Case 6 Acute Coronary Syndromes 2001 American Heart
- Slides: 42
Case 6 Acute Coronary Syndromes © 2001 American Heart Association 1
Learning Objectives At the end of Case 6 be able to u Define acute coronary syndromes u Use the Ischemic Chest Pain Algorithm u Consider the Why? (actions), When? (indications), How? (dose), and Watch Out! (precautions) of medications for ischemic chest pain patients 2
Learning Objectives (cont’d) At the end of Case 6 be able to u Recognize significant ST-segment changes u Know how to measure ST-segment elevation and depression u Know basic principles of anatomic localization of infarct, injury, and ischemia u Know how to use the ECG to risk-stratify patients 3
Case 1 A 55 -year-old man presents with a chief complaint of severe (10 of 10) substernal chest pain. He has pain radiating down his left arm and up into his jaw, nausea, and a profound sense of impending doom. He is covered with small beads of sweat. Vital signs: TEMP = 37. 2°C; HR = 110 bpm; BP = 150/100 mm Hg; RESP = 12 Describe your immediate assessment. Describe your immediate general treatment. 4
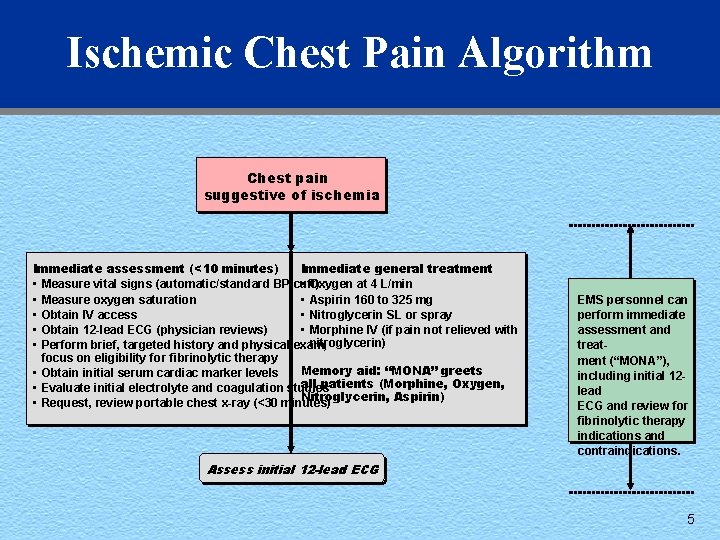
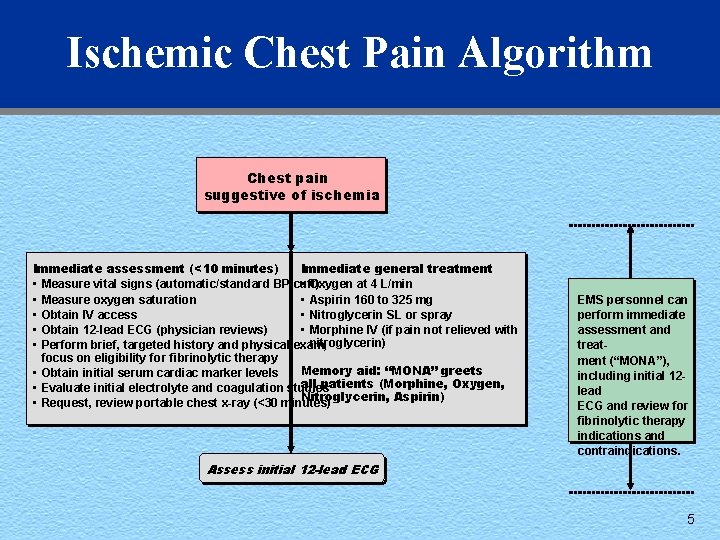
Ischemic Chest Pain Algorithm Chest pain suggestive of ischemia Immediate assessment (<10 minutes) Immediate general treatment • Measure vital signs (automatic/standard BP cuff) • Oxygen at 4 L/min • Measure oxygen saturation • Aspirin 160 to 325 mg • Obtain IV access • Nitroglycerin