Carpal Tunnel Syndrome carpal tunnel syndrome Karpos which





- Slides: 46
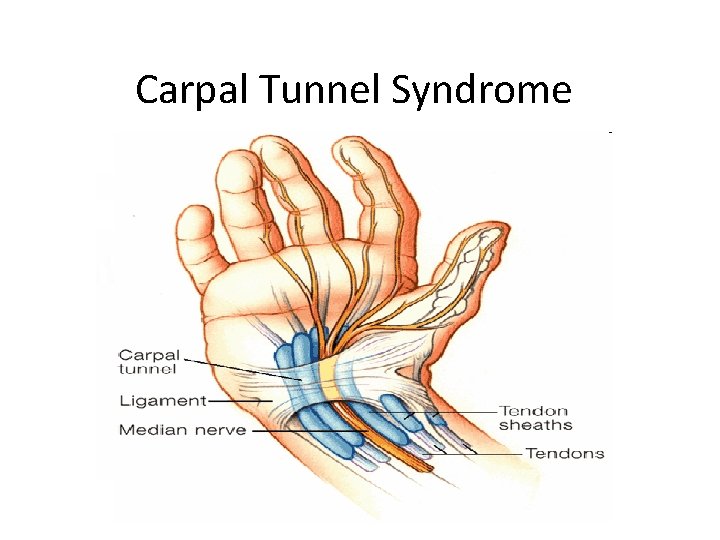
Carpal Tunnel Syndrome

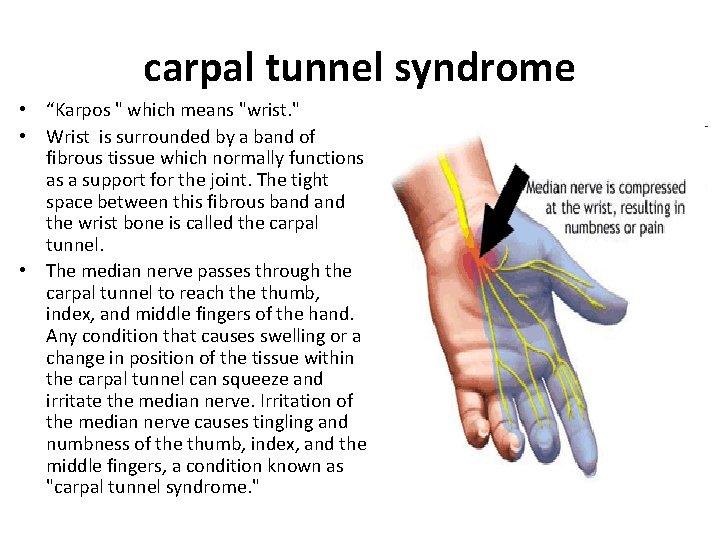
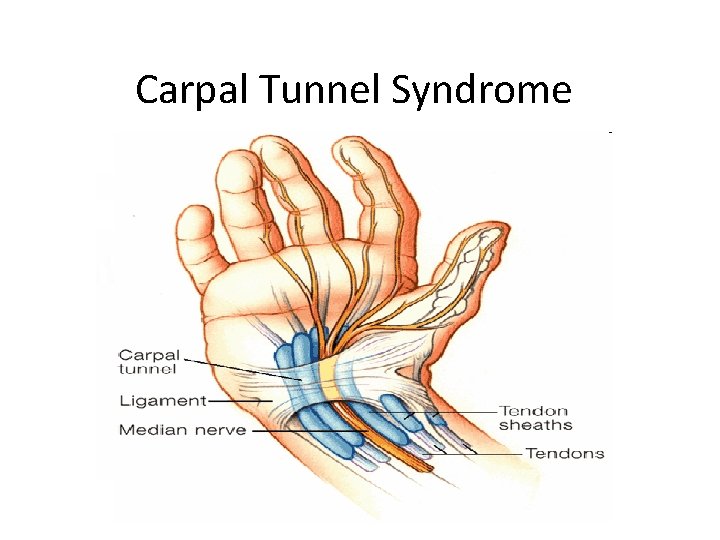
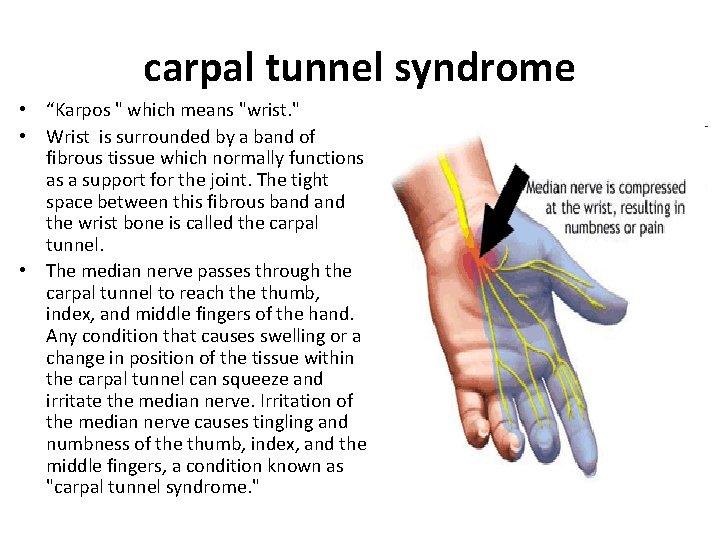
carpal tunnel syndrome • “Karpos " which means "wrist. " • Wrist is surrounded by a band of fibrous tissue which normally functions as a support for the joint. The tight space between this fibrous band the wrist bone is called the carpal tunnel. • The median nerve passes through the carpal tunnel to reach the thumb, index, and middle fingers of the hand. Any condition that causes swelling or a change in position of the tissue within the carpal tunnel can squeeze and irritate the median nerve. Irritation of the median nerve causes tingling and numbness of the thumb, index, and the middle fingers, a condition known as "carpal tunnel syndrome. "
Initial symptoms • Patients initially feel numbness and tingling of the hand in the distribution of the median nerve (the thumb, index, middle, and part of the fourth fingers). • more pronounced at night and can awaken from sleep (due to the flexed-wrist sleeping position and/or fluid accumulating around the wrist and hand while lying flat ). • As the disease progresses, patients can develop a burning sensation, cramping and weakness of the hand. Decreased grip strength can lead to frequent dropping of objects from the hand • Chronic carpal tunnel syndrome can also lead to wasting (atrophy) of the hand muscles.
