Case Mix Reimbursement System Elements 1 Classification System
Case Mix Reimbursement System Elements 1. Classification System 2. Case Mix Weights 3. Reimbursement Methodology
Classification System • RUG-III Version 5. 12 34 Group Model – RUGs model currently has the highest predictor of nursing resource requirements – Utilizes the Minimum Data Set (MDS) 2. 0 • Mandated for use in all Medicaid and Medicare certified facilities • Data is readily available – Computer programs are available that determine RUG classification group • Classification group will be based on index maximization
Case Mix Weights • Standard version 5. 12 case mix indices developed by CMS • Nursing weights only • Case mix weight measures the nursing resource usage of one group vs. another
Case Mix Weights • Data Used by CMS: – 1995 -97 time study minutes – Wage rate factors (RN, LPN, Nurse Aide) – Distribution of residents across RUG classifications • Example calculation of case mix weights: – Uses the 1995 -97 time study minutes – Wage rate factors used • RN – 2. 0, LPN – 1. 5, Nurse Aide – 1. 0 – RUG classification distribution for all NF residents
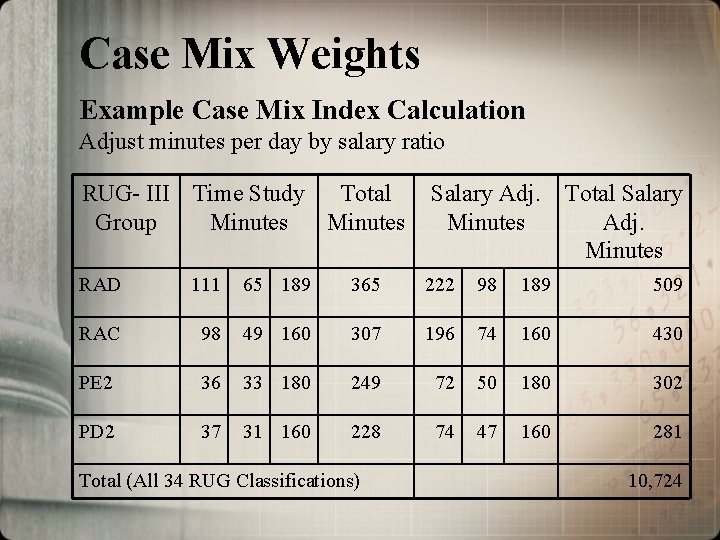
Case Mix Weights Example Case Mix Index Calculation Adjust minutes per day by salary ratio RUG- III Time Study Total Group Minutes Salary Adj. Minutes Total Salary Adj. Minutes RAD 111 65 189 365 222 98 189 509 RAC 98 49 160 307 196 74 160 430 PE 2 36 33 180 249 72 50 180 302 PD 2 37 31 160 228 74 47 160 281 Total (All 34 RUG Classifications) 10, 724

Case Mix Weights Example Case Mix Index Calculation Determine average adjusted salary minutes for nursing facility population and case mix weights RUG-III Group Total Minutes NF Residents Minutes x Residents 1995 -97 Calculated Weights CMS Standard Weights * RAD 509 163 82, 967 1. 83 1. 66 RAC 430 516 221, 880 1. 54 1. 31 PE 2 302 62 18, 724 1. 08 1. 00 PD 2 281 271 76, 151 1. 01 . 91 Total–All Groups Simple Average 10, 724 28, 402 7, 913, 826 28, 402 ¸ 278. 64 RAD Case Mix Weight 509 minutes / 278. 64 avg. minutes = 1. 83 * Standard version 5. 12 34 group weights developed by CMS will be used in LA
Reimbursement Methodology Effective January 1, 2003 Basic Elements 1. 2. Annual rate period from July 1 through June 30 Four cost centers a. b. c. d. 3. 4. 5. Administrative and operating – pricing methodology Direct care and care related – pricing methodology Capital – fair rental value methodology Pass through costs Base year cost report with bi-annual rebasing Cost reports with periods ending July 1, 2000 – June 30, 2001 will be used for initial base year Inflation factor based on skilled nursing facility market basket index
Reimbursement Methodology Effective January 1, 2003 Basic Elements 6. Direct care is case mix adjusted with quarterly rate adjustments for changes in facility-wide acuity 7. Direct care and care related spending floor 8. Adjustments to the rate a. Reflect changes in state/federal laws b. Budget adjustments 9. Current Medicaid SN, IC 1 and IC 2 payment systems will be combined and one rate will be paid
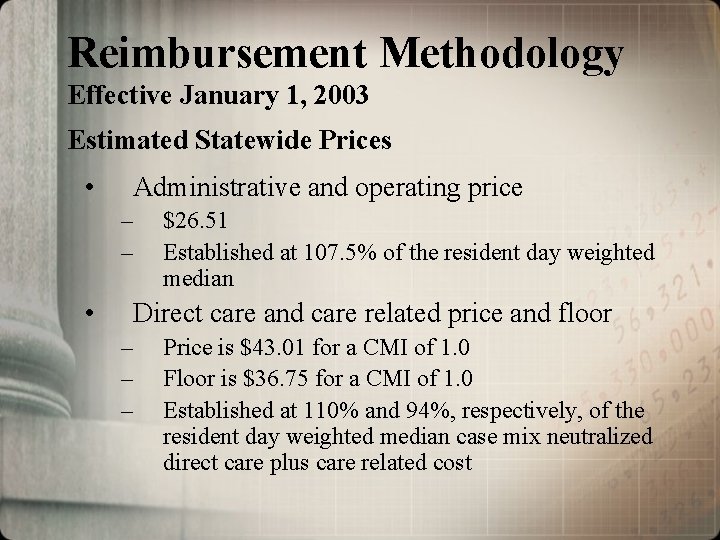