SL or spray • Obtain 12 -lead ECG (physician reviews) • Morphine IV (if pain not relieved with nitroglycerin) • Perform brief, targeted history and physical exam; focus on eligibility for fibrinolytic therapy Memory aid: “MONA” greets • Obtain initial serum cardiac marker levels all patients (Morphine, Oxygen, • Evaluate initial electrolyte and coagulation studies Nitroglycerin, Aspirin) • Request, review portable chest x-ray (<30 minutes) EMS personnel can perform immediate assessment and treatment (“MONA”), including initial 12 lead ECG and review for fibrinolytic therapy indications and contraindications. Assess initial 12 -lead ECG 5
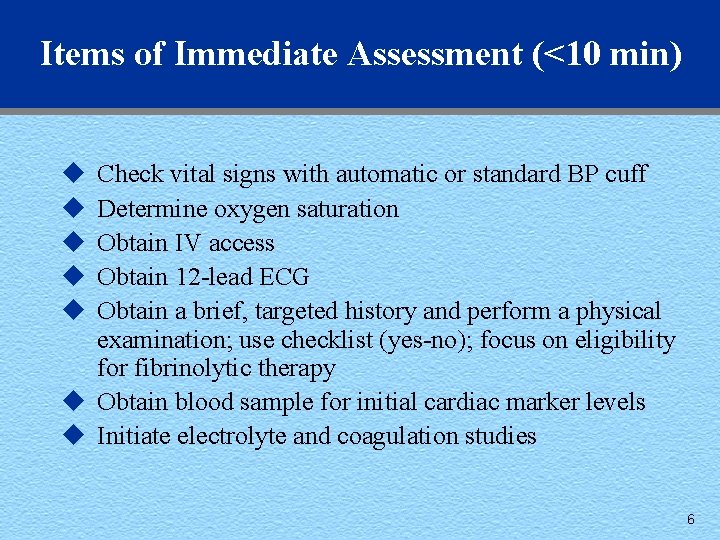
Items of Immediate Assessment (<10 min) u u u Check vital signs with automatic or standard BP cuff Determine oxygen saturation Obtain IV access Obtain 12 -lead ECG Obtain a brief, targeted history and perform a physical examination; use checklist (yes-no); focus on eligibility for fibrinolytic therapy u Obtain blood sample for initial cardiac marker levels u Initiate electrolyte and coagulation studies 6
Immediate General Treatment u Oxygen at 4 L/min u Aspirin 160 to 325 mg u Nitroglycerin SL or spray u Morphine IV (if pain not relieved with nitroglycerin) Review the Why? (actions), When? (indications), How? (dose), and Watch Out! (precautions) of these medications to consider in patients with ischemic chest pain. 7
