Case Malnutrition Iron Deficiency Anemia StatusPost Duodenal Switch









- Slides: 26

Case: Malnutrition & Iron Deficiency Anemia Status/Post Duodenal Switch & Ileostomy Christa Giroux, Dietetic Intern
Overview • Patient’s history • Normal anatomy of GI tract • Present medical status & typical treatments • Lab values • Medications • Present treatment • MNT • Prognosis
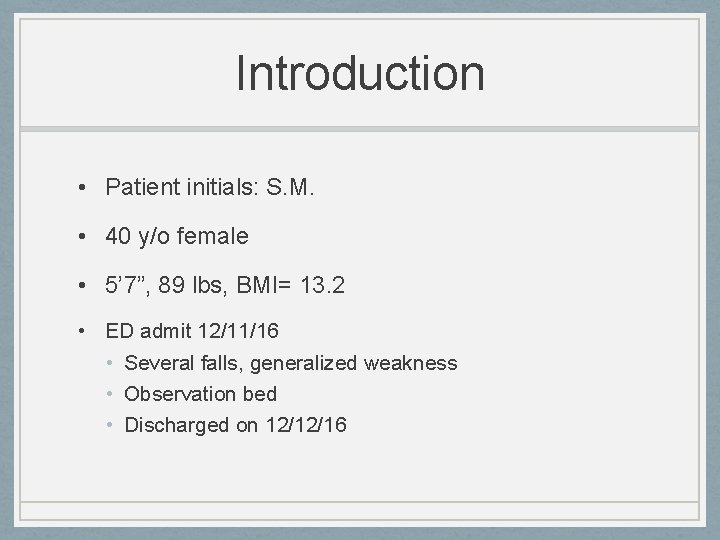
Introduction • Patient initials: S. M. • 40 y/o female • 5’ 7”, 89 lbs, BMI= 13. 2 • ED admit 12/11/16 • Several falls, generalized weakness • Observation bed • Discharged on 12/12/16
Past Medical Hx • Iron deficiency anemia • Protein-energy malnutrition • 8% weight loss 2 months • Opioid dependence • S/p duodenal switch surgery (BPD/DS) • IBD • S/p total colectomy with ileostomy • With high output • Lumbar disc degeneration • Bilateral pleural effusion • Spinal stenosis

Reason for Patient Choice • BPD/DS • Ileostomy • Presence of malnutrition in relation to bariatric surgery • Multiple health complications that are related
Social Hx • Unemployed w/ disability status • Divorced, no children • Lives at home w/ mother (breast CA) • Responsibilities: cooking, laundry, other house chores • Adequate standards of living, but not ideal- lack of income • Medicare • Religion not recorded
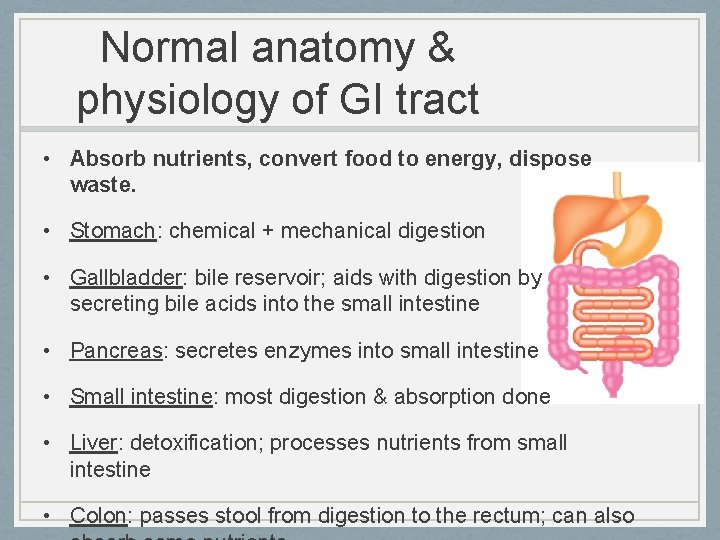
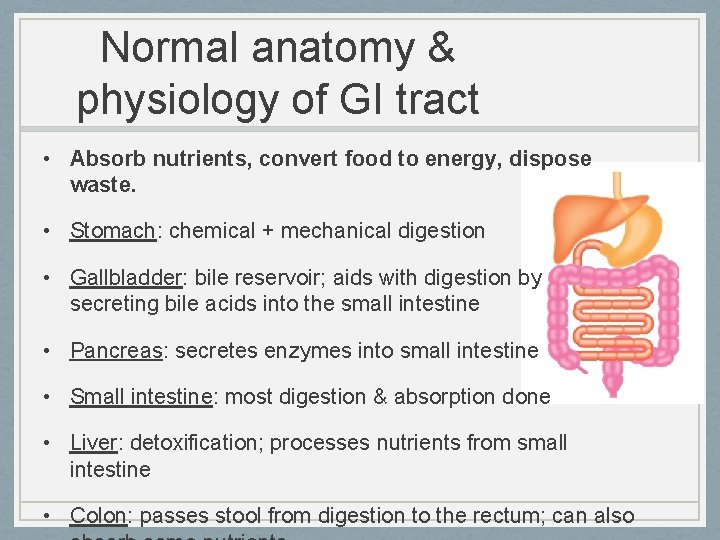
