CASE REPORT MEGHAN MARTIN PGY 5 CASE Expect









- Slides: 27
CASE REPORT MEGHAN MARTIN PGY 5
CASE • Expect call from community PCP about a patient coming in from physical therapy. He was called by the concerned PT about the degree of head deformity and eye movements. • PCP saw the 2 mo patient one month ago, and infant was noted to have some degree of nystagmus and abnormal head shape.
CASE • Mom brings the 2 mo infant to the ED. Mom says the head shape has been worsening, but was noted to be abnormal at birth. The eye movements are also becoming more abnormal. He prefers to have his head facing the left side. • No acute symptoms otherwise. No fevers, emesis (just normal spitting up), altered mental status, high pitched cry. • He has never had any imaging or work up prior.
HISTORY • Born full term, repeat c-section. No complications. • Noted to have slightly abnormal head shape at birth. • At 1 mo visit, had decreased movement of his right side and his head preferentially turned to the left. • Sent to PT • First visit today • No family history of significance • 2 sisters at home, same biological mom and dad • Mom jokes that dad isn’t the bio father
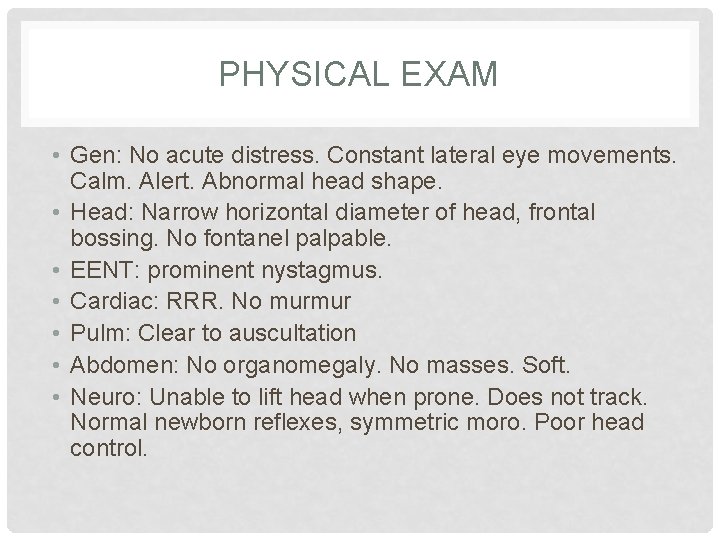
PHYSICAL EXAM • Gen: No acute distress. Constant lateral eye movements. Calm. Alert. Abnormal head shape. • Head: Narrow horizontal diameter of head, frontal bossing. No fontanel palpable. • EENT: prominent nystagmus. • Cardiac: RRR. No murmur • Pulm: Clear to auscultation • Abdomen: No organomegaly. No masses. Soft. • Neuro: Unable to lift head when prone. Does not track. Normal newborn reflexes, symmetric moro. Poor head control.

DIFFERENTIAL • • Genetic/Congenital condition Ischemic event Hydrocephalus Positional Plagiocephaly Crainosynostosis Neoplasm Non accidental trauma
WORK UP • Basic labs • CBC, CMP, PT, INR, PTT • CT Head


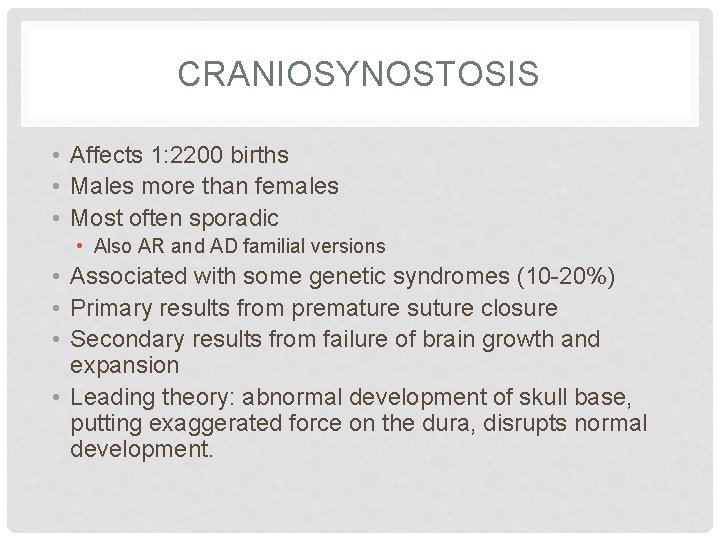
CRANIOSYNOSTOSIS • Affects 1: 2200 births • Males more than females • Most often sporadic • Also AR and AD familial versions • Associated with some genetic syndromes (10 -20%) • Primary results from premature suture closure • Secondary results from failure of brain growth and expansion • Leading theory: abnormal development of skull base, putting exaggerated force on the dura, disrupts normal development.



