Case presentation Int 8831124 Chief complaint A 44


- Slides: 41

Case presentation Int. 8831124 顏志維
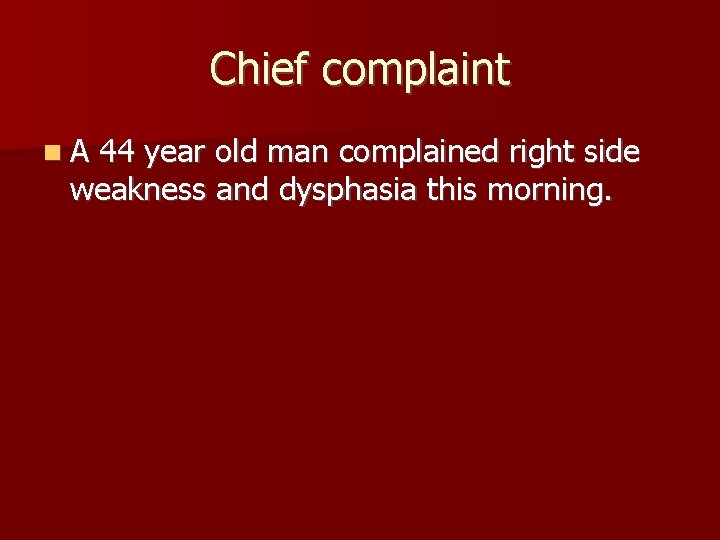
Chief complaint A 44 year old man complained right side weakness and dysphasia this morning.
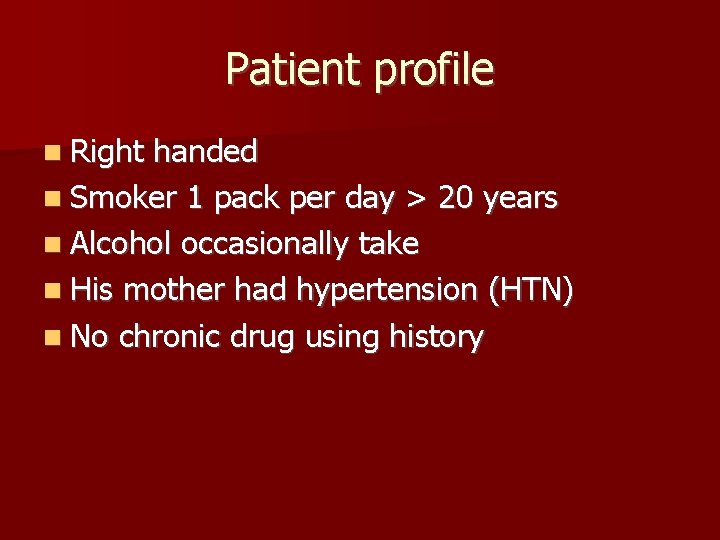
Patient profile Right handed Smoker 1 pack per day > 20 years Alcohol occasionally take His mother had hypertension (HTN) No chronic drug using history
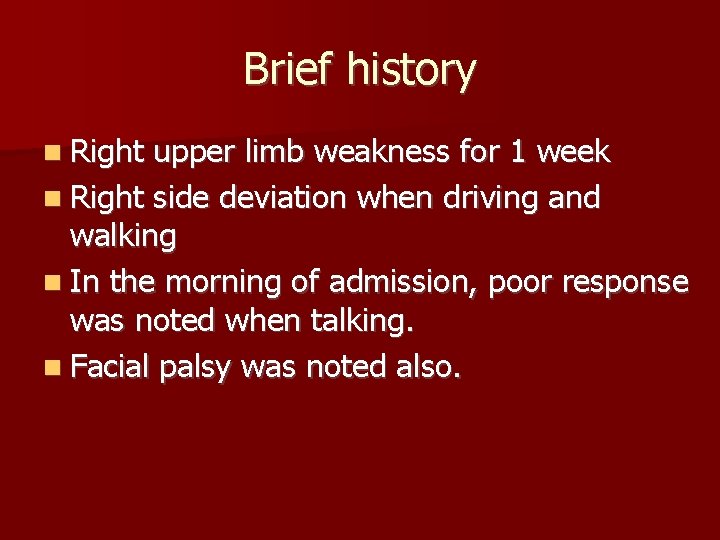
Brief history Right upper limb weakness for 1 week Right side deviation when driving and walking In the morning of admission, poor response was noted when talking. Facial palsy was noted also.
