Case History 67 yo F Progressive visual loss
- Slides: 17
Case History • 67 yo F Progressive visual loss in the SO associated with corneal degeneration and a limbal tumor • Gross description – Opaque white tissue measures 13 x 12 mm – Extends from the limbus to the edge of cornea
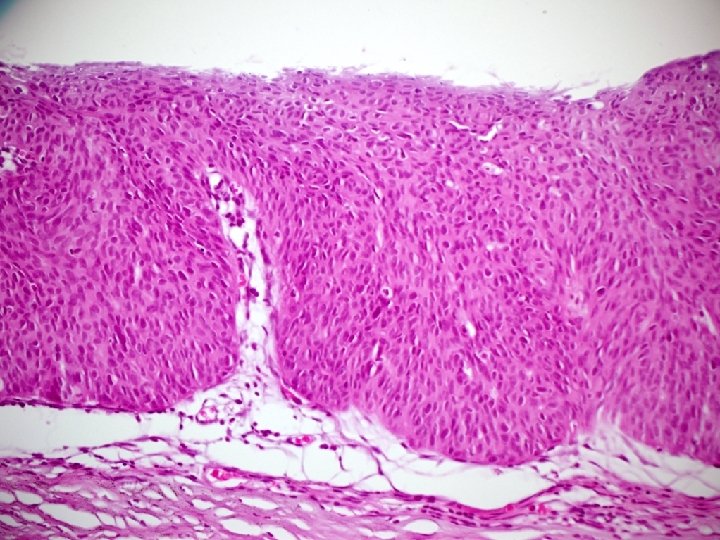
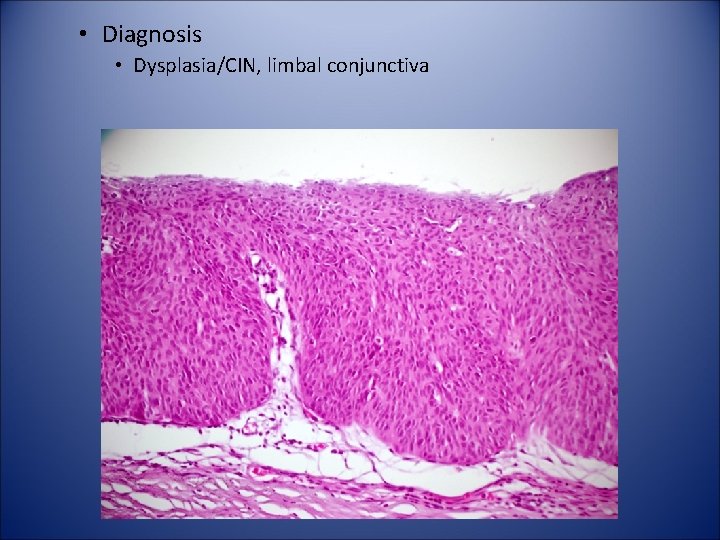
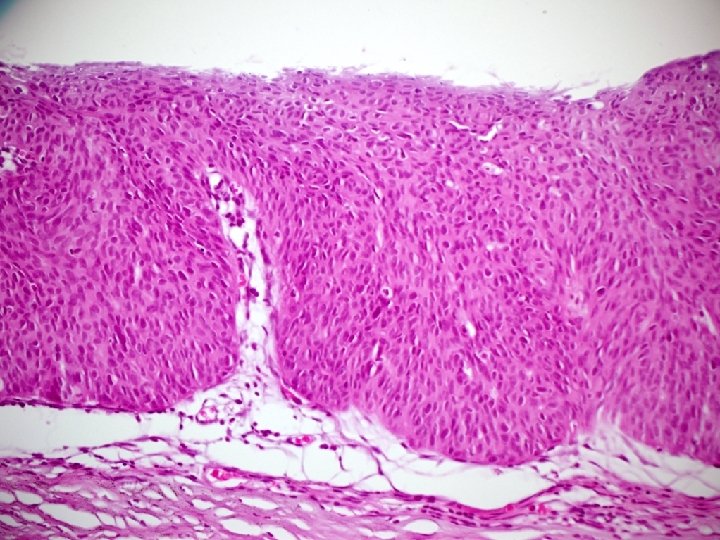
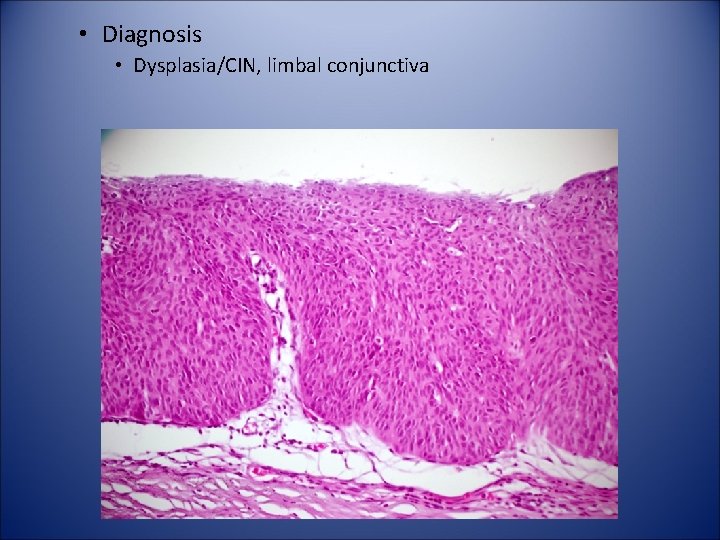
• Diagnosis • Dysplasia/CIN, limbal conjunctiva
Conjunctival intraepithelial neoplasm (CIN) • Definition: CIN includes a wide range of neoplastic intraepithelial changes ranging from dysplasia to full-thickness epithelial neoplasia or carcinoma in situ • Synonyms include mild, moderate, and severe dysplasia, carcinoma in situ, ocular surface squamous neoplasia, intraepithelioma and bowenoid dyskeratosis
CIN • Clinically, lesions are sharply demarcated and arise at the limbus, where corneal stem cells are located, with either or both conjunctival and corneal