Risk Factors • Hand work. • Endocrine imbalance ( hypothyroidism , DM , pregnancy ) • History of neuropathy. • Rheumatoid arthritis. • Amyloidosis. • Multiple myeloma. • Trauma. • Alcoholism. • Gout. • Space-occupying lesions within carpal tunnel.
Pathophysiology • Internal fibrosis of the median nerve. • Epineural scarring and constriction. • Reduced nerve conduction velocity. Etiology • Any factor that increases the pressure within the tunnel compresses the median nerve and leads to CTS.
The most common causes include- Flexor tenosynovitis. - Trauma to the carpal bones. - Ganglion. - Fibroma or lipoma within the tunnel. - Rheumatoid cyst. - Gout. - Diabetic neuropathy.
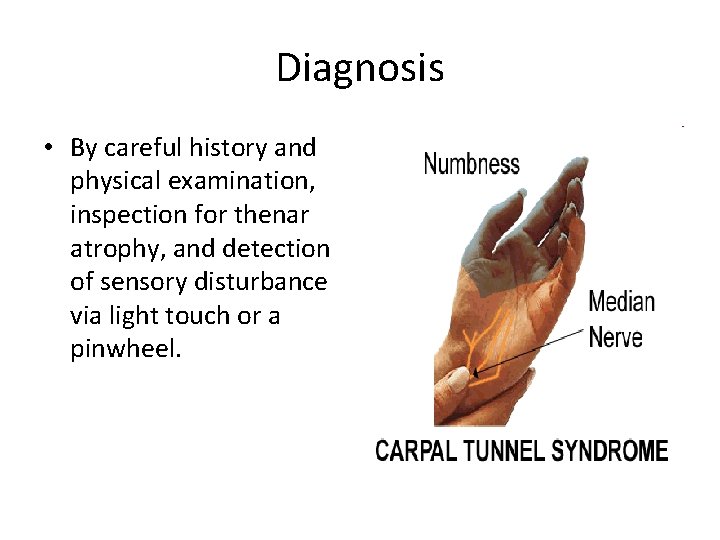
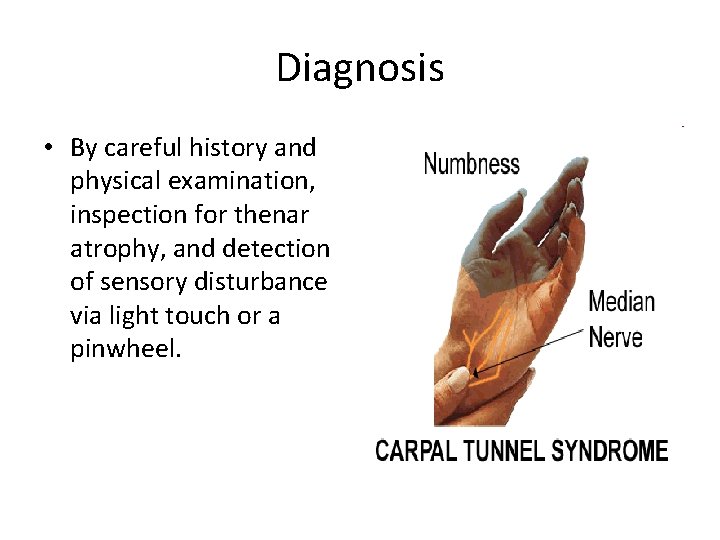
Diagnosis • By careful history and physical examination, inspection for thenar atrophy, and detection of sensory disturbance via light touch or a pinwheel.