Reimbursement Methodology Effective January 1, 2003 Estimated Statewide Prices • Administrative and operating price – – • $26. 51 Established at 107. 5% of the resident day weighted median Direct care and care related price and floor – – – Price is $43. 01 for a CMI of 1. 0 Floor is $36. 75 for a CMI of 1. 0 Established at 110% and 94%, respectively, of the resident day weighted median case mix neutralized direct care plus care related cost
Administrative and Operating Cost Center • • • Administrative and general cost Plant operation and maintenance cost excluding capital cost Dietary cost excluding raw food cost Laundry and linen cost Housekeeping cost (See cross walk from existing cost report to the new case mix cost center categories)
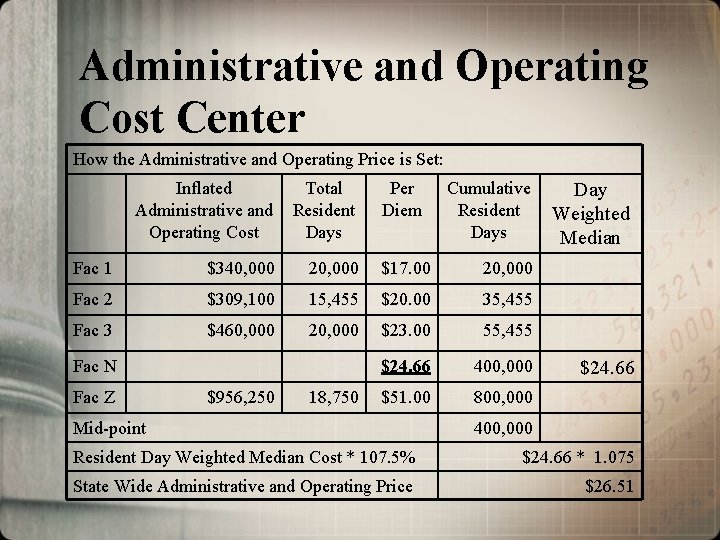
Administrative and Operating Cost Center How the Administrative and Operating Price is Set: Inflated Administrative and Operating Cost Total Resident Days Fac 1 $340, 000 20, 000 $17. 00 20, 000 Fac 2 $309, 100 15, 455 $20. 00 35, 455 Fac 3 $460, 000 20, 000 $23. 00 55, 455 $24. 66 400, 000 $51. 00 800, 000 Fac N Fac Z $956, 250 18, 750 Per Diem Mid-point Cumulative Resident Days Day Weighted Median $24. 66 400, 000 Resident Day Weighted Median Cost * 107. 5% $24. 66 * 1. 075 State Wide Administrative and Operating Price $26. 51
Direct Care and Care Related Cost Center • Direct care cost – case mix adjusted and includes the cost for direct care nursing staff (salaries, wages, benefits) – – Registered nurses Licensed practical nurses Nurse Aides Direct cost of acquiring RNs, LPNs and NAs from staffing companies
Direct Care and Care Related Cost Center • Care Related Costs – not case mix adjusted and, in general, includes allowable cost for: – Director of Nursing salary and benefits – Social service and activity salaries and benefits – Health care consultants (medical director, dietician) – Nursing, social services, activity supplies – Raw Food (See cross walk from existing cost report to the new case mix cost center categories)
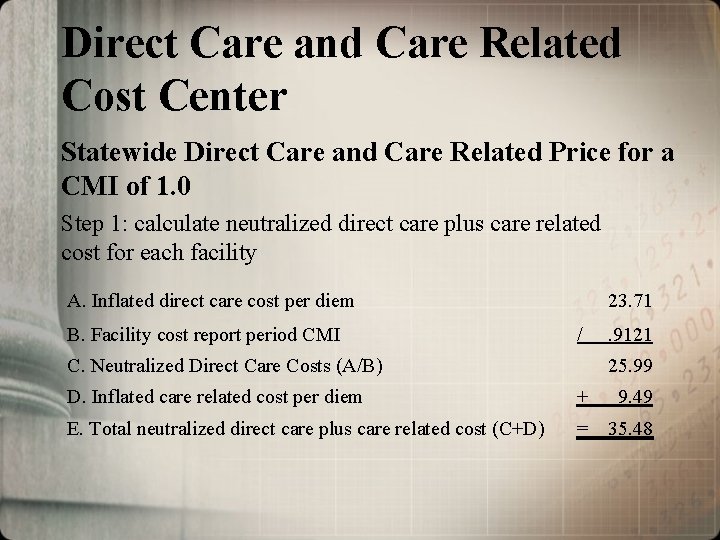
Direct Care and Care Related Cost Center Statewide Direct Care and Care Related Price for a CMI of 1. 0 Step 1: calculate neutralized direct care plus care related cost for each facility A. Inflated direct care cost per diem B. Facility cost report period CMI 23. 71 / C. Neutralized Direct Care Costs (A/B) . 9121 25. 99 D. Inflated care related cost per diem + 9. 49 E. Total neutralized direct care plus care related cost (C+D) = 35. 48
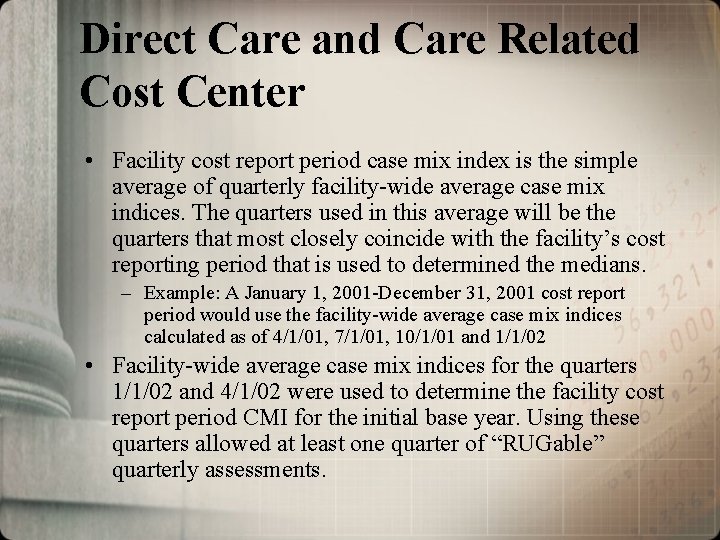
Direct Care and Care Related Cost Center • Facility cost report period case mix index is the simple average of quarterly facility-wide average case mix indices. The quarters used in this average will be the quarters that most closely coincide with the facility’s cost reporting period that is used to determined the medians. – Example: A January 1, 2001 -December 31, 2001 cost report period would use the facility-wide average case mix indices calculated as of 4/1/01, 7/1/01, 10/1/01 and 1/1/02 • Facility-wide average case mix indices for the quarters 1/1/02 and 4/1/02 were used to determine the facility cost report period CMI for the initial base year. Using these quarters allowed at least one quarter of “RUGable” quarterly assessments.
