Carotid Artery Stenting Timing after Stroke Dr Adnan


- Slides: 30
Carotid Artery Stenting: Timing after Stroke Dr. Adnan Siddiqui, MD Ph. D Professor of Neurosurgery, State University of New York at Buffalo CRT 2020 Maryland
Disclosure Statement of Financial Interest § Current Research Grants: Co-investigator: NIH/NINDS 1 R 01 NS 091075 Virtual Intervention of Intracranial Aneurysms § Financial Interest: Amnis Therapeutics, Apama Medical, Blink. TBI, Inc, Buffalo Technology Partners, Inc. , Cardinal Health, Cerebrotech Medical Systems, Inc, Claret Medical, Cognition Medical, Endostream Medical, Ltd, Imperative Care, International Medical Distribution Partners, Rebound Therapeutics Corp. , Rist Neurovascular, Inc. , Serenity Medical, Inc. , Silk Road Medical, Stim. Med, Synchron, Three Rivers Medical, Inc. , Viseon Spine, Inc. , § Consultant/Advisory Board: Amnis Therapeutics, Boston Scientific, Canon Medical Systems USA, Inc. , Cerebrotech Medical Systems, Inc. , Cerenovus, Claret Medical, Corindus, Inc. , Endostream Medical, Ltd, Guidepoint Global Consulting, Imperative Care, Integra, Medtronic, Micro. Vention, Northwest University – DSMB Chair for HEAT Trial, Penumbra, Rapid Medical, Rebound Therapeutics Corp. , Serenity Medical, Inc. , Silk Road Medical, Stim. Med, Stryker, Three Rivers Medical, Inc. , Vas. Sol, W. L. Gore & Associates § National PI/Steering Committees: Cerenovus LARGE Trial and ARISE II Trial; Medtronic SWIFT PRIME and SWIFT DIRECT Trials; Micro. Vention FRED Trial & CONFIDENCE Study; MUSC POSITIVE Trial; Penumbra 3 D Separator Trial, COMPASS Trial, INVEST Trial; § No consulting salary arrangements. All consulting is per project and/or per hour.
Carotid Artery Disease § Significant cause of stroke − 7% of patients present with an initial stroke Liberato, B, Chong, K, Lee, H, Trocio, S, et al. Degree of Carotid Artery Stenosis and Potential Eligibility for Intervention: the Northern Manhattan Stroke Study. Neurology 2004; 62(Suppl 5): A 139. §
Management Options Medical Management ASA +/- Plavix + Statin + Carotid Endarterectomy (CEA) Carotid Angioplasty and Stenting (CAS) Transcarotid artery revascularization (TCAR)
CEA vs CAS vs TCAR § Medical status/comorbidities § Surgical considerations § Angiographic characteristics § Neurologic status § Access Stent Placement Issues
Where does 2 week time-frame come from? § Carotid Endarterectomy Trialists Collaboration –Combined data from 2 RCTs: ECST, NASCET –N=5893 patients with 33, 000 personyears follow-up
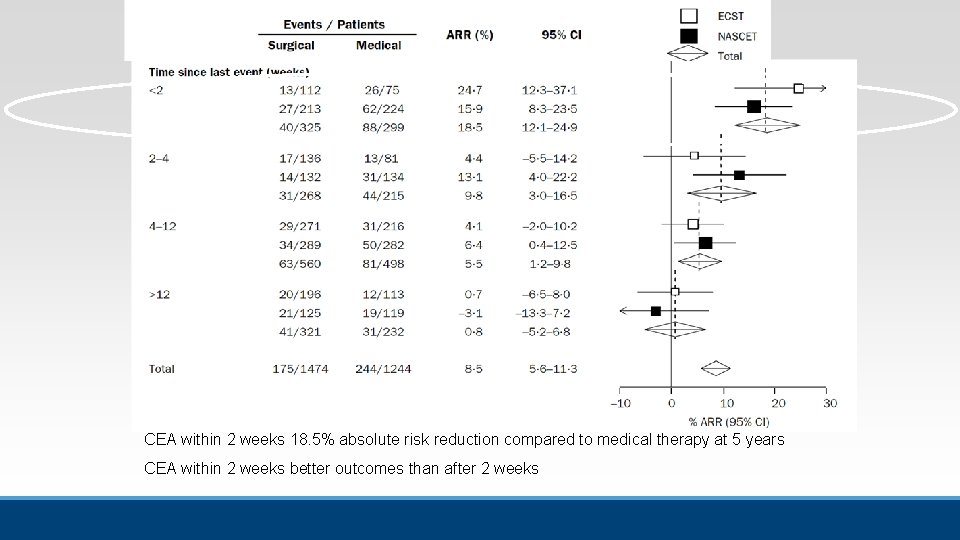
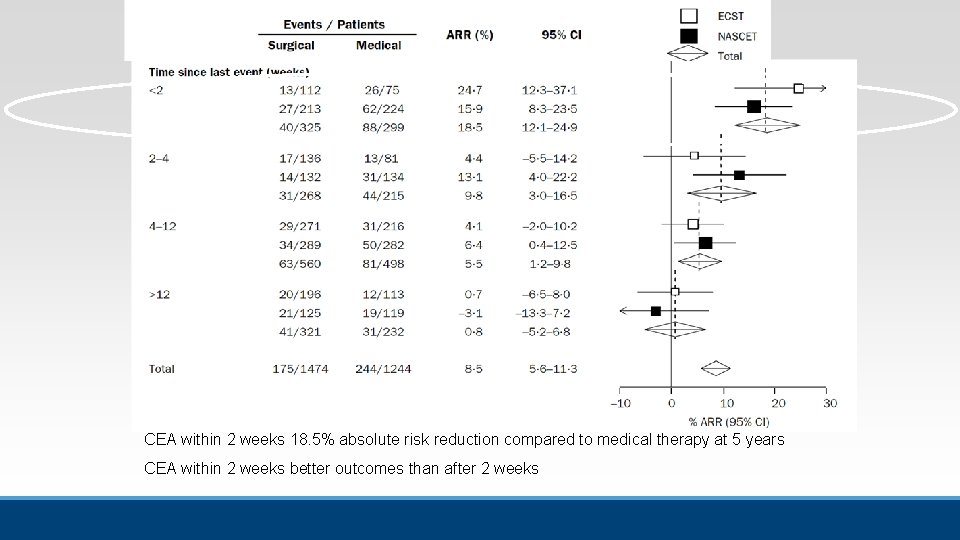
