cases Dr Payal Damor R 2 Radio diagnosis

- Slides: 77
cases Dr Payal Damor R 2 Radio diagnosis S. S. G. H BARODA 25 -11 -08 1
Case 1 2
40 yr female come with Lt sided breast discomfort since 2 weak, she underwent breast implantation 8 yrs back. 3
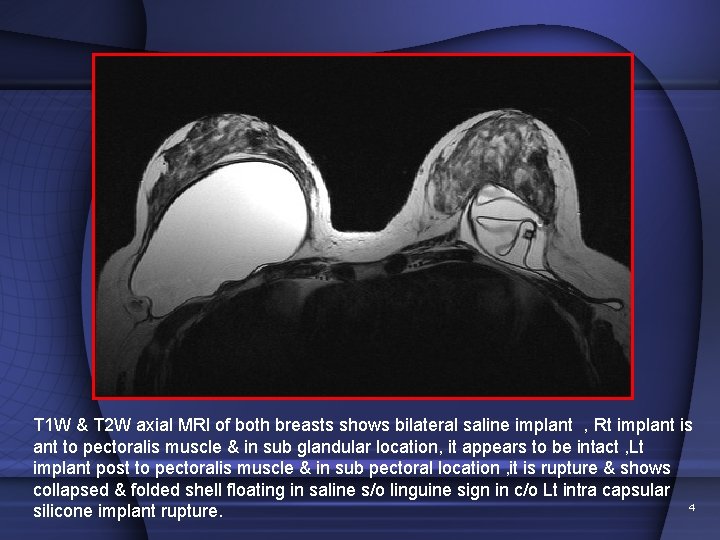
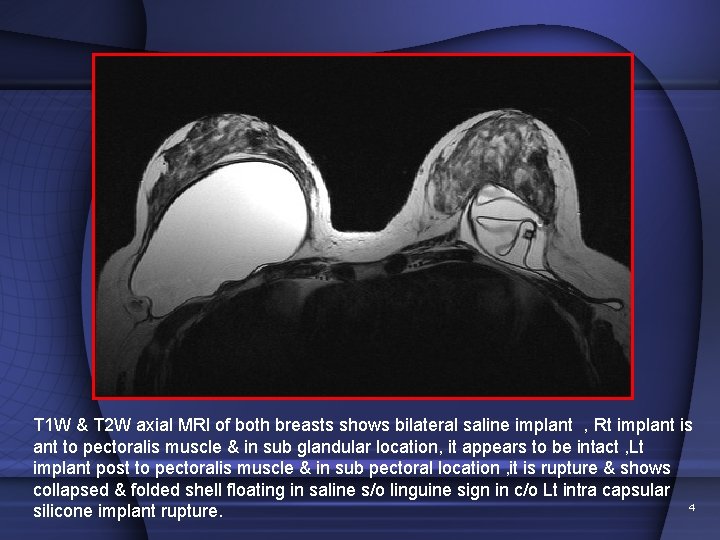
T 1 W & T 2 W axial MRI of both breasts shows bilateral saline implant , Rt implant is ant to pectoralis muscle & in sub glandular location, it appears to be intact , Lt implant post to pectoralis muscle & in sub pectoral location , it is rupture & shows collapsed & folded shell floating in saline s/o linguine sign in c/o Lt intra capsular 4 silicone implant rupture.
DIAGNOSIS: Left sub pectoralis intra capsular silicon implant rupture 5
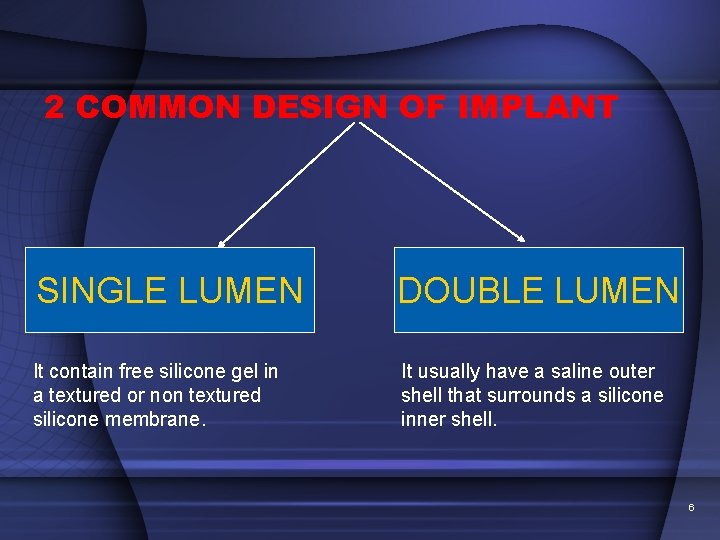
2 COMMON DESIGN OF IMPLANT SINGLE LUMEN DOUBLE LUMEN It contain free silicone gel in a textured or non textured silicone membrane. It usually have a saline outer shell that surrounds a silicone inner shell. 6
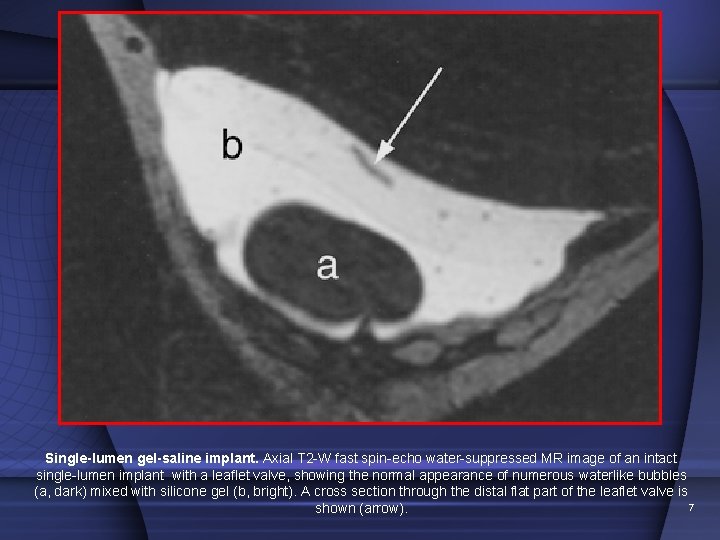
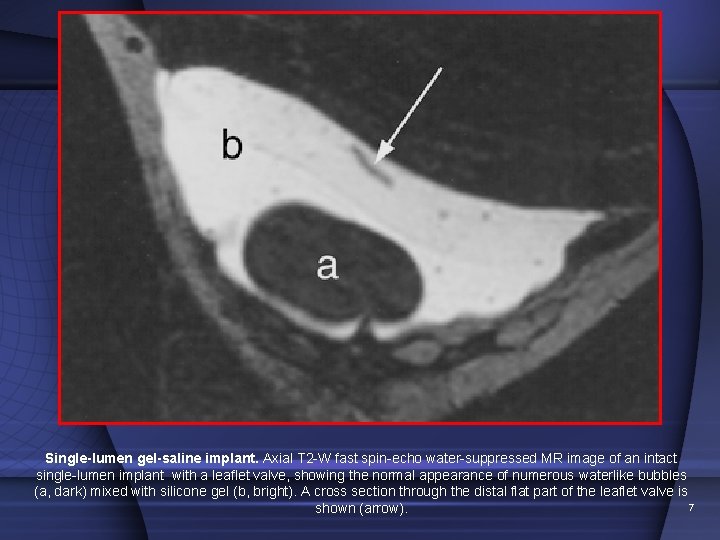
Single-lumen gel-saline implant. Axial T 2 -W fast spin-echo water-suppressed MR image of an intact single-lumen implant with a leaflet valve, showing the normal appearance of numerous waterlike bubbles (a, dark) mixed with silicone gel (b, bright). A cross section through the distal flat part of the leaflet valve is 7 shown (arrow).
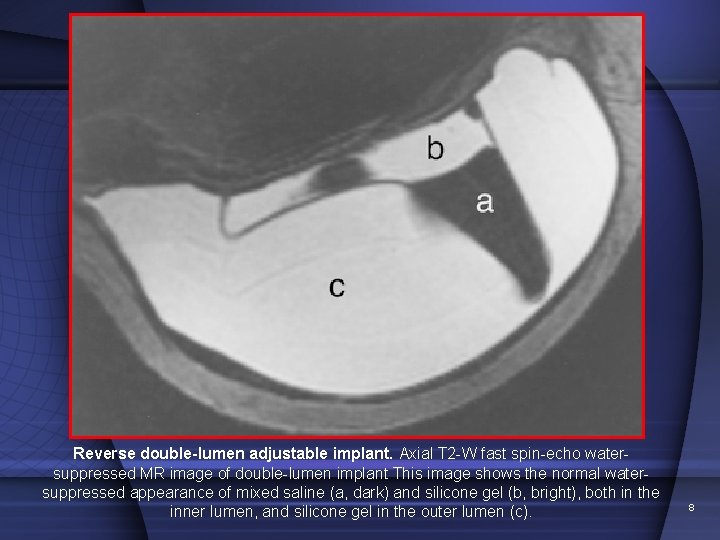
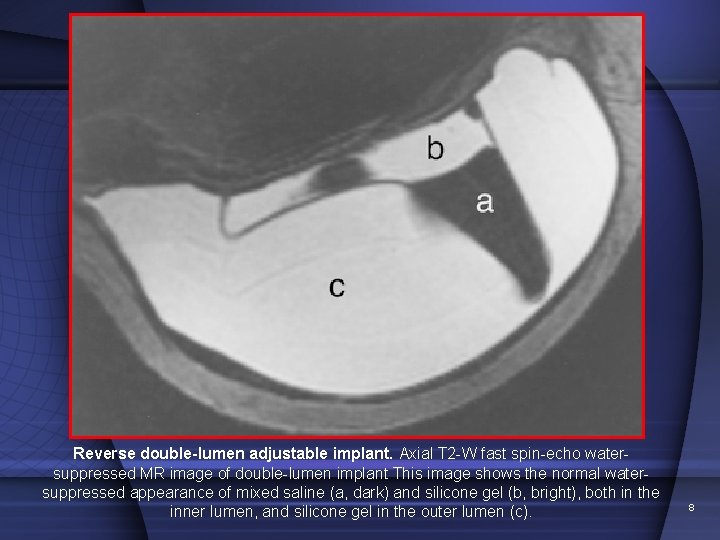
Reverse double-lumen adjustable implant. Axial T 2 -W fast spin-echo watersuppressed MR image of double-lumen implant This image shows the normal watersuppressed appearance of mixed saline (a, dark) and silicone gel (b, bright), both in the inner lumen, and silicone gel in the outer lumen (c). 8
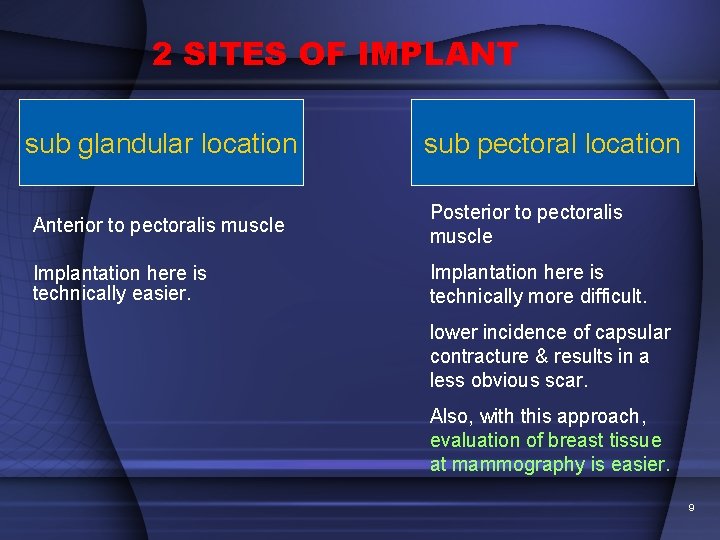
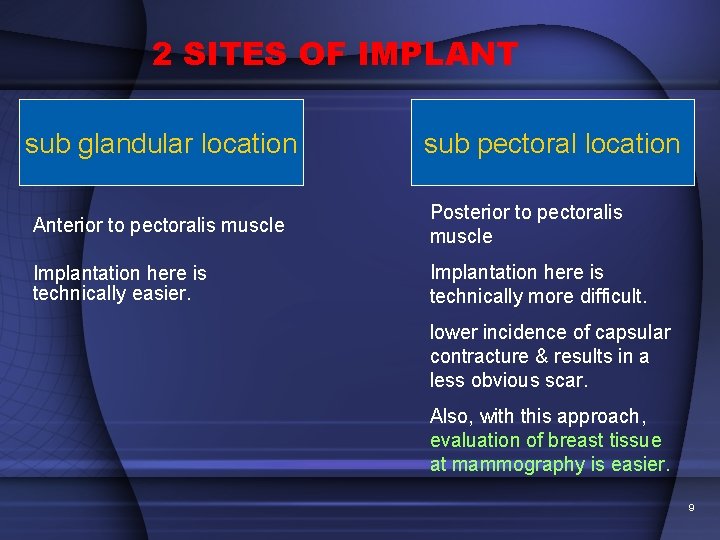
2 SITES OF IMPLANT sub glandular location sub pectoral location Anterior to pectoralis muscle Posterior to pectoralis muscle Implantation here is technically easier. Implantation here is technically more difficult. lower incidence of capsular contracture & results in a less obvious scar. Also, with this approach, evaluation of breast tissue at mammography is easier. 9
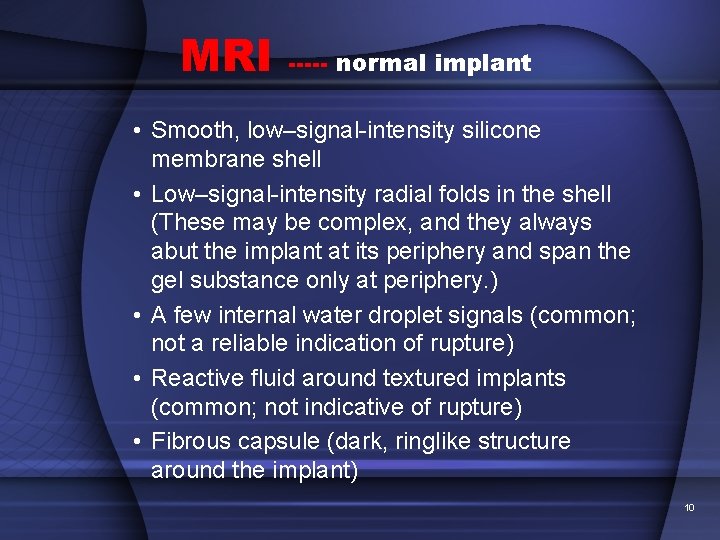
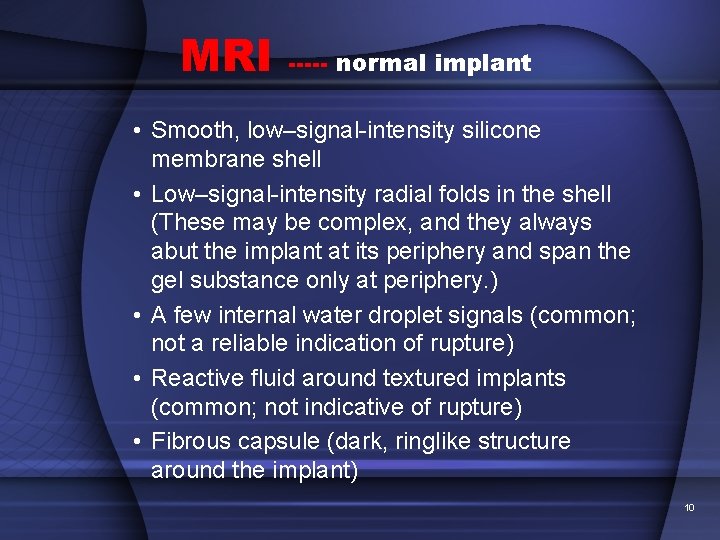
MRI ----- normal implant • Smooth, low–signal-intensity silicone membrane shell • Low–signal-intensity radial folds in the shell (These may be complex, and they always abut the implant at its periphery and span the gel substance only at periphery. ) • A few internal water droplet signals (common; not a reliable indication of rupture) • Reactive fluid around textured implants (common; not indicative of rupture) • Fibrous capsule (dark, ringlike structure around the implant) 10
