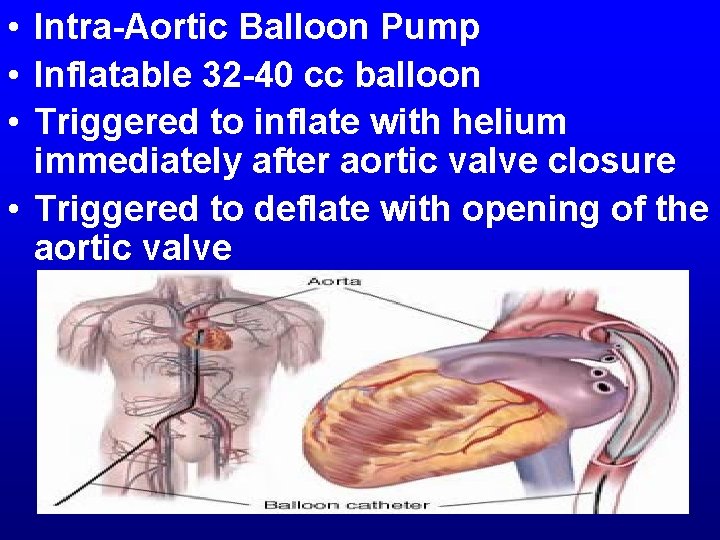
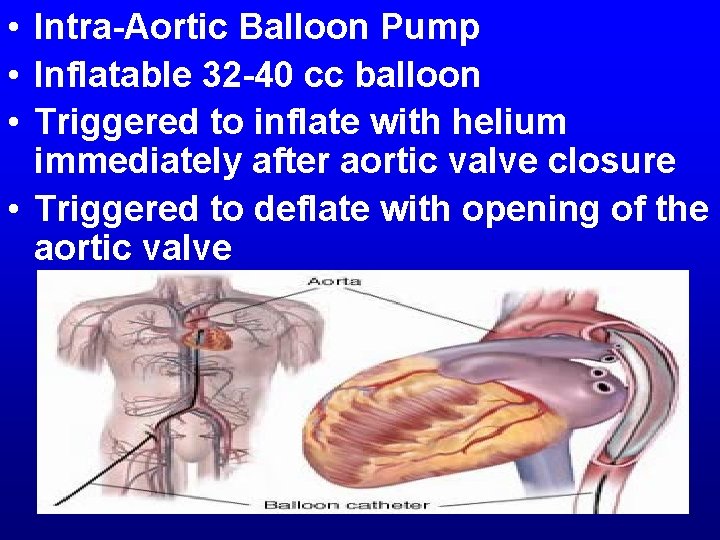
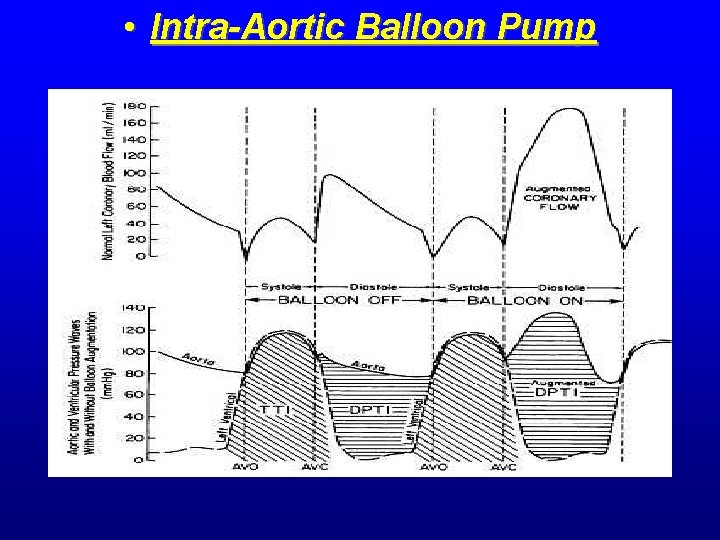
• Intra-Aortic Balloon Pump • Inflatable 32 -40 cc balloon • Triggered to inflate with helium immediately after aortic valve closure • Triggered to deflate with opening of the aortic valve
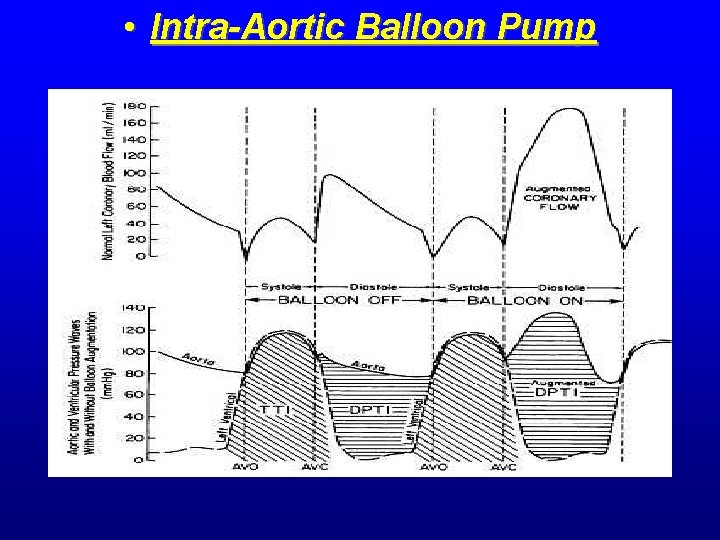
• Intra-Aortic Balloon Pump
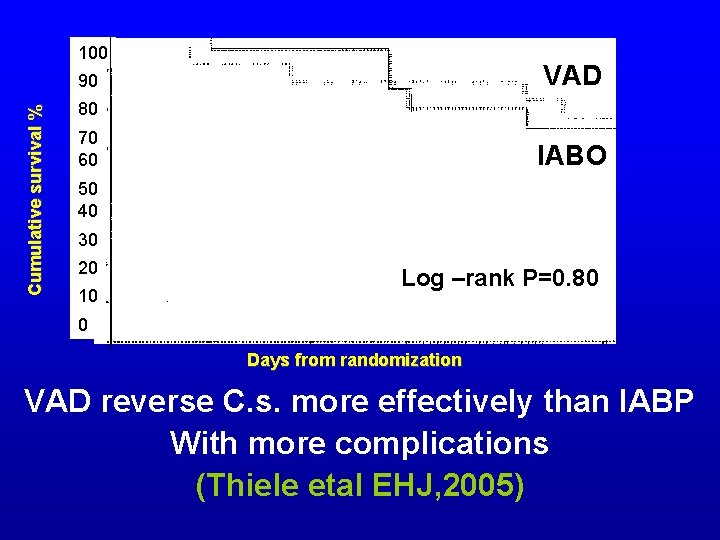
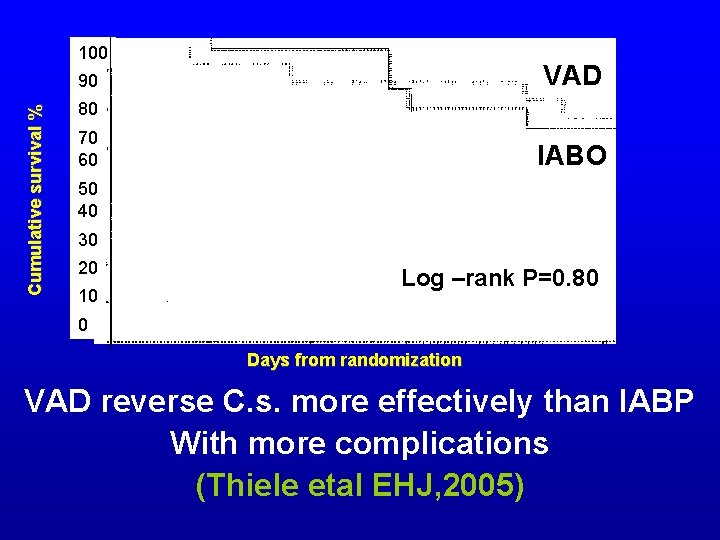
100 VAD Cumulative survival % 90 80 70 60 IABO 50 40 30 20 10 Log –rank P=0. 80 0 Days from randomization VAD reverse C. s. more effectively than IABP With more complications (Thiele etal EHJ, 2005)
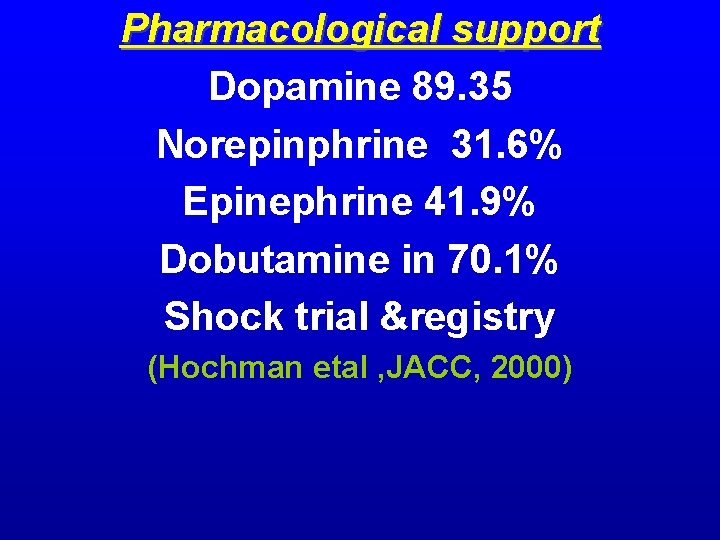
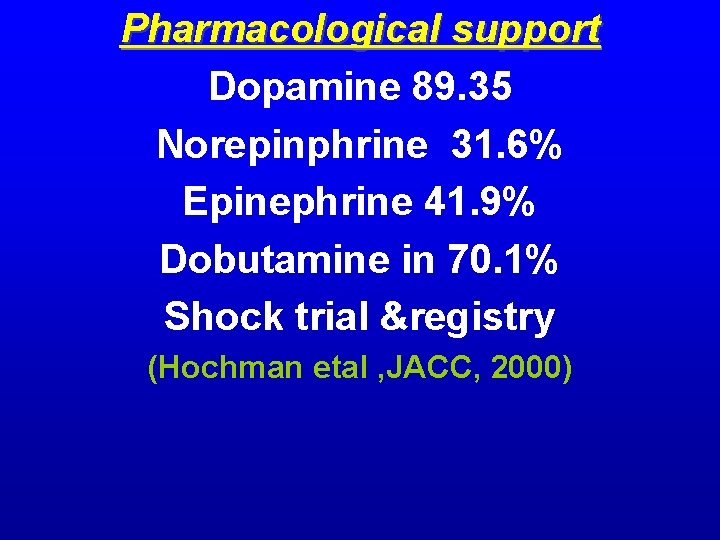
Pharmacological support Dopamine 89. 35 Norepinphrine 31. 6% Epinephrine 41. 9% Dobutamine in 70. 1% Shock trial ®istry (Hochman etal , JACC, 2000)
