CASE of POSTINFARCT VSD History and Physical Exam




- Slides: 16

CASE of POST-INFARCT VSD
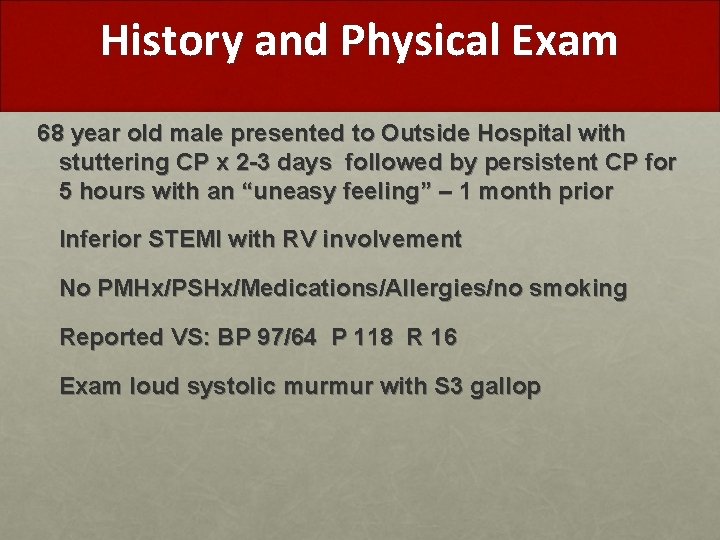
History and Physical Exam 68 year old male presented to Outside Hospital with stuttering CP x 2 -3 days followed by persistent CP for 5 hours with an “uneasy feeling” – 1 month prior Inferior STEMI with RV involvement No PMHx/PSHx/Medications/Allergies/no smoking Reported VS: BP 97/64 P 118 R 16 Exam loud systolic murmur with S 3 gallop
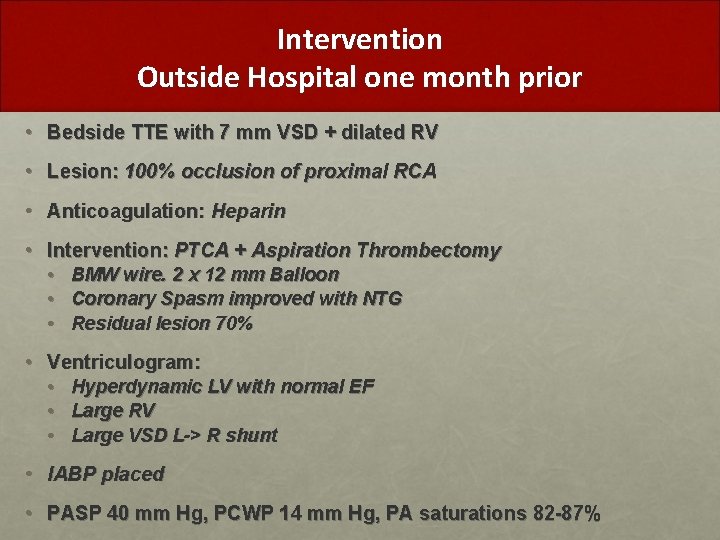
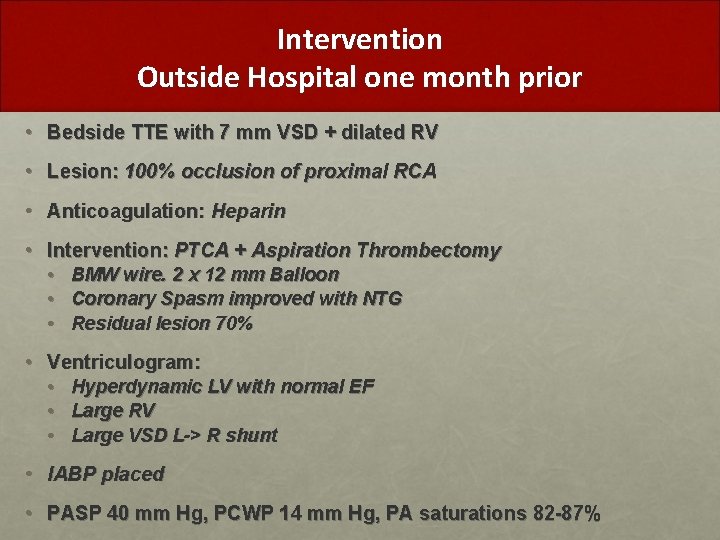