Normal anatomy & physiology of GI tract • Absorb nutrients, convert food to energy, dispose waste. • Stomach: chemical + mechanical digestion • Gallbladder: bile reservoir; aids with digestion by secreting bile acids into the small intestine • Pancreas: secretes enzymes into small intestine • Small intestine: most digestion & absorption done • Liver: detoxification; processes nutrients from small intestine • Colon: passes stool from digestion to the rectum; can also
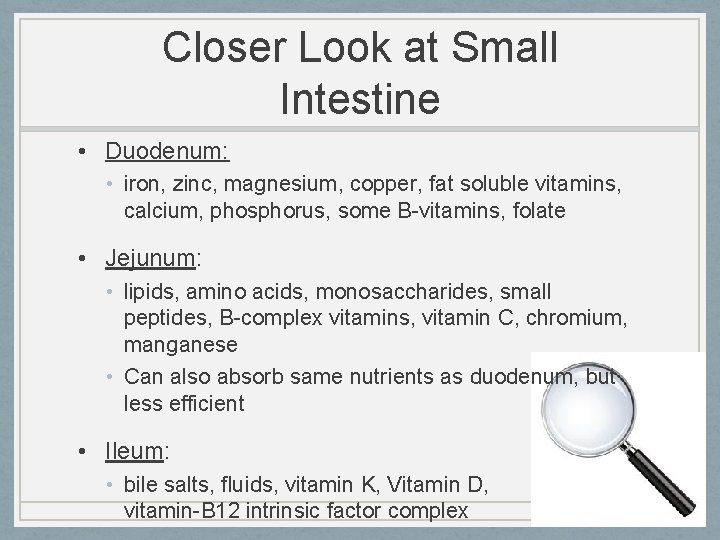
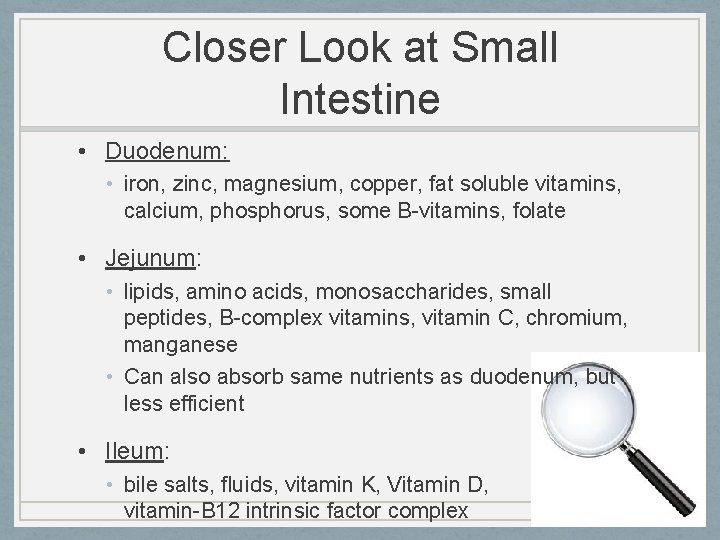
Closer Look at Small Intestine • Duodenum: • iron, zinc, magnesium, copper, fat soluble vitamins, calcium, phosphorus, some B-vitamins, folate • Jejunum: • lipids, amino acids, monosaccharides, small peptides, B-complex vitamins, vitamin C, chromium, manganese • Can also absorb same nutrients as duodenum, but less efficient • Ileum: • bile salts, fluids, vitamin K, Vitamin D, vitamin-B 12 intrinsic factor complex
Prior Admissions/Hx • Medication refills, transfusions, lab testing • Several GI endoscopies • Back complications • 2005 - BPD/DS done since the pt was morbidly obese • 2007 - Total colectomy w/ ileostomy for IBD & severe dumping syndrome • 2015 - Episode of TPN d/t inability to eat & absorption issues. Thoracentesis & R chest tube placed for pleural effusion • Several other admissions for back pain, GI bleeds, abdominal pain, weakness. • Sees digestive specialist in Springboro, OH