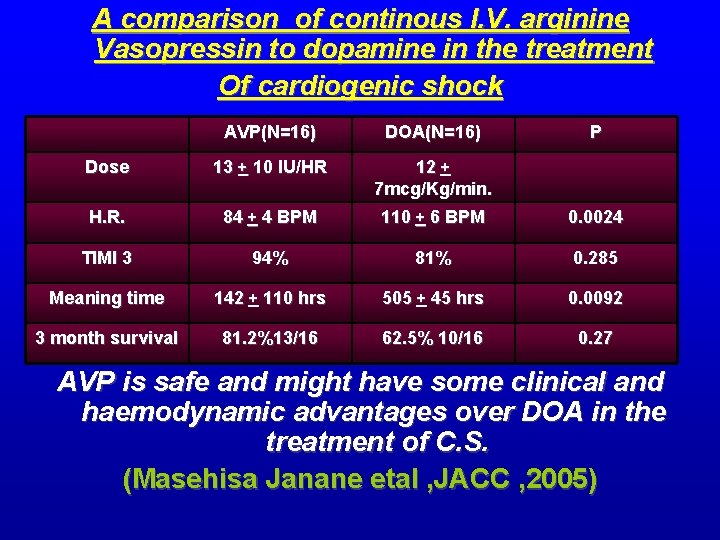
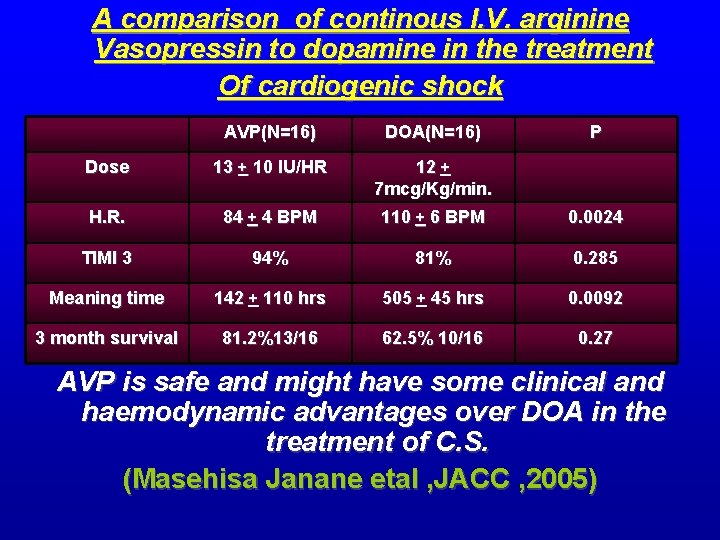
A comparison of continous I. V. arginine Vasopressin to dopamine in the treatment Of cardiogenic shock AVP(N=16) DOA(N=16) P Dose 13 + 10 IU/HR 12 + 7 mcg/Kg/min. H. R. 84 + 4 BPM 110 + 6 BPM 0. 0024 TIMI 3 94% 81% 0. 285 Meaning time 142 + 110 hrs 505 + 45 hrs 0. 0092 3 month survival 81. 2%13/16 62. 5% 10/16 0. 27 AVP is safe and might have some clinical and haemodynamic advantages over DOA in the treatment of C. S. (Masehisa Janane etal , JACC , 2005)
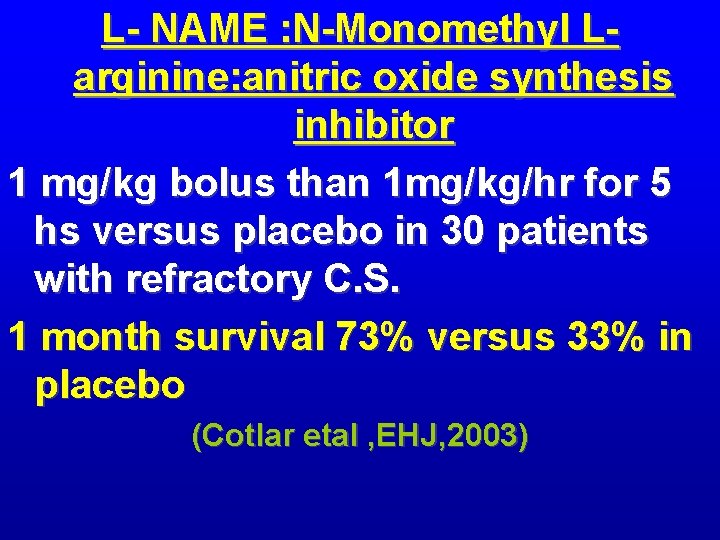
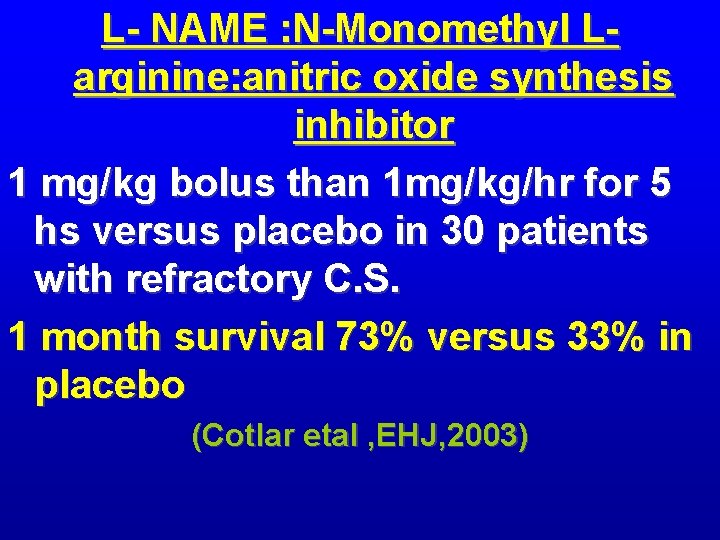
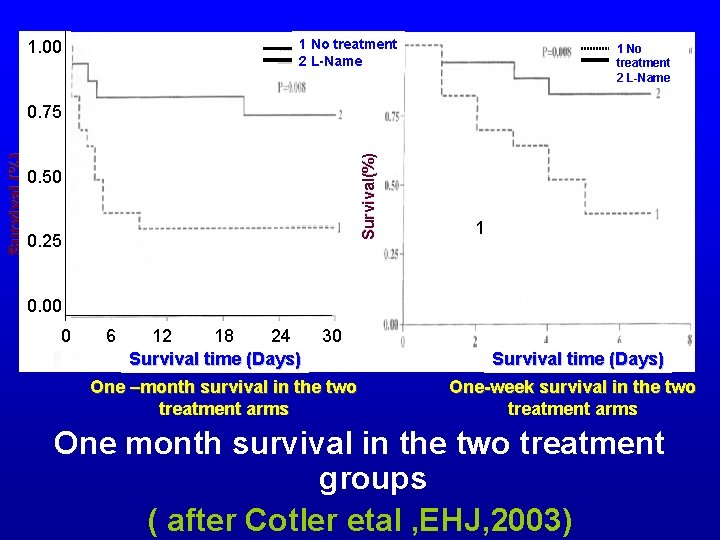
L- NAME : N-Monomethyl Larginine: anitric oxide synthesis inhibitor 1 mg/kg bolus than 1 mg/kg/hr for 5 hs versus placebo in 30 patients with refractory C. S. 1 month survival 73% versus 33% in placebo (Cotlar etal , EHJ, 2003)