Intervention Outside Hospital one month prior • Bedside TTE with 7 mm VSD + dilated RV • Lesion: 100% occlusion of proximal RCA • Anticoagulation: Heparin • Intervention: PTCA + Aspiration Thrombectomy • BMW wire. 2 x 12 mm Balloon • Coronary Spasm improved with NTG • Residual lesion 70% • Ventriculogram: • Hyperdynamic LV with normal EF • Large RV • Large VSD L-> R shunt • IABP placed • PASP 40 mm Hg, PCWP 14 mm Hg, PA saturations 82 -87%
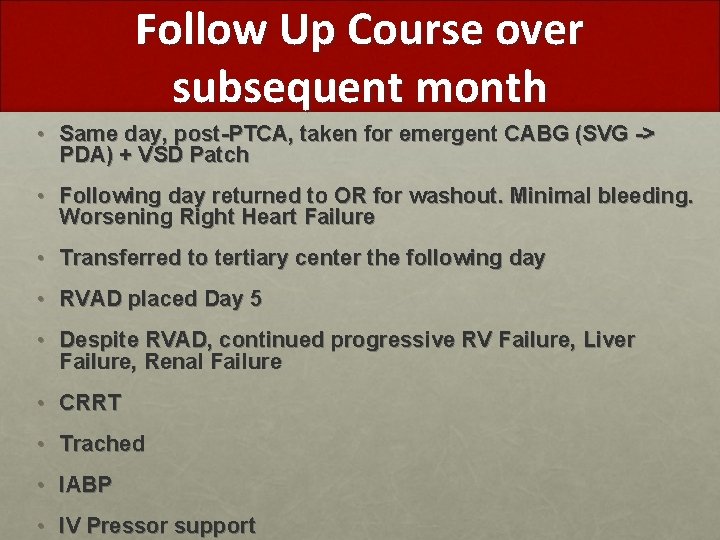
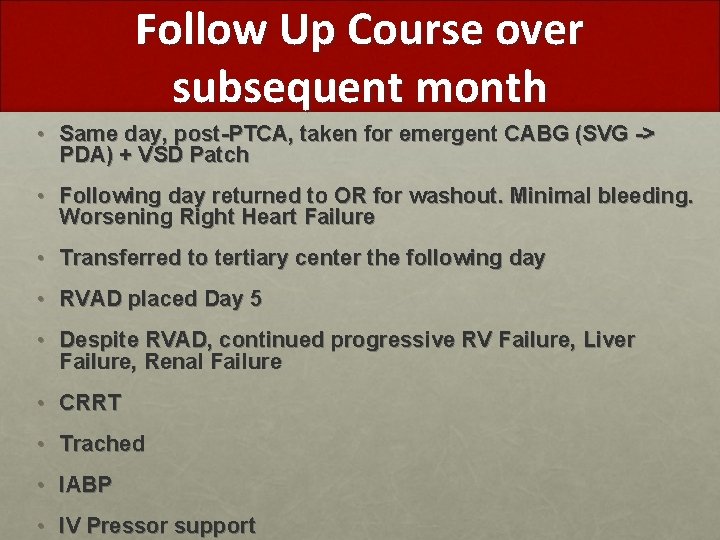
Follow Up Course over subsequent month • Same day, post-PTCA, taken for emergent CABG (SVG -> PDA) + VSD Patch • Following day returned to OR for