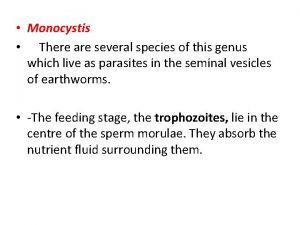
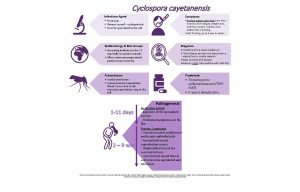
Causal Agent Several protozoan species in the genus
































- Slides: 79


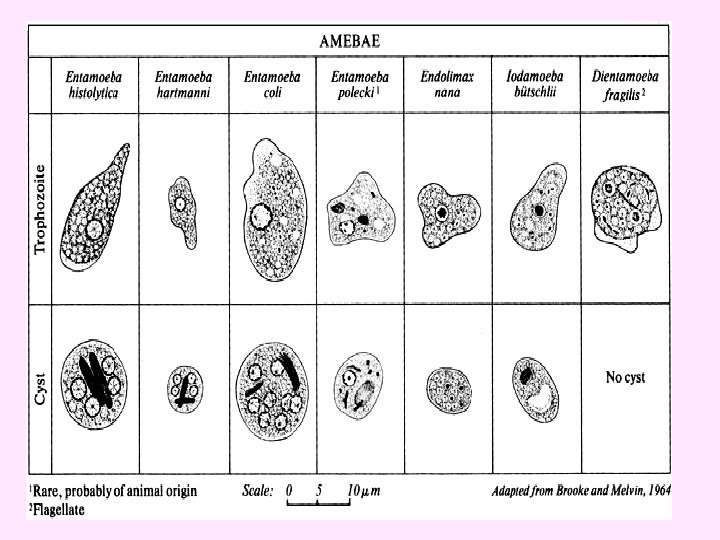
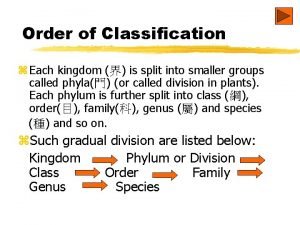
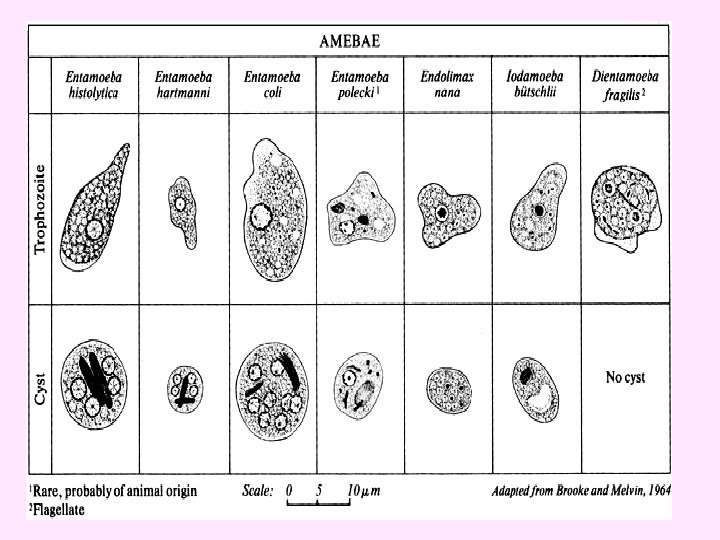
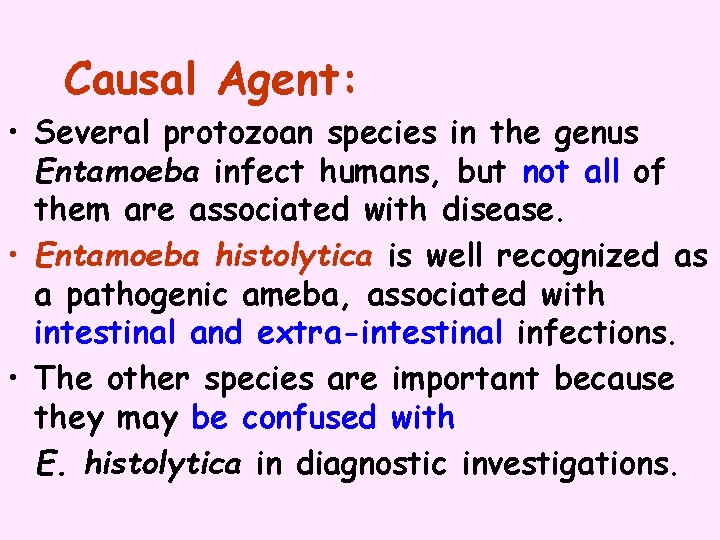
Causal Agent: • Several protozoan species in the genus Entamoeba infect humans, but not all of them are associated with disease. • Entamoeba histolytica is well recognized as a pathogenic ameba, associated with intestinal and extra-intestinal infections. • The other species are important because they may be confused with E. histolytica in diagnostic investigations.
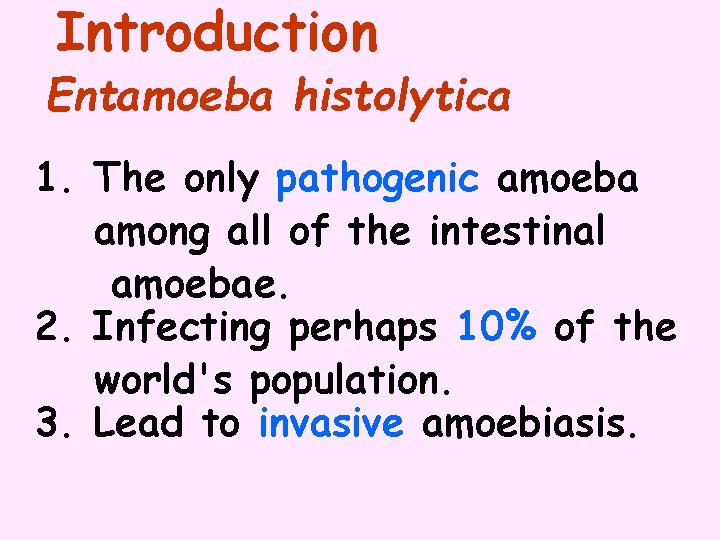
Introduction Entamoeba histolytica 1. The only pathogenic amoeba among all of the intestinal amoebae. 2. Infecting perhaps 10% of the world's population. 3. Lead to invasive amoebiasis.

Entamoeba histolytica • Worldwide, with higher incidence of amoebiasis in developing countries. • risk groups include male homosexuals, travelers and recent immigrants, and institutional populations.
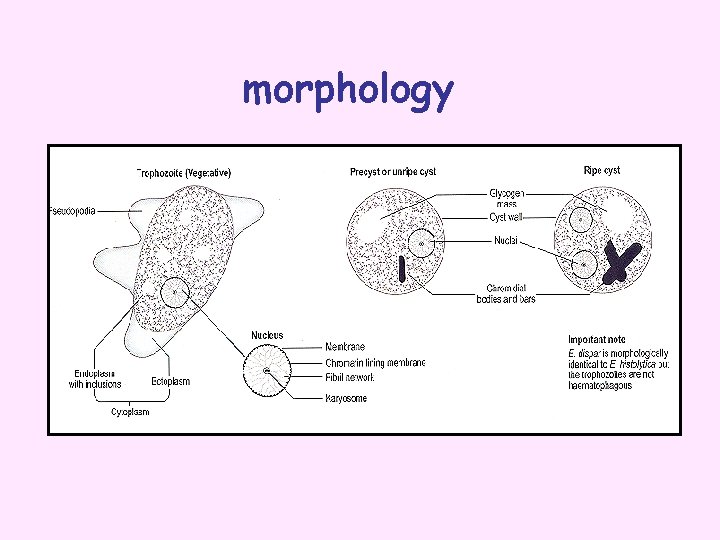
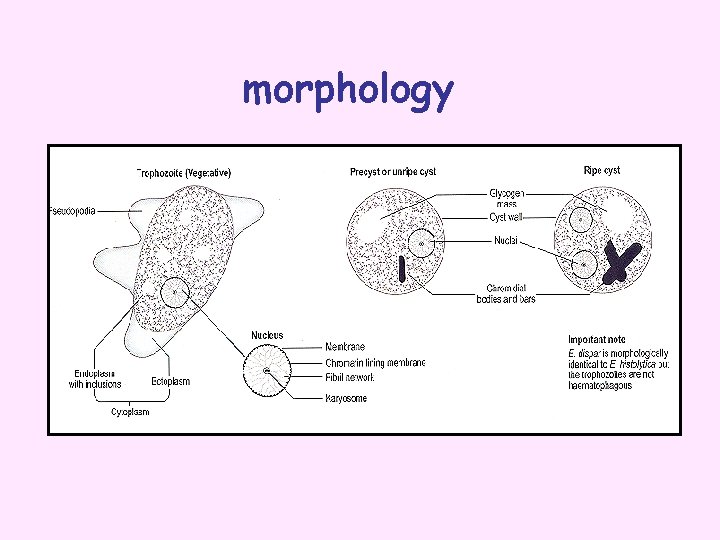
morphology

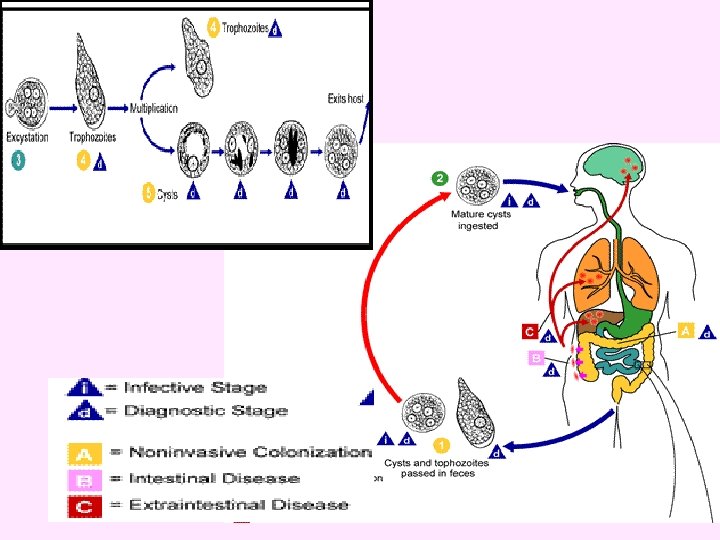

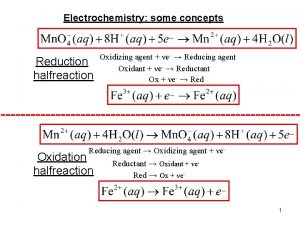
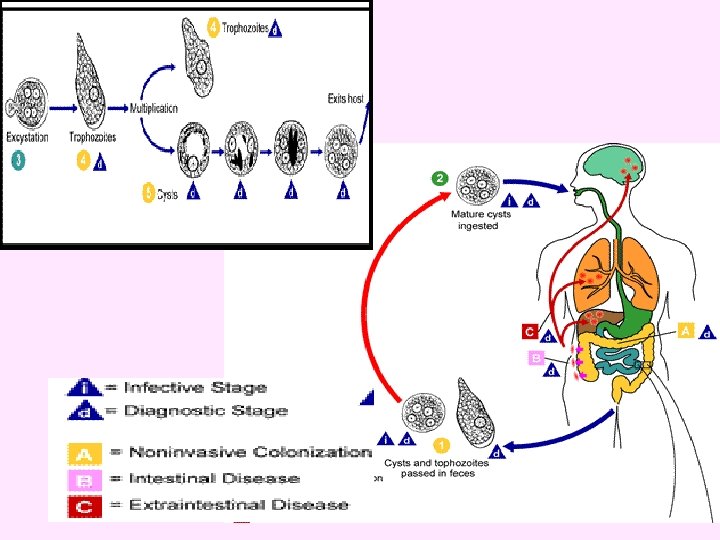
• • Life cycle Infection by Entamoeba histolytica occurs by ingestion of mature cysts in fecally contaminated food, water, or hands. Excystation occurs in the small intestine and trophozoites are released, which migrate to the large intestine. The trophozoites multiply by binary fission and produce cysts. Cysts and trophozoites are passed in feces Cysts are found in formed stool, whereas trophozoites are found in diarrheal stool.