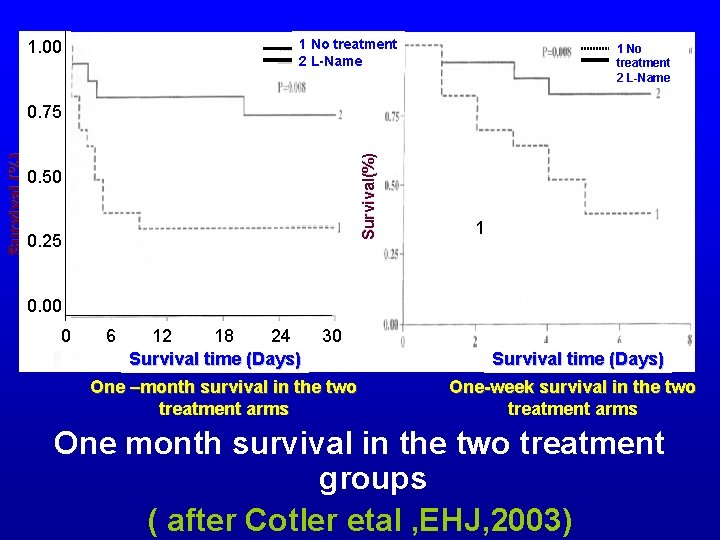
1 No treatment 2 L-Name 1. 00 1 No treatment 2 L-Name Survival(%) Survival (%) 0. 75 0. 50 0. 25 1 0. 00 1 0 6 12 18 24 Survival time (Days) 30 One –month survival in the two treatment arms Survival time (Days) One-week survival in the two treatment arms One month survival in the two treatment groups ( after Cotler etal , EHJ, 2003)
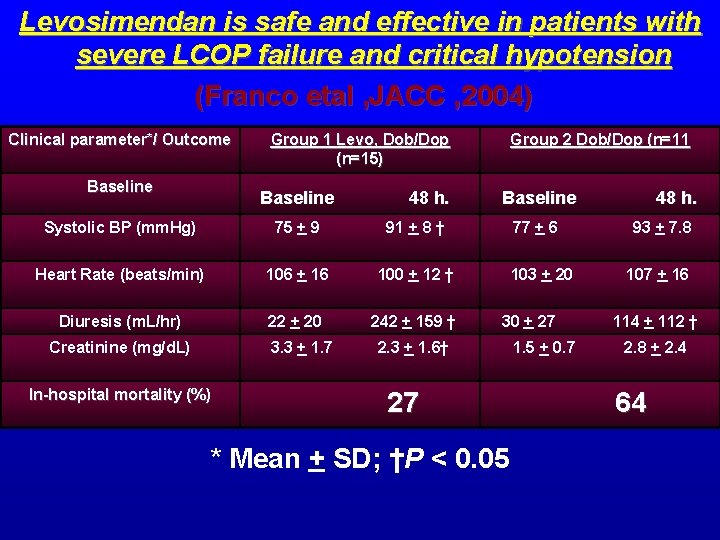
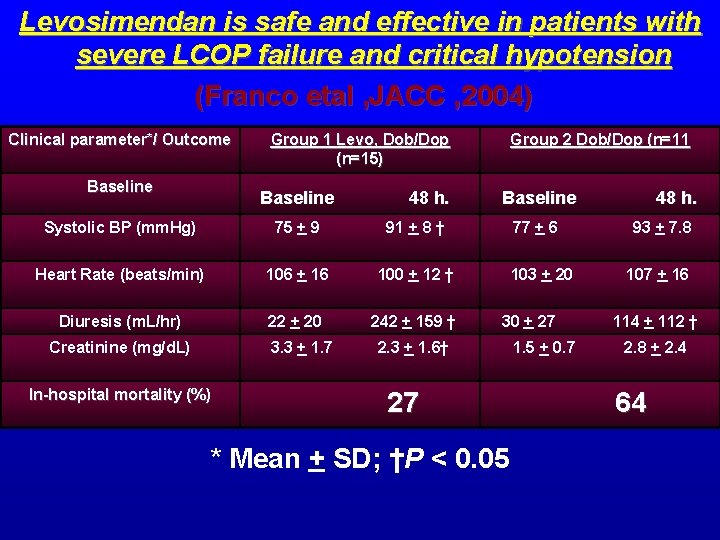
Levosimendan is safe and effective in patients with severe LCOP failure and critical hypotension (Franco etal , JACC , 2004) Clinical parameter*/ Outcome Baseline Group 1 Levo, Dob/Dop (n=15) Baseline 48 h. Systolic BP (mm. Hg) 75 + 9 91 + 8 † Heart Rate (beats/min) 106 + 16 100 + 12 † Diuresis (m. L/hr) 22 + 20 242 + 159 † Creatinine (mg/d. L) 3. 