washout. Minimal bleeding. Worsening Right Heart Failure • Transferred to tertiary center the following day • RVAD placed Day 5 • Despite RVAD, continued progressive RV Failure, Liver Failure, Renal Failure • CRRT • Trached • IABP • IV Pressor support
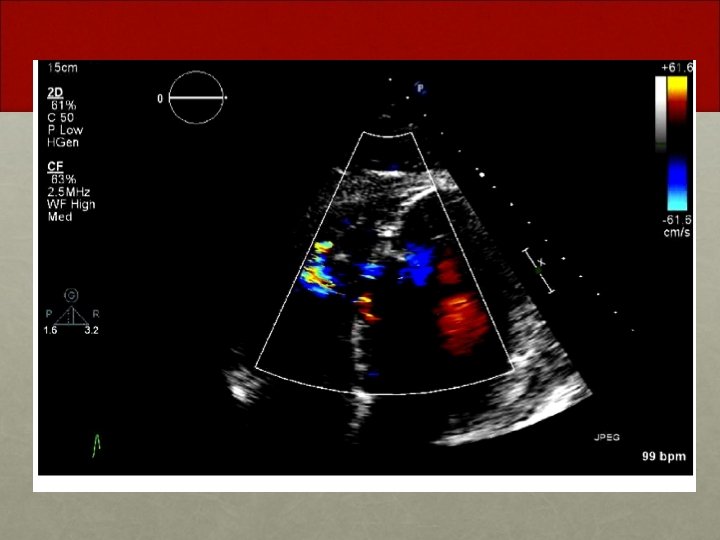
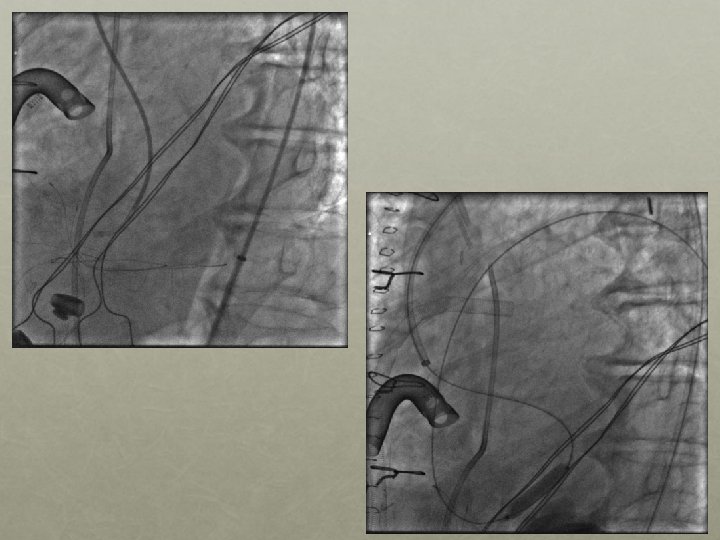
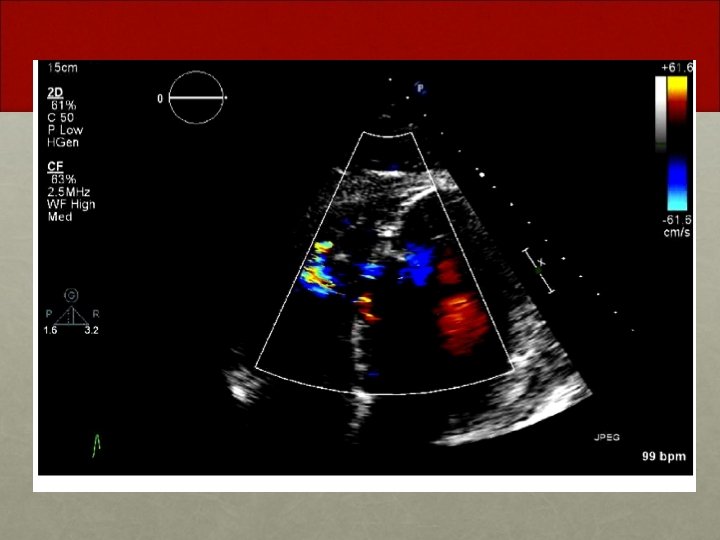
Follow Up One month later • Patient found to have residual VSD despite VSD patch repair post-infarct • Patient brought to the cardiac catheterization suite for possible percutaneous VSD closure

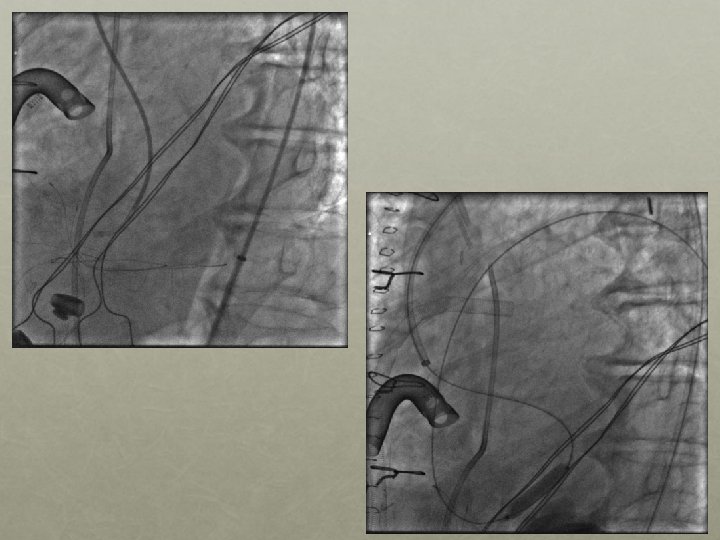