Signs and Symptoms • – – – Paresthesia in the median nerve distribution in the hand Weakness or clumsiness in the hand. Pain in the hand, wrist, or distal forearm. Awakening from sleep with pain or numbness in the hand.
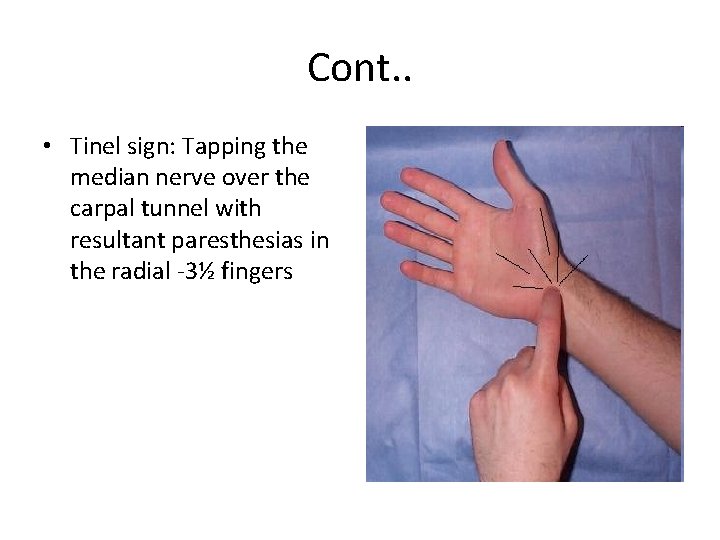
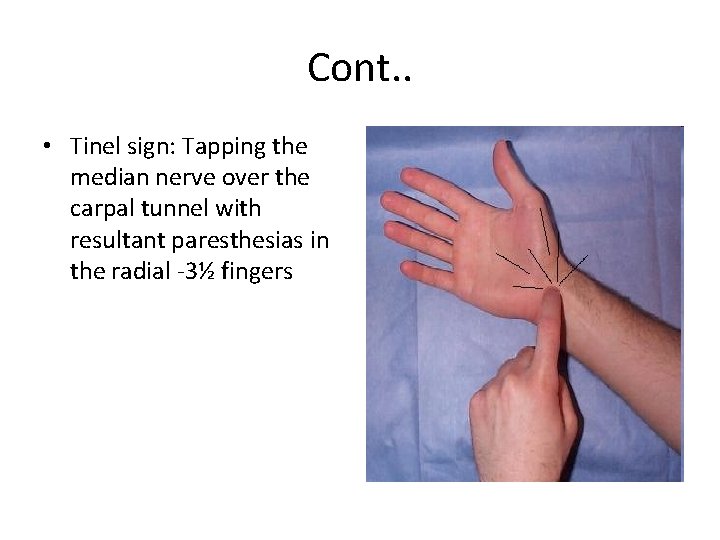
Cont. . • Tinel sign: Tapping the median nerve over the carpal tunnel with resultant paresthesias in the radial -3½ fingers
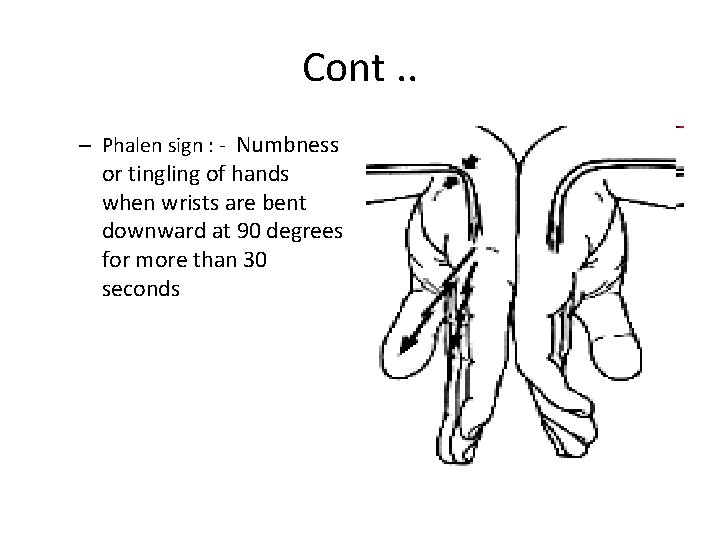
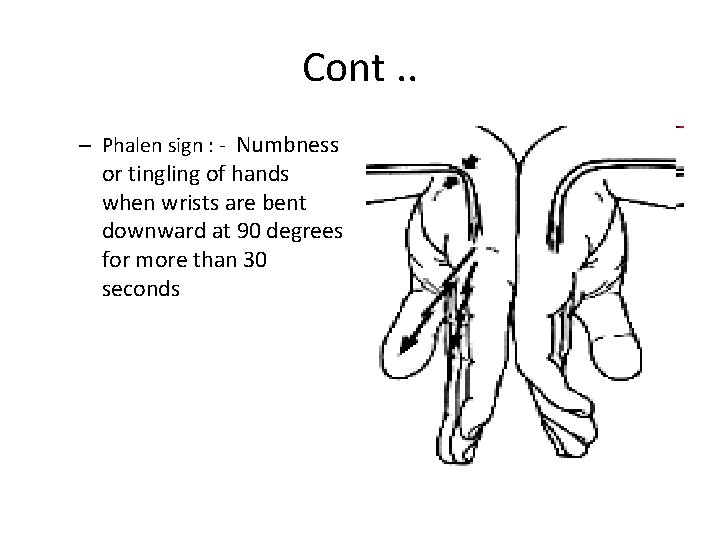
Cont. . – Phalen sign : - Numbness or tingling of hands when wrists are bent downward at 90 degrees for more than 30 seconds
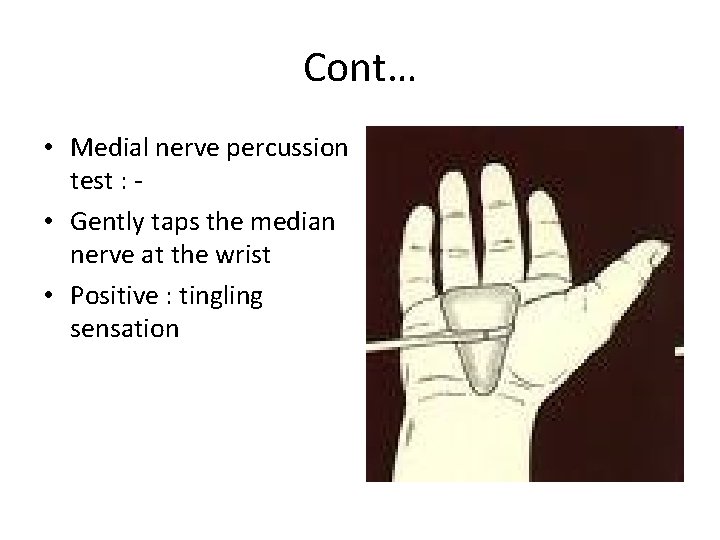
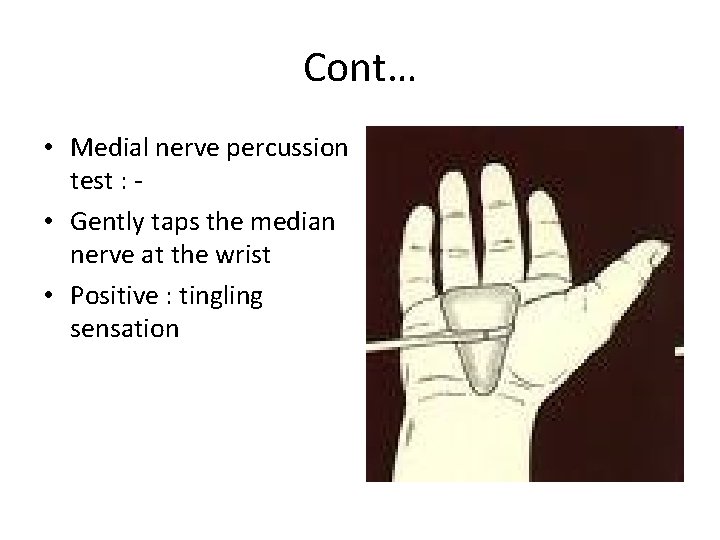
Cont… • Medial nerve percussion test : • Gently taps the median nerve at the wrist • Positive : tingling sensation
Physical Exam • The hand should be examined to detect thenar muscle atrophy. • 2 -point discrimination should be checked at the tips of the fingers on the radial and ulnar borders (should be < 5 -6 mm).
