Case Study Patient with Colon CancerIleostomy placement Laura






- Slides: 32

+ Case Study: Patient with Colon Cancer/Ileostomy placement Laura Salinas KSC Dietetic Intern 12 -13
+ Today, we will discuss 1. Pathophysiology of colon cancer/colectomy/ileostomy 2. Medical Nutrition Therapy & Nutrition Care Process Diagnosis & Hospital course Nutritional Assessments MNT recommendations & Diet Orders Goals Interventions Evaluation/reassessment
+ Northeast Methodist Hospital Operational Vision: To meet the needs and exceed the expectations of those we serve by working together as a team in a culture dedicated to never-ending improvement. 179 Licensed beds n NEMH offers a full array of services: n ER n CABG & cardiac catheterizations n Inpatient rehabilitation n Orthopedic surgery n Oncology/Cancer Care n ICU/PCU n Inpatient and outpatient surgeries and procedures

+ Role of the RD at NEMH n 2 Full Time Registered Dietitians n Screening, Evaluations, Assessing Nutritional Needs n n n N/V, Skin comp, decreased intake, weight loss, difficulty swallowing, TPN/EN, >65 with surgery, Kidney dx, Cancer, DM, GI, Stroke, Liver Dx n Ventilated patient automatically trigger n LOS > 6 days or NPO > 3 days Works with full health care staff n n Screening triggers with a score of 7: Diet office, RN, Doctors, ICU & Rehab rounds Consultations & Diet Educations

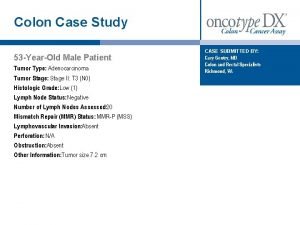
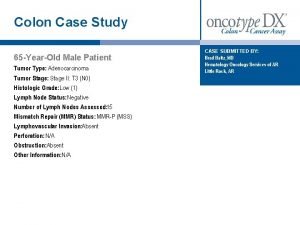
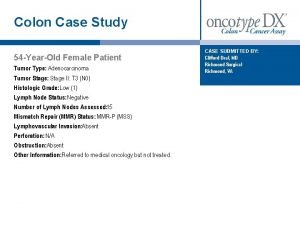
+ Meet Ms. A n 42 year old female admitted June 3, 2013 n Diagnosis: Colon Cancer, Laparoscopic Right Hemicolectomy n Severe Iron Deficiency Anemia n n Iron 18 mcg/d. L, Iron Saturation 5%, Hgb 9. 8 g/d. L Colonoscopy n polyps with tubulovillous adenoma with high-grade dysplasia n Medical History: Hyperlipidemia, Bipolar Disorder, Anemia, Gastric Bypass (2004) n Diet Order: Clear Liquid Diet (POD #1) n Labs (POD #2): Glu 115, Ca 8. 0, PO 4 1. 7, Mg 1. 4, Alb 2. 6, Hgb 8. 5, Hct 25. 7 n (POD #3): Iron 9 mcg/d. L, Iron Sat. 4%, Transferrin 184 mg/d. L
+ Colon Cancer: Pathophysiology n Most cases of colon cancer begin as small benign clumps of cells called adenomatous polyps. n Over time, polyps can develop into colon cancers. n Treatment: n n Surgery n Early stage n Invasive*** n Advanced Chemotherapy Radiation Therapy Targeted Drug Therapy