Medications Used in ACLS u Why? (Actions) u When? (Indications) u How? (Dose) u Watch Out! (Precautions) 8
Oxygen Used in Acute Coronary Syndromes Why? u Increases supply of oxygen to ischemic tissue When? u Always when AMI is suspected How? u Start with nasal cannula at 4 L/min u Remember one word: oxygen-IV-monitor Watch Out! u Rarely COPD patients with hypoxic ventilatory drive will hypoventilate 9
Nitroglycerin: Actions u Decreases pain of ischemia u Increases venous dilation u Decreases venous blood return to heart u Decreases preload and cardiac oxygen consumption u Dilates coronary arteries u Increases cardiac collateral flow 10
Nitroglycerin: Indications u Class I: First 24 to 48 hours in patients with ST-segment elevation or depression including • • LV failure (acute pulmonary edema or CHF) Elevated BP (especially with signs of LV failure) Large anterior infarction Persistent ischemia u Suspected ischemic chest pain u Unstable angina (change in angina pattern) u Acute pulmonary edema (if BP >90 mm Hg systolic) 11
Nitroglycerin: Dose u Sublingual: 0. 3 to 0. 4 mg; repeat every 5 minutes u Spray inhaler: 2 metered doses at 5 -minute intervals u IV infusion: 12. 5 to 25 g bolus, 10 to 20 g/min infusion, titrated 12
Nitroglycerin: Precautions u Use extreme caution if systolic BP <90 mm Hg u Use extreme caution in RV infarction – Suspect RV infarction with inferior ST changes u Limit BP drop to 10% if patient is normotensive u Limit BP drop to 30% if patient is hypertensive u Watch for headache, drop in BP, syncope, tachycardia u Tell patient to sit or lie down during administration 13