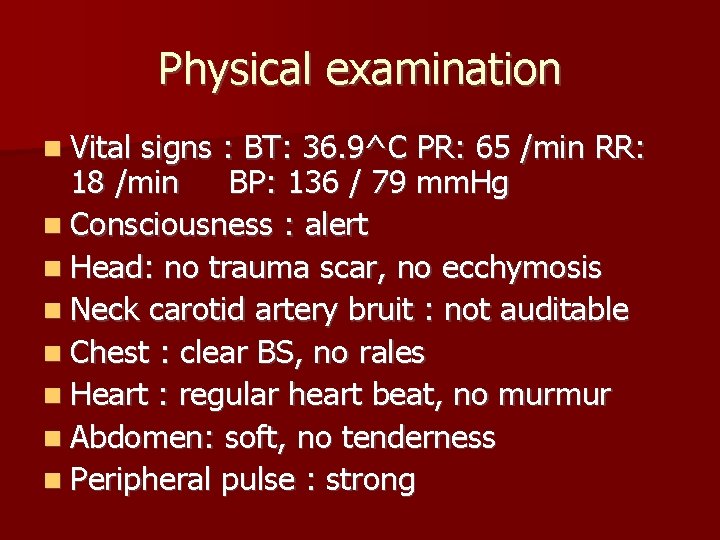
Physical examination Vital signs : BT: 36. 9^C PR: 65 /min RR: 18 /min BP: 136 / 79 mm. Hg Consciousness : alert Head: no trauma scar, no ecchymosis Neck carotid artery bruit : not auditable Chest : clear BS, no rales Heart : regular heart beat, no murmur Abdomen: soft, no tenderness Peripheral pulse : strong
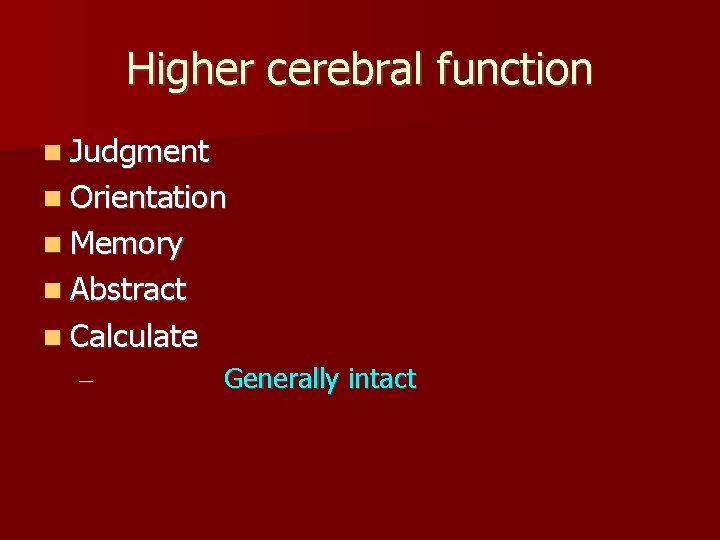
Higher cerebral function Judgment Orientation Memory Abstract Calculate – Generally intact
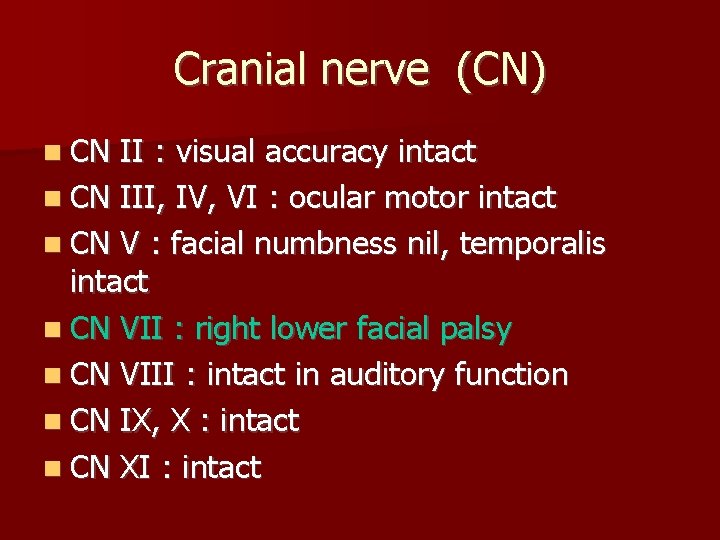
Cranial nerve (CN) CN II : visual accuracy intact CN III, IV, VI : ocular motor intact CN V : facial numbness nil, temporalis