3 + 1. 7 In-hospital mortality (%) Group 2 Dob/Dop (n=11 Baseline 77 + 6 103 + 20 30 + 27 2. 3 + 1. 6† 27 * Mean + SD; †P < 0. 05 1. 5 + 0. 7 48 h. 93 + 7. 8 107 + 16 114 + 112 † 2. 8 + 2. 4 64
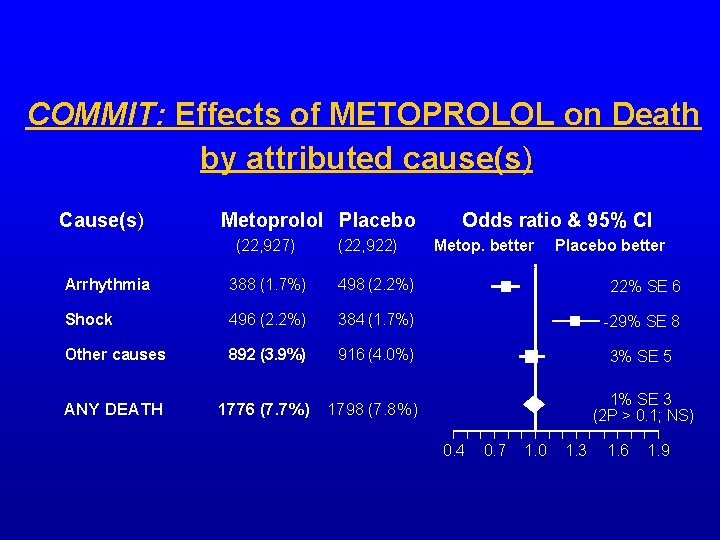
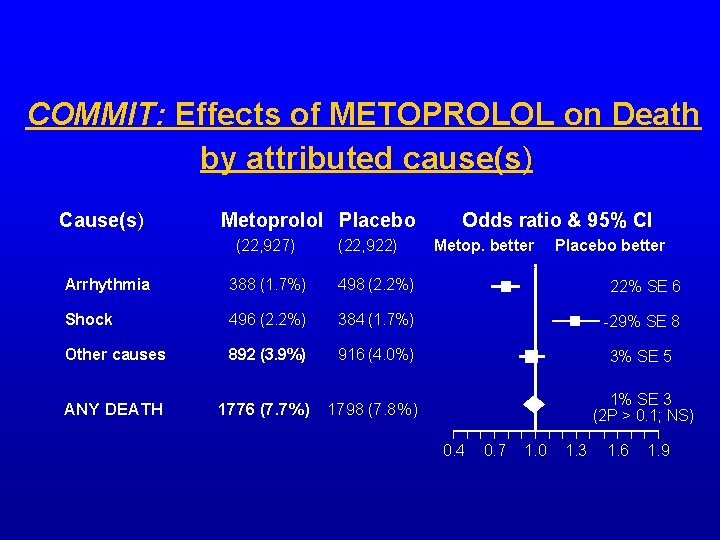
COMMIT: Effects of METOPROLOL on Death by attributed cause(s) Cause(s) Metoprolol Placebo (22, 927) (22, 922) Odds ratio & 95% CI Metop. better Placebo better Arrhythmia 388 (1. 7%) 498 (2. 2%) 22% SE 6 Shock 496 (2. 2%) 384 (1. 7%) -29% SE 8 Other causes 892 (3. 9%) 916 (4. 0%) 3% SE 5 ANY DEATH 1776 (7. 7%) 1798 (7. 8%) 1% SE 3 (2 P > 0. 1; NS) 0. 4 0. 7 1. 0 1. 3 1. 6 1. 9
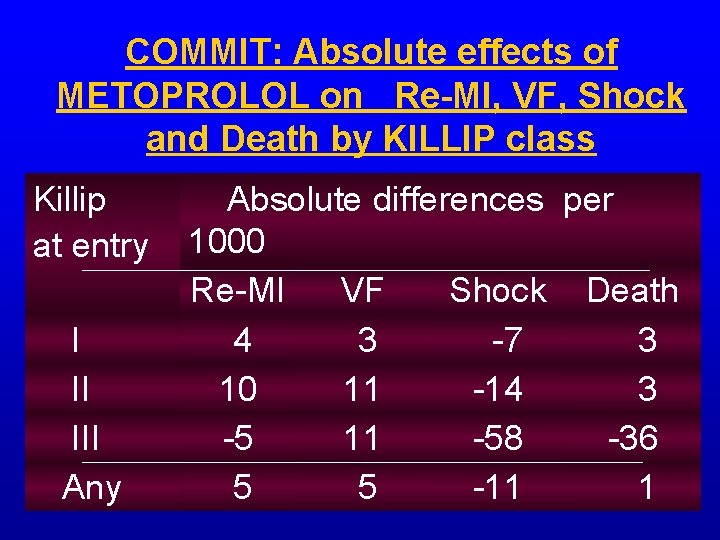
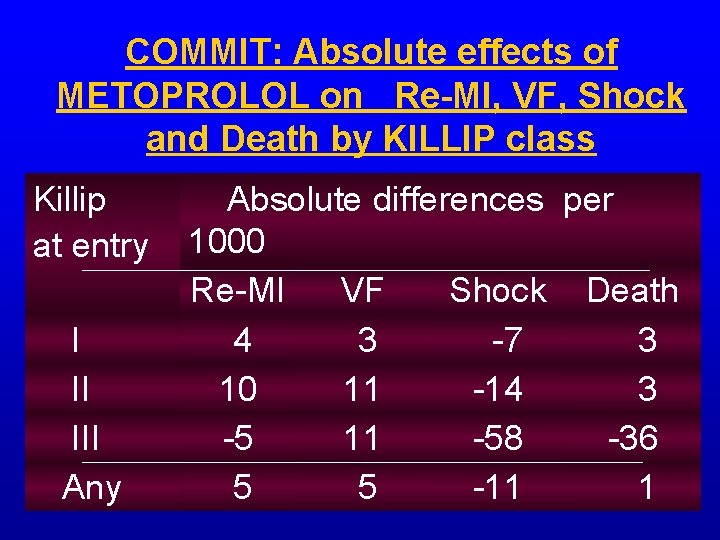