Present Medical Status & Tx • BPD/DS: combination of gastric bypass + sleeve gastrectomy • https: //www. youtube. com/watch? v=p. WW 2 sw. Ea. Hr. Q • 85% stomach removal & duodenal resection • PROS: Significant weight loss • alters gut hormones, restricts absorption, limits consumption, reduces absorption of fat by 70% • CONS: Adverse side effects • Nutrient deficiencies, higher mortality, malnutrition, nausea, vomiting. • Success requires compliance with dietary restrictions, supplementation, physician visits
Present Medical Status & Tx • Total colectomy w/ileostomy: permanent tx for dumping syndrome • Ileum brought through abdominal wall • Colon, rectum, anus removed • Ostomy bag • High ostomy output: • >8 cups per day indicates malnutrition & dehydration • Treatment: Management w/ medication, soluble fiber, protein, several small meals per day
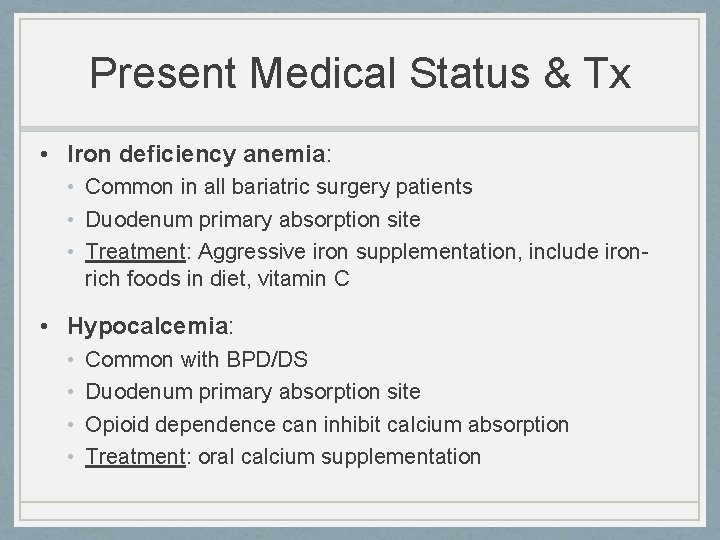
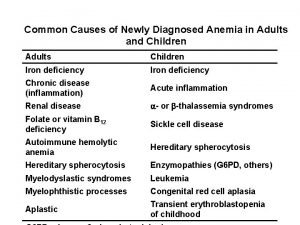
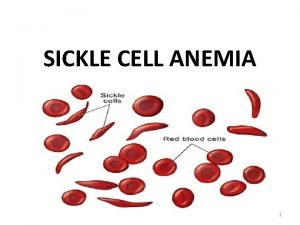
Present Medical Status & Tx • Iron deficiency anemia: • Common in all bariatric surgery patients • Duodenum primary absorption site • Treatment: Aggressive iron supplementation, include ironrich foods in diet, vitamin C • Hypocalcemia: • • Common with BPD/DS Duodenum primary absorption site Opioid dependence can inhibit calcium absorption Treatment: oral calcium supplementation
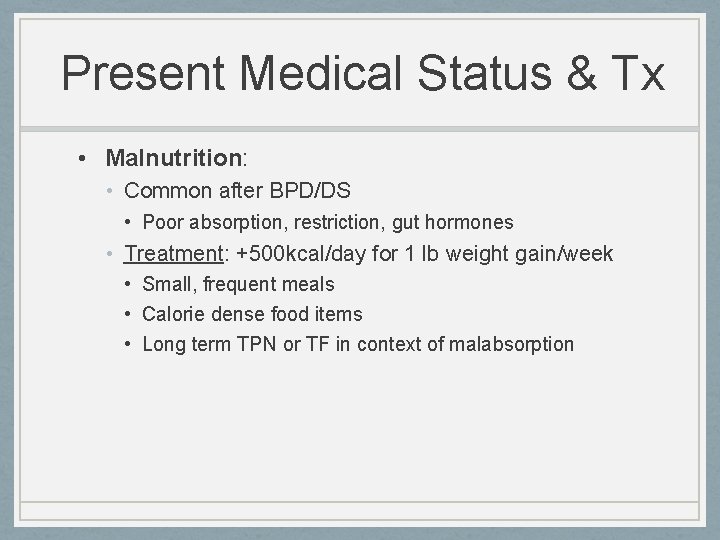
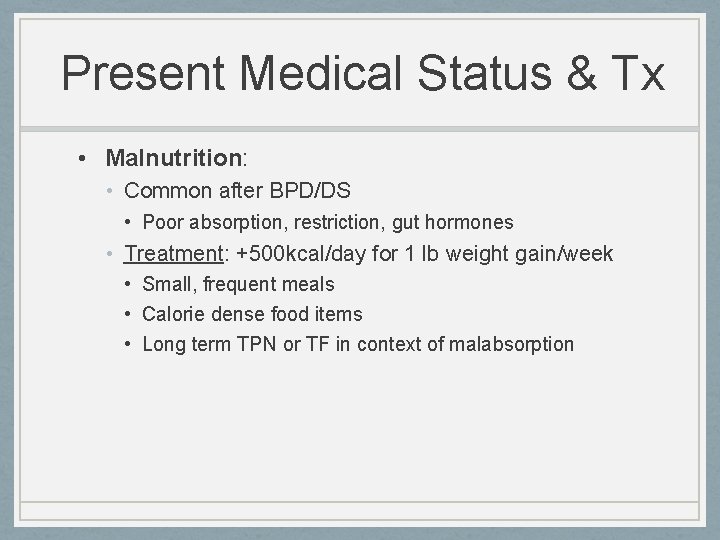
Present Medical Status & Tx • Malnutrition: • Common after BPD/DS • Poor absorption, restriction, gut hormones • Treatment: +500 kcal/day for 1 lb weight gain/week • Small, frequent meals • Calorie dense food items • Long term TPN or TF in context of malabsorption