intact CN VII : right lower facial palsy CN VIII : intact in auditory function CN IX, X : intact CN XI : intact
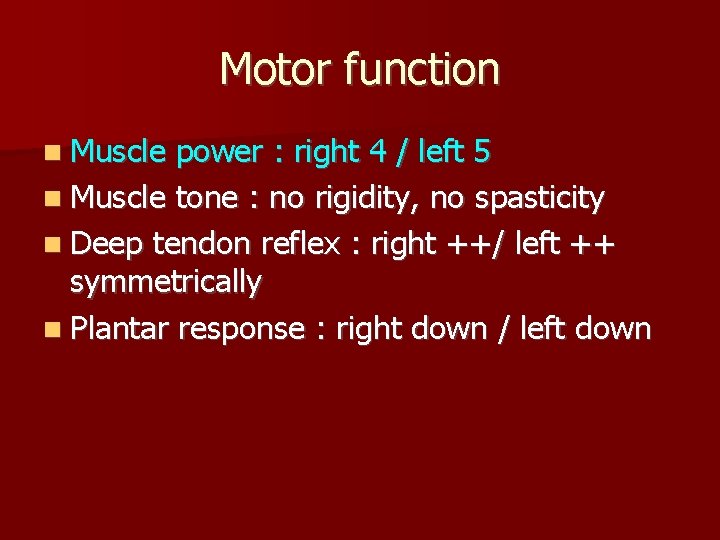
Motor function Muscle power : right 4 / left 5 Muscle tone : no rigidity, no spasticity Deep tendon reflex : right ++/ left ++ symmetrically Plantar response : right down / left down
Sensory function Generally intact
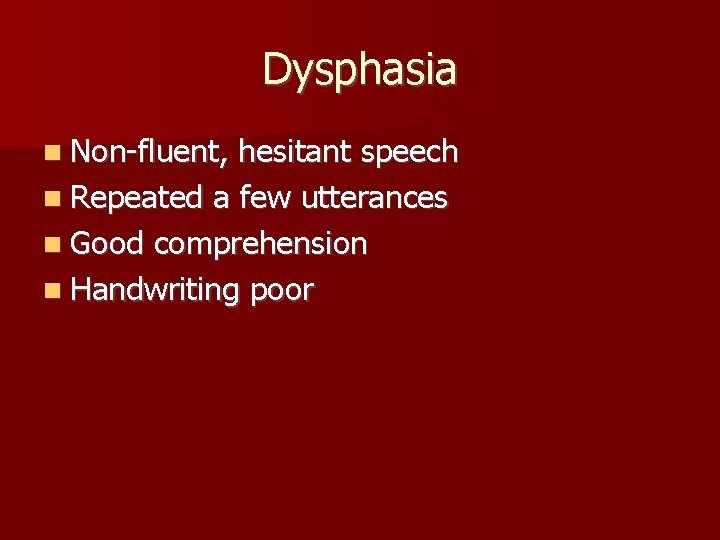
Dysphasia Non-fluent, hesitant speech Repeated a few utterances Good comprehension Handwriting poor
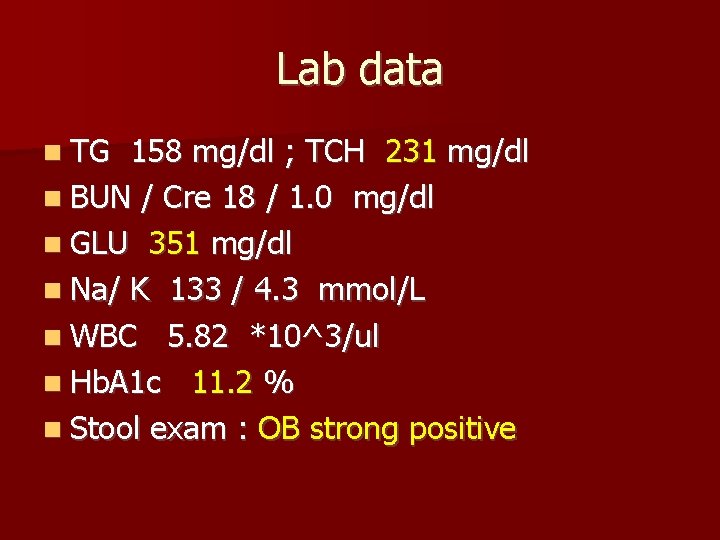
Lab data TG 158 mg/dl ; TCH 231 mg/dl BUN / Cre 18 / 1. 0 mg/dl GLU 351 mg/dl Na/ K 133 / 4. 3 mmol/L WBC 5. 82 *10^3/ul Hb. A 1 c 11. 2 % Stool exam : OB strong positive
