Case Managements influence on HCAHPS We play a








- Slides: 33

Case Management’s influence on HCAHPS We play a bigger role in patient experience than you may think
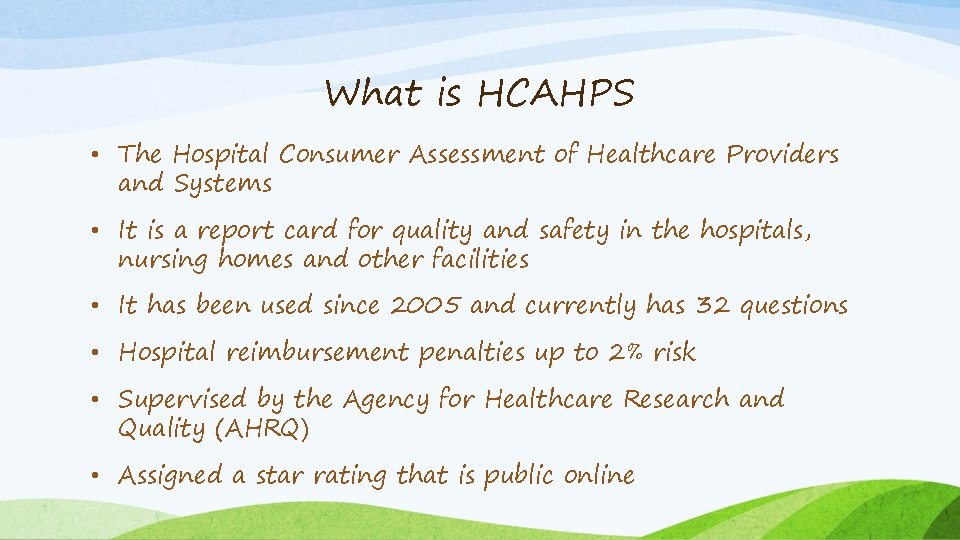
What is HCAHPS • The Hospital Consumer Assessment of Healthcare Providers and Systems • It is a report card for quality and safety in the hospitals, nursing homes and other facilities • It has been used since 2005 and currently has 32 questions • Hospital reimbursement penalties up to 2% risk • Supervised by the Agency for Healthcare Research and Quality (AHRQ) • Assigned a star rating that is public online
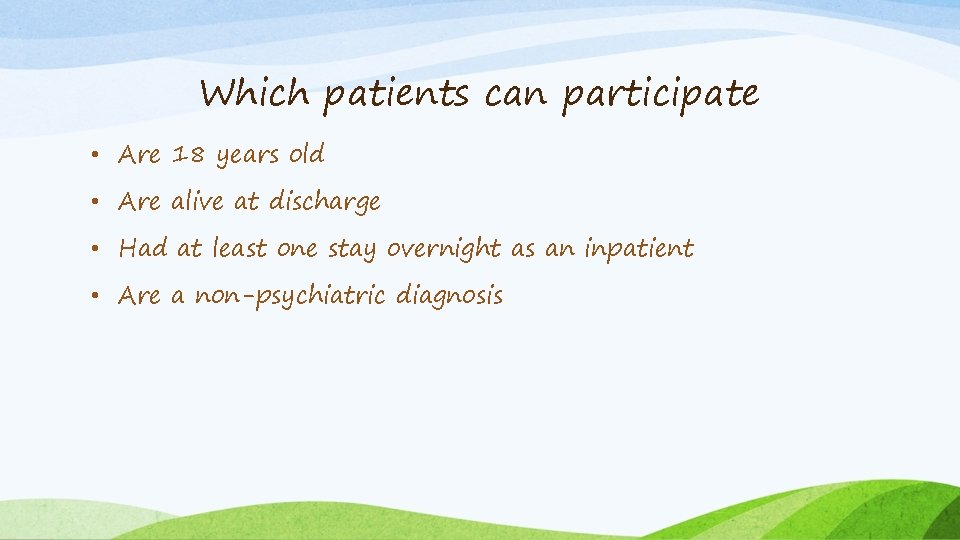
Which patients can participate • Are 18 years old • Are alive at discharge • Had at least one stay overnight as an inpatient • Are a non-psychiatric diagnosis
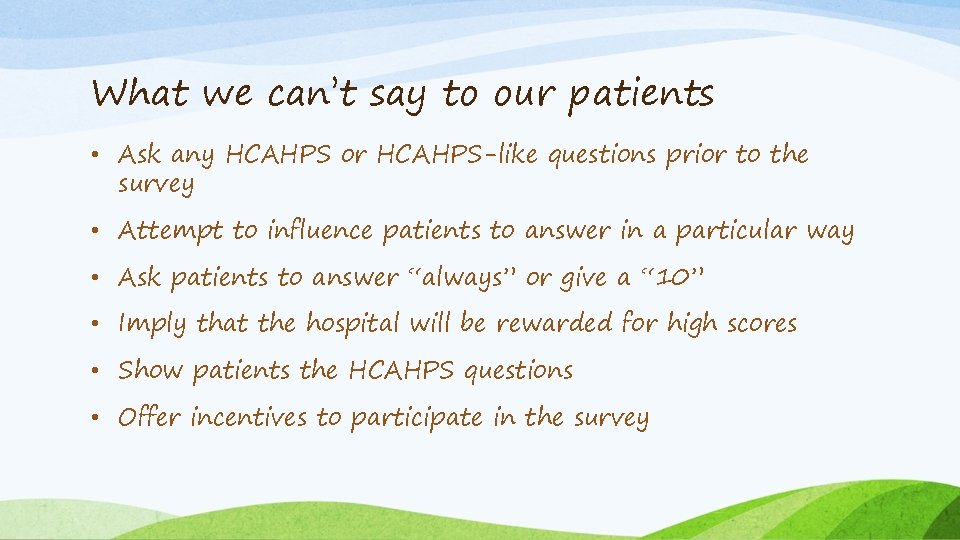
What we can’t say to our patients • Ask any HCAHPS or HCAHPS-like questions prior to the survey • Attempt to influence patients to answer in a particular way • Ask patients to answer “always” or give a “ 10” • Imply that the hospital will be rewarded for high scores • Show patients the HCAHPS questions • Offer incentives to participate in the survey
HCAHPS is not about PATIENT SATISFACTION, it is about PATIENT EXPERIENCE. HCAHPS is not about keeping patients happy. It is about keeping them safe. Providing quality care and keeping them out of the hospital.
Discharge Information questions • During this hospital stay, did doctors, nurses or other hospital staff talk with you about whether you would have the help you needed when you left the hospital? • During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital?
Care Transition questions • The three-question Care Transition questions started in January 2013 and were publicly reported October 2014 • The hospital staff took my preferences and those of my family or caregiver into account in deciding what my healthcare needs would be when I left the hospital • When I left the hospital, I had a good understanding of the things I was responsible for in managing my health • When I left the hospital, I clearly understood the purpose for taking each of my medications
