Carotid Endarterectomy and Stenting Mani K C Vindhya








- Slides: 42

Carotid Endarterectomy and Stenting Mani K. C Vindhya M. D Asst Prof of Anesthesiology Nova Southeastern University
Introduction -- Stroke and Transient Ischemic Attacks (TIA's) Stroke statistics (Heart and Stroke Facts: 1997 Statistical Suppl. Dallas, TX: American Heart Association) Stroke = third leading cause of death in U. S. (after heart disease and cancer) Over 500, 000 new cases in U. S. each year (75% in carotid distribution) Mortality: nearly 1/4 die Morbidity: often significant and permanent disability
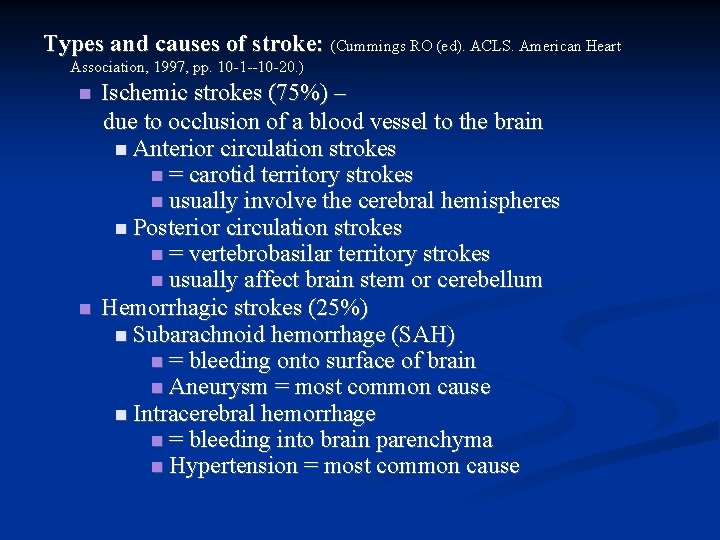
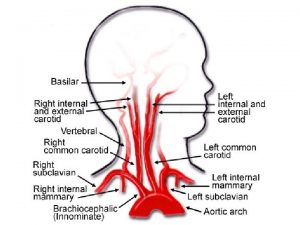
Types and causes of stroke: (Cummings RO (ed). ACLS. American Heart Association, 1997, pp. 10 -1 --10 -20. ) Ischemic strokes (75%) – due to occlusion of a blood vessel to the brain Anterior circulation strokes = carotid territory strokes usually involve the cerebral hemispheres Posterior circulation strokes = vertebrobasilar territory strokes usually affect brain stem or cerebellum Hemorrhagic strokes (25%) Subarachnoid hemorrhage (SAH) = bleeding onto surface of brain Aneurysm = most common cause Intracerebral hemorrhage = bleeding into brain parenchyma Hypertension = most common cause
Treatment of Stroke – now includes thrombolytic therapy Thrombolytic agent = rt-PA I. V. thrombolytic therapy is best initiated within 3 hours after onset of stroke symptoms.

ACLS Algorithm for Suspected Stroke Patients
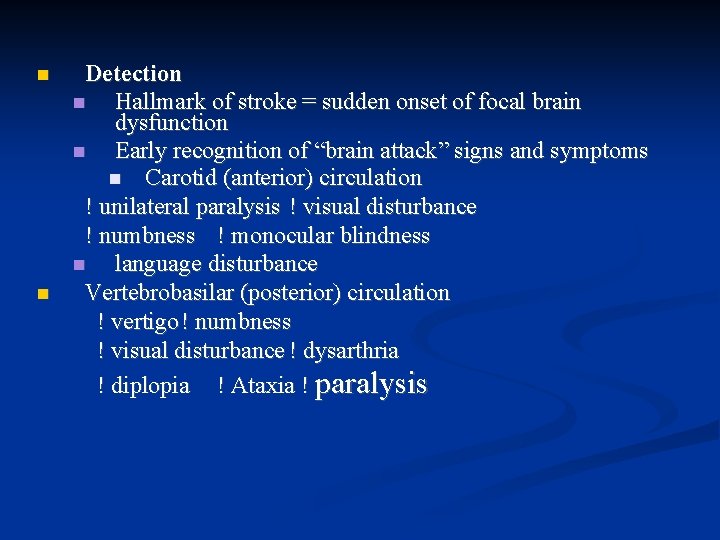
Detection Hallmark of stroke = sudden onset of focal brain dysfunction Early recognition of “brain attack” signs and symptoms Carotid (anterior) circulation ! unilateral paralysis ! visual disturbance ! numbness ! monocular blindness language disturbance Vertebrobasilar (posterior) circulation ! vertigo ! numbness ! visual disturbance ! dysarthria ! diplopia ! Ataxia ! paralysis
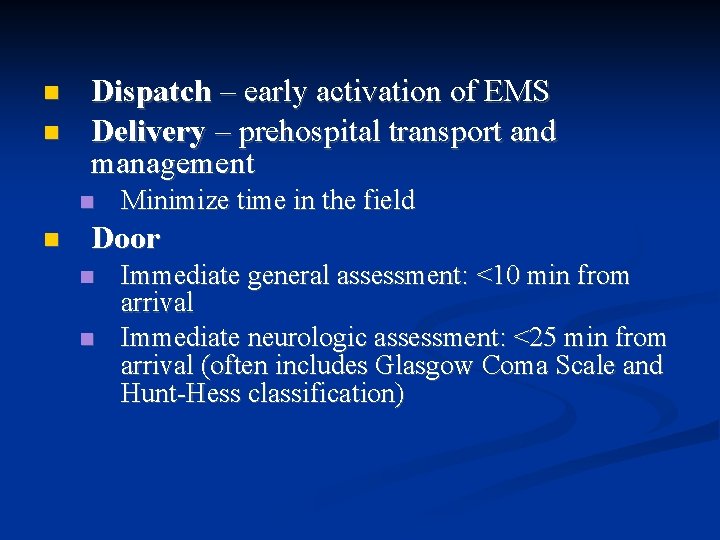
Dispatch – early activation of EMS Delivery – prehospital transport and management Minimize time in the field Door Immediate general assessment: <10 min from arrival Immediate neurologic assessment: <25 min from arrival (often includes Glasgow Coma Scale and Hunt-Hess classification)

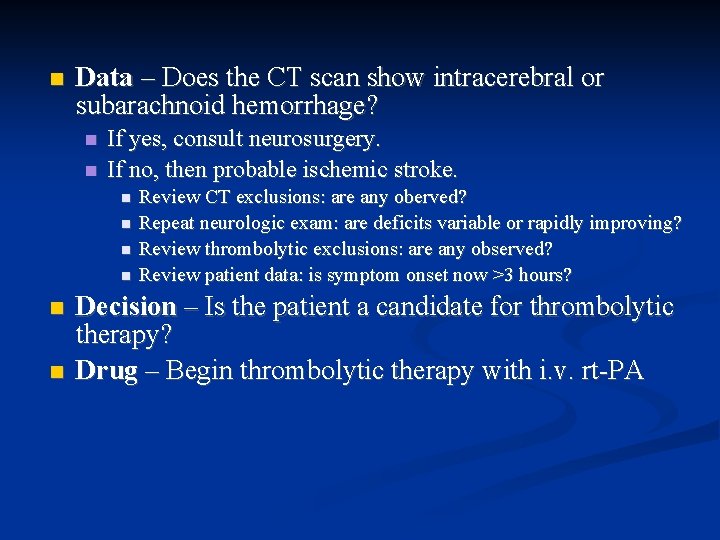
Data – Does the CT scan show intracerebral or subarachnoid hemorrhage? If yes, consult neurosurgery. If no, then probable ischemic stroke. Review CT exclusions: are any oberved? Repeat neurologic exam: are deficits variable or rapidly improving? Review thrombolytic exclusions: are any observed? Review patient data: is symptom onset now >3 hours? Decision – Is the patient a candidate for thrombolytic therapy? Drug – Begin thrombolytic therapy with i. v. rt-PA
