CatheterBase Treatment of Peripheral Venous Reflux Disease Misaki
Catheter-Base Treatment of Peripheral Venous Reflux Disease Misaki Kiguchi, MD, MBA, MSc Med. Star Washington Hospital Med. Star Georgetown University Hospital Washington, DC
Misaki Kiguchi, MD, MBA, MSc I have no relevant financial relationships.
Overview • Evaluation • Indications – Symptomatic – Anatomic • Technology • Outcomes • Tough questions • Summary
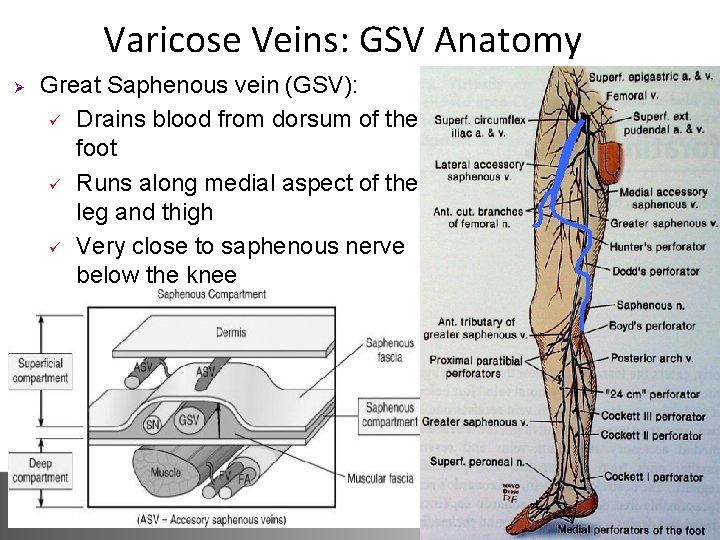
Varicose Veins: GSV Anatomy Ø Great Saphenous vein (GSV): ü Drains blood from dorsum of the foot ü Runs along medial aspect of the leg and thigh ü Very close to saphenous nerve below the knee
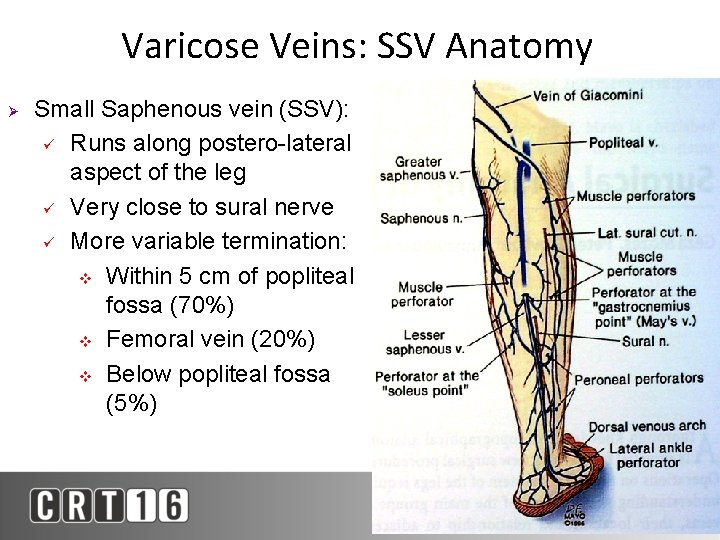
Varicose Veins: SSV Anatomy Ø Small Saphenous vein (SSV): ü Runs along postero-lateral aspect of the leg ü Very close to sural nerve ü More variable termination: v Within 5 cm of popliteal fossa (70%) v Femoral vein (20%) v Below popliteal fossa (5%)
Venous Disease: Epidemiology Ø Ø Ø Incidence: 25 - 40% of women and 15 - 30% of men Risk increases with age Predisposing factors: ü ü ü DVT Multiple pregnancies Family hx – pattern suggestive of autosomal dominant inheritance with variable penetrance v Both parents + 90% risk of varicose veins v One parent + 25% risk male, 62% female v No family hx < 20% risk