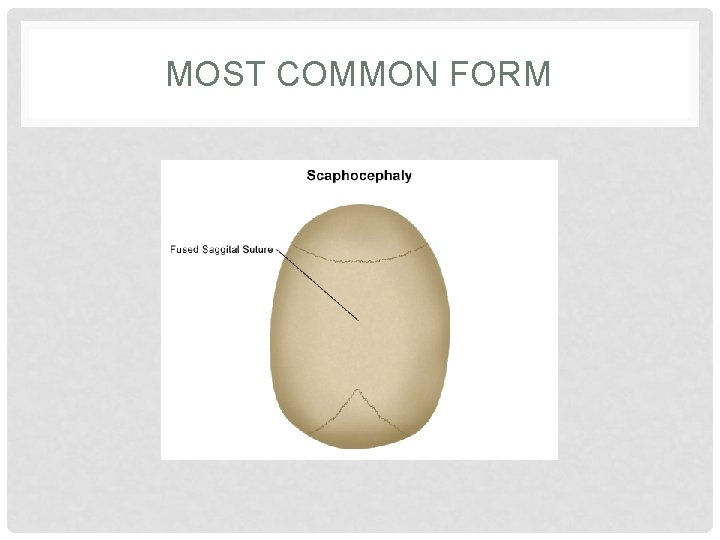
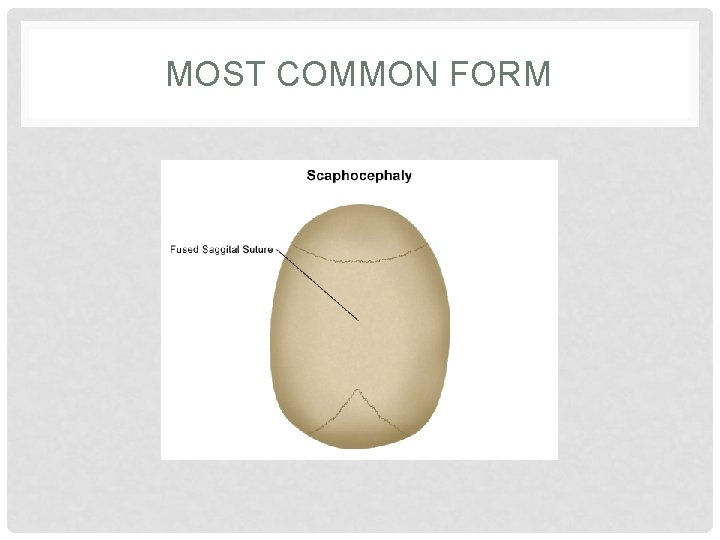
MOST COMMON FORM
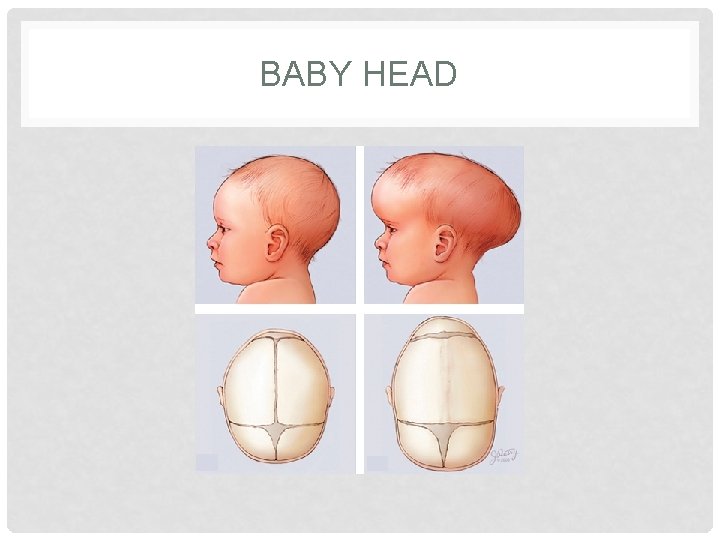
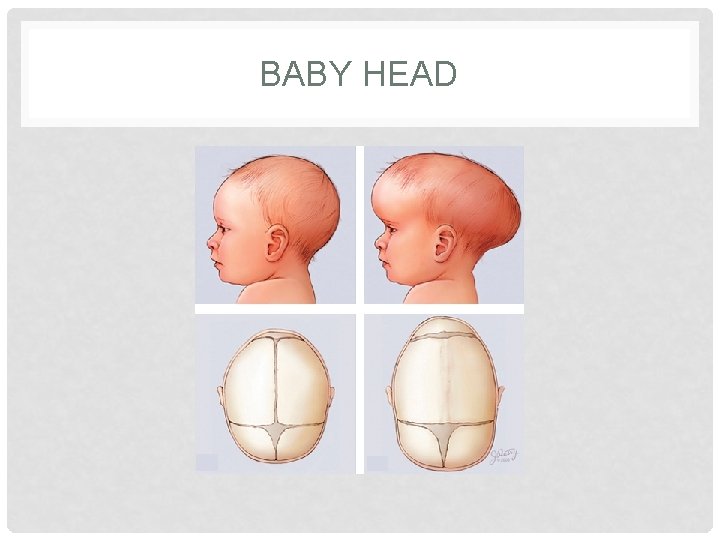
BABY HEAD
SCAPHOCEPHALY • • • Male predominant Most common form Prominent occiput Broad forehead C-sections for cephalopelvic disproportion Does not produce increased ICP or hydrocephalus • Complications occur if two or more sutures close