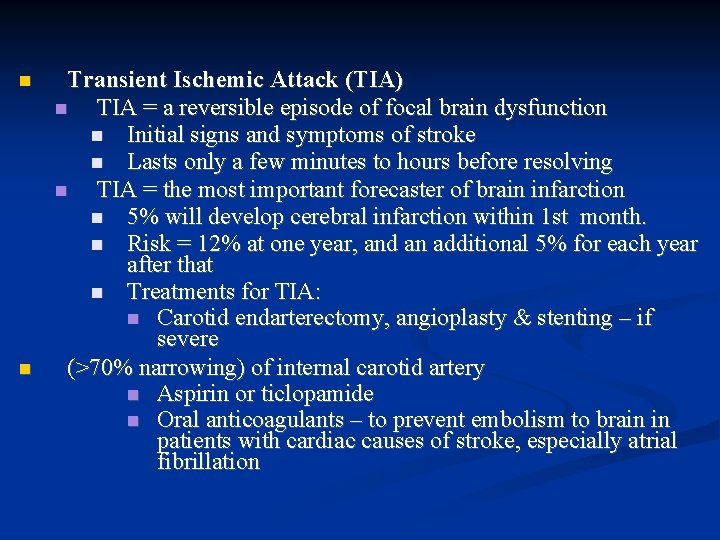
Transient Ischemic Attack (TIA) TIA = a reversible episode of focal brain dysfunction Initial signs and symptoms of stroke Lasts only a few minutes to hours before resolving TIA = the most important forecaster of brain infarction 5% will develop cerebral infarction within 1 st month. Risk = 12% at one year, and an additional 5% for each year after that Treatments for TIA: Carotid endarterectomy, angioplasty & stenting – if severe (>70% narrowing) of internal carotid artery Aspirin or ticlopamide Oral anticoagulants – to prevent embolism to brain in patients with cardiac causes of stroke, especially atrial fibrillation
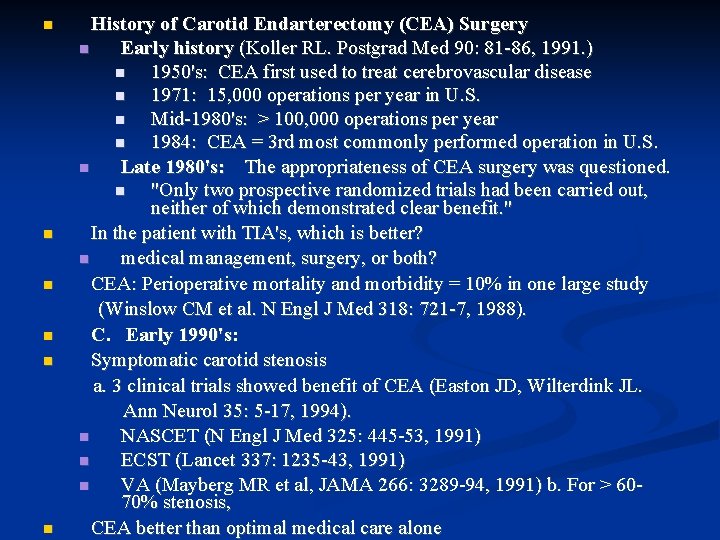
History of Carotid Endarterectomy (CEA) Surgery Early history (Koller RL. Postgrad Med 90: 81 -86, 1991. ) 1950's: CEA first used to treat cerebrovascular disease 1971: 15, 000 operations per year in U. S. Mid-1980's: > 100, 000 operations per year 1984: CEA = 3 rd most commonly performed operation in U. S. Late 1980's: The appropriateness of CEA surgery was questioned. "Only two prospective randomized trials had been carried out, neither of which demonstrated clear benefit. " In the patient with TIA's, which is better? medical management, surgery, or both? CEA: Perioperative mortality and morbidity = 10% in one large study (Winslow CM et al. N Engl J Med 318: 721 -7, 1988). C. Early 1990's: Symptomatic carotid stenosis a. 3 clinical trials showed benefit of CEA (Easton JD, Wilterdink JL. Ann Neurol 35: 5 -17, 1994). NASCET (N Engl J Med 325: 445 -53, 1991) ECST (Lancet 337: 1235 -43, 1991) VA (Mayberg MR et al, JAMA 266: 3289 -94, 1991) b. For > 6070% stenosis, CEA better than optimal medical care alone
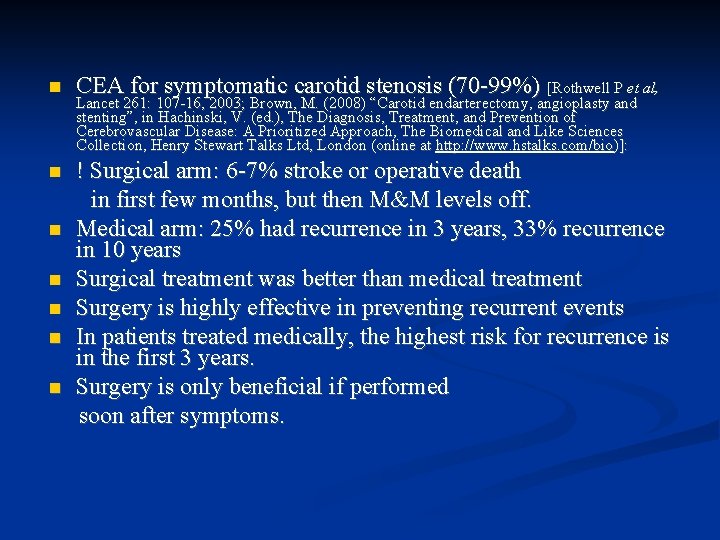
CEA for symptomatic carotid stenosis (70 -99%) [Rothwell P et al, ! Surgical arm: 6 -7% stroke or operative death in first few months, but then M&M levels off. Medical arm: 25% had recurrence in 3 years, 33% recurrence in 10 years Surgical treatment was better than medical treatment Surgery is highly effective in preventing recurrent events In patients treated medically, the highest risk for recurrence is in the first 3 years. Surgery is only beneficial if performed soon after symptoms. Lancet 261: 107 -16, 2003; Brown, M. (2008) “Carotid endarterectomy, angioplasty and stenting”, in Hachinski, V. (ed. ), The Diagnosis, Treatment, and Prevention of Cerebrovascular Disease: A Prioritized Approach, The Biomedical and Like Sciences Collection, Henry Stewart Talks Ltd, London (online at http: //www. hstalks. com/bio)]:
Asymptomatic carotid stenosis Asymptomatic Carotid Atherosclerosis Study (ACAS) (JAMA 1421 -28, 1995): Surgery also of value for asymptomatic stenosis (>60%). 53% reduction in risk of ipsilateral stroke and any perioperative stroke or death. Asymptomatic carotid bruits are common. Occur in 5% of population > age 45 More common in women Risk of stroke = 2% per year ACST: Risk of Stroke or Death after CEA or Medical Treatment for Asymptomatic Carotid Stenosis (6099%) (Halliday A et al, Lancet 363: 1491 -1502, 2004): Initial risk greater for surgical treatment (CEA) Risk at 5 years greater for medical treatment Surgical vs. medical: Risks cross at 2 years.
Carotid Angioplasty and Stenting Carotid Angioplasty – Carotid and Vertebral Artery Transluminal Angioplasty Study (CAVITAS): Comparison of Endovascular vs. Surgical Treatment (Mc. Cabe DJH et al, Stroke 36: 281 -6, 2005) The 5 -year risk of stroke or death was the same. Cranial nerve palsies or hematomas were more common with surgery. The 5 -year rate of restenosis was greater with endovascular treatment.
. Carotid Stenting – Stenting and Angioplasty with Protection in Patients at High Risk for Endarterectomy (SAPPHIRE) (Yadav JS et al, New Engl J Med 361: 1493 -1501, 2004). ! “. . . Carotid stenting with the use of an emboli-protection device is not inferior to carotid endarterectomy. ”
Anesthetic Management of Carotid Angioplasty and Stenting (Drummond J. Anesthesia for Carotid Endarterectomy / Stenting. Dannemiller Anesthesiology Review Course, 2008) Dual antiplatelet treatment (aspirin and clopidogrel) Usually transfemoral (sometimes transcarotid) Usually MAC (neurologic exam) Two stages: Dilatation and Stenting Heparin to maintain ACT 250 -300 e. g. 500 units + 1000 units/hr Prevent / treat bardycardia independent arterial line glycopyrrolate pre-treatment atropine before dilatation (+/-) external pacer (on and available) Carotid stenting can cause severe bradycardia, hypotension, and cerebral hypoperfusion.

Preoperative Evaluation Typical diagnostic workup for TIA/stroke (Koller RL. Postgrad Med 90: 81 -96, 1991) CT scan and/or MRI Lab studies -- CBC, platelet count, PT/PTT Carotid studies Carotid ultrasound Carotid angiography Cardiac studies Electrocardiogram Echocardiography
Cardiac evaluation of patients with TIA's or stroke (Sirna S et al, Stroke 14 -23, 1990) Strong association between carotid and coronary artery disease Cardiac events often determine the fate of the TIA patient. Abnormal exercise EKG's = 28% in patients with TIA's and no known cardiac symptoms. Abnormal stress or dipyridamole thallium studies = 45% in patients with TIA or mild stroke and no apparent heart disease.