CEA within 2 weeks 18. 5% absolute risk reduction compared to medical therapy at 5 years CEA within 2 weeks better outcomes than after 2 weeks
AHA/ASA recommended CEA within 2 weeks of symptoms in 2006
§ Suggestion that CEA very early after symptom onset (< 48 h) has higher complications –Risk of hemorrhagic transformation –Dislodging acute thrombus
My Typical Setup -Preop ASA/Plavix (or Brillinta), with Plavix response < 200 -R femoral 9 F sheath, micropuncture set, In. Qwire, 7 F dilator, U/S guidance, -VTK or SIM 2 select catheter, 038 exchange glidewire or Supercore for MOMA -50 U/kg heparin IV with ACT>250, 0. 4 mg glycopyrrolate -Access MOMA for most lesions 9 F balloon guide catheter for lesions involving the ECA Neuron Max guide if ++ tortuous -Distal embolic protection device 7. 2 mm for Balloon Guide and 8 F Guide -Angioplasty balloon (pre-plasty only – and if needed) -Closed cell Stent -IVUS post stenting
§Timing of treatment in Sx ICA stenosis depending on severity of stroke –Urgent NIHSS >7, how to assess and treat carotid –TIA/Minor, Mod, Large, Crescendo/Evolving §Method of treatment –CEA vs CAS, same as any elective case –Take high risk of both CEA and CAS and select best for pt including use of TCAR –Consider newer stents and use of IVUS on all CAS –Mod stroke, consider CEA>CAS if equivocal
Historical trends § 2004: pooled analysis of trials suggested tx sx ica stenosis within two weeks § 2006 AHA/ASA guidelines made formal recommendation § 2017 paper analyzing treatment trends from coded data: – 25 days in 2005 to 6 days in 2013 – 40% in 2005 to 73% in 2013 § 2007 UK National Stroke Strategy rec Tx for Sx ICA >70% within 48 hrs or TIA or minor stroke
§ Acute Stroke with NIHSS>7 and ipsilateral carotid stenosis § TIA § Minor/Mod § Large § Evolving/crescendo
Acute Simultaneous intervention § Evaluate carotid, not always occluded, ICA T § Aspiration catheter…if crosses easily…aspirate to petrous segment being careful not to push…then focus on crossing lesion and access M 1 § If unable to advance aspiration catheter…balloon guide and obtain ica access, exchange filter, then stent. § Ensure can climb guide through stent if planning use of sten-triever intracranially, otherwise only use aspiration systems. § Stent vs Plasty – I favor stent (Plavix vs Brilinta, Effient contraindicated) –What if t. PA? § If high grade, beware reperfusion ICH, tight blood pressure control after opening intracranially
Natural History TIA/Minor Stroke § Tsantilas J Cardiovasc Surg 2015, 56: 845 – 6. 4% days 2 -3 – 19. 5% within 7 days – 26% within 14 days § Amarenco NEJM 2016 374(16): 1533 –Natural history of TIA, 50% of second event is within 48 hrs!