Direct Care and Care Related Cost Center Statewide Direct Care and Care Related Price for a CMI of 1. 0 Step 2: Determine resident day weighted median neutralized direct care plus care related cost Step 3: Multiply resident day weighted median by 110%
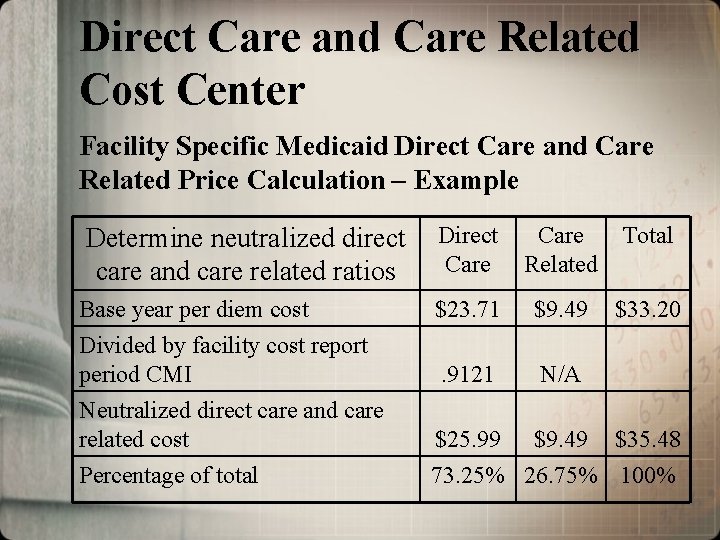
Direct Care and Care Related Cost Center Facility Specific Medicaid Direct Care and Care Related Price Calculation – Example Determine neutralized direct care and care related ratios Direct Care Related Total Base year per diem cost Divided by facility cost report period CMI $23. 71 $9. 49 $33. 20 . 9121 N/A Neutralized direct care and care related cost Percentage of total $25. 99 $9. 49 $35. 48 73. 25% 26. 75% 100%
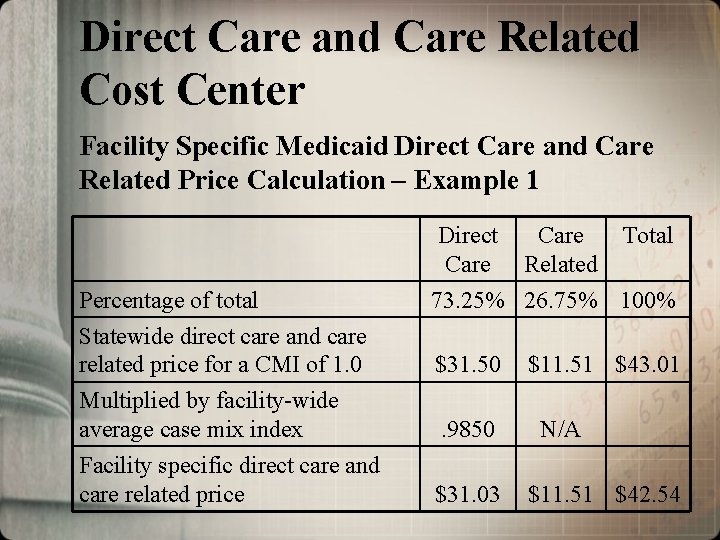
Direct Care and Care Related Cost Center Facility Specific Medicaid Direct Care and Care Related Price Calculation – Example 1 Direct Care Percentage of total Statewide direct care and care related price for a CMI of 1. 0 Multiplied by facility-wide average case mix index Facility specific direct care and care related price Care Related Total 73. 25% 26. 75% 100% $31. 50. 9850 $31. 03 $11. 51 $43. 01 N/A $11. 51 $42. 54
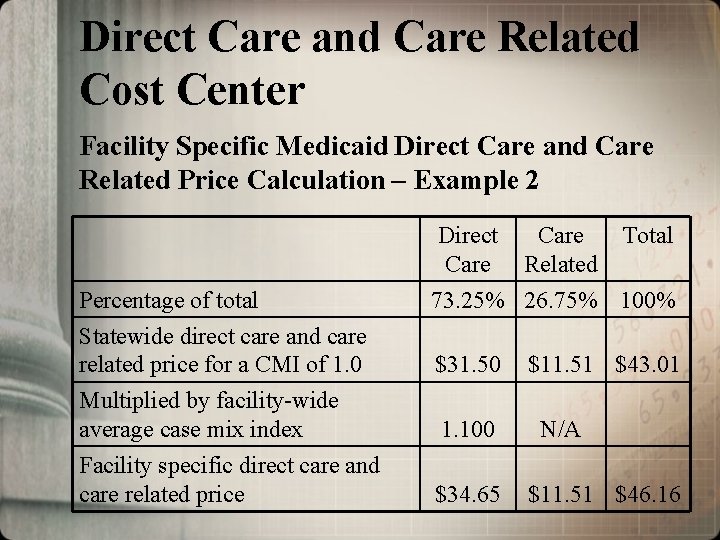
Direct Care and Care Related Cost Center Facility Specific Medicaid Direct Care and Care Related Price Calculation – Example 2 Direct Care Percentage of total Statewide direct care and care related price for a CMI of 1. 0 Multiplied by facility-wide average case mix index Facility specific direct care and care related price Care Related Total 73. 25% 26. 75% 100% $31. 50 1. 100 $34. 65 $11. 51 $43. 01 N/A $11. 51 $46. 16
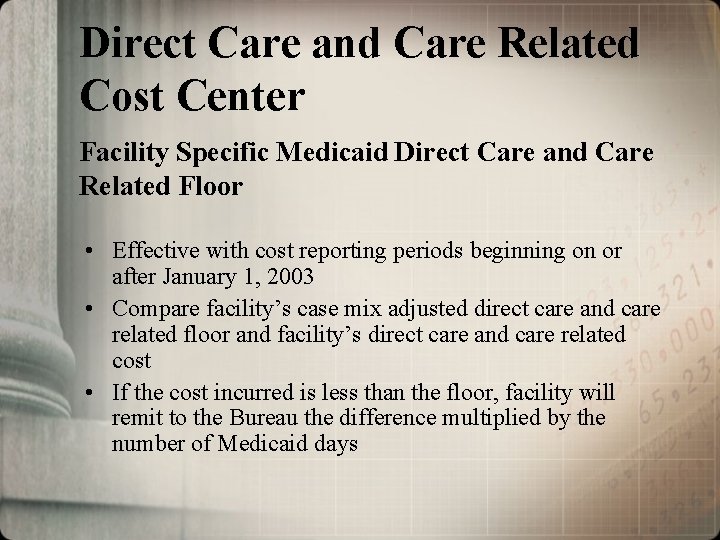