Morphine Sulfate: Actions, Indications u Why? (Actions) • To reduce pain of ischemia • To reduce anxiety • To reduce extension of ischemia by reducing oxygen demands u When? (Indications) • Continuing pain • Evidence of vascular congestion (acute pulmonary edema) • Systolic blood pressure >90 mm Hg • No hypovolemia 14
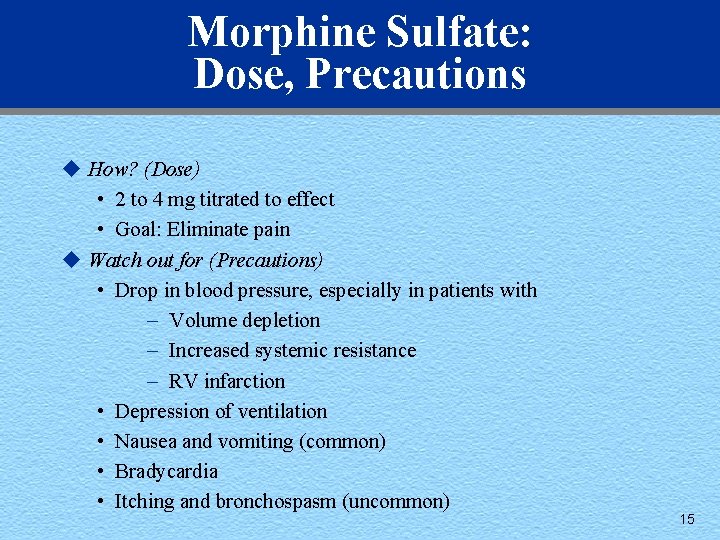
Morphine Sulfate: Dose, Precautions u How? (Dose) • 2 to 4 mg titrated to effect • Goal: Eliminate pain u Watch out for (Precautions) • Drop in blood pressure, especially in patients with – Volume depletion – Increased systemic resistance – RV infarction • Depression of ventilation • Nausea and vomiting (common) • Bradycardia • Itching and bronchospasm (uncommon) 15
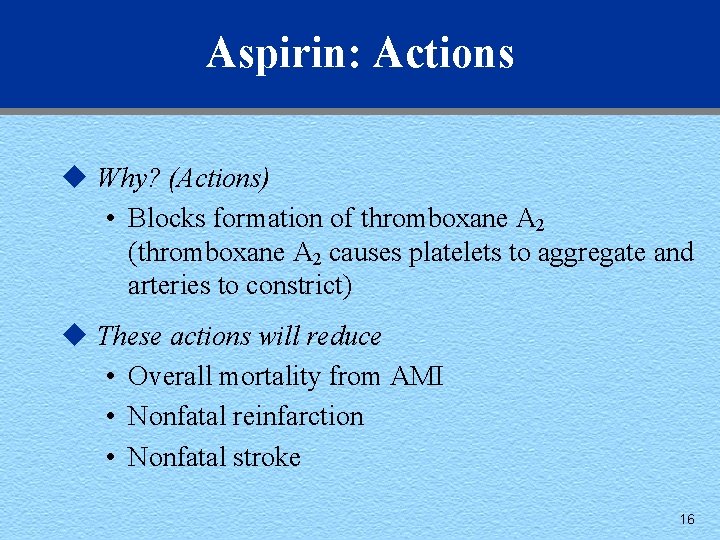
Aspirin: Actions u Why? (Actions) • Blocks formation of thromboxane A 2 (thromboxane A 2 causes platelets to aggregate and arteries to constrict) u These actions will reduce • Overall mortality from AMI • Nonfatal reinfarction • Nonfatal stroke 16
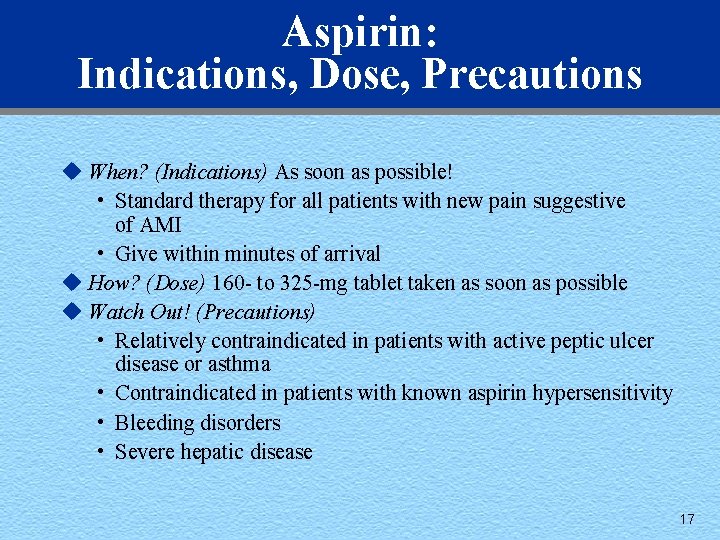
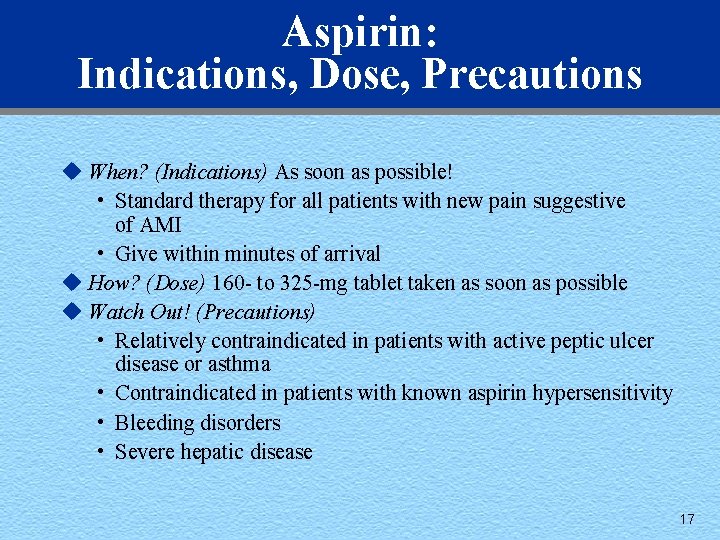
Aspirin: Indications, Dose, Precautions u When? (Indications) As soon as possible! • Standard therapy for all patients with new pain suggestive of AMI • Give within minutes of arrival u How? (Dose) 160 - to 325 -mg tablet taken as soon as possible u Watch Out! (Precautions) • Relatively contraindicated in patients with active peptic ulcer disease or asthma • Contraindicated in patients with known aspirin hypersensitivity • Bleeding disorders • Severe hepatic disease 17
