Cartilage Stiffness and Thickness Distributions Revealed by an
Cartilage Stiffness and Thickness Distributions Revealed by an Automated Indentation Technique in the Temporomandibular Joint Sotcheadt Sim, Andrea Matuska, Martin Garon, Eric Quenneville, Peter Mc. Fetridge and Michael D. Buschmann TMJ Bioengineering Conference Barcelona, Spain September 12 -13, 2016
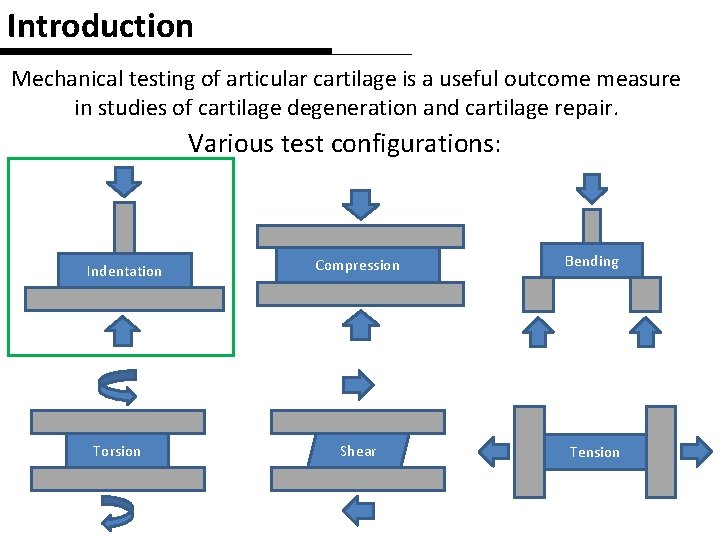
Introduction Mechanical testing of articular cartilage is a useful outcome measure in studies of cartilage degeneration and cartilage repair. Various test configurations: Indentation Torsion Compression Bending Shear Tension
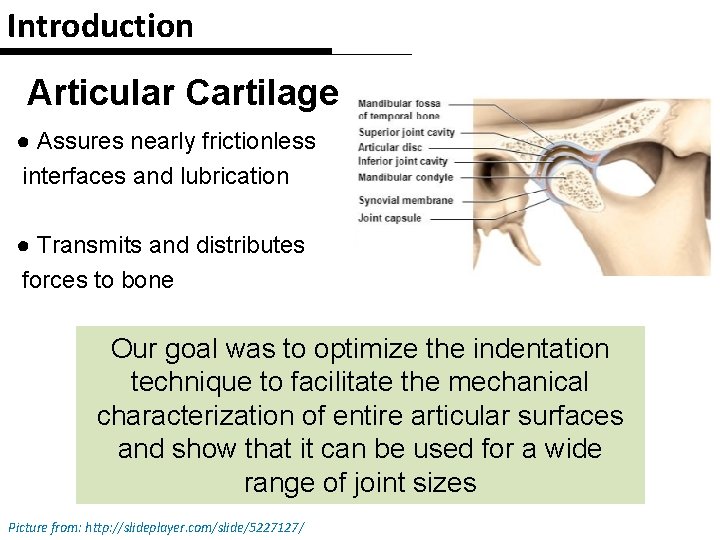
Introduction Articular Cartilage ● Assures nearly frictionless interfaces and lubrication ● Transmits and distributes forces to bone Our goal was to optimize the indentation technique to facilitate the mechanical characterization of entire articular surfaces and show that it can be used for a wide range of joint sizes Picture from: http: //slideplayer. com/slide/5227127/
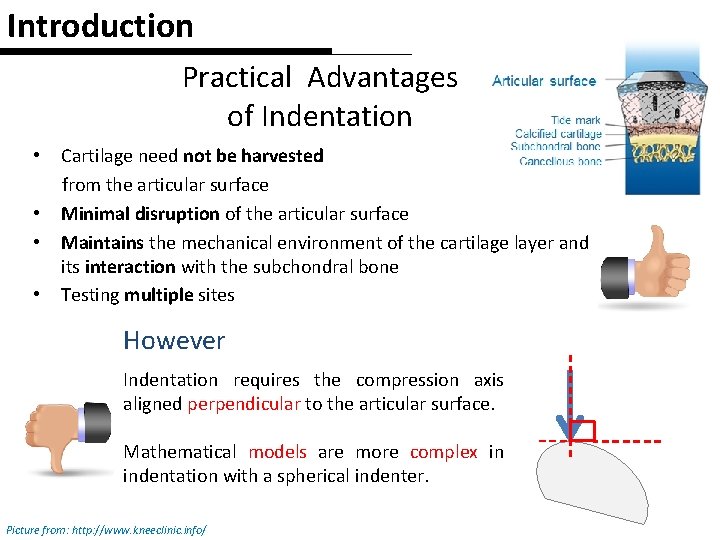