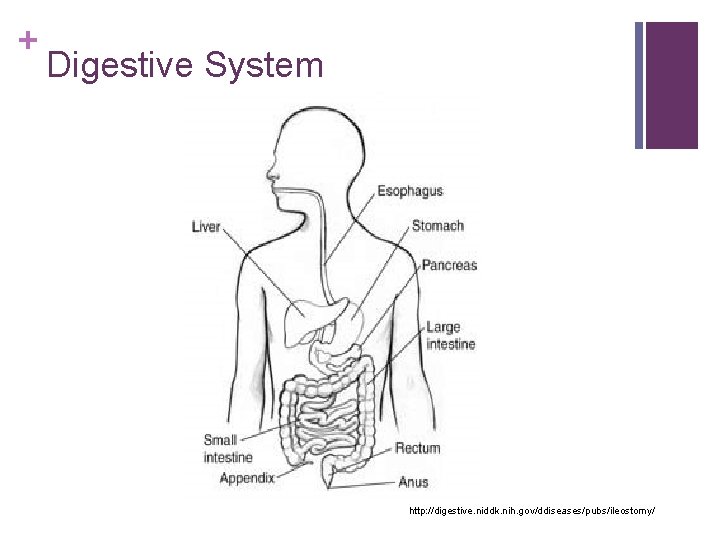
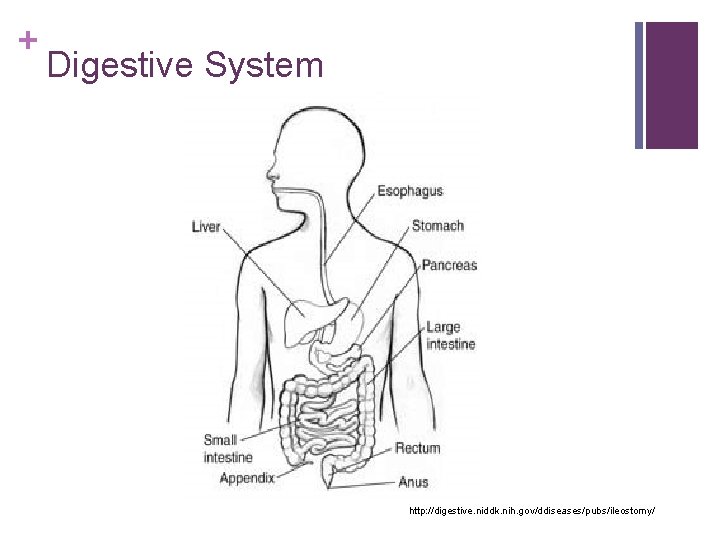
+ Digestive System http: //digestive. niddk. nih. gov/ddiseases/pubs/ileostomy/
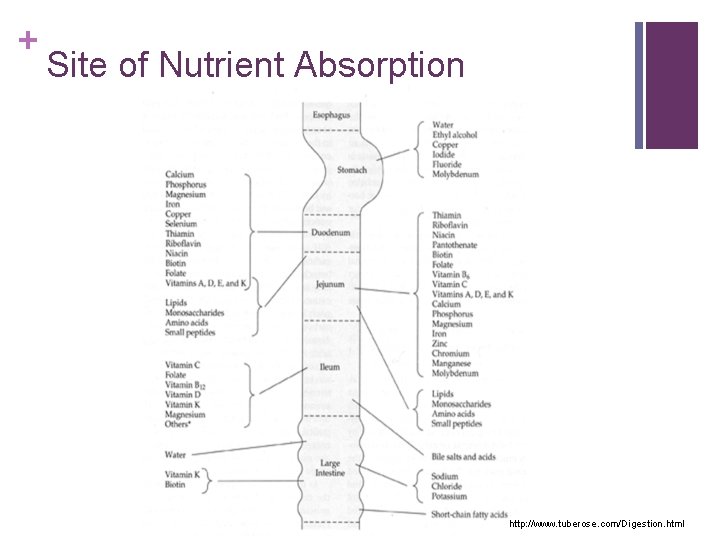
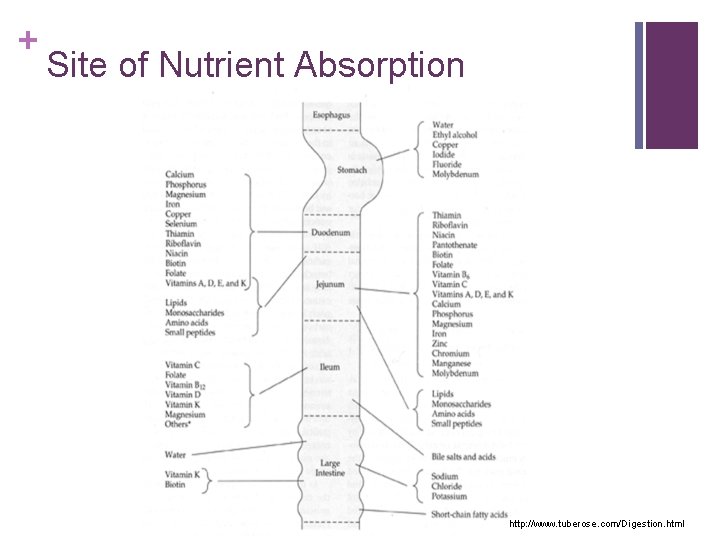
+ Site of Nutrient Absorption http: //www. tuberose. com/Digestion. html
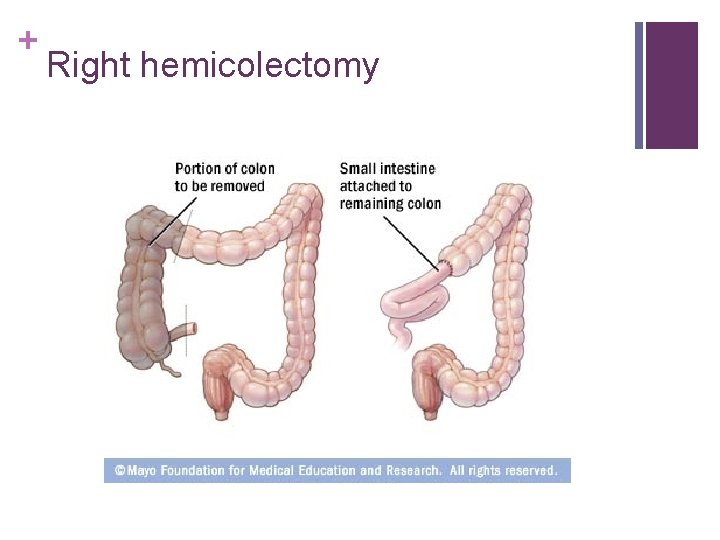
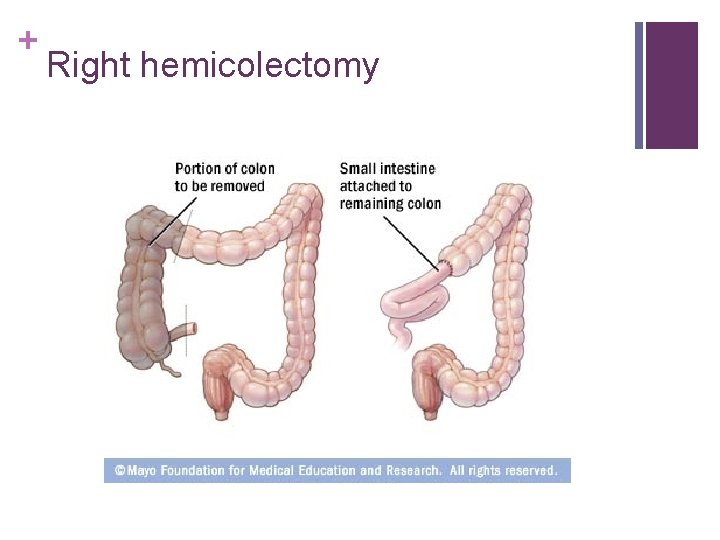
+ Right hemicolectomy
+ What went wrong? n POD #4 (6/7/13) n Pt experiencing persistent abdominal pain and dark urine n Enema revealed brownish/red stool n Temperature spiked to 100. 4 F. n Hold heparin, protonix, KUB ordered n KUB revealed ileus with free air n Lab Values: Na 134, Cl 97, BUN 28, ALB 2. 2, GFR 58, GLU 114, CA 8. 4, MG 2. 7 n Nutrition Status n Diet Order: Bariatric/Gastric Bypass Diet
+ Clinical Course n POD #5 (6/8/13) n Nutrition Status n Declining – notes indicate pt is unable to eat n Pain with passing gas and burping n Phenergan for N/V n POD #6 (6/9/13) n Pt required 2 units of blood (327 cc)
+ Clinical Course n POD #7 (6/10/13) n Problem List: n S/P right hemicolectomy n Severe Iron Deficiency Anemia n PMH of gastric bypass – limited ability to absorb oral iron n n Anemia n n IV replaced Hypomagnesemia n n Acute on chronic; blood loss from surgery; iron deficiency Hypophosphatemia n n IV iron IV replaced Ileus
+ Clinical Course n POD #7 (6/10/13) n Acute events: n n severe abdominal pain/abdominal distention n Nausea & vomiting n KUB showed ileus and nonspecific inflammation n Likely anastomotic leak Ms. A to OR for washout and Ileostomy n n 2 L washed out of the abdomen Nutrition Status: NPO n TPN & Lipids ordered through triple lumen IJ
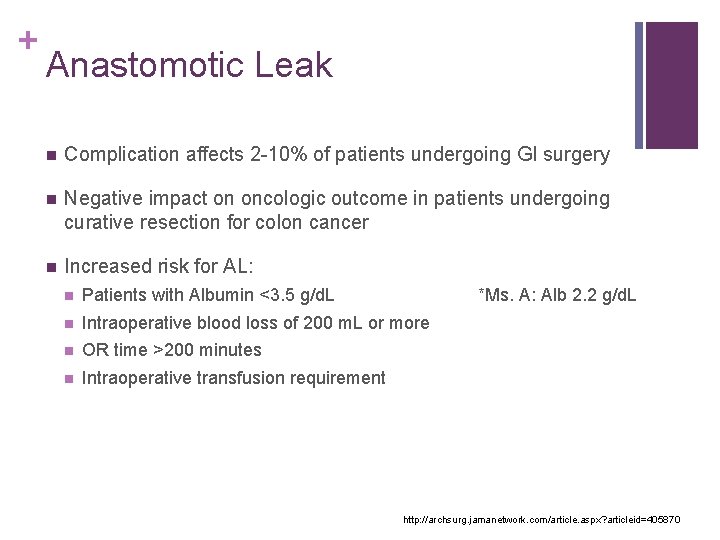
+ Anastomotic Leak n Complication affects 2 -10% of patients undergoing GI surgery n Negative impact on oncologic outcome in patients undergoing curative resection for colon cancer n Increased risk for AL: n Patients with Albumin <3. 5 g/d. L *Ms. A: Alb 2. 2 g/d. L n Intraoperative blood loss of 200 m. L or more n OR time >200 minutes n Intraoperative transfusion requirement http: //archsurg. jamanetwork. com/article. aspx? articleid=405870