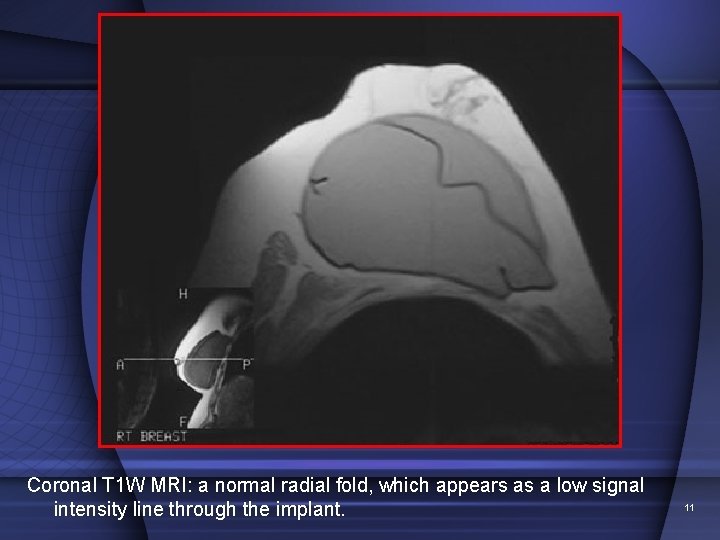
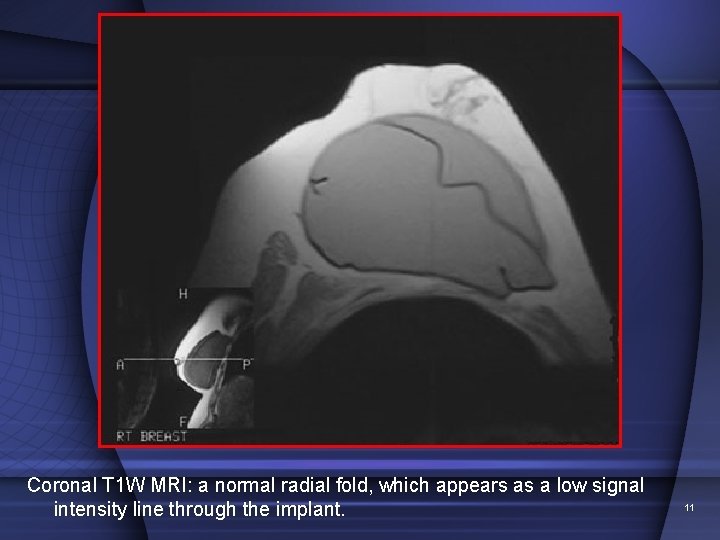
Coronal T 1 W MRI: a normal radial fold, which appears as a low signal intensity line through the implant. 11
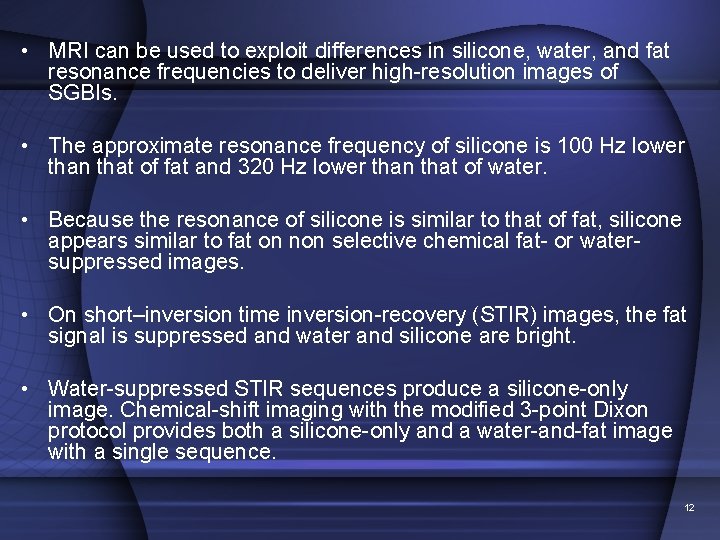
• MRI can be used to exploit differences in silicone, water, and fat resonance frequencies to deliver high-resolution images of SGBIs. • The approximate resonance frequency of silicone is 100 Hz lower than that of fat and 320 Hz lower than that of water. • Because the resonance of silicone is similar to that of fat, silicone appears similar to fat on non selective chemical fat- or watersuppressed images. • On short–inversion time inversion-recovery (STIR) images, the fat signal is suppressed and water and silicone are bright. • Water-suppressed STIR sequences produce a silicone-only image. Chemical-shift imaging with the modified 3 -point Dixon protocol provides both a silicone-only and a water-and-fat image with a single sequence. 12
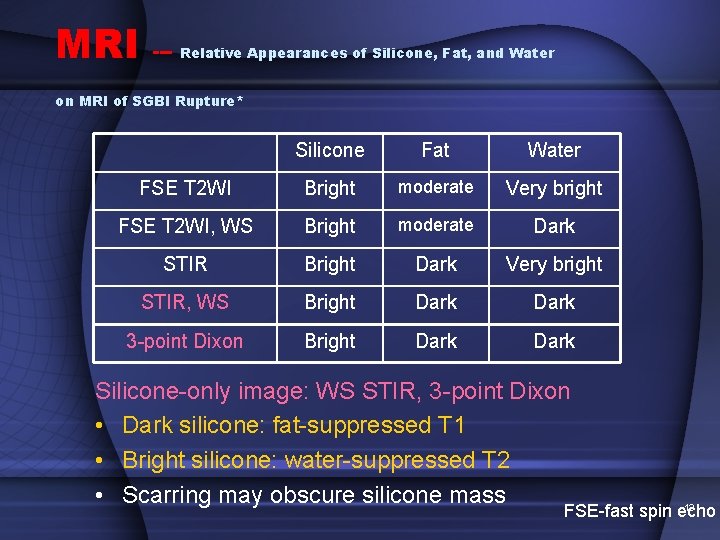
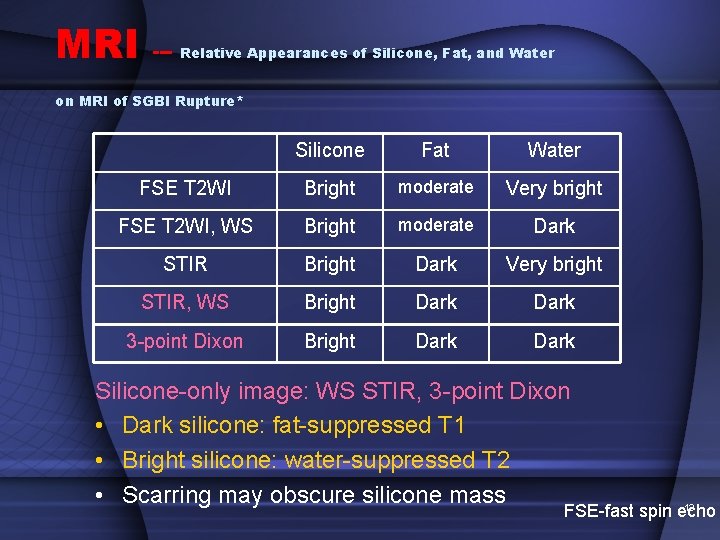
MRI --- Relative Appearances of Silicone, Fat, and Water on MRI of SGBI Rupture* Silicone Fat Water FSE T 2 WI Bright moderate Very bright FSE T 2 WI, WS Bright moderate Dark STIR Bright Dark Very bright STIR, WS Bright Dark 3 -point Dixon Bright Dark Silicone-only image: WS STIR, 3 -point Dixon • Dark silicone: fat-suppressed T 1 • Bright silicone: water-suppressed T 2 • Scarring may obscure silicone mass 13 FSE-fast spin echo
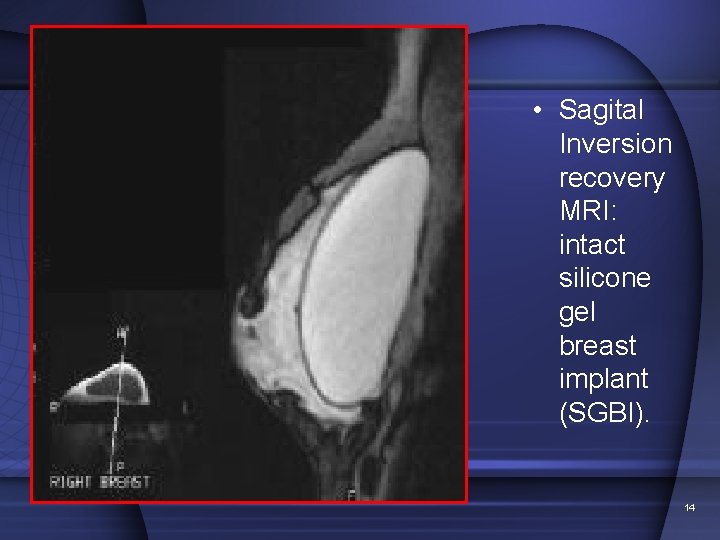
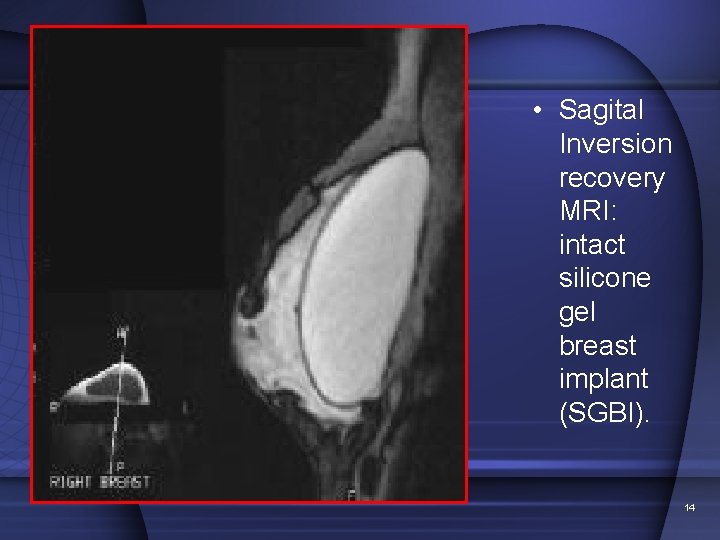
• Sagital Inversion recovery MRI: intact silicone gel breast implant (SGBI). 14
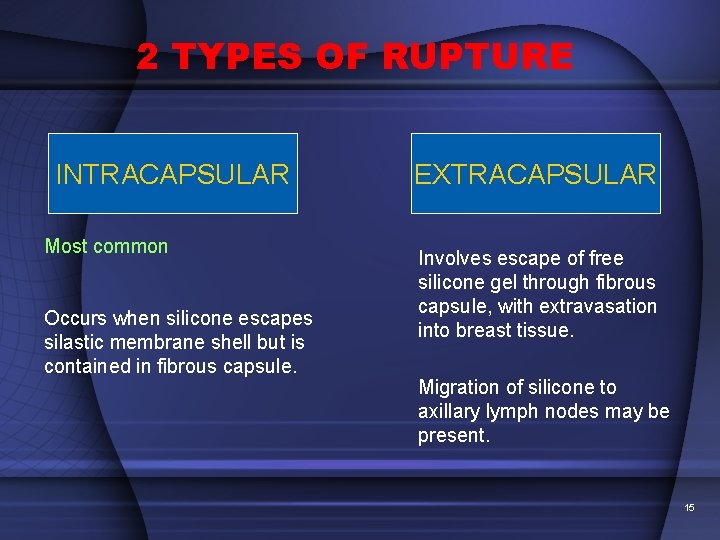
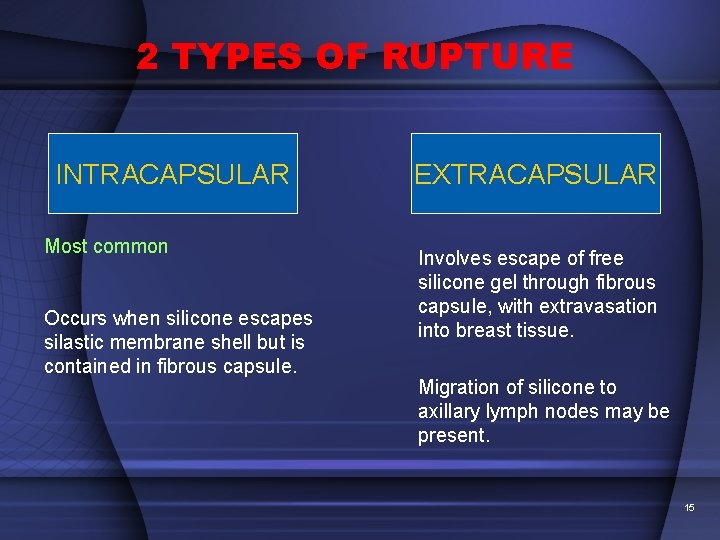
2 TYPES OF RUPTURE INTRACAPSULAR Most common Occurs when silicone escapes silastic membrane shell but is contained in fibrous capsule. EXTRACAPSULAR Involves escape of free silicone gel through fibrous capsule, with extravasation into breast tissue. Migration of silicone to axillary lymph nodes may be present. 15
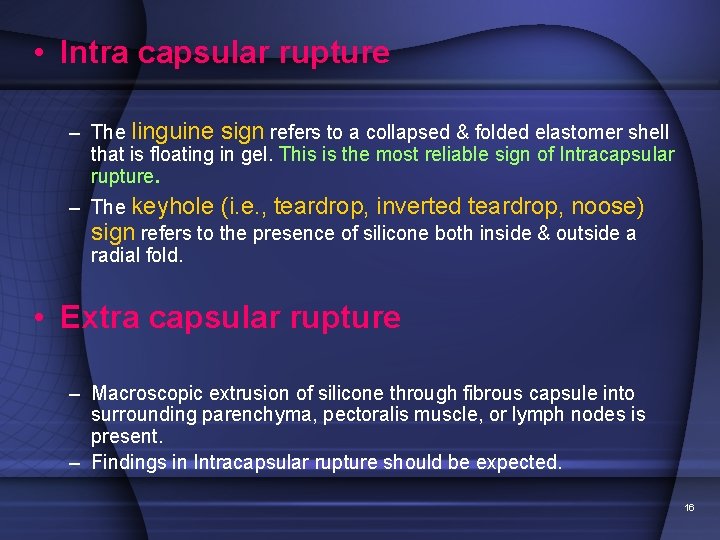
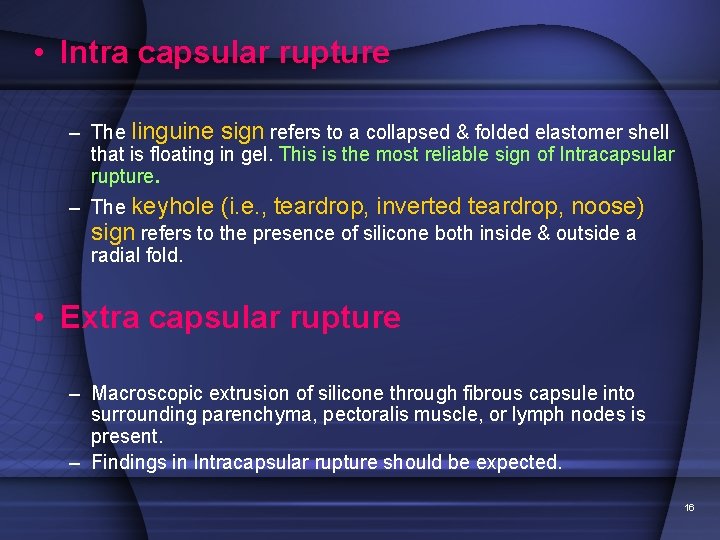
• Intra capsular rupture – The linguine sign refers to a collapsed & folded elastomer shell that is floating in gel. This is the most reliable sign of Intracapsular rupture. – The keyhole (i. e. , teardrop, inverted teardrop, noose) sign refers to the presence of silicone both inside & outside a radial fold. • Extra capsular rupture – Macroscopic extrusion of silicone through fibrous capsule into surrounding parenchyma, pectoralis muscle, or lymph nodes is present. – Findings in Intracapsular rupture should be expected. 16