Venous Disease: Evaluation Ø History: Ø Ø Ø Symptoms – heaviness, fatigue, swelling, itching, aching Compression use DVT / hypercoagulability, personal or family Differential Dx: CHF, cirrhosis, renal failure, lymphedema, obesity, psoriasis, skin cancer Physical Exam: Ø Ø Ø Tactile and visual exam for varicosities Assess for skin discoloration, swelling Assess distribution of varicosities to pinpoint site of venous dysfunction
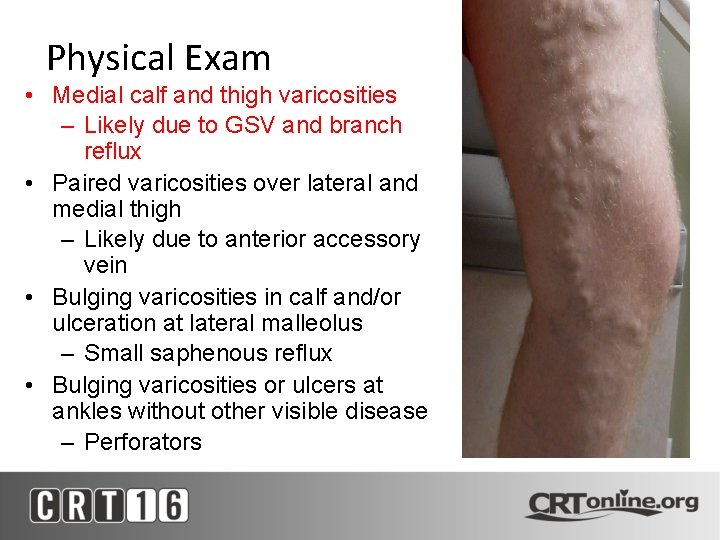
Physical Exam • Medial calf and thigh varicosities – Likely due to GSV and branch reflux • Paired varicosities over lateral and medial thigh – Likely due to anterior accessory vein • Bulging varicosities in calf and/or ulceration at lateral malleolus – Small saphenous reflux • Bulging varicosities or ulcers at ankles without other visible disease – Perforators
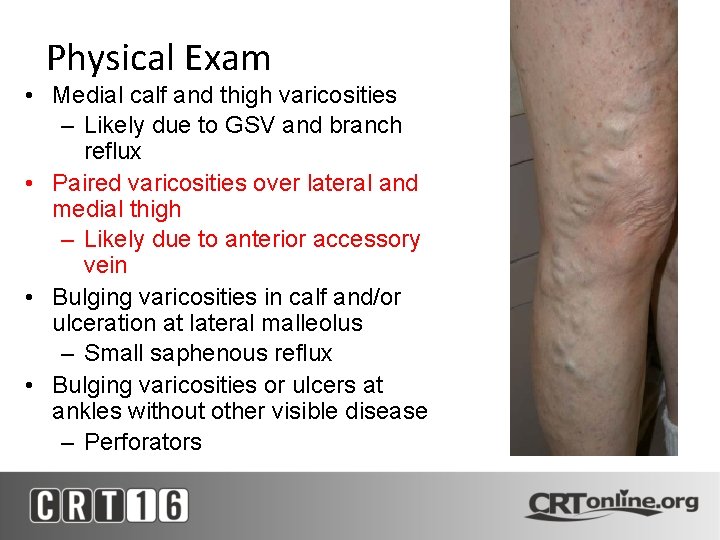
Physical Exam • Medial calf and thigh varicosities – Likely due to GSV and branch reflux • Paired varicosities over lateral and medial thigh – Likely due to anterior accessory vein • Bulging varicosities in calf and/or ulceration at lateral malleolus – Small saphenous reflux • Bulging varicosities or ulcers at ankles without other visible disease – Perforators