ACC/AHA Gudielines on Peri-operative Cardiovascular Evaluation and Care for Non-Cardiac Surgery (Fleisher LA et al, Circulation 116: e 418 -99, 2007) Active Cardiac Conditions a. Unstable coronary syndromes (unstable or severe angina, recent MI) Decompensated heart failure Significant arrhythmias Severe valvular disease (severe aortic stenosis, symptomatic mitral stenosis) Functional Capacity a. If there are no “active cardiac conditions” and the functional capacity is > 4 METs without symptoms, proceed with planned surgery. b. If the functional capacity is < 4 METs or unknown: CEA is considered to be “intermediate risk surgery” (reported cardiac risk = 1 -5 %) Clinical Risk Factors include: H/o ischemic heart disease H/o compensated or prior heart failure H/o cerebrovascular disease (i. e. , carotid stenosis) diabetes mellitus renal insufficiency With 1 or more clinical risk factors, “Proceed with planned surgery with HR control or consider non-invasive testing if it will change management. ”
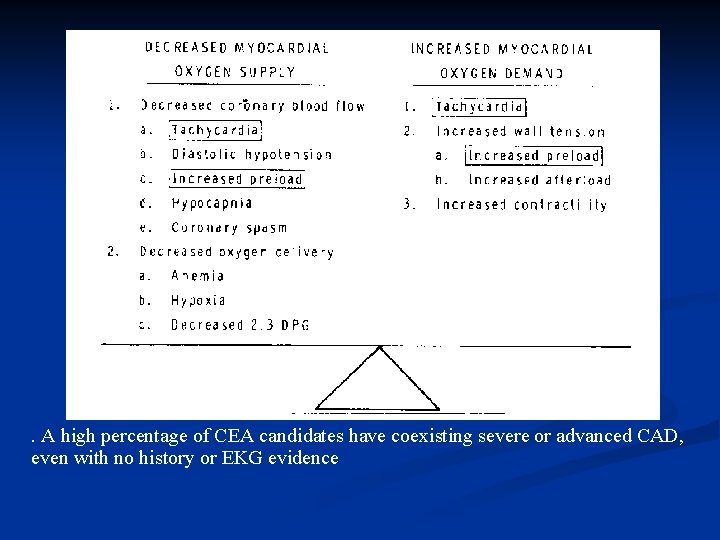
Intraoperative management Three main goals of anesthesia for CEA surgery -- to protect the heart from ischemia, to protect the brain from ischemia, and to have the patient awaken quickly at the end of surgery (Roizen MF, Anesthesia for Vascular Surgery, In: Barash PG et al (eds. ), Clinical Anesthesia, 1989, pp. 1015 -47). Protect the heart from ischemia. Maintain normal hemodynamics, oxygenation, and ventilation. Myocardial oxygen supply and demand balance (Thys DM, Kaplan JA. Cardiovascular Physiology. In: Miller RD (ed), Anesthesia, 3 rd. Ed. New. York: Churchill-Livingstone, 1990, pp. 551 -83. ) Avoid factors that decrease myocardial O 2 supply Avoid factors that increase myocardial O 2 demand
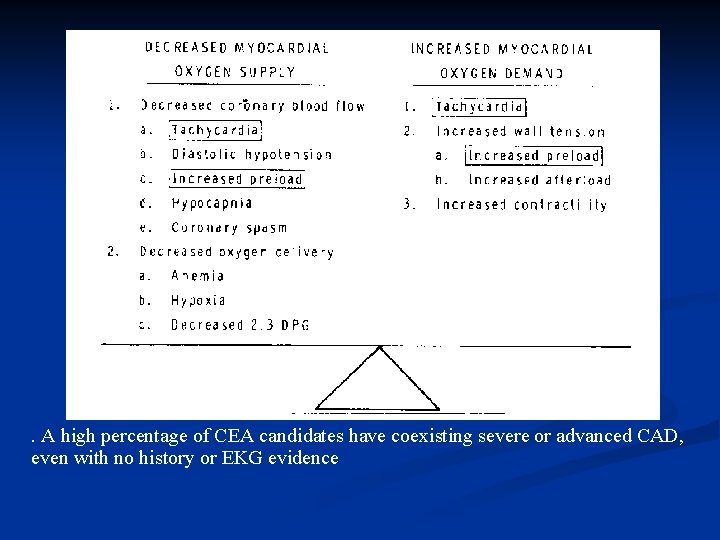
. A high percentage of CEA candidates have coexisting severe or advanced CAD, even with no history or EKG evidence
Protect the brain from ischemia. Some guidelines: (Wendling WW, Carlsson C. Guidelines for anesthesia and cerebral protection in neurovascular surgery. In: Rosenwasser RH et al (eds. ), Cerebral Ischemia: Clinical Implications and. Therapeutics. Commack, NY: Nova Scientific Publishers, 1994, pp. 77 -100) Maintain a normal or high normal blood pressure. Maintain normocarbia or slight hypocarbia. Avoid extreme hyperglycemia. Monitor for cerebral perfusion. Treat cerebral ischemia if it occurs. Have the patient awaken quickly after the operation.
Premedication -- "light" premedication is recommended, to permit: Neurologic assessment during regional anesthesia. Fast "wakeup" after general anesthesia.
Monitors: Use routine monitors as reminder for additional monitors.