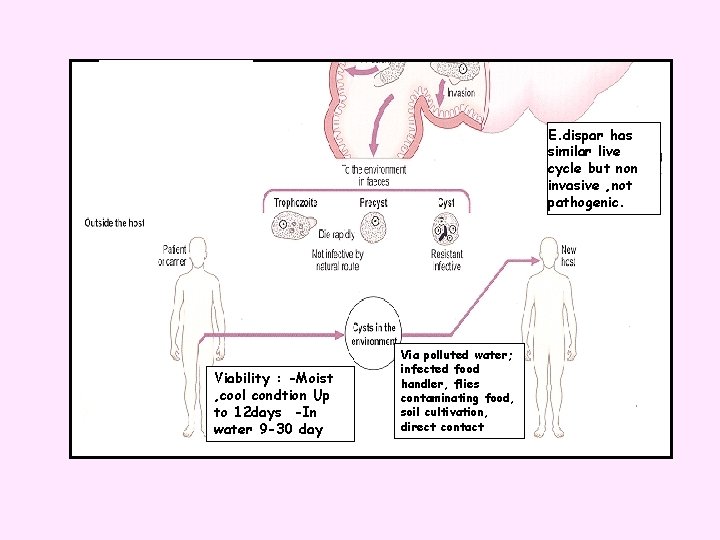
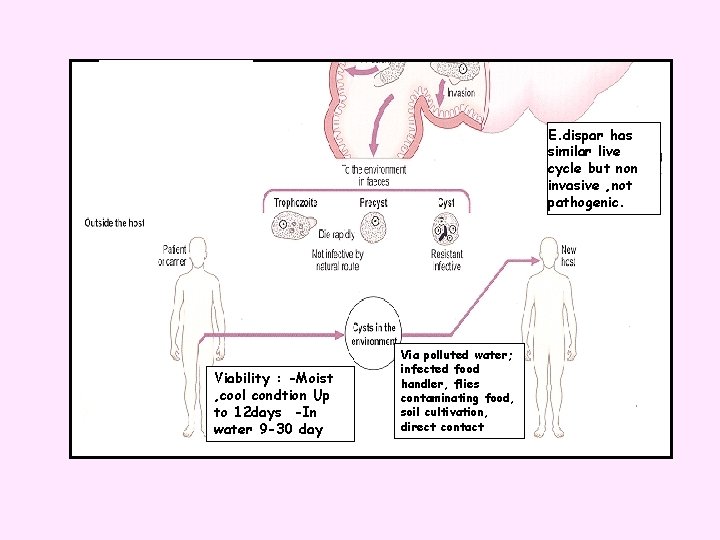
E. dispar has similar live cycle but non invasive , not pathogenic. Viability : -Moist , cool condtion Up to 12 days -In water 9 -30 day Via polluted water; infected food handler, flies contaminating food, soil cultivation, direct contact
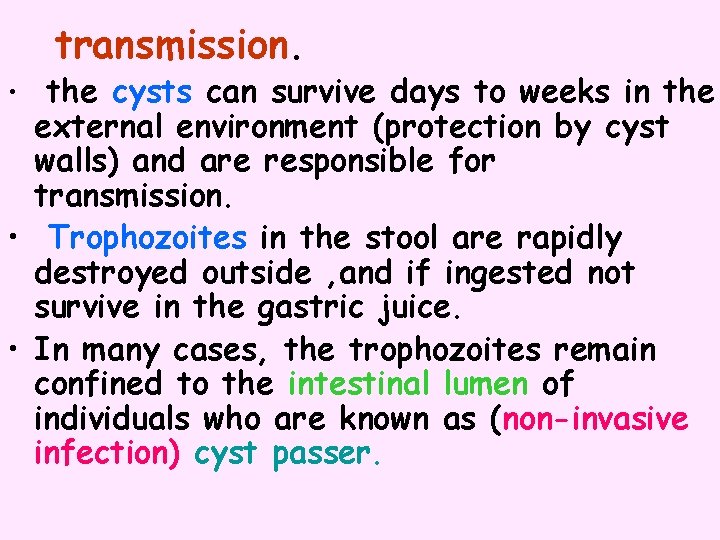
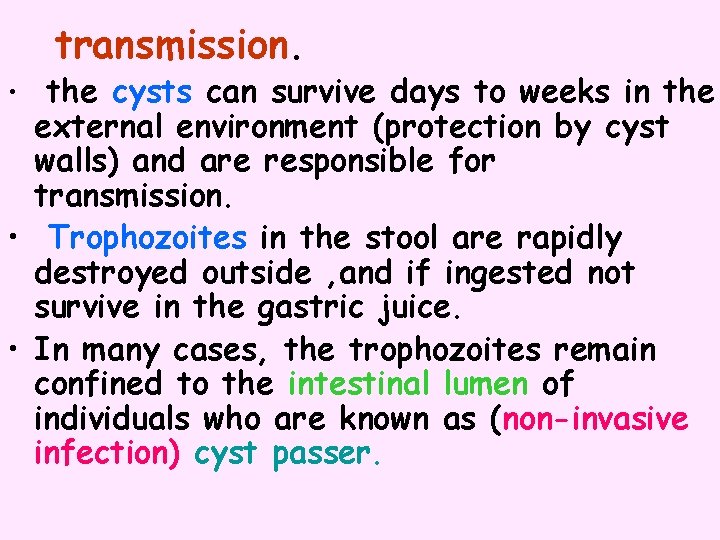
transmission. • the cysts can survive days to weeks in the external environment (protection by cyst walls) and are responsible for transmission. • Trophozoites in the stool are rapidly destroyed outside , and if ingested not survive in the gastric juice. • In many cases, the trophozoites remain confined to the intestinal lumen of individuals who are known as (non-invasive infection) cyst passer.