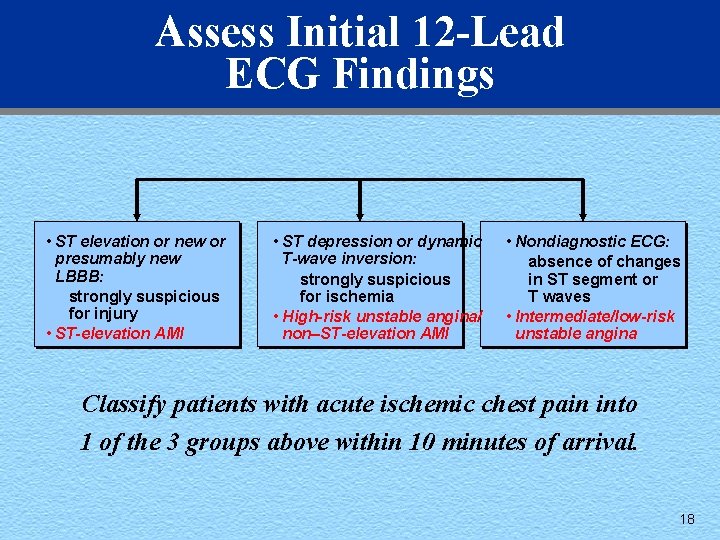
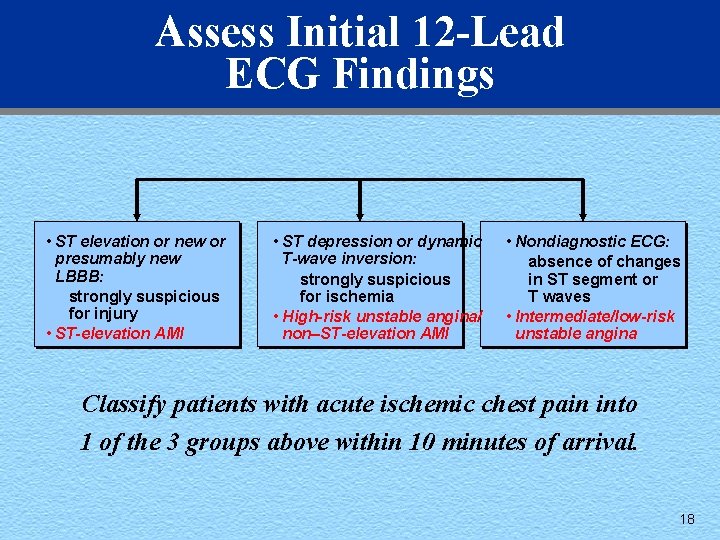
Assess Initial 12 -Lead ECG Findings • ST elevation or new or presumably new LBBB: strongly suspicious for injury • ST-elevation AMI • ST depression or dynamic T-wave inversion: strongly suspicious for ischemia • High-risk unstable angina/ non–ST-elevation AMI • Nondiagnostic ECG: absence of changes in ST segment or T waves • Intermediate/low-risk unstable angina Classify patients with acute ischemic chest pain into 1 of the 3 groups above within 10 minutes of arrival. 18
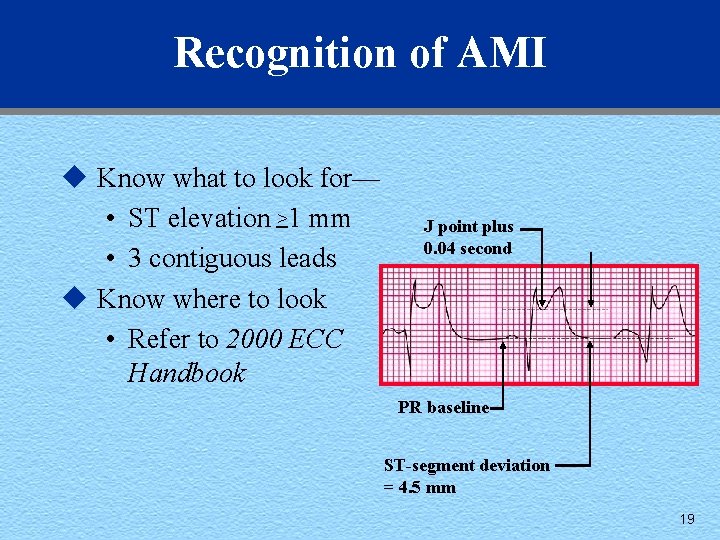
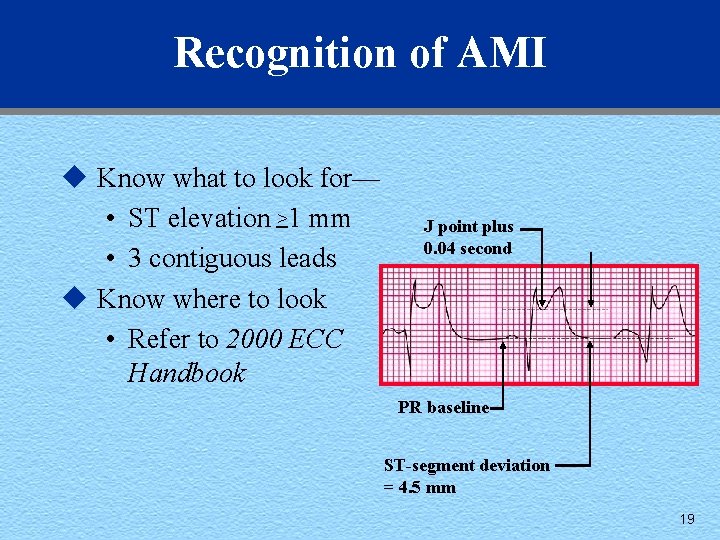
Recognition of AMI u Know what to look for— • ST elevation >1 mm • 3 contiguous leads u Know where to look • Refer to 2000 ECC Handbook J point plus 0. 04 second PR baseline ST-segment deviation = 4. 5 mm 19
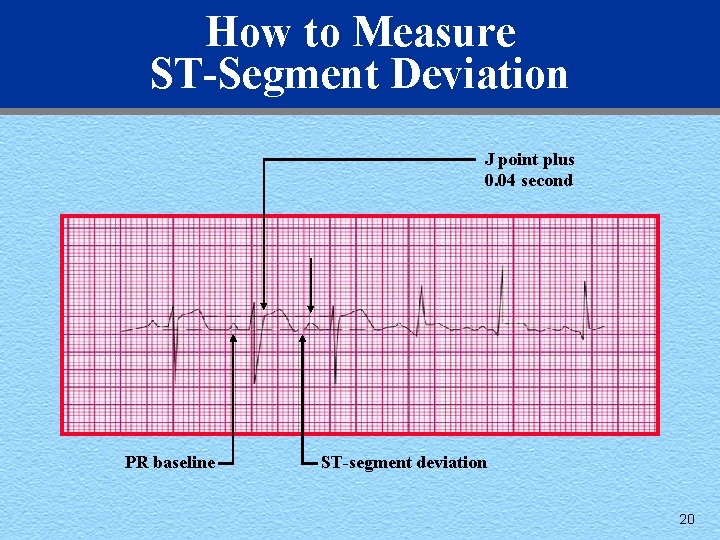
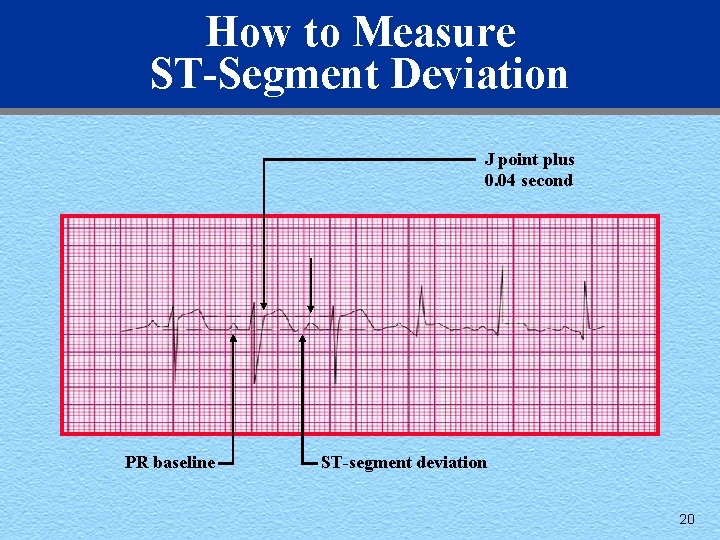
How to Measure ST-Segment Deviation J point plus 0. 04 second PR baseline ST-segment deviation 20
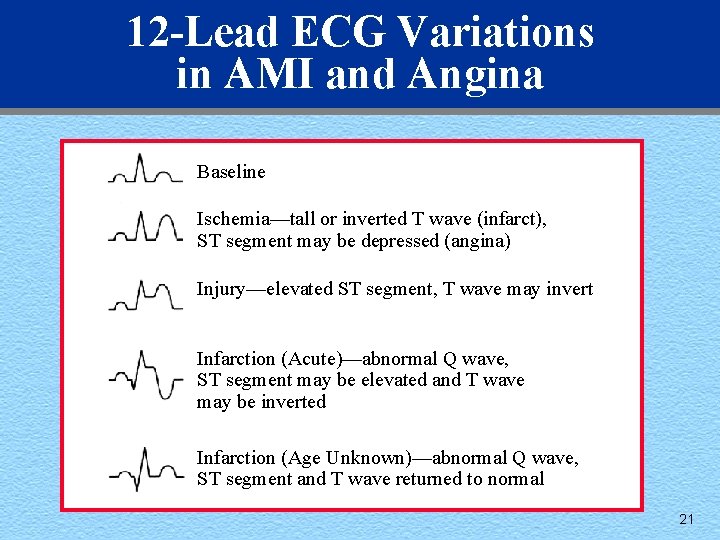
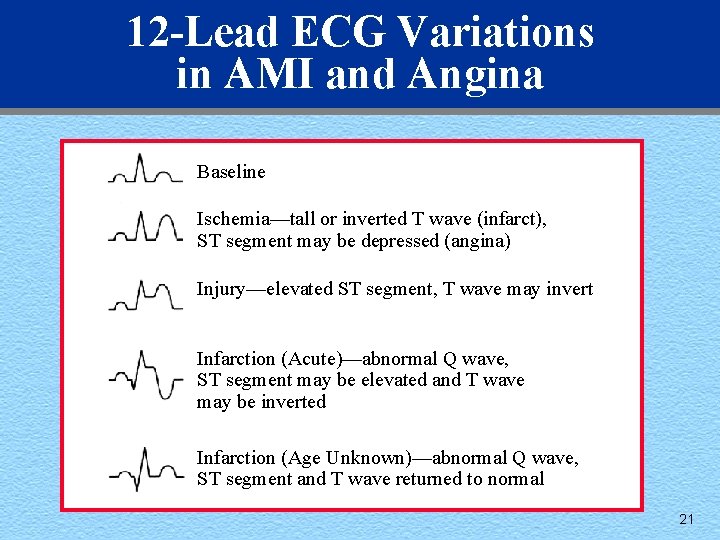