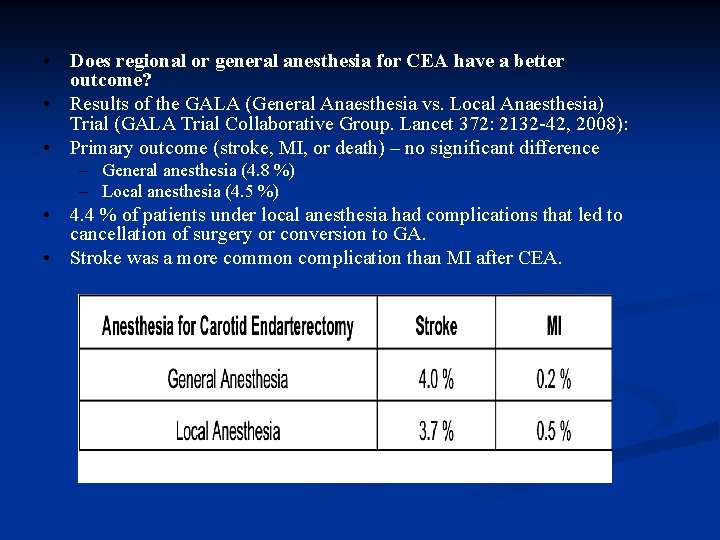
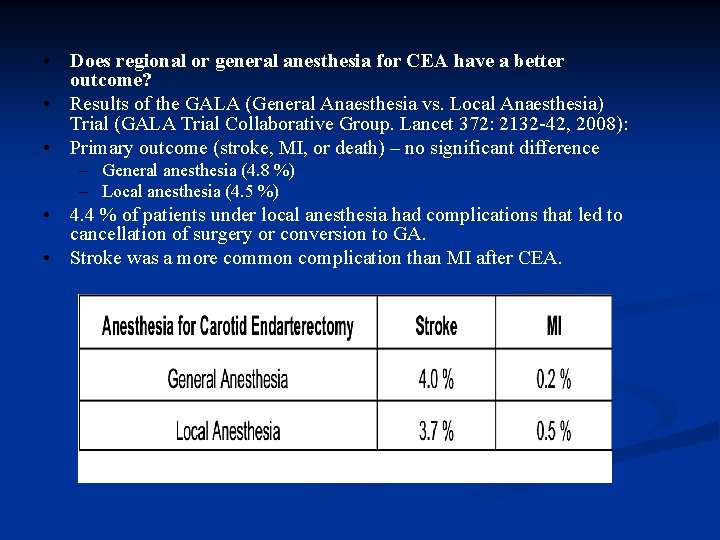
• Does regional or general anesthesia for CEA have a better outcome? • Results of the GALA (General Anaesthesia vs. Local Anaesthesia) Trial (GALA Trial Collaborative Group. Lancet 372: 2132 -42, 2008): • Primary outcome (stroke, MI, or death) – no significant difference – General anesthesia (4. 8 %) – Local anesthesia (4. 5 %) • 4. 4 % of patients under local anesthesia had complications that led to cancellation of surgery or conversion to GA. • Stroke was a more common complication than MI after CEA.
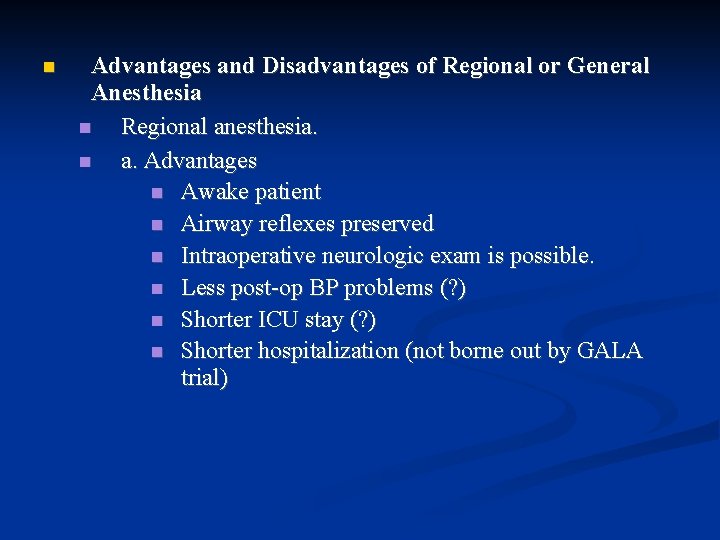
Advantages and Disadvantages of Regional or General Anesthesia Regional anesthesia. a. Advantages Awake patient Airway reflexes preserved Intraoperative neurologic exam is possible. Less post-op BP problems (? ) Shorter ICU stay (? ) Shorter hospitalization (not borne out by GALA trial)

b. Disadvantages (Roizen MF. Anesthesia goals for operations to relieve or Need for patient cooperation Possible loss of patient cooperation, with onset of new neurologic deficit, because of: confusion panic seizures Inability to secure airway if panic, seizure, or oversedation occur ! An unexpected delayed deficit may occur sometime after the test period. ! Inability to administer drugs such as thiopental that might protect the brain against ischemia prevent cerebrovascular insufficiency. In: Roizen MF (ed), Anesthesia for Vascular Surgery. New York: Churchill-Livingstone, 1990, pp. 103 -22. )
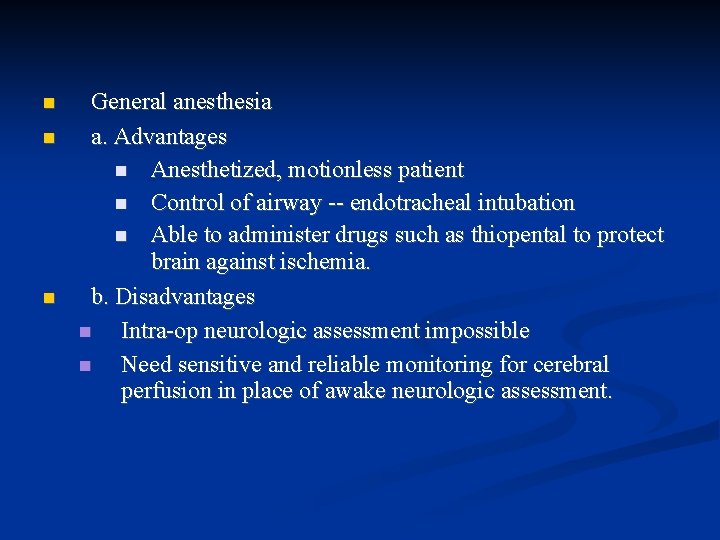
General anesthesia a. Advantages Anesthetized, motionless patient Control of airway -- endotracheal intubation Able to administer drugs such as thiopental to protect brain against ischemia. b. Disadvantages Intra-op neurologic assessment impossible Need sensitive and reliable monitoring for cerebral perfusion in place of awake neurologic assessment.

