Case Report LE Limb weighting for AtaxiaProprioception Discussion
Case Report -LE Limb weighting for Ataxia/Proprioception -Discussion: EBM Garett Manack SPT
CASE REPORT- BACKGROUND • 73 YO MALE admitted to ACH for T 5 Laminectomy and Ligation of Dural arteriovenous fistula (AVF) • Prior to surgery, neurogenic bladder and bowel • Not ambulating d/t pain, but was ambulating with walker when d/c prior stay at SRH. • PRECAUTIONS: Spine, WBAT, Fall risk, Rev. Iso • PLOF: B/L platform FWW at home, recently power scooter for mobilty, transferring w/out assist; Wife assist w/ transportation and some IADLS. (+) Hx of falls • Home Set-up: Basement apartment, walk-out entry w/out stairs, chair-lift b/w basement and main floor, ramp entry garage to main level
EXAMINATION • Cognition: A&O x 4; follows mult step commands • Sensory: • Decreased proprioception • LT diminished B/L LEs • (+) Numbness/tingling in B/L feet • MMT: • LE: Hip flex, knee flex/ext, ankle PF/DF grossly 3+ to 4 -/5, R LE slightly weaker than L • UE: grossly WFL B/L • Posture: • Seated: FW head rounded shoulders • Standing: FW head, rounded shoulders, retropulsive and often w/ B/L knee hyper-extension
FIMs • BED MOBILITY: Min/CGA- instructed in log roll technique for neutral spine • TRANSFERS: • Sit to Stand- Max A x 2 in // bars; pt. vaults to stand • BED to/from WC: • Scoot-pivot CG/Min • SPT Max Assist w/ B/L knee blocking- demo and cues required t/o for safe transfer set-up, technique and sequencing
FIMs cont. . • GAIT: TOTAL A <50 feet • 3 ft x 1 and 8 ft x 1 in // bars, mod-max A x 1 and SBA/WC follow for safety. • Unsteady and ataxic • Recurvatum • Retropulsion at times • Additional demo, 1 -step cues t/o for step-to sequence, upright posture • Unable to perform stairs • WC MOBILITY: Min/CG • 150 ft x 1 assist for leg rest set-up, cues and occasional min assit for steering; (+) obstacle collision
EXAM cont. • Safety awareness- fair, very receptive to education provided, at time fearful of falling with mobility • Seated balance: • Good Static • Fair Dynamic- UE often needed with dynamic tasks • Standing balance: • Poor static and dynamic • Activity tolerance: good minus- required frequent rest breaks; pleasant and highly motivated
PROBLEM LIST • FUNCTIONAL LIMITATIONSDECREASED: • ADLS • IADLS • BEDMOB • TRANSFERS • FUNCTIONAL WC SKILLS • FUNCTIONAL GAIT • STAIR CLIMBING • IMPAIRMENTS: • • • Impaired strength Decreased Endurance Impaired motor control Abnormal muscle tone Abnormal postural control Impaired balance Decreased coordination Decreased sensation Decreased proprioception Pain Decreased skin integrity
Prognosis and Assessment • Good based on mod impairments, but functional gains can be accomplished; motivation and understanding of rehab process (round 2 with AVF) and familycaregiver support is good of optimal outcome • ASSESSMENT: 73 y/o male, previously mod I at power WC level and living with family, who now presents with pain, LE weakness and decreased motor control/coordination, decreased balance and postural control, and requires physical assist with all mobility secondary to recent functional decline and T 5 laminectormy/ligation of dural AVF. Further skilled PT needed to improve pt’s level of IND and safety with funct mobility and ADLs.
PLAN • Pt to be seen as part of a interdisciplinary approach for 5 -7 days per weeks up to 3 hours/day in conjunction with all other discplines • Progress bed mob, transfers, strength, motor control/coordination, balance/postural control, WC mob, safety, conditioning/endurance, gait and stair training as tolerated
GOALS: • Pt GOAL: To walk again using FWW, return home with increased independence. • BED MOB: Mod I • TRANSFERS: • Sit to Stand: SBA • WC to/from Bed: Mod I via squat pivot and/or stand pivot and LRD • Car: SBA • WC: Mod I (150 ft+) on smooth, carpeted and 3% grade ramp • GAIT: 50 -149 ft w/ LRD SBA on level and carpeted surfaces • 10 ft or greater on uneven SBA • STAIRS: 4 -6 stairs w/ 2 rails step to gait and min A • BALANCE: Good static and fair+ dynamic
TREATMENT • Transfer training: • Sit to Stand- sequencing, hand placement, and motor control for smooth transition w/out vaulting • SPT with B/L platform walker • THER ACT/NEURO RE-ED: • • WB in stander Stepping to targets for improved accuracy and coordination Seated dynamic balance- balloon taps Lateral stepping in // bars to improve hip strength, weight shifting and balance • THER EX: • Standing and seated- focus on isolated control of hips/trunk • Ex- mini squats and bridges with focus on full hip ext
GAIT TRAINING • Progression: 3 -8’ in // bars to multiple length of parallel bars to 30’ w/ FWW on flat ground Mod A for balance (varied balance- CG to Mod) • Distance continued to improve through first couple of sessions, but ataxia/coordination and dysmetric steps did not show as much improvement • Until… Erin suggested trialing gait with 2. 5# cuff weights around ankles • Instant significant improvement in step length/accuracy, coordination and ataxia • Not other variables were adjusted, subsequent session with same results
D/C EVAL • Significant functional improvements from baseline during IRF stay • Not all D/C goals were met- high goals were set d/t pt familiarity with rehab process and repeat admit Dx. • Pt likely would have achieved these goals with longer stay, but improvements in bed mob, transfers, gait made quickly allowing safe d/c home and continued improvements with home PT.