12 -Lead ECG Variations in AMI and Angina Baseline Ischemia—tall or inverted T wave (infarct), ST segment may be depressed (angina) Injury—elevated ST segment, T wave may invert Infarction (Acute)—abnormal Q wave, ST segment may be elevated and T wave may be inverted Infarction (Age Unknown)—abnormal Q wave, ST segment and T wave returned to normal 21
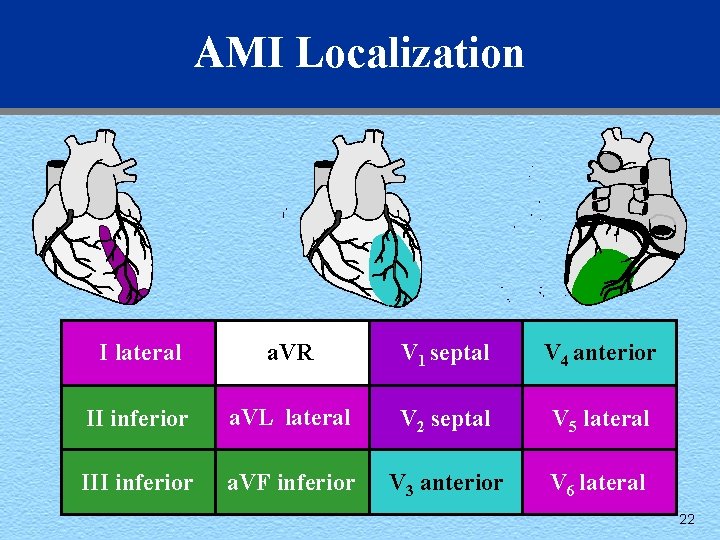
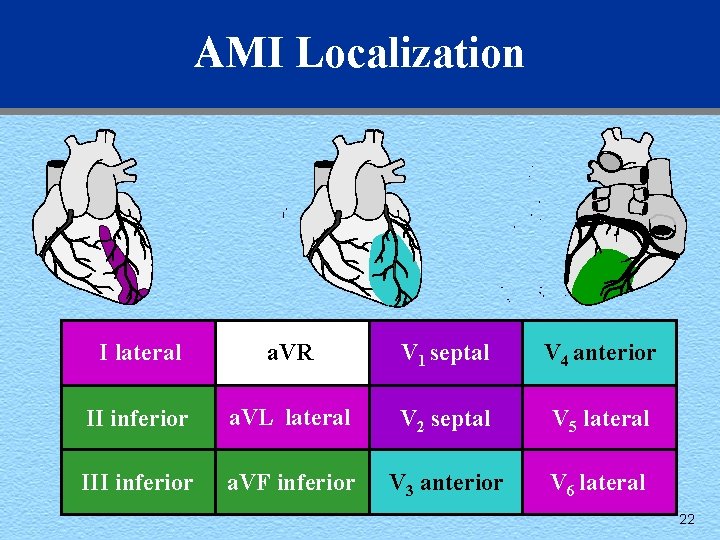
AMI Localization I lateral a. VR V 1 septal V 4 anterior II inferior a. VL lateral V 2 septal V 5 lateral III inferior a. VF inferior V 3 anterior V 6 lateral 22
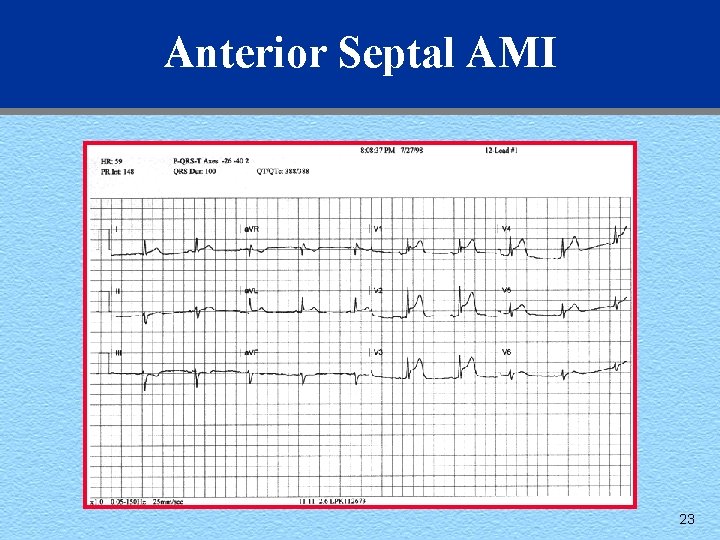
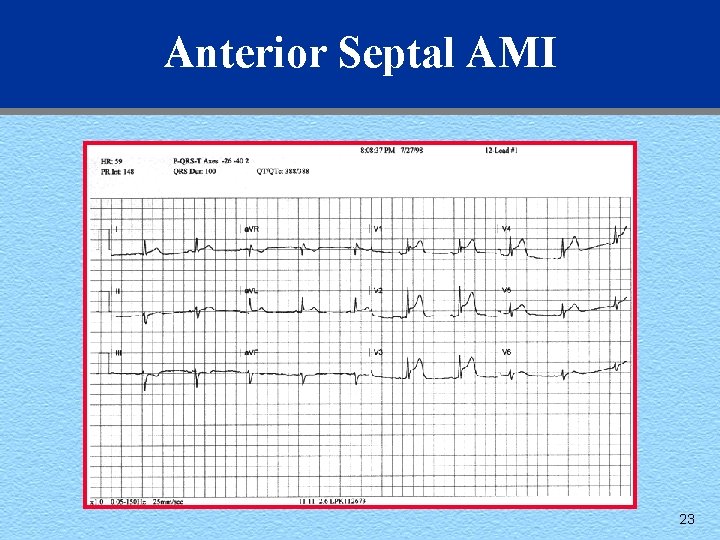
Anterior Septal AMI 23
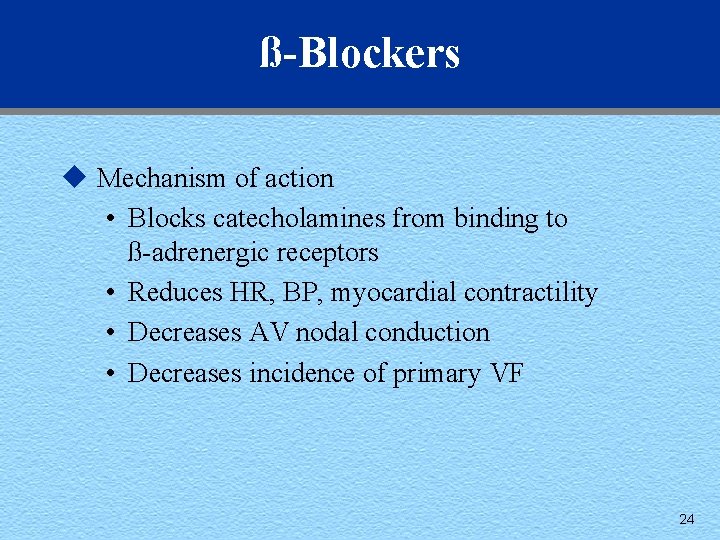
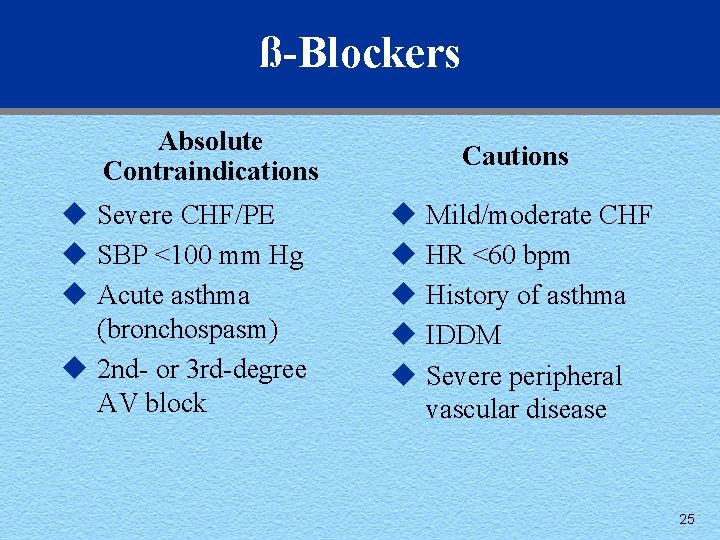
ß-Blockers u Mechanism of action • Blocks catecholamines from binding to ß-adrenergic receptors • Reduces HR, BP, myocardial contractility • Decreases AV nodal conduction • Decreases incidence of primary VF 24
ß-Blockers Absolute Contraindications u Severe CHF/PE u SBP <100 mm Hg u Acute asthma (bronchospasm) u 2 nd- or 3 rd-degree AV block Cautions u Mild/moderate CHF u HR <60 bpm u History of asthma u IDDM u Severe peripheral vascular disease 25
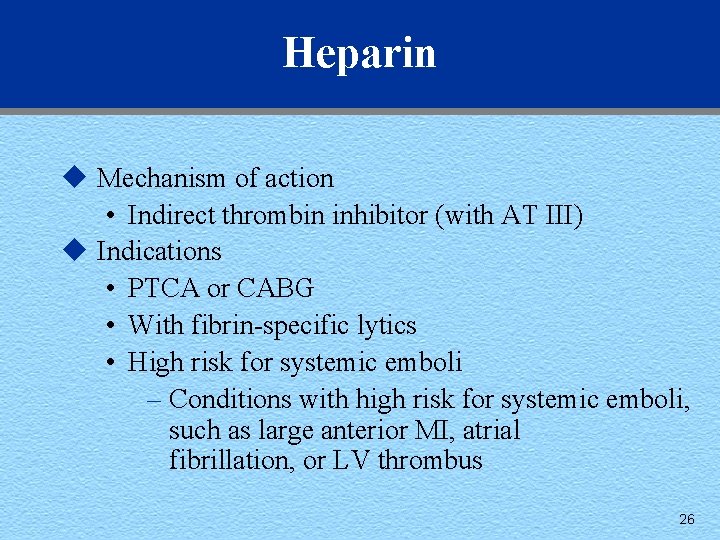
Heparin u Mechanism of action • Indirect thrombin inhibitor (with AT III) u Indications • PTCA or CABG • With fibrin-specific lytics • High risk for systemic emboli – Conditions with high risk for systemic emboli, such as large anterior MI, atrial fibrillation, or LV thrombus 26
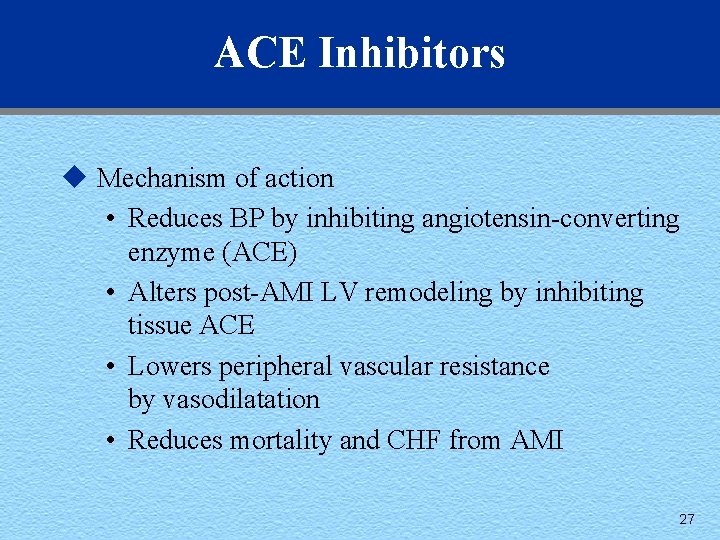