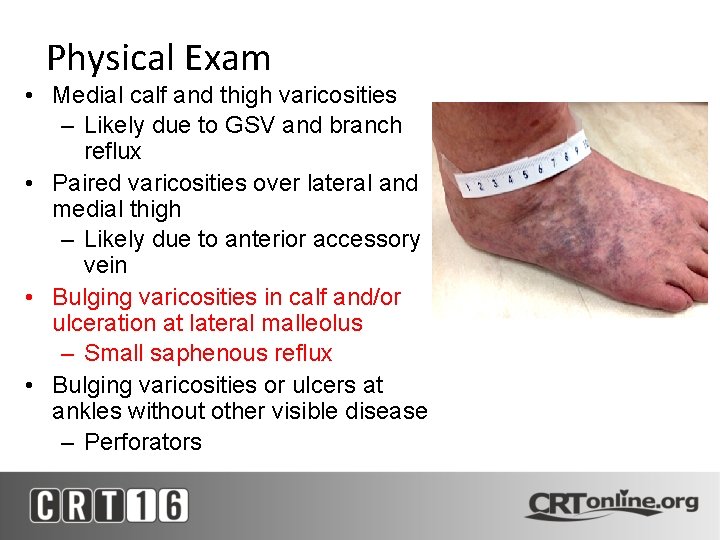
Physical Exam • Medial calf and thigh varicosities – Likely due to GSV and branch reflux • Paired varicosities over lateral and medial thigh – Likely due to anterior accessory vein • Bulging varicosities in calf and/or ulceration at lateral malleolus – Small saphenous reflux • Bulging varicosities or ulcers at ankles without other visible disease – Perforators
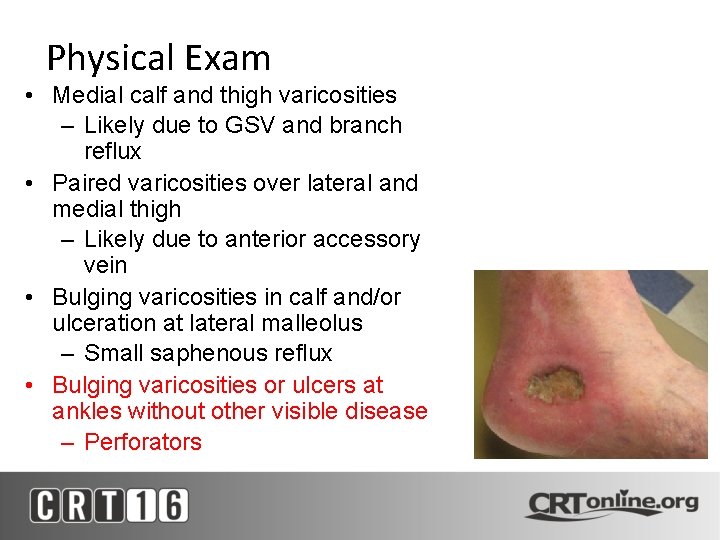
Physical Exam • Medial calf and thigh varicosities – Likely due to GSV and branch reflux • Paired varicosities over lateral and medial thigh – Likely due to anterior accessory vein • Bulging varicosities in calf and/or ulceration at lateral malleolus – Small saphenous reflux • Bulging varicosities or ulcers at ankles without other visible disease – Perforators
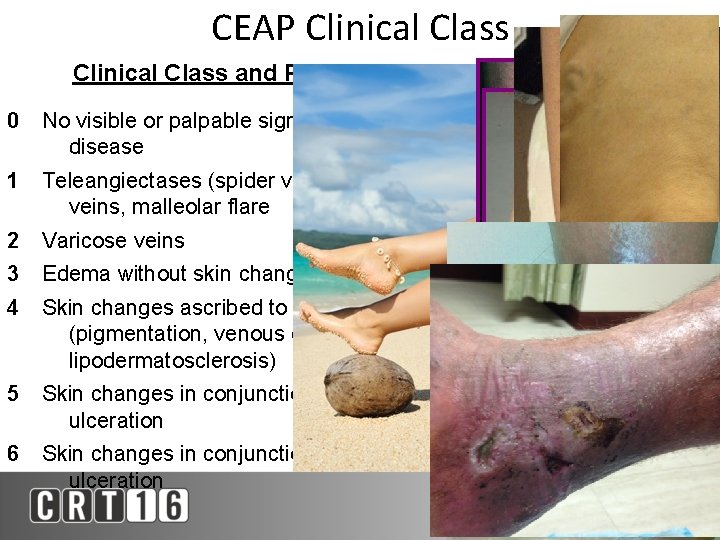
CEAP Clinical Class and Presentation 0 No visible or palpable signs of venous disease 1 Teleangiectases (spider veins), reticular veins, malleolar flare 2 Varicose veins 3 Edema without skin changes 4 Skin changes ascribed to venous disease (pigmentation, venous eczema, lipodermatosclerosis) 5 Skin changes in conjunction with healed ulceration 6 Skin changes in conjunction with active ulceration