§ 2 single center studies showed no difference in risk of stroke or mortality related to timing of CEA after neurologic event (Sharpe, 2013, Rantner 2015) § 1 study showed increased periprocedural risk with early CEA (Stromberg, Swedvasc Registry, Stroke 2012) – 11. 5% within 48 hrs (Possible inclusion of crescendo/evolution) – 3. 6% from 3 -7 days § German study, retrospective review, Tsantilas, Stroke 2016; 47: 2783 – 56366 elective CEA for sx ICA stenosis –I: 0 -2, II: 3 -7, III: 8 -14, IV: 15 -180 –I: 3. 0%, II: 2. 5%, III: 2. 6%, IV: 2. 3% –In hospital any stroke or death
§ Systematic Review of stroke after CEA for crescendo and evolution (Rerkasem, Stroke 2009, 40: e 564 –Crescendo 11. 4% –Evolution 20. 2%
TIA/Minor/Mod § TIA: Unstable Angina of the Brain –Ferrero Ann Vasc Surg 2014: 28(1) Jan 227 – 891 pts with sx ICA stenosis –CEA within 48 hrs in 176 –TIA: 1. 8% stroke –Crescendo: 0% stroke –Evolving: 7. 5% stroke (slowly continuously getting worse)
TIA/Minor/Mod § Capoccia J Vas Surg 2011; 53(3): 622 – 62 pts with Sx ICA stenosis –CEA mean 34 hrs –NIHSS 4 -15 –No post op stroke (? Imaging? ) –All with improved NIHSS (? Discharge or 30 day? )
TIA/Minor/Mod § Barbetta J Vasc Surg 2014 59(2): 440 – 90 pts Sx ICA stenosis –CEA (13 -117 hrs) – 27 TIA: 0% stroke – 52 mild/mod: 5. 8% stroke – 11 Evolution: 27% stroke
Large Stroke § Mortality very high § Share internal data of high NIHSS § Min salvagle tissue § Only if pt makes significant recovery consider revasc § Rec: Not early or acute setting
Crescendo/Evolving § Crescendo § Evolving: pt continues to gradually become more and more symptomatic and core infarct continues to increase § Rec: treat
CEA or CAS § Rantner Stroke 2017, 48 –Carotid Stenosis Trialists Collaboration, pooled analysis of 4 randomized Trials (sx pts from CREST, EVA-3 S, SPACE, ICSS) – 4138 pts, those treated within 7 days included only 14% CEA and 11% CAS of total pts, among those risk of stroke and death were – 8. 3% CAS vs 1. 3% CEA –> 7 days, 7. 1% CAS vs 3. 6% CEA
The Timing Issue § For symptomatic carotid stenosis, clear benefit of CEA and CAS for prevention of stroke § For tandem LVO and carotid stenosis, preference to avoid stenting acutely unless absolutely needed to cross with guide catheter § Timing of carotid revascularization still area of debate § Guidelines suggest carotid intervention within 2 weeks of symptom onset

How about time-frame for carotid angioplasty and stenting after initial event?
