Case Management Monitoring Using Risk Assessment and Mitigation

- Slides: 38
Case Management Monitoring: Using Risk Assessment and Mitigation Strategies
Monitoring Services and Supports What’s required? Ê What’s important? Ê What’s good practice? Ê How to develop a comprehensive plan? Ê How to individualize monitoring? Ê
Challenges Increased scrutiny from regulators and the general public. Greater diversity of services and service settings. Increasingly litigious society.
Challenges Funding stream changes over the past few years; Complexity of CM/RC role; CCB size and geographic variables; Unchanging responsibility of CMs/RCs to monitor individuals on their caseload.
Challenges Changing face of Case Management/Resource Coordination More documentation 4 Less time in the field 4 Changing Roles in Support Services 4 Less familiarity with consumers 4
Basic Questions ´ ´ ´ Who is responsible for monitoring? How to determine what should be monitored? How do you determine how monitoring occurs? How do you determine how often monitoring occurs? What do you do with the results?
Who is Responsible for Monitoring? n DDS n n CCB n n Overall Service Provider Organization monitoring SPO n n Overall Service Provider Organization monitoring Individual and overall organizational monitoring CM/RC n Individual specific monitoring
DDS Monitoring Requirements n Monitoring by Case Management ensures that: n n n The IP is implemented; Health and safety needs are addressed; People’s rights are respected People are satisfied with services and supports Monitoring activities are documented Follow-up is completed in a timely manner.
What Should Be Monitored? n Health, Safety and Welfare n n n n Medical/medication needs are being addressed. Therapy needs are being addressed. Dietary needs are being addressed. Home safety is being addressed. ADA/Accessibility is being addressed. Community safety is being addressed. Critical incidents receive proper follow-up.

What Should Be Monitored? n Rights are Respected n n n Statutory Requirements are Met Involvement of Other Authorities Possible Dangerous Behavior n n n Endangering Self Endangering Others Endangering Property