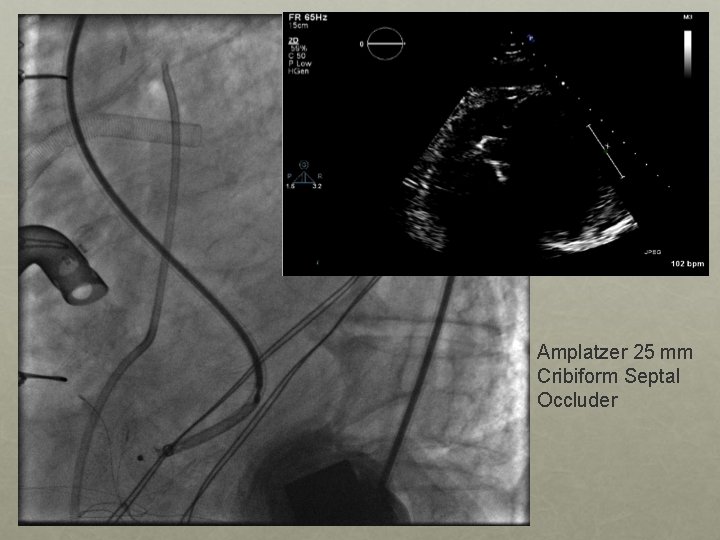
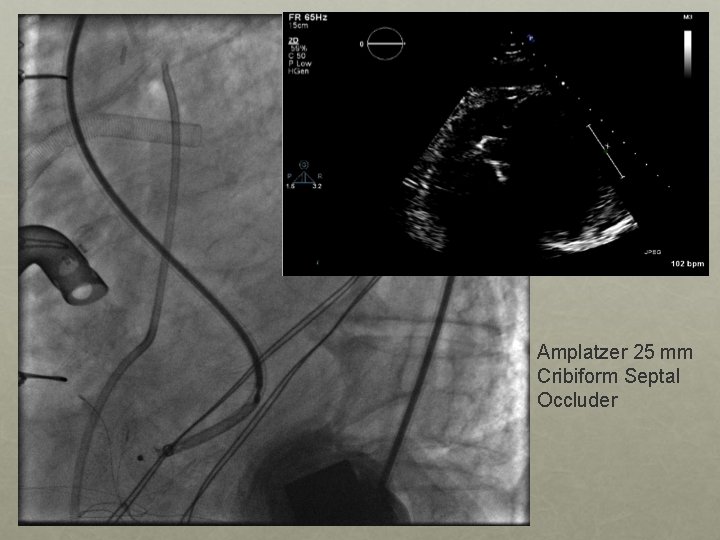
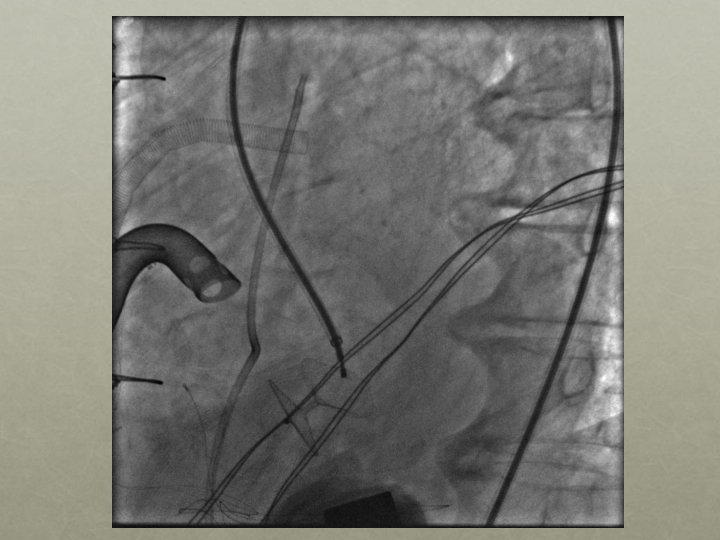
Amplatzer 25 mm Cribiform Septal Occluder
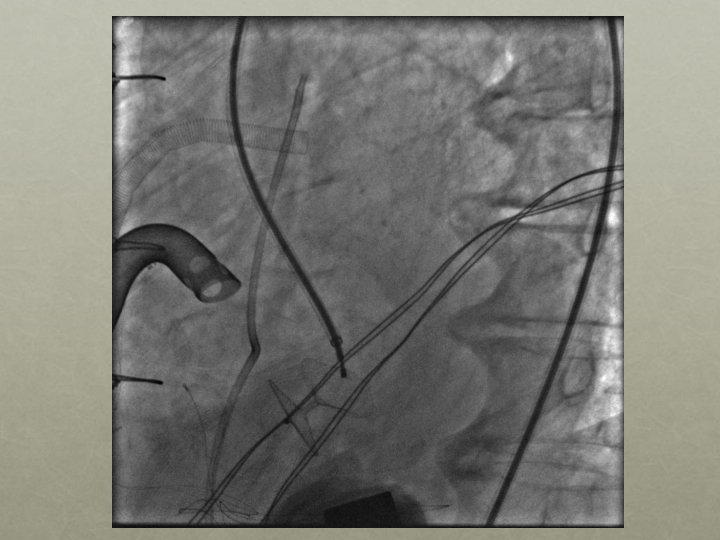

Significant Residual shunt

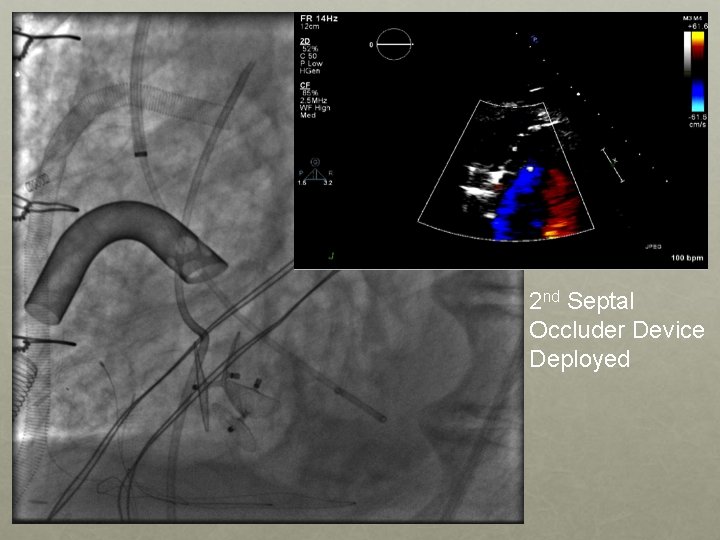
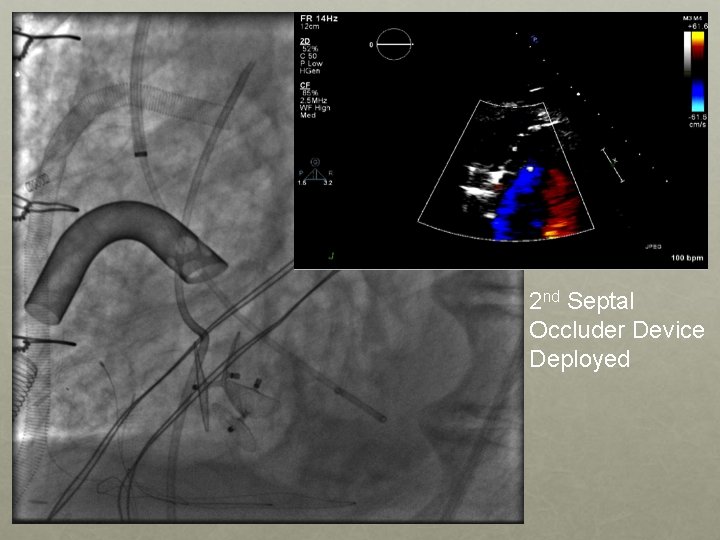
2 nd Septal Occluder Device Deployed
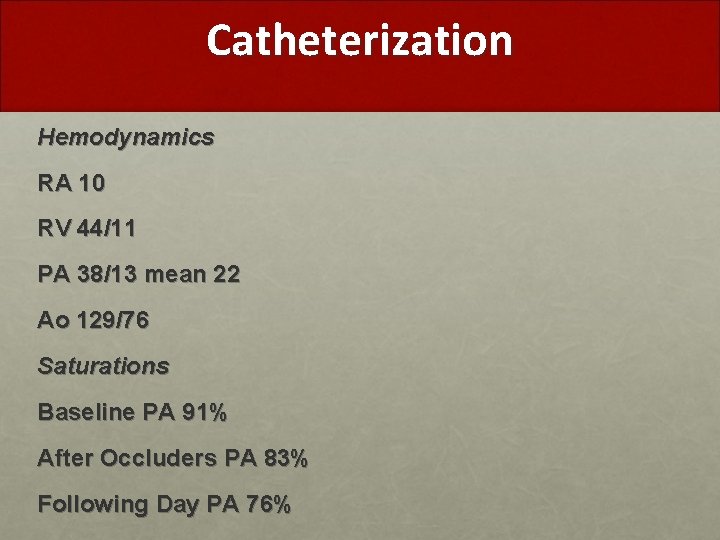
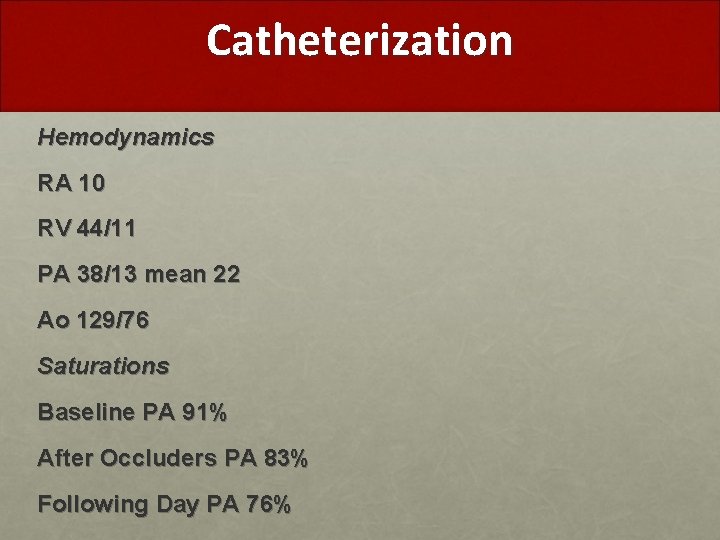
Catheterization Hemodynamics RA 10 RV 44/11 PA 38/13 mean 22 Ao 129/76 Saturations Baseline PA 91% After Occluders PA 83% Following Day PA 76%
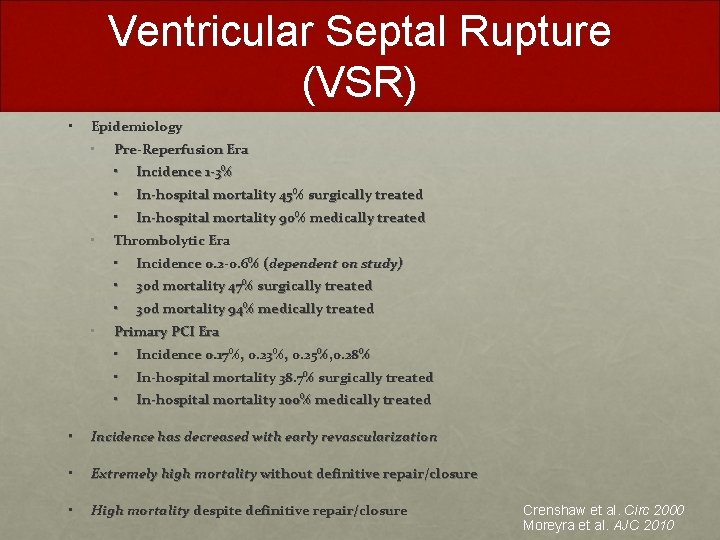
