Causation in Clinical Negligence ANDREW RITCHIE QC 9










- Slides: 51
Causation in Clinical Negligence ANDREW RITCHIE QC 9 Gough Square LONDON PI & clin neg QC of the year Legal 500 2015 PI & Clin neg QC of the year Chambers & partners 2015 Head of Chambers, 9 GS MD of PIc. Arbs Copyright A Ritchie QC
The Buffalo Lecture
Causation in clin neg § Breach is a test but Causation overwhelms the rest § We get excited about breach § We are tested by causation § Standard test is the but for test § But for the negligence of the hospital C would have been: uninjured, much healthier, mobile … § The but for test is all about opinion evidence and logic
Logic is dangerous: it can prove anything … § “Is God willing to prevent evil, but not able? § Then he is not omnipotent. § Is he able, but not willing? § Then he is malevolent. § Is he both able and willing? § Then whence cometh evil? § Is he neither able nor willing? § Then why call him God? ” ― Epicurus
Clinical negligence Hypoxia claims produce the most tricky causation issues Hypoxia at birth creates the most mild/moderate brain injuries
What is hypoxia? § Intrauterine hypoxia occurs when the fetus is deprived of an adequate supply of oxygen. § Either: during gestation or during birth (perinatal asphyxia) Andrew Ritchie QC 6

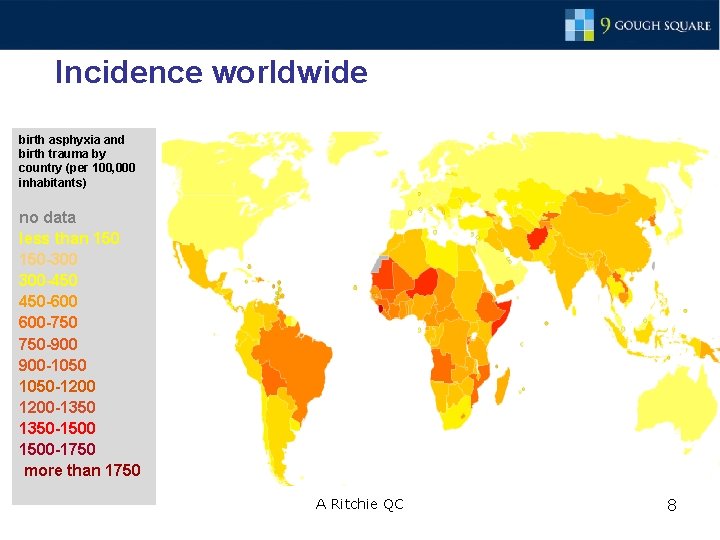
How many each year? § The World Health Organization estimates globally, 4– 9 million newborns pa suffer birth asphyxia. § 1. 2 million die pa. § Over 1 million babies develop severe disability. § In technologically advanced countries the incidence of hypoxic-ischemic encephalopathy is around 150 per 100, 000 births. § But elsewhere …. . A Ritchie QC 7
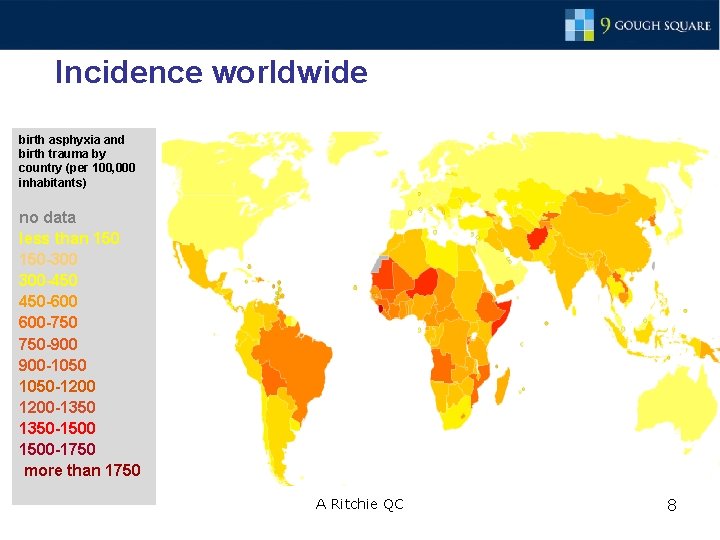
Incidence worldwide birth asphyxia and birth trauma by country (per 100, 000 inhabitants) no data less than 150 -300 300 -450 450 -600 600 -750 750 -900 900 -1050 1050 -1200 1200 -1350 1350 -1500 1500 -1750 more than 1750 A Ritchie QC 8
Causation: the Causes of hypoxia § § There are many natural causes: § cord prolapse or occlusion § placental infarction, abruption or failure § maternal smoking, § prolonged labour, § breech delivery, § uterine rupture. There also negligent causes: § failure to spot fetal distress – usually by failing to use/read/understand an “ominous” CTG trace; § failure to do a C-section fast enough or at all; § taking too long with a ventouse/forceps or failing to release an impacted head; § failure to intubate or resuscitate properly after birth. A Ritchie QC 9