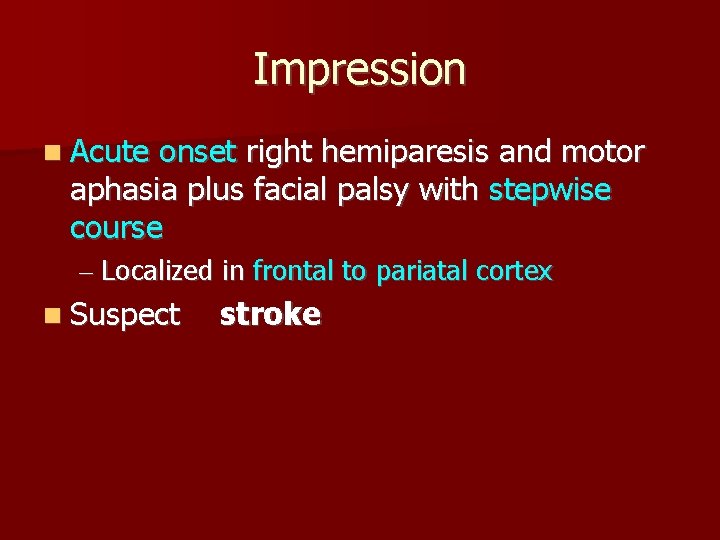
Impression Acute onset right hemiparesis and motor aphasia plus facial palsy with stepwise course – Localized in frontal to pariatal cortex Suspect stroke
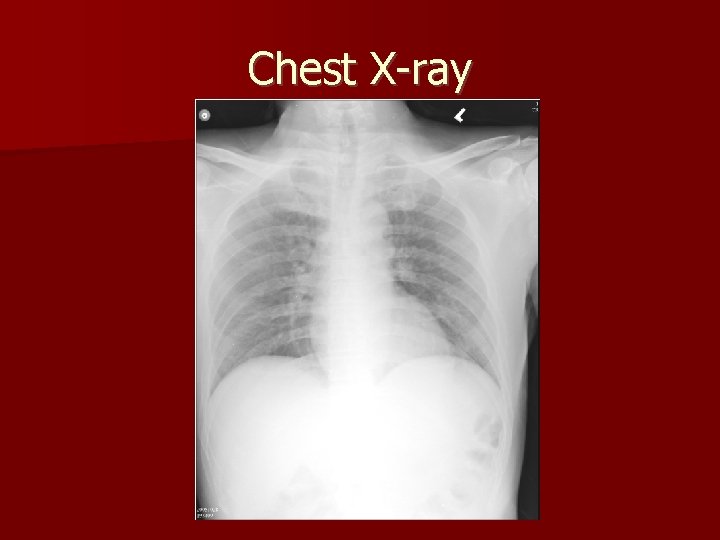
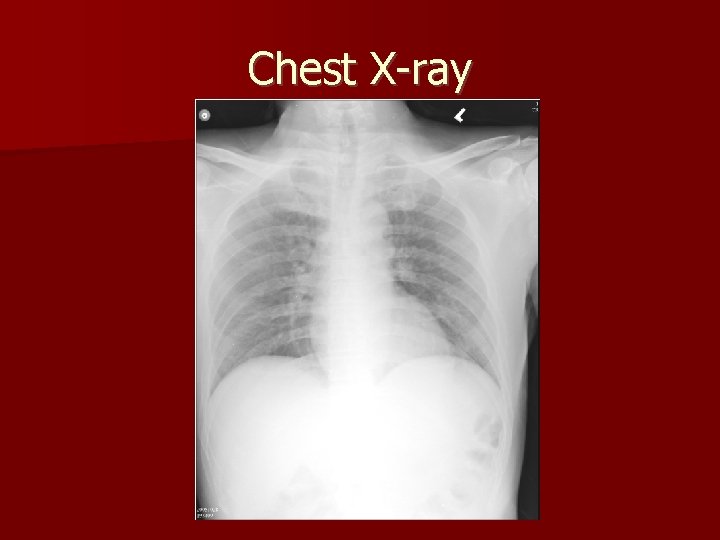
Chest X-ray
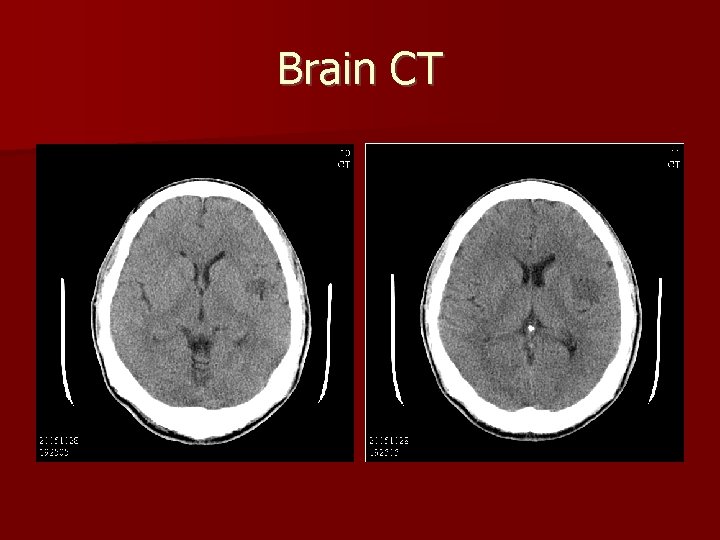
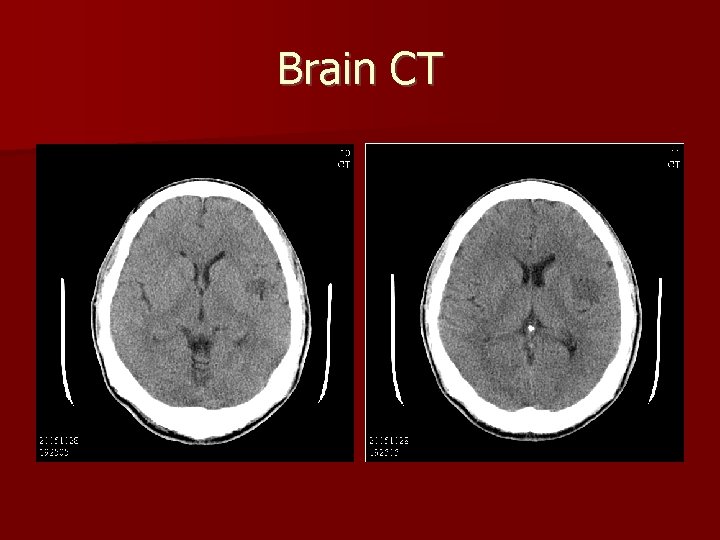
Brain CT
Transcranial Doppler, Carotid Duplex The carotid duplex study showed neither plaques nor tortuosity. The flow patterns were all normal. It implies normal study.
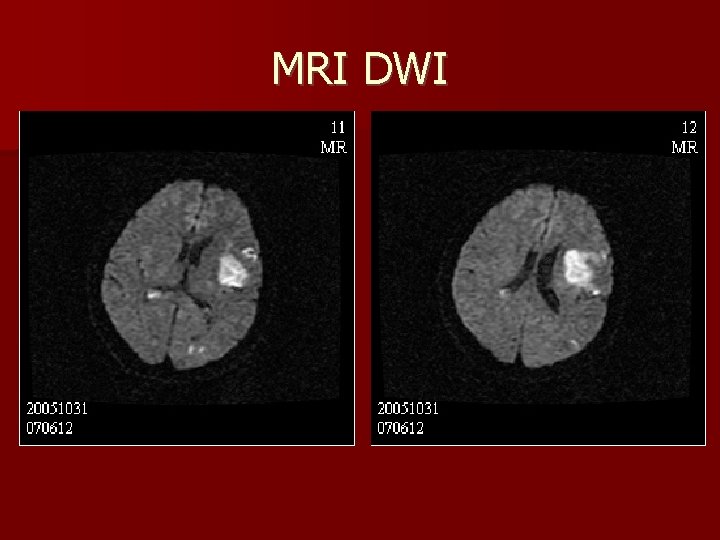