The Literature • Randomized parallel-group trial of 58 participants: • Participants completed gastric bypass or BPD/DS • Malnutrition only seen in BPD/DS patients • Prospective study on all bariatric surgeries: • Iron deficiency anemia in 42. 9% BPD/DS patients within 30 months • 49. 9% with iron deficiency anemia within 60 months • Retrospective review of BPD/DS patients (1999 -2011): • 37% of patients needed further surgery d/t side effects

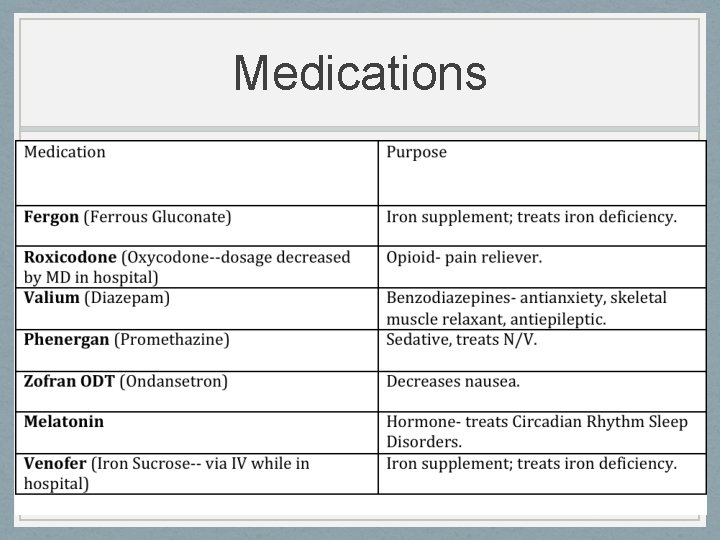
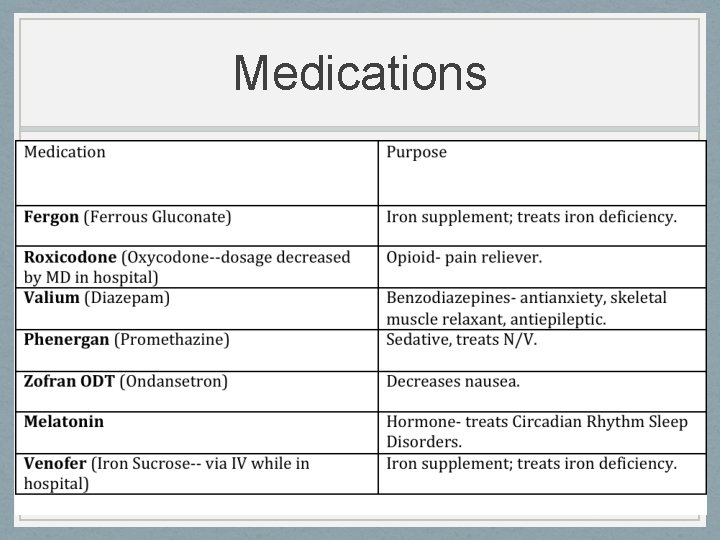
Medications

Tx (Medical & Surgical) • Blood transfusion • IVF for dehydration • IV iron sucrose • Opioid cessation by physician • Switched to Fergon at discharge, noncompliant w/ previous iron medication • Oral nutrition supplements with coupons • No surgical interventions at this admission
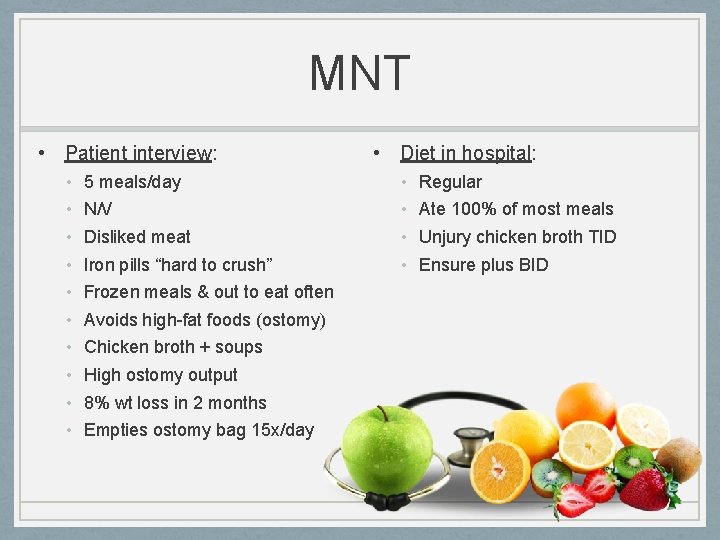
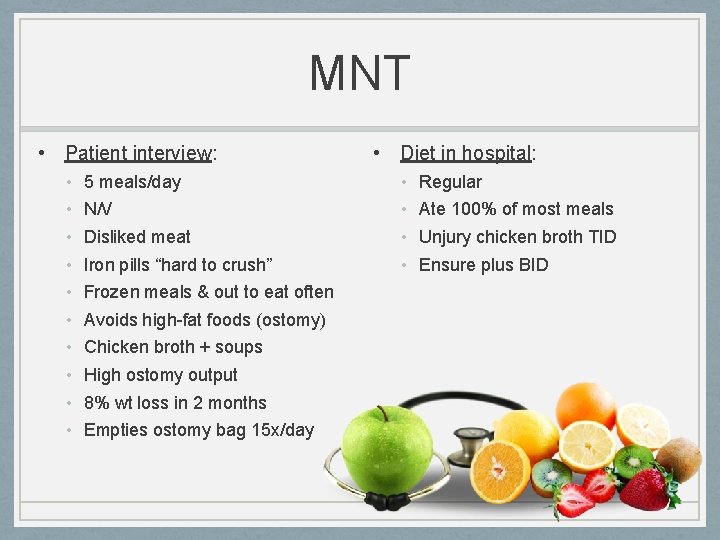
MNT • Patient interview: • • • 5 meals/day N/V Disliked meat Iron pills “hard to crush” Frozen meals & out to eat often Avoids high-fat foods (ostomy) Chicken broth + soups High ostomy output 8% wt loss in 2 months Empties ostomy bag 15 x/day • Diet in hospital: • • Regular Ate 100% of most meals Unjury chicken broth TID Ensure plus BID
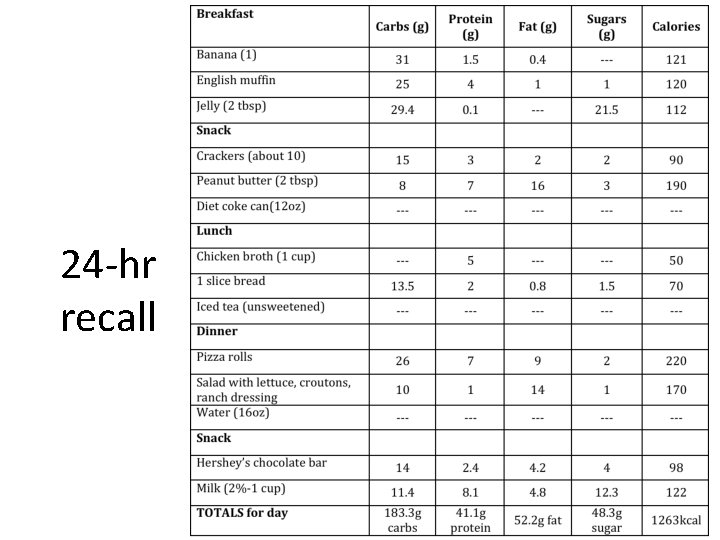
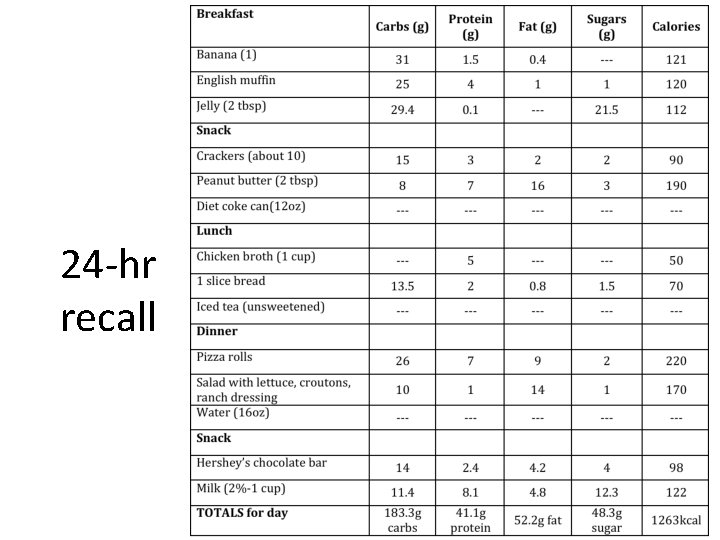
24 -hr recall