Causation: the types of hypoxia § Two types of hypoxia § total hypoxia – acute profound – complete cessation of the oxygenated blood supply. For instance: blocking the umbilical cord. § partial hypoxia, “on and off” blood supply. For instance: gripping the cord and then letting go, then gripping it again (during contractions). A Ritchie QC 10
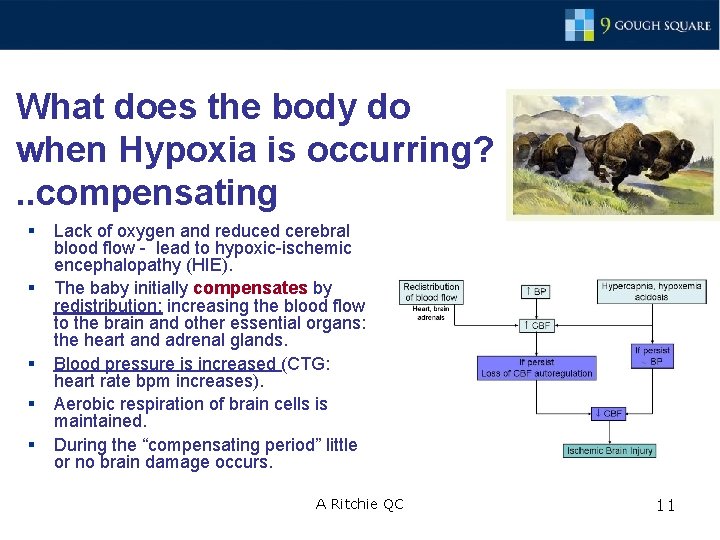
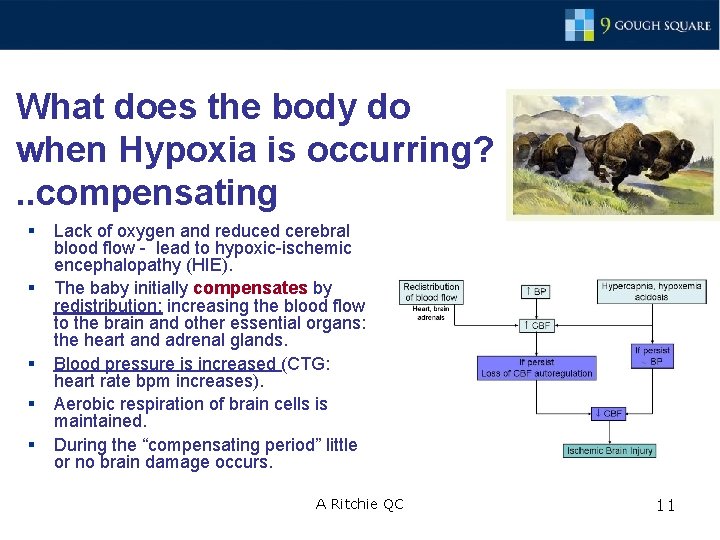
What does the body do when Hypoxia is occurring? . . compensating § § § Lack of oxygen and reduced cerebral blood flow - lead to hypoxic-ischemic encephalopathy (HIE). The baby initially compensates by redistribution: increasing the blood flow to the brain and other essential organs: the heart and adrenal glands. Blood pressure is increased (CTG: heart rate bpm increases). Aerobic respiration of brain cells is maintained. During the “compensating period” little or no brain damage occurs. A Ritchie QC 11
Then cells fall off the cliff § Then when the compensation mechanisms fail § The heart rate goes down and become erratic: (CTG: trace: pathological decelerations) § Aerobic respiration is no longer possible § Anaerobic respiration starts § Acidosis builds up (cord blood ph test) § Cell damage arises quickly § Cells fall off a cliff A Ritchie QC 12
So what is Aerobic respiration? § Aerobic respiration is good: § Cells take in oxygen, burn sugar and excrete CO 2 and water. § Anaerobic Respiration is bad: § As the hypoxia builds, with no oxygen, brain cells cease aerobic respiration. § When there is no oxygen cells start anaerobic respiration. A Ritchie QC 13
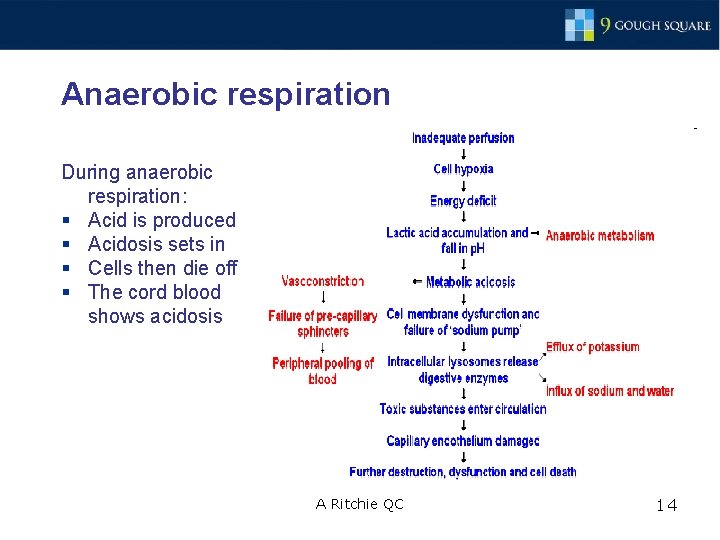
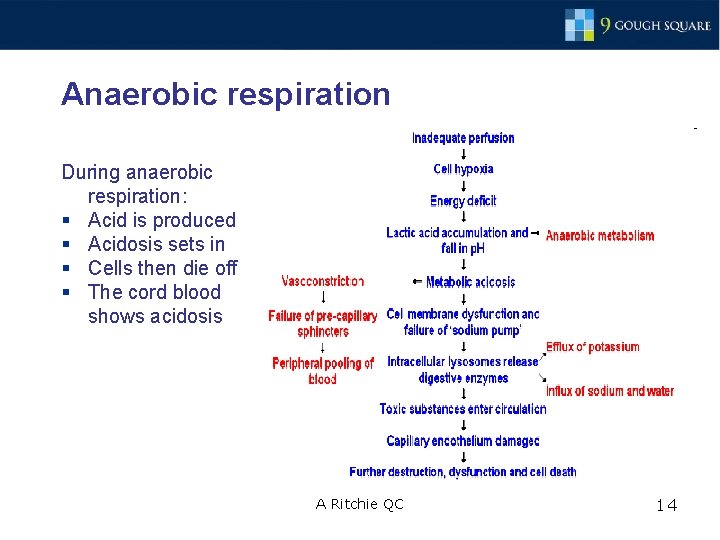
Anaerobic respiration During anaerobic respiration: § Acid is produced § Acidosis sets in § Cells then die off § The cord blood shows acidosis A Ritchie QC 14
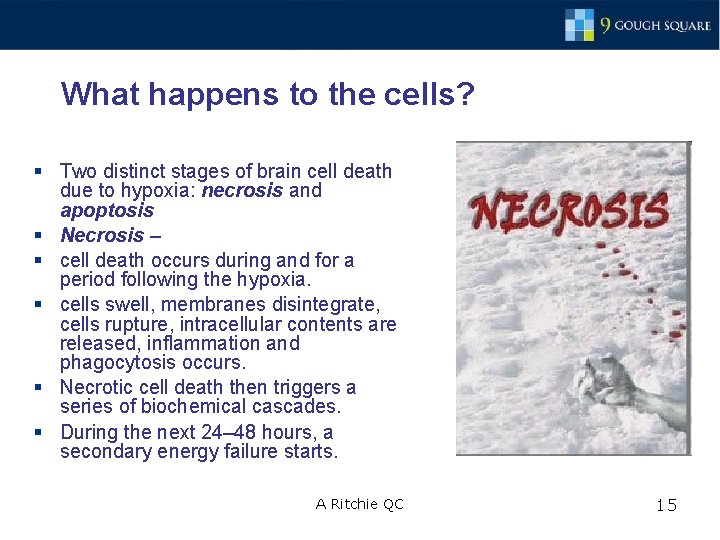
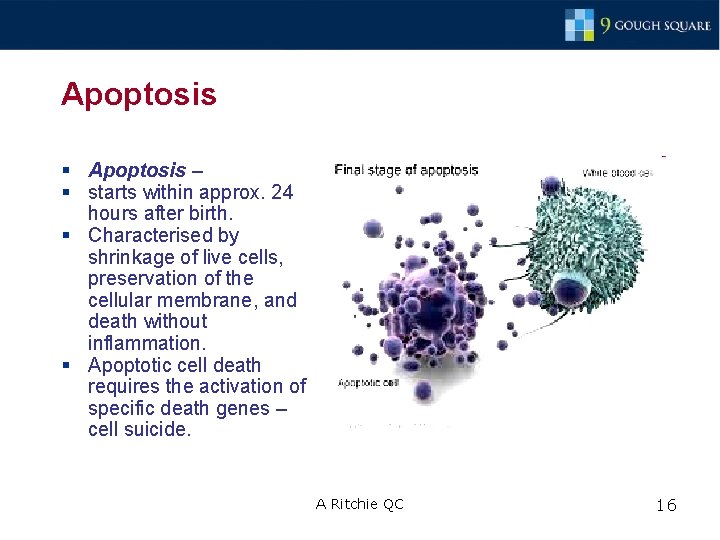
What happens to the cells? § Two distinct stages of brain cell death due to hypoxia: necrosis and apoptosis § Necrosis – § cell death occurs during and for a period following the hypoxia. § cells swell, membranes disintegrate, cells rupture, intracellular contents are released, inflammation and phagocytosis occurs. § Necrotic cell death then triggers a series of biochemical cascades. § During the next 24– 48 hours, a secondary energy failure starts. A Ritchie QC 15
Apoptosis § Apoptosis – § starts within approx. 24 hours after birth. § Characterised by shrinkage of live cells, preservation of the cellular membrane, and death without inflammation. § Apoptotic cell death requires the activation of specific death genes – cell suicide. A Ritchie QC 16