Care Transition • Think about the long-term implications of what we do • After a patient discharges is equally as important as taking care of them in the hospital • When we improve the continuum of care, we improve all patient outcomes • Our patients are leaving the hospital not knowing how to approach the next phase of their care
Two other discharge-related questions • Answer “yes” or “no” • During this hospital stay, did doctors, nurses and other staff talk with you about whether you would have the help you needed when you left the hospital? • During this hospital stay, did you get information in writing about what symptoms or health problems to look out for after you left the hospital?
Research suggests…. • A patients perception of how prepared they were to care for themselves when they discharged from the hospital greatly influenced how they perceived the quality of care in the hospital
Great Communication is most important for a positive patient experience
Communication matters! • What is your patient responsible for when they go home? • Medical and medication errors happen during transitions • Mitigates risk • Value based purchasing • Readmissions (3 days before admission to 30 and 90 days after readmission) • 40% of patients don’t even know what their diagnosis is
Case management is an important role • Explain things in layman terms … LTAC vs IRF vs SNF vs HHC • The hospital is a common place for us but it is a unique situation for our patients • Make eye contact • Relax and don’t be in a hurry • Avoid interruptions • Sit down (impression is that you spent more time in the room) • Don’t ignore the patient’s family. . Your patient depends on them • Write the estimated discharge date on their white board