MRI --- Linguine sign • Indicates intracapsular rupture of the breast implant. • Most sensitive among all signs of intracapsular rupture from other imaging modalities, with a sensitivity of 96% & a specificity of 94%. • Wavy lines on MR images represent collapsed shell floating in silicone. • Although linguine sign is fairly easy to detect, the signs of early intracapsular rupture (tear drop sign, keyhole sign, subcapsular line sign) were more common than linguine sign. 17
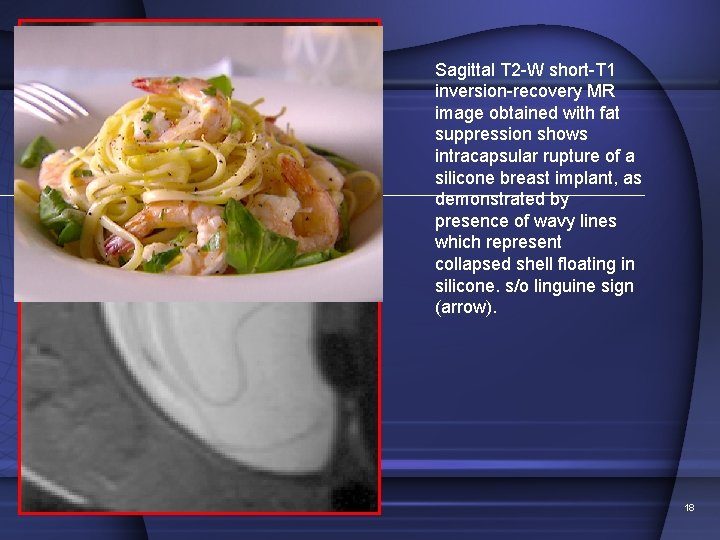
Sagittal T 2 -W short-T 1 inversion-recovery MR image obtained with fat suppression shows intracapsular rupture of a silicone breast implant, as demonstrated by presence of wavy lines which represent collapsed shell floating in silicone. s/o linguine sign (arrow). 18
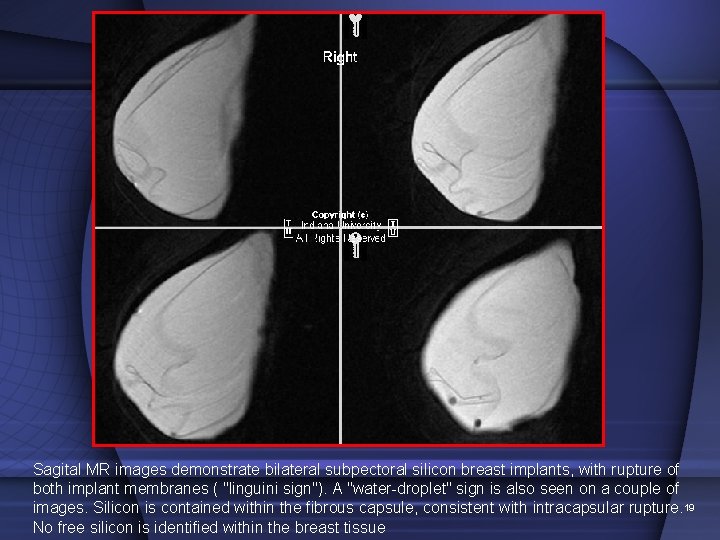
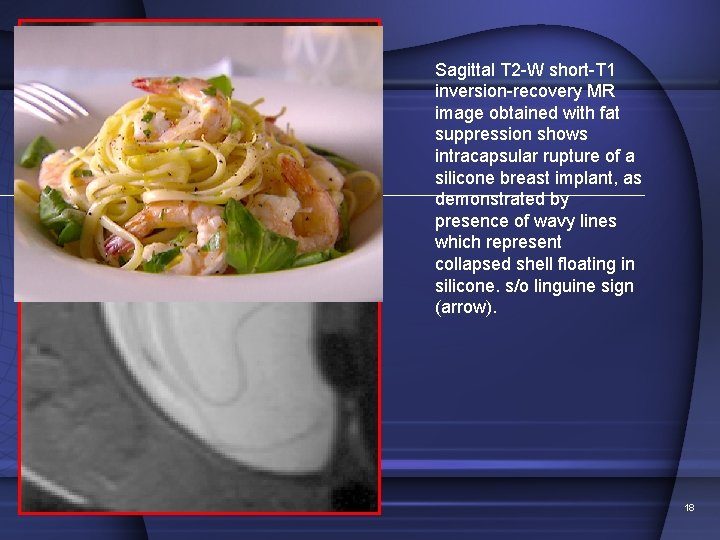
Sagital MR images demonstrate bilateral subpectoral silicon breast implants, with rupture of both implant membranes ( "linguini sign"). A "water-droplet" sign is also seen on a couple of images. Silicon is contained within the fibrous capsule, consistent with intracapsular rupture. 19 No free silicon is identified within the breast tissue
MRI --- keyhole sign, noose sign, inverted teardrop sign • Trapping of small amount of silicone gel within a radial fold • Silicone on both sides of the elastomer shell • Small intracapsular rupture or large gel bleed: cannot be differentiated!!! 20
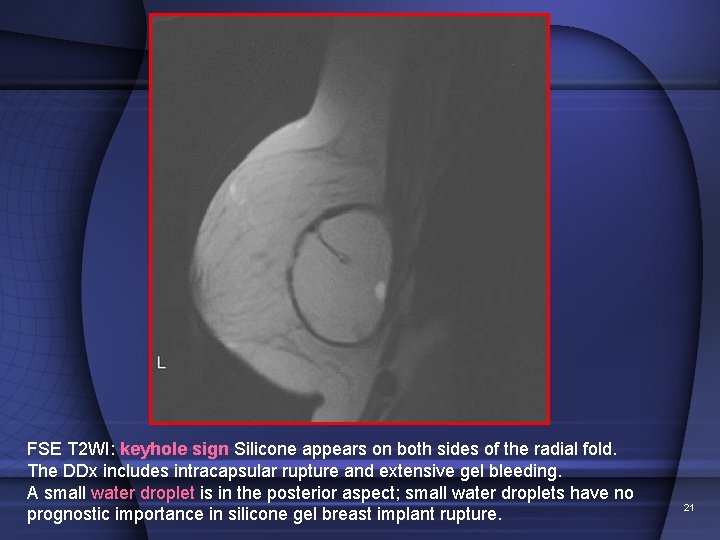
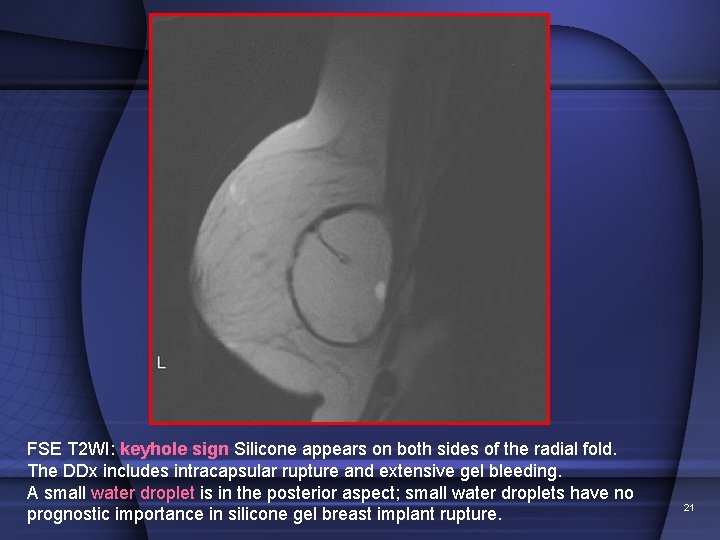
FSE T 2 WI: keyhole sign Silicone appears on both sides of the radial fold. The DDx includes intracapsular rupture and extensive gel bleeding. A small water droplet is in the posterior aspect; small water droplets have no prognostic importance in silicone gel breast implant rupture. 21
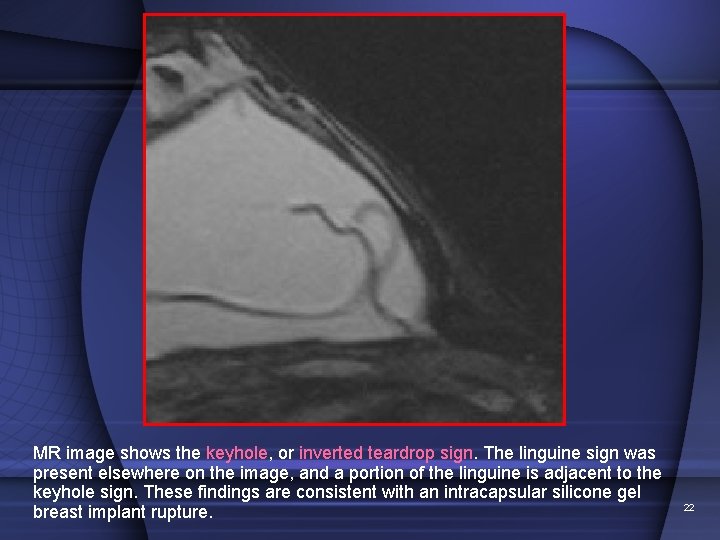
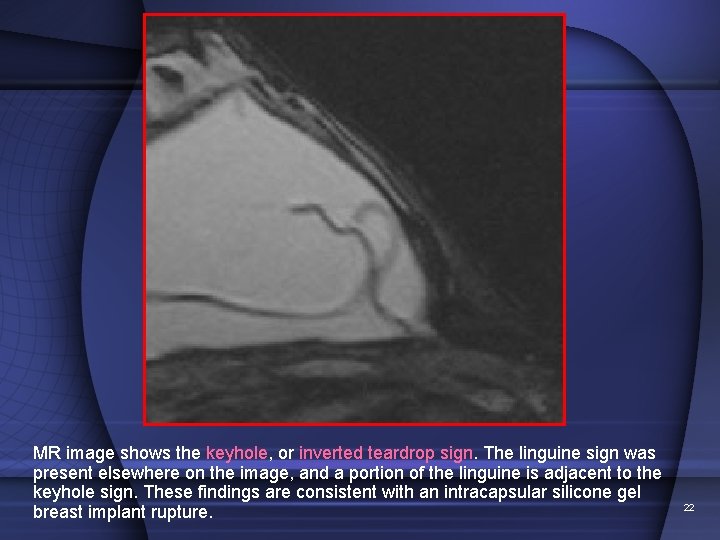
MR image shows the keyhole, or inverted teardrop sign. The linguine sign was present elsewhere on the image, and a portion of the linguine is adjacent to the keyhole sign. These findings are consistent with an intracapsular silicone gel breast implant rupture. 22
MRI --- extracapsular rupture Rupture of both elastomer shell (envelope) and fibrous capsule Silicone outside implant + linguine sign Best seen on silicone-only sequence: Bright silicone in dark tissue (Silicone outside implant) Dark lines in bright silicone (linguine sign) 23
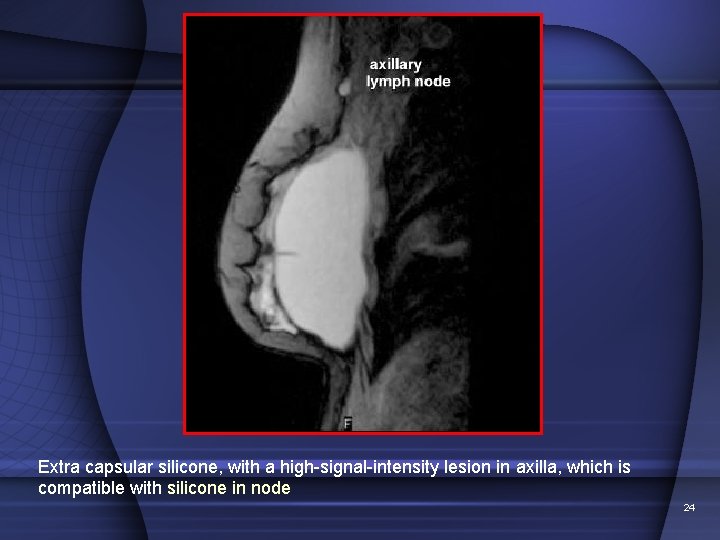