What sort of injuries does hypoxia result in? § § § Hypoxia can cause: § Hypoxic-ischemic encephalopathy (HIE): Hypoxic – a diminished amount of oxygen Ischemia – a diminished amount of blood perfusing the brain Encephalopathy – any dysfunction of the brain § brain damage plus neurological and neuropsychiatric disorders such as restricted mobility, epilepsy, ADHD, eating disorders In severe HIE, the mortality rate is reportedly 25– 50%. Most deaths occur in the first week of life due to multiple organ failure. A Ritchie QC 17
Cerebral Palsy What is cerebral palsy (CP)? § Definition: An abnormality of motor function (the ability to move and control movements) that is acquired at an early age, is due to a brain injury that is non-progressive. § CP caused by perinatal asphyxia: § HIE is one part of the Cerebral Palsy group of injuries § HIE is characterised by § [1] clinical symptoms and § [2] patterns of brain injury shown on MRI scans. A Ritchie QC 18
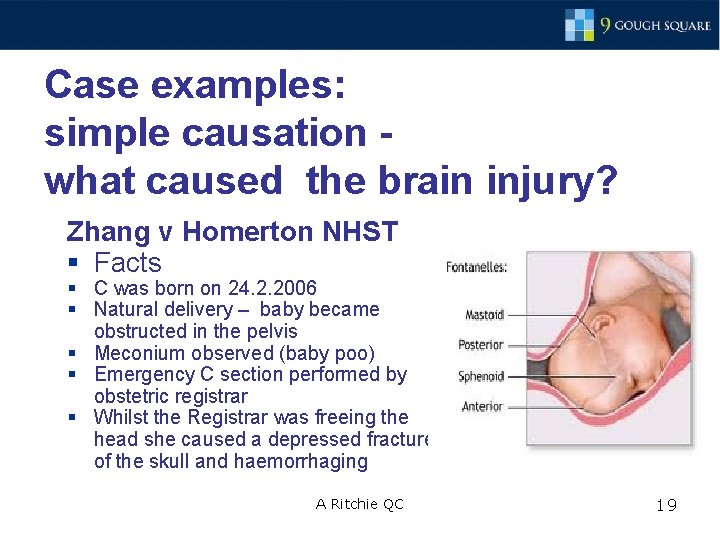
Case examples: simple causation - what caused the brain injury? Zhang v Homerton NHST § Facts § C was born on 24. 2. 2006 § Natural delivery – baby became obstructed in the pelvis § Meconium observed (baby poo) § Emergency C section performed by obstetric registrar § Whilst the Registrar was freeing the head she caused a depressed fracture of the skull and haemorrhaging A Ritchie QC 19
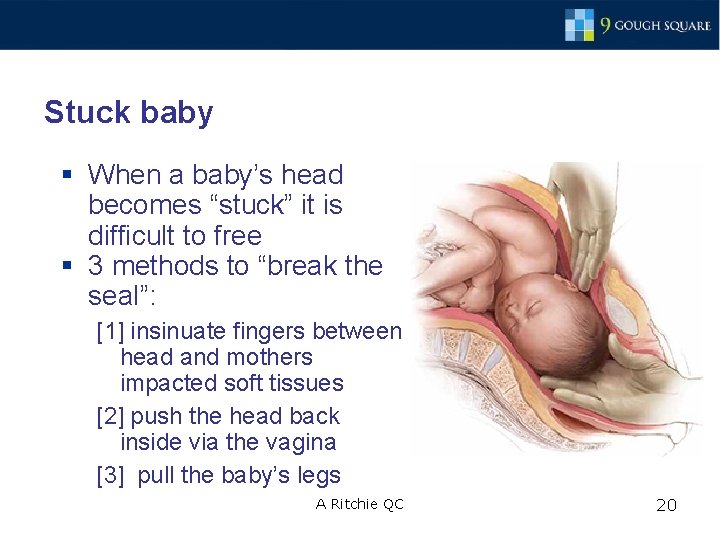
Stuck baby § When a baby’s head becomes “stuck” it is difficult to free § 3 methods to “break the seal”: [1] insinuate fingers between head and mothers impacted soft tissues [2] push the head back inside via the vagina [3] pull the baby’s legs A Ritchie QC 20
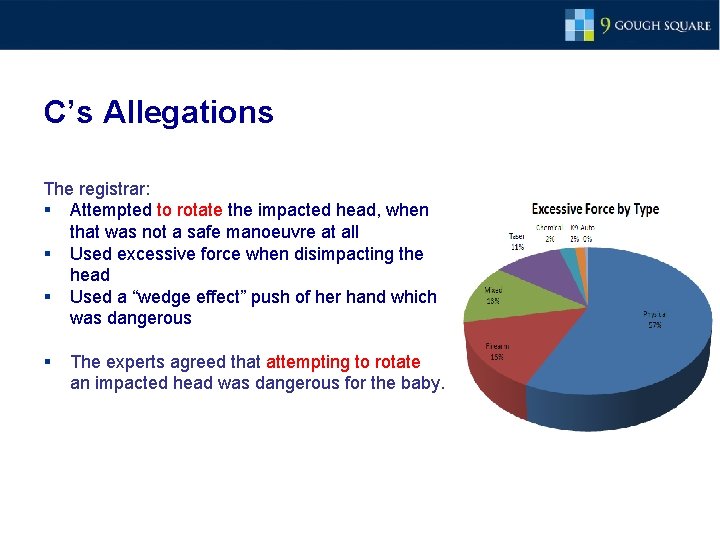
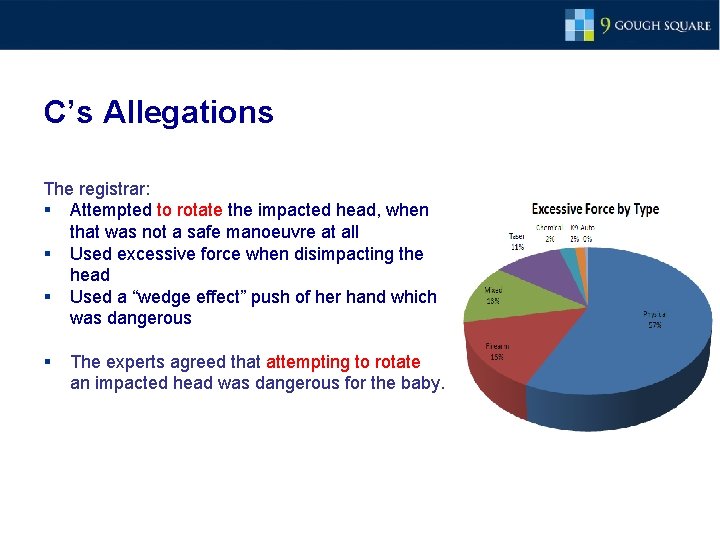
C’s Allegations The registrar: § Attempted to rotate the impacted head, when that was not a safe manoeuvre at all § Used excessive force when disimpacting the head § Used a “wedge effect” push of her hand which was dangerous § The experts agreed that attempting to rotate an impacted head was dangerous for the baby.
the Doctor’s evidence: Judge’s summary of the registrar’s evidence: “The baby’s head was firmly stuck in [mother’s] pelvis…. [T]here was essentially no space at all. ” 22. Keeping her hand where it was, she discussed the problem with Midwife Harling, and it was agreed (i) that the midwife would move to between mother’s legs, and push the baby’s head upwards from the vagina, and (ii) the on-call consultant should be crash-called “in case we were unable to deliver the baby” Theatre staff called the consultant. 