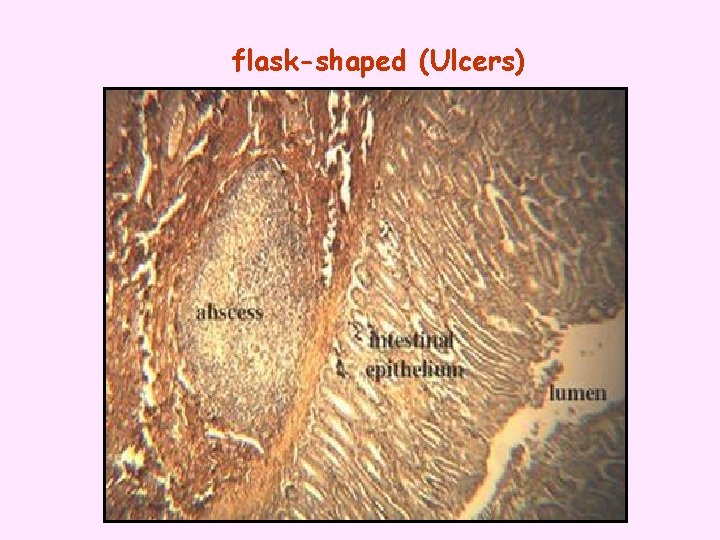
1 2 3 4 1 - the primary ulcer invasion of mucosa via crypts repair may occur. 2 - extension in mucosa muscularis mucosa relatively resistant. 3 -formation of sinus accumulation of amoebae superficial to muscularis mucosa with lateral extension of lytic necrosis; abscesses may coalesce under intact mucosa , mucosa may slough with widespread ulceration 4 -deep extension muscularis mucosa eventually pierced (direct or via blood) deep necrosis of sub-mucosa even muscle and sub-serosa
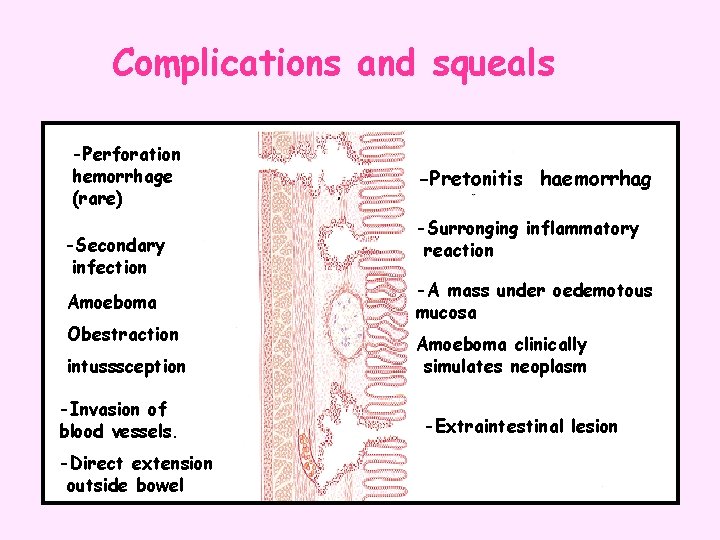
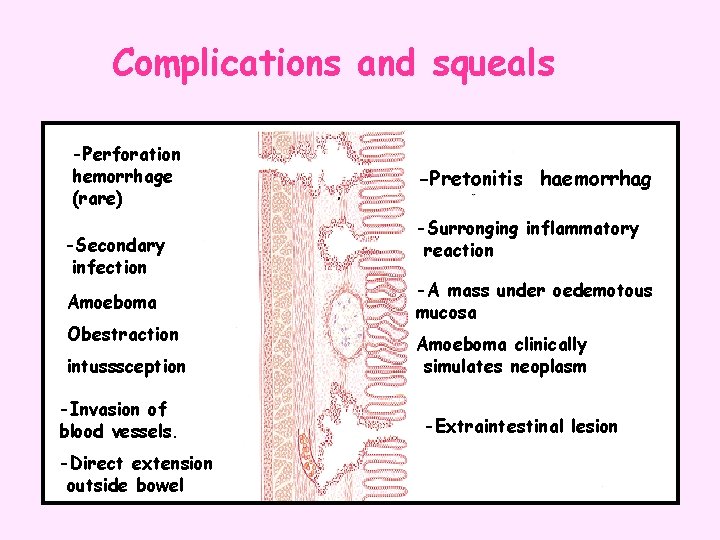
Complications and squeals -Perforation hemorrhage (rare) -Secondary infection Amoeboma Obestraction intusssception -Invasion of blood vessels. -Direct extension outside bowel -Pretonitis haemorrhag -Surronging inflammatory reaction -A mass under oedemotous mucosa Amoeboma clinically simulates neoplasm -Extraintestinal lesion
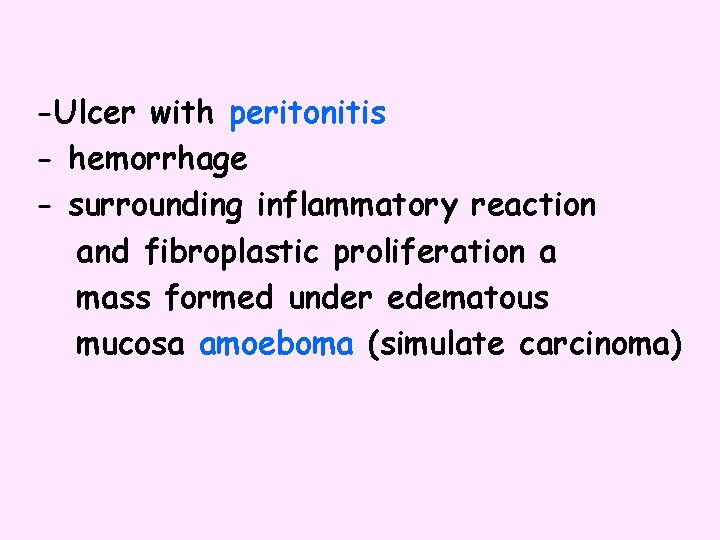
-Ulcer with peritonitis - hemorrhage - surrounding inflammatory reaction and fibroplastic proliferation a mass formed under edematous mucosa amoeboma (simulate carcinoma)
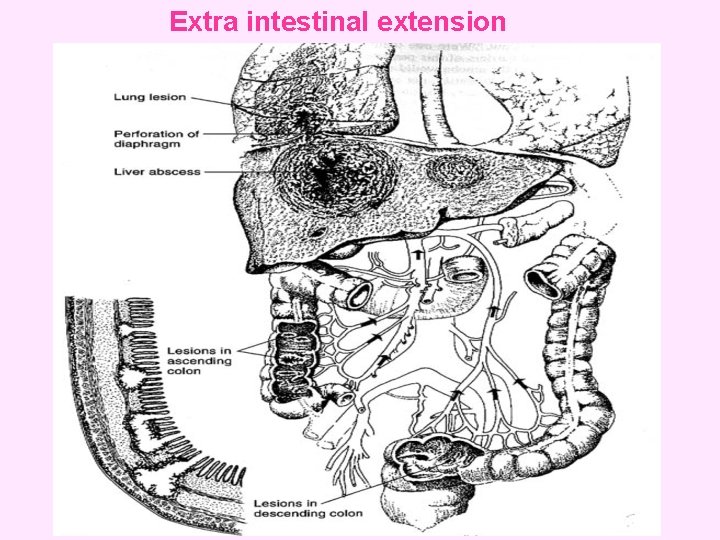
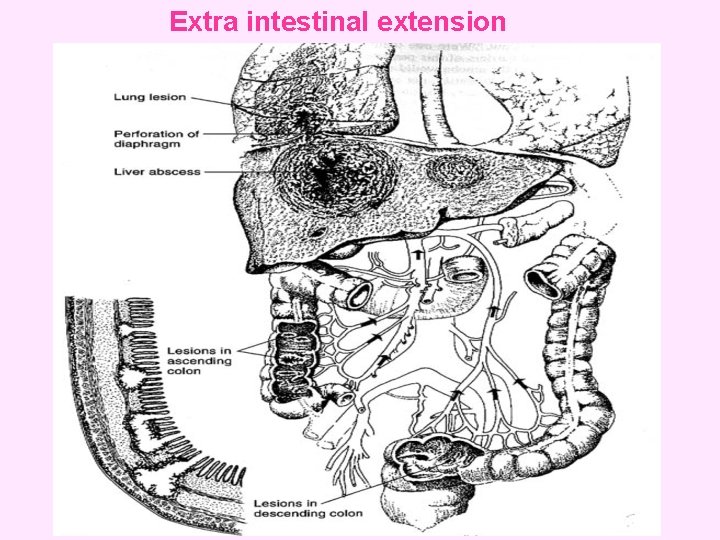
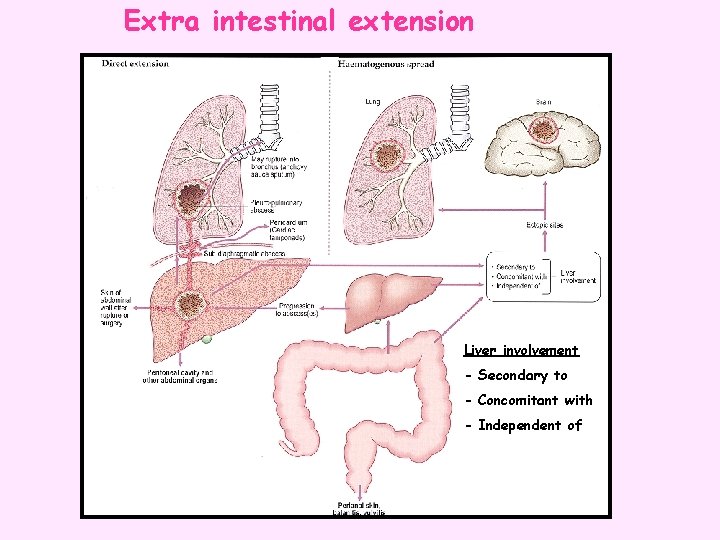
Extra intestinal extension
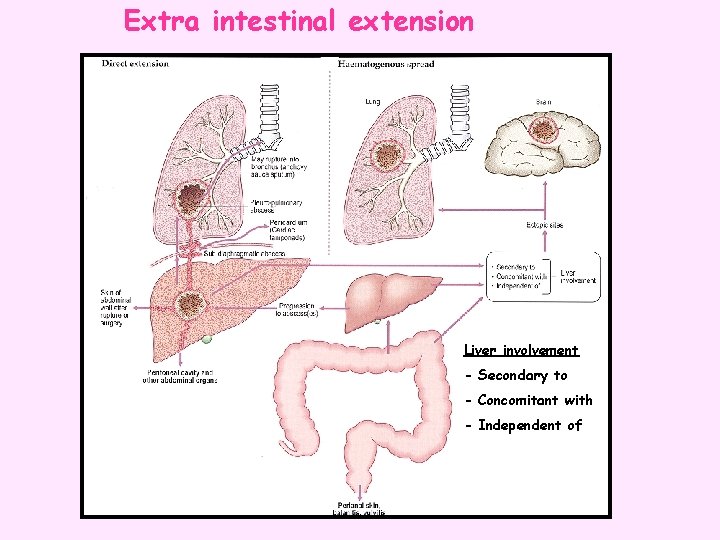
Extra intestinal extension Liver involvement - Secondary to - Concomitant with - Independent of
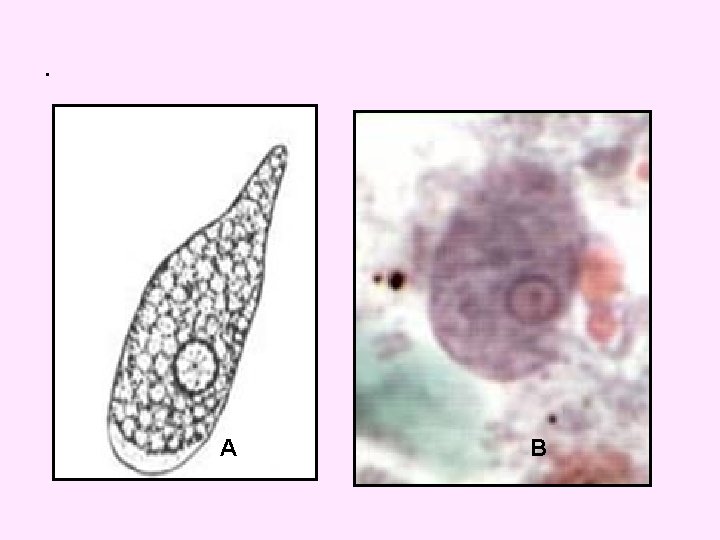
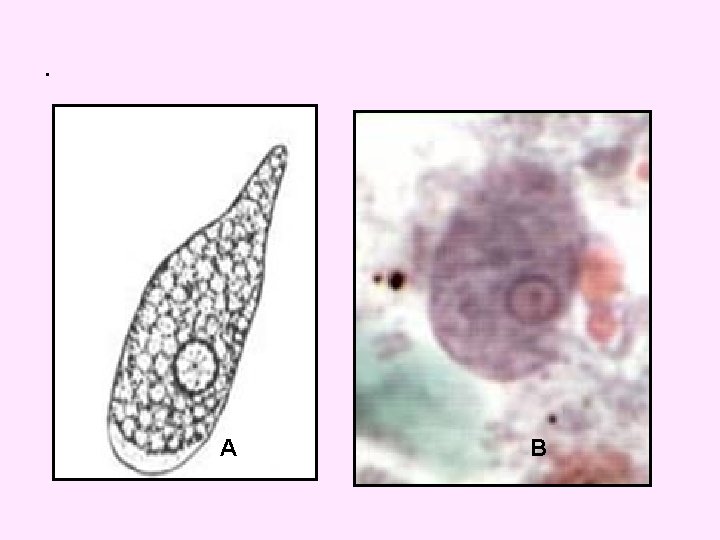
. A B
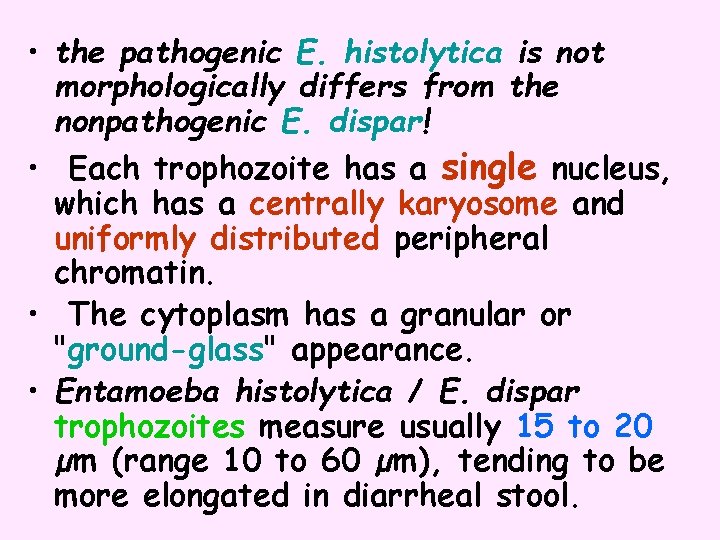
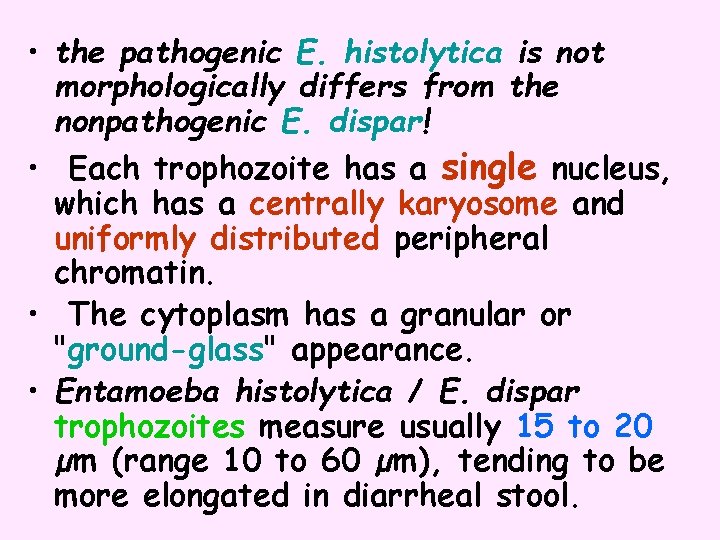
• the pathogenic E. histolytica is not morphologically differs from the nonpathogenic E. dispar! • Each trophozoite has a single nucleus, which has a centrally karyosome and uniformly distributed peripheral chromatin. • The cytoplasm has a granular or "ground-glass" appearance. • Entamoeba histolytica / E. dispar trophozoites measure usually 15 to 20 µm (range 10 to 60 µm), tending to be more elongated in diarrheal stool.
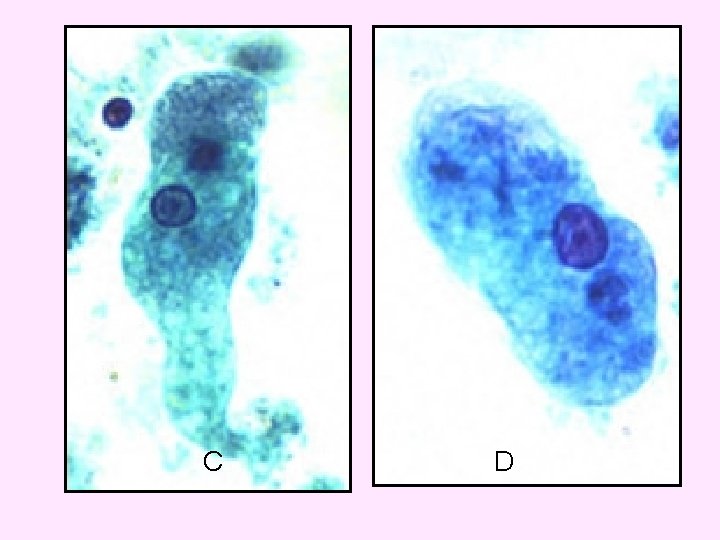
C D
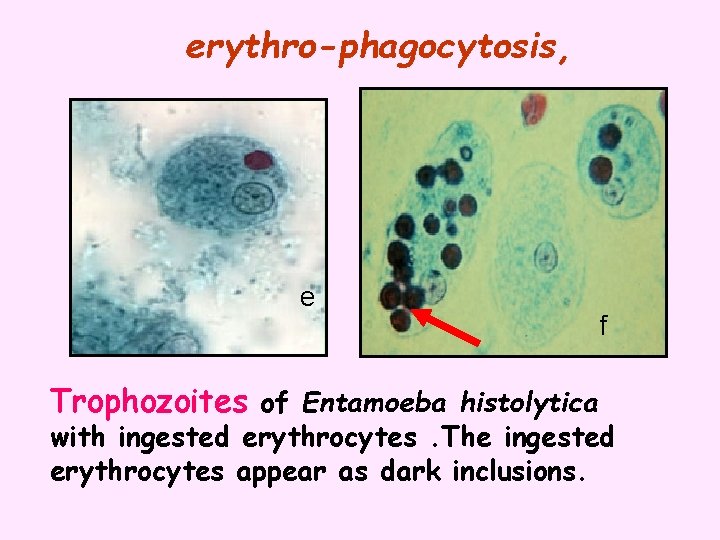
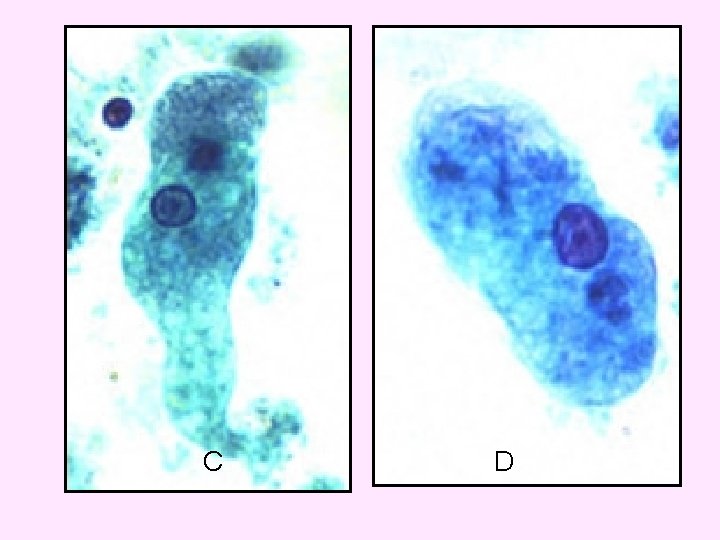
erythro-phagocytosis, e Trophozoites of Entamoeba histolytica f with ingested erythrocytes. The ingested erythrocytes appear as dark inclusions.