Introduction Practical Advantages of Indentation • • Cartilage need not be harvested from the articular surface Minimal disruption of the articular surface Maintains the mechanical environment of the cartilage layer and its interaction with the subchondral bone Testing multiple sites However Indentation requires the compression axis aligned perpendicular to the articular surface. Mathematical models are more complex in indentation with a spherical indenter. Picture from: http: //www. kneeclinic. info/
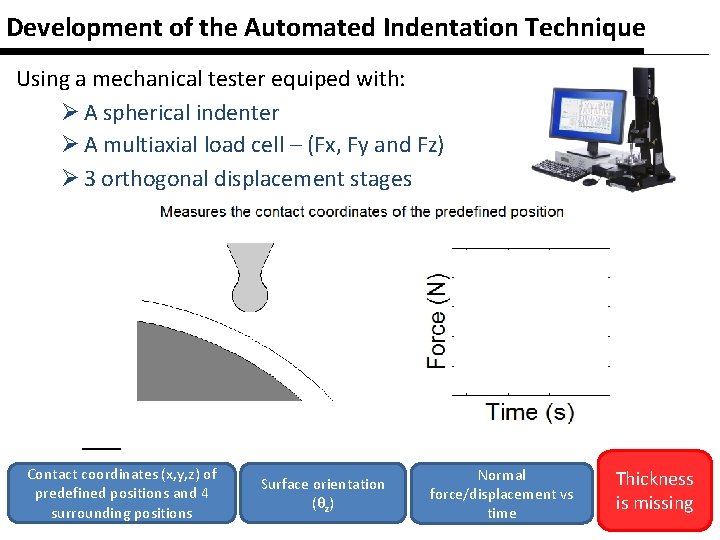
Development of the Automated Indentation Technique Using a mechanical tester equiped with: Ø A spherical indenter Ø A multiaxial load cell – (Fx, Fy and Fz) Ø 3 orthogonal displacement stages Contact coordinates (x, y, z) of predefined positions and 4 surrounding positions Surface orientation (θz) Normal force/displacement vs time Thickness is missing
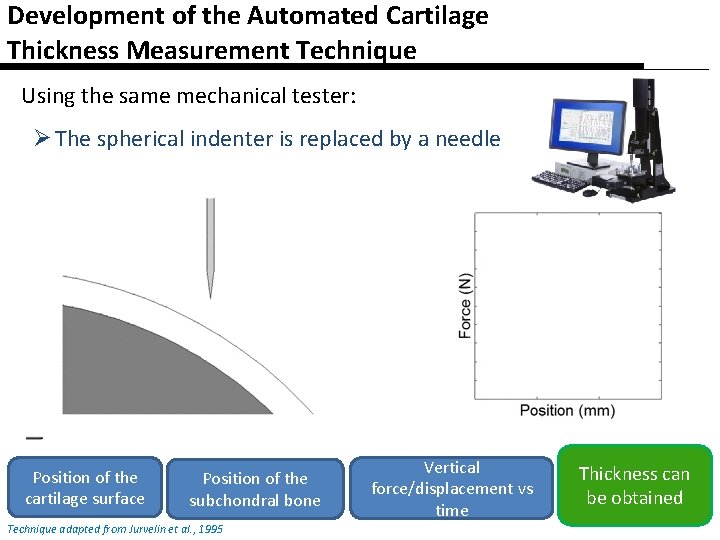
Development of the Automated Cartilage Thickness Measurement Technique Using the same mechanical tester: Ø The spherical indenter is replaced by a needle Position of the cartilage surface Position of the subchondral bone Technique adapted from Jurvelin et al. , 1995 Vertical force/displacement vs time Thickness can be obtained
