CASE STUDY SILENT DISEASE Fran Connolly FNP S



- Slides: 23
CASE STUDY: SILENT DISEASE Fran Connolly FNP- S

PATIENT & ENCOUNTER B. H. is a 57 year old white female who presents in her gynecology office (Capital Region OB/GYN) for her annual exam. Her initial visit occurred on 2/10/2015. She had no complaints. The only significant finding on her ROS was her 24 hour dietary review which consisted of eating ½ gallon of ice cream nightly and 3 nights a week it was her dinner.
HISTORY OF PRESENT ILLNESS Initial visit to her Primary Care Physician was on 1/6/15 At that visit she had routine lab work done which consisted of a CBC with diff, CMP, thyroid panel, cholesterol, and Hg. A 1 c. With results of her labs, her PCP ordered an U/S which was completed on 2/2/15. She had no complaints at her PCP visit as well.

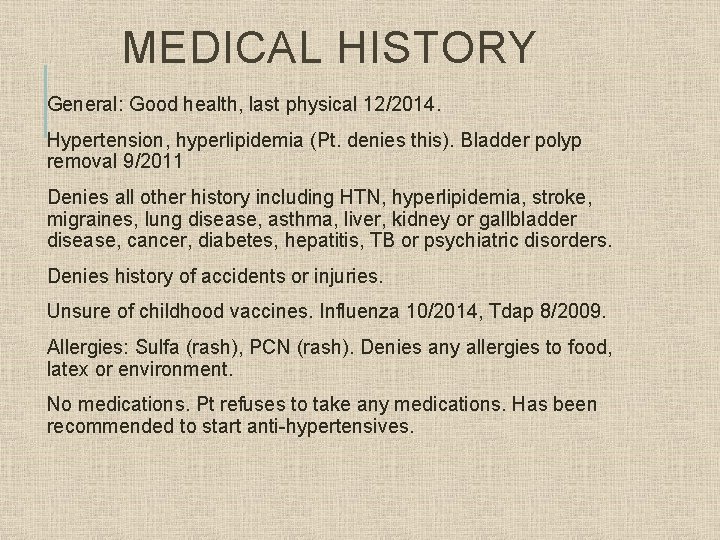
INITIAL PLAN Lifestyle Modification to include: Dietary changes Exercise
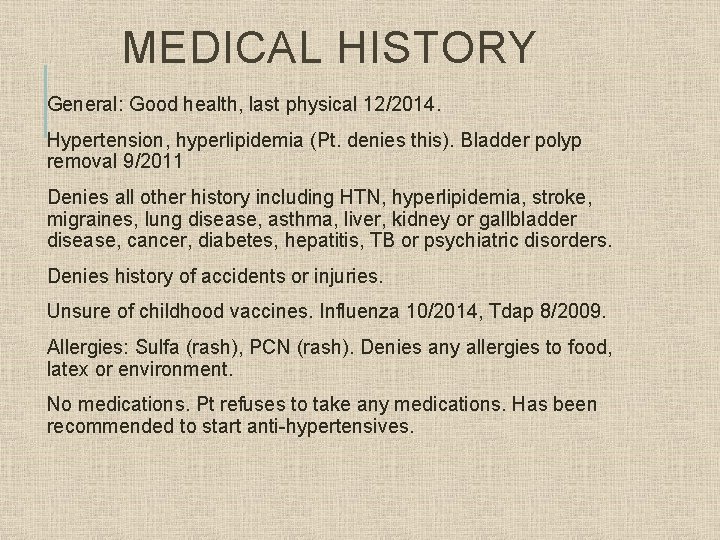
MEDICAL HISTORY General: Good health, last physical 12/2014. Hypertension, hyperlipidemia (Pt. denies this). Bladder polyp removal 9/2011 Denies all other history including HTN, hyperlipidemia, stroke, migraines, lung disease, asthma, liver, kidney or gallbladder disease, cancer, diabetes, hepatitis, TB or psychiatric disorders. Denies history of accidents or injuries. Unsure of childhood vaccines. Influenza 10/2014, Tdap 8/2009. Allergies: Sulfa (rash), PCN (rash). Denies any allergies to food, latex or environment. No medications. Pt refuses to take any medications. Has been recommended to start anti-hypertensives.