Nutrition-Related Problems & Evidence • Malnutrition • Visible muscle wasting, fat store loss, weight loss, poor intake • Altered nutrition-related lab values: • Iron • Calcium • H&H • Underweight • BMI • Inadequate intake • Weight loss • Per patient • Undesirable food choices • Per 24 -hr recall • Per patient

Nutrient Needs • Malnourished with absorptive issues- increased needs • Kcals: 35 -38 g/kg/day • 1415 -1530 kcal/day • Protein: 1. 4 -1. 5 g/kg/day • 55 -60 g PRO/day
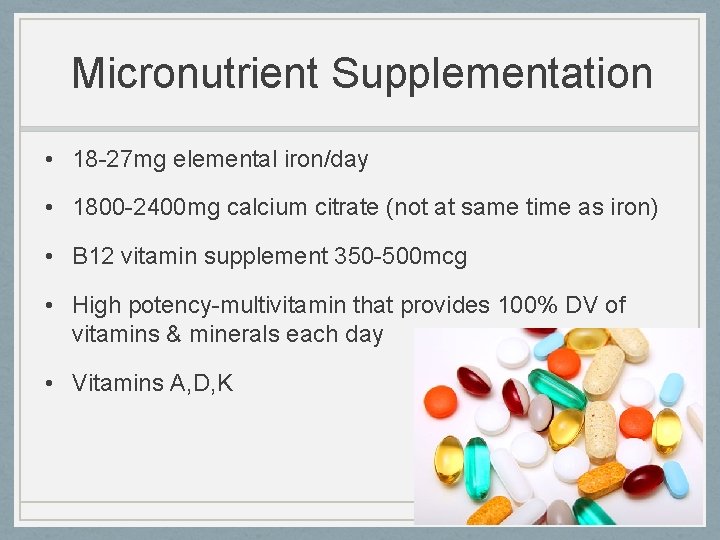
Micronutrient Supplementation • 18 -27 mg elemental iron/day • 1800 -2400 mg calcium citrate (not at same time as iron) • B 12 vitamin supplement 350 -500 mcg • High potency-multivitamin that provides 100% DV of vitamins & minerals each day • Vitamins A, D, K

Nutrition-related recommendations • Increased kcal + protein intake • Calorically dense foodssupplement coupons given • Compliance with iron supplements • Small meals/snacks throughout the day • Hydration • Increased vegetable & fruit intake • Avoiding foods that would affect ileostomy: • • • Sugary foods Carbonation High-fat foods Caffeine Alcohol • Foods high in pectin • To slow down ostomy output

Prognosis • Fair, secondary to hx of noncompliance • Several issues r/t duodenal switch • Adherence to nutrition-related recommendations, compliance with supplements & lower intake of opioids • Patient can improve current state of health