Regional Anesthesia for CEA Techniques Local infiltration by surgeon Superficial cervical plexus block Deep cervical plexus block Combined superficial and deep cervical plexus blocks
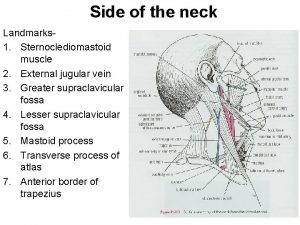
Superficial cervical plexus block (Carron H et al. Regional anesthesia: Techniques and Clinical Applications. Orlando, FL: Grune & Stratton, 1984, pp. 10 -15) Landmarks? Crossing of. . . External jugular vein and Posterior border of sternocleidomastoid muscle Possible complications include: Accidental injection into internal jugular vein. Hematoma formation (tear in wall of vein) Venous air embolus Anatomy Superficial cervical space communicates with the deep cervical plexus space. Inject below the investing fascia, not just subcutaneously (Pandit et al. Brit J Anaesth 91: 733 -5, 2003).
Deep Cervical Plexus Block (Carron H et al. Regional anesthesia: Techniques and Clinical Applications. Orlando, FL: Grune & Stratton, 1984, pp. 10 -15) Landmarks? Line between mastoid process and suprasternal notch Aim perpendicularly for transverse processes of C 2 -C 4. Possible complications? Recurrent laryngeal nerve paralysis = most common Stellate ganglion block = next most common Cervical subarachnoid block with possible phrenic nerve block Direct injection of local anesthetic into vertebral artery, resulting in seizures or apnea
General Anesthesia for CEA A. Induction. Goal = to avoid extreme changes in blood pressure and heart rate. One suggested regimen: Preoxygenate Defasciculating or priming dose of non-depolarizing muscle relaxant. Titrate anesthetics slowly. One possible regimen: Fentanyl Lidocaine Propofol or etomidate Esmolol Institute controlled ventilation with 100% O 2. Muscle relaxant for intubation: Succinylcholine (unless patient has hemiplegia) Vecuronium or rocuronium (alternate choices) Aim for smooth intubation

Maintenance. "Balanced anesthesia" = a reasonable choice Volatile inhalational agent (isoflurane, sevoflurane, or desflurane) Nitrous oxide (? ) Narcotic (fentanyl) Nondepolarizing muscle relaxant (vecuronium or rocuronium)
Two Potential Intraoperative Complications Cardiac arrhythmias: Bradycardia -- during neck dissection Most likely cause = compression of carotid baroreceptor Mechanism? Reflex involving: CN IX (Glossopharyngeal) = afferent CN X (Vagus) = efferent Lidocaine injection of carotid baroreceptor by surgeon Evidence of decreased cerebral perfusion -- during carotid clamping Is monitoring for cerebral perfusion even necessary? These monitors have not been shown to improve outcome. Logic dictates that monitoring techniques assuring adequate cerebral function at the lowest myocardial work have a place in CEA surgery (Roizen MF, 1990). Types of cerebral perfusion monitors Raw 16 -20 lead encephalogram (EEG) Considered to be the "gold standard" monitor Disadvantages: Need specially trained personnel Electrically "noisy" OR environment Bulky equipment Significant change = > 50% reduction in EEG amplitude flattening of EEG
Processed EEG only monitors 2 -4 channels. EEG electrodes placed on "watershed" areas Still may miss ischemia during clamping Somatosensory evoked potentials (Lam AM et al. Anesthesiology 75: 1521, 1991) a) "Subtracts out" background EEG activity, leaving only the evoked potential from: median nerve (wrist) posterior tibial nerve (ankle) Significant change = > 50% reduction in amplitude flattening of SSEP Similar sensitivity and specificity to EEG Both SSEP's and EEG are associated with a considerable false positive rate.