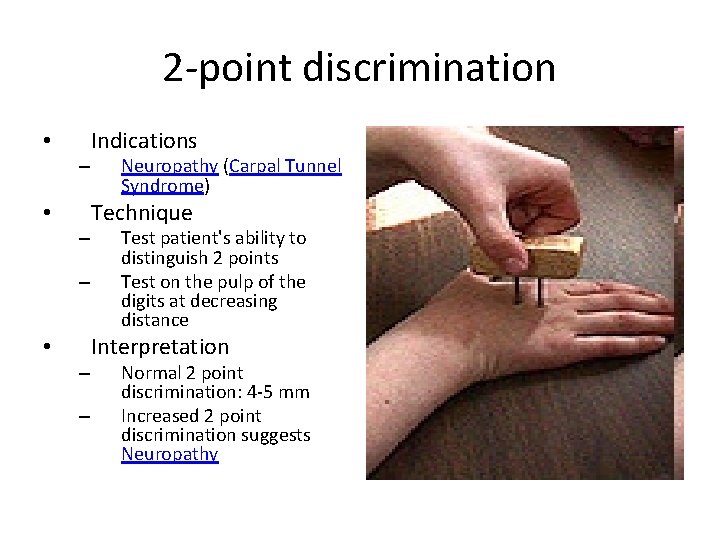
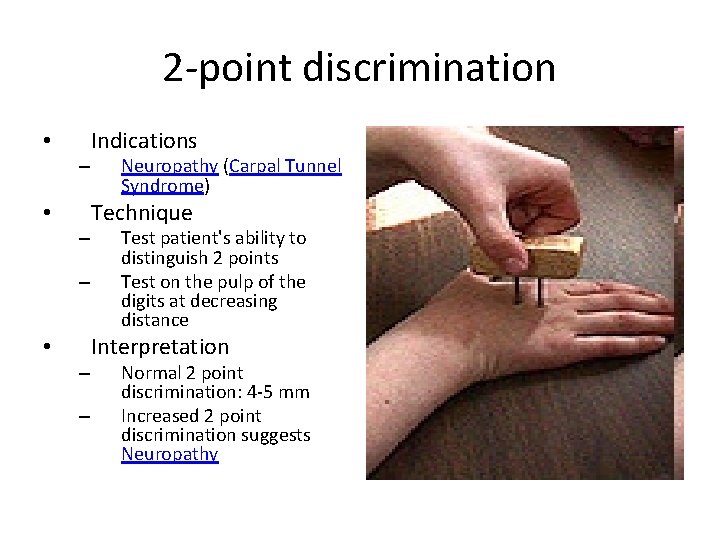
2 -point discrimination • – – Indications Neuropathy (Carpal Tunnel Syndrome) Technique Test patient's ability to distinguish 2 points Test on the pulp of the digits at decreasing distance Interpretation Normal 2 point discrimination: 4 -5 mm Increased 2 point discrimination suggests Neuropathy
Tests • The following basic tests should be ordered to rule out systemic causes of CTS: – Sedimentation rate. – Serum glucose concentration. – Serum uric acid level. – Thyroid function test. – Electromyography/nerve conduction velocity
Treatment General Measures. • Nonoperative intervention: – Modalities: Cockup wrist splinting, NSAIDs (not proven effective), diuretics, and cortisone injections (which must be performed by an experienced physician to avoid direct injury to the median nerve) – The patient should wear a wrist splint during sleep. • Activity modification in work-related CTS is recommended.

• Surgical release is indicated when nonoperative measures have failed or in patients with constant numbness, motor weakness, or increased distal median nerve motor latency noted on electromyography. • Open carpal tunnel release is made through a longitudinal incision that begins on the distal border of the transverse carpal tunnel ligament and extends proximally to the proximal wrist crease, in line with the ulnar border of the axis of the ring finger.