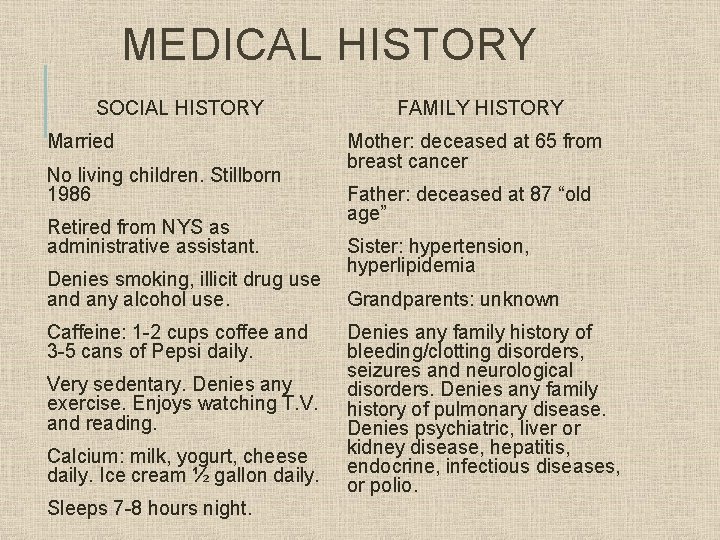
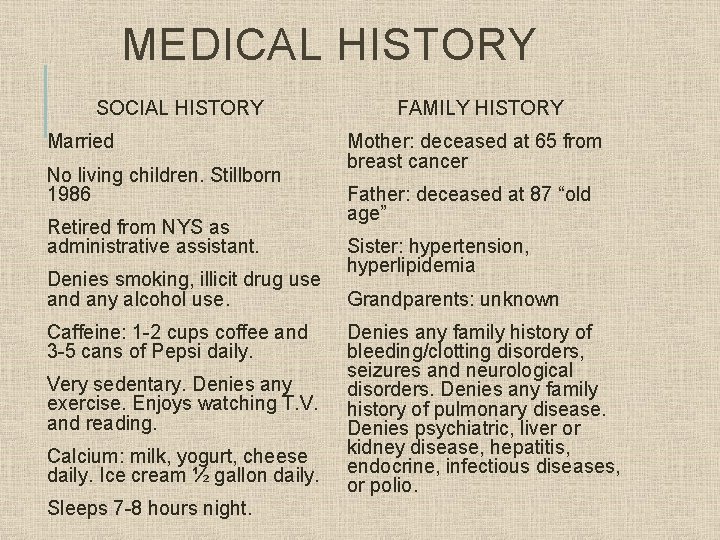
MEDICAL HISTORY SOCIAL HISTORY Married No living children. Stillborn 1986 Retired from NYS as administrative assistant. Denies smoking, illicit drug use and any alcohol use. Caffeine: 1 -2 cups coffee and 3 -5 cans of Pepsi daily. Very sedentary. Denies any exercise. Enjoys watching T. V. and reading. Calcium: milk, yogurt, cheese daily. Ice cream ½ gallon daily. Sleeps 7 -8 hours night. FAMILY HISTORY Mother: deceased at 65 from breast cancer Father: deceased at 87 “old age” Sister: hypertension, hyperlipidemia Grandparents: unknown Denies any family history of bleeding/clotting disorders, seizures and neurological disorders. Denies any family history of pulmonary disease. Denies psychiatric, liver or kidney disease, hepatitis, endocrine, infectious diseases, or polio.