COMMIT: Absolute effects of METOPROLOL on Re-MI, VF, Shock and Death by KILLIP class Killip at entry I II III Any Absolute differences per 1000 Re-MI VF Shock Death 4 3 -7 3 10 11 -14 3 -5 11 -58 -36 5 5 -11 1
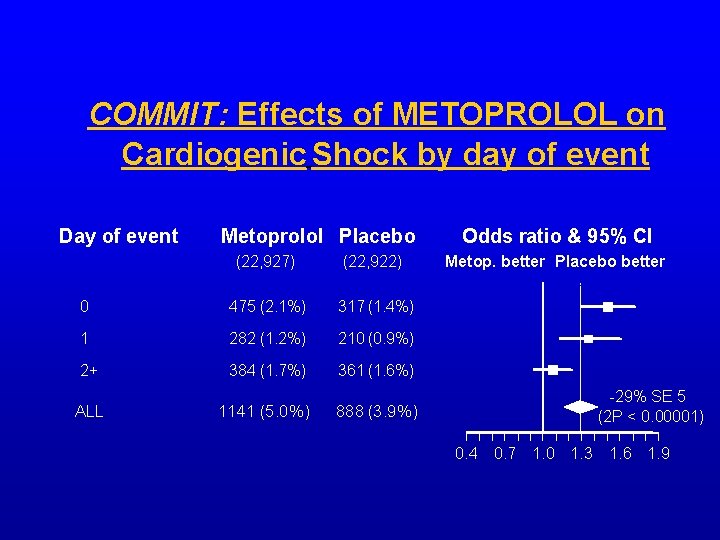
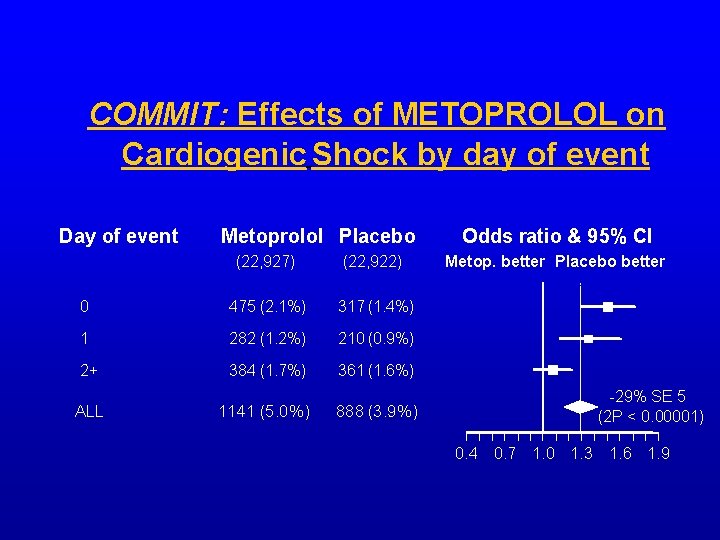
COMMIT: Effects of METOPROLOL on Cardiogenic Shock by day of event Day of event Metoprolol Placebo (22, 927) (22, 922) 0 475 (2. 1%) 317 (1. 4%) 1 282 (1. 2%) 210 (0. 9%) 2+ 384 (1. 7%) 361 (1. 6%) ALL 1141 (5. 0%) Odds ratio & 95% CI Metop. better Placebo better -29% SE 5 (2 P < 0. 00001) 888 (3. 9%) 0. 4 0. 7 1. 0 1. 3 1. 6 1. 9
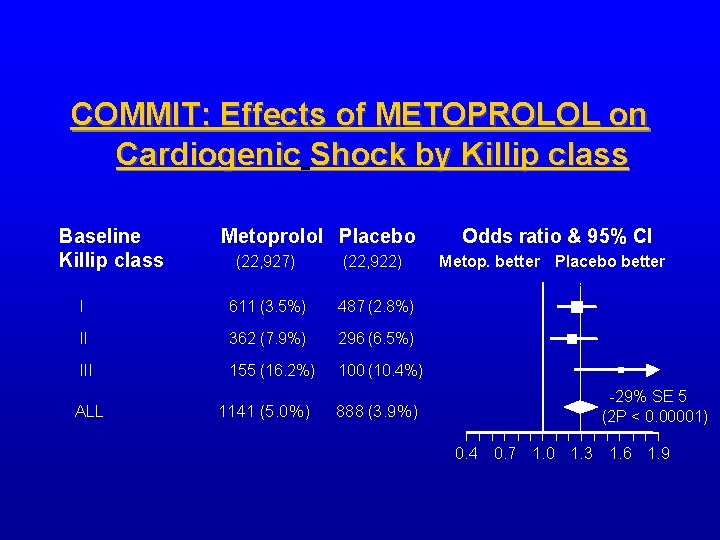
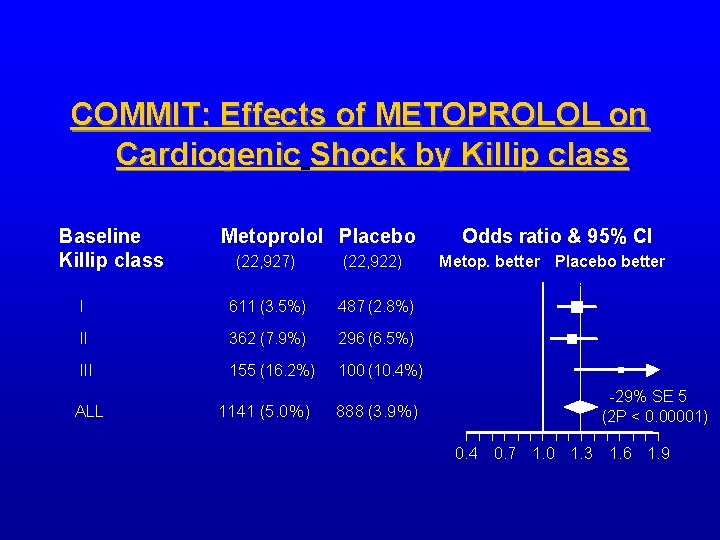
COMMIT: Effects of METOPROLOL on Cardiogenic Shock by Killip class Baseline Killip class Metoprolol Placebo (22, 927) (22, 922) I 611 (3. 5%) 487 (2. 8%) II 362 (7. 9%) 296 (6. 5%) III 155 (16. 2%) 100 (10. 4%) ALL 1141 (5. 0%) Odds ratio & 95% CI Metop. better Placebo better -29% SE 5 (2 P < 0. 00001) 888 (3. 9%) 0. 4 0. 7 1. 0 1. 3 1. 6 1. 9