• Erythro-phagocytosis is the only morphologic characteristic that can be used to differentiate E. histolytica from the non-pathogenic E. dispar
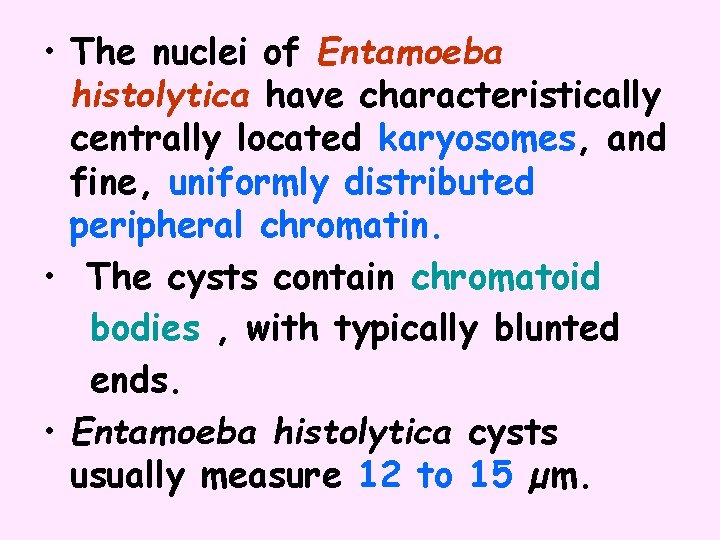
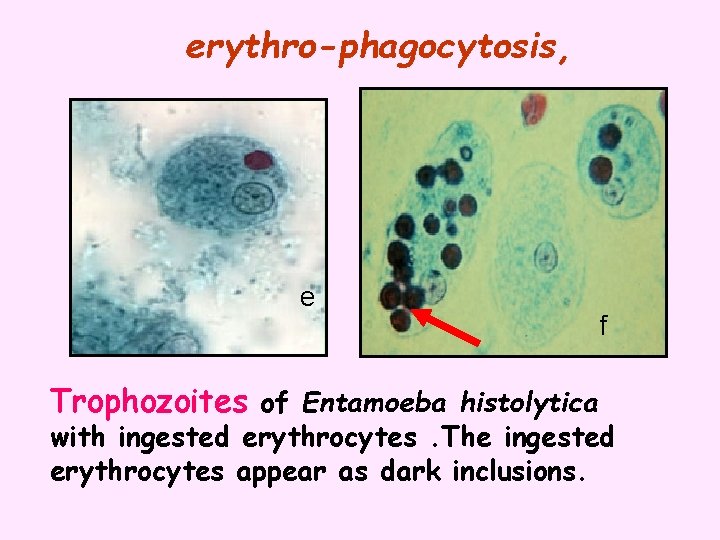
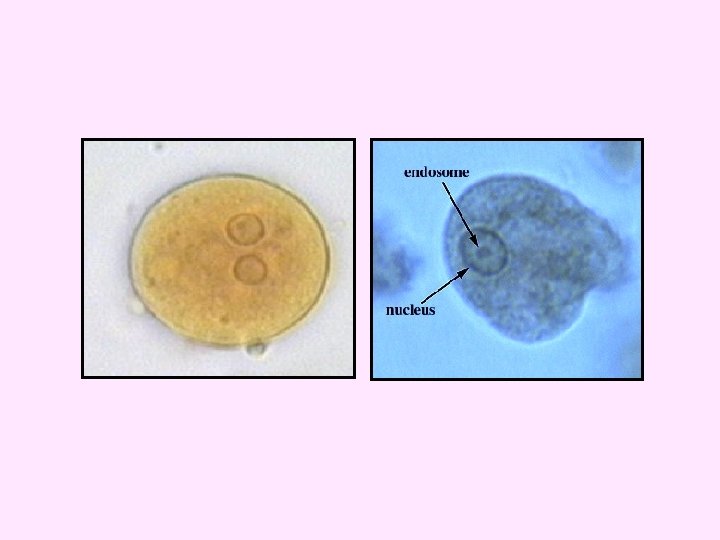
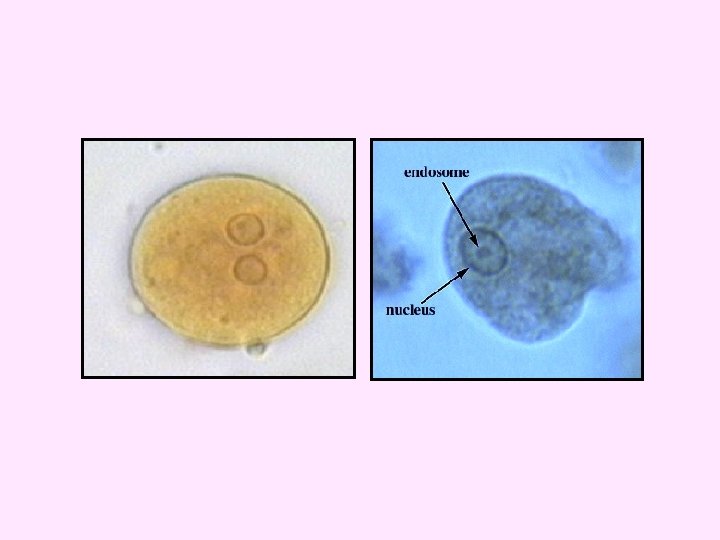
• The nuclei of Entamoeba histolytica have characteristically centrally located karyosomes, and fine, uniformly distributed peripheral chromatin. • The cysts contain chromatoid bodies , with typically blunted ends. • Entamoeba histolytica cysts usually measure 12 to 15 µm.