Ganglia ( Ganglion cyst ) • Ganglia = cystic tumor • Defined as a localised , tense , painless , cystic swelling , containing clear gelatinous fluid • Origin : leakage of synovial fluid through the capsule of a joint or a tendon sheath • Sites : • Dorsum of the wrist , • Flexor aspect of the fingers and • Dorsum of the foot

Treatment • Resolve spontaneously over a period of time • Excision
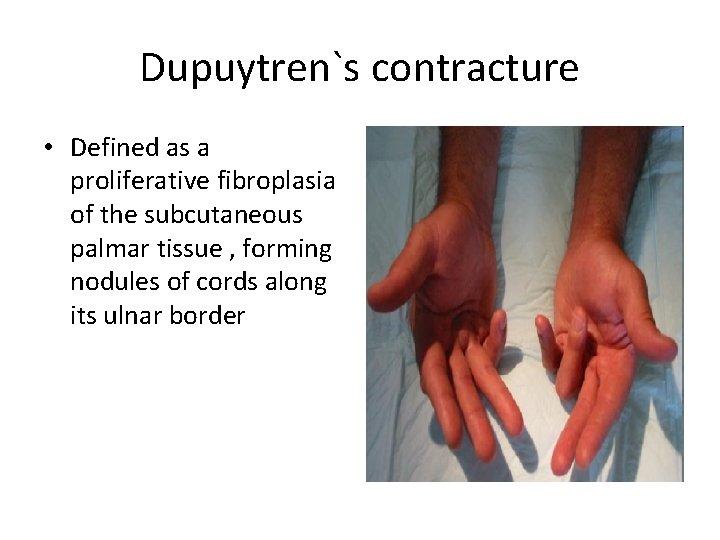
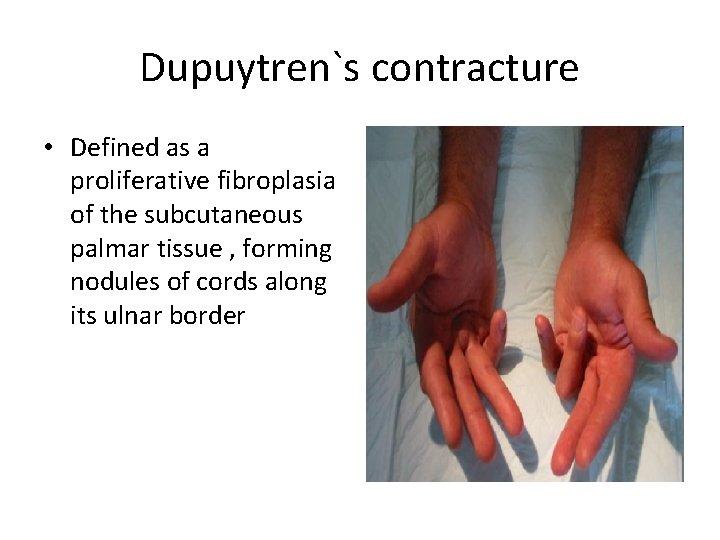
Dupuytren`s contracture • Defined as a proliferative fibroplasia of the subcutaneous palmar tissue , forming nodules of cords along its ulnar border
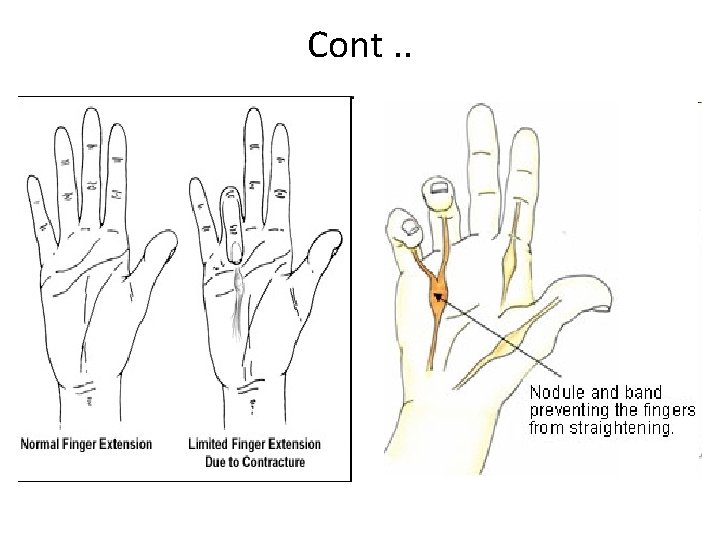
Cont. .
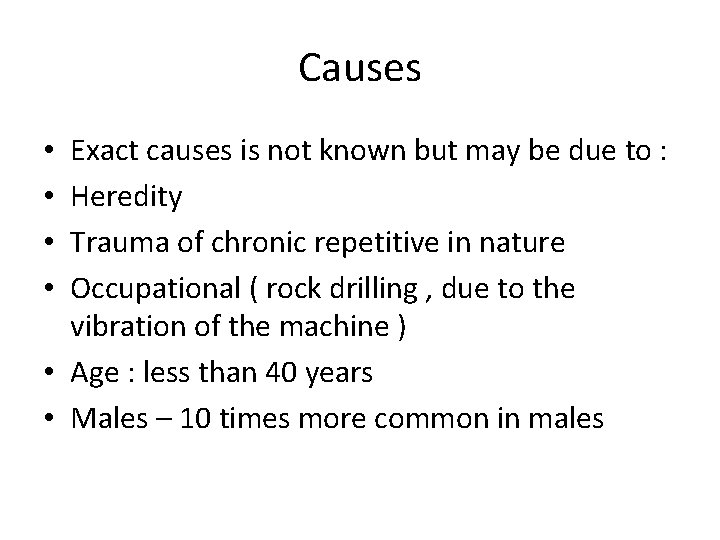
Causes Exact causes is not known but may be due to : Heredity Trauma of chronic repetitive in nature Occupational ( rock drilling , due to the vibration of the machine ) • Age : less than 40 years • Males – 10 times more common in males • •
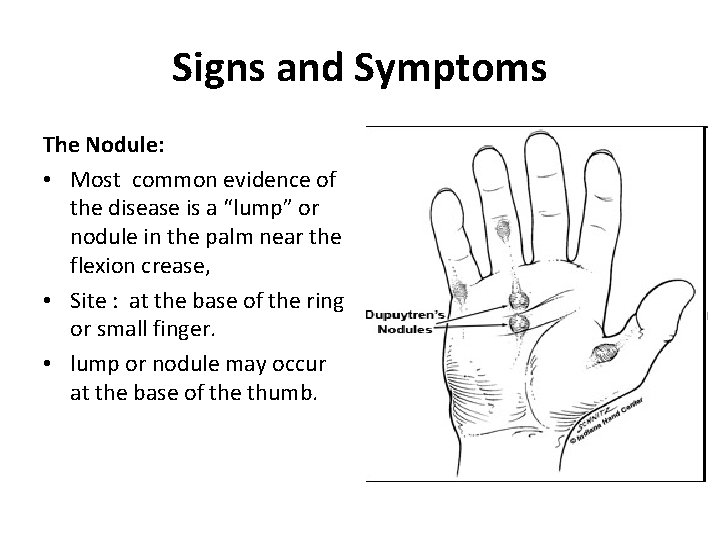
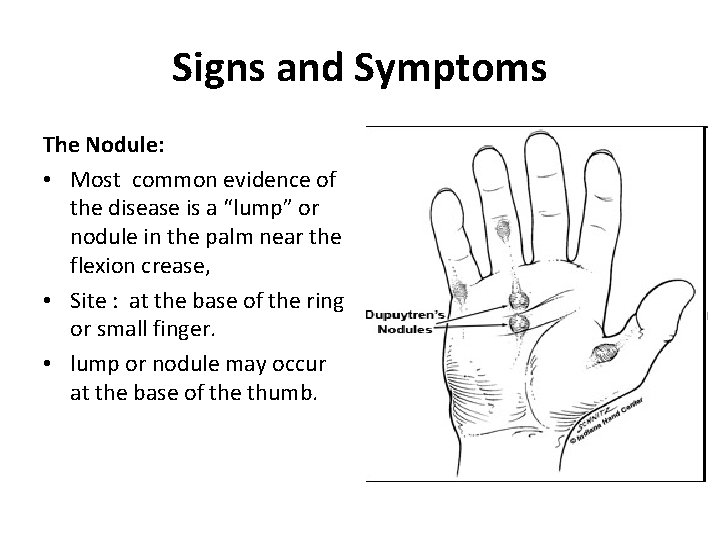
Signs and Symptoms The Nodule: • Most common evidence of the disease is a “lump” or nodule in the palm near the flexion crease, • Site : at the base of the ring or small finger. • lump or nodule may occur at the base of the thumb.