Determining Monitoring Frequency n n Everybody, Everything, Everywhere at a Fixed Frequency; or, Everybody, Everything, Everywhere at a Variable Frequency; or, Everybody, and/or Everything, and/or Everywhere at a Fixed and or Variable Frequency; or Everybody, Everything, Everywhere at a Frequency Based Upon Identified Risks.
Risk Management “A planned and proactive process for reducing and minimizing an individual’s potential loss or injury. ” Risks are activities, situations and circumstances that may lead to any unintended consequence which is or may potentially be harmful to the individual.
Risk Management n n Identify the risks; Evaluate the risks; Prepare and implement a plan to mitigate the risks; and Evaluate the effectiveness of the plan.
Identify Risks n n n Who- Case managers/RC with input from the IDT. When- Identify risk factors at the time of annual assessment, IP development and during monitoring; How- Utilize a risk assessment tool or checklist;
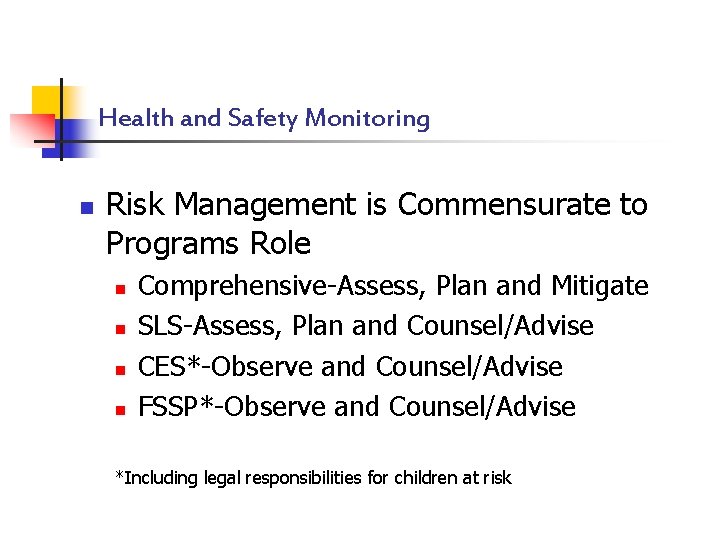
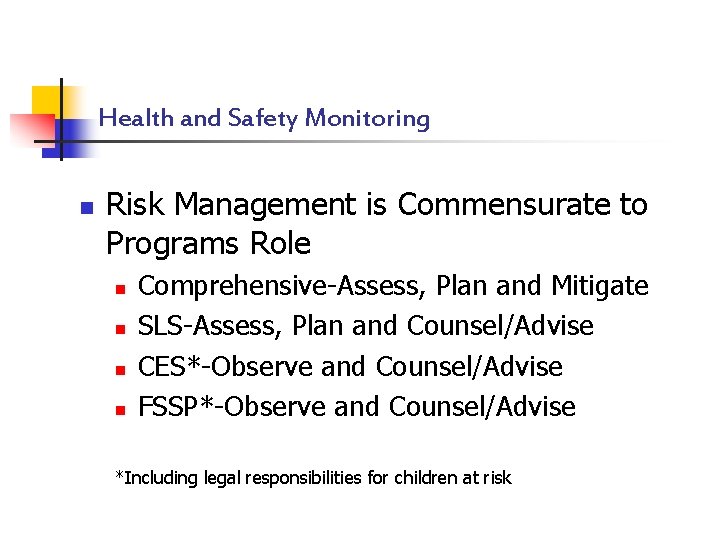
Health and Safety Monitoring n Risk Management is Commensurate to Programs Role n n Comprehensive-Assess, Plan and Mitigate SLS-Assess, Plan and Counsel/Advise CES*-Observe and Counsel/Advise FSSP*-Observe and Counsel/Advise *Including legal responsibilities for children at risk
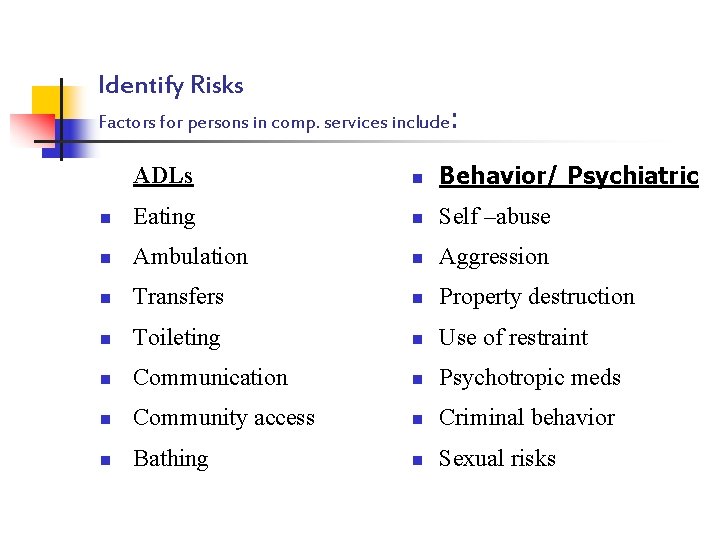
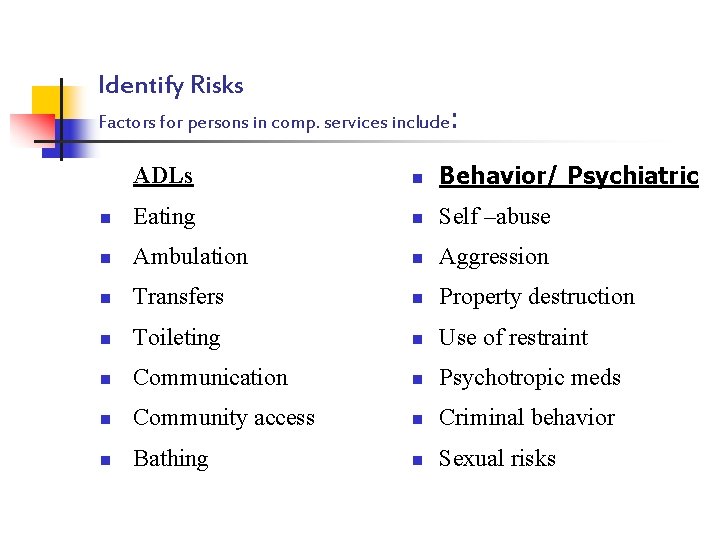
Identify Risks Factors for persons in comp. services include: ADLs n Behavior/ Psychiatric n Eating n Self –abuse n Ambulation n Aggression n Transfers n Property destruction n Toileting n Use of restraint n Communication n Psychotropic meds n Community access n Criminal behavior n Bathing n Sexual risks
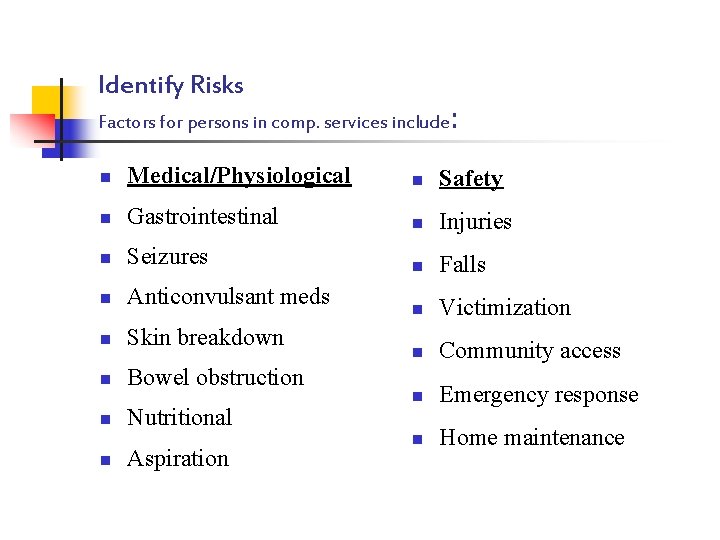
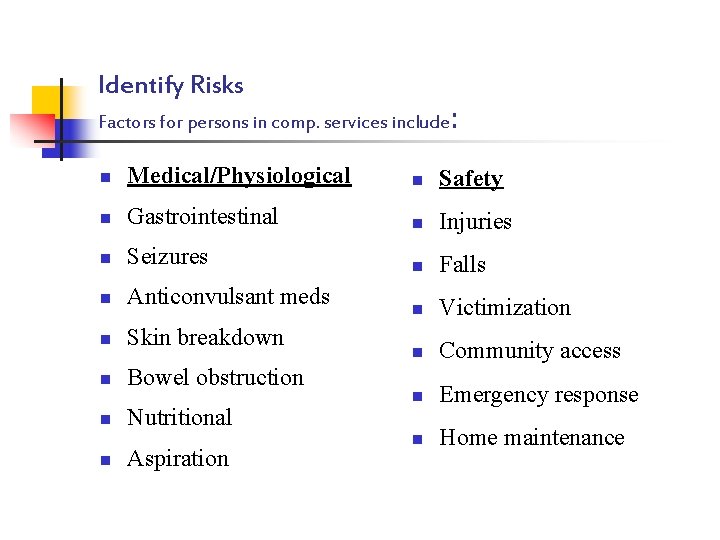
Identify Risks Factors for persons in comp. services include: n Medical/Physiological n Safety n Gastrointestinal n Injuries n Seizures n Falls n Anticonvulsant meds n Victimization n Skin breakdown n n Bowel obstruction Community access n Emergency response n Home maintenance n n Nutritional Aspiration
