Casemix Funding James Downie A Project Director National






- Slides: 21
Casemix Funding James Downie A/ Project Director, National Reform Projects
National Health Reforms National Health Reform i) 2008 NPA – “National ABF System” ii) 2010 COAG – “Dominant Funder” iii) 2011 COAG – “Transparency, Transparency and Transparency” But 1 common theme – National ABF, National Efficient Price, based on nationally consistent costing. ABF starts 1 July 2012

National Reform Agreement From 2014, the Commonwealth will contribute 45% of “efficient growth” funding. From 2016, this increases to 50%. Overtime, the Commonwealth’s share of funding may increase. There is a guarantee of a minimum $16. 4 B in additional Commonwealth funding by 2020.

ABF Proposal 2008 NPA recognises differing degrees of development of various workstreams. Admitted Acute was completed in June 2010. Outpatients, ED, Sub Acute and Mental Health was scheduled for June 30 2012. 2010 and 2011 Agreements propose “proxy” classifications for the underdeveloped areas.
What is ABF? ? A method of allocating funds Based on activity or outputs Funding based on agreed volume & price Funding that provides equity, transparency & accountability A platform for driving technical efficiency
So what is this ABF thing… The Australian Feb 26 2011

Casemix: Misconceptions vs Actual Case
But is it perfect? ? NO! Not everything can be output funded – very high cost, statewide services, specialist hospitals Measures and rewards outputs – no measure of outcomes Potential for perverse incentives
General Principles Every Patient Type Identified (acute, sub acute, mental health) Every Patient Classified (eg DRG B 77 Z – Headache) Patients Costed Cost weights and prices calculated
Limitations of a basic casemix model One cost weight applied to each and every patient in a DRG Not every patient in a DRG needs exactly the same level of care Creates financial risk to providers & purchasers of health care

Cost versus time in hospital Patient Cost versus Time in Hospital Total Cost $ Days in Hospital
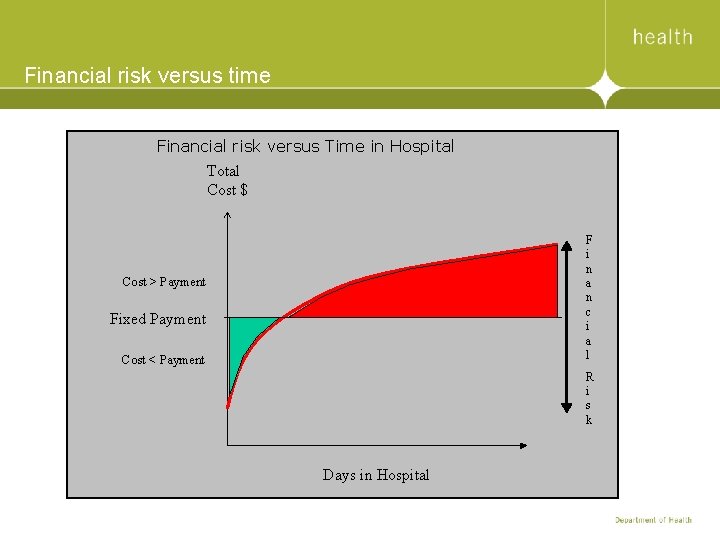
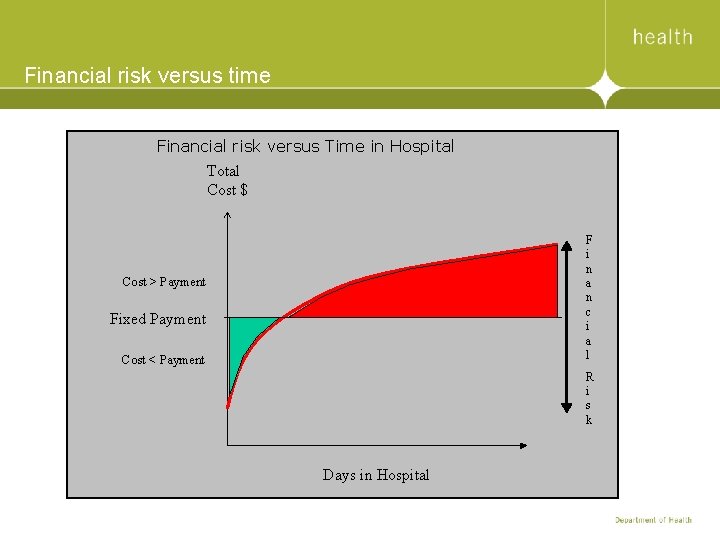
Financial risk versus time Financial risk versus Time in Hospital Total Cost $ F i n a n c i a l Cost > Payment Fixed Payment Cost < Payment R i s k Days in Hospital
Victorian casemix model: WIES (Weighted Inlier Equivalent Separations) Adjusts cost weights for patients with different types of stay Extended hospital stay (high outlier) Typical hospital stay (inlier) Short hospital stay (low outlier) Same day & overnight care Allocates additional cost weights for special types of care (copayments) Patients requiring ventilation support in ICUs Some specific conditions & treatments

Cost weight adjustments for length of stay (IES) Average Cost 1. 00 Low Boundary AVG Length of stay (days) High Boundary
Setting DRG boundaries Victorian uses multiplicative boundaries For most DRGs: • Low boundary = 1/3 * Ave LOS • High boundary = 3 * Ave LOS For a minority of DRGs: • Low boundary = 2/3 * Ave LOS • High boundary = 3/2 * Ave LOS
Cost weights are updated every financial year To ensure funding policy captures Latest cost data More activity (hospitals & separations) Changes in clinical practice New technologies New policy initiatives Updated policy • Refresh boundaries • Refresh same-day DRG status

WIES Targets DH agrees to fund a set number of WIES (Target) Variable payment for each HS = WIES Target * WIES price Hospitals largely decide which DRGs to fund Target payments are made by instalments through a financial year
Why different WIES prices? Payment = WIES Value x WIES Prices vary by: Hospital type • Different economies of scale • Remoteness Patient type • Different funding mechanisms
How much cost does WIES price cover? About 70 -80% of the average cost of treating a patient WIES price not set to cover 100% of cost Other sources of funding (e. g. grants) Change in WIES price should match change in overall average cost of treating a patient
Grant funding Types of grants Teaching and Research New technology Specified grants for specific reasons Incentive schemes Compensation grants Other funds Donations, research grants, canteen, laundry services, etc. These additional funding steams mean that WIES on average reimburses ~70 -80% of actual cost
Questions?
 Wies funding
Wies funding Sig distribution cardiff
Sig distribution cardiff Jeff james director
Jeff james director Clem brohier
Clem brohier National lottery funding application form 2010/1
National lottery funding application form 2010/1 Komponen casemix
Komponen casemix Komponen casemix
Komponen casemix Komponen casemix
Komponen casemix Casemix rekam medis
Casemix rekam medis Kswan
Kswan Disorganized crime scene
Disorganized crime scene Russell odom and clay lawson
Russell odom and clay lawson Participating funding arrangement
Participating funding arrangement Marcus scheuren
Marcus scheuren Hcrp harvard
Hcrp harvard Panasas funding
Panasas funding How to invest in garuda aerospace
How to invest in garuda aerospace Esfa funding
Esfa funding Cihr funding opportunities
Cihr funding opportunities Cape funding list
Cape funding list Unit 5 operating your business lesson 1 funding sources
Unit 5 operating your business lesson 1 funding sources Apprenticeship funding bands
Apprenticeship funding bands