23. Meanwhile, Dr G tried to insinuate her hand further, with Midwife Harling pushing from below. Their fingers touched, but the seal was not broken and Dr G was still unable to insert her hand sufficiently to flex the baby’s head. 24. Dr G then said this: “I then managed to move the baby’s head slightly to the mother’s right and I tried to flex the baby’s head again. At this point, I felt the head dislodge from the pelvis (the breaking of the vacuum) and I was able to deliver the baby…. It was the slight movement of the baby’s head to the mother’s right which enabled me to then flex the head and the head then automatically rotated without any pressure/force applied from me and the rest of the delivery followed. I would not describe using excessive force at this time. I only used the necessary force to dislodge the head. In fact, it was the change in position of my hand the breaking of suction that effected delivery…. ”. A Ritchie QC 22

The Medical notes Evidence • In the defence the registrar denied rotating the head • The operation notes of the registrar contained the line: “rotated in 3 rd attempt” • Registrar’s investigation statement stated: “I … managed to rotate and deliver…” • Midwife’s statement: “Dr G… said she had difficulty rotating the head”. . A Ritchie QC 23
Findings § The registrar did try to rotate the head and that was dangerous “Primarily on the basis of Prof Bennett’s evidence, I am satisfied that the attempted rotation of the head caused the subgaleal haemorrhaging suffered by the Claimant; and the movement of the head caused the right parietal fracture and consequent intracranial haemorrhaging. ” A Ritchie QC 24
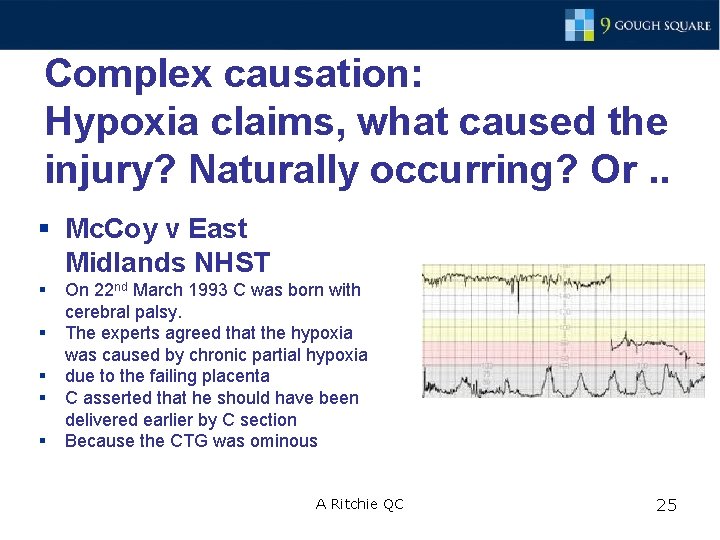
Complex causation: Hypoxia claims, what caused the injury? Naturally occurring? Or. . § Mc. Coy v East Midlands NHST § § § On 22 nd March 1993 C was born with cerebral palsy. The experts agreed that the hypoxia was caused by chronic partial hypoxia due to the failing placenta C asserted that he should have been delivered earlier by C section Because the CTG was ominous A Ritchie QC 25

Facts § C’s mother detected reduced fetal movement and went to hospital on 17 th March 1993 § 5 days before the actual birth § CTG trace was taken for an hour § Staff Grade obstetrician interpreted the trace as “satisfactory” § mother discharged home A Ritchie QC 26

Experts agreed: § Having looks at the MRI scans and taking into account it was chronic partial hypoxia § C was undamaged on 17 th and 18 th March § The brain damage occurred between 19 th and 21 st March, when M returned to hospitals for the birth § Issues: [1] was the CTG normal? [2] if C had been kept in what would the CTG have looked like? [3] would M have been kept in?