Conclusion • BPD/DS successful for some, but has potential to cause major side effects. • Malnutrition difficult to reverse when normal absorption function is altered • Compliance is important for patients with any GI surgeries or alterations • RD role is vital in patients before & after bariatric surgery, ostomies, or other GI surgeries • Education process important to avoid adverse conditions

References • • • • Digestive System Function & Organs. (2013). Retrieved December 29, 2016, from http: //my. clevelandclinic. org/health/articles/the-structure-and-function-of-the-digestive-system. Stephenson, T. J. , MS, RD, LD. (2015, September). The Digestive System. Lecture presented at Advanced Nutrition Course at University of Kentucky, Lexington, Kentucky. Mahan, K. , Escott-Stump, S. , & Raymond, J. L. (2012). Krause's Food and the Nutrition Care Process (13 th ed. ). St. Louis, MO: Elsevier. Your Digestive System and How It Works. (2013, September). Retrieved December 29, 2016, from https: //www. niddk. nih. gov/health-information/health-topics/Anatomy/your-digestive-system/Pages/anatomy. aspx. Escott-Stump, S. (2012). Nutrition and diagnosis-related care. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. Duodenal Switch (DS). (2014). Retrieved January 09, 2017, from http: //www. cpmc. org/advanced/obesity/ds. html. Nabipour, S. , Said, M. A. , & Habil, M. H. (2014, August). Burden and Nutritional Deficiencies in Opiate Addiction- Systematic Review Article. Retrieved January 09, 2017, from https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 4411899/. BPD/DS Weight-Loss Surgery - Hopkins Medicine. (n. d. ). Retrieved January 9, 