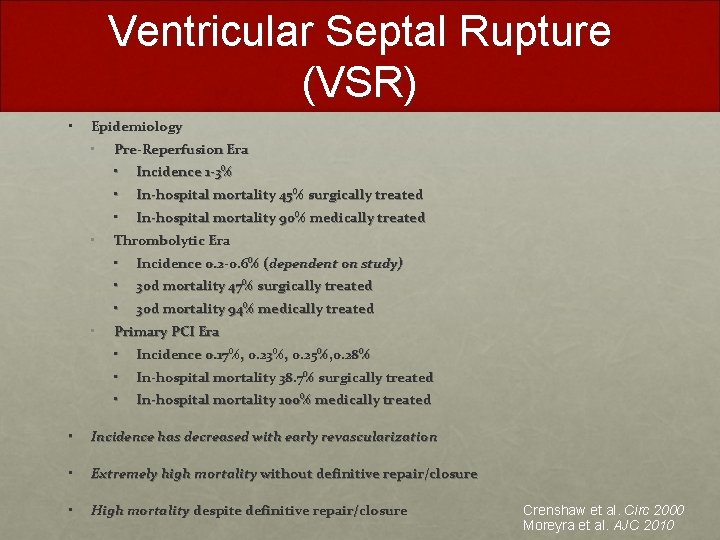
Ventricular Septal Rupture (VSR) • Epidemiology • • • Pre-Reperfusion Era • Incidence 1 -3% • In-hospital mortality 45% surgically treated • In-hospital mortality 90% medically treated Thrombolytic Era • Incidence 0. 2 -0. 6% (dependent on study) • 30 d mortality 47% surgically treated • 30 d mortality 94% medically treated Primary PCI Era • Incidence 0. 17%, 0. 23%, 0. 25%, 0. 28% • In-hospital mortality 38. 7% surgically treated • In-hospital mortality 100% medically treated • Incidence has decreased with early revascularization • Extremely high mortality without