Allegations § C alleged that the trace was “suspicious” not satisfactory § C should not have been discharged § Keeping her in would have led to earlier C section and avoidance of hypoxia A Ritchie QC 28
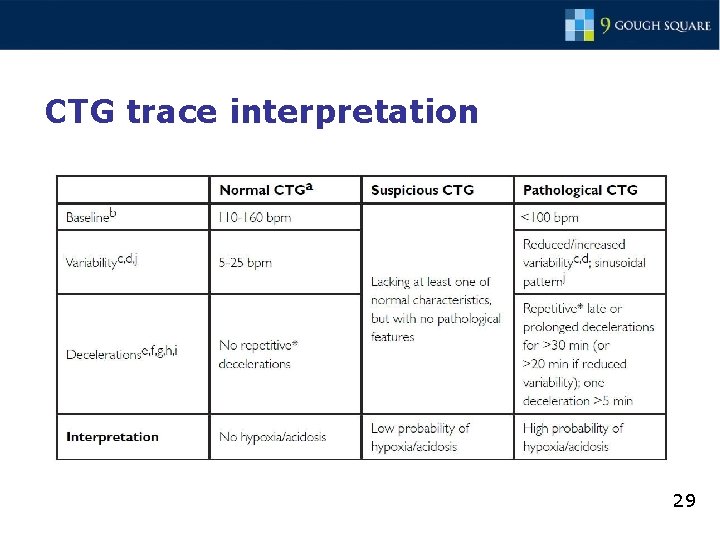
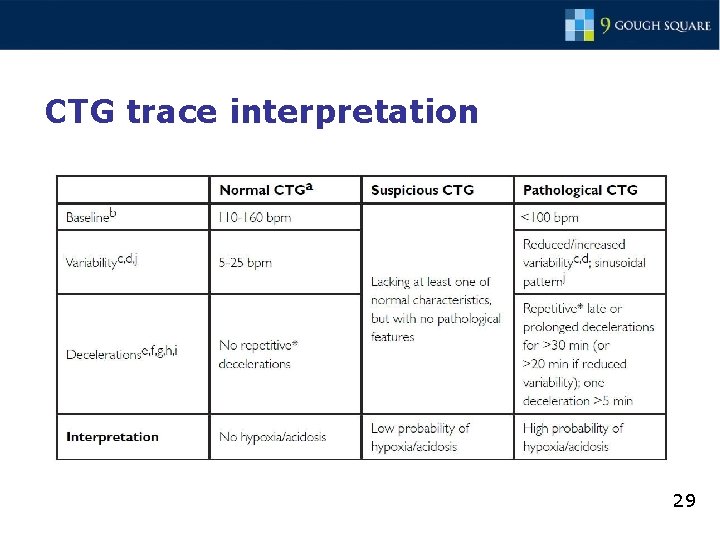
CTG trace interpretation 29
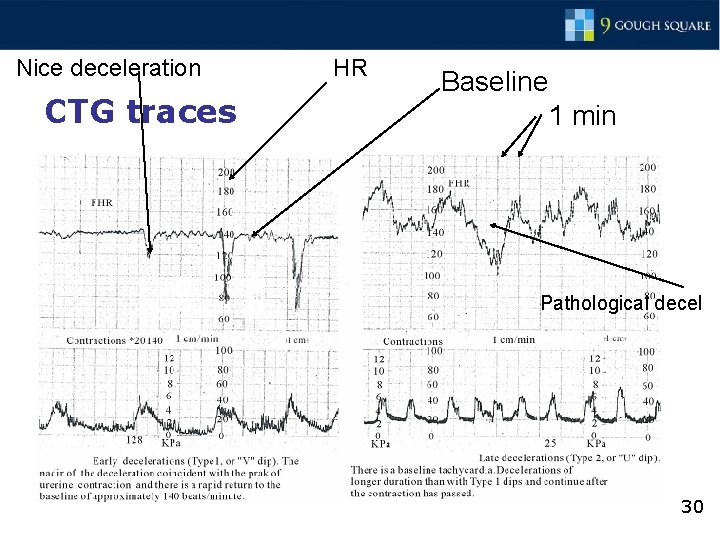
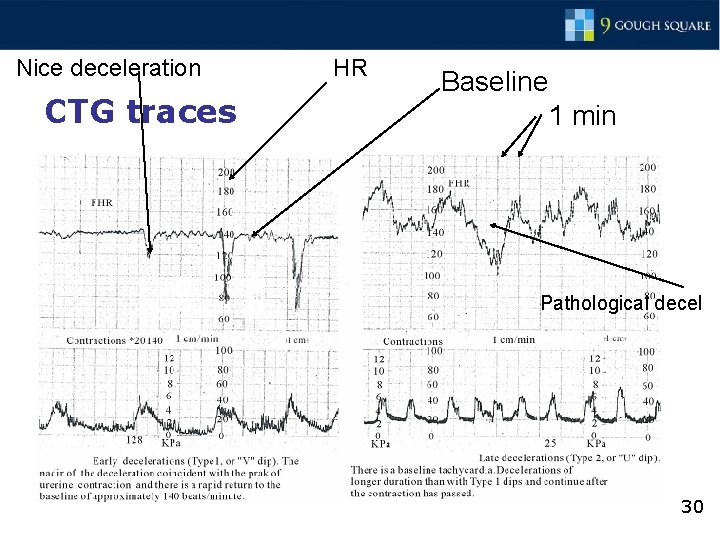
Nice deceleration CTG traces HR Baseline 1 min Pathological decel 30
Slade J – background findings “The placenta has two main functions: a) To provide nutrition to the foetus, b) To provide for an exchange of gases – oxygen in and carbon dioxide out. iv) When a placenta is failing, nutrition is provided to the brain in favour of the body. A disproportion in the centiles of head circumference and body weight is an indication of a failing placenta; v) When a placenta is failing, oxygen continues to be supplied in favour of nutrition; vi) Hypoxia can be sustained by a foetus without causing damage. Contractions in the course of birth can inflict pressure on the placenta causing hypoxia without damage resulting; vii) C was undamaged on 17 th March 1993. It is likely that damage was caused to her brain after 17 th March and before her mother’s admission to hospital on 21 st March 1993. viii) The degree of C’s disability indicated that …she was highly unlikely to have sustained damage by 18 th March 1993. ” A Ritchie QC 31
Finding of Negligence – the CTG on 17 March “ 49. When the trace terminated there had been two decelerations of the fetal heart rate without any intervening accelerations. It was not clear from the trace whether the fetal heart rate had returned to the baseline before the CTG was stopped. I have found that Dr L. did not know whether the heart rate had returned to normal. 50. In my judgment Dr L. acted negligently in describing the trace as ‘satisfactory’ and in failing to re-start the CTG or at least to admit Ms Jones after a few hours to carry out a further CTG scan when, as Mr Porter stated in evidence, it should have been continued…” A Ritchie QC 32
Causation of the brain injury § The hospital asserted that but for the negligence: § if she had been kept in § the further CTG trace on 18 th would have shown nothing suspicious § so she would have been released next day anyway. § The but for Causation issue A Ritchie QC 33

Judgment on that issue “ 80. I accept the evidence of Mr Porter …he considered that injury occurred between 24 and 48 hours before birth (21 -23 March). This evidence accords with that of the Claimant’s impressive expert, Professor Weindling, who agreed that the duration of the hypoxia could be limited safely to 48 hours before delivery. 81. Accordingly I find on a balance of probabilities that the Claimant has not established that a second or resumed CTG on 17 th March 1993 would have been suspicious or pathological so as to lead her obstetrician to decide that Ms Jones’ baby should be delivered on 18 th March 1993 or at any time before 21 st March 1993. 