The CAPTIM Had a lower incidince of cardiogenic shock in the pre-hospital thrombolysis arm than in the primary PCI arm (Bonnefoy E et al , Lancet , 2002)
C. S. death predictors (1) Previous MI (2) Age > 70 Y. (3) Failed thrombolysis (Suttor et al , BMJ , 2005)
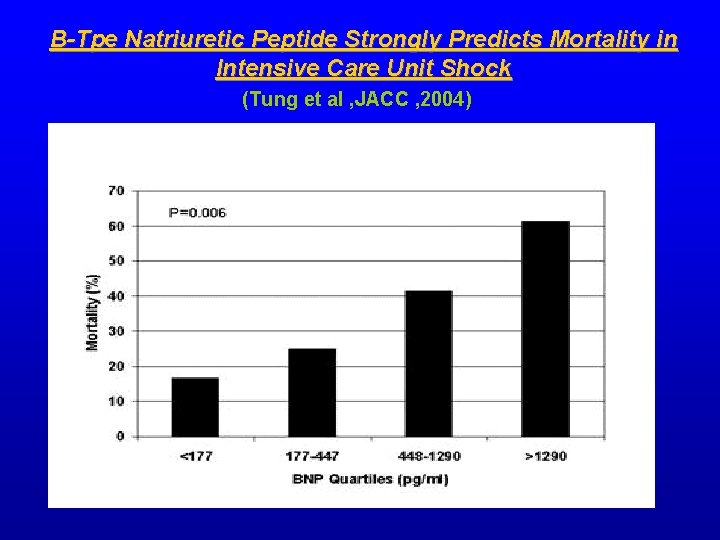
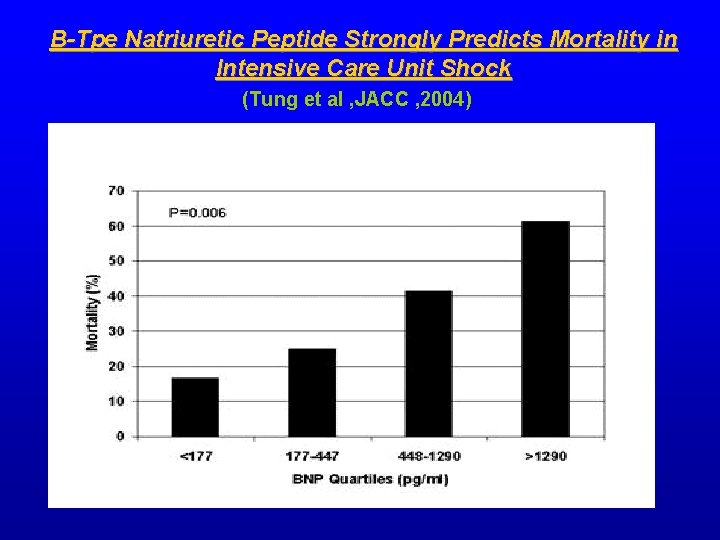
B-Tpe Natriuretic Peptide Strongly Predicts Mortality in Intensive Care Unit Shock (Tung et al , JACC , 2004)
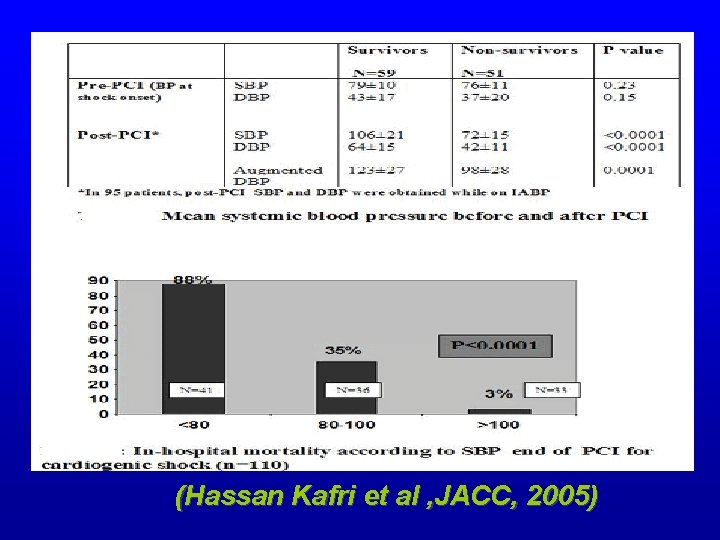
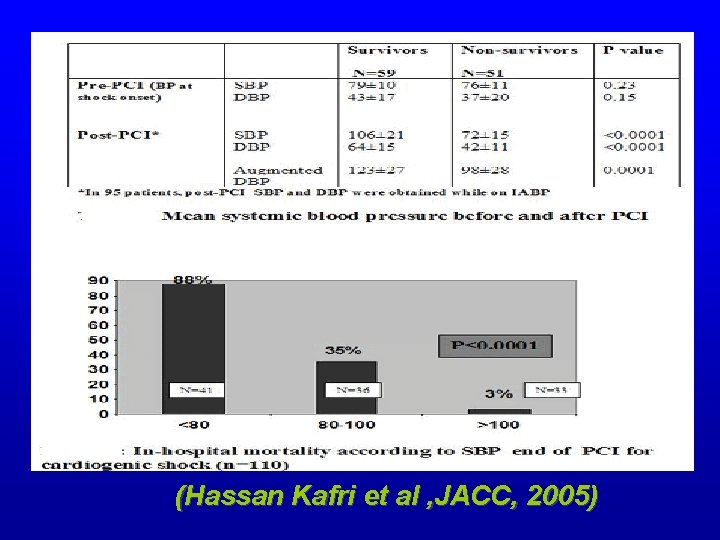
(Hassan Kafri et al , JACC, 2005)
C. S. with preserved L. V. systolic function (Nayar etal , JACC , 2004) Shock trial : 24 patient had EF > 37% Had non-dilated L. V. + abnormal vascular tone C. S.
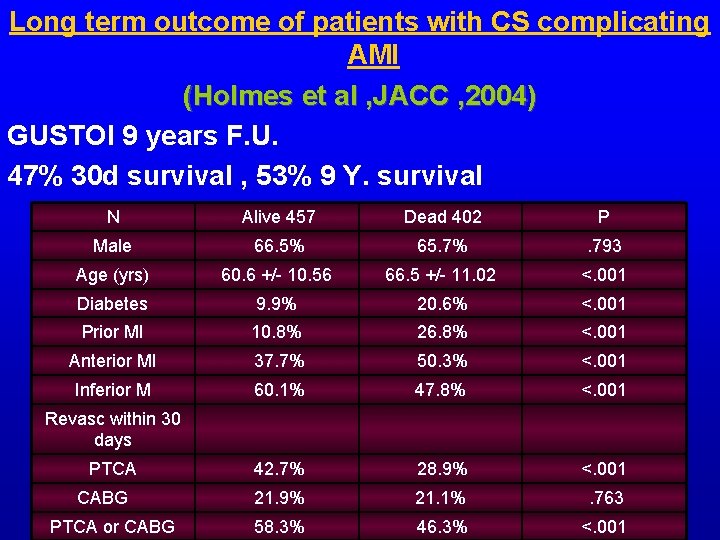