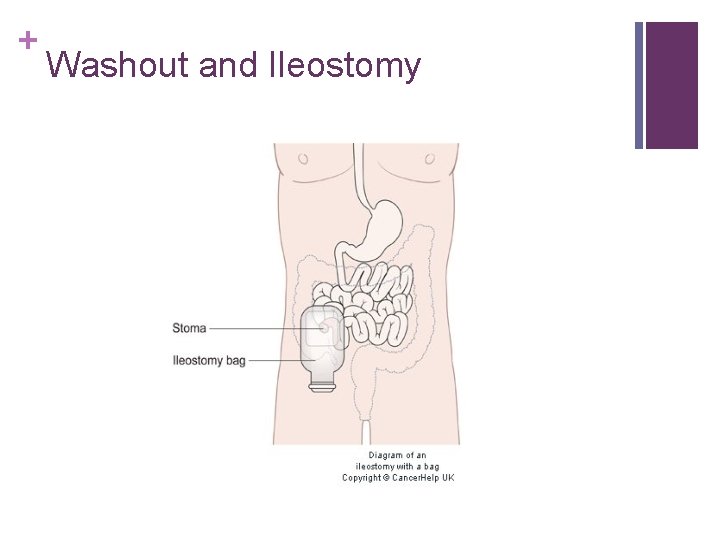
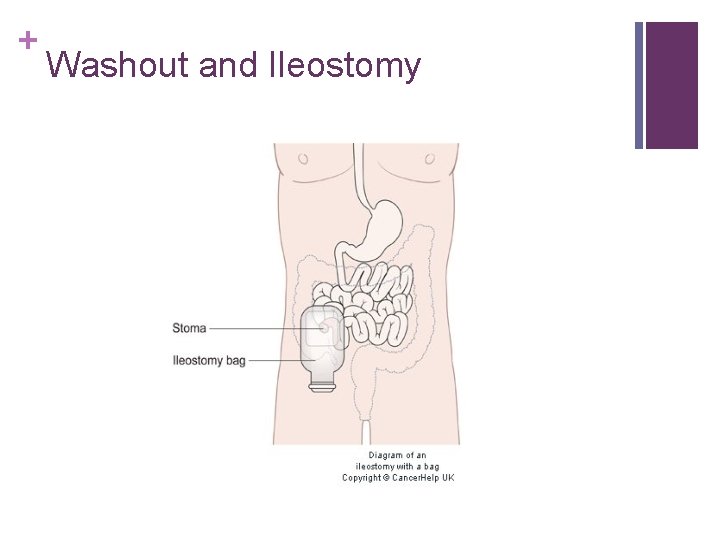
+ Washout and Ileostomy

+ Nutrition Assessment n 6/10/13* Initial Nutrition Screening Assessment n n Diet Order: NPO Weight: 226 lb (reported by patient) Estimated needs: 1659 -1990 (MSJ*1. 0 -1. 2) n Actual weight n Protein needs: 113 -135 gm/day (1. 1 -1. 3 gm/kg) n Labs: NA 133, GLU 100, CR 0. 5, ALB 1. 9, WBC 15. 6, H/H 9. 6/30. 0 n Meds: Insulin, Lovenox, Protonix, Pepcid, Phenergan, Lasix, Zofran, Morphine, Narcan, Bactroban, Ativan
+ Nutrition Assessment n 6/10/13* Initial Nutrition Screening Assessment n Diet Order: NPO Weight: 226 lb (reported by patient) n PES: Altered GI function related to altered GI structure as evidence by CT scan showing air/fluid in RLQ, patient experiencing n/v, abdominal distention, and no BM. n Goal: n n Determine nutritional status & GI function post op n Advance oral diet if functional; if not, consider nutrition support Intervention: Monitor symptoms, lab values, & diet changes
+ Clinical Course n POD #8 (6/11/13) n Ms. A S/P exploratory laparoscopy after finding free air on KUB n Ileostomy Placement n Postoperatively Hypotensive (secondary to third spacing of fluid or septic shock) n n Requiring high doses of Levophed ICU: Intubated/sedated (propofol) n TPN running at goal rate of 75 cc/hr with 150 cc 20% lipids n 2 JP drains to left abdomen with bloody output n Ileostomy with liquid brown output http: //www. cc. nih. gov/ccc/patient_education/pepubs/jp. pdf
+ Academy’s Recommendation n “Enteral nutrition should always be considered as the first line of nutrition support, with parenteral nutrition used only when the GI tract is nonfunctional either as a result of physical or physiologic (obstruction) events. ” “In some cases, the GI tract may be functional but cannot be accessed due to anatomical or pathophysiologic conditions; in those cases, parenteral nutrition should be considered. ”
+ MNT Recommendation: TPN n TPN with Lipids n Clin 5/25 n n 1050 kcal/L n Amino Acid: 50 g/L (5%) n Dextrose: 250 g/L (25%) Clin 5/25 at a rate of 75 m. L/hr with 150 m. L of 20% lipid per 24 hour infusion: n 2100 total kcal n 1700 non-protein kcal n 90 gm protein