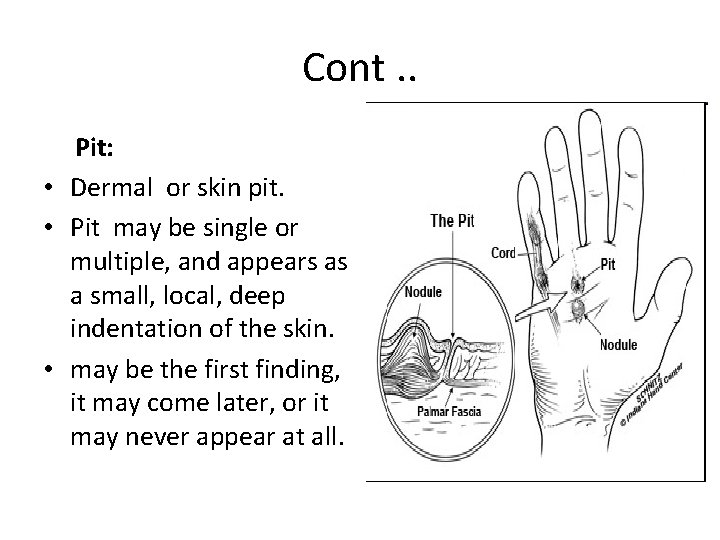
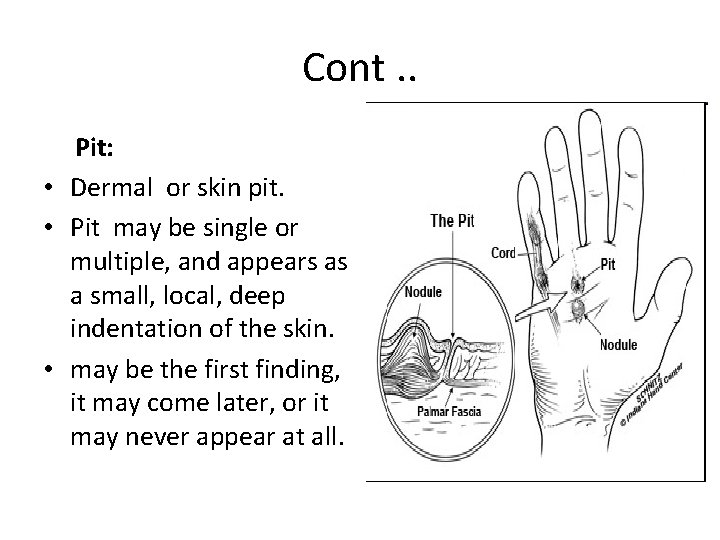
Cont. . Pit: • Dermal or skin pit. • Pit may be single or multiple, and appears as a small, local, deep indentation of the skin. • may be the first finding, it may come later, or it may never appear at all.
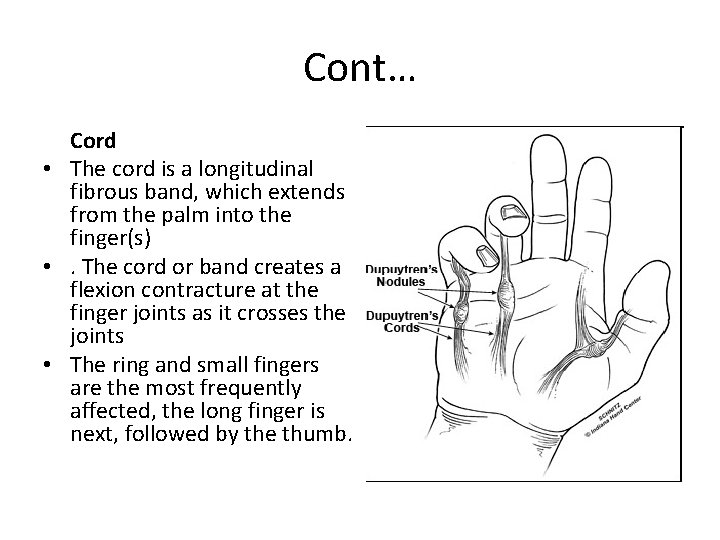
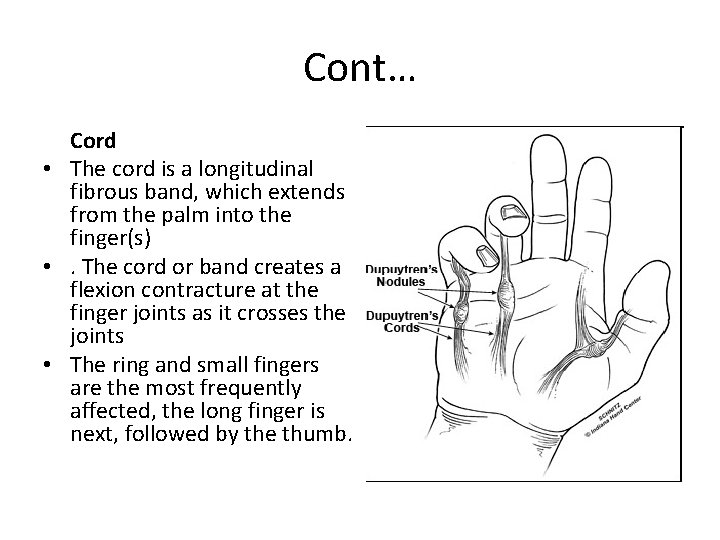
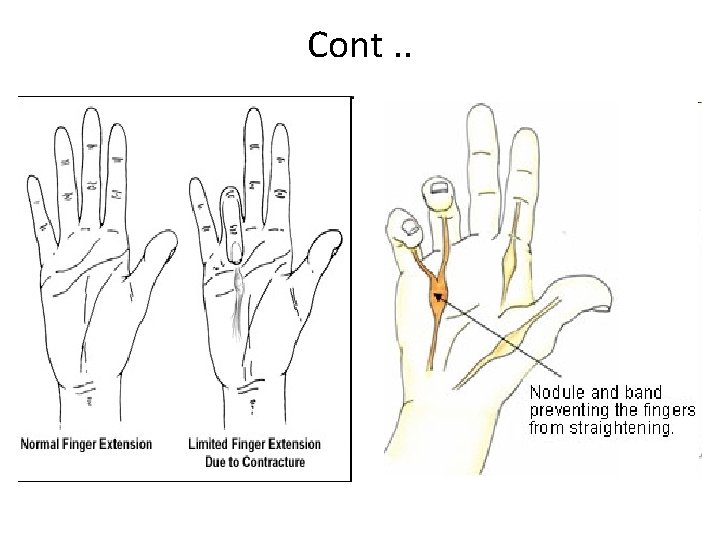
Cont… Cord • The cord is a longitudinal fibrous band, which extends from the palm into the finger(s) • . The cord or band creates a flexion contracture at the finger joints as it crosses the joints • The ring and small fingers are the most frequently affected, the long finger is next, followed by the thumb.