ACE Inhibitors u Mechanism of action • Reduces BP by inhibiting angiotensin-converting enzyme (ACE) • Alters post-AMI LV remodeling by inhibiting tissue ACE • Lowers peripheral vascular resistance by vasodilatation • Reduces mortality and CHF from AMI 27
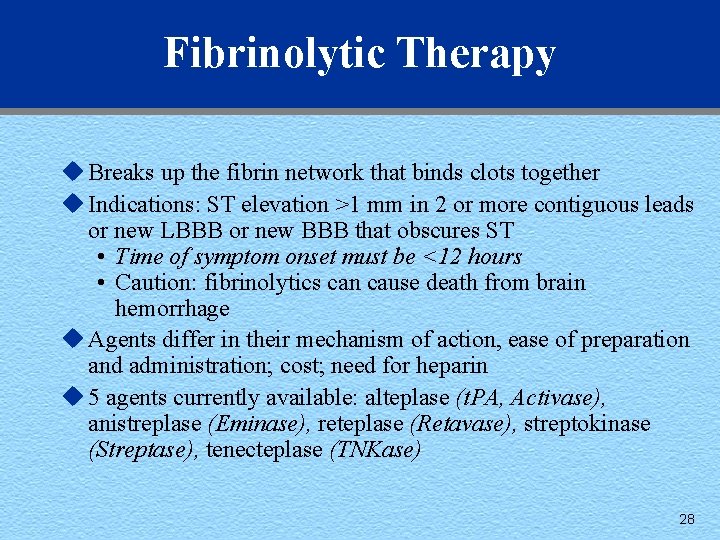
Fibrinolytic Therapy u Breaks up the fibrin network that binds clots together u Indications: ST elevation >1 mm in 2 or more contiguous leads or new LBBB or new BBB that obscures ST • Time of symptom onset must be <12 hours • Caution: fibrinolytics can cause death from brain hemorrhage u Agents differ in their mechanism of action, ease of preparation and administration; cost; need for heparin u 5 agents currently available: alteplase (t. PA, Activase), anistreplase (Eminase), reteplase (Retavase), streptokinase (Streptase), tenecteplase (TNKase) 28
Antiplatelet Agents u Blocks glycoprotein IIb/IIIa receptors on platelets u Blocked receptors cannot attach to fibrinogen u Fibrinogen cannot aggregate platelets to platelets u Indications: ACS with NO ST-segment elevation: • Non–Q-wave MI • Unstable angina managed medically • UA undergoing PCI u Examples: abciximab (Reo. Pro), eptifibitide (Integrilin), tirofiban (Aggrastat) 29
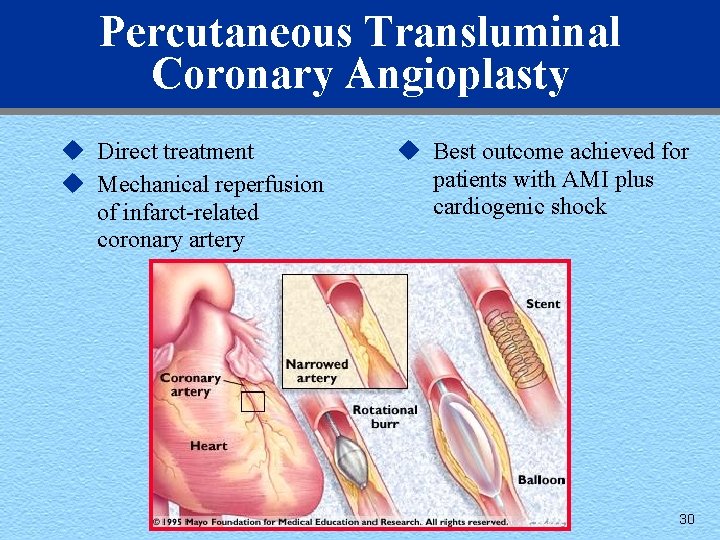
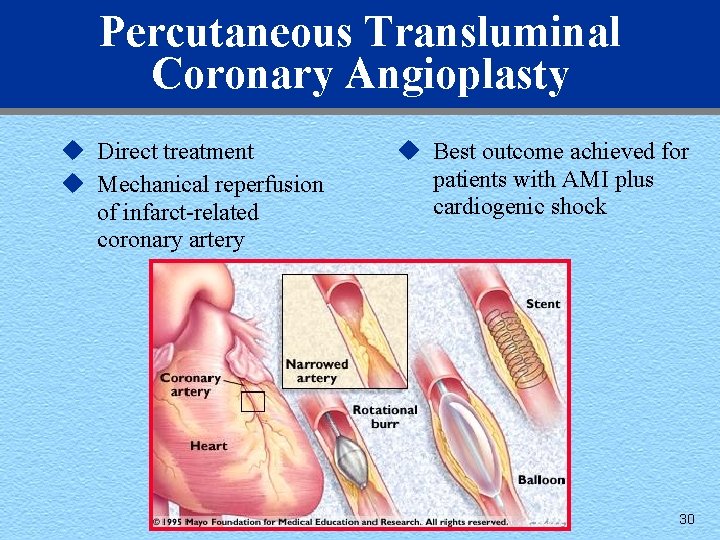
Percutaneous Transluminal Coronary Angioplasty u Direct treatment u Mechanical reperfusion of infarct-related coronary artery u Best outcome achieved for patients with AMI plus cardiogenic shock 30