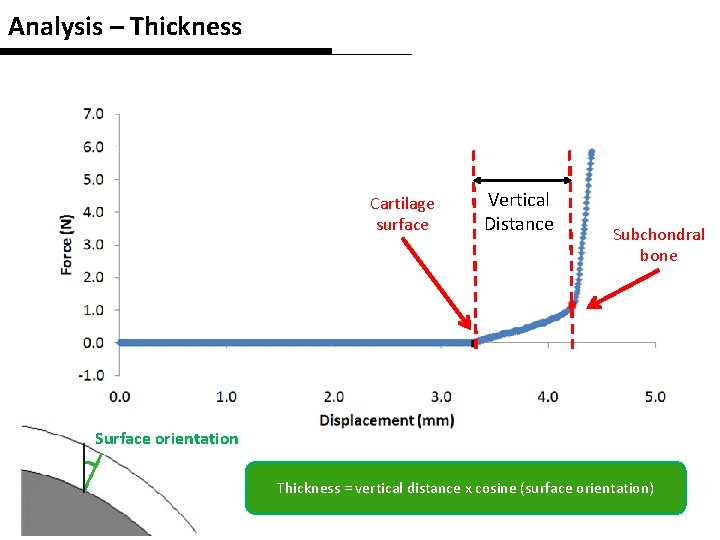
Analysis – Thickness Cartilage surface Vertical Distance Subchondral bone Surface orientation Thickness = vertical distance x cosine (surface orientation)
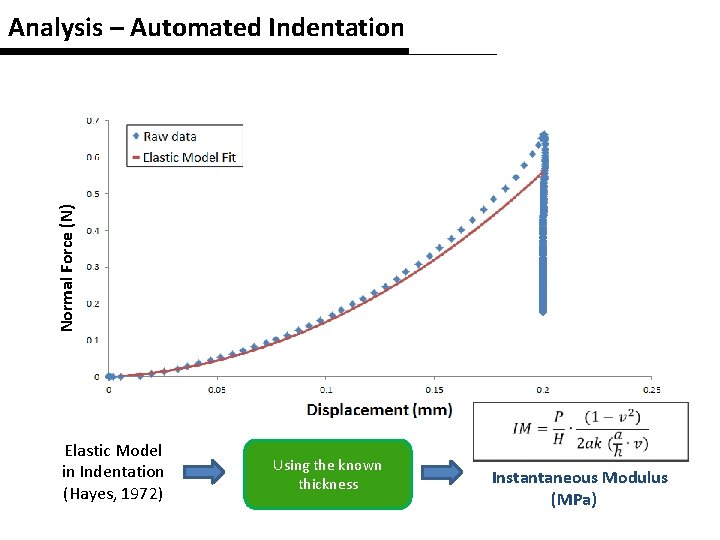
Normal Force (N) Analysis – Automated Indentation Elastic Model in Indentation (Hayes, 1972) Using the known thickness Instantaneous Modulus (MPa)
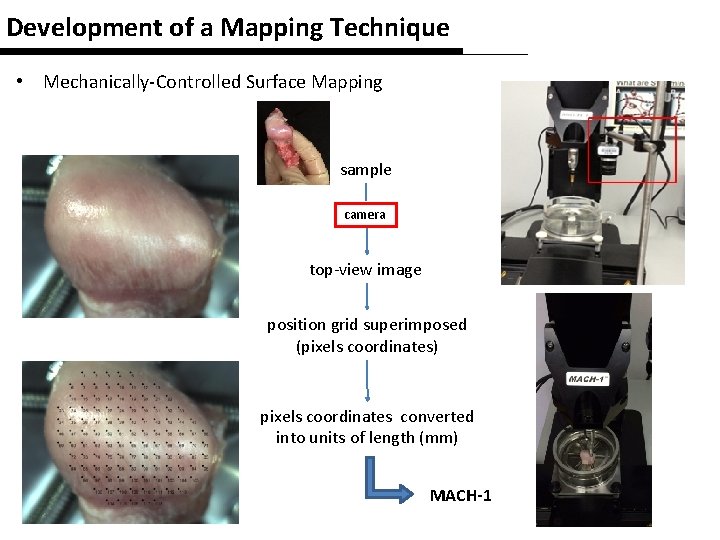
Development of a Mapping Technique • Mechanically-Controlled Surface Mapping sample camera top-view image position grid superimposed (pixels coordinates) pixels coordinates converted into units of length (mm) MACH-1
Study Objective The purpose of this study was to evaluate the capability of an automated indentation technique to reveal the topographical variation of mechanical properties over the entire articular surface of the temporomandibular joint (TMJ), especially the thickness and instantaneous modulus (IM).