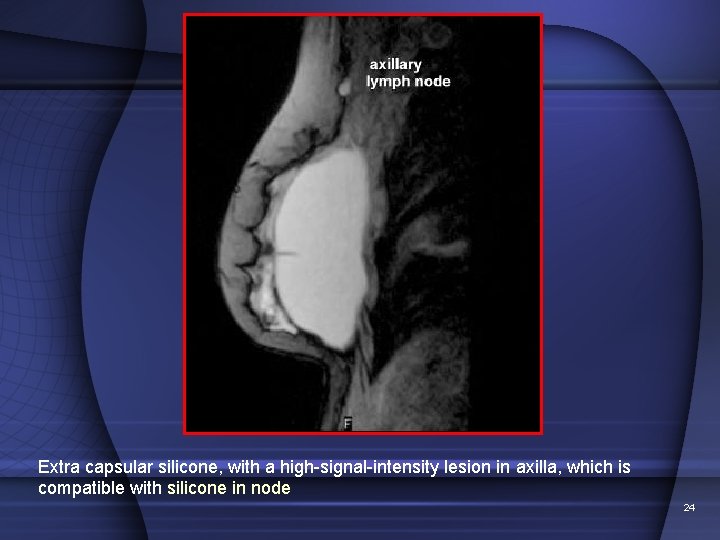
Extra capsular silicone, with a high-signal-intensity lesion in axilla, which is compatible with silicone in node 24
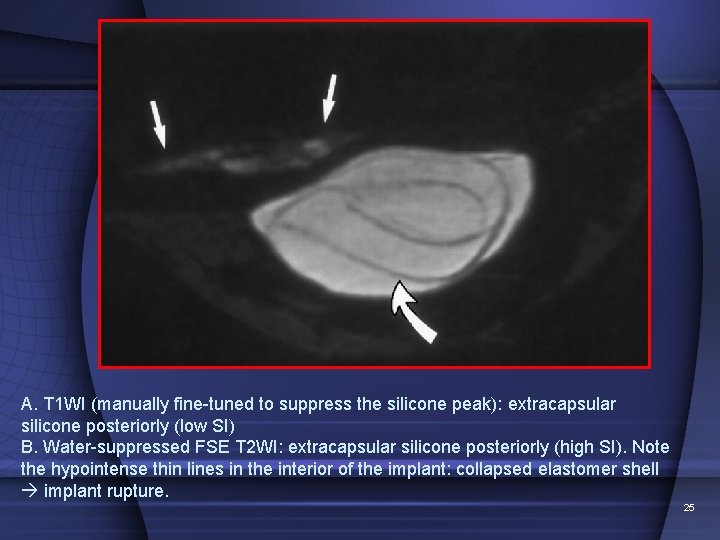
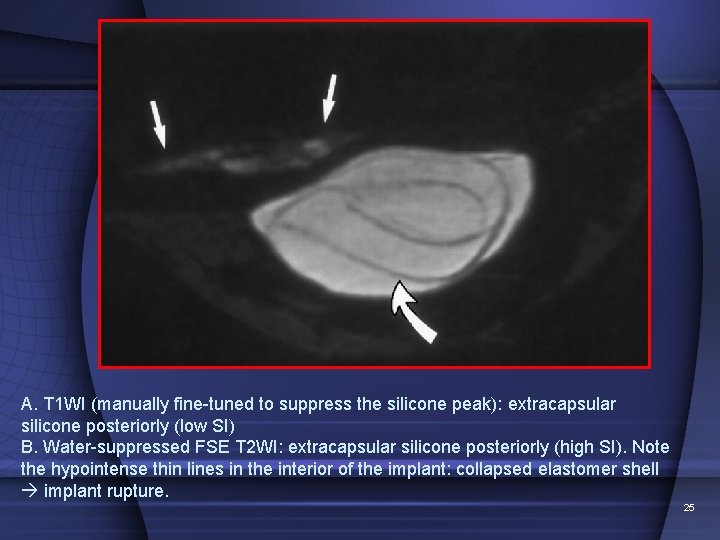
A. T 1 WI (manually fine-tuned to suppress the silicone peak): extracapsular silicone posteriorly (low SI) B. Water-suppressed FSE T 2 WI: extracapsular silicone posteriorly (high SI). Note the hypointense thin lines in the interior of the implant: collapsed elastomer shell implant rupture. 25
• Internal rupture of double-lumen implants Failure of the inner shell may be depicted as saline droplets that are floating in the silicone gel; this is considered a form of intracapsular rupture. – The presence of some saline droplets is a normal finding in single-lumen implants. • Capsular contracture – Asymmetric, serrated, focal folding of the fibrous capsule that changes the normal ovoid appearance of the implant may be present. (A transverse diameter of less than twice the anteroposterior depth corresponds well to clinically evident contracture) 26
• Management of ruptured SGBIs Involves explantation of prosthesis, with or without reconstruction. • Reasons for removal include the potential for silicone migration with subsequent inflammatory reaction; development of adverse local symptoms in pt, including pain, deformity, & granuloma formation. pts who have symptoms of connective tissue disease, fibromyalgia, or chronic fatigue syndrome is advocated as well. 27
• Screening for SGBI rupture in asymptomatic women remains controversial. • Some authors advocate mass screening with MRI, while others advocate prophylactic removal at or around 8 -10 years after implantation. • Still others advocate no removal unless pt is symptomatic & has imaging & clinical evidence of rupture. 28
Case 2 29
Six year-old female presents with 1. Two months of decreasing vision 2. Right eye-Squint 30
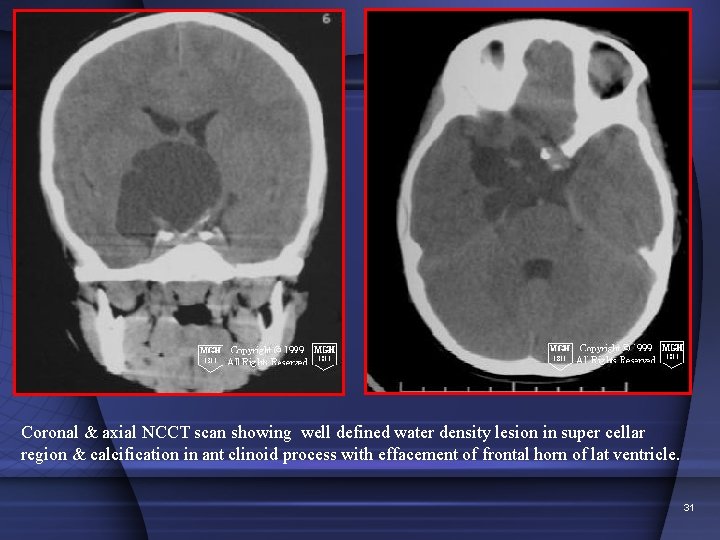
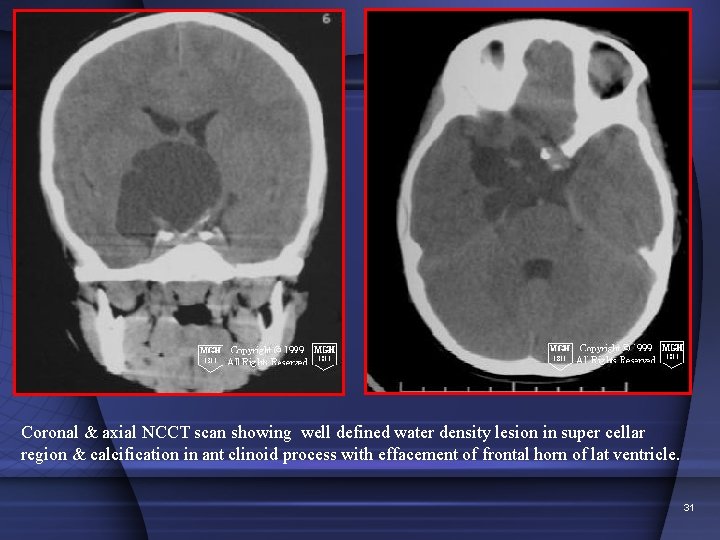
Coronal & axial NCCT scan showing well defined water density lesion in super cellar region & calcification in ant clinoid process with effacement of frontal horn of lat ventricle. 31
Differential Diagnosis - cystic suprasellar mass • • Craniopharyngioma Rathke cleft cyst Arachnoid cyst. Epidermoid. 32
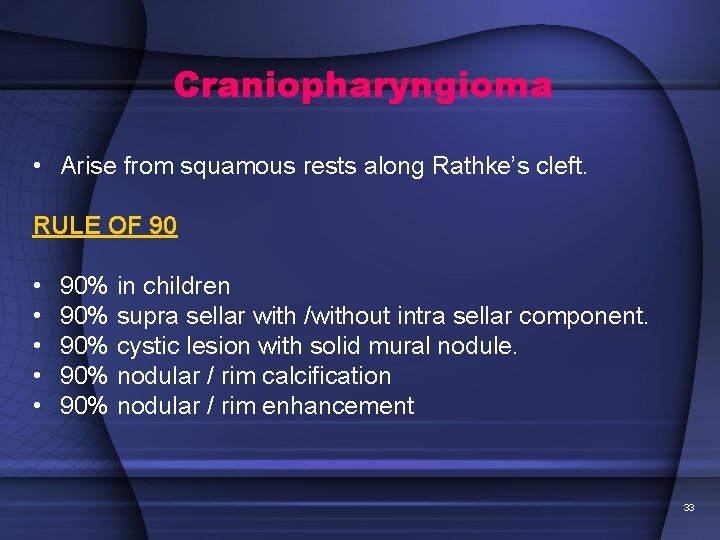
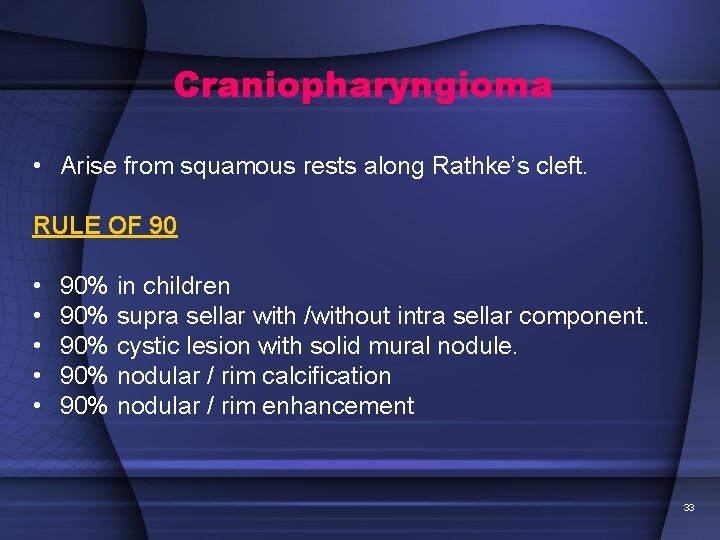
Craniopharyngioma • Arise from squamous rests along Rathke’s cleft. RULE OF 90 • • • 90% in children 90% supra sellar with /without intra sellar component. 90% cystic lesion with solid mural nodule. 90% nodular / rim calcification 90% nodular / rim enhancement 33