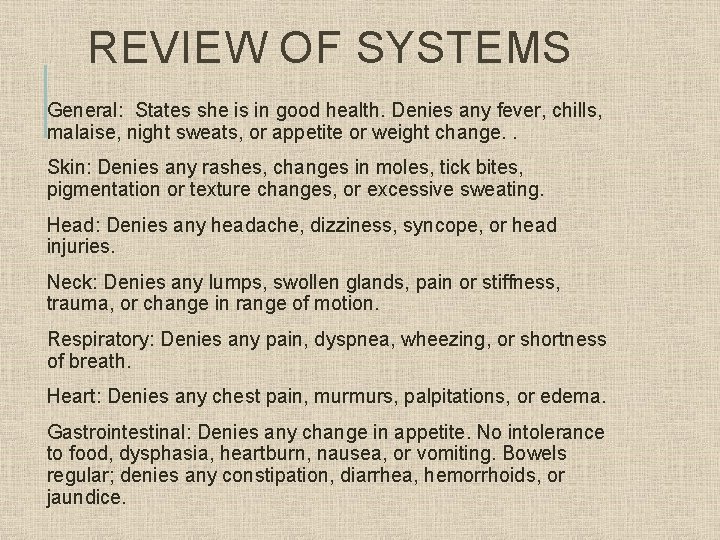
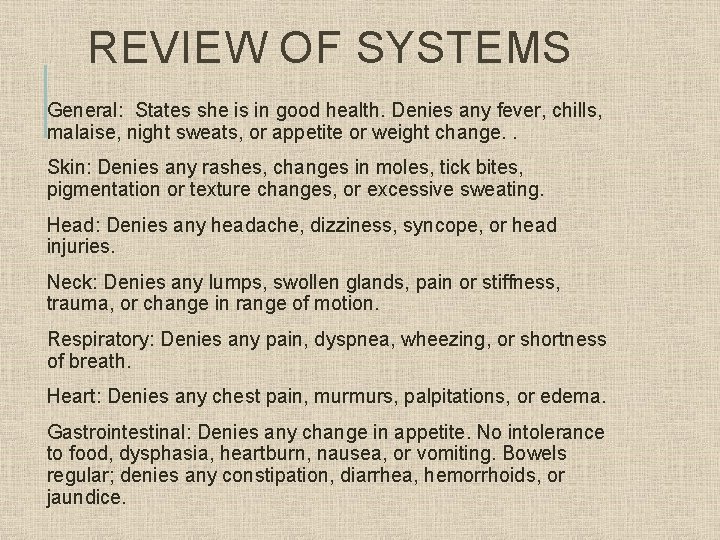
REVIEW OF SYSTEMS General: States she is in good health. Denies any fever, chills, malaise, night sweats, or appetite or weight change. . Skin: Denies any rashes, changes in moles, tick bites, pigmentation or texture changes, or excessive sweating. Head: Denies any headache, dizziness, syncope, or head injuries. Neck: Denies any lumps, swollen glands, pain or stiffness, trauma, or change in range of motion. Respiratory: Denies any pain, dyspnea, wheezing, or shortness of breath. Heart: Denies any chest pain, murmurs, palpitations, or edema. Gastrointestinal: Denies any change in appetite. No intolerance to food, dysphasia, heartburn, nausea, or vomiting. Bowels regular; denies any constipation, diarrhea, hemorrhoids, or jaundice.
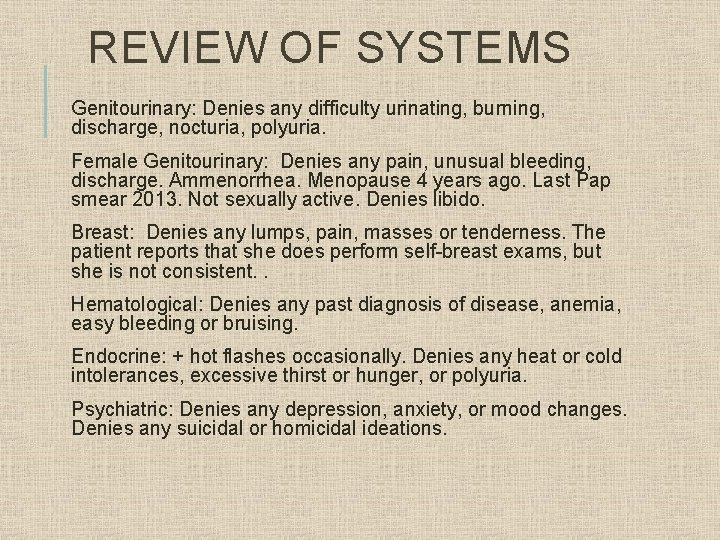
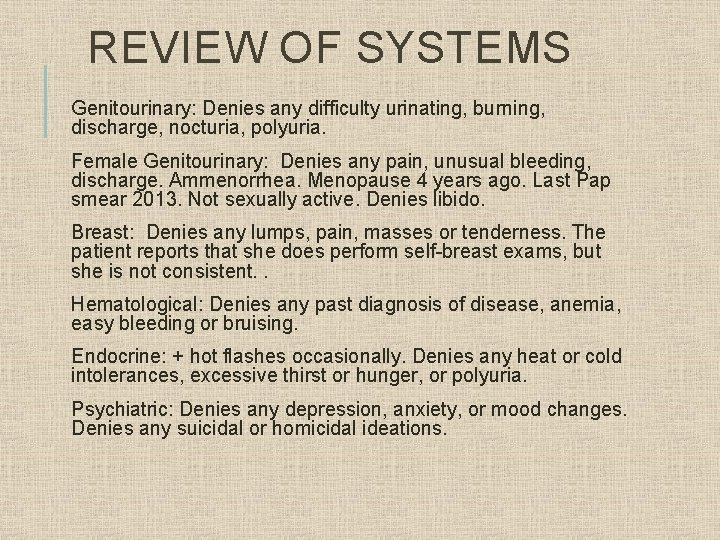
REVIEW OF SYSTEMS Genitourinary: Denies any difficulty urinating, burning, discharge, nocturia, polyuria. Female Genitourinary: Denies any pain, unusual bleeding, discharge. Ammenorrhea. Menopause 4 years ago. Last Pap smear 2013. Not sexually active. Denies libido. Breast: Denies any lumps, pain, masses or tenderness. The patient reports that she does perform self-breast exams, but she is not consistent. . Hematological: Denies any past diagnosis of disease, anemia, easy bleeding or bruising. Endocrine: + hot flashes occasionally. Denies any heat or cold intolerances, excessive thirst or hunger, or polyuria. Psychiatric: Denies any depression, anxiety, or mood changes. Denies any suicidal or homicidal ideations.