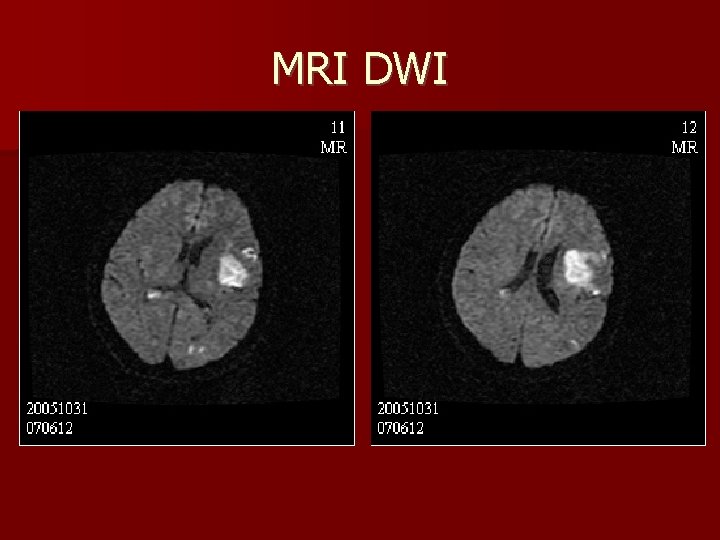
MRI DWI
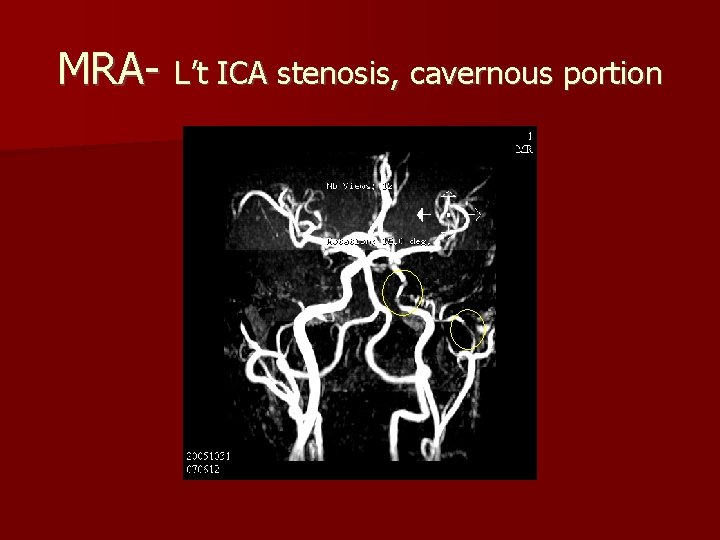
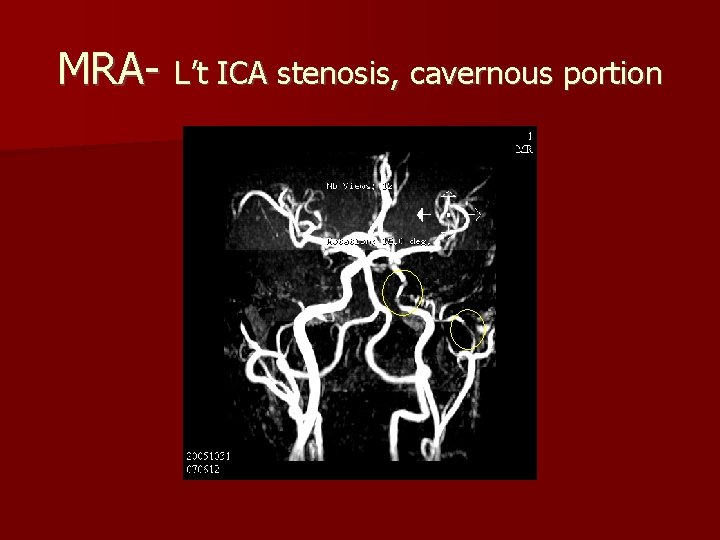
MRA- L’t ICA stenosis, cavernous portion
Diagnosis Neurological defect + image study proved -> cerebral infarction Diabetes Hyperlipidemia
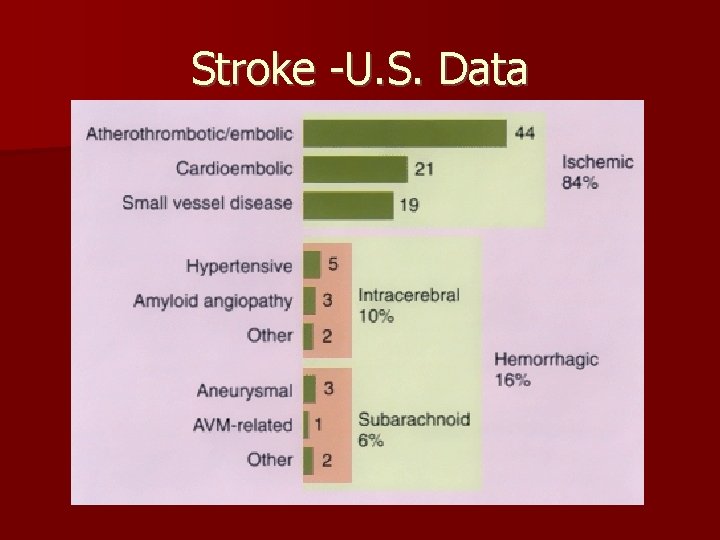
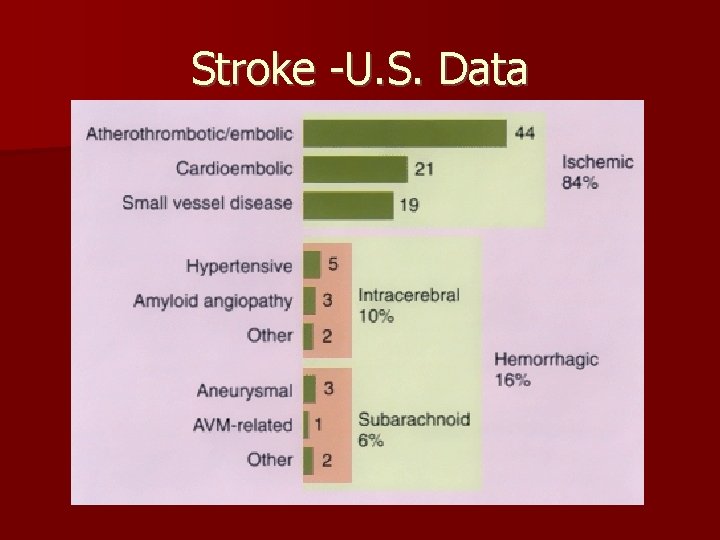
Stroke -U. S. Data
Management of acute stroke 1. prevent progress of present event 2. prevent immediate complications 3. prevent subsequent events 4. to rehabilitate the patient
As this patient Well known control diabetes and lipid What current treatment exist? What is the choice and their evidence?