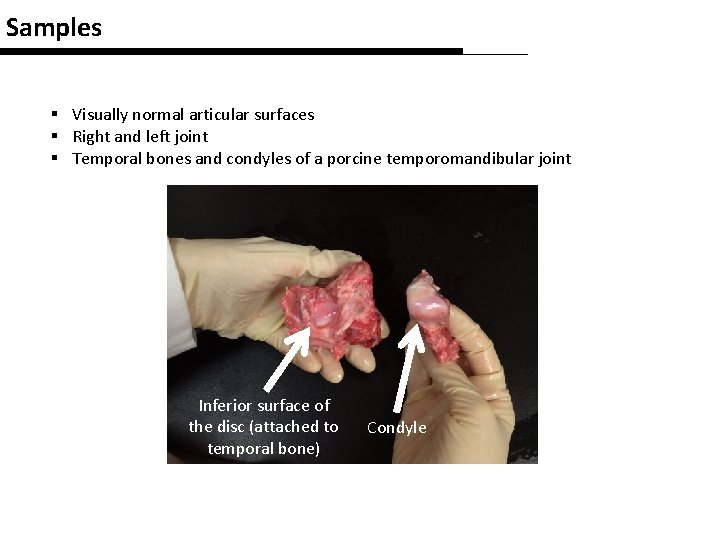
Samples § Visually normal articular surfaces § Right and left joint § Temporal bones and condyles of a porcine temporomandibular joint Inferior surface of the disc (attached to temporal bone) Condyle
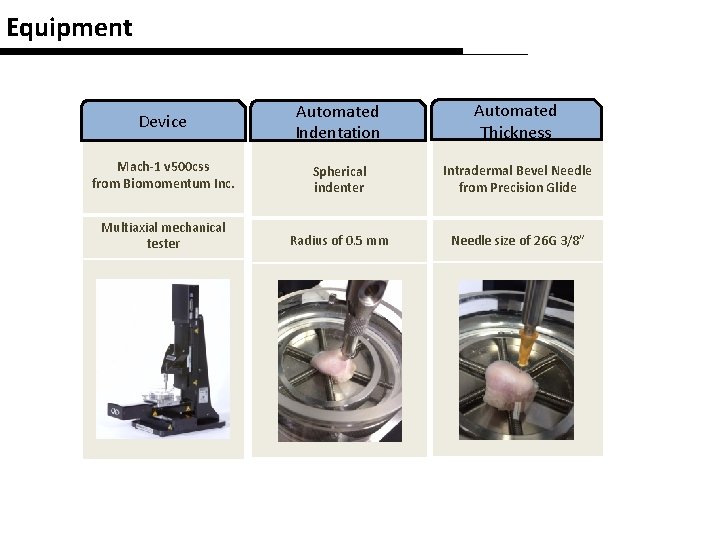
Equipment Device Automated Indentation Automated Thickness Mach-1 v 500 css from Biomomentum Inc. Spherical indenter Intradermal Bevel Needle from Precision Glide Multiaxial mechanical tester Radius of 0. 5 mm Needle size of 26 G 3/8”
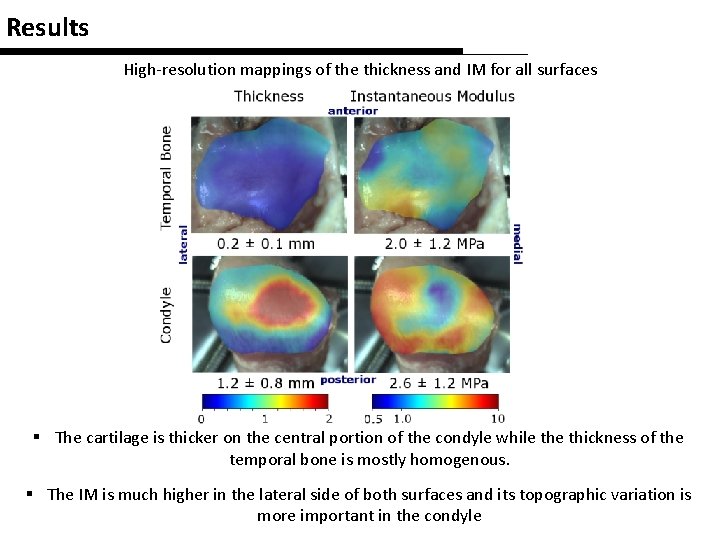
Results High-resolution mappings of the thickness and IM for all surfaces § The cartilage is thicker on the central portion of the condyle while thickness of the temporal bone is mostly homogenous. § The IM is much higher in the lateral side of both surfaces and its topographic variation is more important in the condyle