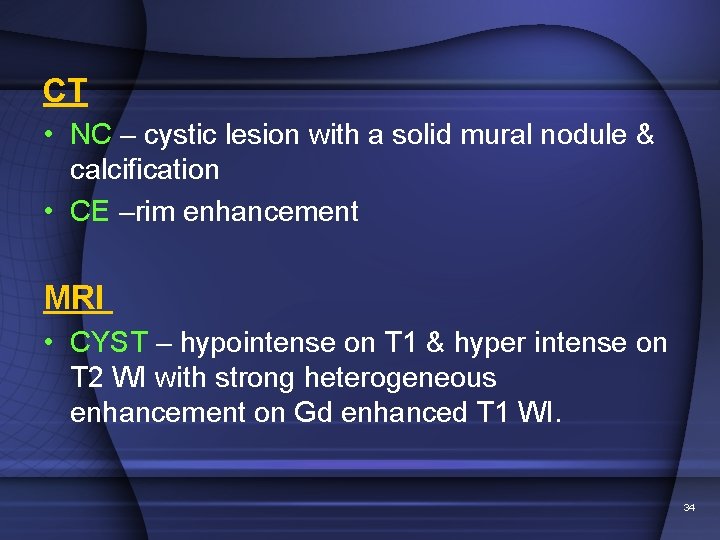
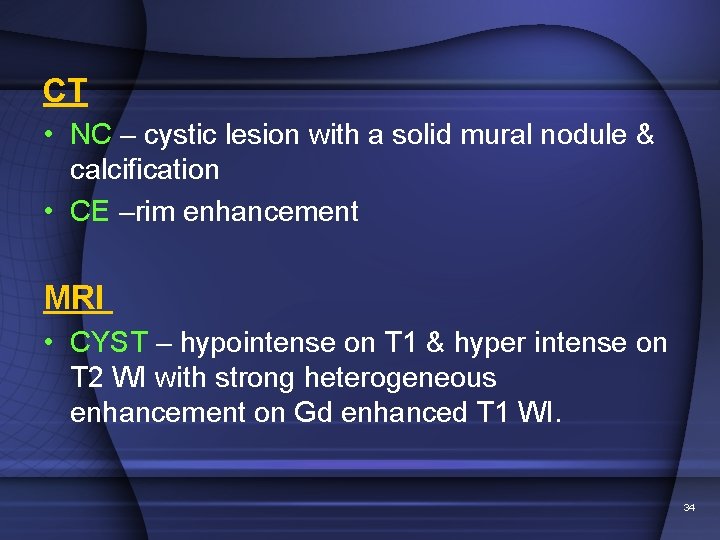
CT • NC – cystic lesion with a solid mural nodule & calcification • CE –rim enhancement MRI • CYST – hypointense on T 1 & hyper intense on T 2 WI with strong heterogeneous enhancement on Gd enhanced T 1 WI. 34
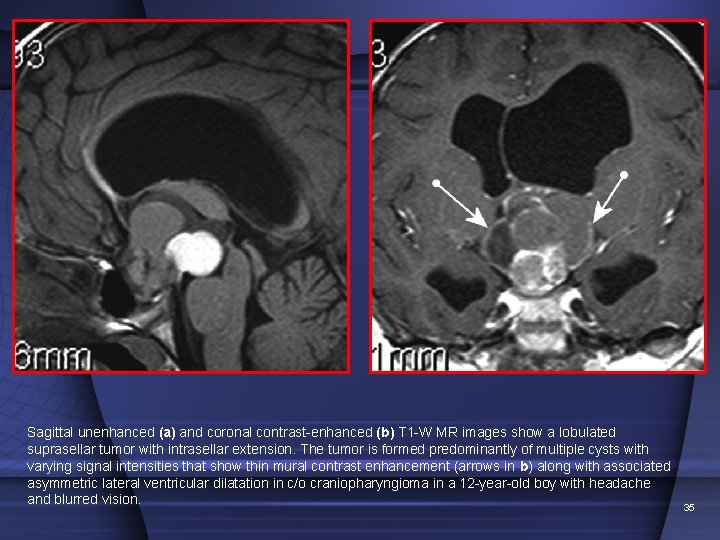
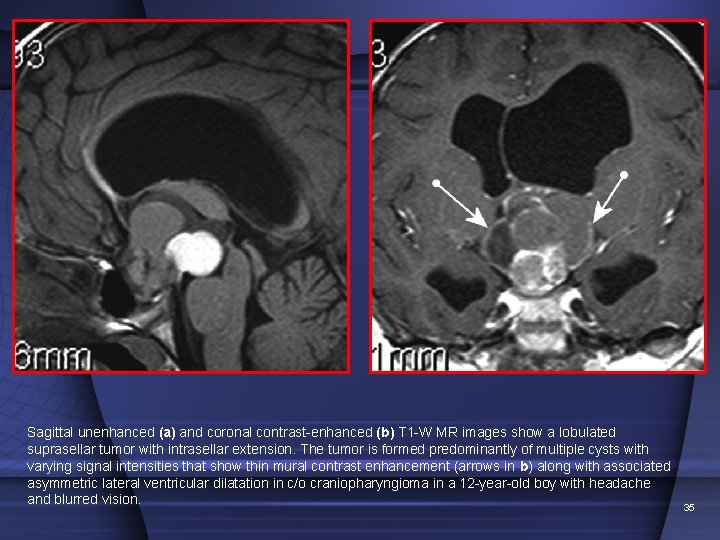
Sagittal unenhanced (a) and coronal contrast-enhanced (b) T 1 -W MR images show a lobulated suprasellar tumor with intrasellar extension. The tumor is formed predominantly of multiple cysts with varying signal intensities that show thin mural contrast enhancement (arrows in b) along with associated asymmetric lateral ventricular dilatation in c/o craniopharyngioma in a 12 -year-old boy with headache and blurred vision. 35
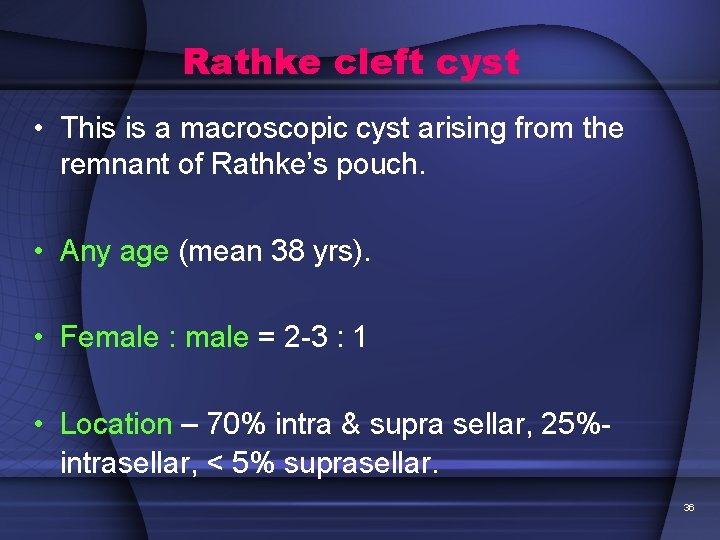
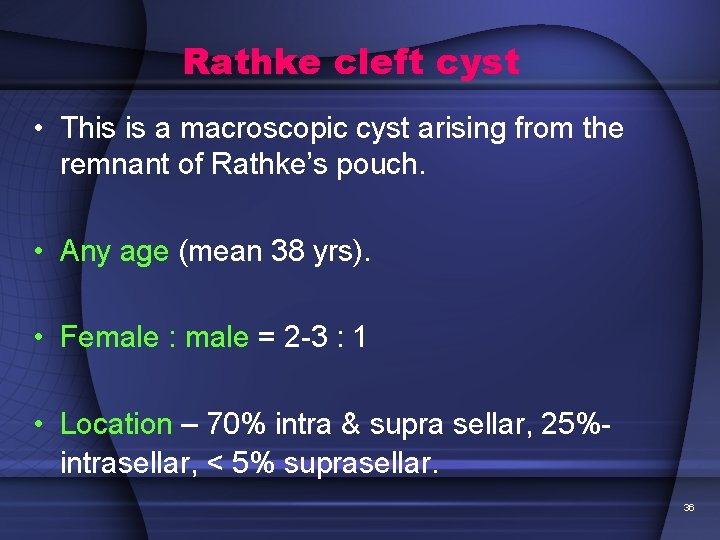
Rathke cleft cyst • This is a macroscopic cyst arising from the remnant of Rathke’s pouch. • Any age (mean 38 yrs). • Female : male = 2 -3 : 1 • Location – 70% intra & supra sellar, 25%- intrasellar, < 5% suprasellar. 36
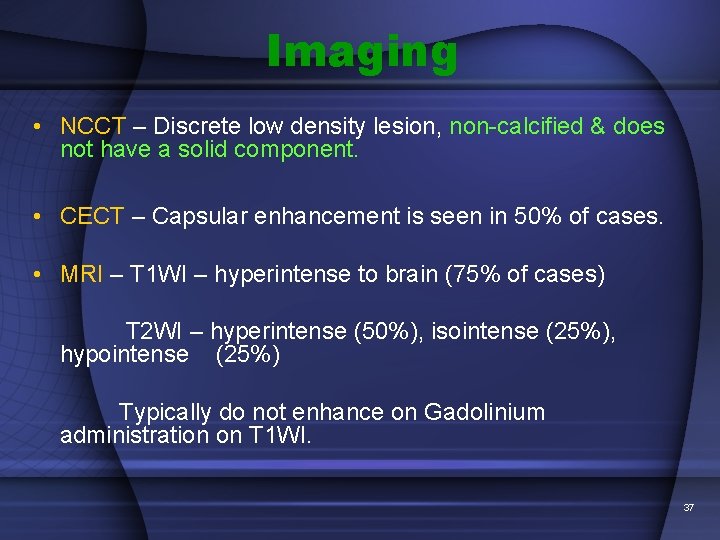
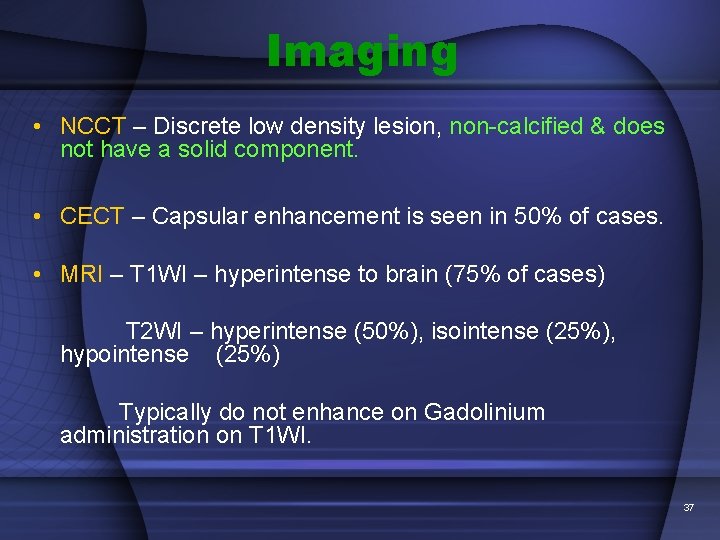
Imaging • NCCT – Discrete low density lesion, non-calcified & does not have a solid component. • CECT – Capsular enhancement is seen in 50% of cases. • MRI – T 1 WI – hyperintense to brain (75% of cases) T 2 WI – hyperintense (50%), isointense (25%), hypointense (25%) Typically do not enhance on Gadolinium administration on T 1 WI. 37
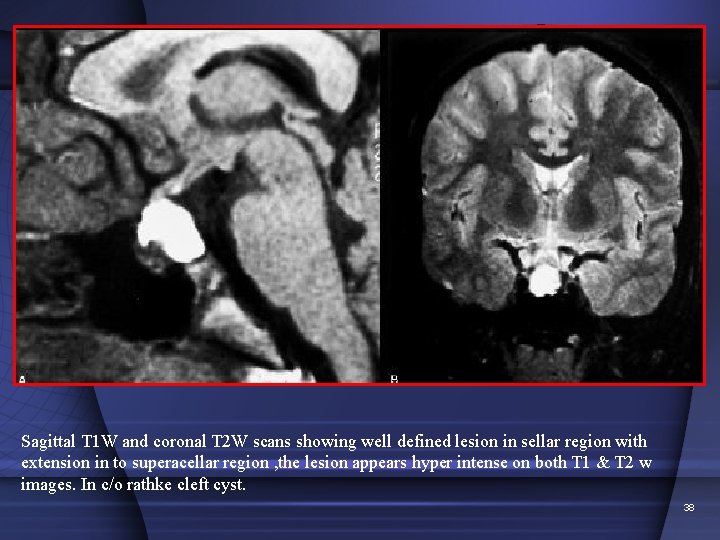
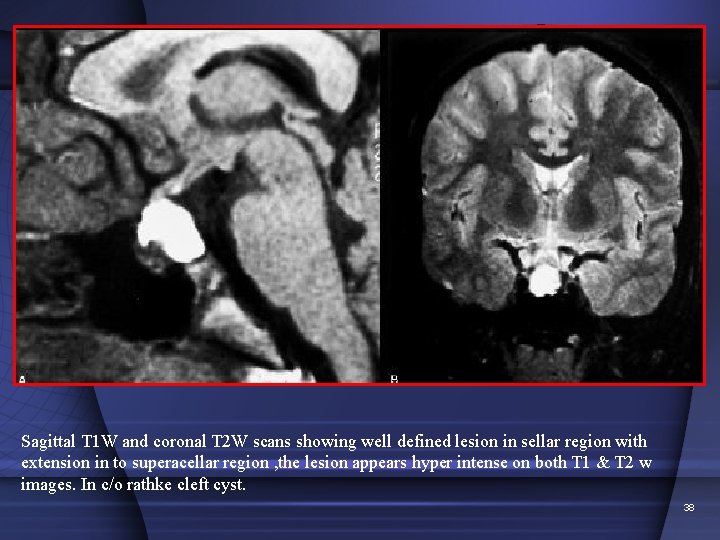
Sagittal T 1 W and coronal T 2 W scans showing well defined lesion in sellar region with extension in to superacellar region , the lesion appears hyper intense on both T 1 & T 2 w images. In c/o rathke cleft cyst. 38
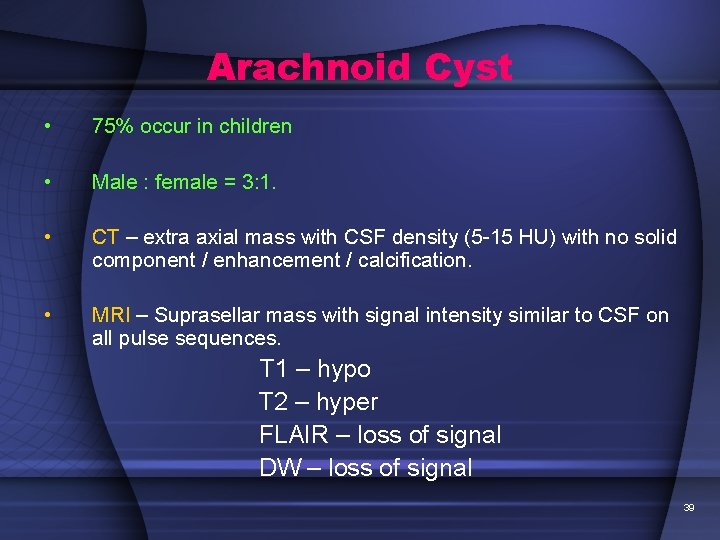
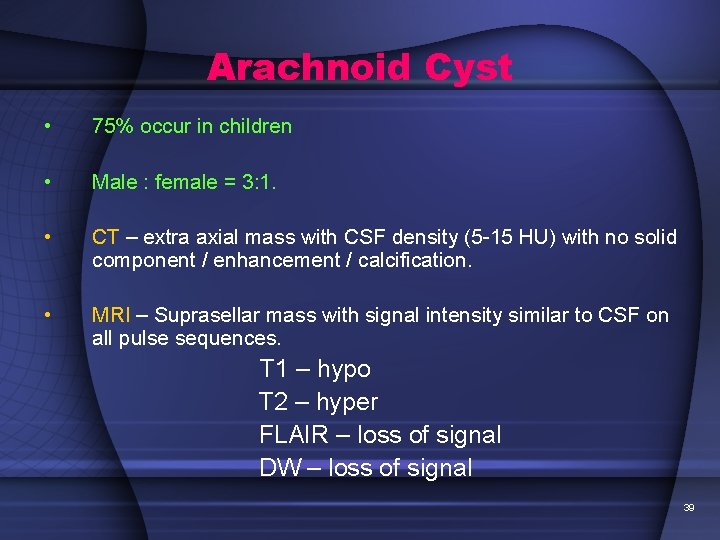
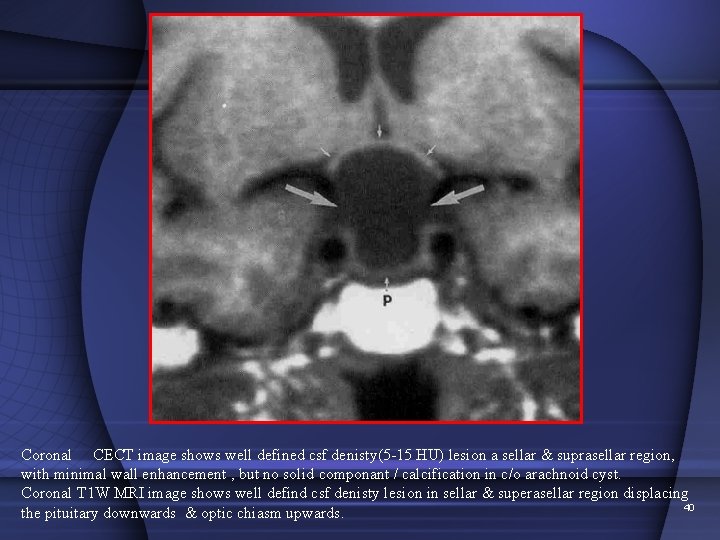
Arachnoid Cyst • 75% occur in children • Male : female = 3: 1. • CT – extra axial mass with CSF density (5 -15 HU) with no solid component / enhancement / calcification. • MRI – Suprasellar mass with signal intensity similar to CSF on all pulse sequences. T 1 – hypo T 2 – hyper FLAIR – loss of signal DW – loss of signal 39
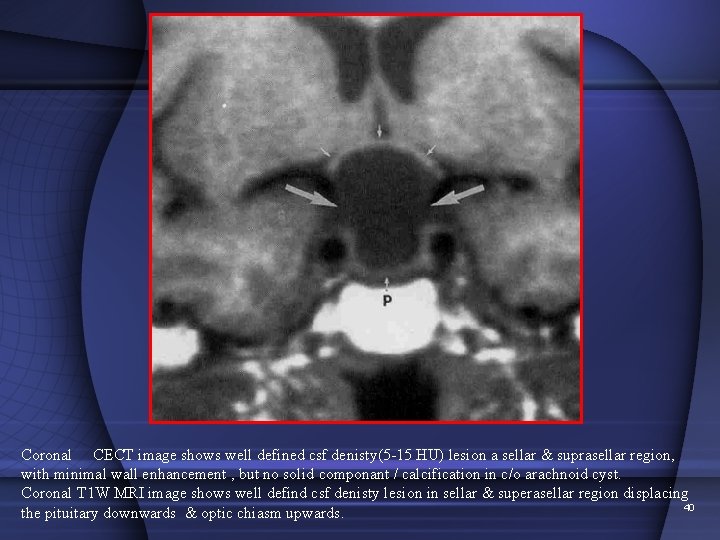
Coronal CECT image shows well defined csf denisty(5 -15 HU) lesion a sellar & suprasellar region, with minimal wall enhancement , but no solid componant / calcification in c/o arachnoid cyst. Coronal T 1 W MRI image shows well defind csf denisty lesion in sellar & superasellar region displacing 40 the pituitary downwards & optic chiasm upwards.