Nonsurgical Treatment In the early stages : Frequent examination and follow-up. Inject cortisone into the painful nodules. Splint ( that keeps the finger straight ) This splint is usually worn at night. • Surgery to release the contracture and to prevent disability • •
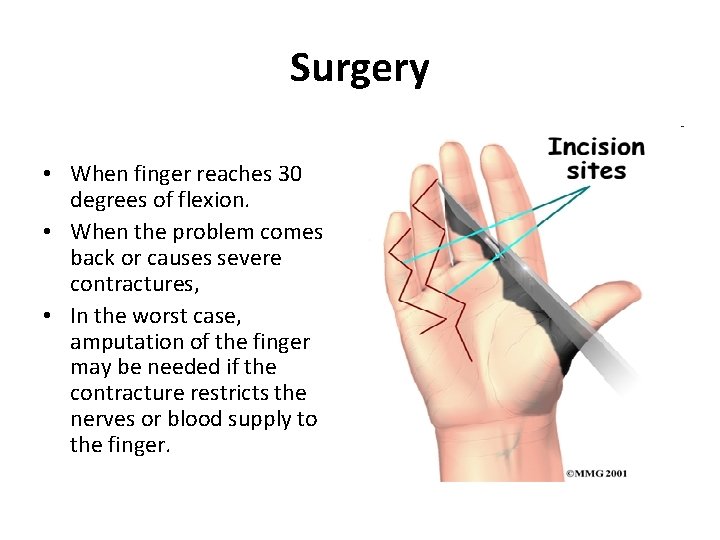
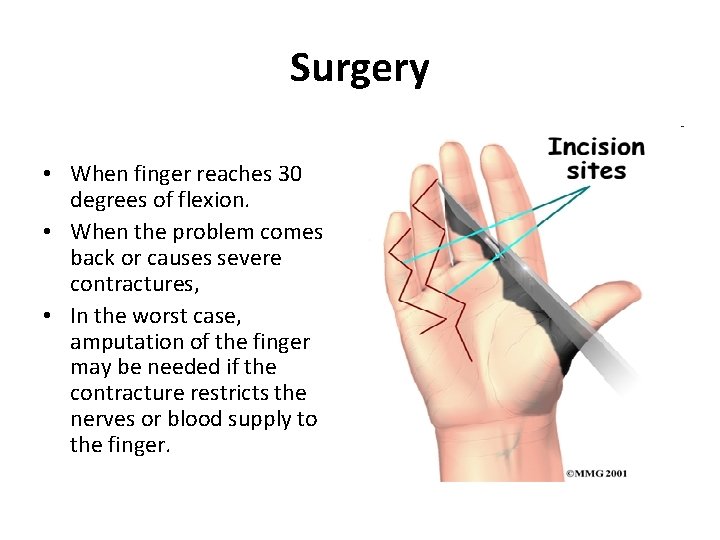
Surgery • When finger reaches 30 degrees of flexion. • When the problem comes back or causes severe contractures, • In the worst case, amputation of the finger may be needed if the contracture restricts the nerves or blood supply to the finger.
Cont… • • • Tissue Release release the fibrous attachments between the palmar fascia and the tissues around it, If the problem is not severe, it may be possible to free the contracture simply by cutting the cord under the skin. If the palmar fascia is more involved and more than one finger is bent, take out the whole sheet of fascia. Palmar Fascia Removal of the entire palmar fascia. Skin Graft Method A skin graft may be needed if the skin surface has contracted so much that the finger cannot relax as it should and the palm cannot be stretched out flat (from the wrist, elbow, or groin )
complications • • • General complications : Pain Bleeding Infection in the surgical wound Scarring Specific complications Injury to the small arteries in a finger Incomplete correction of the Dupuytren’s contracture Stiffness of the finger joints Numbness Wound-healing problems Severe pain, stiffness and loss of use of the hand
Blunt abdominal trauma.
Common causes • Motor vehicle accidents and pedestrian accidents. • Falls. • Industrial accidents. . automobile-
The most reliable signs and symptoms in alert patients are – • • • Pain, Tenderness, Gastrointestinal hemorrhage, Hypovolemia, and Evidence of peritoneal irritation.
Physical examination: • Head –pupils, level of consciousness, reflexes, • Respiratory system, • Cardiovascular system, • Abdominal.
Examination: Abdomen • Inspection • For abdominal distention due to pneumoperitoneum, gastric dilatation, or ileus produced by peritoneal irritation but this is usually delayed for several hours to days. • Bradycardia may indicate the presence of free intraperitoneal blood in a patient with blunt abdominal injuries.
• Signs of peritonitis (eg, involuntary guarding, rigidity) soon after an injury suggest leakage of intestinal content. • Peritonitis due to intra-abdominal hemorrhage may take several hours to develop. • Pelvic instability indicates the lower urinary tract injury as well as pelvic and retroperitoneal hematoma. • Open pelvic fractures are associated with a mortality rate exceeding 50%.
Rectal examination. • Should be performed to search for evidence of bony penetration resulting from a pelvic fracture. • The stool should be evaluated for gross or occult blood. • The evaluation of rectal tone is important for determining the patient's neurologic status, and palpation of a high-riding prostate suggests urethral injury.
Some common abdominal injuries: Liver injury, • Liver laceration is common. Clinical Findings • In blunt trauma, there will often be fractures of the 7 -9 th ribs overlying the liver. • Right upper quadrant tenderness. • Rebound sensitivity and guarding will not be present until blood has been in the abdomen long enough to cause peritoneal irritation - about two hours.