Discharging is a vulnerable time • One in five patients experience an adverse event during this transition, a third of which are preventable • It is hard to retain all of the information especially if it is given all at once • Preventable readmissions cost the healthcare system about $25 billion each year
Some patients expect assistance to continue after discharge • Did we listen to the patient and their family to incorporate their needs into the discharge plan? • Do you have someone to help you at home? • Will you need help getting to the bathroom? • Do you have someone to prepare your meals? • Can you call on family or friends if you need help?
Listen to your patients and their family • Make a plan that your patient helped create • What family member will be assisting the patient? • Do they know what they are responsible for after discharge? • Do they understand what will happen if they don’t follow the plan? • If our plan is in conflict with their plan, you must explain the why! • When we listen to our patients and their family members and take their preferences and desires into account, their compliance increases and their outcomes improve.
Communication, Coordination and Collaboration • What 3 concerns do you have about leaving the hospital? • Who are 3 people you can contact when you have a question or need help? (Include their PCP) • What are 3 possible obstacles that might prevent you from being successful at home? • Can the family arrange for visits from family, friends to help the patient and keep them from feeling depressed and isolated? • Ask for their agreement on discharge responsibilities

Depression, Loneliness and Isolation • Patients who have depression, rate their hospital stay lower • Many patients feel lonely and isolated when they get home due to decreased mobility, functional decline and financial hardship. • Loneliness and social isolation is linked with more hospital visits and negative health outcomes including increased mortality • Give your patients community resources to help combat this!

Educate your patients! Start teaching them from the day they are admitted

Importance of education • What are they responsible for when they get home? • Do they understand their medications? • Follow up appointments? • Do they know what to do if they start experiencing symptoms?
Educate the staff about resources • Case Management can’t be everywhere. Educate your nursing staff about resources • Create an electronic folder of discharge resources for the emergency department and nursing floors • Electronic resources will help with after hours patients and discharge phone calls
Medications • Taking medications is very confusing • The #1 reason for patients having complications and being readmitted is taking medication incorrectly • Medication errors harm 1. 5 million people each year at an annual cost of $3. 5 billion dollars • What was prescribed during the hospital stay AND what do they still have at home?
Who can help with medications? • Can pharmacy help explain medications, doses and side effects? • Is family involved in this education? • Can a HHC RN help once the patient gets home? • Can a PCP appointment help with medication reconciliation? • Make sure your patient agrees with the plan
Research • Re-Engineered Discharge (RED) toolkit • Improves discharge process and reduces readmission • The RED is the product of 7 years of works supported by funding from the AHRQ and the National Heart, Lung, and Blood Institute • Nationally…readmission rates are 1 in 5 or 20%
RED findings • Delayed transfer of discharge summary to PCP • Unknown pending test results when the patient leaves the hospital. Results not included in discharge packet • Lack of follow-up for appointments or procedures. 1/3 of patients need follow-up • Medicine reconciliation and adverse events • These all contribute to adverse events, ED visits and readmissions
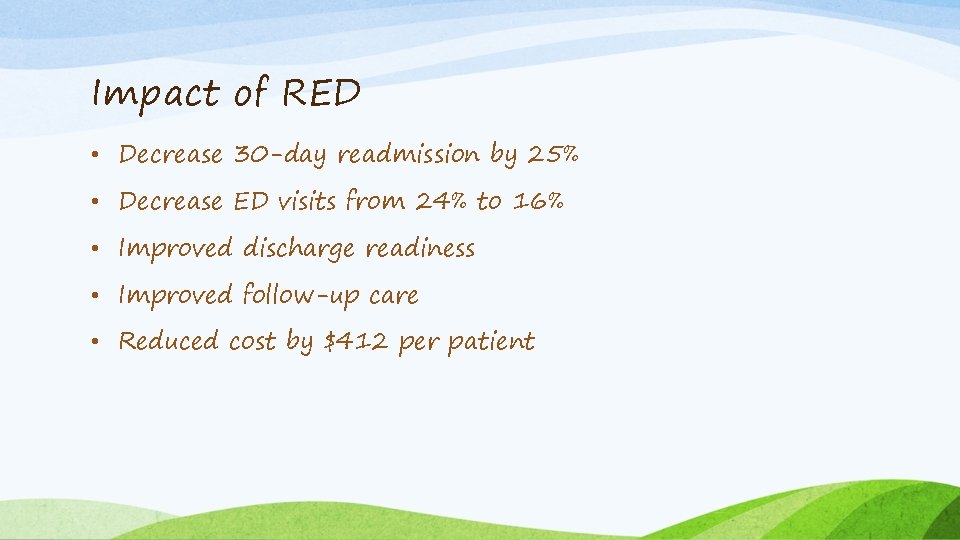
Impact of RED • Decrease 30 -day readmission by 25% • Decrease ED visits from 24% to 16% • Improved discharge readiness • Improved follow-up care • Reduced cost by $412 per patient