Epidermoid tumor • Developmental epithelial inclusion cyst • Majority are intradural (basal CSF spaces) • 40 -50% CP angle cistern, 7% each in supra and para sellar regions. • Epidermoids are confined to & insinuate along basilar CSF cisterns. They typically encase & engulf arteries & cranial nerves. 41
Imaging • SI similar to CSF • T 1 – hypo SI • T 2 – hyper SI • FLAIR –Marked loss of SI noted. • Occasionally, Epidermoid may not show loss of SI on FLAIR because of high protein content. 42
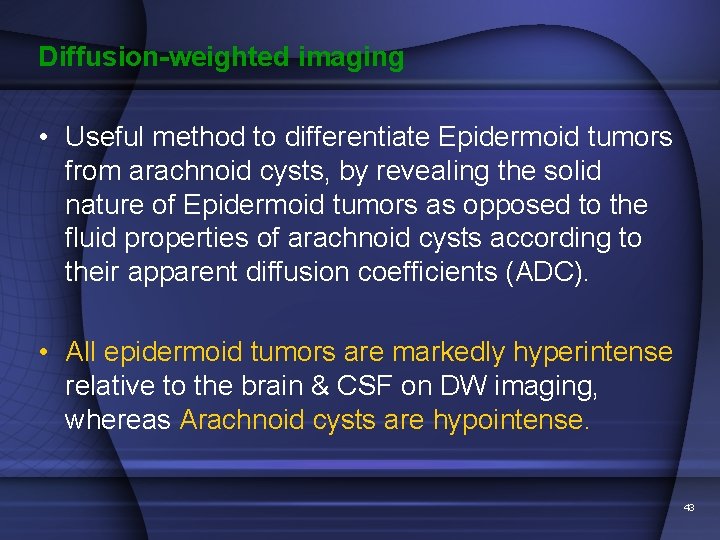
Diffusion-weighted imaging • Useful method to differentiate Epidermoid tumors from arachnoid cysts, by revealing the solid nature of Epidermoid tumors as opposed to the fluid properties of arachnoid cysts according to their apparent diffusion coefficients (ADC). • All epidermoid tumors are markedly hyperintense relative to the brain & CSF on DW imaging, whereas Arachnoid cysts are hypointense. 43
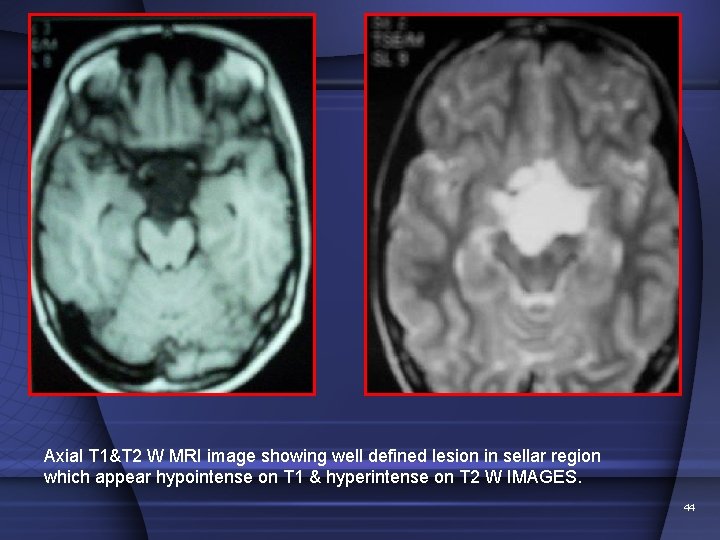
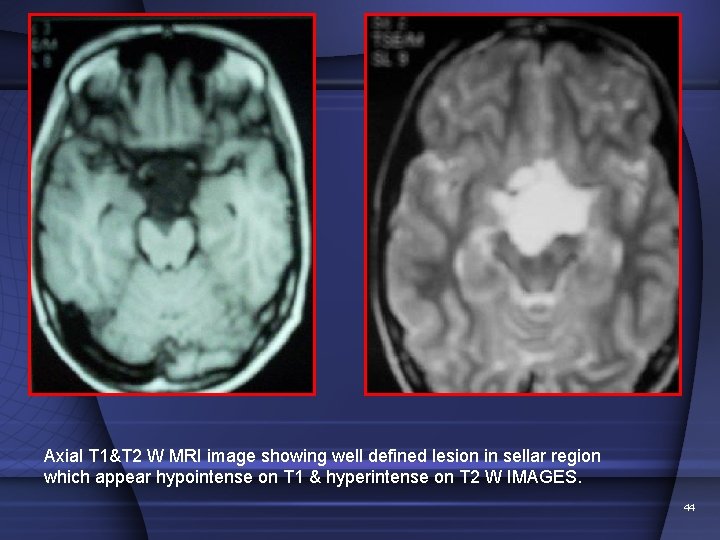
Axial T 1&T 2 W MRI image showing well defined lesion in sellar region which appear hypointense on T 1 & hyperintense on T 2 W IMAGES. 44
The lesion shows high signal intensity on DWI. In c/o epidermoid. 45
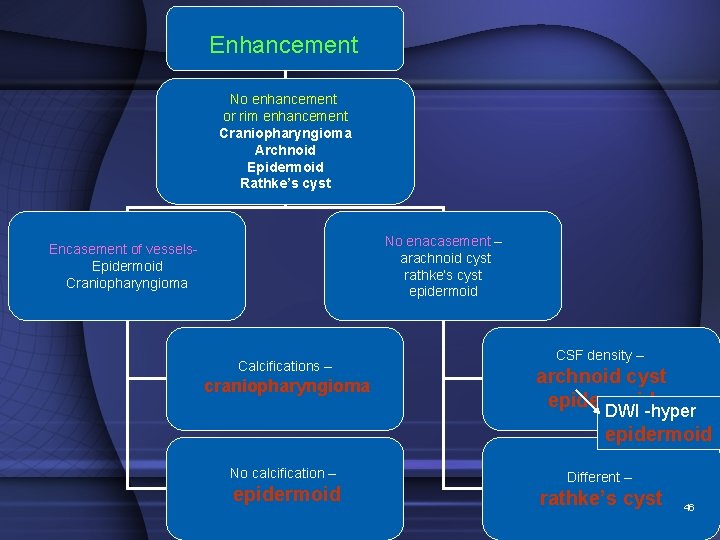
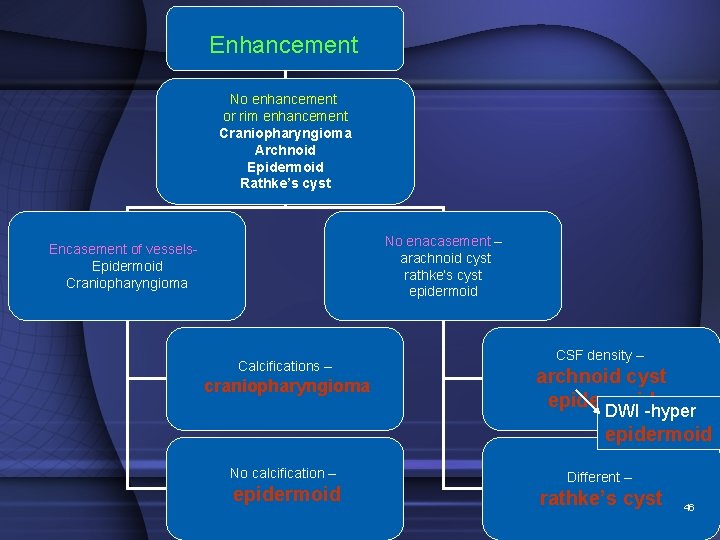
Enhancement No enhancement or rim enhancement Craniopharyngioma Archnoid Epidermoid Rathke’s cyst No enacasement – arachnoid cyst rathke’s cyst epidermoid Encasement of vessels- Epidermoid Craniopharyngioma Calcifications – craniopharyngioma CSF density – archnoid cyst epidermoid DWI -hyper epidermoid No calcification – epidermoid Different – rathke’s cyst 46
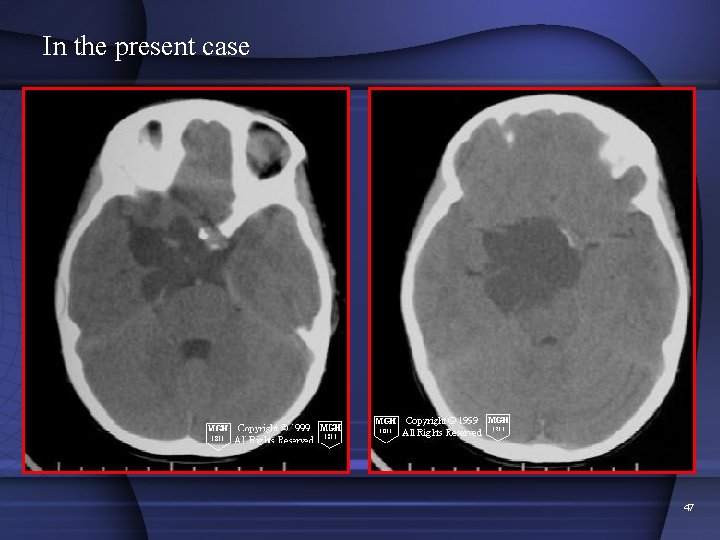
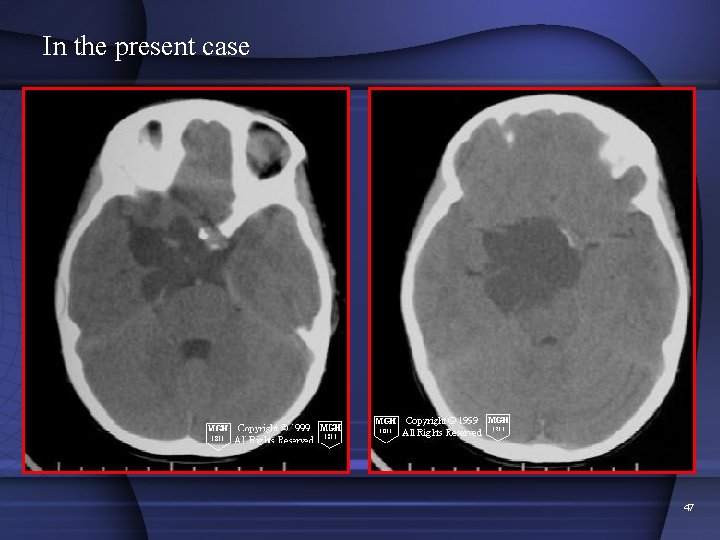
In the present case 47
Diagnosis Craniopharyngioma 48
Discussion • Accounts for 50% of all suprasellar tumors in children. • Most common nonglial brain tumor in children. • It is predominantly a pediatric tumor, although it is also seen in adults about 25% of the time. • Arise from squamous epithelial rests along the involuted craniopharyngial duct. 49
• It is a histologically benign, extra-axial, slow-growing tumor that predominately involves sella & suprasellar space. • Despite its histologic appearance, it occasionally behave like malignant tumors & can metastasize. • Recurrence, both local & along surgical tracts & meningeal seeding have been reported. 50
• Sex: male/female : equal. • Age: A bimodal age distribution 1. First peak - childhood & early adolescence predominately at age 5 -10 years. 2. The second peak (for papillary types) - 40 -60 years. 51
• 1. 2. 3. 3 distinct histologic subtypes: Adamantinomatous Papillary Mixed. • The tumors occur in suprasellar (75%), suprasellar and intrasellar (21%), or entirely intrasellar (4%) locations. 52
Clinical presentation • Asymptomatic to endocrine, visual, or psychological disorders. • The most common presenting symptoms are headache, nausea, vomiting, and visual disturbances. • The most common visual disturbances are bitemporal hemianopsia and homonomous hemianopsia. • Hydrocephalus may result from a tumor that obstructs the third ventricle. 53
IMAGING • The best imaging tool is MRI without and with contrast enhancement. • CT can clearly demonstrate the characteristic calcifications and size of the tumor, while MRI demonstrates the size and extent of the tumor. • MRI results can confirm cystic features of the tumor. Sequences such as FLAIR, gradient-echo (GRE), diffusion-weighted imaging, as well as MR spectroscopy, can be used to make a confident and correct diagnosis. 54