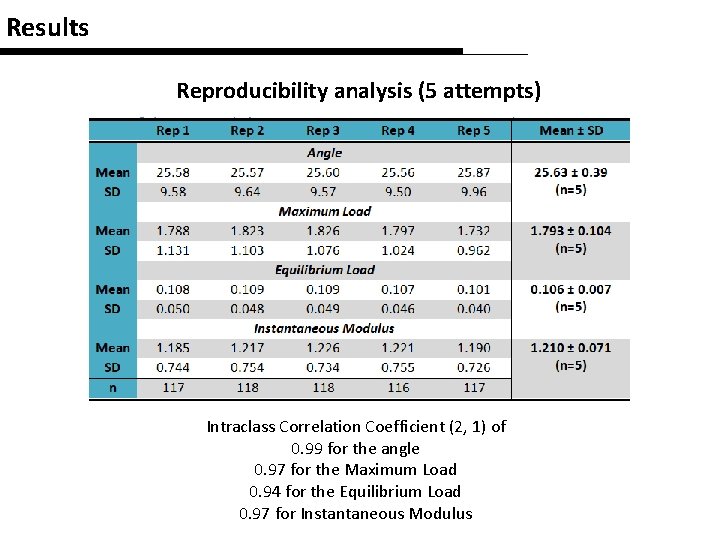
Results Reproducibility analysis (5 attempts) Intraclass Correlation Coefficient (2, 1) of 0. 99 for the angle 0. 97 for the Maximum Load 0. 94 for the Equilibrium Load 0. 97 for Instantaneous Modulus
Discussion § Similar regional differences in mechanical properties have already been reported but never at such high spatial resolution. § These findings support the use of this non-destructive technique in TMJ articular surface characterization.
Conclusion • We have demonstrated the ability of this novel automated indentation mapping technique to map the biomechanical properties of full articular surfaces ü ü Rapidly Reproducibly Sensitively Non-destructively • This automated indentation mapping technique could be of great value in the identification of wear patterns in TMJ disorders.