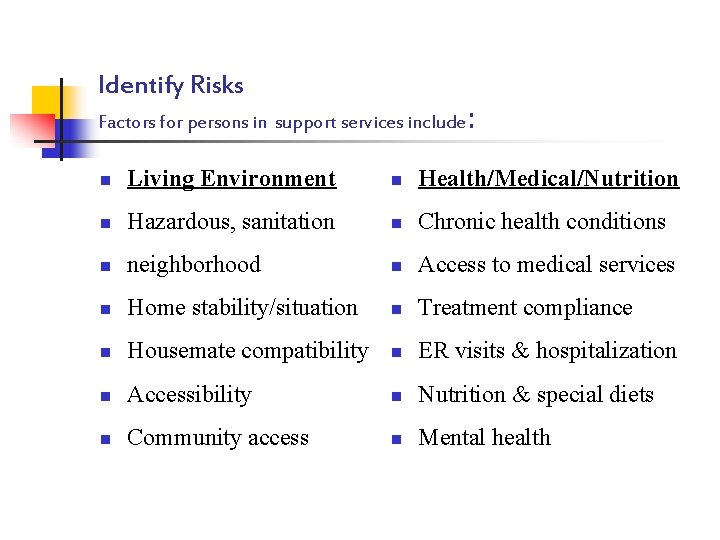
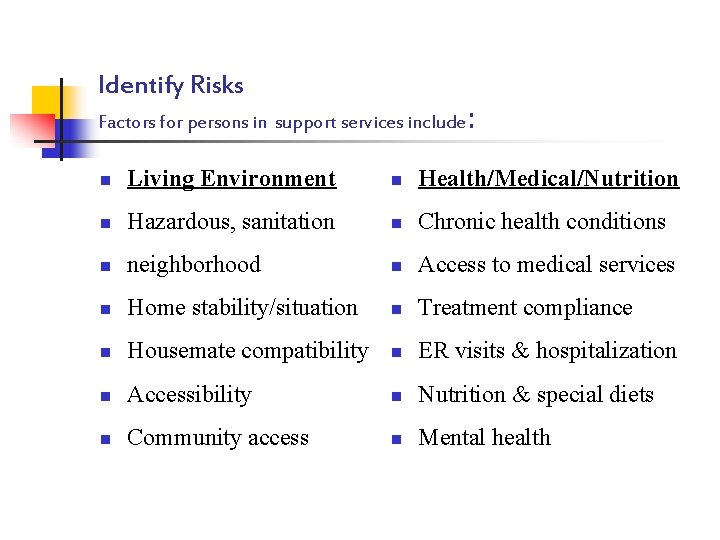
Identify Risks Factors for persons in support services include: n Living Environment n Health/Medical/Nutrition n Hazardous, sanitation n Chronic health conditions n neighborhood n Access to medical services n Home stability/situation n Treatment compliance n Housemate compatibility n ER visits & hospitalization n Accessibility n Nutrition & special diets n Community access n Mental health
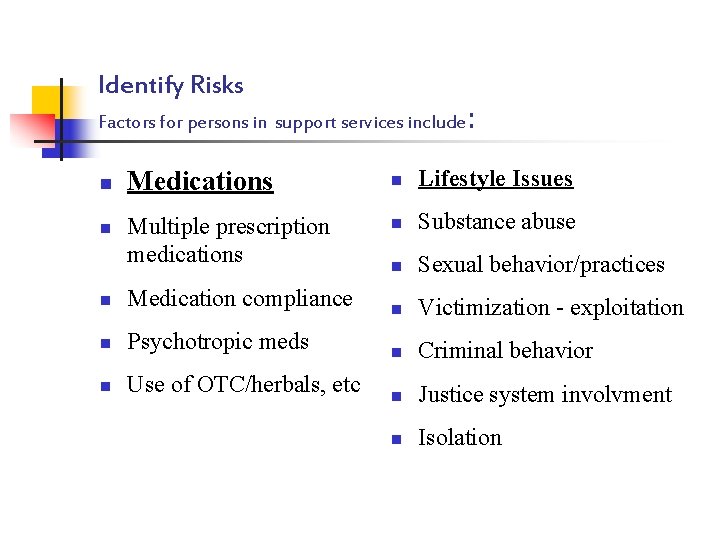
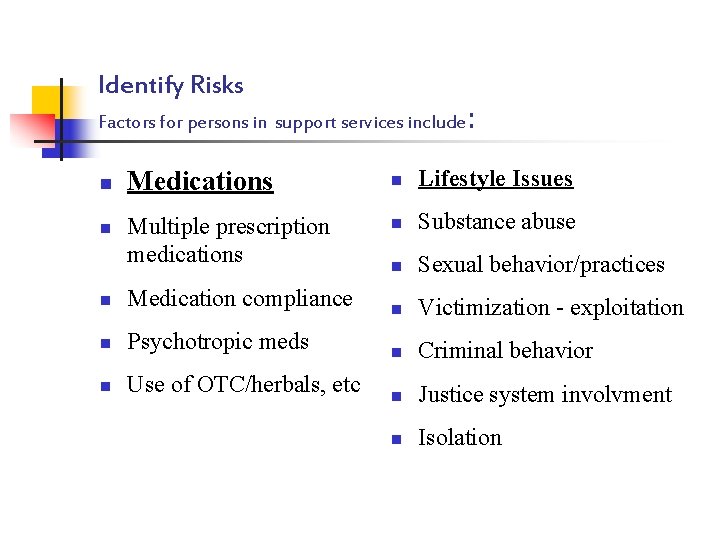
Identify Risks Factors for persons in support services include: n n Medications Multiple prescription medications n Medication compliance n Psychotropic meds n Use of OTC/herbals, etc n Lifestyle Issues n Substance abuse n Sexual behavior/practices n Victimization - exploitation n Criminal behavior n Justice system involvment n Isolation
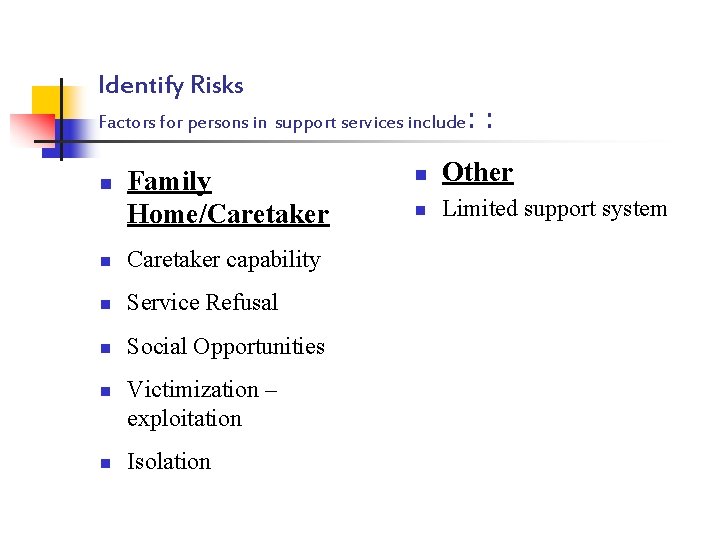
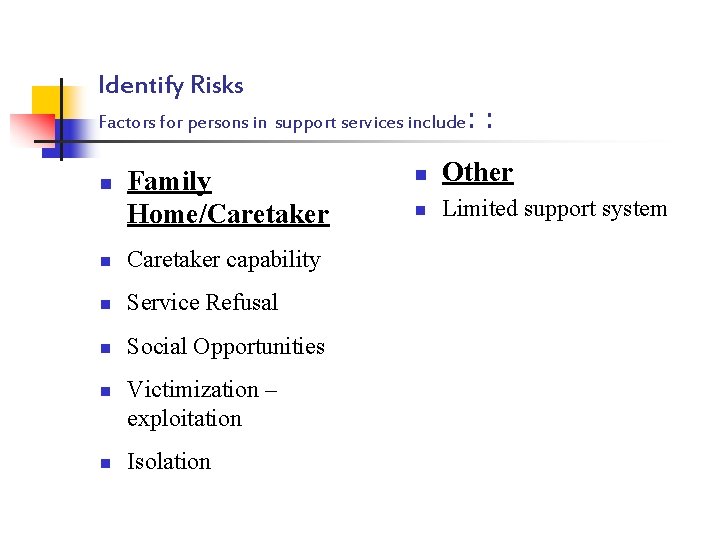