CT • On CT, the adamantinomatous-type tumor appears as a predominately cystic mass with a solid component (>90%). The solid component appears isoattenuating and usually contains calcifications (>80%). • The sella may be expansile, and hydrocephalus may be present. • Papillary type is usually solid, isoattenuating, and rarely calcified. • On contrast-enhanced CT, greater than 90% have some component of nodular rim enhancement. 55
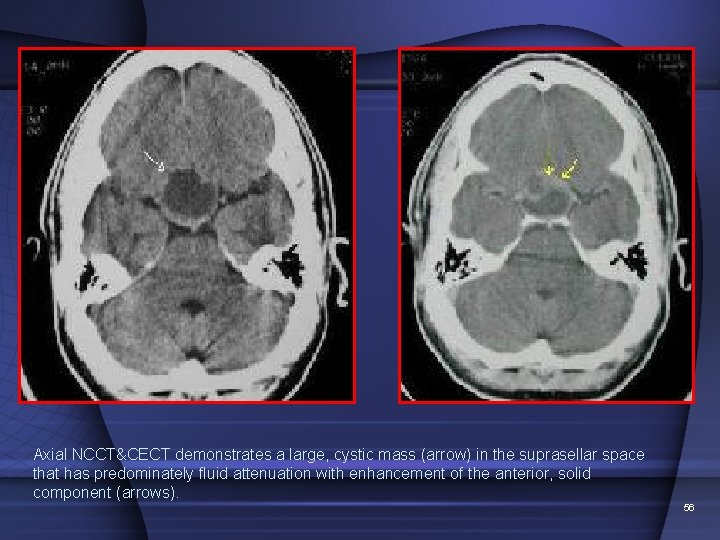
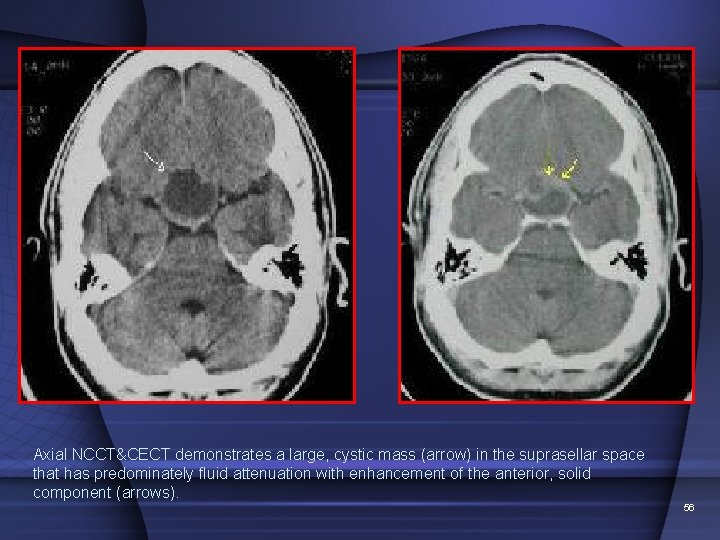
Axial NCCT&CECT demonstrates a large, cystic mass (arrow) in the suprasellar space that has predominately fluid attenuation with enhancement of the anterior, solid component (arrows). 56
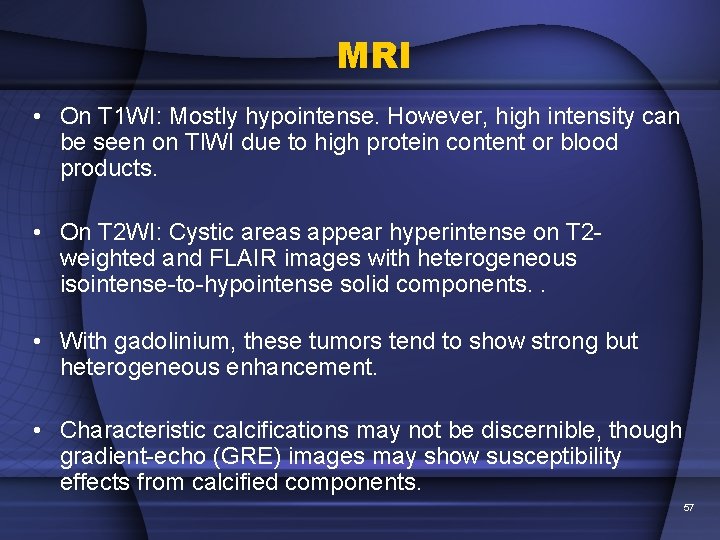
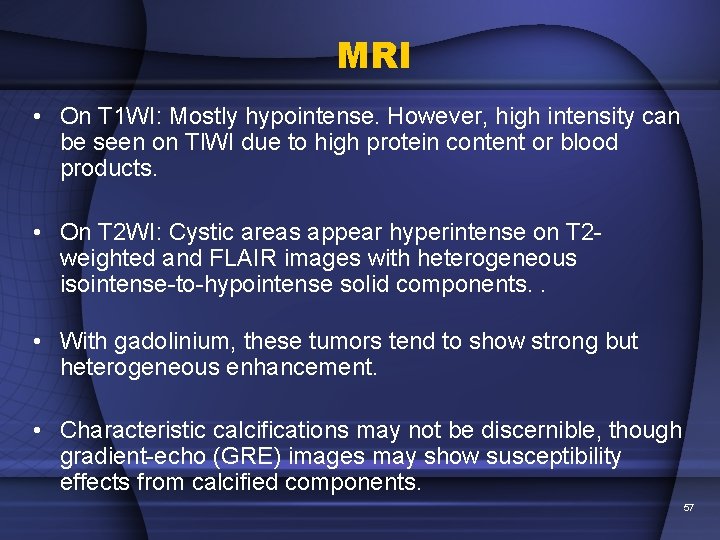
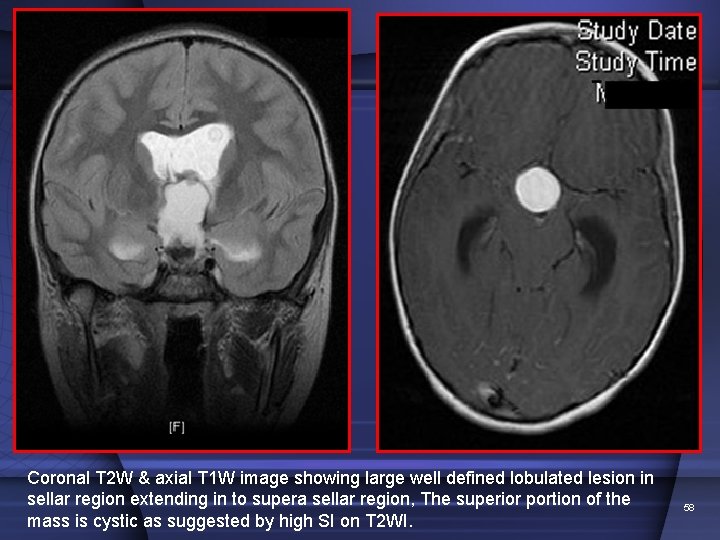
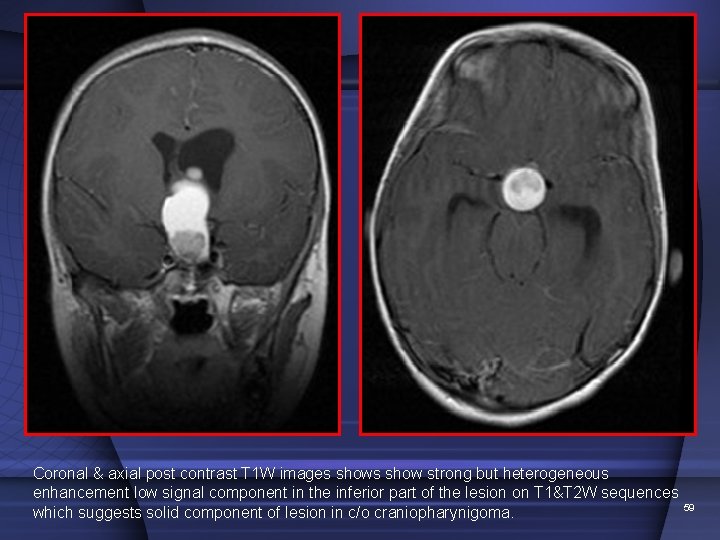
MRI • On T 1 WI: Mostly hypointense. However, high intensity can be seen on Tl. WI due to high protein content or blood products. • On T 2 WI: Cystic areas appear hyperintense on T 2 weighted and FLAIR images with heterogeneous isointense-to-hypointense solid components. . • With gadolinium, these tumors tend to show strong but heterogeneous enhancement. • Characteristic calcifications may not be discernible, though gradient-echo (GRE) images may show susceptibility effects from calcified components. 57
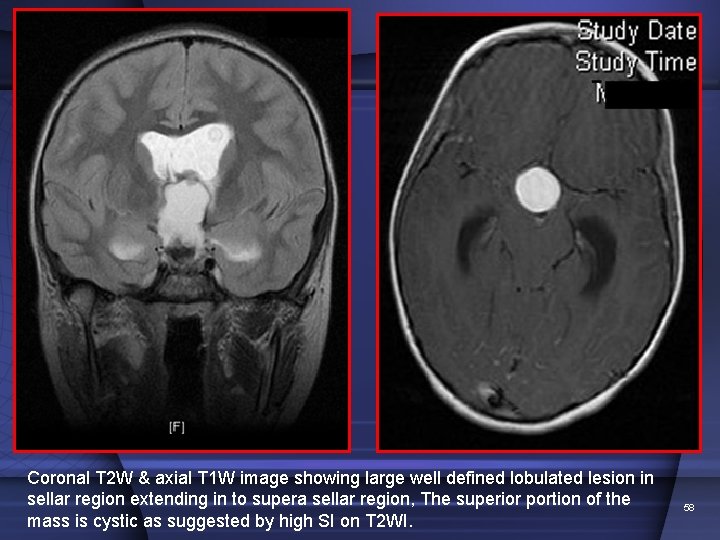
Coronal T 2 W & axial T 1 W image showing large well defined lobulated lesion in sellar region extending in to supera sellar region, The superior portion of the mass is cystic as suggested by high SI on T 2 WI. 58
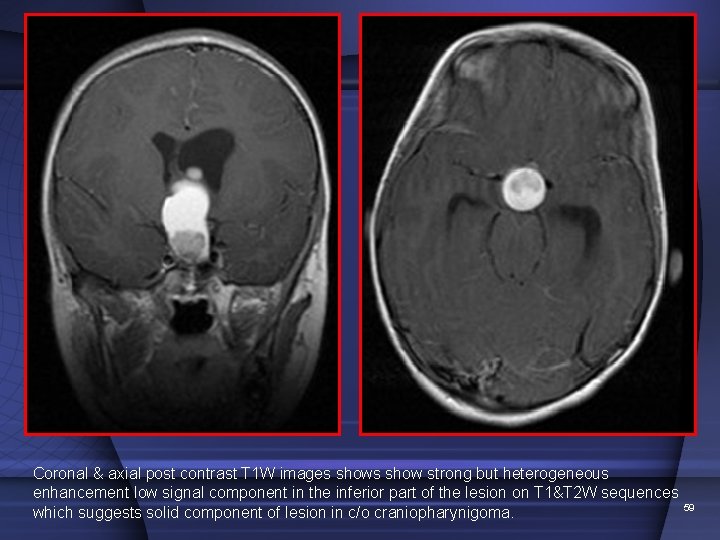
Coronal & axial post contrast T 1 W images show strong but heterogeneous enhancement low signal component in the inferior part of the lesion on T 1&T 2 W sequences 59 which suggests solid component of lesion in c/o craniopharynigoma.
Radiologic sign The Fat C 2 Sign 60
APPEARANCE The so-called "fat" C 2 sign refers to an apparent increase in distance between ant & post margins of C 2 vertebra when compared with distance between two margins of C 3 vertebra on a lateral conventional radiograph of cervical spine in setting of trauma. 61
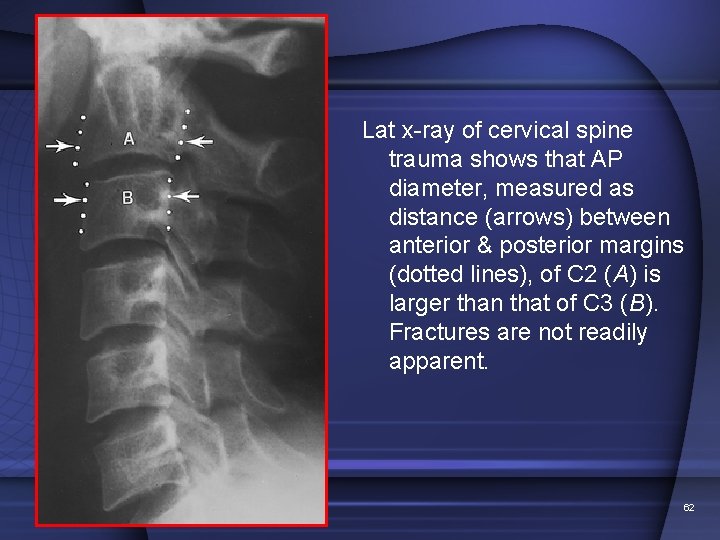
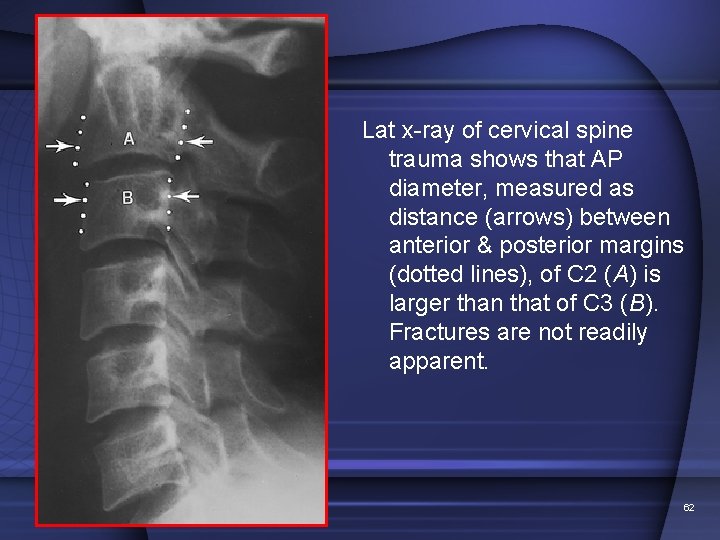
Lat x-ray of cervical spine trauma shows that AP diameter, measured as distance (arrows) between anterior & posterior margins (dotted lines), of C 2 (A) is larger than that of C 3 (B). Fractures are not readily apparent. 62
EXPLANATION • A fat C 2 sign results from an obliquely oriented fracture, involving body of C 2, that causes displacement of either one or both of ant & post margins & creates an increased AP distance between the two surfaces. • The degree of obliquity of fracture plane with respect to coronal plane will determine whether actual fracture will be visualized on the lateral radiograph. 63
• injury may occur due to hyperflexion or hyperextension forces. • The identification of a fat C 2 sign implies that a potentially unstable fracture with fragment displacement is present & that further imaging evaluation is needed. 64
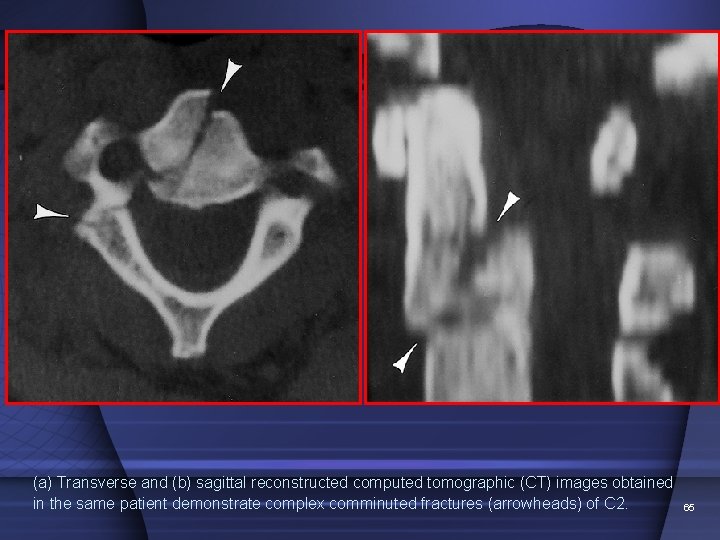
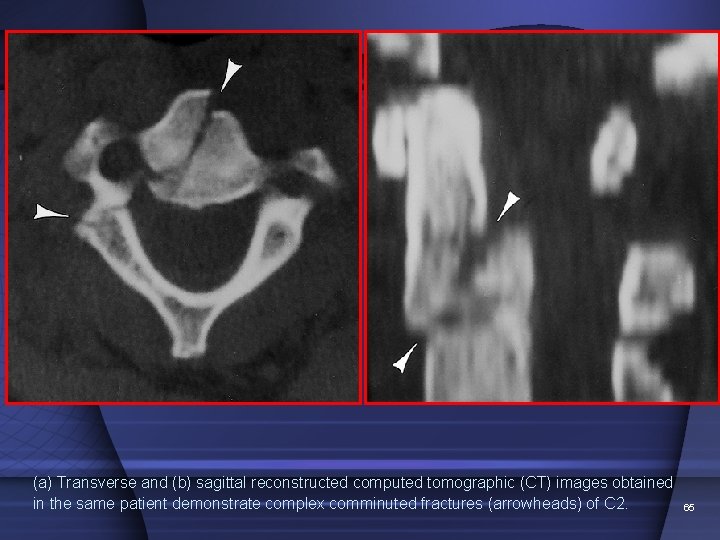
(a) Transverse and (b) sagittal reconstructed computed tomographic (CT) images obtained in the same patient demonstrate complex comminuted fractures (arrowheads) of C 2. 65
DISCUSSION • The fat C 2 sign is indicative of a fracture that involves the body of C 2. • It results from one of several types of injuries: 1. a complex vertical fracture of the body of the C 2 , 2. a low (type III) dens fracture , or 3. an atypical traumatic spondylolisthesis. • Complex vertical fractures of the body of C 2 result from a combination of applied forces. • often obscured on conventional radiographs because the combined forces produce an oblique fracture that is not tangential to the x-ray beam. 66