Ultrasound Testing Ø Imaging of choice = Doppler Ultrasound Delineates anatomy Ø Mapping and planning therapy Ø Assess reflux and visualize valves Ø Assess for DVT, scarring, webs Ø Assess perforator veins Ø Can visualize nerves and surrounding structures MUST BE PERFORMED STANDING! Ø
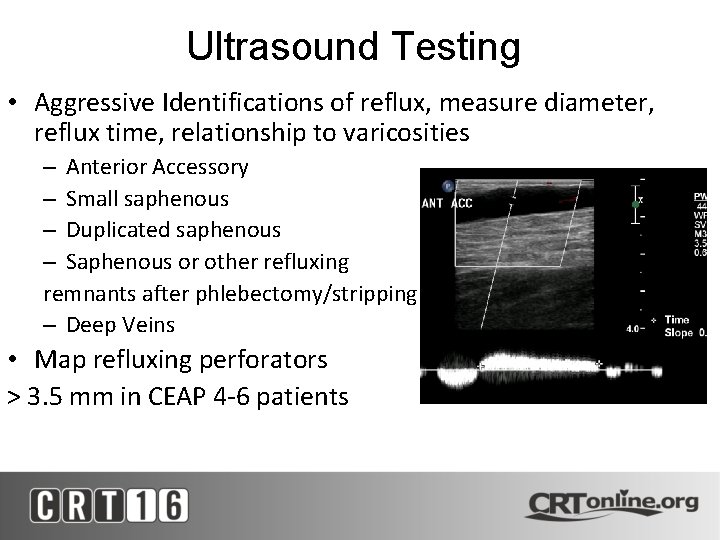
Ultrasound Testing • Aggressive Identifications of reflux, measure diameter, reflux time, relationship to varicosities – Anterior Accessory – Small saphenous – Duplicated saphenous – Saphenous or other refluxing remnants after phlebectomy/stripping – Deep Veins • Map refluxing perforators > 3. 5 mm in CEAP 4 -6 patients
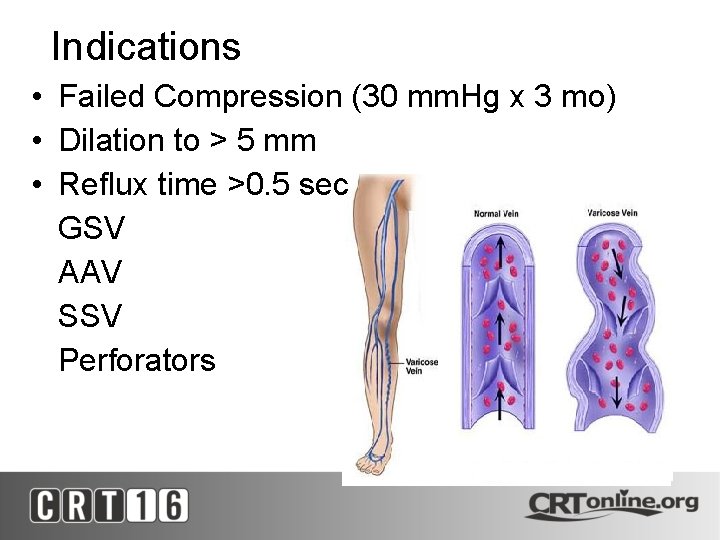
Indications • Failed Compression (30 mm. Hg x 3 mo) • Dilation to > 5 mm • Reflux time >0. 5 sec GSV AAV SSV Perforators
Thermal Ablation • Revolutionized venous treatment, performed in office with tumescent anesthesia • Catheter inserted in vein and passed up length of GSV/SSV • Laser: emits a single wavelength of light to damage endothelial lining • Radio Frequency creates resistive heating that contracts vein collagen and occludes • Laser and RFA effective; >90% closure rates • Both with 1 -5% DVT (EHIT) rate
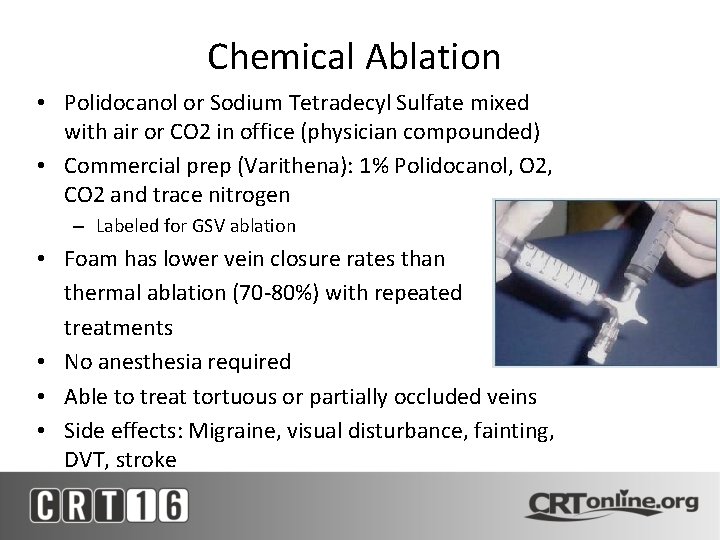