11 steps to implement RED 1. Make a clear and decisive decision – senior management 2. Identify implementation leadership – who will lead? One person or more? 3. Analyze your readmission rate and determine goal 4. Which patients should receive the RED? 5. Create your process map 6. Revise current discharge workflow 7. Assign responsibilities – hire someone new? 8. Train discharge educator and follow-up telephone callers 9. Decide how to generate the “after hospital care plan” booklet 10. Provide RED for diverse populations 11. Plan to measure the progress of RED implementation

6 different tools to help implement RED 1. Overview 2. How to begin implementation of RED 3. How to deliver RED discharge at your hospital 4. How to deliver RED for diverse populations 5. How to conduct a post discharge follow-up call 6. How to monitor RED discharge implantation and outcomes
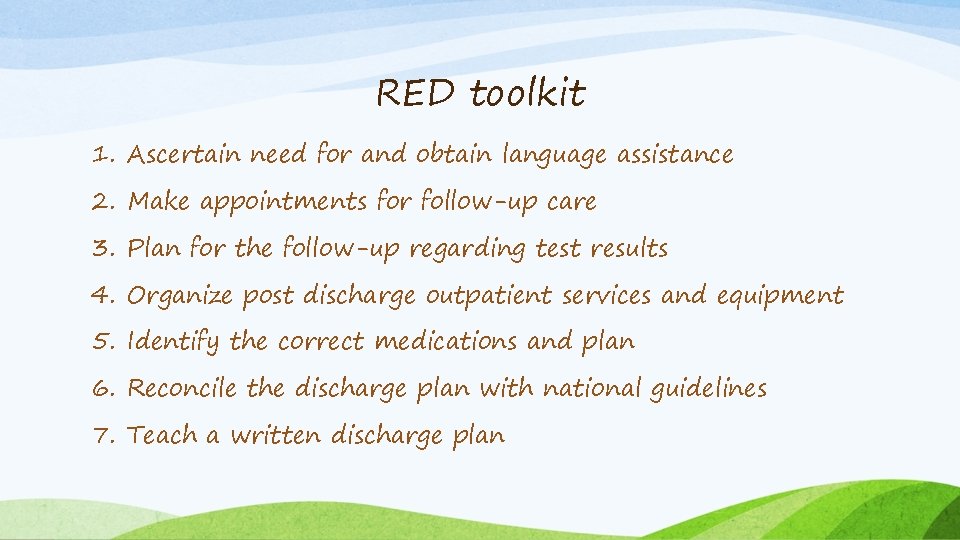
RED toolkit 1. Ascertain need for and obtain language assistance 2. Make appointments for follow-up care 3. Plan for the follow-up regarding test results 4. Organize post discharge outpatient services and equipment 5. Identify the correct medications and plan 6. Reconcile the discharge plan with national guidelines 7. Teach a written discharge plan

RED toolkit (cont. ) 8. Educate the patient about their diagnosis and medications 9. Review with the patient what to do if a problem arises 10. Assess the degree of the patients understanding 11. Communicate care plan to clinicians accepting care of the patient 12. Provide telephone reinforcement of the discharge plan • Additional considerations: dietary, religious, sexual orientation and gender
Realities of discharge planning….
References • Ketelsen RN, Lyn, Cook RN, Karen, Bekki, Kennedy, The HCAHPS handbook: Tactics to Improve Quality and the Patient Experience, The Studer Group 2014 • Re-Engineered Discharge (RED) toolkit, AHRQ 2013 • Lewis, Ebony, Samperi, Sarah, Boyd-Skinner, Christopher, Telephone follow-up calls for older patients after hospital discharge, The Simpson Centre for Health Services Research 2017 • 4 strategies to boost hospitals HCAHPS scores, Becker’s Hospital Review 2012 • 15 powerful ways to improve HCAHPS scores, Med. Pro disposal 2017 • Caskey RN, Debbie, Topjian RN, MSN, Diana, Transitions of Care: Moving from acute care to home with comprehensive care plans, Studer Group 2017
Thank you for your time! Questions?