• However, the fracture fragments may be displaced by applied forces and result in the interruption of the anterior or posterior margins or both, with apparent enlargement of the body of C 2 on the lateral radiograph. • This creates the fat C 2 sign. • Primary hyperflexion injuries predominantly disrupt the anterior margin. • If the posterior margin is disrupted, a primary hyperextension injury is suggested. • Combined hyperextension-hyperflexion injuries may result in the interruption of both margins. 67
• A low (type III) dens fracture may result from any combination of hyperflexion, hyperextension, and lateral bending mechanisms. • It is actually a horizontal or oblique fracture of the body of C 2, just inferior to the dens. • It is considered unstable because it separates the upper portion of C 2, the dens, the C 1 vertebra, and the occiput from the remainder of the cervical spine. • often isolated injuries but are sometimes as/d with mandibular fractures , extension teardrop fractures, Jefferson fractures, or atlanto-occipital dislocations. 68
• CLASSIFICATION of traumatic spondylolisthesis (bilateral fractures through the neural arch of C 2) and correlation with mech of injury – • hyperextension-vertical loading (type I), • hyperextension-vertical loading f/d by flexion and compression (type II), • flexion and distraction (type IIa), • flexion and compression (type III). 69
• an atypical traumatic spondylolisthesis in which the vertical component of the fracture line in a type I or type II injury passes through the posterior cortex of the vertebral body. • In this variant, there is disruption of the posterior cortex of C 2 and the AP diameter of C 2 is subsequently widened. • greater tendency for mechanical instability, canal compromise, and neurologic sequelae than do the pure type I or type II injuries. 70
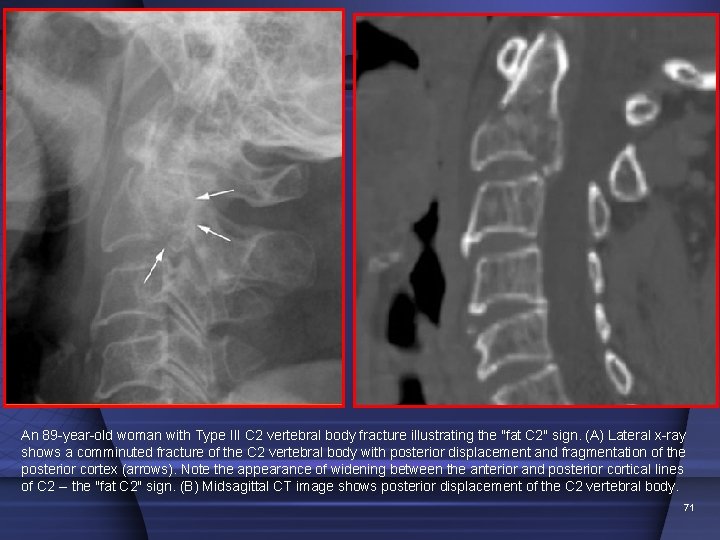
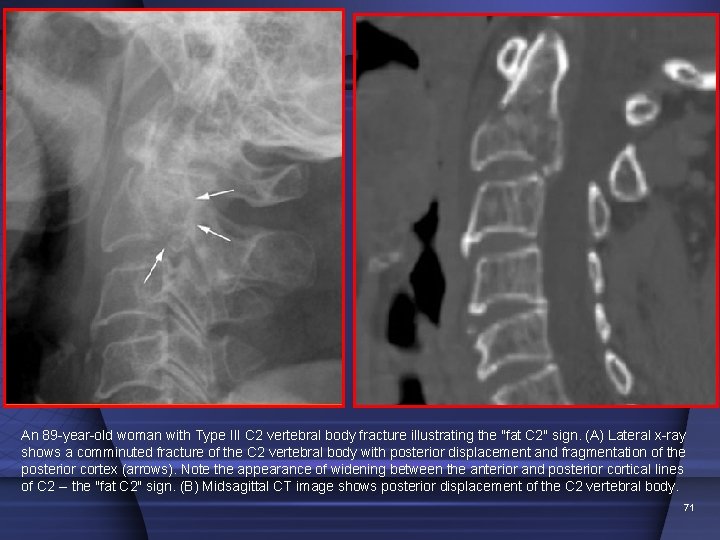
An 89 -year-old woman with Type III C 2 vertebral body fracture illustrating the "fat C 2" sign. (A) Lateral x-ray shows a comminuted fracture of the C 2 vertebral body with posterior displacement and fragmentation of the posterior cortex (arrows). Note the appearance of widening between the anterior and posterior cortical lines of C 2 -- the "fat C 2" sign. (B) Midsagittal CT image shows posterior displacement of the C 2 vertebral body. 71
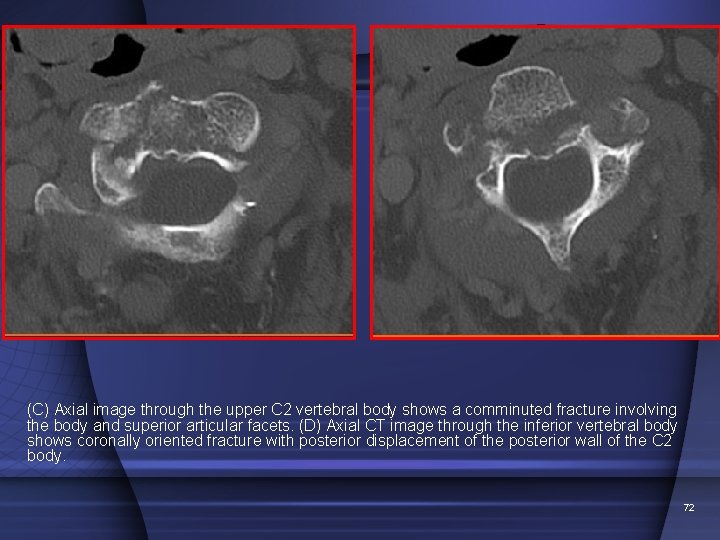
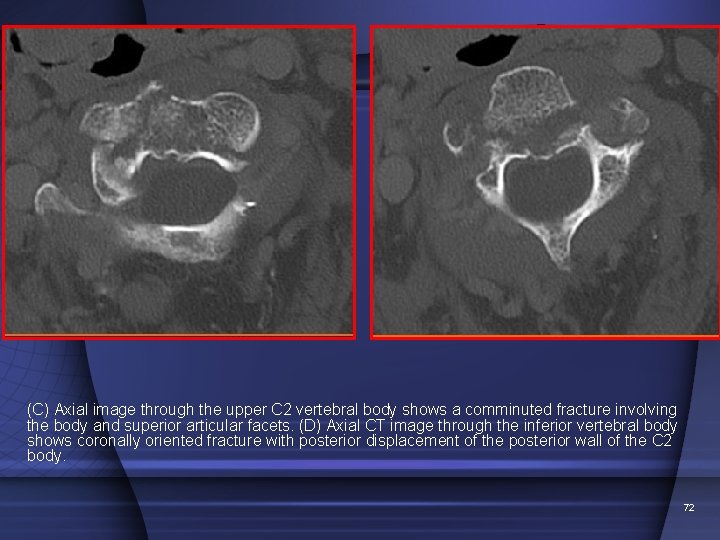
(C) Axial image through the upper C 2 vertebral body shows a comminuted fracture involving the body and superior articular facets. (D) Axial CT image through the inferior vertebral body shows coronally oriented fracture with posterior displacement of the posterior wall of the C 2 body. 72
73

74
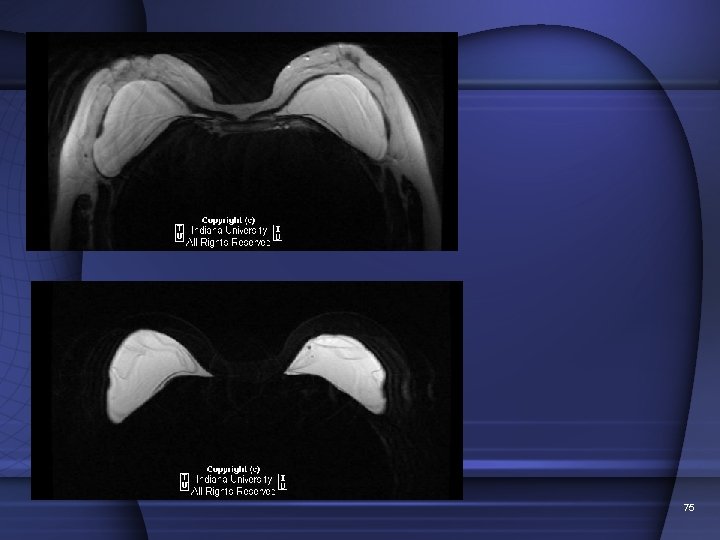
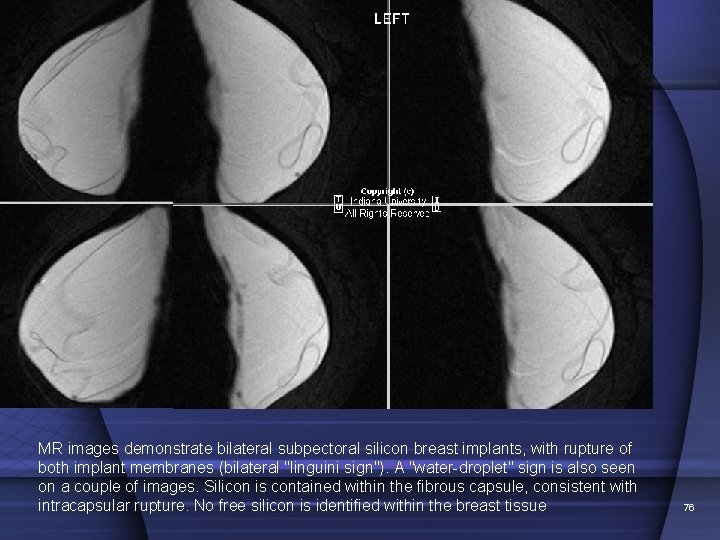
75
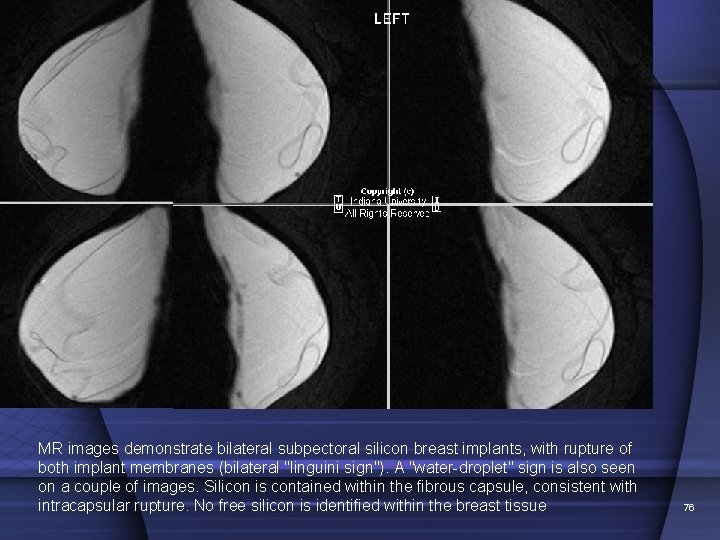
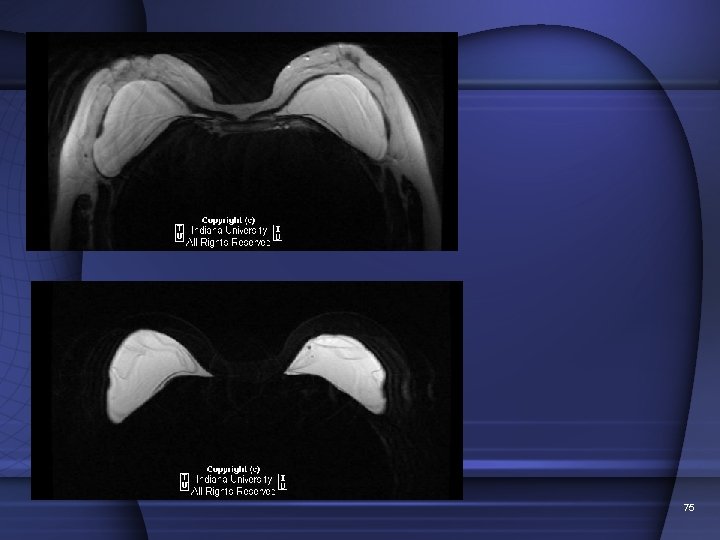
MR images demonstrate bilateral subpectoral silicon breast implants, with rupture of both implant membranes (bilateral "linguini sign"). A "water-droplet" sign is also seen on a couple of images. Silicon is contained within the fibrous capsule, consistent with intracapsular rupture. No free silicon is identified within the breast tissue 76
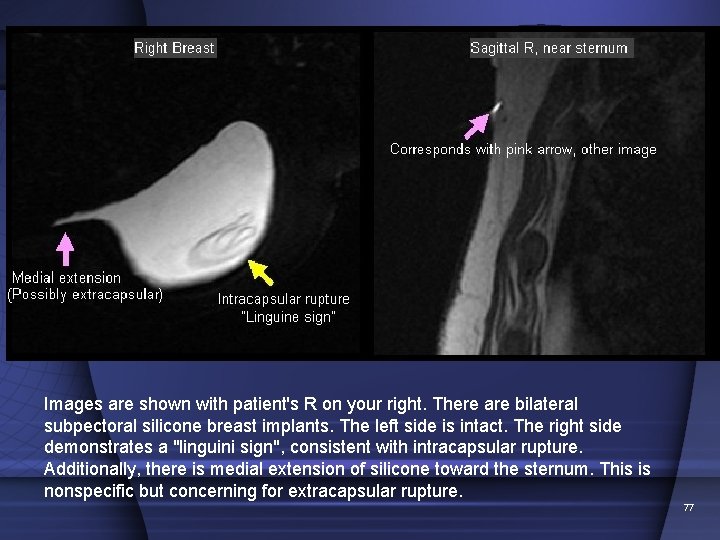
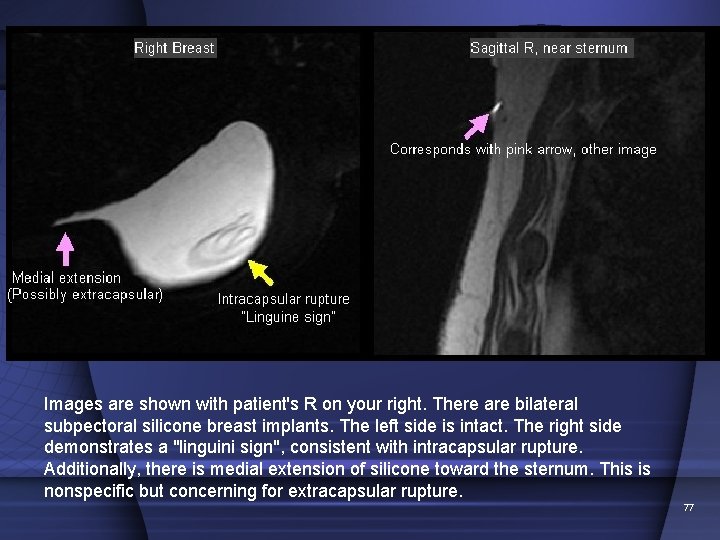
Images are shown with patient's R on your right. There are bilateral subpectoral silicone breast implants. The left side is intact. The right side demonstrates a "linguini sign", consistent with intracapsular rupture. Additionally, there is medial extension of silicone toward the sternum. This is nonspecific but concerning for extracapsular rupture. 77