Chemical Ablation • Polidocanol or Sodium Tetradecyl Sulfate mixed with air or CO 2 in office (physician compounded) • Commercial prep (Varithena): 1% Polidocanol, O 2, CO 2 and trace nitrogen – Labeled for GSV ablation • Foam has lower vein closure rates than thermal ablation (70 -80%) with repeated treatments • No anesthesia required • Able to treat tortuous or partially occluded veins • Side effects: Migraine, visual disturbance, fainting, DVT, stroke
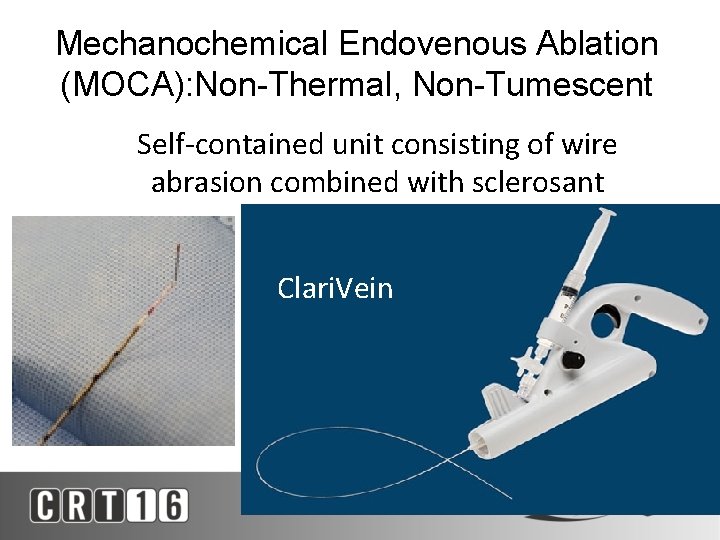
Mechanochemical Endovenous Ablation (MOCA): Non-Thermal, Non-Tumescent Self-contained unit consisting of wire abrasion combined with sclerosant Clari. Vein
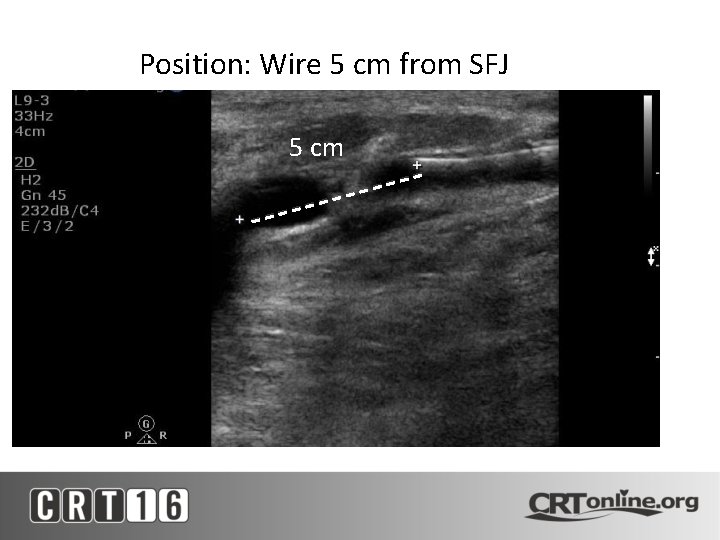
Position: Wire 5 cm from SFJ 5 cm

Wire Agitation with STS Infusion
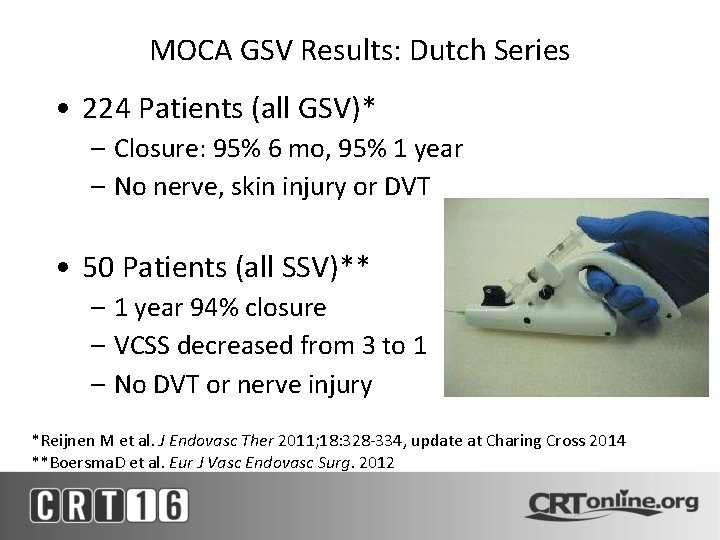
MOCA GSV Results: Dutch Series • 224 Patients (all GSV)* – Closure: 95% 6 mo, 95% 1 year – No nerve, skin injury or DVT • 50 Patients (all SSV)** – 1 year 94% closure – VCSS decreased from 3 to 1 – No DVT or nerve injury *Reijnen M et al. J Endovasc Ther 2011; 18: 328 -334, update at Charing Cross 2014 **Boersma. D et al. Eur J Vasc Endovasc Surg. 2012
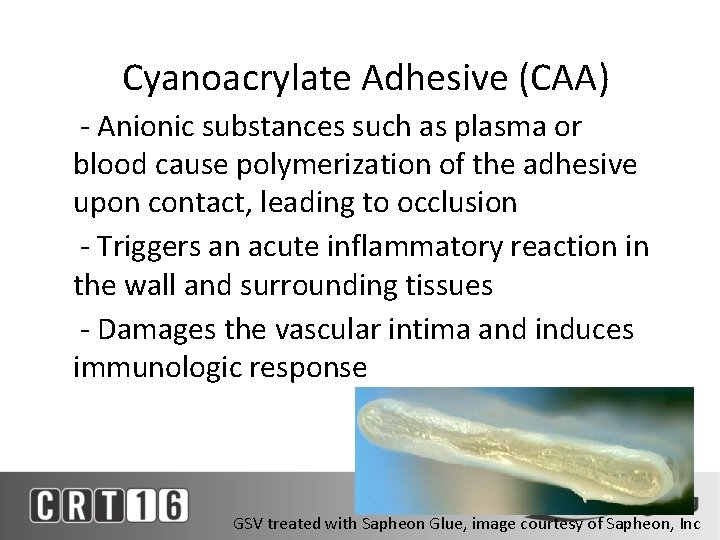