Mature. Entamoeba histolytica cysts usually measure 12 to 15 µm. cysts have 4 nuclei. h I
Entamoeba coli
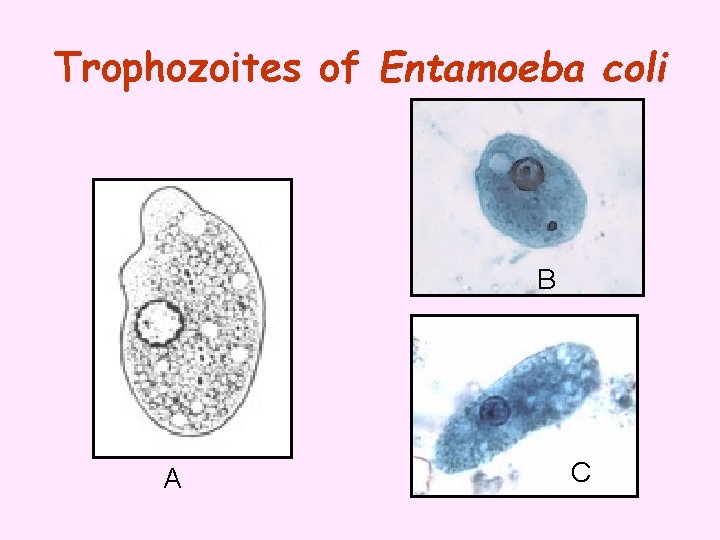
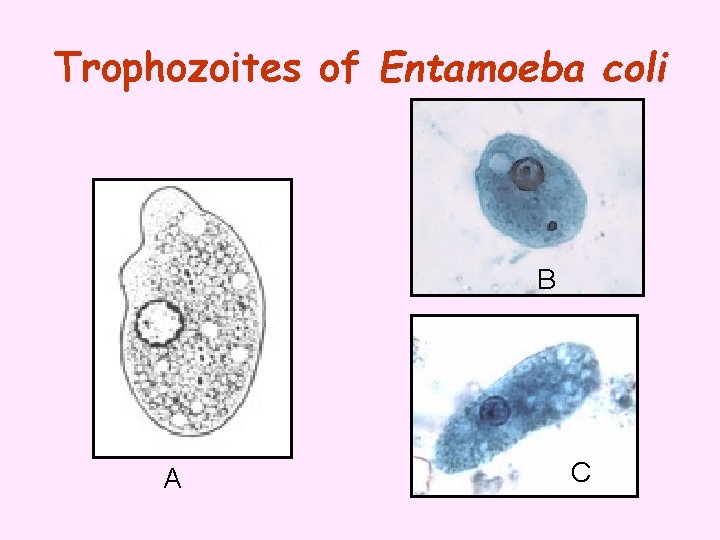
Trophozoites of Entamoeba coli B A C
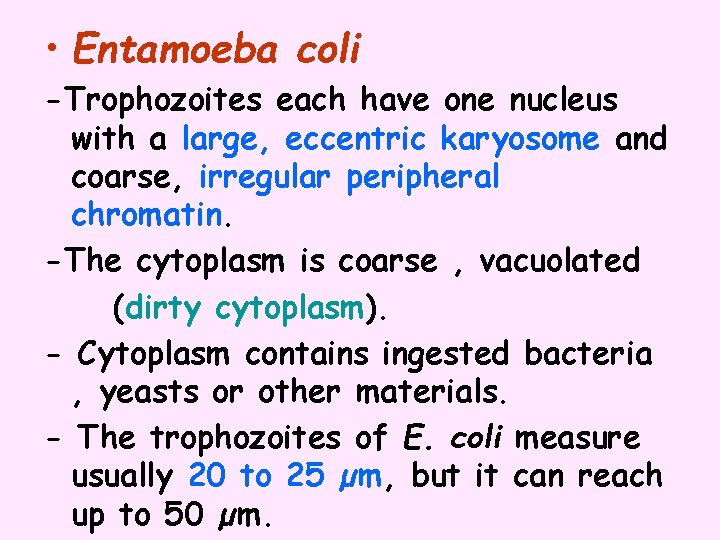
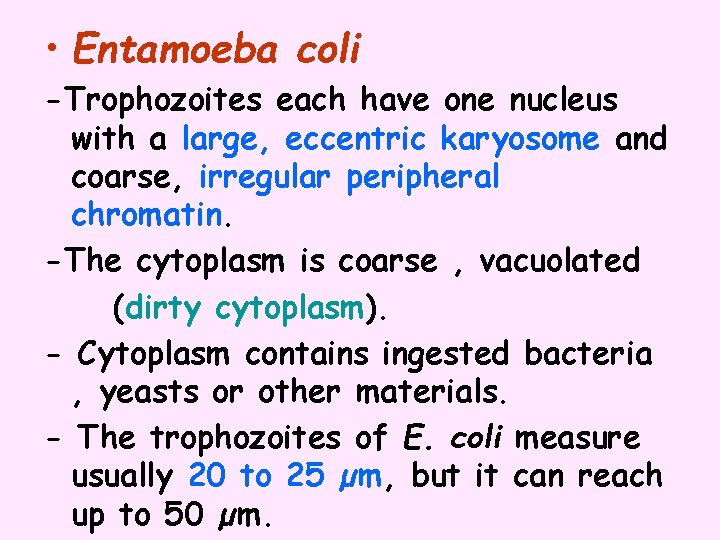
• Entamoeba coli -Trophozoites each have one nucleus with a large, eccentric karyosome and coarse, irregular peripheral chromatin. -The cytoplasm is coarse , vacuolated (dirty cytoplasm). - Cytoplasm contains ingested bacteria , yeasts or other materials. - The trophozoites of E. coli measure usually 20 to 25 µm, but it can reach up to 50 µm.
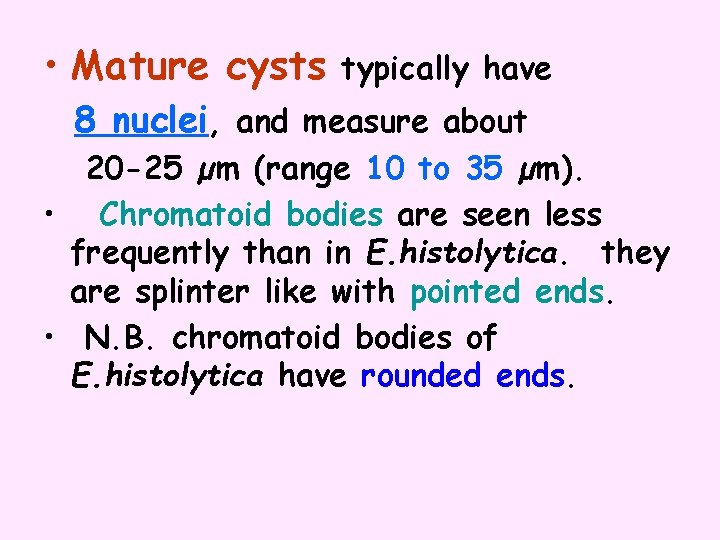
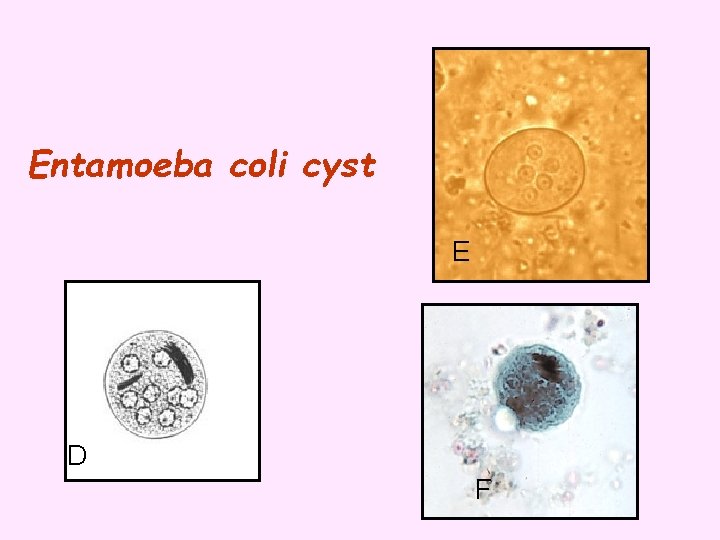
• Mature cysts typically have 8 nuclei, and measure about 20 -25 µm (range 10 to 35 µm). • Chromatoid bodies are seen less frequently than in E. histolytica. they are splinter like with pointed ends. • N. B. chromatoid bodies of E. histolytica have rounded ends.
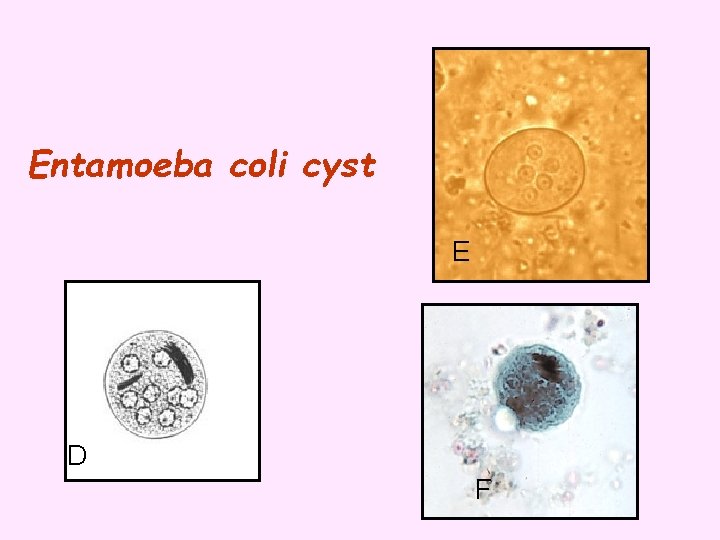
Entamoeba coli cyst E D F