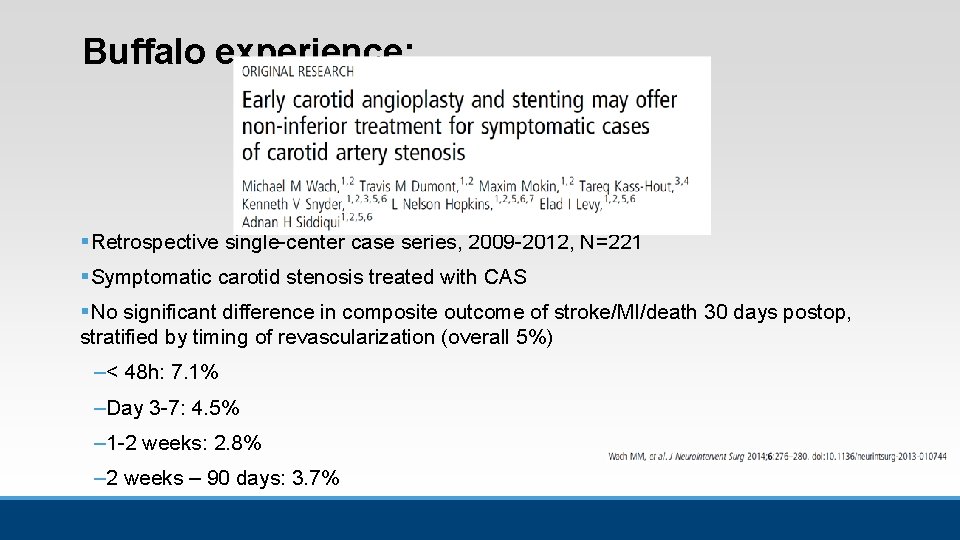
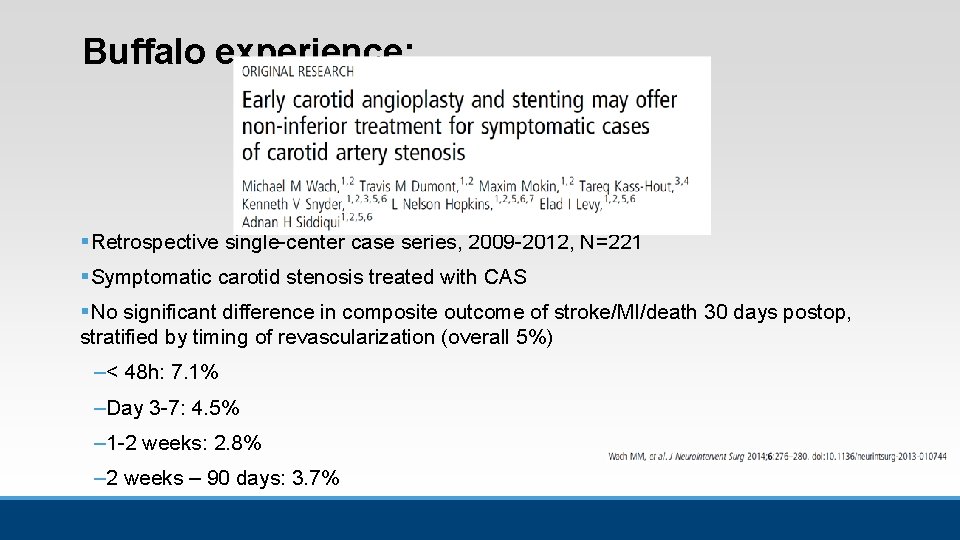
Buffalo experience: § Retrospective single-center case series, 2009 -2012, N=221 § Symptomatic carotid stenosis treated with CAS § No significant difference in composite outcome of stroke/MI/death 30 days postop, stratified by timing of revascularization (overall 5%) –< 48 h: 7. 