Spleen injury, The spleen is the most commonly injured organ in blunt abdominal trauma. Hypotension from hemorrhage is the most common presenting finding. Clinical Findings: • The injury should be suspected when the 9 -10 th ribs on the left are fractured, • When left upper quadrant tenderness and tachycardia are present.
Diagnosis : (spleen injury) • Any patient with tachycardia or hypotension and left upper quadrant tenderness is assumed to have a ruptured spleen Kidney Injury : • kidney injury is common with falls and automobile accidents. • It is suspected with fractures of the 11 th-12 th ribs or flank tenderness. • If hematuria (to any degree) is present, the nature of the injury must be determined. Kidney lacerations can bleed extensively into the retroperitoneal space.
(Kidney injury. . ) Clinical Findings: • The ruptured kidney usually presents with pain on inspiration in the abdomen and flank. • Gross hematuria will almost invariably be present, but the injury can still occur with only microscopic hematuria. • Flank discoloration is a late finding that will never be present in the emergency department. • Diagnosis: requires IVP examination or CT scan
Bowel Rupture; • Most commonly, injuries that break the wall of the bowel are due to penetrating injury. • In penetrating trauma, the small bowel is most frequently injured, followed by the stomach and large intestine. Clinical Findings: • Symptoms are caused by the intestinal contents, rather than blood loss. • Stomach rupture causes rapid onset of burning epigastric pain, followed quickly by rigidity
Clinical Findings: • Small bowel and colon injury may present only with vague generalized pain, with peritonitis following after hours. • Duodenal injury may cause back pain. Diagnosis: • The diagnosis of bowel rupture is made by finding free air on abdominal x-ray. • Duodenal or sigmoid colon injury may result in retroperitoneal air only.
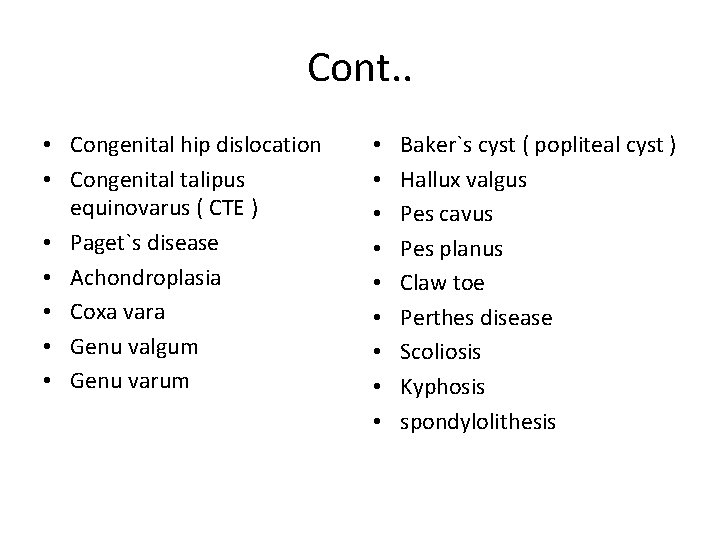
Cont. . • Congenital hip dislocation • Congenital talipus equinovarus ( CTE ) • Paget`s disease • Achondroplasia • Coxa vara • Genu valgum • Genu varum • • • Baker`s cyst ( popliteal cyst ) Hallux valgus Pes cavus Pes planus Claw toe Perthes disease Scoliosis Kyphosis spondylolithesis
 Carpal tunnel syndrome differential diagnosis
Carpal tunnel syndrome differential diagnosis Assistive devices for carpal tunnel syndrome
Assistive devices for carpal tunnel syndrome Median nerve innervation
Median nerve innervation Owcp schedule award carpal tunnel
Owcp schedule award carpal tunnel Carpal tunnel release scar
Carpal tunnel release scar Art spheroidea
Art spheroidea Metakarpo falangeal eklem
Metakarpo falangeal eklem Carpal bones
Carpal bones Radiografía carpal
Radiografía carpal How deep is the channel tunnel
How deep is the channel tunnel Tunnel terminology
Tunnel terminology Kaybiang tunnel construction
Kaybiang tunnel construction Induction tunnel furnace
Induction tunnel furnace Anton anderson tunnel
Anton anderson tunnel Tunnel sequence adalah
Tunnel sequence adalah Typical process
Typical process Tunnel
Tunnel Poly tunnel working model
Poly tunnel working model Zebedee tunnel
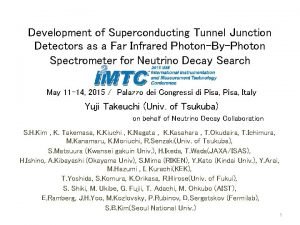
Zebedee tunnel Superconducting tunnel junction
Superconducting tunnel junction Clay kicking method of tunnel construction
Clay kicking method of tunnel construction Mole tunnel stoichiometry answers
Mole tunnel stoichiometry answers Tunnel inspection checklist
Tunnel inspection checklist Furcation plasty definition
Furcation plasty definition Superconducting tunnel junction
Superconducting tunnel junction Tunnel effect
Tunnel effect Tunnel traffic
Tunnel traffic Coband
Coband Superconducting tunnel junction
Superconducting tunnel junction Haiku tunnel books
Haiku tunnel books Tunnel boring machine
Tunnel boring machine Wrist tendon
Wrist tendon Atom tunnel switzerland
Atom tunnel switzerland Transatlantic tunnel project
Transatlantic tunnel project Symbols in through the tunnel
Symbols in through the tunnel Through the tunnel plot diagram
Through the tunnel plot diagram Iit kanpur wind tunnel
Iit kanpur wind tunnel Consider a mach 4 airflow at a pressure of 1 atm. we wish
Consider a mach 4 airflow at a pressure of 1 atm. we wish Coraline door tunnel
Coraline door tunnel Faciovenous plane of patey
Faciovenous plane of patey This drawing illustrates the u.s. rationale behind —
This drawing illustrates the u.s. rationale behind — Hales bar dam tunnel
Hales bar dam tunnel Pulaski tunnel trail
Pulaski tunnel trail 0 pds suture
0 pds suture Raimond tunnel
Raimond tunnel What is blast freezer
What is blast freezer Iodine dns tunnel tutorial
Iodine dns tunnel tutorial