Direct Care and Care Related Cost Center Facility Specific Medicaid Direct Care and Care Related Floor • Effective with cost reporting periods beginning on or after January 1, 2003 • Compare facility’s case mix adjusted direct care and care related floor and facility’s direct care and care related cost • If the cost incurred is less than the floor, facility will remit to the Bureau the difference multiplied by the number of Medicaid days
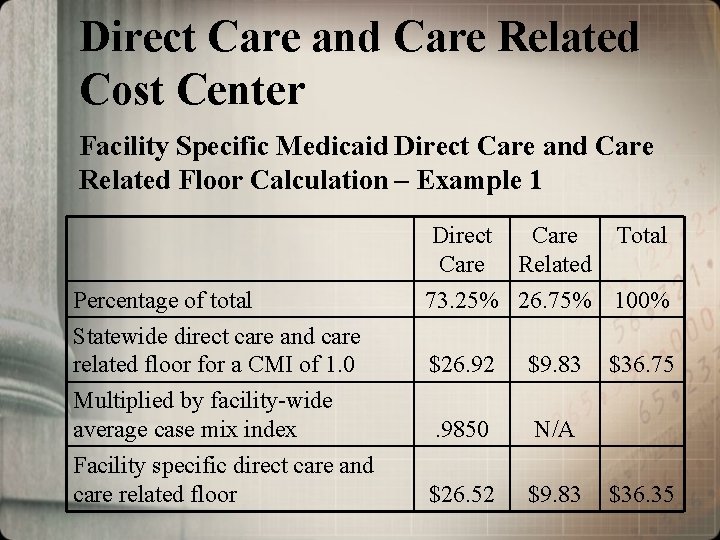
Direct Care and Care Related Cost Center Facility Specific Medicaid Direct Care and Care Related Floor Calculation – Example 1 Direct Care Percentage of total Statewide direct care and care related floor for a CMI of 1. 0 Multiplied by facility-wide average case mix index Facility specific direct care and care related floor Care Related Total 73. 25% 26. 75% 100% $26. 92 $9. 83 . 9850 N/A $26. 52 $9. 83 $36. 75 $36. 35
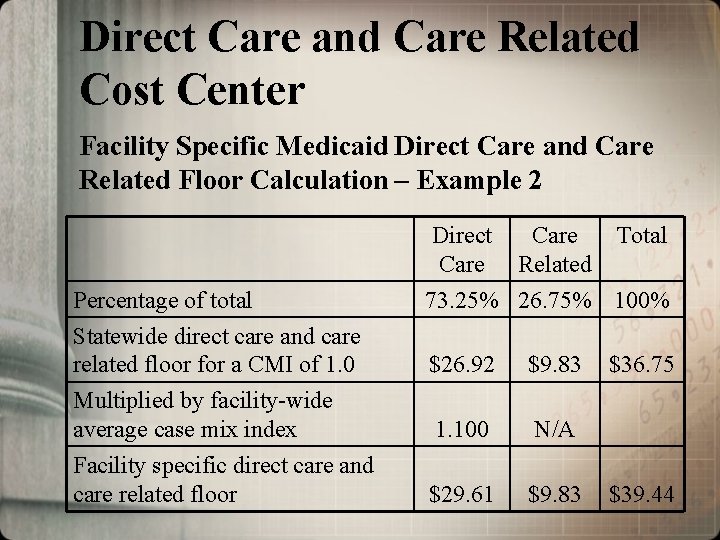
Direct Care and Care Related Cost Center Facility Specific Medicaid Direct Care and Care Related Floor Calculation – Example 2 Direct Care Percentage of total Statewide direct care and care related floor for a CMI of 1. 0 Multiplied by facility-wide average case mix index Facility specific direct care and care related floor Care Related Total 73. 25% 26. 75% 100% $26. 92 $9. 83 1. 100 N/A $29. 61 $9. 83 $36. 75 $39. 44
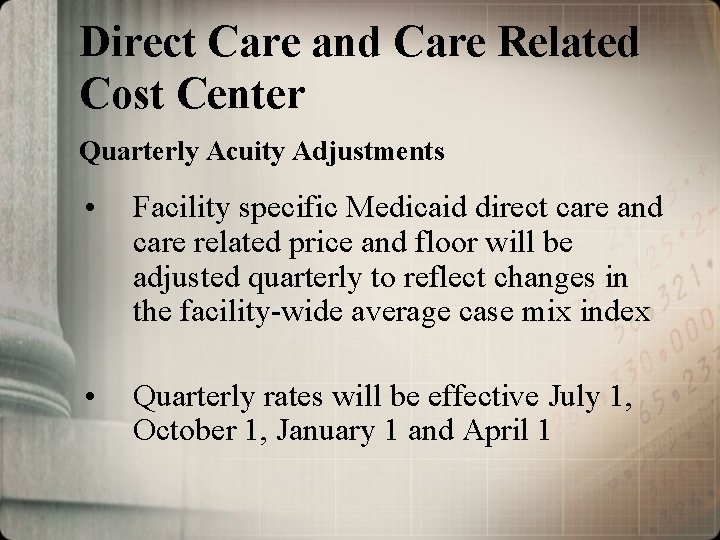
Direct Care and Care Related Cost Center Quarterly Acuity Adjustments • Facility specific Medicaid direct care and care related price and floor will be adjusted quarterly to reflect changes in the facility-wide average case mix index • Quarterly rates will be effective July 1, October 1, January 1 and April 1
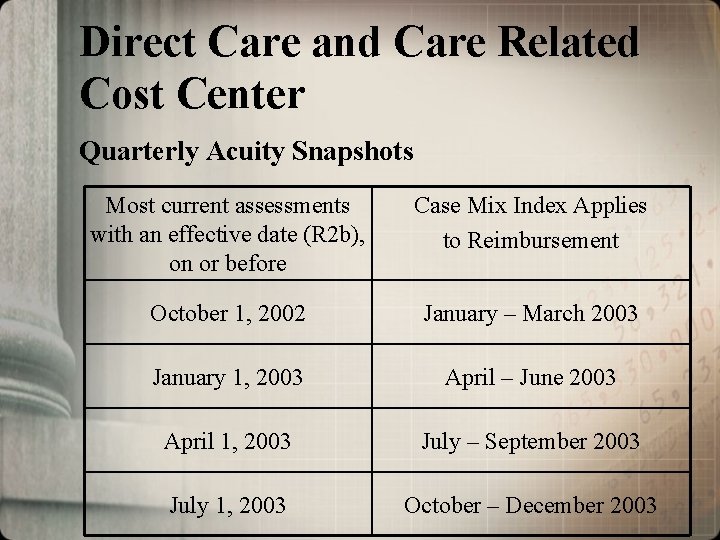
Direct Care and Care Related Cost Center Quarterly Acuity Snapshots Most current assessments with an effective date (R 2 b), on or before Case Mix Index Applies to Reimbursement October 1, 2002 January – March 2003 January 1, 2003 April – June 2003 April 1, 2003 July – September 2003 July 1, 2003 October – December 2003