involvement. • Most lesions are pink, nonkeratinized, wellvascularized and have a raspberry-like configuration. • Rarely, these changes spontaneously regress.
CIN • Microscopic findings – Keratinization and dyskeratosis are not a common feature of CIN. – Atypical mitosis are frequent and may be located at all levels of the epithelium. – The intraepithelium dysplastic changes are graded as mild, moderate, or severe based on the thickness of intraepithelial involvement.
CIN • Differential diagnosis. – UV-related epithelial hyperplasia – Intraepithelial sebaceous gland carcinoma – Inraepithelial invasion by adenocarcinoma originating from aprocrine glands of moll – Primary acquired melanosis (HMB 45, S-100, Melan A)
Case 2
Case History • 50 yo F • 2 Y/H progressively enlarging pigmented area involving the conjunctiva and cornea of the left eye. • 3 X 3. 5 mm. pigmented limbal nodule appeared in this area of heavily pigmented conjunctiva, which had been previously biopsied and diagnosed as “primary acquired melanosis”
Case History (Cont. ) • The left eye and a broad zone of bulbar conjunctiva were excised because of the clinical diagnosis of malignant melanoma of the conjunctiva.
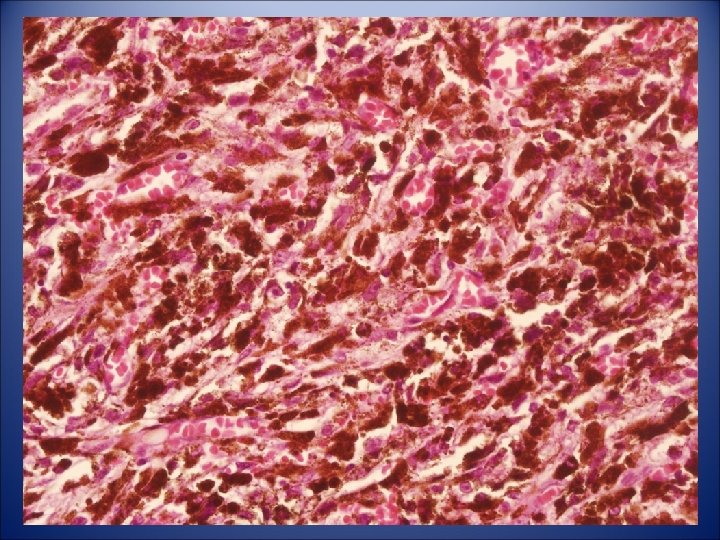
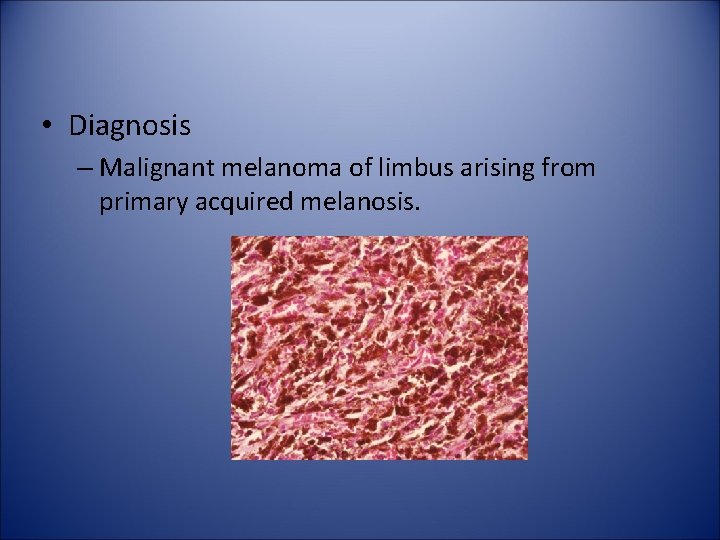
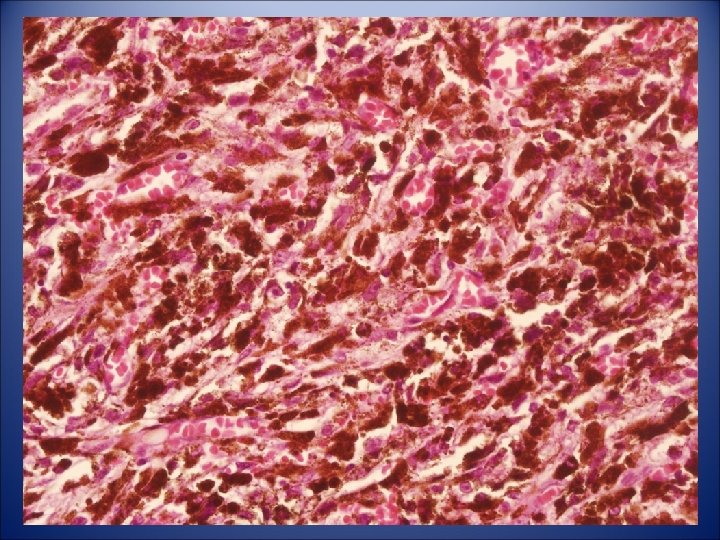
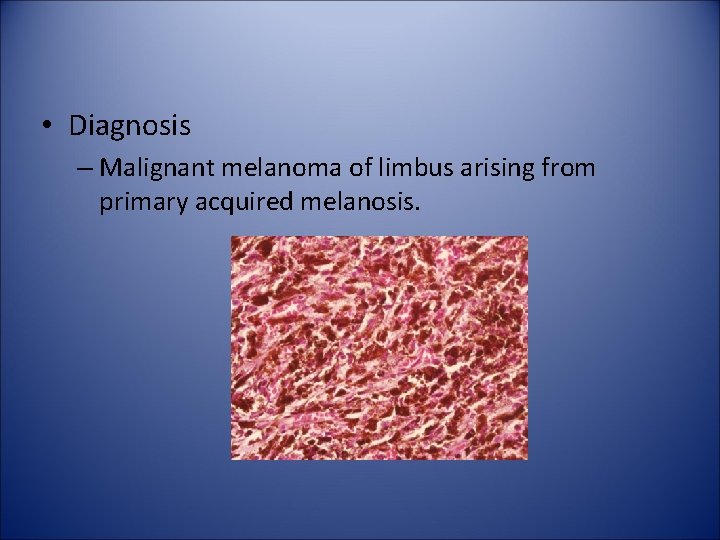
• Diagnosis – Malignant melanoma of limbus arising from primary acquired melanosis.
Melanocytic tumors of the conjunctiva • • • Ephelis(Freckle) Lentigo Nevus Primary Acquired Melanosis(PAM) Malignant Melanoma
PAM • Clinical Characteristics – The melanosis of unilateral, diffuse, brown pigmentation that moves with the conjunctiva over the sclera (analogous to lentigo maligna of the skin). – Age of onset is 40 to 50 years of age. – No clinical differentiation in PAM with or without atypia
Corneal Cases
Case 3
Case History • • • 60 yo M H/O Pseudophakic bullous keratopathy Waxing and waning corneal edema Decreased vision in his left eye Penetrating keratoplasty