+ Clinical Course n n POD #10 (6/13/13) n Weight: 255 lb n Ms. A remains critically ill – TPN still running POD #12 (6/15/13) n n Orders to extubate – TPN still running POD #13 (6/16/13) n Weight: 246 lb n Ms. A advanced to Full Liquid Diet – TPN still running
+ MNT recommendations: PES: Malnutrition related to alteration in GI structure and function as evidence by lap right colectomy and anastomotic leak repair with ileostomy placement, NPO status, critically ill, and ventilated/sedated. Goal: Monitor TPN & provide adequate energy to meet increased needs. Intervention: Monitor TPN, lab values, weight changes, and diet advancement

+ Clinical Course n POD #16 (6/19/13) n Weight: 242 lb n Ms. A advanced to Bariatric/Gastric Bypass Diet & TPN d/c n n MD notes indicate Ms. A tolerating PO with imodium POD #18 (6/21/13) n Ileostomy bag continually leaking n Ms. A not eating well, nausea Malnutrition related to altered GI structure/function as evidence by s/p lap right colectomy, ileostomy, and 25% full liquid diet intake. n POD #23 (6/26/13) n Ms. A discharged to Heartland for Rehab
+ Re-admit: July 3, 2013 n Diagnosis: Sepsis; Intra-abdominal abscess; Peritonitis n Nutritional Indicators with Ileostomy: n Inadequate oral intake; Inadequate fluid intake n Fluid and electrolyte imbalances n Evidence of malabsorption n Weight loss 15# since past admission n Reduced visceral protein stores Albumin 2. 1 n Vitamin & Mineral Deficiencies
+ Nutritional Assessment n 7/3/13* Initial Nutrition Consult for Supplementation n Diet Order: Full Liquid Weight: 212 lb (reported by patient) n Estimated needs: 1770 -1930 (MSJ*1. 1 -1. 2) n Protein needs: 82 -109 gm/day (1. 5 - 2. 0 gm/kg IBW) n Labs: NA 131, GLU 101, ALB 1. 7, MG 1. 7, WBC 19. 2, H/H 11. 5/34. 5 n Meds: Lactinex, Pepcid, Zofran, Imodium, Folic Acid, Marinol
+ Nutritional Assessment n 7/3/13* Initial Nutrition Consult for Supplementation n Diet Order: Full Liquid Weight: 212 lb (reported by patient) n PES: Malnutrition related to altered GI structure/function & complications as evidence by inadequate oral intake and increased protein/kcal needs. n Goal: n n Pt will tolerate oral diet >75% to meet estimated nutrition needs. n Pt will consume meals with supplements to meet estimated needs n Correct protein calorie malnutrition and promote repletion of visceral protein stores Intervention: monitor PO intake/tolerance; monitor lab values