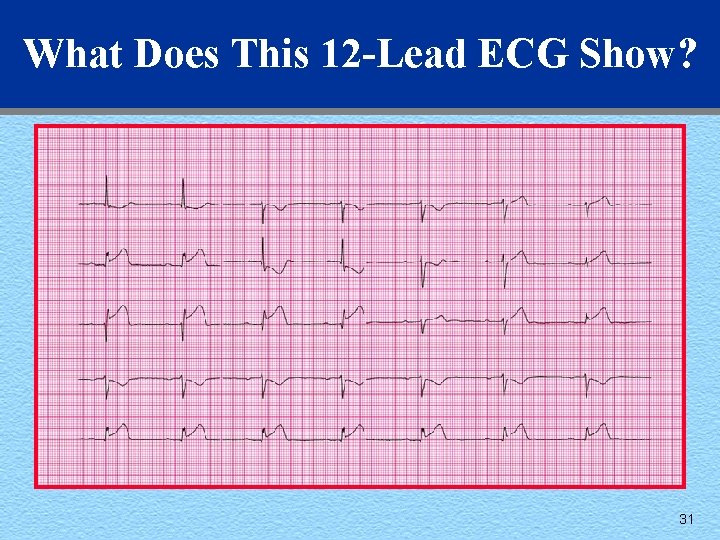
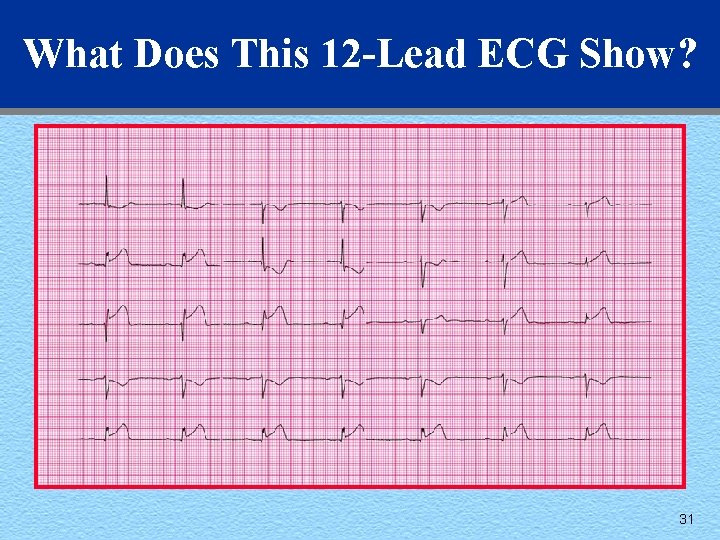
What Does This 12 -Lead ECG Show? 31
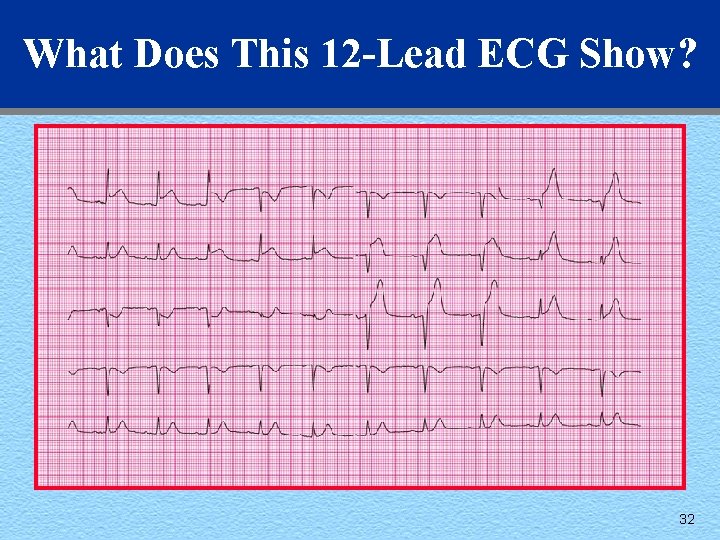
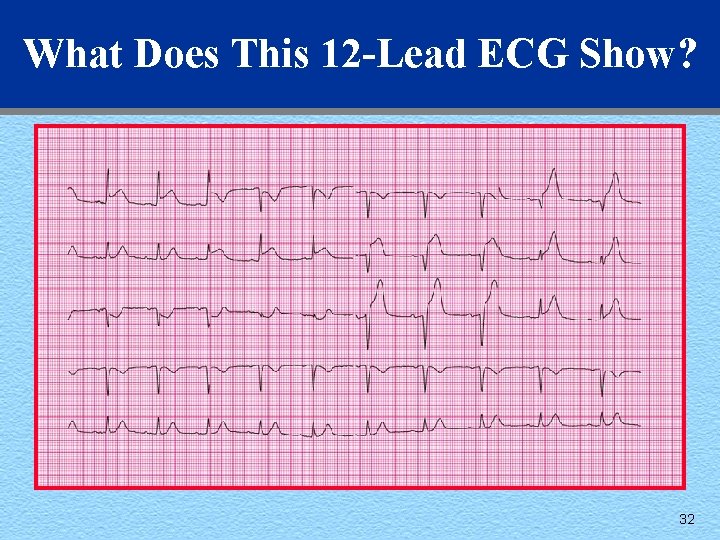
What Does This 12 -Lead ECG Show? 32
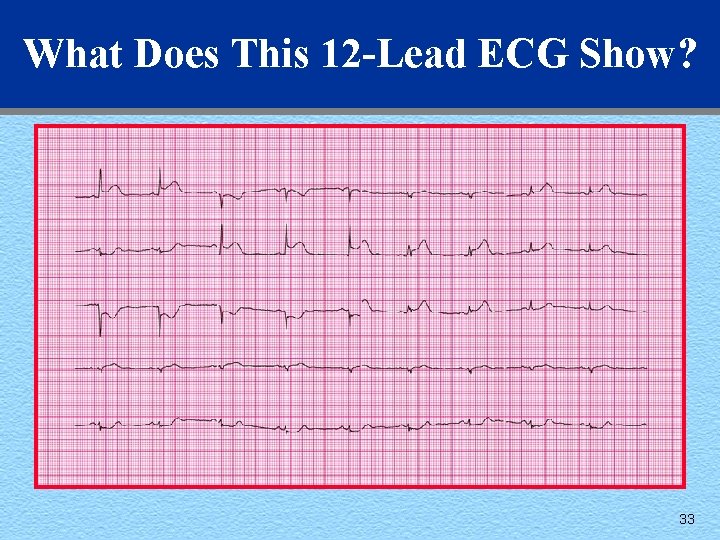
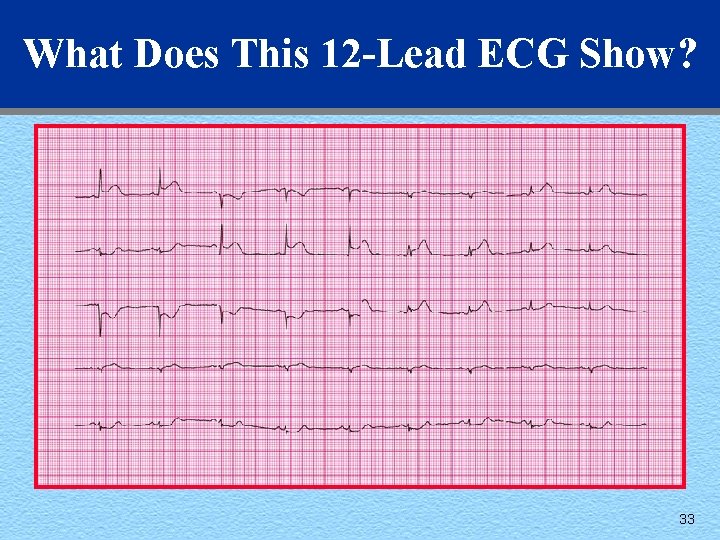
What Does This 12 -Lead ECG Show? 33
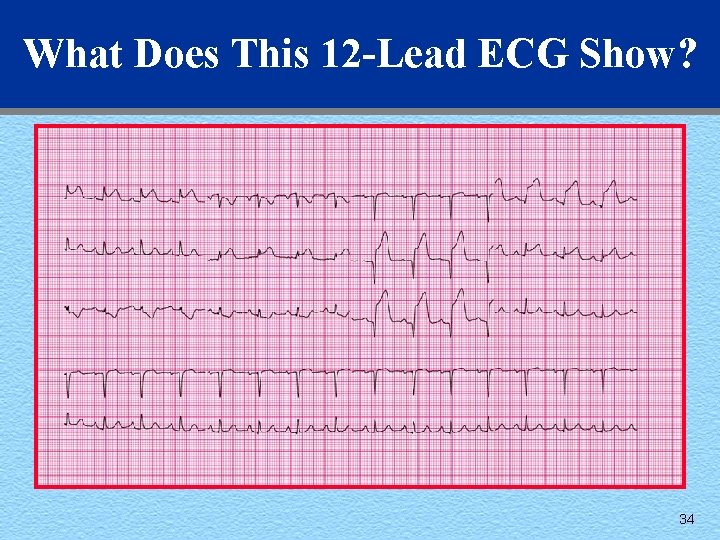
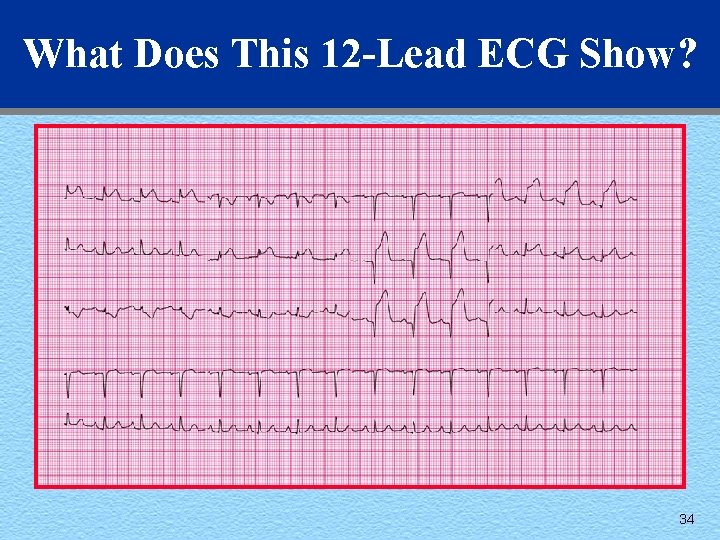
What Does This 12 -Lead ECG Show? 34
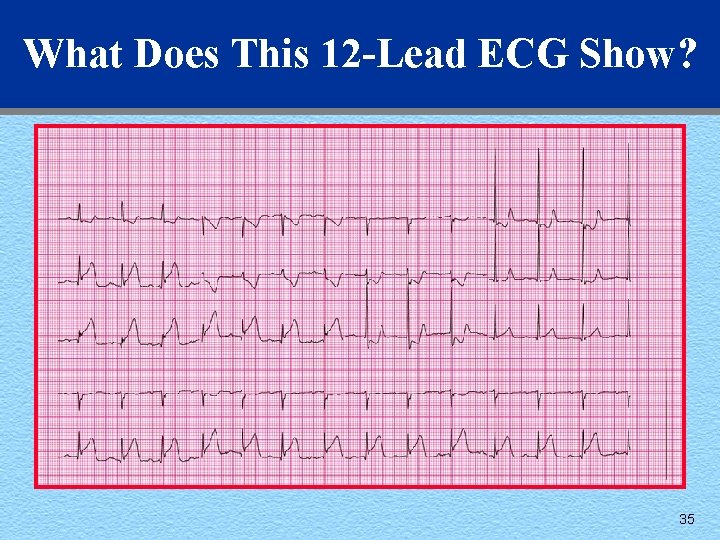
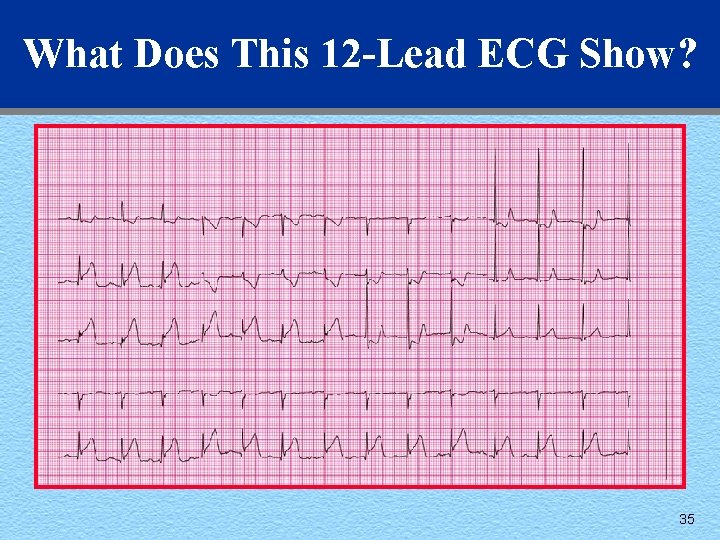
What Does This 12 -Lead ECG Show? 35
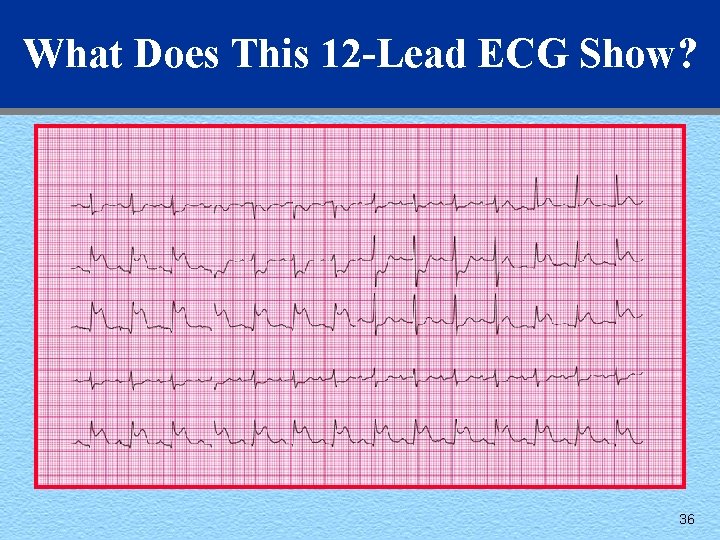
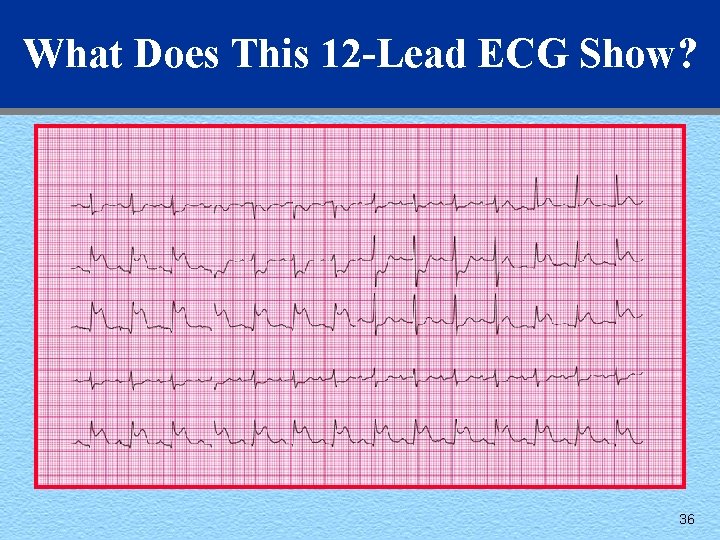
What Does This 12 -Lead ECG Show? 36
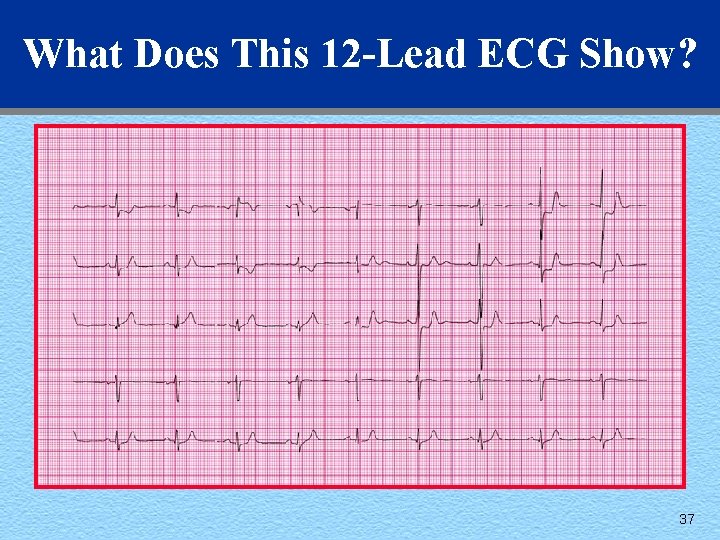
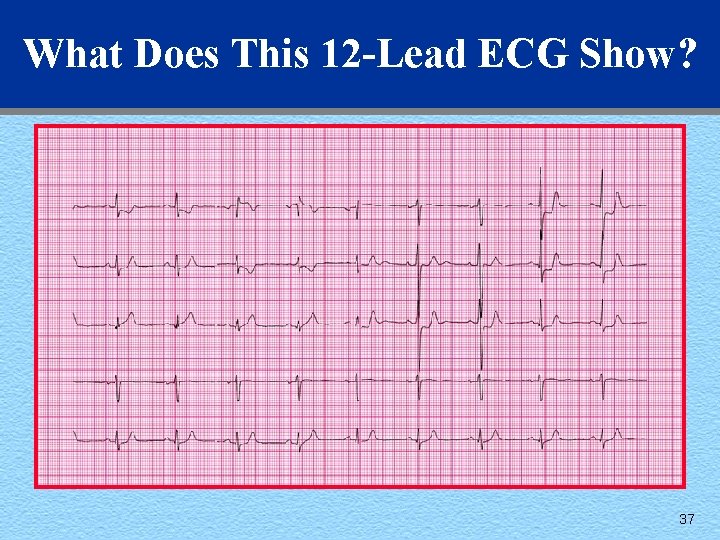
What Does This 12 -Lead ECG Show? 37
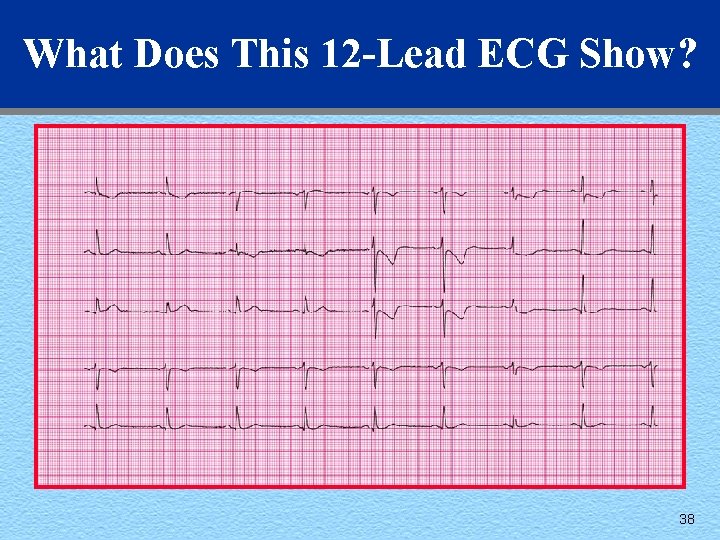
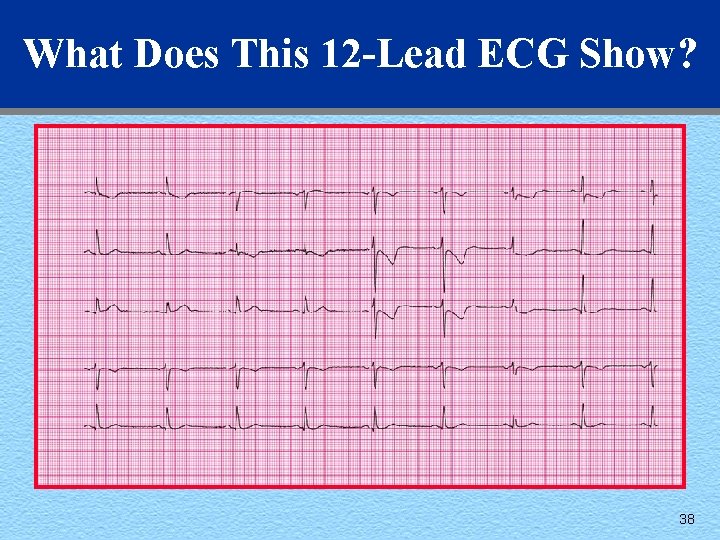
What Does This 12 -Lead ECG Show? 38
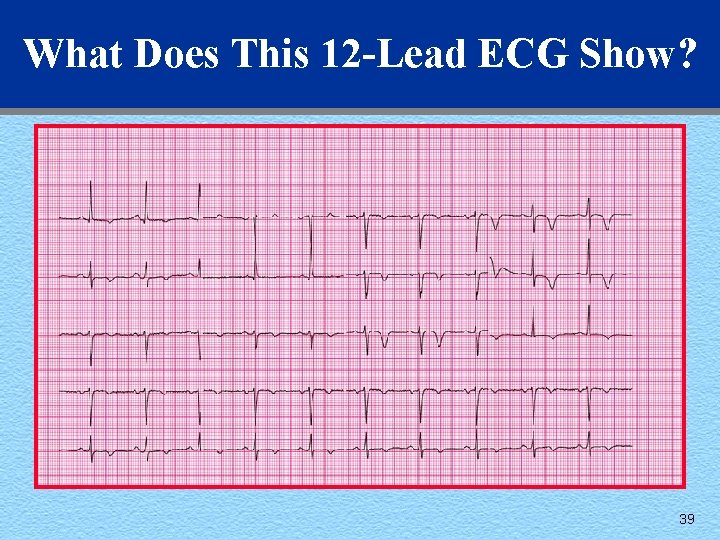
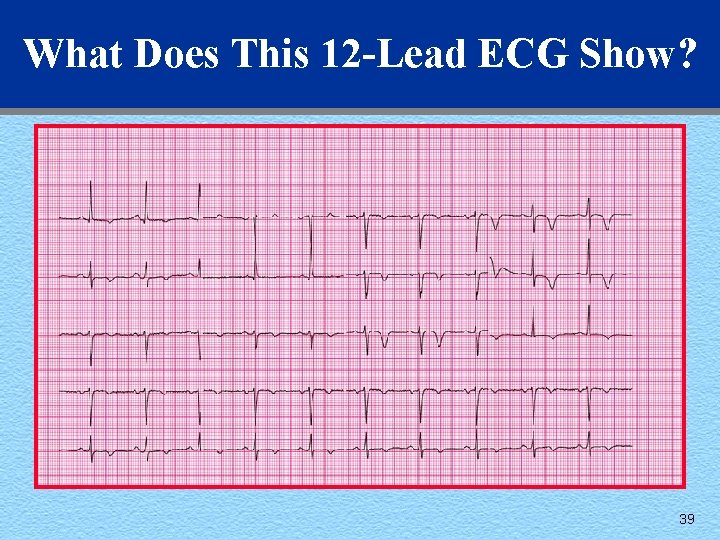
What Does This 12 -Lead ECG Show? 39
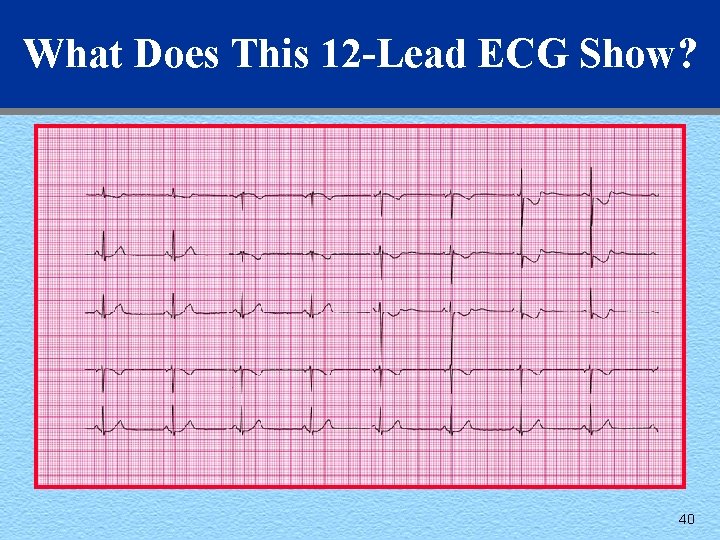
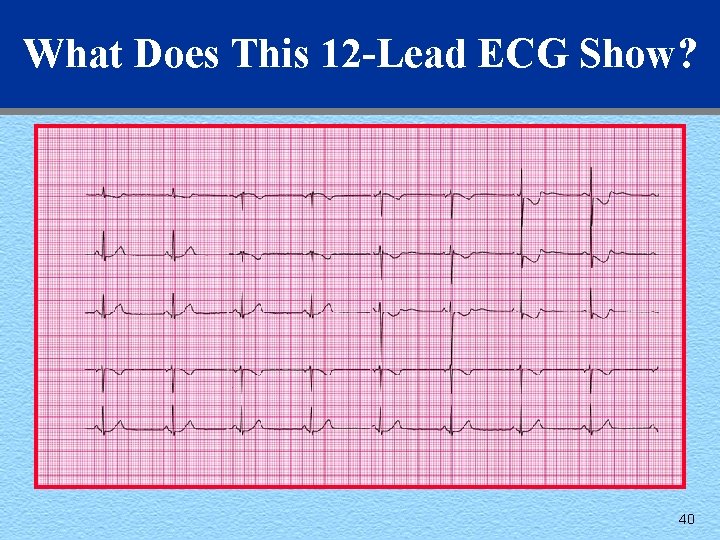
What Does This 12 -Lead ECG Show? 40
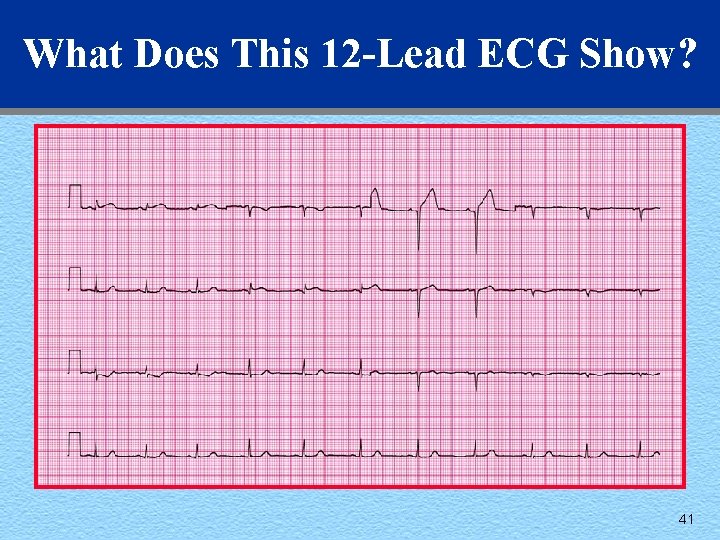
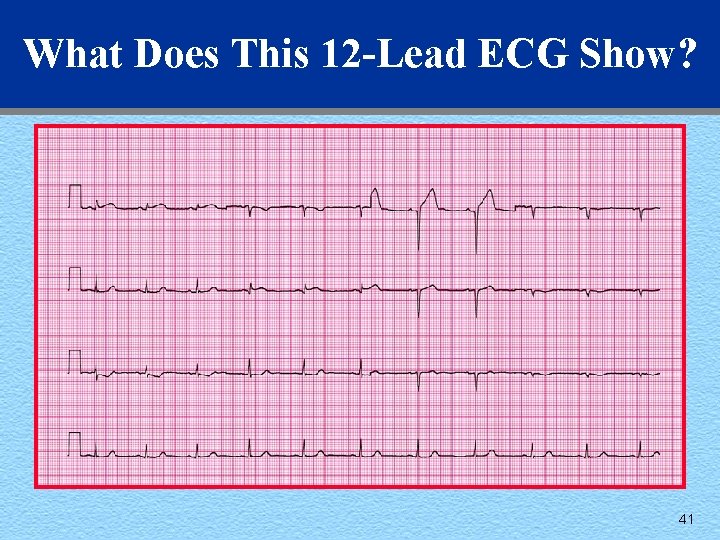
What Does This 12 -Lead ECG Show? 41
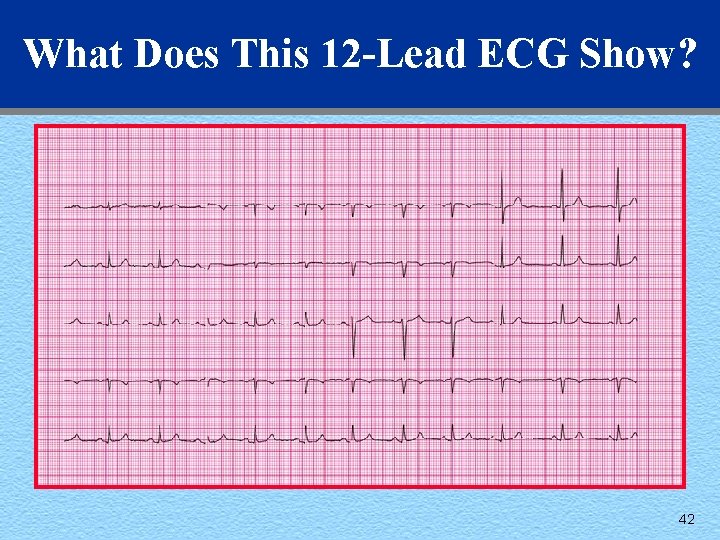
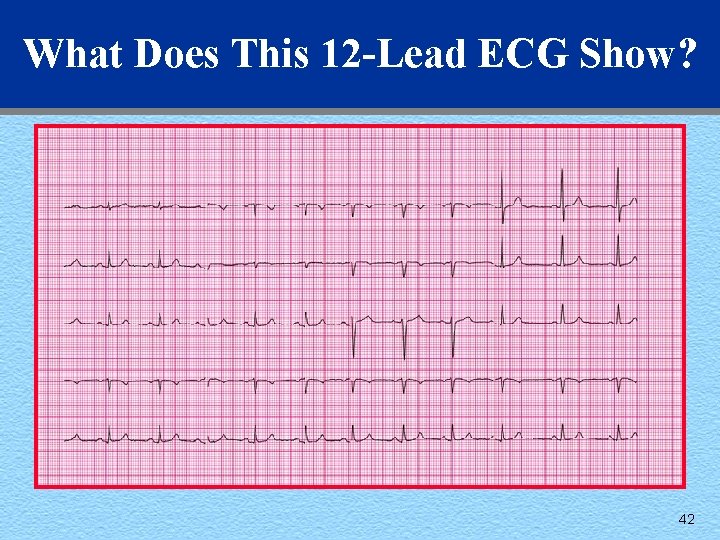
What Does This 12 -Lead ECG Show? 42