Capital Cost Center • A fair rental value rate is paid in lieu of allowable depreciation, capital related interest, rent/lease and amortization expenses. • Fair rental value rate is based on the age and size of the facility
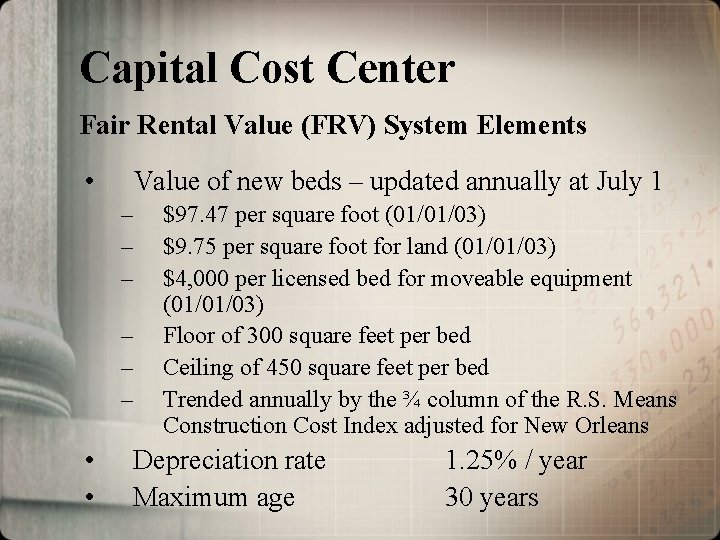
Capital Cost Center Fair Rental Value (FRV) System Elements • Value of new beds – updated annually at July 1 – – – • • $97. 47 per square foot (01/01/03) $9. 75 per square foot for land (01/01/03) $4, 000 per licensed bed for moveable equipment (01/01/03) Floor of 300 square feet per bed Ceiling of 450 square feet per bed Trended annually by the ¾ column of the R. S. Means Construction Cost Index adjusted for New Orleans Depreciation rate Maximum age 1. 25% / year 30 years
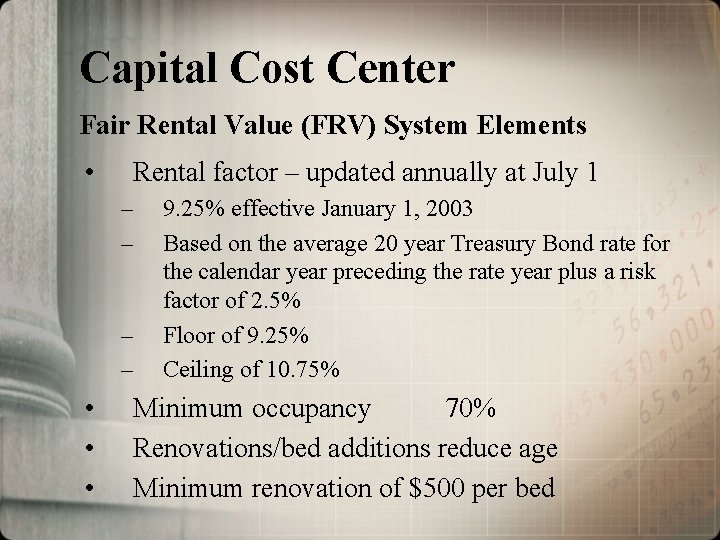
Capital Cost Center Fair Rental Value (FRV) System Elements • Rental factor – updated annually at July 1 – – • • • 9. 25% effective January 1, 2003 Based on the average 20 year Treasury Bond rate for the calendar year preceding the rate year plus a risk factor of 2. 5% Floor of 9. 25% Ceiling of 10. 75% Minimum occupancy 70% Renovations/bed additions reduce age Minimum renovation of $500 per bed
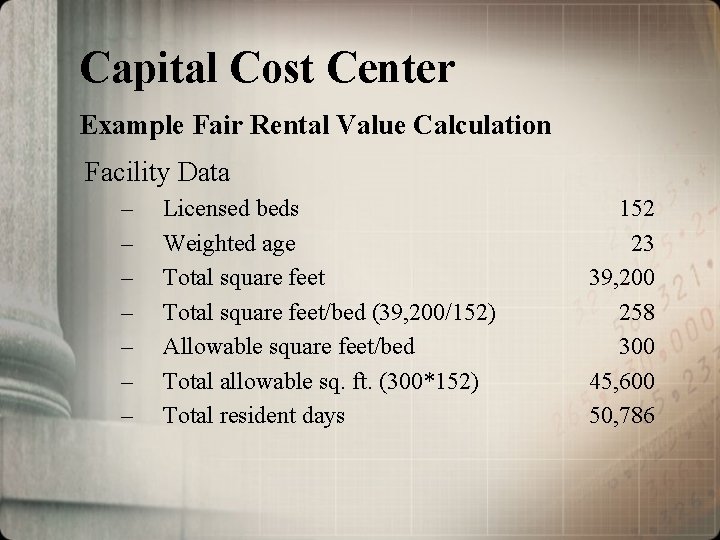
Capital Cost Center Example Fair Rental Value Calculation Facility Data – – – – Licensed beds Weighted age Total square feet/bed (39, 200/152) Allowable square feet/bed Total allowable sq. ft. (300*152) Total resident days 152 23 39, 200 258 300 45, 600 50, 786
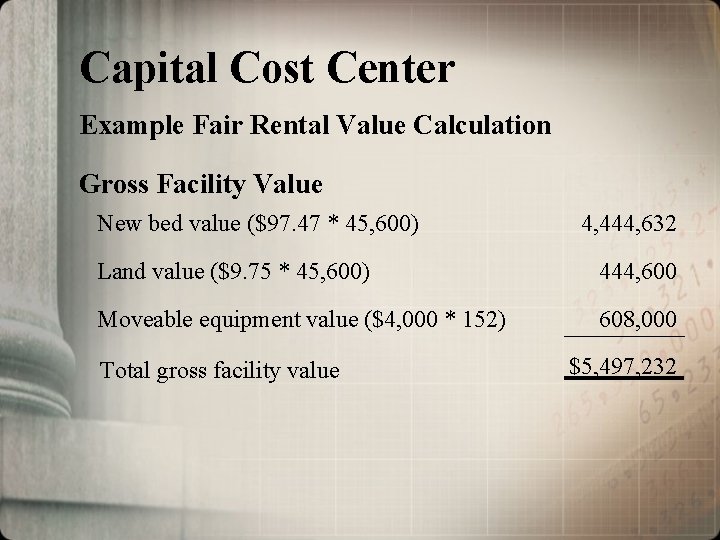
Capital Cost Center Example Fair Rental Value Calculation Gross Facility Value New bed value ($97. 47 * 45, 600) 4, 444, 632 Land value ($9. 75 * 45, 600) 444, 600 Moveable equipment value ($4, 000 * 152) 608, 000 Total gross facility value $5, 497, 232
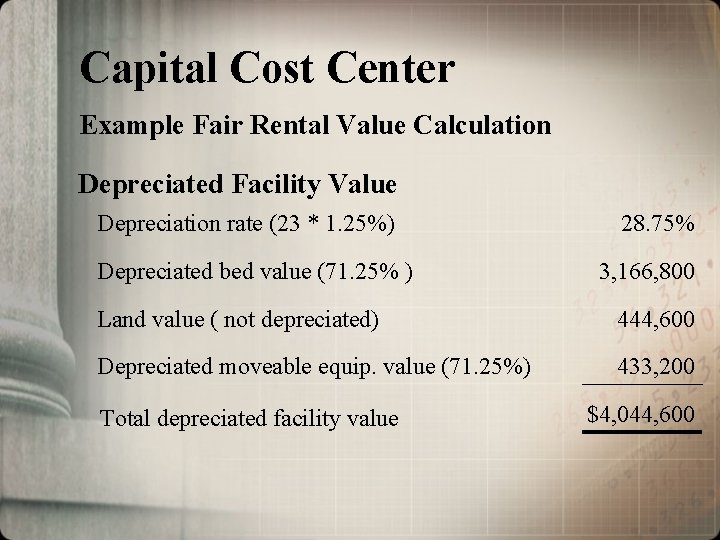