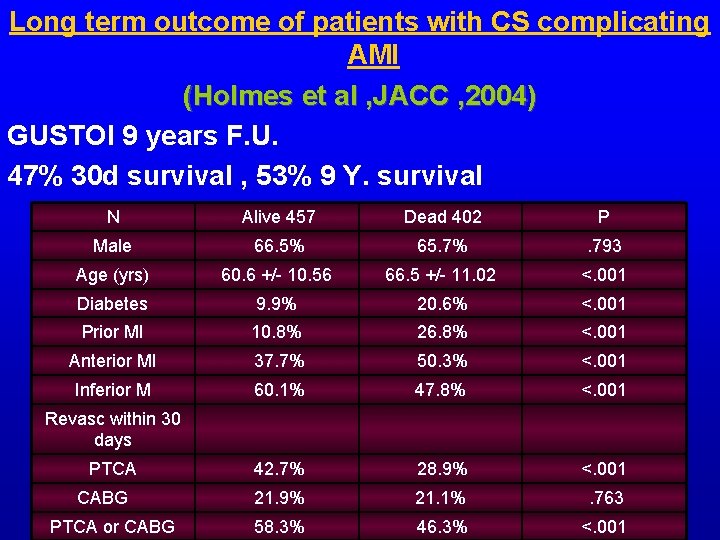
Long term outcome of patients with CS complicating AMI (Holmes et al , JACC , 2004) GUSTOI 9 years F. U. 47% 30 d survival , 53% 9 Y. survival N Alive 457 Dead 402 P Male 66. 5% 65. 7% . 793 Age (yrs) 60. 6 +/- 10. 56 66. 5 +/- 11. 02 <. 001 Diabetes 9. 9% 20. 6% <. 001 Prior MI 10. 8% 26. 8% <. 001 Anterior MI 37. 7% 50. 3% <. 001 Inferior M 60. 1% 47. 8% <. 001 42. 7% 28. 9% <. 001 21. 9% 21. 1% . 763 58. 3% 46. 3% <. 001 Revasc within 30 days PTCA CABG PTCA or CABG
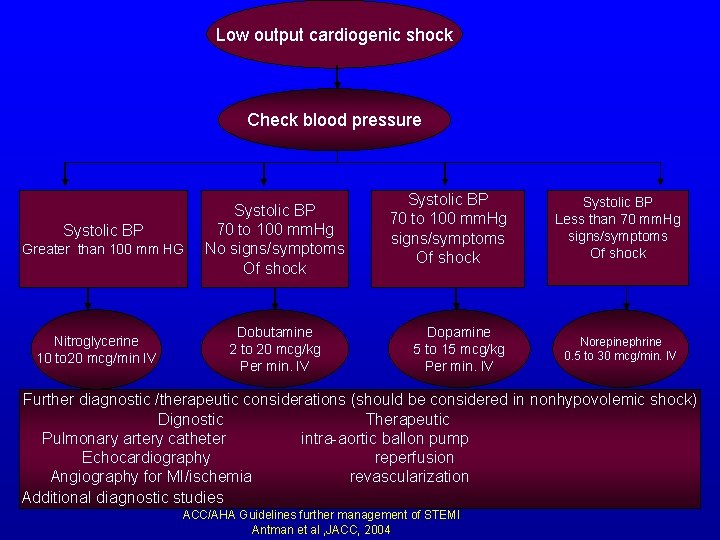
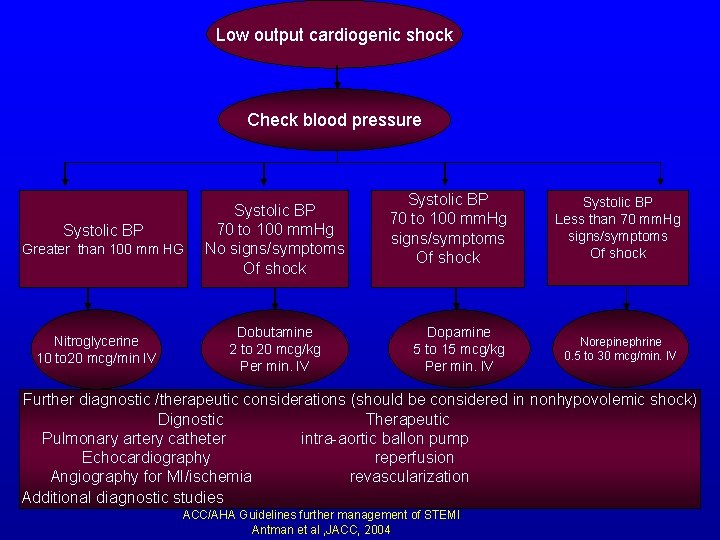
Low output cardiogenic shock Check blood pressure Systolic BP Greater than 100 mm HG Nitroglycerine 10 to 20 mcg/min IV Systolic BP 70 to 100 mm. Hg No signs/symptoms Of shock Dobutamine 2 to 20 mcg/kg Per min. IV Systolic BP 70 to 100 mm. Hg signs/symptoms Of shock Systolic BP Less than 70 mm. Hg signs/symptoms Of shock Dopamine 5 to 15 mcg/kg Per min. IV Norepinephrine 0. 