Identify Risks Factors for persons in support services include: n Family Home/Caretaker n Caretaker capability n Service Refusal n Social Opportunities n n Victimization – exploitation Isolation : n Other n Limited support system
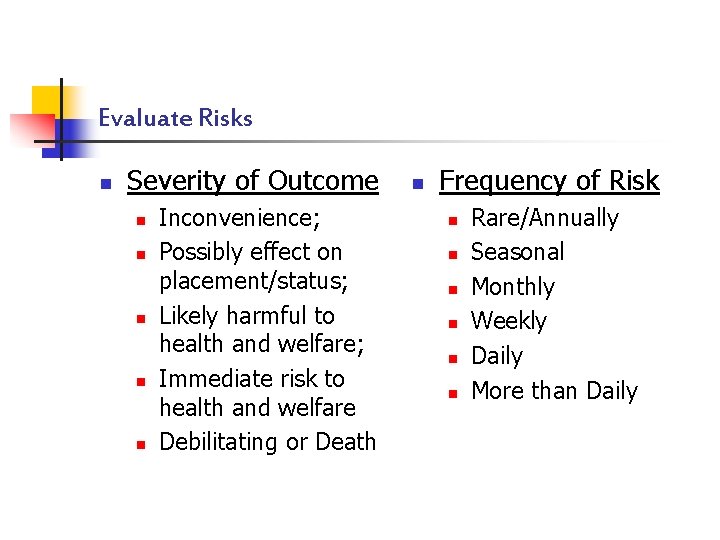
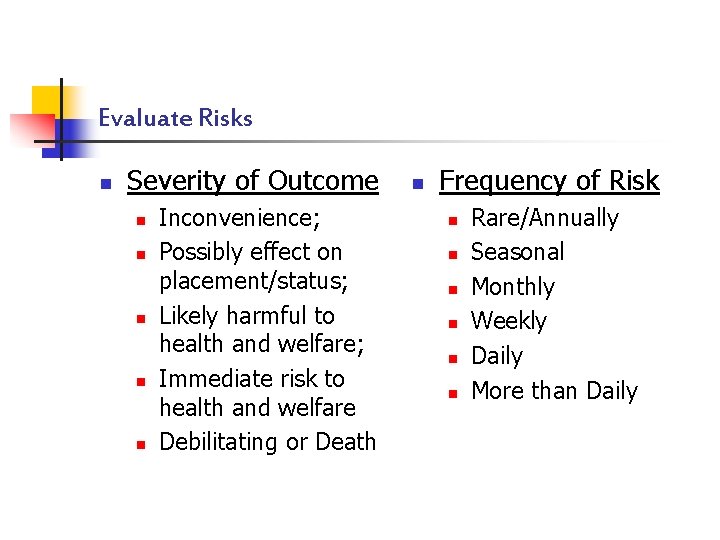
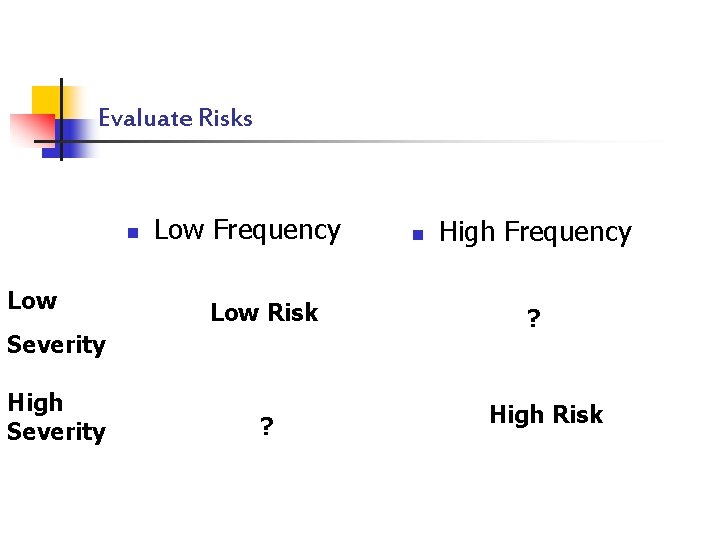
Evaluate Risks n Severity of Outcome n n n Inconvenience; Possibly effect on placement/status; Likely harmful to health and welfare; Immediate risk to health and welfare Debilitating or Death n Frequency of Risk n n n Rare/Annually Seasonal Monthly Weekly Daily More than Daily
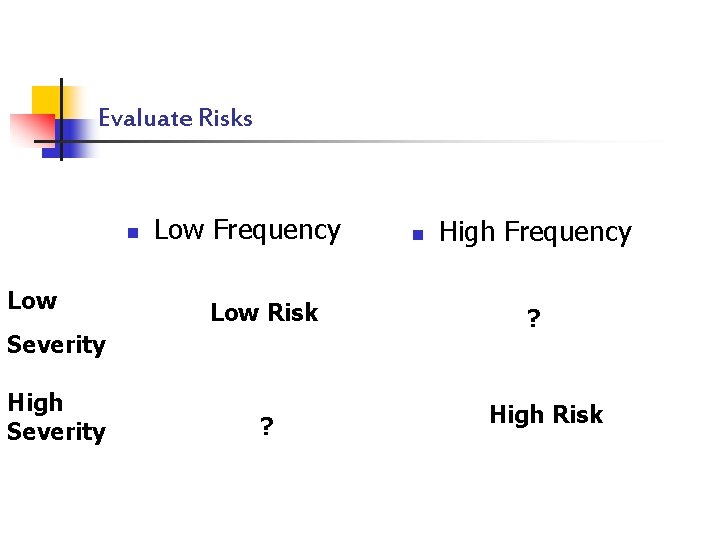
Evaluate Risks n Low Frequency Low Risk Severity High Severity ? n High Frequency ? High Risk
Risk Reduction n Utilize the IP process to specify programs and protocols for mitigating risks prioritized through risk assessment. n n n Specify as services and supports; Require ISSPs where required and appropriate; Ensure documentation of implementation and effectiveness of risk reduction plans.