+ Clinical Course: Goals n 7/5/13: Calorie count consult received n n Intervention n n Goal to correct protein/calorie malnutrition n Optimize postoperative healing needs n Correct nutrient deficiencies & meet estimated needs n Prevent dehydration and electrolyte imbalances Calorie Counts (7/5/13 -7/8/13) Ensure Enlive Q 4 hrs n Each Ensure Enlive provides 200 kcal & 7 gm protein Food Preferences/Monitoring by dietary staff & RD Diet Education n n Minimize symptoms of malabsorption/maldigestion Prevent gas/odor/obstruction
+ Clinical Course: Nutrients n Nutrients of greater concern n Iron n B 12 n Sodium n Potassium n Chloride n Total kcal n Total protein
+ Clinical Course n 7/10/13 n Continuing calorie count n Patient visited on many occasions to encourage PO n Ms. A voiced that she is trying to get her appetite up n Frustrations with ileostomy bag leaking/coming off n Explained symptoms and foods to avoid n Low intakes continually on calorie counts n 7/6: 753 kcal, 49 gm protein n 7/7: 766 kcal, 39 gm protein Inadequate oral intake related to dx/hx and poor appetite as evidence by patient unable to meet estimated needs in two 24 hour calorie counts.

+ Plan for d/c: n Low-fiber diet that provides adequate energy, protein, fluid, and electrolytes (Sodium/Chloride/Potassium) for healing n Increase sodium intake because of losses n Smaller more frequent meals with supplementation n Limit fluids with meals to decrease output n Education: supplementation and higher kcal/protein needs n Obstruction/Odor/Gas n Avoid chewing gum, drinking straws, carbonated beverages
+ Questions? Thank You!
+ References: American Cancer Society. Ileostomy: A Guide. Available at: www. cancer. org/acs/groups/cid/documents/webcontent/002870 -pdf. pdf National Institute of Health. How to Care for the Jackson-Pratt Drain. Available at: http: //www. cc. nih. gov/ccc/patient_education/pepubs/jp. pdf Nutrition Care Manual. Available at: www. nutritioncaremanual. org Telem DA, Chin EH, Nguyen SQ, Divino CM. Risk Factors for Anastomotic Leak Following Colorectal Surgery: A Case-Control Study. Arch Surg. 2010; 145(4): 371 -376. doi: 10. 