PHYSICAL FINDINGS Constitutional: BP 180/95, repeat 162/92 after exam, HR 85, RR 18, T 98. 1, denies pain. Ht: 5’ 4” Wt: 163 lbs BMI: 26 General: Well nourished, well developed, well hydrated, slightly over-weight. Alert & oriented x 3. Not in acute distress. Appropriate mood and affect. Skin: Pink, warm & dry. No rashes or lesions. Skin: Pink, warm, and dry. No rashes, moles or lesions. Head: Normocephalic, symmetric, no lesions. Hair grey & course, even distribution. Neck/Lymph: Supple with full range of motion. Trachea midline. No carotid bruits. No lymphadenopathy. Thyroid not palpable. Thorax/Lungs: Pt sitting upright, Resp resting 18/min, regular and even; Chest expansion symmetric. Lungs clear with auscultation anteriorly/posteriorly in all lobes. No rales, rhonchi, or wheezing.
PHYSICAL FINDINGS CV/PV: S 1 S 2 present in APETM with bell and diaphragm. Regular apical rate. No heaves or thrills. No murmurs, rubs, gallops, or clicks. RRR. Extremities pink, warm to touch without edema. Abdomen: Rounded, no lesions, bulges, scars/striae, masses or rashes. Smooth, pink, even color, hair with even distribution. Movement only with respirations. Umbilicus inverted, midline. No hernia visible. BS x 4 quadrants. No bruits. Percussion yields tympany in all 4 quadrants. Abd soft, no tenderness, no guarding, no masses, organomegaly or herniations. No CVA tenderness. No rebound tenderness. Breasts: Pendulous, symmetrical with no visible lesions, dimpling or lumps. Breast exam performed sitting and supine with hands overhead. No lumps or masses palpated. No lymphadenopathy present on breast, tail or axilla, no tenderness with palpation. Nipples present, equal, no discharge. Female: Pubic hair grey, distribution scattered. Vaginal wall pink, moist, and well rugated without lesions. Introitus pale pink, dry. Cervix visualized, pink, without lesions, and negative for cervical motion tenderness on palpation. No blood or discharge present.