Acknowledgement
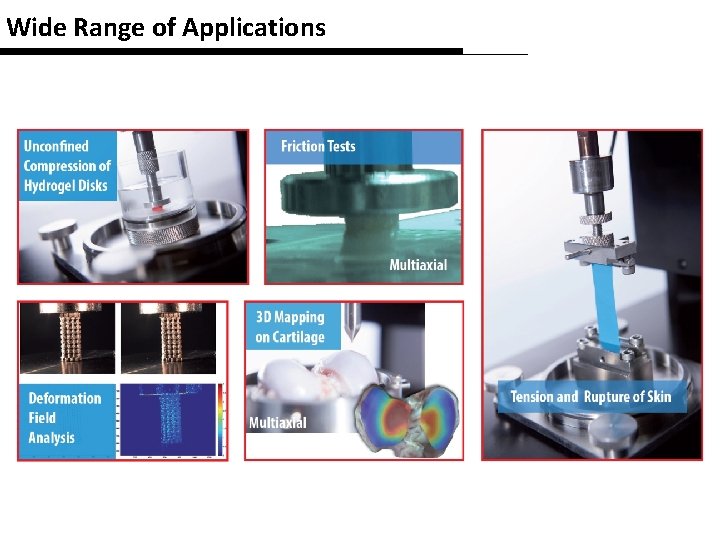
Wide Range of Applications
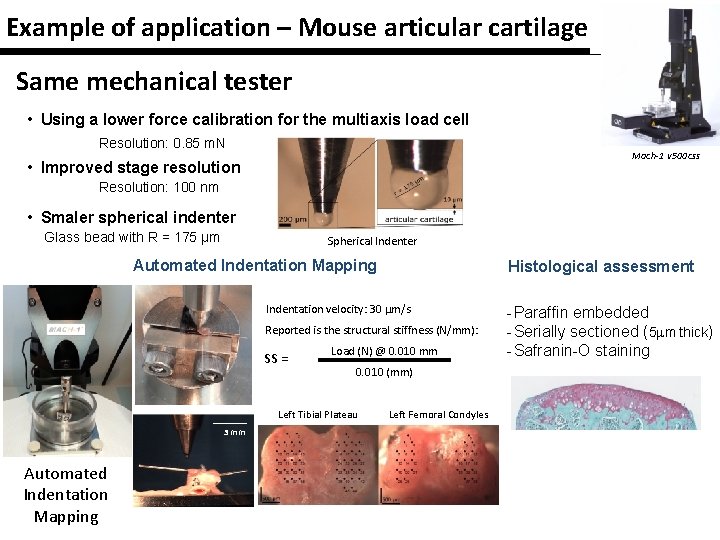
Example of application – Mouse articular cartilage Same mechanical tester • Using a lower force calibration for the multiaxis load cell Resolution: 0. 85 m. N Mach-1 v 500 css • Improved stage resolution Resolution: 100 nm • Smaler spherical indenter Glass bead with R = 175 µm Spherical Indenter Automated Indentation Mapping Histological assessment Indentation velocity: 30 mm/s Reported is the structural stiffness (N/mm): SS = Load (N) @ 0. 010 mm 0. 010 (mm) Left Tibial Plateau 3 mm Automated Indentation Mapping Left Femoral Condyles - Paraffin embedded - Serially sectioned (5 mm thick) - Safranin-O staining
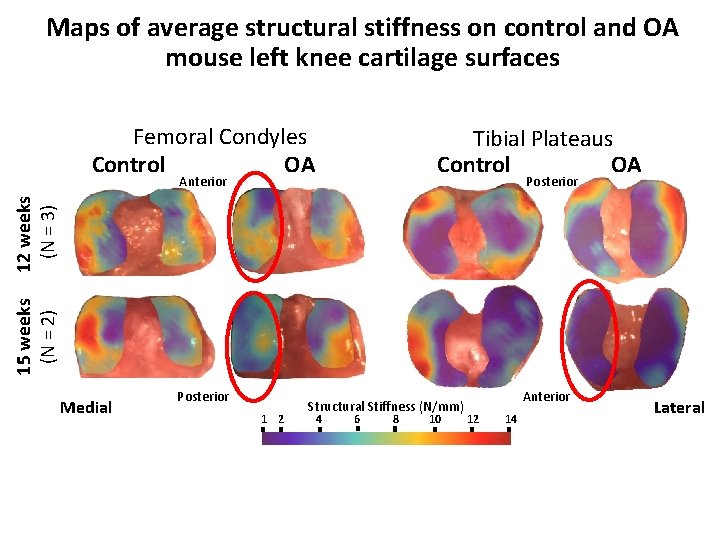
Maps of average structural stiffness on control and OA mouse left knee cartilage surfaces Femoral Condyles Control OA Tibial Plateaus Control OA Anterior 15 weeks (N = 2) 12 weeks (N = 3) Posterior Medial Posterior 1 2 Structural Stiffness (N/mm) 4 6 8 10 Anterior 12 14 Lateral
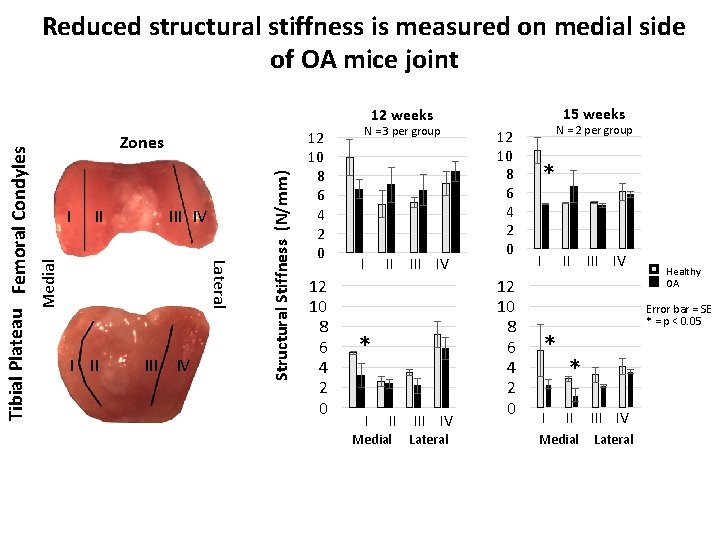