Stump pressures Surgeon measures pressure in stump of carotid artery above cross-clamp. Significant reduction = stump pressure < 50 mm Hg Problem = poor correlation with EEG findings: False positives = stump pressure < 50 mm Hg with normal EEG False negatives = stump pressure > 50 mm Hg with "ischemic" EEG May not adequately assess cerebral perfusion after stroke or RIND Regional cerebral blood flow (Xenon washout) only available in certain centers indicates global well-being rather than focal cerebral ischemia Jugular venous oxygen saturation ! global well-being rather than focal ischemia Transcranial Doppler (to detect emboli or ischemia) Neurologic assessment under regional anesthesia
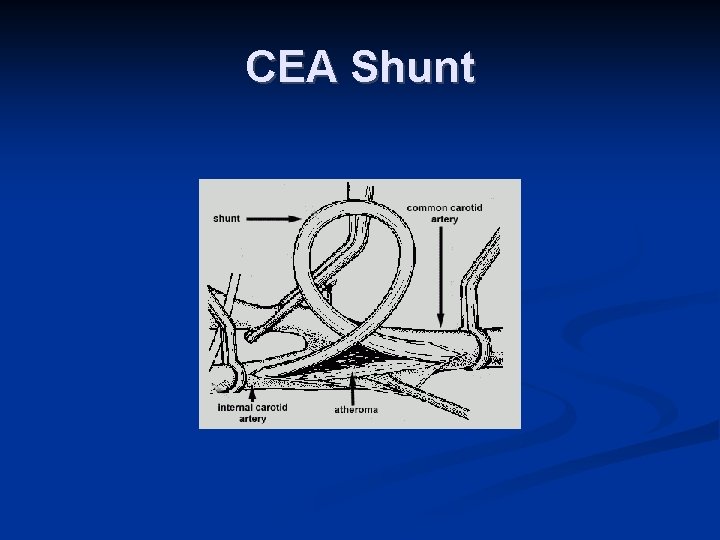
Responses to evidence of decreased cerebral perfusion. Surgeon can unclamp the carotid artery and insert shunt. a) Shunting during carotid endarterectomy -- three schools of practice: Shunt routinely. Shunt never, or very rarely. Shunt selectively, based on monitoring to detect cerebral ischemia. Advantage -- preserves carotid flow Potential risks: Thromboembolism Intimal dissection Thrombus formation Air embolism Obstruction of surgical field
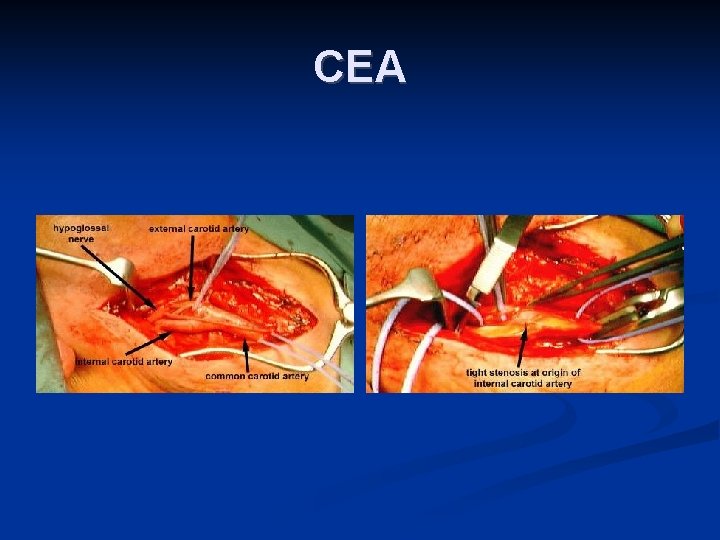
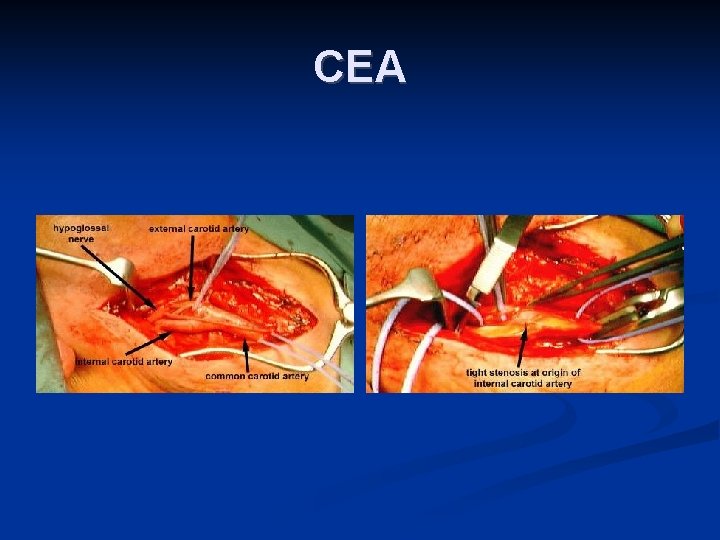
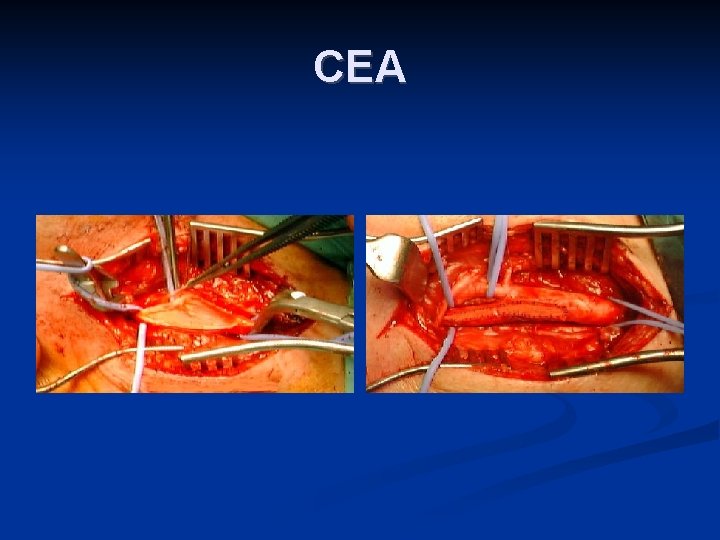
CEA
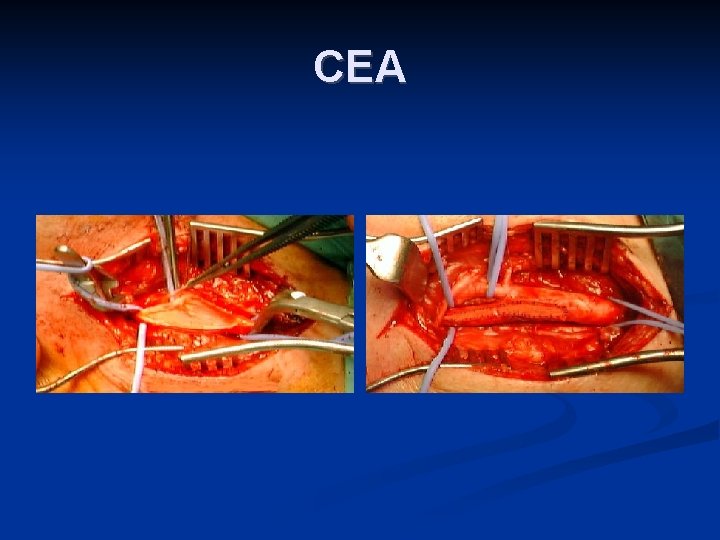
CEA
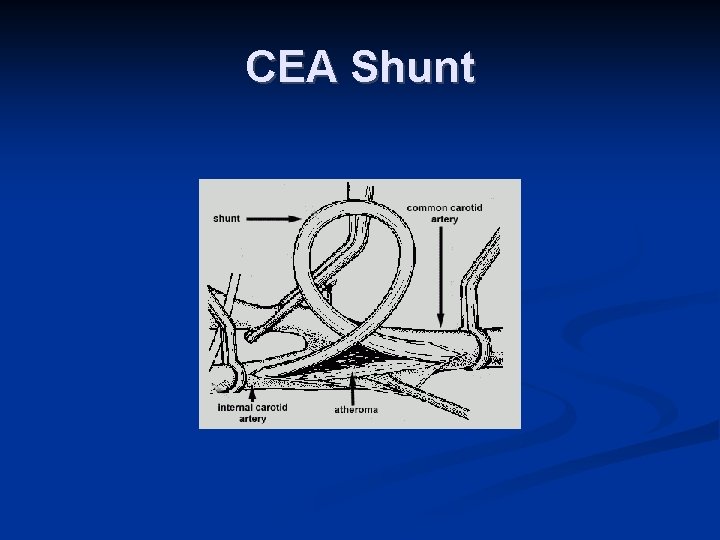
CEA Shunt
Increase the mean arterial pressure Increases cerebral perfusion pressure Increases cardiac afterload and may precipitate myocardial ischemia. So follow ST segments on EKG Pharmacologic cerebral protection with thiopental Used more commonly for clipping of intracerebral aneurysms than for carotid endarterectomy Thiopental was cerebroprotective in one prospective randomized study in humans (Nussmeyer NA et al. Anesthesiology 64: 165 -70, 1986). Emergence -- Main concerns: Smooth and rapid awakening from general anesthesia, in order to obtain a neurologic assessment. Control of blood pressure

Post-operative considerations. Potential postoperative complications occur in 4 locations: “In the arm. ” Hypertension = a very common complication Incidence was 19% in one study. More common if patient was hypertensive preoperatively. Hypotension – in approximately 5% of patients In the neck. Problems secondary to surgery on the neck: Wound hematoma – occurred in 5. 