82. The Claimant has not established that the negligence of Dr L in failing to carry out a further trace on 17 th March 1993 was the cause of the damage suffered by Brodie. 83. The claim is dismissed. ” A Ritchie QC What happened was the brain compensated through 17/18/19/20 March and then fell off a cliff on 21/22/23 34
Times up, …. more slides in the pack Thank you Andrew Ritchie QC 9 Gough Square A Ritchie QC 35
Hypoxia claims: Timing determines breach and causation § Goncalves v Newham Hospital § Facts: § C was born on 19. 1. 1996 with his twin § C suffered tetraplegic dyskinetic cerebral; palsy § Due to hypoxia at birth § ? Due to delayed C section § D called no witnesses of fact at trial and had lost some of the notes. Simply put the C to proof. A Ritchie QC 36

timings § The twin brother was born at 19. 10 hours § Mother’s contractions stopped and restart was delayed beyond normal § C was in the breech position § C was born 37 minutes later (@19. 47) by caesarian § C was born “flat” with no respiration and APGAR 3/5, HR below 100 bmp A Ritchie QC 37
Allegations Defence § The C section was delayed by 10 -15 minutes § The obstetric registrar was not in the delivery room § Registrar not called until bradycardia arose (despite breech) § Registrar took 10 -15 minutes to arrive to do the C section § The C section should have been done 10 -15 minutes earlier § Causation: that would have avoided the brain damage • The hypoxia probably started 20 minutes before the birth (@19. 27) • The signs of hypoxia: bardycardia commenced around 19. 28. • The C section was done within 20 minutes which is commendable speed and not negligent A Ritchie QC 38
Expert Evidence § The experts agreed: § An obstetrician should be present for birth of twins. § Twins: more likely to present problems § The operating theatre should be prepared and ready to do a C section with twins § Fetal heart should be monitored constantly § C suffered 25 minutes of hypoxia § The damage occurred in the last 10 -15 minutes § C’s compensating mechanisms coped for the first 10 minutes. A Ritchie QC 39

Differing expert views Claimant – Mr Lewis Defendant - Mr Woolfson • Breech probably noticed by midwives § It took only 17 minutes from decision to C section in this case • If the obstetrician had been present he/she would have done C section earlier due to breech and delayed restart of contractions and bardycardia when it started § 30 minutes is the normal time for that to occur. § The damage would have occurred anyway • For a predicted C section taking 30 minutes is too long A Ritchie QC 40