2017, from http: //www. hopkinsmedicine. org/healthlibrary/test_procedures/gastroenterology/bpdds_weight-loss_surgery_135, 64/. Bariatric Surgery Procedures - ASMBS. (2017). Retrieved January 09, 2017, from https: //asmbs. org/patients/bariatric-surgery -procedures#bpd. Long-term outcomes after biliopancreatic diversion with. . . (2016). Retrieved January 9, 2017, from http: //www. soard. org/article/S 1550 -7289(16)00096 -4/abstract. Ostomy Information. (2017). Retrieved January 09, 2017, from http: //www. ostomy. org/Ostomy_Information. html#ileostomy. Ostomy; What to eat and drink when you have a high output. . . (2009, November). Retrieved January 9, 2017, from http: //www. hamiltonhealthsciences. ca/documents/Patient%20 Education/High. Output. Ostomy. What. To. Eat-trh. pdf. Jáuregui-Lobera, I. (2013, May). Iron Deficiency and Bariatric Surgery. Retrieved January 09, 2017, from https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 3708339/. Post-Gastrectomy Syndrome Symptoms. (2017). Retrieved January 09, 2017, from http: //my. clevelandclinic. org/health/articles/post-gastrectomy-syndrome-overview. Sovik, T. T. (2011, September 6). Weight Loss, Cardiovascular Risk Factors, and Quality of Life After Gastric Bypass and Duodenal Switch: A Randomized Trial. Retrieved January 9, 2017, from http: //annals. org. ezproxy. uky. edu/aim/article/747095/weight-loss-cardiovascular-risk-factors-quality-life-after-gastricbypass.
 Iron deficiency anemia smear