Reduced structural stiffness is measured on medial side of OA mice joint 15 weeks I II IV Medial I II IV Structural Stiffness (N/mm) Zones Lateral Tibial Plateau Femoral Condyles 12 weeks 12 10 8 6 4 2 0 N = 3 per group I II IV * I II Medial III IV Lateral 12 10 8 6 4 2 0 N = 2 per group * I III IV Healthy OA Error bar = SE * = p < 0. 05 * II Medial III IV Lateral
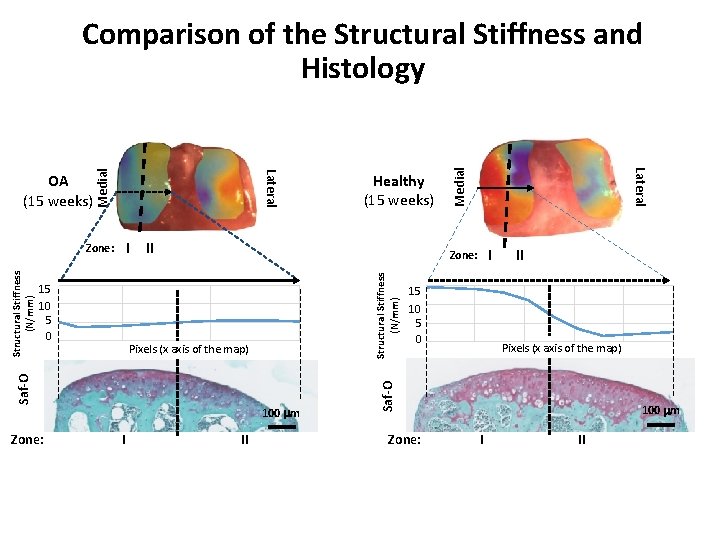
I II Structural Stiffness (N/mm) Pixels (x axis of the map) 100 mm I II Medial 15 10 5 0 II Pixels (x axis of the map) Saf-O 15 10 5 0 I Zone: Saf-O Structural Stiffness (N/mm) Zone: Healthy (15 weeks) Lateral OA (15 weeks) Medial Comparison of the Structural Stiffness and Histology Zone: 100 mm I II
Conclusions § Mechanical properties can be mapped on entire articular surfaces of tiny mouse joints. § Structural stiffness maps show similar distribution patterns to those previously observed for the stifle joints of larger species, with stiffer cartilage in the region covered by the meniscus. § Decrease of the average structural stiffness for the medial compartment of the OA-developing mouse is in agreement with the literature (Walton M. J. Pathol. 1977) § The decrease in structural stiffness of the medial compartment is more obvious than the decrease in proteoglycan staining.