Judgment - causation § The obstetric registrar should have been present from the start § D was negligent in failing to have him there § Any reasonable registrar would have started the C section earlier and delivery would have been 10 -15 minutes earlier § Brain damage would have been avoided. § The hospital’s negligence caused the tragedy A Ritchie QC 41
Some medicine: MRI Scans do they help? When the baby suffers prolonged partial hypoxia: § the first areas to suffer are those with the poorest blood supply and/or the most need for oxygen (those with the highest metabolic rate) – the weakest. § If hypoxia continues after that the damage spreads to the strongest cells and the better supplied areas … A Ritchie QC 42
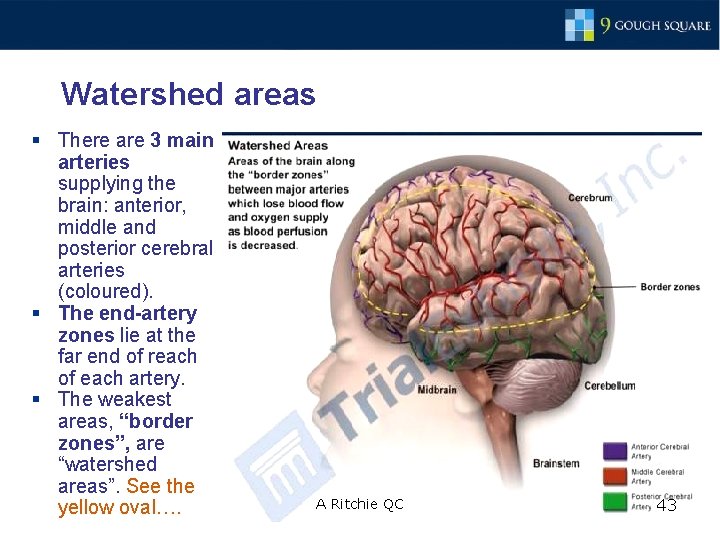
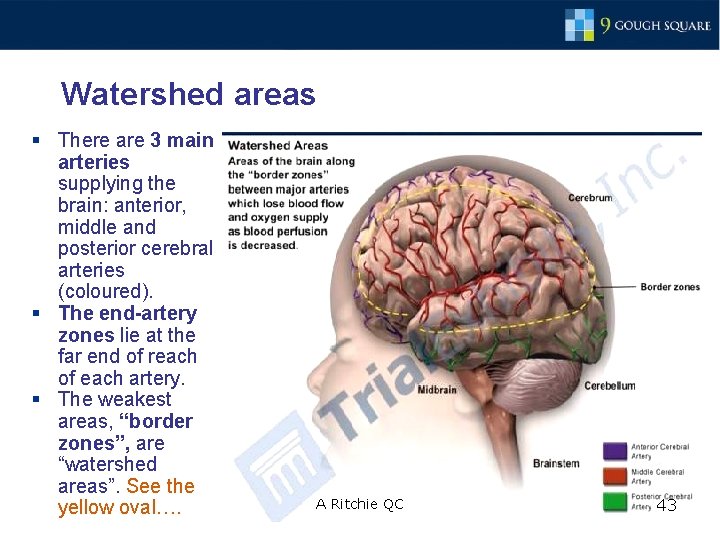
Watershed areas § There are 3 main arteries supplying the brain: anterior, middle and posterior cerebral arteries (coloured). § The end-artery zones lie at the far end of reach of each artery. § The weakest areas, “border zones”, are “watershed areas”. See the yellow oval…. A Ritchie QC 43

Key arguments on causation in Hypoxia cases • If the watershed areas are damaged • That means that there has been hypoxia • but it was not severe enough to damage the well watered areas
Causation – would it have happened anyway? • How long have the midwives or obstetricians got? • This depends on Monkey Studies from long ago …. A Ritchie QC 45
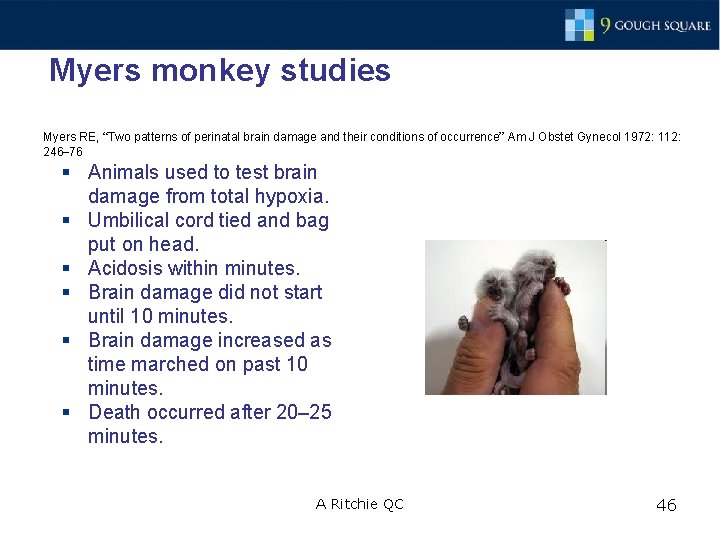
Myers monkey studies Myers RE, “Two patterns of perinatal brain damage and their conditions of occurrence” Am J Obstet Gynecol 1972: 112: 246– 76 § Animals used to test brain damage from total hypoxia. § Umbilical cord tied and bag put on head. § Acidosis within minutes. § Brain damage did not start until 10 minutes. § Brain damage increased as time marched on past 10 minutes. § Death occurred after 20– 25 minutes. A Ritchie QC 46

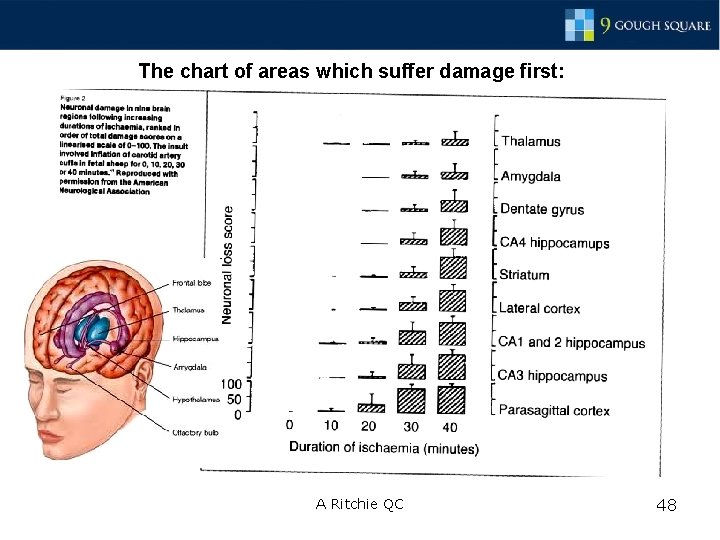
Which areas are damaged first? § Myers reported a “monotonously repetitive” rank order: § 10 -13 minutes: Colliculi; posterior and lateral ventral thalamic nuclei. § 16 -18 minutes: more of the thalamus. A Ritchie QC 47
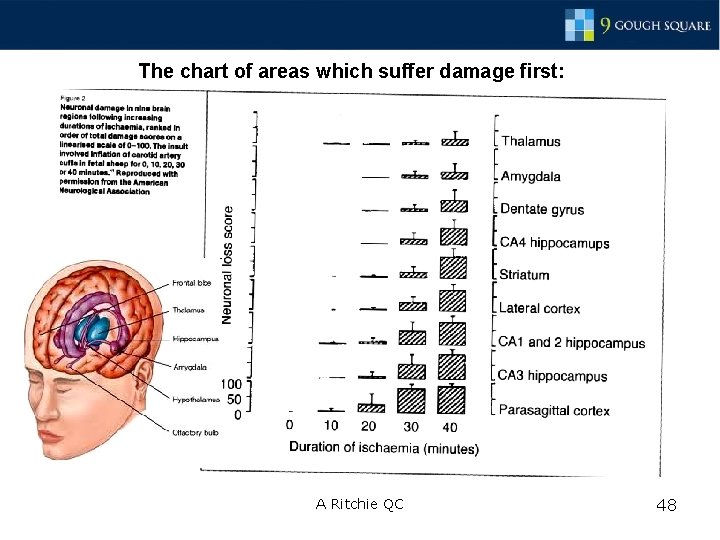
The chart of areas which suffer damage first: A Ritchie QC 48
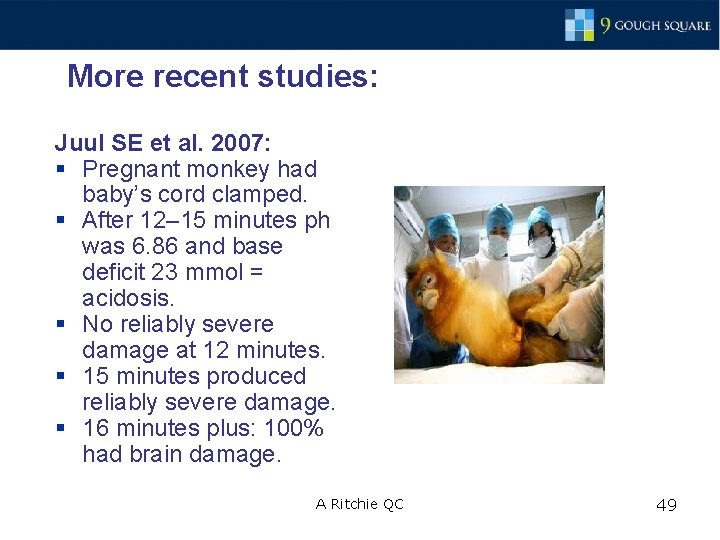
More recent studies: Juul SE et al. 2007: § Pregnant monkey had baby’s cord clamped. § After 12– 15 minutes ph was 6. 86 and base deficit 23 mmol = acidosis. § No reliably severe damage at 12 minutes. § 15 minutes produced reliably severe damage. § 16 minutes plus: 100% had brain damage. A Ritchie QC 49
Conclusions Hypoxia/brain injury cases: • Are the most difficult clinical negligence cases • Often occurred up to 21 years ago • Memories have usually faded • Heavily reliant on expert evidence to prove breach and causation • Involve detailed analysis of the timing of events within only 1 -2 hour period • Causation is the most difficult issue • Would the injury have occurred anyway? A Ritchie QC 50