Iron deficiency anemia smear Elemental iron dose
Elemental iron dose Hypochromic anemia
Hypochromic anemia Labs for iron deficiency anemia
Labs for iron deficiency anemia Iron deficiency anemia
Iron deficiency anemia Ferritin level iron deficiency anemia
Ferritin level iron deficiency anemia Megaloblastic anemia lab values
Megaloblastic anemia lab values Iron deficiency anemia
Iron deficiency anemia Classification of anemia
Classification of anemia A/g ratio high
A/g ratio high Minerals are inorganic elements that the body
Minerals are inorganic elements that the body Losmosis
Losmosis Sleeve gastrectomy complications
Sleeve gastrectomy complications Duodenal switch
Duodenal switch Megaloblastic anemia is caused due to deficiency of
Megaloblastic anemia is caused due to deficiency of Bazophile
Bazophile Pernicious anemia vs megaloblastic anemia
Pernicious anemia vs megaloblastic anemia Iron deficiency in roses
Iron deficiency in roses Microcytic hypochromic anemia
Microcytic hypochromic anemia Sickle cell anemia symptoms
Sickle cell anemia symptoms Malnutrition case presentation
Malnutrition case presentation Mass of iron in an iron tablet
Mass of iron in an iron tablet Iron sharpens iron friendship
Iron sharpens iron friendship The resources need to be reserved during the setup phase in
The resources need to be reserved during the setup phase in Leverless limit switch
Leverless limit switch Best case worst case average case
Best case worst case average case Anemia case study
Anemia case study