Discussion- Ankle Weights during gait to improve proprioception, decrease ataxic gait • Not well supported in literature- Disproven vs Unproven? • Larger discussion- Research based practice vs Clinical Expertise/Experience
Where is this strategy most commonly used? • Peds in children with sensory processing disorders • Poor proprioception or sense of where there bodies are in space- these children are sensory seekers • Wearing weighted vests, hat, shorts, wrist or ankle weights provides that proprioceptive and tactile (deep pressure) input they’re searching for • Pt Case- Decreased LT and proprioception • Neuro Adult?
What does the literature say for external body weights for ataxia/tremor 1 • Controversial • Some studies show weighting limbs or axial skeleton controlled extraneous movements • Others shows similar intervention to have negative effects • Various Dx studied: Friedreich’s, MS, cerebellar degeneration, CVA, trauma, alcoholism, toxicity • Varying rationales given by researchers • Joint compression- increased sensory input facilitates cocontraction of muscles that leads to increased stability • Weights change center of mass based on area weights are placed • Weighting body part improves awareness of that part
Studies 2, 3 • 11/14 patients with ataxia showed gait improvement when weighted at waist and lower extremities 2 • One severely disabled subject not able to walk unless weighted • Optimum amount 1 -2 kg and position (trunk and/or extremities) • 2. Gait effects with weighting 10% BW on shoulders then at waist 3 • • Two subjects improved more with weight at shoulders Two subjects improved more with weight at waist One improved with both But overall, some showed just as much gait deterioration (i. e. increased double stance time, decreased velocity)
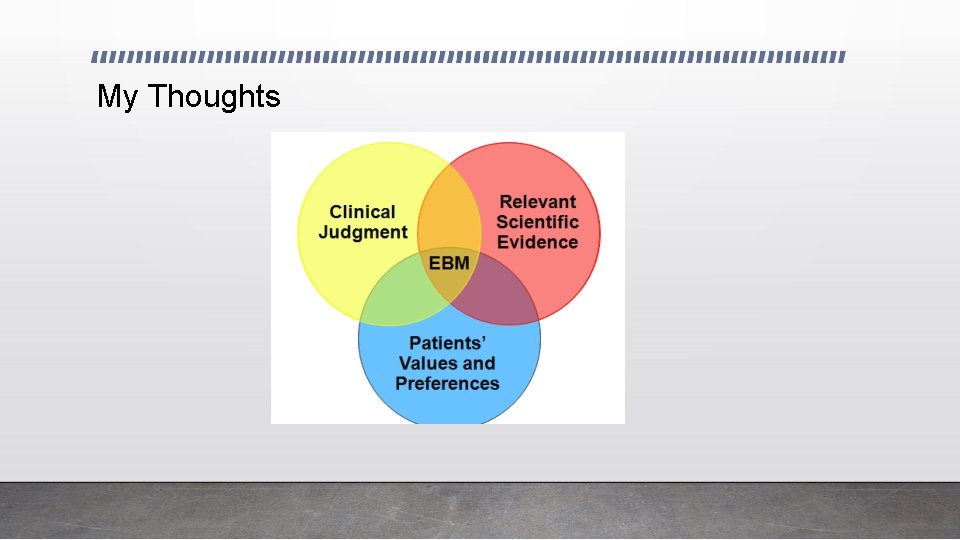
My Thoughts
Your thoughts?
Resources 1. Gibson-Horn C. Balance-based torso-weighting in a patient with ataxia and multiple sclerosis: a case report. Journal Of Neurologic Physical Therapy: JNPT [serial online]. September 2008; 32(3): 139 -146. Available from: MEDLINE, Ipswich, MA. Accessed May 2, 2017. 2. Morgan MH. Ataxia and weights. Physiotherapy. 1975; 61: 332– 334. 3. Clopton N, Schultz D, Boren C, et al. Effects of axial loading on gait forsubjects with cerebellar ataxia: preliminary findings. Neurol Rep. 2003; 27: 15– 21.
- Slides: 20