Risk Reduction n Examples of services and support to be provided to mitigate risks include: n n Fire evacuation drills, safety skill training; Bathing, feeding, bowel protocols; Behavioral programming, health monitoring, nutrition plans, PT/OT, psychotherapy; Sex offender containment and treatment, safety control procedures, rights suspensions.
Develop a Monitoring Plan • Monitor settings in which high risks occur. • Frequency of monitoring should be commensurate with the level of risk. • Use multifaceted methods. • Specify documentation/feedback mechanism.
Monitor Risk Plan Effectiveness n Target Efforts to High Risk Issues n n n What are the High Risks? Where do the High Risks Occur? When do the High Risks Occur? What plans have been implemented to reduce the High Risks? How Effective are the risk reduction plans?
Monitor Risk Plan Effectiveness n Utilize a multi-faceted approach in monitoring: n n Review program data in summary reports and onsite in program files and other data documenting risk reduction (e. g. , fire drills, med. admin. records, use of restrictive procedures etc. ); Review SPO contact notes, incident reports and Interview staff/providers. Interview the individual, their family and friends; Visit the person at home and review the status of identified risk issues (e. x. , adequate food, safe medications, etc. )
Methods of Monitoring n n Must include direct observation Includes a variety of activities: n n n Face to face Site visits Consultations Phone calls Documentation review
Individualizing Monitoring n Other Factors affecting Monitoring: n n n n The IP History of the individual History of the provider History of the SPO Funding Setting: Family, Host Home, Independent Home, PCA, Group Home Services for people with higher needs should be monitored more frequently
Planning On-site Monitoring n Determine the Mode: n n n Unannounced Visit- Often useful if the agency/provider has a mixed history or if there have been indications or reports that the provider has prepared for monitoring visits. Announced Visits- Always the preferred mode for logistical reasons and to maintain rapport. Good Practice- Vary your pattern.
Conducting On-site Monitoring n Maintain Rapport: n Agency Staff n n n Ask inquisitive and supportive questions. Be polite and be prepared to provide support and information Be candid, clear and concise. Avoid expressing displeasure, bias or confusion. Validate good work and express concern re: questionable/bad practice.
Conducting On-site Monitoring n Maintain Rapport: n Host Home Providers n n n Same list as agency staff. Monitoring=Intrusion vs Visit=Concern Understand role of the person to the family unit Review only those environments & documents related to the person. Consider only communicating negative outcomes to provider agency.
Conducting On-site Monitoring n Maintain Rapport: n Day Program Providers n n Same list as agency staff. Often very busy and can be short on time to discuss person. For integrated work- Need to consider setting as typical employment and adjust monitoring accordingly. Attempt to be discrete.
Conducting On-site Monitoring n Monitor Broadly n n n Follow-up on items not on the checklist. Look, listen, and smell. Consider emerging issues. Identify obvious problems for other persons. If in doubt, reference others
Documentation and Follow-up n Documentation n Monitoring activities are documented Follow-up, where needed, on findings is documented. Follow-up n n Follow-up is completed in a timely manner Others notified as needed or required
Documentation n n When did monitoring occur? What was monitored? How did monitoring occur? Outcome of the monitoring Actions needed/taken as appropriate
Follow-up n n n Documented What actions were needed as a result of the monitoring activity? Timeliness is commensurate with risk. Loop closed What is done with information gathered? Obligations regarding rules and regulations, Social Services, agency Policy and Procedures
Case Management Administration n Formal Supports n Policies, Procedures and Protocols n n Requirements for risk assessment and monitoring Conflicts with SPO (Including CCB SPO) Collection and analysis of data Personnel Practices n n n Job Design Validates Importance of Monitoring Training Addresses Needed Knowledge and Skills Evaluation Includes Performance re: Monitoring