1001/archsurg. 2010. 40. UPMC. Ostomy Nutrition Guide. Available at: www. upmc. com/patientsvisitors/education/nutrition/pages/ostomy-nutrition-guide. aspx
 Semicolon vs colon
Semicolon vs colon Semicolon and colon quiz
Semicolon and colon quiz What is colon used for
What is colon used for When do i use a semicolon
When do i use a semicolon Colon
Colon Semicolons vs colons
Semicolons vs colons When to use a semicolon examples
When to use a semicolon examples Case of kf
Case of kf Laura conocía bien a elián. elián conocía bien a laura
Laura conocía bien a elián. elián conocía bien a laura Best worst and average case
Best worst and average case Hershey's erp failure
Hershey's erp failure Patient 2 patient
Patient 2 patient Short case vs long case
Short case vs long case Binary search time complexity average case
Binary search time complexity average case Case western reserve university case school of engineering
Case western reserve university case school of engineering Bubble sort best case and worst case
Bubble sort best case and worst case Bubble sort best case and worst case
Bubble sort best case and worst case Bubble sort best case and worst case
Bubble sort best case and worst case The ambiguous case for the law of sines
The ambiguous case for the law of sines Information system of zara
Information system of zara Yelp elite benefits
Yelp elite benefits Whole foods case study
Whole foods case study Action research vs case study
Action research vs case study Volkswagen case study ppt
Volkswagen case study ppt Plant machinery valuation
Plant machinery valuation Phil stephens villanova
Phil stephens villanova Starbucks foreign direct investment case study
Starbucks foreign direct investment case study Case study 11
Case study 11 Notasi uml
Notasi uml Illustrative case study example
Illustrative case study example Tuna for lunch case study answer key
Tuna for lunch case study answer key Tuna for lunch case study answers
Tuna for lunch case study answers Rainforest case study
Rainforest case study