DIFFERENTIAL DIAGNOSIS Viral Hepatitis (070. 9) Alcohol Hepatitis (571. 1) Hemochromatosis (275. 03) Wilson Disease (275. 1) Cirrhosis (571. 5) Autoimmune Hepatitis (571. 42) Celiac Disease (579. 0) Hypertension (401. 9) Hyperlipidemia (272. 4)
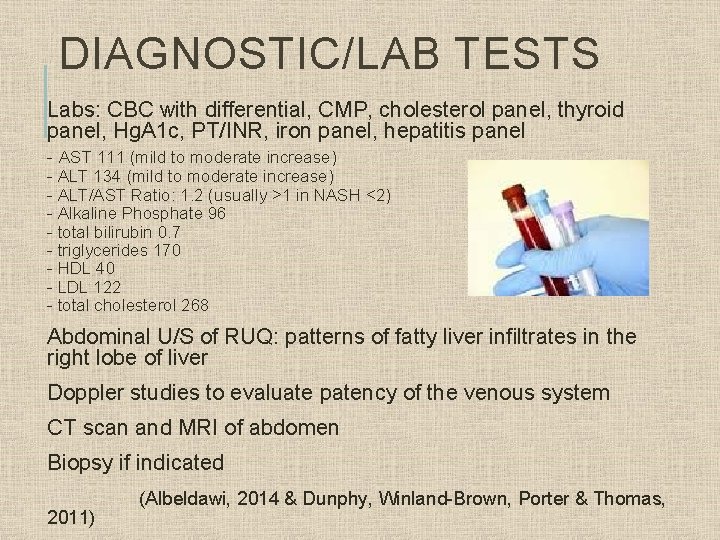
DIAGNOSTIC/LAB TESTS Labs: CBC with differential, CMP, cholesterol panel, thyroid panel, Hg. A 1 c, PT/INR, iron panel, hepatitis panel - AST 111 (mild to moderate increase) - ALT 134 (mild to moderate increase) - ALT/AST Ratio: 1. 2 (usually >1 in NASH <2) - Alkaline Phosphate 96 - total bilirubin 0. 7 - triglycerides 170 - HDL 40 - LDL 122 - total cholesterol 268 Abdominal U/S of RUQ: patterns of fatty liver infiltrates in the right lobe of liver Doppler studies to evaluate patency of the venous system CT scan and MRI of abdomen Biopsy if indicated 2011) (Albeldawi, 2014 & Dunphy, Winland-Brown, Porter & Thomas,
DIAGNOSIS Nonalcoholic Steatohepatitis (NASH) (571. 9) A. K. A. Nonalcoholic Fatty Liver Disease (NAFLD) Hypertension (401. 9) Hyperlipidemia (272. 4) Menopausal Status (V 49. 81)
NONALCOHOLIC STEATOHEPATITIS (NASH) The term for nonalcoholic fatty liver disease (NAFLD) which can lead to cirrhosis and end-stage liver disease. NASH can range from fatty infiltrates of the liver to steatosis with inflammation and hepatocyte necrosis. Clinical diagnosis requires: - hepatic steatosis by imaging/histology - no significant alcohol consumption - no competing etiologies - no coexisting causes for chronic liver disease NASH is the most severe form of NAFLD. Coexistent conditions that are associated with NASH are obesity, DM 2, metabolic syndrome and hyperlipidemia. (Albeldawi, 2014 & Porth, 2011)
ETIOLOGY The cause is unknown, but linked to obesity, insulin resistance and metabolic syndrome. Insulin resistance is the most important trigger of fatty liver disease and NASH. These conditions can remain stable for years and therefore progression may come when another comorbidity appears. Triggers can include cytokine-mediated inflammation, lipid peroxidation and apoptosis. (Albeldawi, 2014)
INCIDENCE There is a worldwide distribution and is the most common form of chronic liver disease in the Western world. NAFLD affects 6. 3 -33% and NASH 3 -17% of people in the US. 9 -20% of NASH patients develop cirrhosis. 22 -33% of cirrhotics die of complications of liver failure or require liver transplant. The increase in prevalence is on track with the epidemic in obesity and DM. Predominant age group 50 -60’s The presence of metabolic syndromes can increase the future development of NASH by 4 -11 fold. (Albeldawi, 2014)
RISK FACTORS Obesity - associated in 25 -93% of patients with NASH Diabetes - present in 30 -50% of patients with NASH Hyperlipidemia - found in up to 92% of patients with NASH Less common risk factors: hypothyroidism, hypopituitarism, sleep apnea, and polycystic ovarian syndrome. (Albeldawi, 2014 & Porth, 2011)
PATHOPHYSIOLOGY NASH is a lipid accumulation within hepatocytes and formation of free radicals. The primary metabolic abnormalities that lead to this accumulation is yet to be fully discovered, but thought to include shifts in the pathways for uptake, synthesis, degradation, or secretion of hepatic lipids resulting from insulin resistance. When insulin resistance develops, free fatty acids are inappropriately shifted to non adipose tissue including the liver. The insulin resistance also decreases the inhibition of lipolysis and increase lipogenesis. Obesity increases the synthesis and reduces oxidation of free fatty acids. When the capacity of the liver to export triglyceride is exceeded, excess fatty acids are deposited within the liver, hence the development of steatosis.