Capital Cost Center Example Fair Rental Value Calculation Depreciated Facility Value Depreciation rate (23 * 1. 25%) Depreciated bed value (71. 25% ) 28. 75% 3, 166, 800 Land value ( not depreciated) 444, 600 Depreciated moveable equip. value (71. 25%) 433, 200 Total depreciated facility value $4, 044, 600
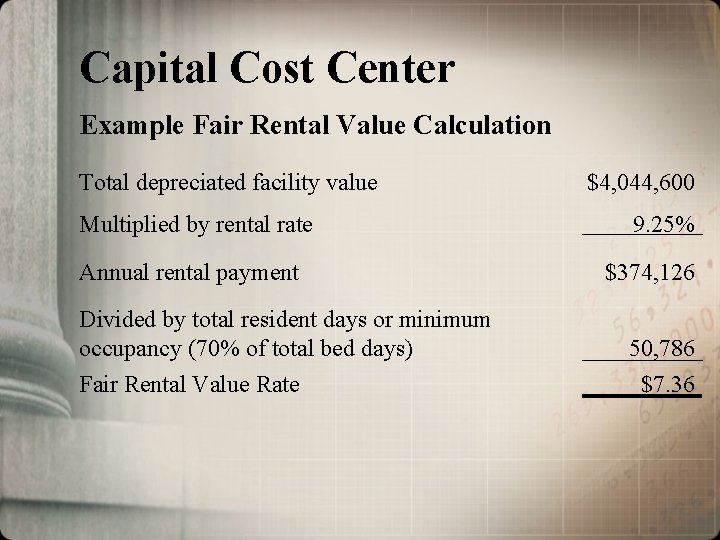
Capital Cost Center Example Fair Rental Value Calculation Total depreciated facility value Multiplied by rental rate Annual rental payment Divided by total resident days or minimum occupancy (70% of total bed days) Fair Rental Value Rate $4, 044, 600 9. 25% $374, 126 50, 786 $7. 36
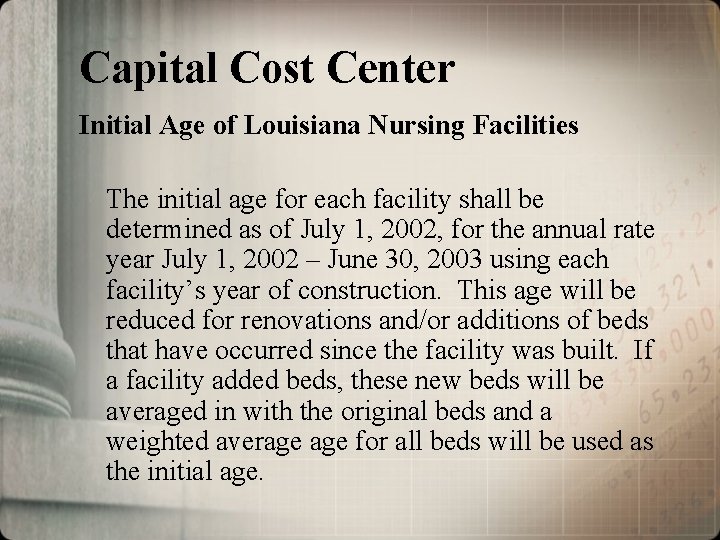
Capital Cost Center Initial Age of Louisiana Nursing Facilities The initial age for each facility shall be determined as of July 1, 2002, for the annual rate year July 1, 2002 – June 30, 2003 using each facility’s year of construction. This age will be reduced for renovations and/or additions of beds that have occurred since the facility was built. If a facility added beds, these new beds will be averaged in with the original beds and a weighted average for all beds will be used as the initial age.
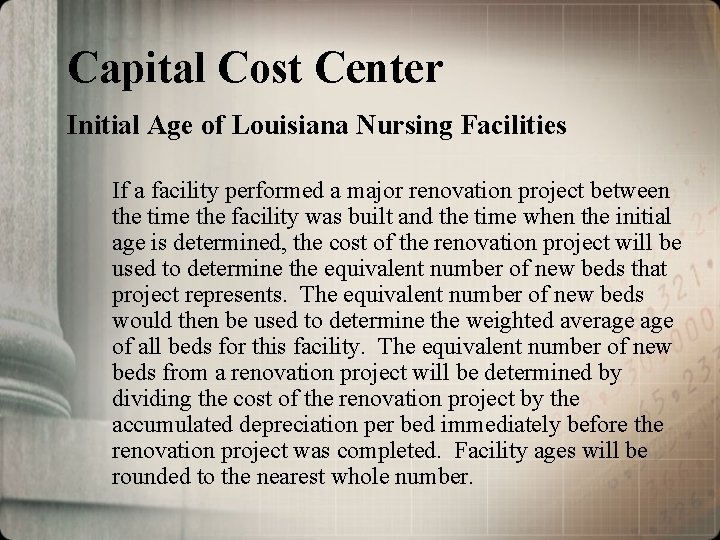
Capital Cost Center Initial Age of Louisiana Nursing Facilities If a facility performed a major renovation project between the time the facility was built and the time when the initial age is determined, the cost of the renovation project will be used to determine the equivalent number of new beds that project represents. The equivalent number of new beds would then be used to determine the weighted average of all beds for this facility. The equivalent number of new beds from a renovation project will be determined by dividing the cost of the renovation project by the accumulated depreciation per bed immediately before the renovation project was completed. Facility ages will be rounded to the nearest whole number.