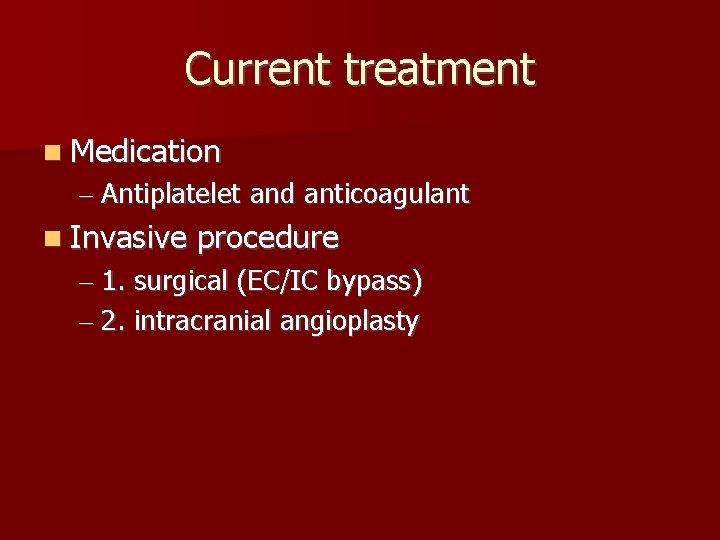
Current treatment Medication – Antiplatelet and anticoagulant Invasive procedure – 1. surgical (EC/IC bypass) – 2. intracranial angioplasty
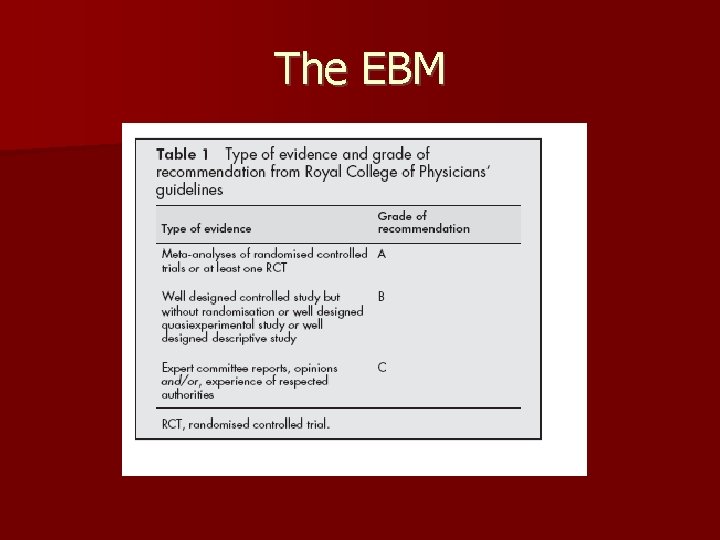
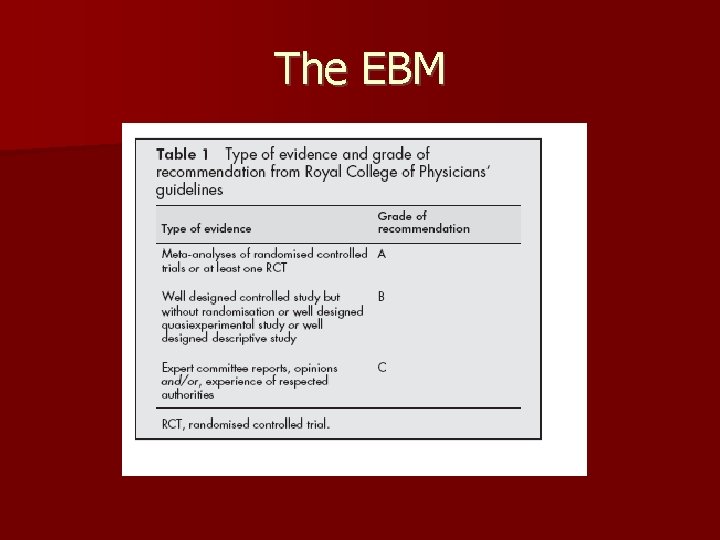
The EBM
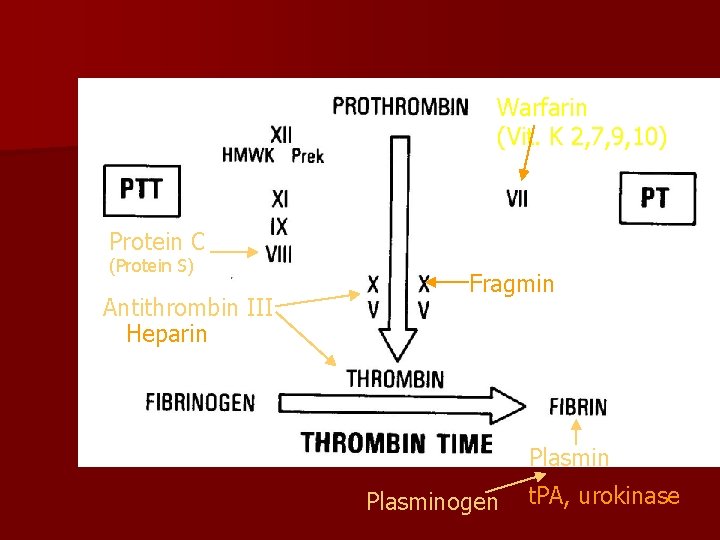
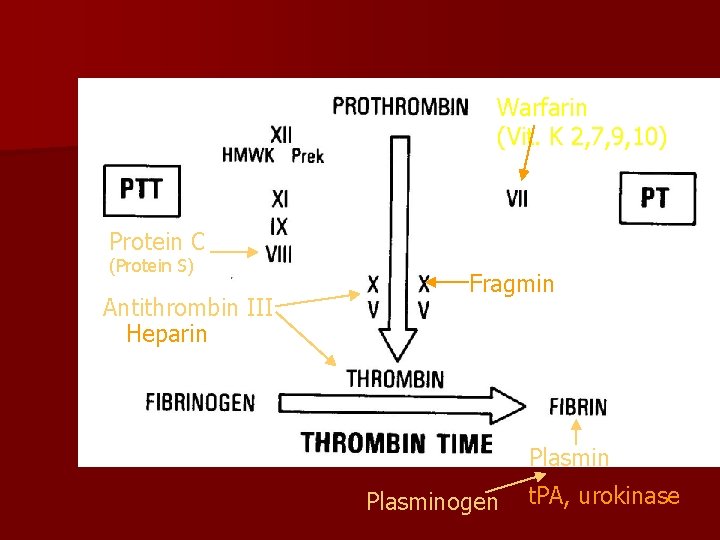
Warfarin (Vit. K 2, 7, 9, 10) Protein C (Protein S) Antithrombin III Heparin Fragmin Plasminogen t. PA, urokinase
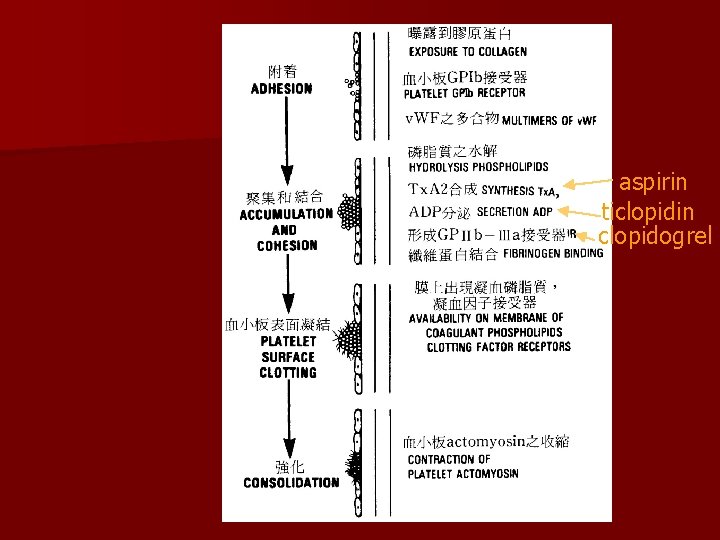
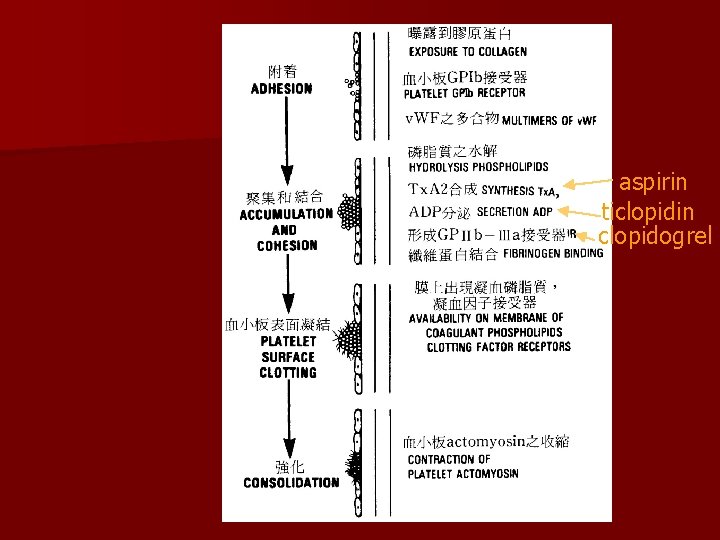
aspirin ticlopidin clopidogrel
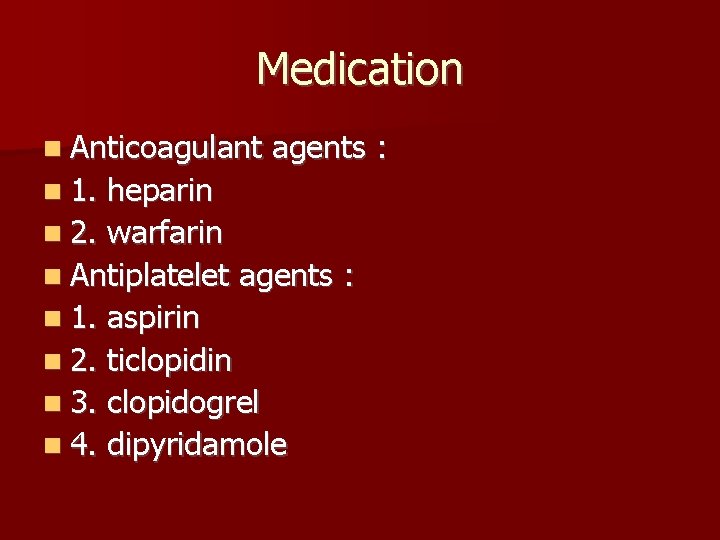
Medication Anticoagulant 1. agents : heparin 2. warfarin Antiplatelet agents : 1. aspirin 2. ticlopidin 3. clopidogrel 4. dipyridamole
Anticoagulant or antiplatelet ? Aspirin superior to warfarin in death rate, cardiac event and hemorrhagic rate. (grade A) The WASID Studies 2005 Mar. NEJM Clopidogrel was more effective than Aspirin in reducing the risk of ischaemic stroke, myocardial infarction, or vascular death. (grade A) The CAPRIE studies Lancet 1996 Nov.
Ticlopidine is not more effective than aspirin but increasing TTP, neutropenia, skin rash and diarrhea rate. (Grade A) – Stroke 2000
Dipyridamole and aspirin showed similar effect in reduction stroke risk (16% : 18%) and combination therapy showed more effective (37%) grade A ESPS 2. J Neurol Sci 1996
Medication conclusion Dipyridamole – Aspirin + Aspirin > Aspirin or treatment effective for prevent stroke > Ticlopidine Clopidogrel > Aspirin
Other specific therapies 1. Surgical Revascularization : EC/IC Bypass Trial (Extracranial to Intracranial). (grade A) 1377 patients 71 centers, 714 with medical control, while 663 receive STA-MCA bypass plus medication Failed to show definite benefit in this study – NEJM 1985.