5% of NASCET patients Paralysis of cranial nerves (VII, IX, X, or XII) Carotid body dysfunction In the head. Cerebrovascular complications include: Carotid artery thrombosis Emboli Stroke Hyperperfusion syndrome Manifests as severe unilateral headache, which is postural Related to preoperative hypoperfusion and loss of autoregulation Seizures – relatively uncommon D. In the chest. Myocardial infarction often occurs
 Mani vindhya
Mani vindhya Femoral endarterectomy
Femoral endarterectomy Reverse tap stenting technique
Reverse tap stenting technique Mini culotte stenting
Mini culotte stenting Inverted provisional stenting
Inverted provisional stenting Lana schumacher md
Lana schumacher md Carotid sinus hypersensitivity
Carotid sinus hypersensitivity Orbital fissure anatomy
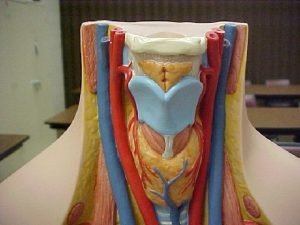
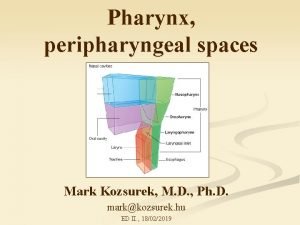
Orbital fissure anatomy Contents of carotid sheath
Contents of carotid sheath Left subclavian vein
Left subclavian vein Fascia of parotid gland
Fascia of parotid gland Branches of subclavian artery
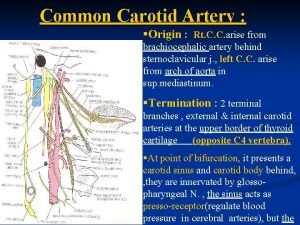
Branches of subclavian artery Carotid sheath contents
Carotid sheath contents Carotid sheath
Carotid sheath Carotid terminus
Carotid terminus Combat lifesaver powerpoint
Combat lifesaver powerpoint Branch of basilar artery
Branch of basilar artery Triangle
Triangle Tympanic antrum
Tympanic antrum Salpingopharyngeus
Salpingopharyngeus Carotid cavernous fistula
Carotid cavernous fistula Carotid cana
Carotid cana Cat sinus anatomy
Cat sinus anatomy Blood vessel man model
Blood vessel man model Lymph nodes ear
Lymph nodes ear Amurosis fugax
Amurosis fugax Brain arterial supply
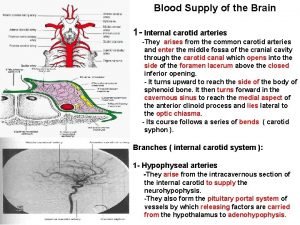
Brain arterial supply Carotid cochlear dehiscence
Carotid cochlear dehiscence Carotid sinus
Carotid sinus Posterior auricular vein
Posterior auricular vein Pheocromocytoma
Pheocromocytoma Carotid artery pulse
Carotid artery pulse Neck veins waves
Neck veins waves Difference between doppler and duplex
Difference between doppler and duplex External carotid artery
External carotid artery Carotid anatomy
Carotid anatomy Cinaslı mani özellikleri
Cinaslı mani özellikleri Solenoide
Solenoide Mani srivastava
Mani srivastava Mani vaya
Mani vaya Mani srivastava
Mani srivastava Koşma kafiye düzeni
Koşma kafiye düzeni Mani parkhe
Mani parkhe