Thank you Andrew Ritchie QC 9 Gough Square A Ritchie QC 51
 Wheel model of disease causation
Wheel model of disease causation Proximate and ultimate behavior examples
Proximate and ultimate behavior examples Proximate causation vs ultimate causation
Proximate causation vs ultimate causation Brain watershed areas
Brain watershed areas Tort of negligence
Tort of negligence Contributory negligence ppt
Contributory negligence ppt Conclusion for negligence
Conclusion for negligence Defences to negligence
Defences to negligence Negligence per se vs res ipsa loquitur
Negligence per se vs res ipsa loquitur Gross negligence manslaughter actus reus
Gross negligence manslaughter actus reus Setting quotes jekyll and hyde
Setting quotes jekyll and hyde Elements of negligence
Elements of negligence Negligence past tense
Negligence past tense Ritchie feed and seed
Ritchie feed and seed Jean ritchie one i love
Jean ritchie one i love Executive dysfunction
Executive dysfunction Madonna age
Madonna age Rock latino origin
Rock latino origin Kernighan ritchie
Kernighan ritchie Anna ritchie allan
Anna ritchie allan Concepcion valenzuela joseph steven valenzuela
Concepcion valenzuela joseph steven valenzuela Tolman ritchie and kalish (1946)
Tolman ritchie and kalish (1946) Ritchie feed and seed
Ritchie feed and seed Chacn
Chacn How do you write an leq
How do you write an leq Jaring-jaring sebab akibat penyakit tbc
Jaring-jaring sebab akibat penyakit tbc Pyramide des accidents
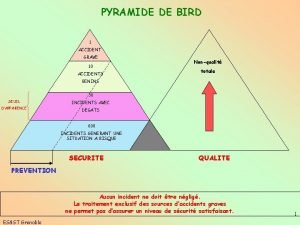
Pyramide des accidents Psychological theory of criminal behavior
Psychological theory of criminal behavior What is causal research design
What is causal research design The army accident causation model
The army accident causation model Causation with a human face
Causation with a human face Petersen's accident/incident theory
Petersen's accident/incident theory Pixabay
Pixabay Leq
Leq Free will theory
Free will theory Heinrich triangle theory
Heinrich triangle theory Proximate behaviour in animals
Proximate behaviour in animals Causatio
Causatio Footloose definition ap human geography
Footloose definition ap human geography Association and causation
Association and causation World history
World history Model of disease causation
Model of disease causation Causation in criminal law
Causation in criminal law Association and causation
Association and causation The army accident causation model
The army accident causation model Reverse causation examples
Reverse causation examples Contoh web of causation
Contoh web of causation Analysis and reasoning leq
Analysis and reasoning leq Recall bias example
Recall bias example Statistics correlation vs causation
Statistics correlation vs causation What is disease theory
What is disease theory Correlation mistaken for causation
Correlation mistaken for causation