Cyanoacrylate Adhesive (CAA) - Anionic substances such as plasma or blood cause polymerization of the adhesive upon contact, leading to occlusion - Triggers an acute inflammatory reaction in the wall and surrounding tissues - Damages the vascular intima and induces immunologic response GSV treated with Sapheon Glue, image courtesy of Sapheon, Inc
Cyanoacrylate Adhesive (CAA) - Permitted for use in endovascular procedures in Europe for several decades - FDA approved in U. S. 2000 Trufill CA (Cordis, Miami, FL) clearance for treatment of cerebral AVMs - The Vena. Seal® Sapheon Closure System (Medtronic) is a CE-marketed medical device and is commercially available in Europe, Australia, Hong Kong, and Canada. FDA approved May 2015, selected release now
Cyanoacrylate Glue • Ve. CLOSE US Trial; 242 patients – 98. 9% closure at 6 months – No differences in outcomes or patients pain vs Closure. Fast • European Multicenter Trial; 70 patients – 94% occlusion at 12 months – 8. 7% phlebitis – VCSS 4. 3 to 1. 3 – No DVT/PE/nerve injury Nick Morrison, presented at ACP 2014 Proebstle et al JVSVLD Vol 1 2014
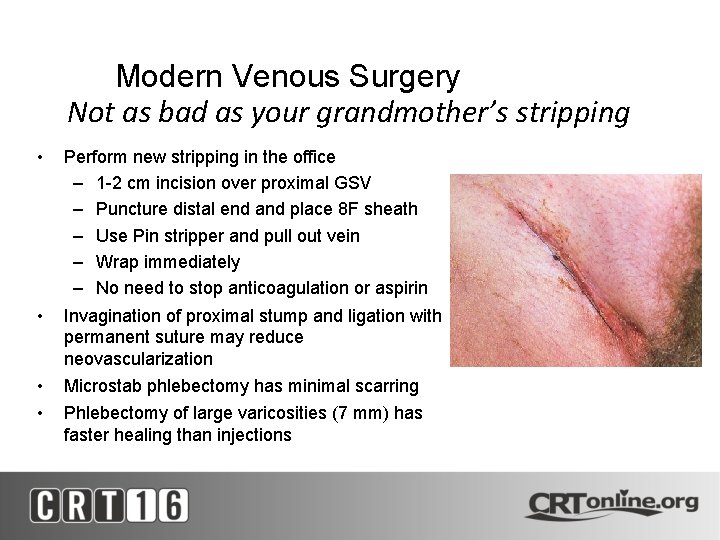
Modern Venous Surgery Not as bad as your grandmother’s stripping • Perform new stripping in the office – 1 -2 cm incision over proximal GSV – Puncture distal end and place 8 F sheath – Use Pin stripper and pull out vein – Wrap immediately – No need to stop anticoagulation or aspirin • Invagination of proximal stump and ligation with permanent suture may reduce neovascularization • • Microstab phlebectomy has minimal scarring Phlebectomy of large varicosities (7 mm) has faster healing than injections

Pre-Op incisions 3 wks post-op
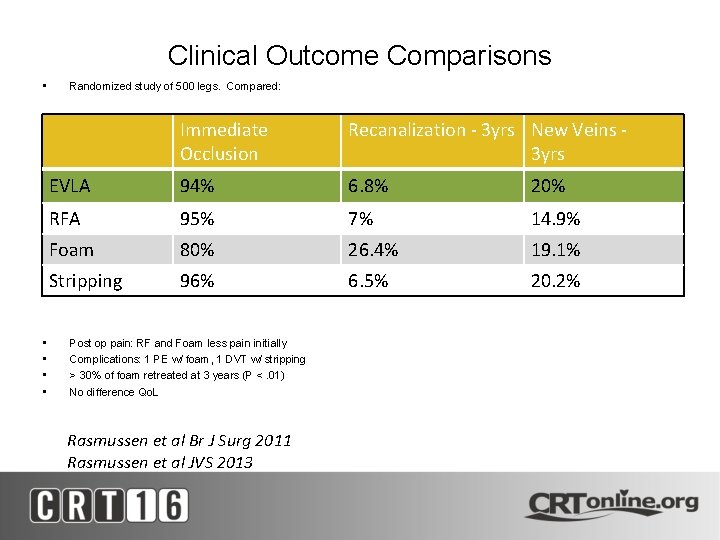
Clinical Outcome Comparisons • • • Randomized study of 500 legs. Compared: Immediate Occlusion Recanalization - 3 yrs New Veins 3 yrs EVLA 94% 6. 8% 20% RFA 95% 7% 14. 9% Foam 80% 26. 4% 19. 1% Stripping 96% 6. 5% 20. 2% Post op pain: RF and Foam less pain initially Complications: 1 PE w/ foam, 1 DVT w/ stripping > 30% of foam retreated at 3 years (P <. 01) No difference Qo. L Rasmussen et al Br J Surg 2011 Rasmussen et al JVS 2013

What Do We Do? • Compression: - Aces/ Coban daily – Unnas boot 1 -2 x/wk • Assessment: – Reflux US of Superficial and Deep Veins – R/O DVT • Treatment: – Debride wound – Ablate refluxing varicosities • Lifestyle Change: – Compression for life – Weight reduction, Medical Optimization
Conclusions • Lots of good choices for Venous Disease – Excellent safety profiles – Easy to use, tolerate – Expect patients to have improved Qo. L • Better outcomes than ever before • Educate that venous disease is lifelong, and lifestyle changes may be needed
- Slides: 29