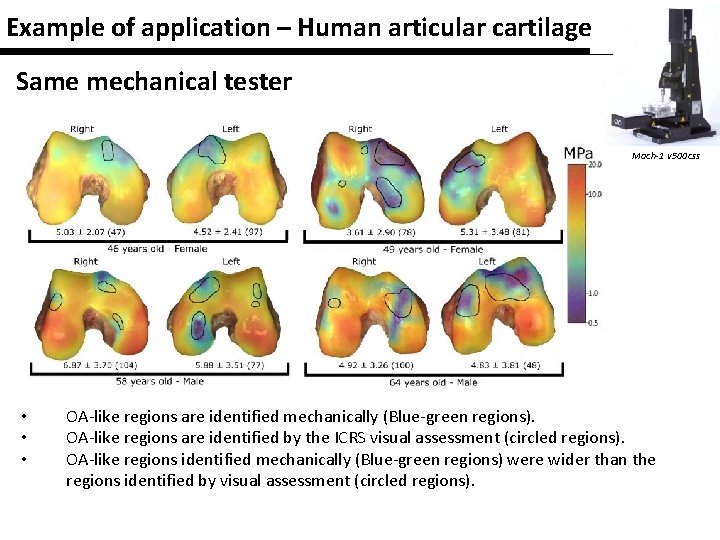
Example of application – Human articular cartilage Same mechanical tester Mach-1 v 500 css • • • OA-like regions are identified mechanically (Blue-green regions). OA-like regions are identified by the ICRS visual assessment (circled regions). OA-like regions identified mechanically (Blue-green regions) were wider than the regions identified by visual assessment (circled regions).
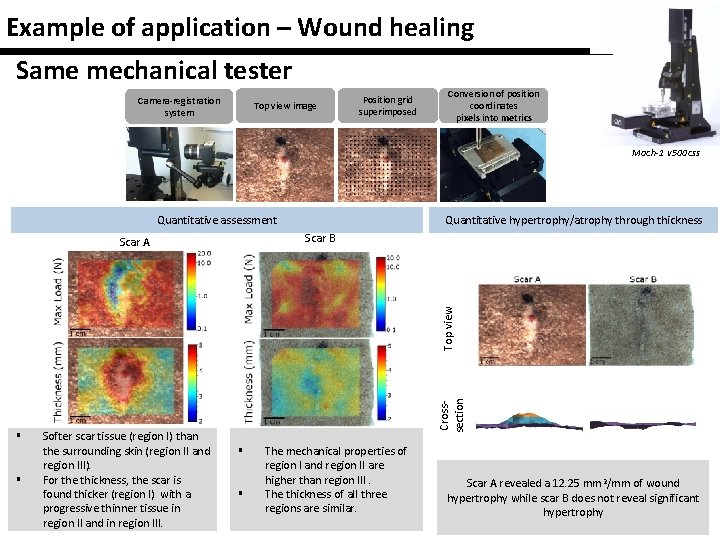
Example of application – Wound healing Same mechanical tester Camera-registration system Top view image Position grid superimposed Conversion of position coordinates pixels into metrics Mach-1 v 500 css Quantitative assessment Quantitative hypertrophy/atrophy through thickness Scar B § § Softer scar tissue (region I) than the surrounding skin (region II and region III). For the thickness, the scar is found thicker (region I) with a progressive thinner tissue in region II and in region III. Crosssection Top view Scar A § § The mechanical properties of region I and region II are higher than region III. The thickness of all three regions are similar. Scar A revealed a 12. 25 mm 2/mm of wound hypertrophy while scar B does not reveal significant hypertrophy
- Slides: 25