definitive repair/closure • High mortality despite definitive repair/closure Crenshaw et al. Circ 2000 Moreyra et al. AJC 2010
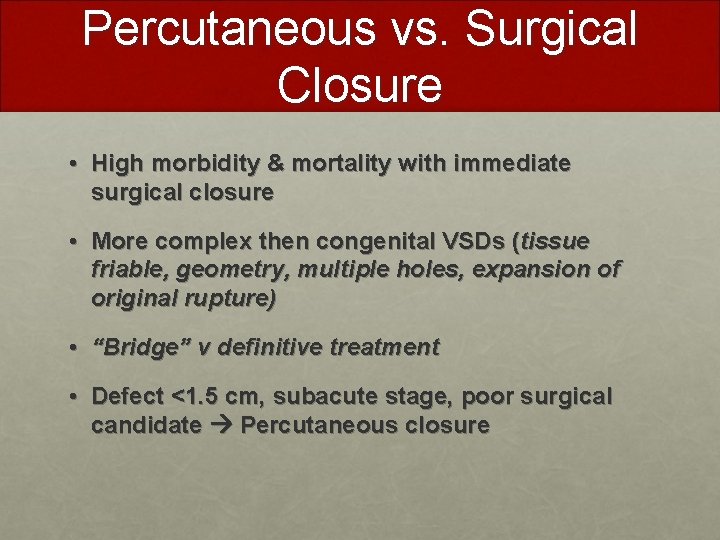
Percutaneous vs. Surgical Closure • High morbidity & mortality with immediate surgical closure • More complex then congenital VSDs (tissue friable, geometry, multiple holes, expansion of original rupture) • “Bridge” v definitive treatment • Defect <1. 5 cm, subacute stage, poor surgical candidate Percutaneous closure
 Vsd hjartagalli
Vsd hjartagalli Paramembranous vsd
Paramembranous vsd Type of vsd
Type of vsd 737 vsd
737 vsd Vitiumok
Vitiumok Vsd closure
Vsd closure Vsd
Vsd Vsd enterprise
Vsd enterprise Vsd uzantısı
Vsd uzantısı Best worst and average case
Best worst and average case History also history physical
History also history physical World geography spring final review
World geography spring final review Apwh course and exam description
Apwh course and exam description Gcse history past papers edexcel
Gcse history past papers edexcel Short case vs long case
Short case vs long case Binary search time complexity average case
Binary search time complexity average case Bubble sort best case and worst case
Bubble sort best case and worst case