5 to 30 mcg/min. IV Further diagnostic /therapeutic considerations (should be considered in nonhypovolemic shock) Dignostic Therapeutic Pulmonary artery catheter intra-aortic ballon pump Echocardiography reperfusion Angiography for MI/ischemia revascularization Additional diagnostic studies ACC/AHA Guidelines further management of STEMI Antman et al , JACC, 2004
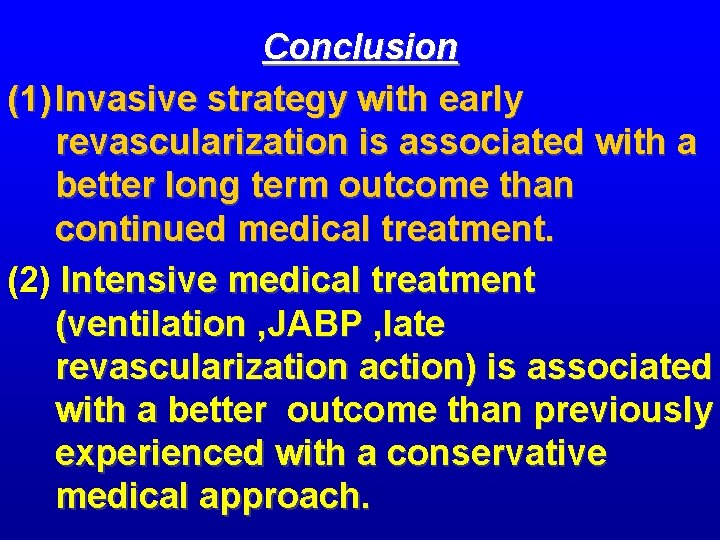
Conclusion (1) Invasive strategy with early revascularization is associated with a better long term outcome than continued medical treatment. (2) Intensive medical treatment (ventilation , JABP , late revascularization action) is associated with a better outcome than previously experienced with a conservative medical approach.