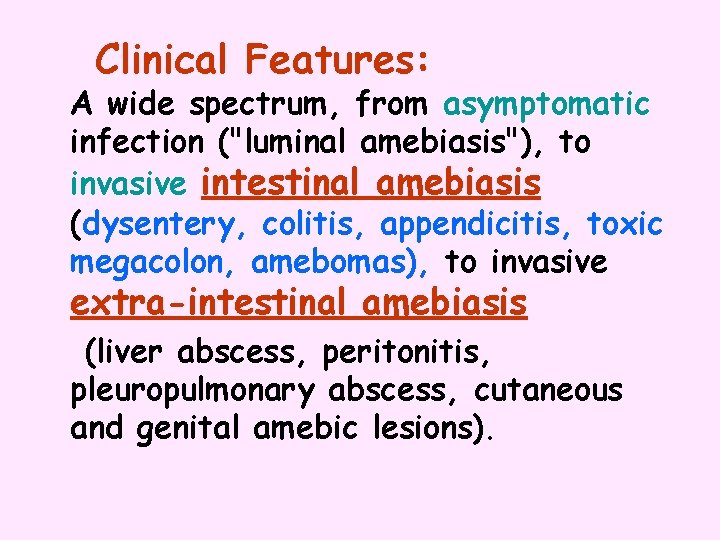
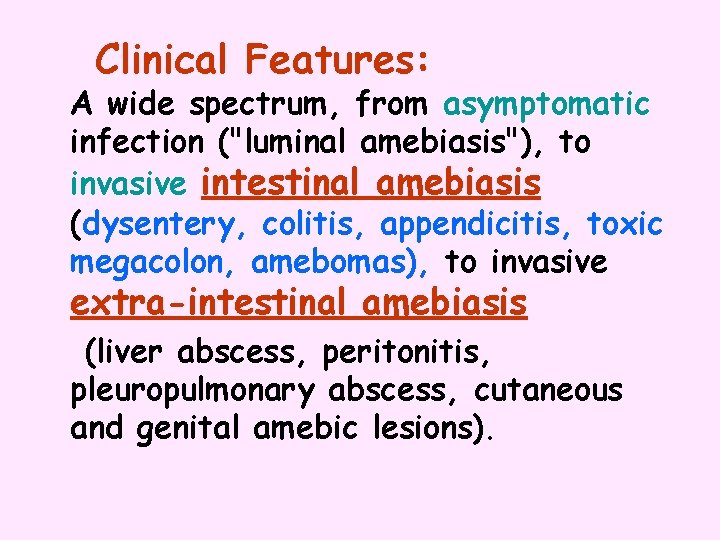
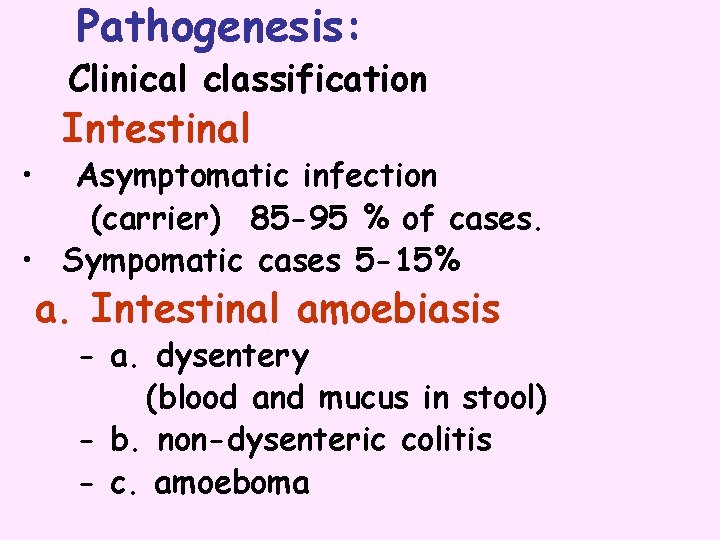
Clinical Features: A wide spectrum, from asymptomatic infection ("luminal amebiasis"), to invasive intestinal amebiasis (dysentery, colitis, appendicitis, toxic megacolon, amebomas), to invasive extra-intestinal amebiasis (liver abscess, peritonitis, pleuropulmonary abscess, cutaneous and genital amebic lesions).
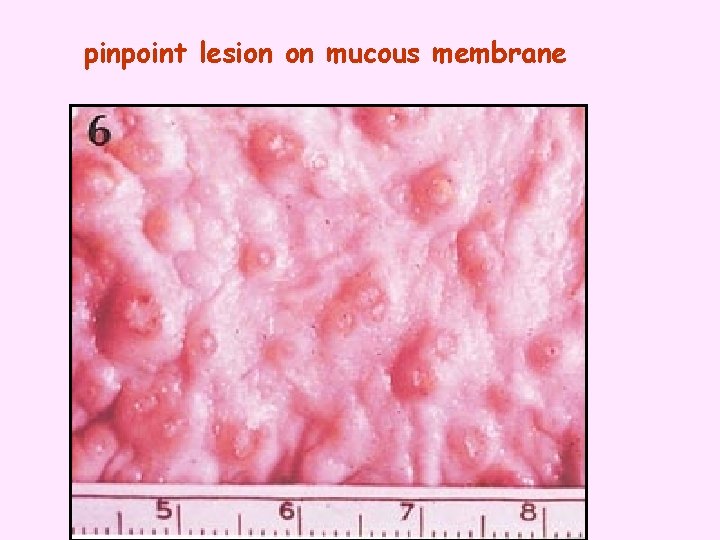
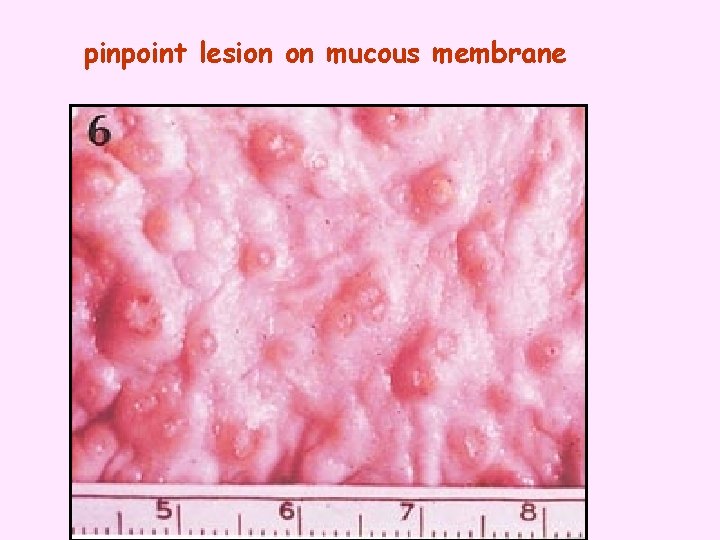
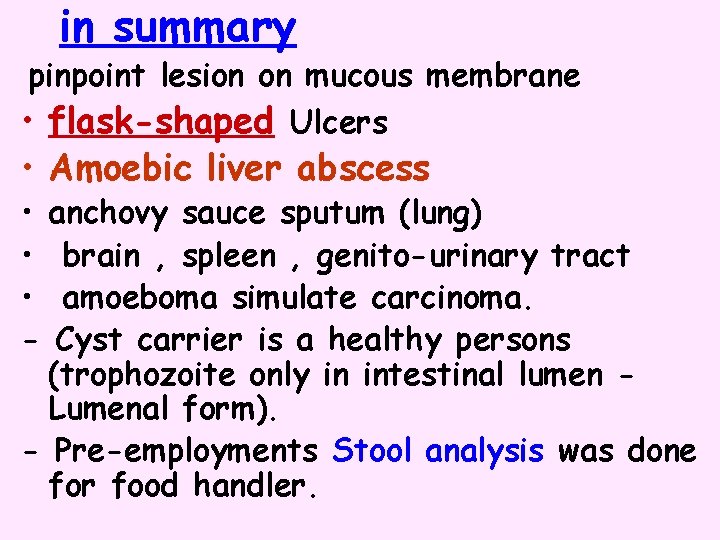
pinpoint lesion on mucous membrane

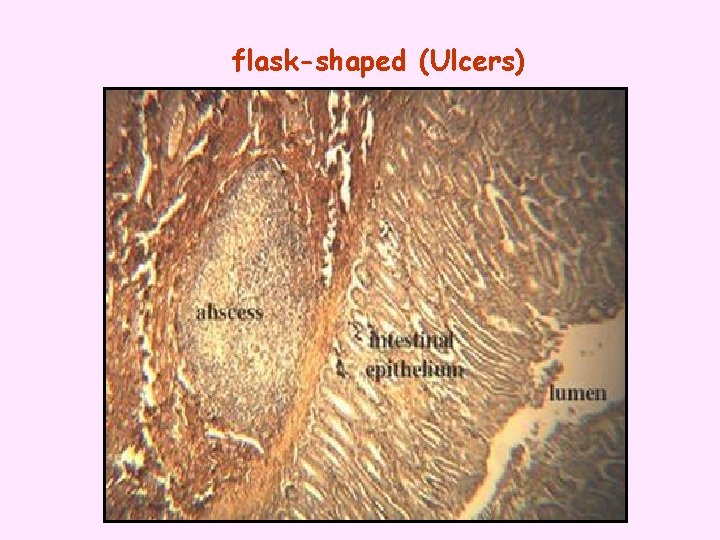
flask-shaped (Ulcers)
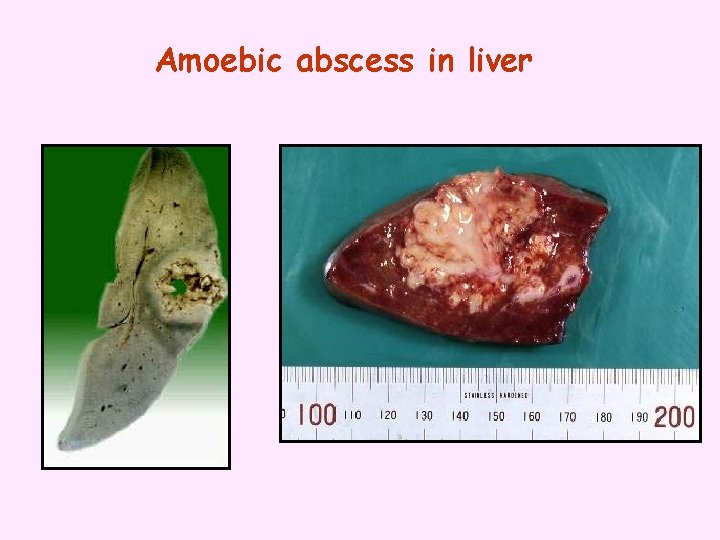
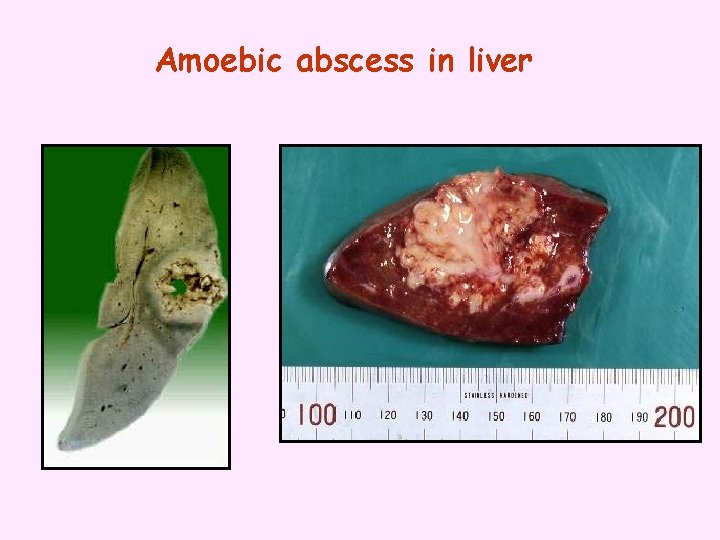
Amoebic abscess in liver