SOOOO…. . ? • CT shows scaphocephaly, but normal ventricles. • No acute neurosurgical concerns • Primarily sent for nystagmus • Could the nystagmus be anything else?
OPSOCLONUS-MYOCLONUS-ATAXIA • Paraneoplastic syndrome associated with neuroblastoma • Autoimmune reaction • Ultrasound abdomen performed and WNL
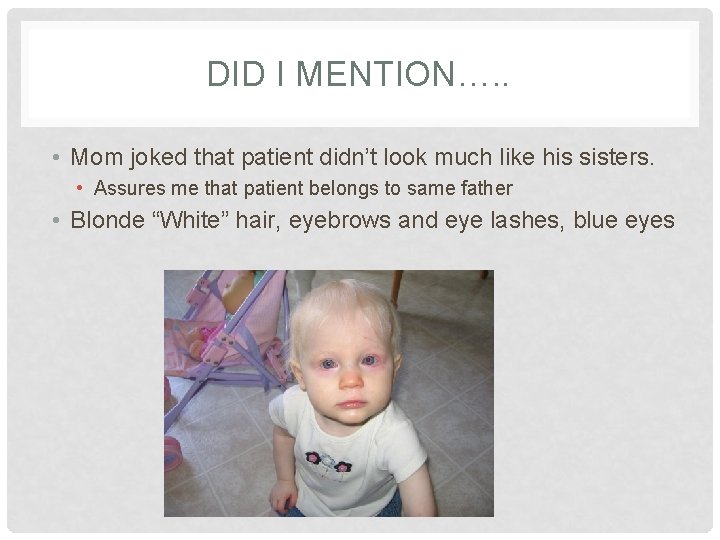
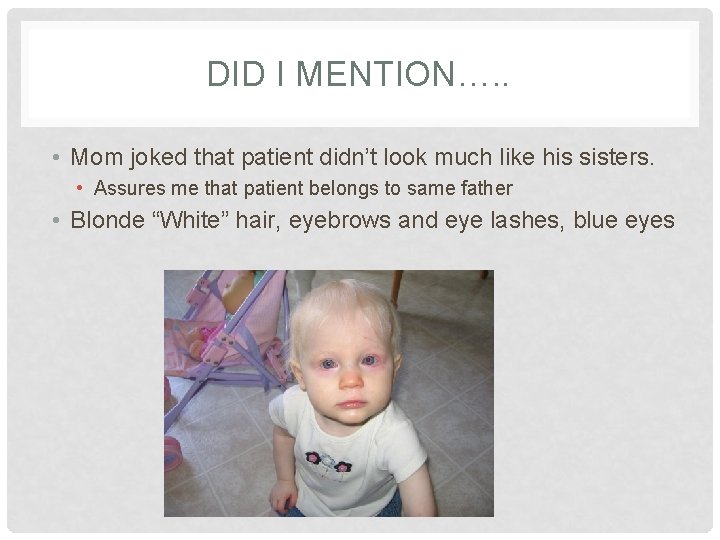
DID I MENTION…. . • Mom joked that patient didn’t look much like his sisters. • Assures me that patient belongs to same father • Blonde “White” hair, eyebrows and eye lashes, blue eyes
ALBINSIM • Deficiency of melanin • Can be ocular or oculocutaneous • Oculocutaneous are all AR • Clinical syndromes in association with • Platelet dysfunction • Immunological dysfunction • Neurological dysfunction
OCULAR MANIFESTATIONS • Hypopigmentation • Including foveal hypoplasia • • • Reduced visual acuity Refractory errors Nystagmus Alternating strabismus Abnormality of optic nerve routing
OTHER MANIFESTATION • Melanin is also present in the cochlea • Very susceptible to ototoxic agents • Avoid gentamicin • Don’t make them blind and deaf!! • Skin sensitive to UV • Protective clothing and SPF >30
FOLLOW UP • Neurology consulted after CT and Ultrasound • Agreed with albinism and scaphocephaly • Outpatient follow up with: • • Neurology Neurosurgery Ophtho (pending) Genetics • PCP contacted and updated. Agrees with plan. • Patient had cranial reconstruction on 8/8/14 • Did well, discharged 8/12/14 • Genetics diagnosed albinism, Neurology in agreement