Other specific therapies 2. Intracranial angioplasty and Stenting Use balloon Use stent Use balloon + stent Stroke rate and their risks
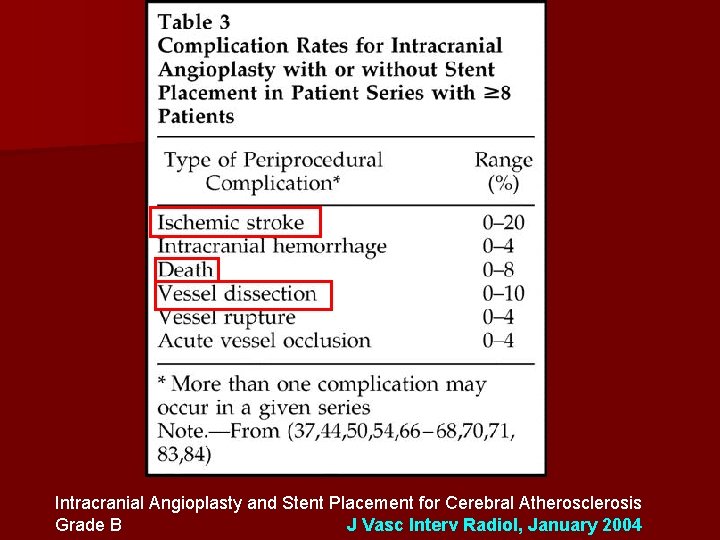
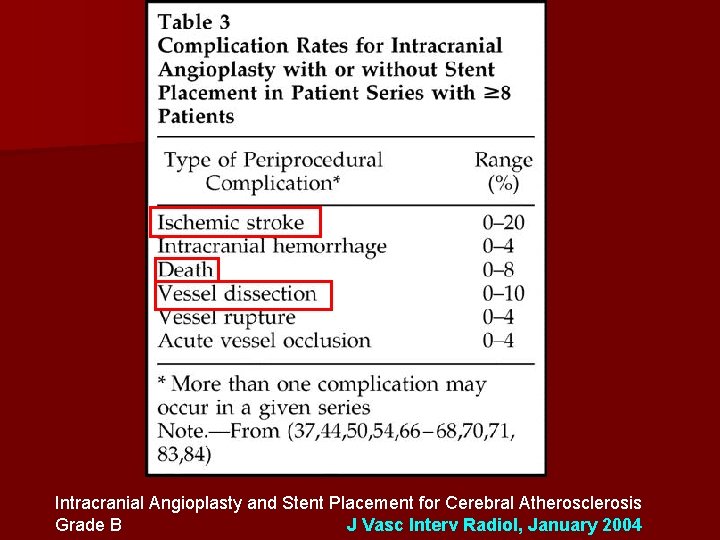
Intracranial Angioplasty and Stent Placement for Cerebral Atherosclerosis Grade B J Vasc Interv Radiol, January 2004
Angioplasty (grade C) Use balloon without stent : The peri-procedural death and stroke rate was 8. 3% The annual stroke rate was 3. 36% A residual stenosis of > or =50% it was 4. 5%. – American Journal of Neuroradiology, March 2005
SSYLVIA Trial (grade B) Stenting of SYmptomatic atherosclerotic Lesions in the Vertebral or Intracranial Arteries. Enrolled symptoms attributed to a single target lesion of > 50% stenosis 61 Pts Risk: peri-procedure mortality 0% Benefit: recurrent stroke 30 days after procedure 7. 3% – Stroke 2004
WINGSPAN Trial (grade B) Combination of balloon dilatation and microstent 15 patients Symptomatic with intracranial stenosis All patients were either stable or improved 4 weeks after the treatment. – The Wingspan Study. Neuroradiology 2004
WINGSPAN Trial (grade B) 2005 update to this study 45 medically refractory, >50% stenosis Pts Peri-procedure risk: stroke and death 4. 4% Benefit : 7. 1% six-month stroke and death rate.
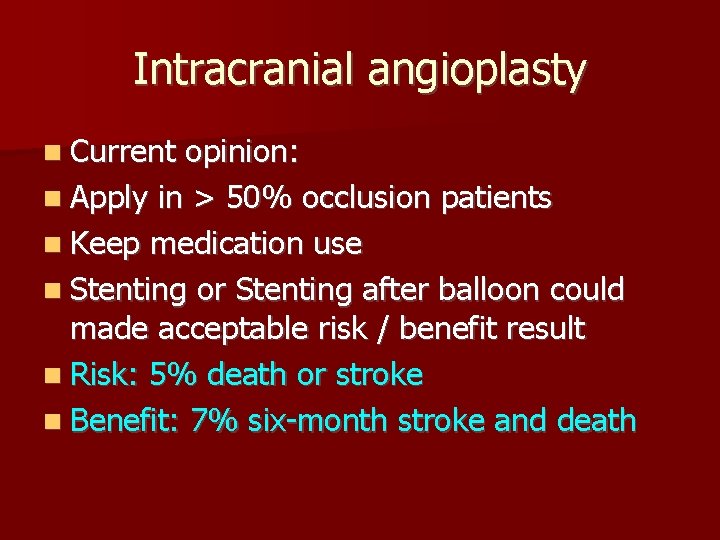
Intracranial angioplasty Current opinion: Apply in > 50% occlusion patients Keep medication use Stenting or Stenting after balloon could made acceptable risk / benefit result Risk: 5% death or stroke Benefit: 7% six-month stroke and death
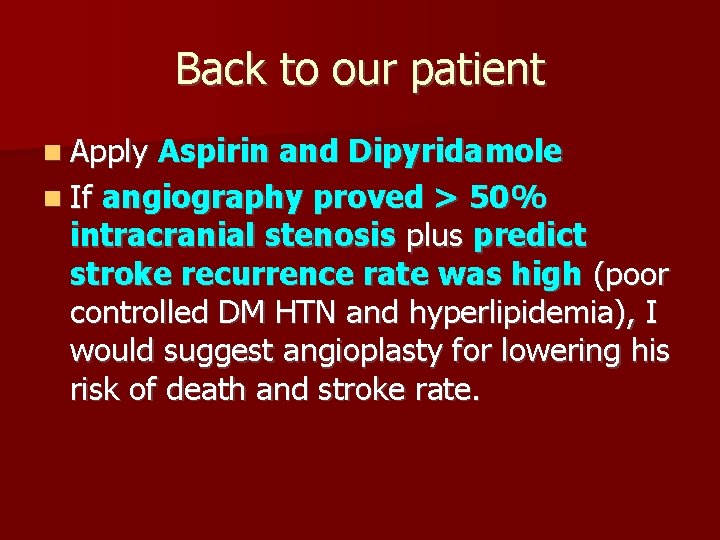
Back to our patient Apply Aspirin and Dipyridamole If angiography proved > 50% intracranial stenosis plus predict stroke recurrence rate was high (poor controlled DM HTN and hyperlipidemia), I would suggest angioplasty for lowering his risk of death and stroke rate.

Thanks a lot !