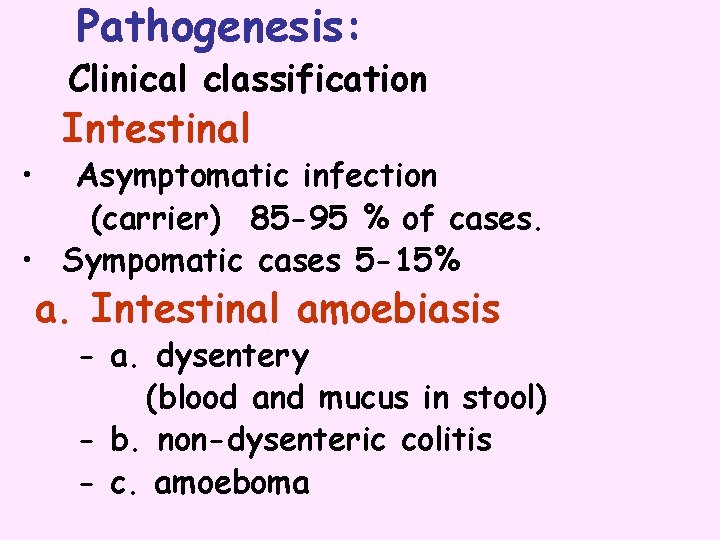
Pathogenesis: Clinical classification • Intestinal Asymptomatic infection (carrier) 85 -95 % of cases. • Sympomatic cases 5 -15% a. Intestinal amoebiasis - a. dysentery (blood and mucus in stool) - b. non-dysenteric colitis - c. amoeboma
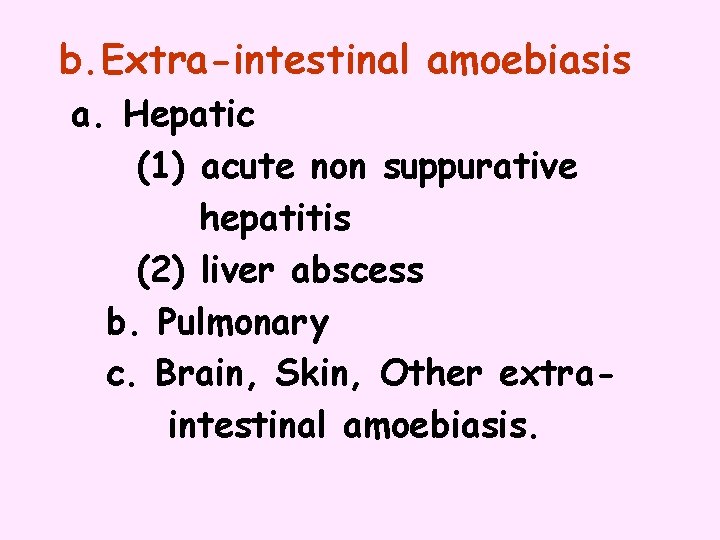
b. Extra-intestinal amoebiasis a. Hepatic (1) acute non suppurative hepatitis (2) liver abscess b. Pulmonary c. Brain, Skin, Other extraintestinal amoebiasis.
Hepatic amoebiasis: sing & symptoms • Local discomfort. • Malaise, fluctuant temperature • Toxemia. • Pain in right shoulder.
Diagnosis : intestinal Direct _ Microscopic identification of cysts and trophozoites in the stool _ trophozoites can also be identified in aspirates or biopsy samples obtained during colonoscopy or surgery. Indirect by immunodiagnosis (elisa)

Diagnosis: of Amoebic liver abscess • X-ray or ct scan show raised diaphragm • Blood picture –leucoytosis. • Serological test (elisa). • Examination of aspirate if indicated as treatment.

• Treatment: -For asymptomatic infections, (furamide) is the drugs of choice. -For symptomatic intestinal disease, or extra intestinal, infections (e. g. hepatic abscess), the drugs of choice are metronidazole or tinidazole, immediately followed by treatment with diloxanide furoate.
Prevention • human feces should not be used as fertilizer • food and drinks must be protected from flies. (mechanical transmission) • personal hygiene. wash hands after defecation and before meals. (autoinfection)
in summary pinpoint lesion on mucous membrane • flask-shaped Ulcers • Amoebic liver abscess • anchovy sauce sputum (lung) • brain , spleen , genito-urinary tract • amoeboma simulate carcinoma. - Cyst carrier is a healthy persons (trophozoite only in intestinal lumen Lumenal form). - Pre-employments Stool analysis was done for food handler.


FREE-LIVING PROTOZOA Ameba Diseases • Naegleria fowleri PAM • Acanthamoeba spp. GAE, skin or lung lesions, amebic keratitis.

Acanthameoba Have only 2 stage cyst And trophozoite. • Trophozoite and cyst are infective form. • portal of entry unknown, possibly respiratory tract, eyes, skin. • presumed hematogenous dissemination to the CNS. •
Acanthamoeba Encephalitis • infection associated with debilitation or immunosuppression. opportunistic parasitic inf. • chronic GAE (granulomatous amebic encephalitis). the organisms cause a granulomatous encephalitis that leads to death. • occurred in wearers of contact lenses.
Amebic Keratitis • Predisposing factors ocular trauma, contact lens (contaminated cleaning solutions). • Symptoms ocular pain, corneal lesions (refractory to usual treatments). • Diagnosis demonstration of amebas in corneal scrapings. • Treatment difficult, limited success corneal grafts often required.


Naegleria fowleri • found in fresh water. • ameba with loblose Pseudopodia. • motile bi-flagellated form. • PAM first recognized by Fowler (1965).

Primary Amebic Meningoencephalitis (PAM) • Symptoms usually within a few days after swimming in warm still waters. • Infection believed to be introduced through nasal cavity and olfactory bulbs. • Symptoms include headache, disorientation, coma.




Clinical picture A-Asymptomatic infection majority , about 80% B-Symptomatic infection: 1* typical picture most of symptomatic cases: incubation period 1 -2 weeks followed by diarrhea for bout 6 weeks. 2* atypical picture - malabsorption in children - fatty diahrrea - Sever diarrhoea.
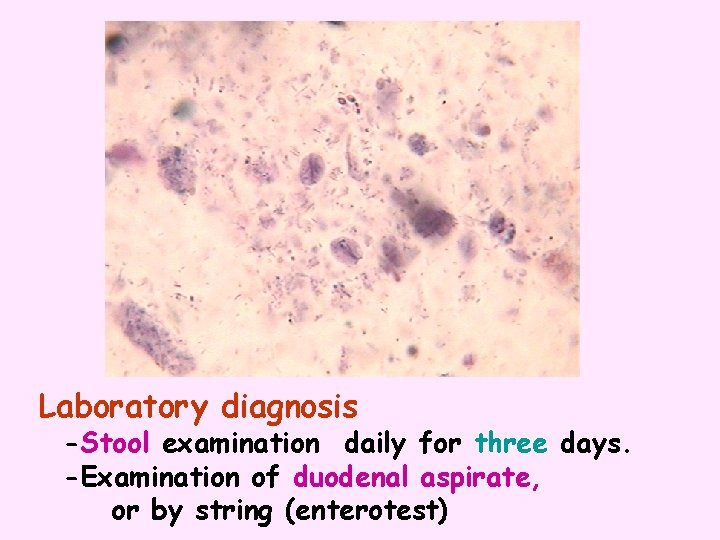
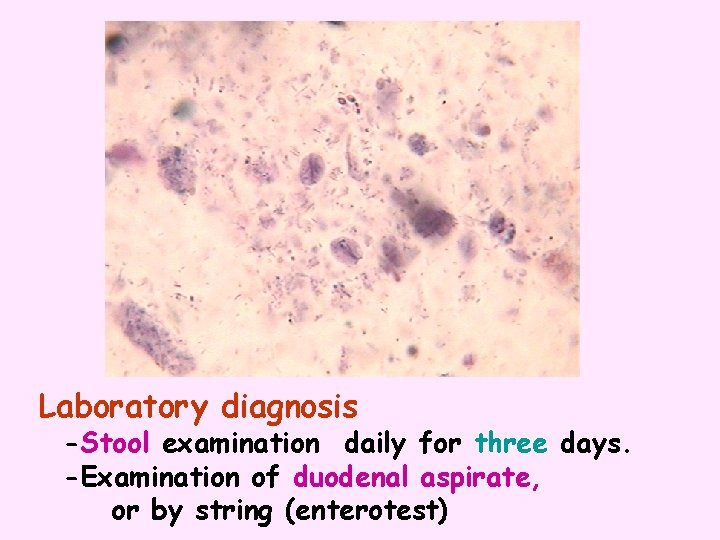
Laboratory diagnosis -Stool examination daily for three days. -Examination of duodenal aspirate, or by string (enterotest)



No cyst form

Trichomonas vaginalis • Transmission : sexual intercourse or contact with contaminated objects. • Pathology: • Female: vaginitis , profuse thin yellowish discharge with bad smell. • Male : invasion of urethra , prostate and seminal vesicles , causing urethritis but mostly asymptomatic.
• Diagnosis : identification of parasites by microscopy of discharge. (Examination of vaginal or uretheral discharge for T. vaginalis). • N. B. No cyst stage Imp