SIGNS & SYMPTOMS Usually asymptomatic and an incidental finding on annual exam which can include an enlarged liver on exam and increased liver enzymes on labs. -Fatigue/Malaise -Discomfort RUQ of abdomen -Hepatomegaly is present in 75% of patients with NASH Once advanced: Can include weakness, nausea, anorexia, weight loss, fatigue, malnutrition, puritis, jaundice, edema, menstrual abnormalities, loss of libido, impotence, sterility, gynomastia, enlarged firm liver edge palpable below the right costal margin. - Ascites - Varices - Encephalopathy (Albeldawi, 2014 & Dunphy, Winland-Brown, Porter & Thomas, 2011)
INTERVENTIONS The aim of treatment is to slow progression of the disease and prevent liver related illness. Treat associated comorbidities such as cholesterol, DM, & obesity. Medications should be restricted to patients at risk for developing advanced liver disease. There is no evidenced-based medications proven to treat NASH. Vitamin E 800 IU daily improves liver histology (1 st Line therapy) OTC Medications: MVI, Vitamin B 12, folate, thiamine, magnesium, milk thistle and zinc Liver biopsy for definitive diagnosis and staging Bariatric surgery for weight loss (which can also cause NASH) Liver transplant. Although NASH can redevelop after transplantation (Albeldawi, 2014 & Porth, 2011)
EDUCATION Dietary education - Protein intake should be increased to 1 -1. 5 grams per kg daily - Restrict calories, carbohydrates - Avoid alcohol Exercise education With progression: - daily weights to monitor fluid retention and ascites - medications to avoid Tylenol, Vitamin A, Tetracycline, Dilantin (Albeldawi, 2014, Dunphy, Winland-Brown, Porter & Thomas, 2011 & Porth, 2011)

FOLLOW-UP Should be regular monitoring to detect progression through physical exam, labs, symptoms and diagnostics. Referral to registered dietitian or nutritionist Consult Hepatologist Consult Gastroenterologist 2011) (Albeldawi, 2014 & Porth,
REFERENCES Albeldawi, M. (2014). The 5 -minute clinical consult 2014 (22 nd ed. ). Lippincott, Williams & Wilkins, Philadelphia, PA. Dunphy, L. M. , Winland-Brown, J. E. , Porter, B. O. & Thomas, D. J. (2011). Primary care: The art and science of advanced practice nursing (3 rd ed. ). Philadelphia, PA: F. A. Davis Company. Porth, C. M. (2011). Essentials of Pathophysiology (3 rd ed. ). Philadelphia, PA: Lippincott Williams & Wilkins
 The way my mother speaks
The way my mother speaks Pes statement for celiac disease
Pes statement for celiac disease Micaela connolly
Micaela connolly Prashan patel grant thornton
Prashan patel grant thornton Fundamentals of web development randy connolly ppt
Fundamentals of web development randy connolly ppt Clare partridge
Clare partridge Connolly recovery audit
Connolly recovery audit Connolly lodge buckingham street
Connolly lodge buckingham street Connolly & hickey historical architects
Connolly & hickey historical architects Ocd and school refusal
Ocd and school refusal Meditrek walden login
Meditrek walden login Chamberlain practicum handbook
Chamberlain practicum handbook Inversion lenta fnp
Inversion lenta fnp Nurse practitioner core competencies
Nurse practitioner core competencies Best case worst case average case
Best case worst case average case Fbi virtual case file case study
Fbi virtual case file case study Communicable disease and non communicable disease
Communicable disease and non communicable disease Kinesiska muren från månen
Kinesiska muren från månen State of ct division of criminal justice
State of ct division of criminal justice Ta bort stearin från matta
Ta bort stearin från matta Matens väg
Matens väg Från student till docent
Från student till docent Vad är en gen
Vad är en gen Decentralizimi fiskal
Decentralizimi fiskal