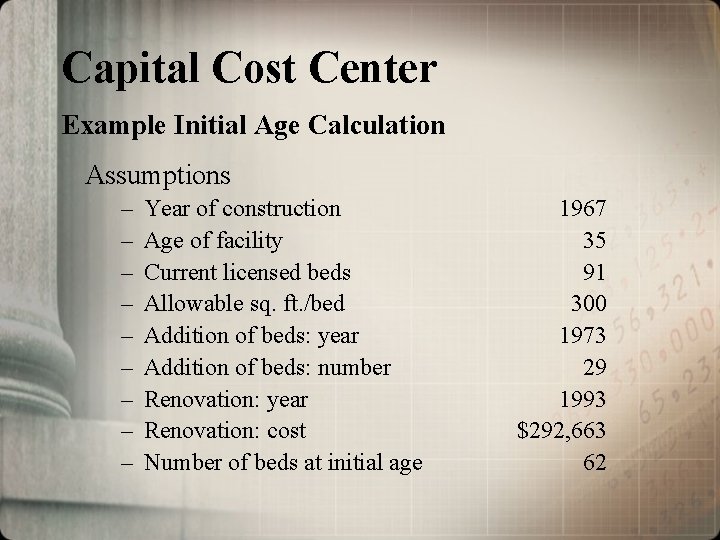
Capital Cost Center Example Initial Age Calculation Assumptions – – – – – Year of construction Age of facility Current licensed beds Allowable sq. ft. /bed Addition of beds: year Addition of beds: number Renovation: year Renovation: cost Number of beds at initial age 1967 35 91 300 1973 29 1993 $292, 663 62
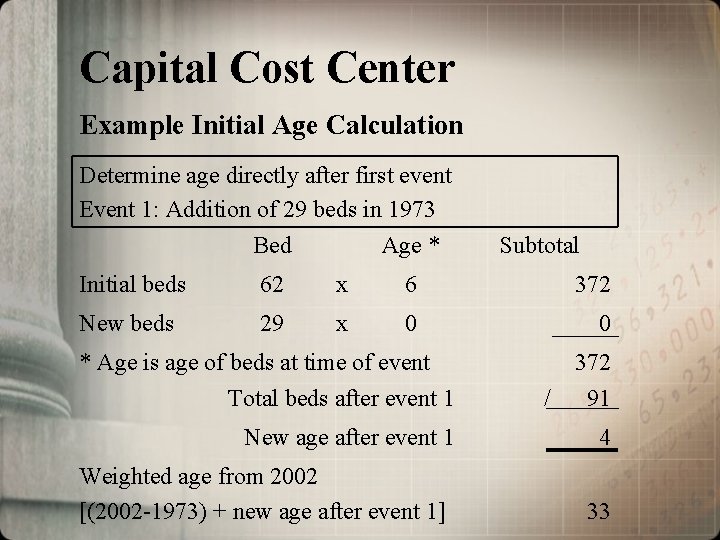
Capital Cost Center Example Initial Age Calculation Determine age directly after first event Event 1: Addition of 29 beds in 1973 Bed Age * Subtotal Initial beds 62 x 6 372 New beds 29 x 0 0 * Age is age of beds at time of event Total beds after event 1 New age after event 1 Weighted age from 2002 [(2002 -1973) + new age after event 1] / 372 91 4 33
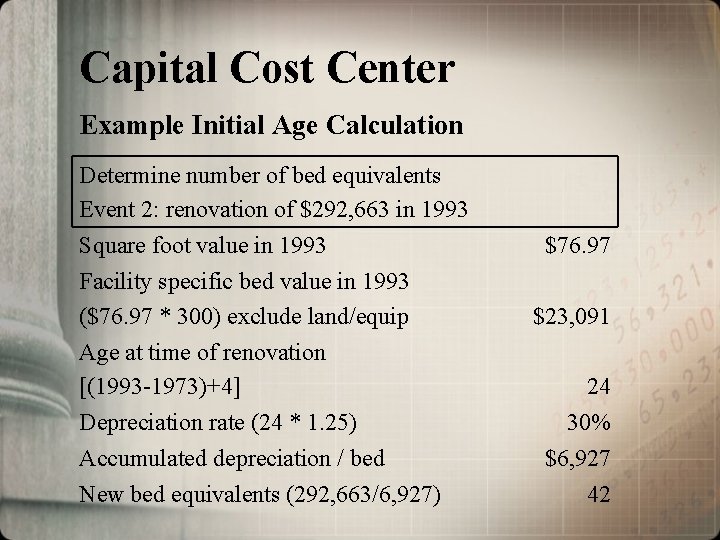
Capital Cost Center Example Initial Age Calculation Determine number of bed equivalents Event 2: renovation of $292, 663 in 1993 Square foot value in 1993 Facility specific bed value in 1993 ($76. 97 * 300) exclude land/equip Age at time of renovation [(1993 -1973)+4] Depreciation rate (24 * 1. 25) Accumulated depreciation / bed New bed equivalents (292, 663/6, 927) $76. 97 $23, 091 24 30% $6, 927 42
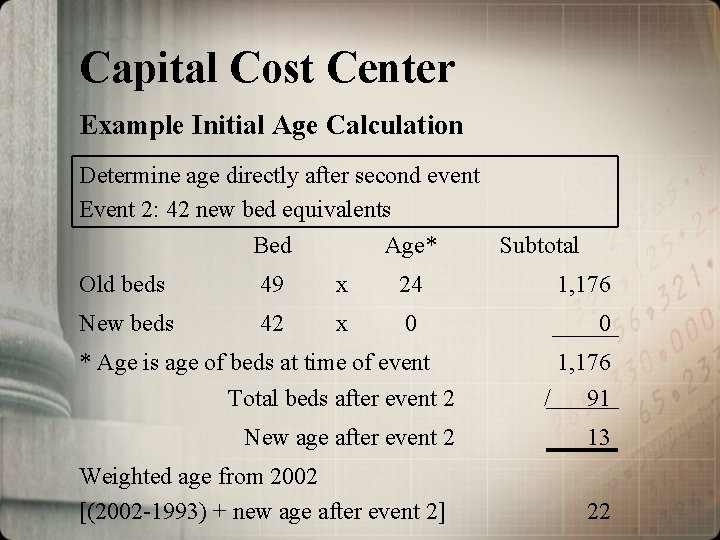
Capital Cost Center Example Initial Age Calculation Determine age directly after second event Event 2: 42 new bed equivalents Bed Age* Subtotal Old beds 49 x 24 1, 176 New beds 42 x 0 0 * Age is age of beds at time of event Total beds after event 2 1, 176 / 91 New age after event 2 13 Weighted age from 2002 [(2002 -1993) + new age after event 2] 22
Capital Cost Center Future FRV Capital Renovation / Remodeling Projects The fair rental value of each facility will be adjusted (increased) to reflect the cost of major renovation / replacement projects completed by each facility during a 24 -month period ending prior to a July 1 rate year. The renovation / replacement adjustment would be made at the start of the first rate year following completion of the renovation / replacement project.