Cryptosporidium parvum
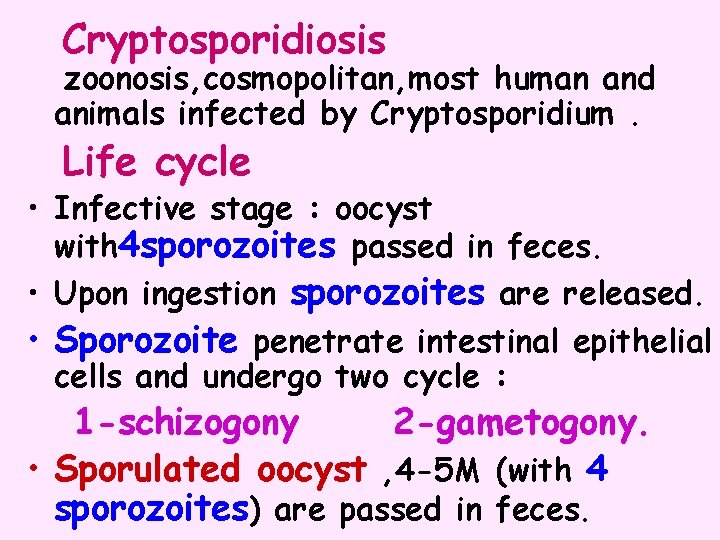
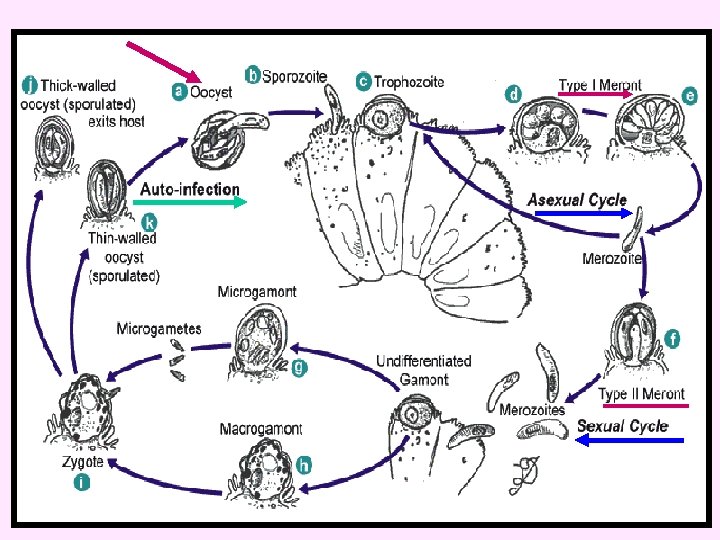
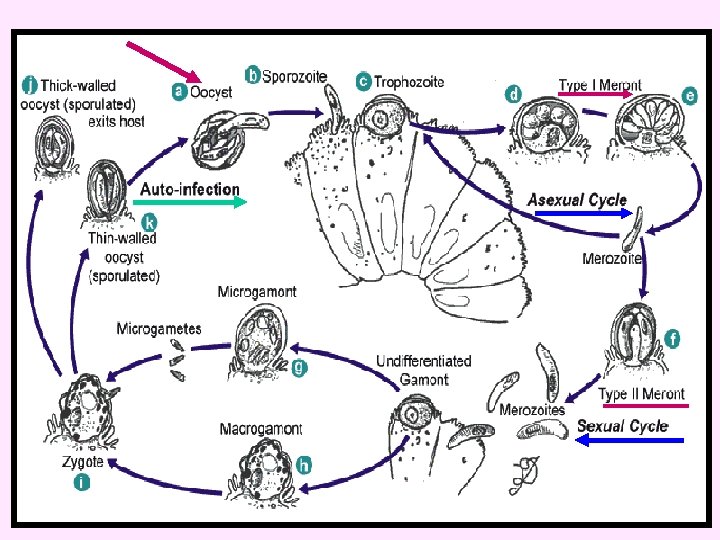
Cryptosporidiosis zoonosis, cosmopolitan, most human and animals infected by Cryptosporidium. Life cycle • Infective stage : oocyst with 4 sporozoites passed in feces. • Upon ingestion sporozoites are released. • Sporozoite penetrate intestinal epithelial cells and undergo two cycle : 1 -schizogony 2 -gametogony. • Sporulated oocyst , 4 -5 M (with 4 sporozoites) are passed in feces.
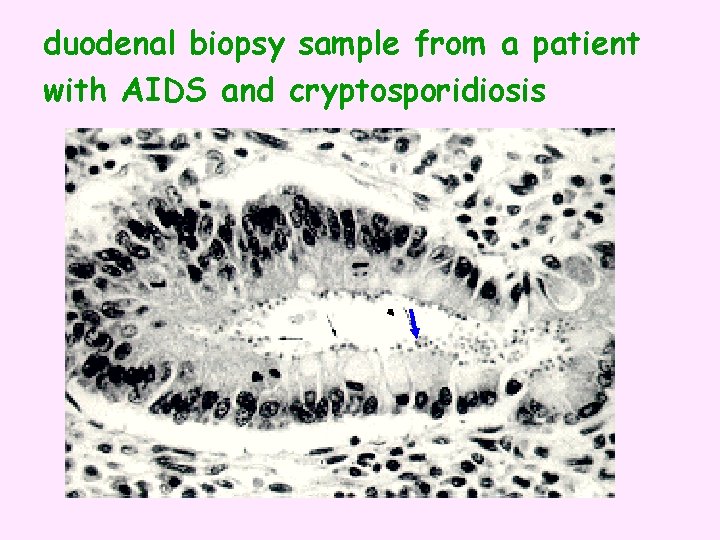
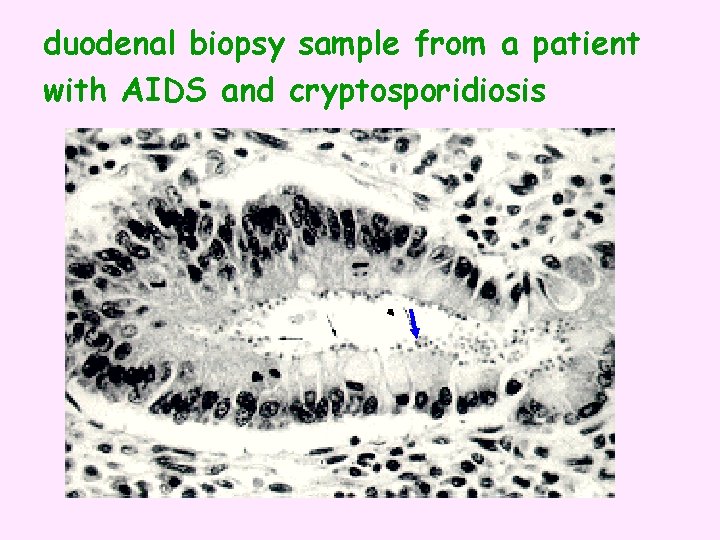
duodenal biopsy sample from a patient with AIDS and cryptosporidiosis

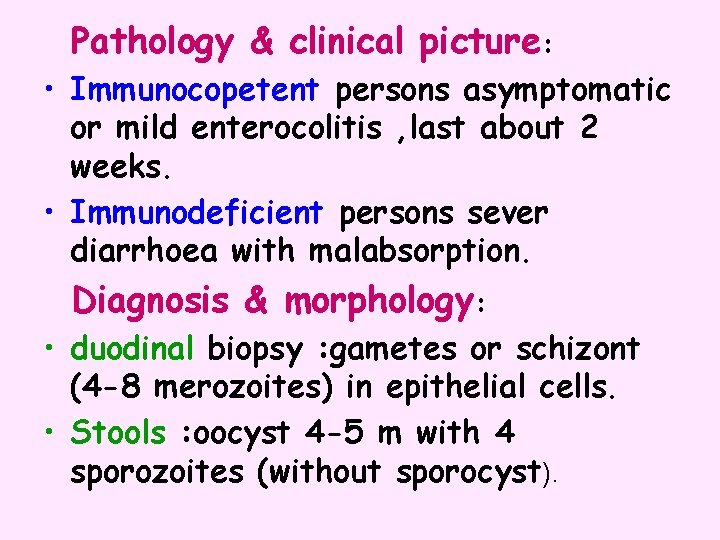
Pathology & clinical picture: • Immunocopetent persons asymptomatic or mild enterocolitis , last about 2 weeks. • Immunodeficient persons sever diarrhoea with malabsorption. Diagnosis & morphology: • duodinal biopsy : gametes or schizont (4 -8 merozoites) in epithelial cells. • Stools : oocyst 4 -5 m with 4 sporozoites (without sporocyst).
• Treatment - Self limited in immunocomptant persons , no effective drugs in cases of AIDS. - Management of fluid and electrolytes loss. • Prevention and control: -person-to person or animal to person transmission controlled by sanitation. -Identify common sources e. g. contaminated water
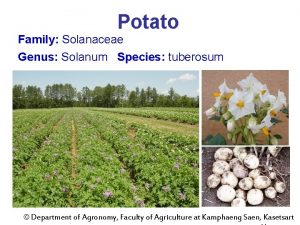
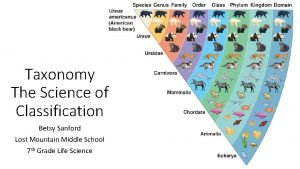
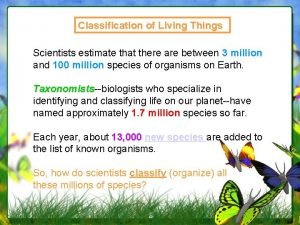
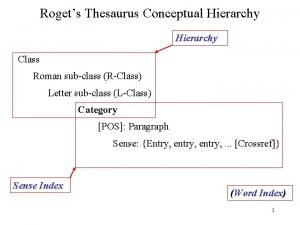
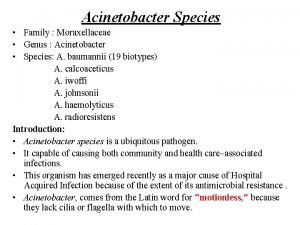
 Genus and species difference
Genus and species difference What is an autonym
What is an autonym Genus species format
Genus species format In which kingdom do humans belong to
In which kingdom do humans belong to Tuberosum is species or genus
Tuberosum is species or genus Species genus order
Species genus order Phylum order
Phylum order Genus and species names
Genus and species names Wolf classification
Wolf classification Kingdom family genus species
Kingdom family genus species Domain kingdom phylum
Domain kingdom phylum Scientific classification order
Scientific classification order Genus species
Genus species Biology
Biology Italicize genus and species
Italicize genus and species Sweet potato
Sweet potato Canis lupus genus
Canis lupus genus Genus and species examples
Genus and species examples Fibrobacteria
Fibrobacteria Classification of plant
Classification of plant Kingdom phylum class order family
Kingdom phylum class order family Genus and species difference
Genus and species difference 18-1 finding order in diversity answer key
18-1 finding order in diversity answer key Family order genus species
Family order genus species Triangle disease
Triangle disease Why is the saguaro cactus a keystone species
Why is the saguaro cactus a keystone species Oil rig oxidation
Oil rig oxidation Agent function vs agent program
Agent function vs agent program Reducing agent vs oxidizing agent
Reducing agent vs oxidizing agent Standard reduction table
Standard reduction table Agent a chapter 2
Agent a chapter 2 Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công của trọng lực
Công của trọng lực Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Các môn thể thao bắt đầu bằng tiếng đua
Các môn thể thao bắt đầu bằng tiếng đua Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập điện thế nghỉ
điện thế nghỉ Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ độ dài liên kết
độ dài liên kết Gấu đi như thế nào
Gấu đi như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Fecboak
Fecboak Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Ng-html
Ng-html Số nguyên tố là số gì
Số nguyên tố là số gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Tư thế ngồi viết
Tư thế ngồi viết Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Bổ thể
Bổ thể Tư thế ngồi viết
Tư thế ngồi viết V cc
V cc Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Hát lên người ơi alleluia
Hát lên người ơi alleluia Hươu thường đẻ mỗi lứa mấy con
Hươu thường đẻ mỗi lứa mấy con đại từ thay thế
đại từ thay thế Diễn thế sinh thái là
Diễn thế sinh thái là Genus
Genus Pravila definisanja
Pravila definisanja Autoinfection and retroinfection
Autoinfection and retroinfection King phillip came over from germany swimming
King phillip came over from germany swimming Fca genus
Fca genus Trypanosoma cruzi genus
Trypanosoma cruzi genus Bacteria genus
Bacteria genus