Capital Cost Center Future FRV Capital Renovation / Remodeling Projects The cost of renovation / replacement projects must be documented within each facility’s depreciation schedule, must be reported to the Medicaid program prior to the July 1 st rate year when they would first be eligible for incorporation into the FRV rate setting process, and must exceed $500. 00 per licensed bed in order to be considered a major renovation /replacement.
Pass Through Costs • Property Taxes • Property Insurance • Provider Fee
Pass Through Rate Pass through rate is the sum of the facility’s per diem property tax and property insurance cost from the base year period trended forward plus the provider fee determined by the DHH.
Adjustments to the Rate • Rate adjustments may be made when changes occur that will eventually be recognized in updated cost report data Examples: • • • Minimum wage mandates Utility rate changes Rate adjustments may be made when legislative appropriations would increase or decrease the rates
Rate Adjustment Effective January 1, 2003 • Nursing wage and staffing enhancement add -on • Estimated at $1. 26 PPD
Additional Reimbursement Elements Inflation Factor When establishing the medians/prices for the administrative and operating and direct care and care related cost centers, cost will be adjusted from the midpoint of each provider’s base year cost report to the midpoint of each state fiscal year using the Nursing Home without Capital Market Basket Index published by DRI, or a comparable index if this index ceases to be published. In non-rebasing years, the medians/prices and property taxes and property insurance cost from the most recent rebasing period will be indexed forward to the midpoint of the current rate year using this indexing methodology.
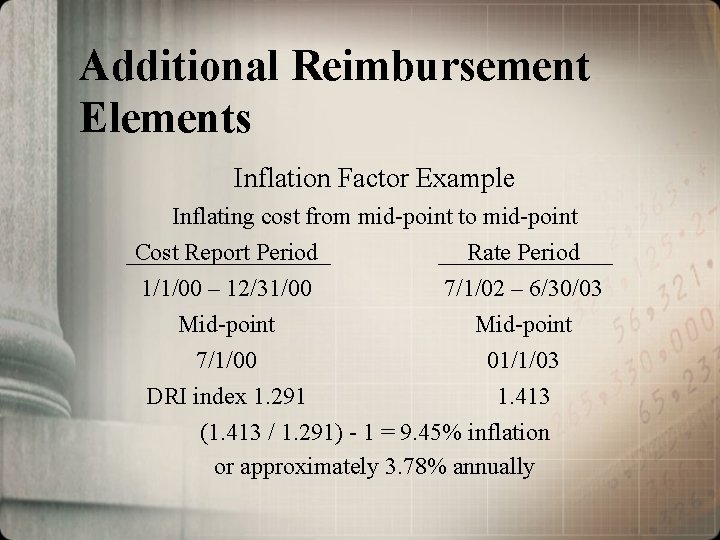
Additional Reimbursement Elements Inflation Factor Example Inflating cost from mid-point to mid-point Cost Report Period Rate Period 1/1/00 – 12/31/00 7/1/02 – 6/30/03 Mid-point 7/1/00 01/1/03 DRI index 1. 291 1. 413 (1. 413 / 1. 291) - 1 = 9. 45% inflation or approximately 3. 78% annually
Additional Reimbursement Elements • Base Year Cost Report (July 1, 2002 Rate Year) – Cost and occupancy data used in rate setting will be from cost reporting periods ending July 1, 2000 through June 30, 2001. • System Rebasing – Effective July 1, 2004 and every second year thereafter – Cost report data used will be the most recently audited or desk reviewed cost reports that are available as of the April 1 prior to the July 1 rate setting
Additional Reimbursement Elements Cost Report Requirements • Effective for periods ending on or after June 30, 2002, nursing facilities will be required to submit the skilled nursing facility cost report adopted by the Medicare program (HCFA 2540). In addition to filing the HCFA 2540, nursing facilities will be required to file supplemental schedules designated by the Bureau.
Cost Report Requirements • Cost report must be submitted annually • Due last day of the fourth month following facility’s fiscal year-end • 30 -day filing extension (must be requested) • Prepared in accordance with cost report instructions adopted by Medicare program

Supplemental Cost Report Schedules • Specific cost detail • Ancillary/therapy charge schedule for specialized services • Specialized services cost and statistics schedule • Reconciliation of Medicare allowable cost and Medicaid allowable cost
Supplemental Cost Report Schedules Specific Cost Detail • Schedule is used to report facility expenses that need to be easily identified for use in the rate setting process • For example, property tax expense is reimbursed in a separate pass-through cost center. • However, these expenses are typically commingled with other expenses on the Medicare cost report and are not easily identified.

Supplemental Cost Report Schedules Ancillary/therapy charge schedule This schedule is used to collect charges for ancillary/therapy services provided to Medicaid and other non-Medicare residents.
Supplemental Cost Report Schedules Ancillary/therapy charge schedule for specialized services This schedule is used to separate charges for ancillary/therapy services provided to Medicaid residents only into the following Medicaid resident categories: • • Standard Medicaid nursing facility charges Skilled Nursing/Infectious Disease (SN/ID) Skilled Nursing/Technology Dependent Care (SN/TDC) Neurological Rehabilitation Treatment Program (NRTP)
Supplemental Cost Report Schedules Specialized services cost and statistics schedule Schedule is used to separate the nursing facility’s cost associated with SN/ID, SN/TDC and NRTP from the nursing facility’s standard Medicaid costs
Supplemental Cost Report Schedules Reconciliation of Medicare allowable cost and Medicaid allowable cost Schedule is used to report allowable cost claimed on the HCFA 2540 that may be determined as unallowable per Medicaid program reimbursement criteria
Crosswalk between Medicare cost report and supplemental schedules to case mix cost centers • Direct care cost center – Nursing facility and skilled nursing facility salaries from Worksheet A – Allocation of benefits – Contract nursing from supplemental schedule
Crosswalk between Medicare cost report and supplemental schedules to case mix cost centers • Care related cost center – Nursing facility and skilled nursing facility other cost from Worksheet A – Social services cost from Worksheet B Pt. 1 – Raw food from supplemental schedule – Nursing administration cost from Worksheet B Pt. 1 – Allocation of benefits
Crosswalk between Medicare cost report and supplemental schedules to case mix cost centers • Administrative and operating cost center – Admin and general cost from Worksheet B Pt. 1 – Plant operation, maintenance and repair from Worksheet B Pt. 1 – Laundry and linen from Worksheet B Pt. 1 – Housekeeping from Worksheet B Pt. 1 – Dietary from Worksheet B Pt. 1 – Central services and supply from Worksheet B Pt. 1 – Other general services from Worksheet B Pt. 1 – Medical records from Worksheet B Pt. 1 – Allocation of benefits
Questions? ?
- Slides: 58