1% –Day 3 -7: 4. 5% – 1 -2 weeks: 2. 8% – 2 weeks – 90 days: 3. 7%
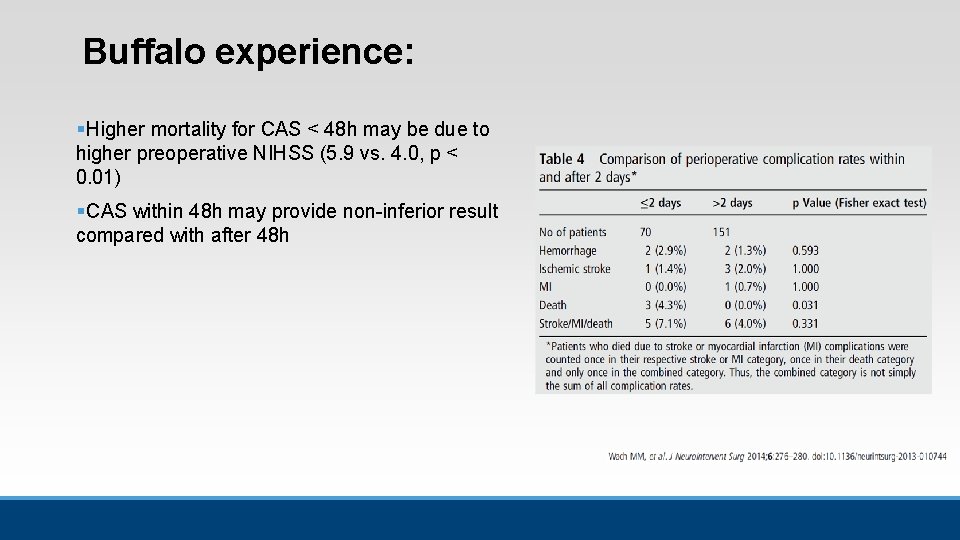
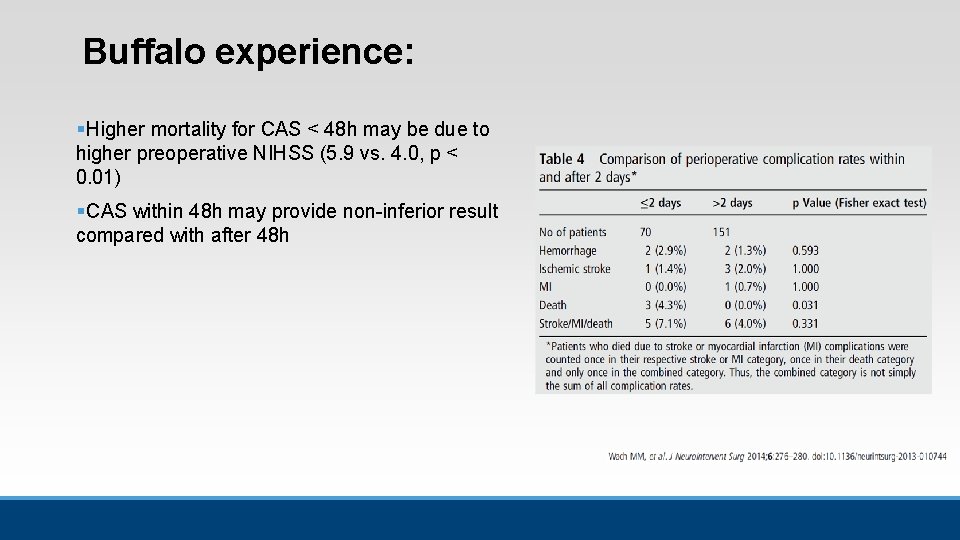
Buffalo experience: § Higher mortality for CAS < 48 h may be due to higher preoperative NIHSS (5. 9 vs. 4. 0, p < 0. 01) § CAS within 48 h may provide non-inferior result compared with after 48 h
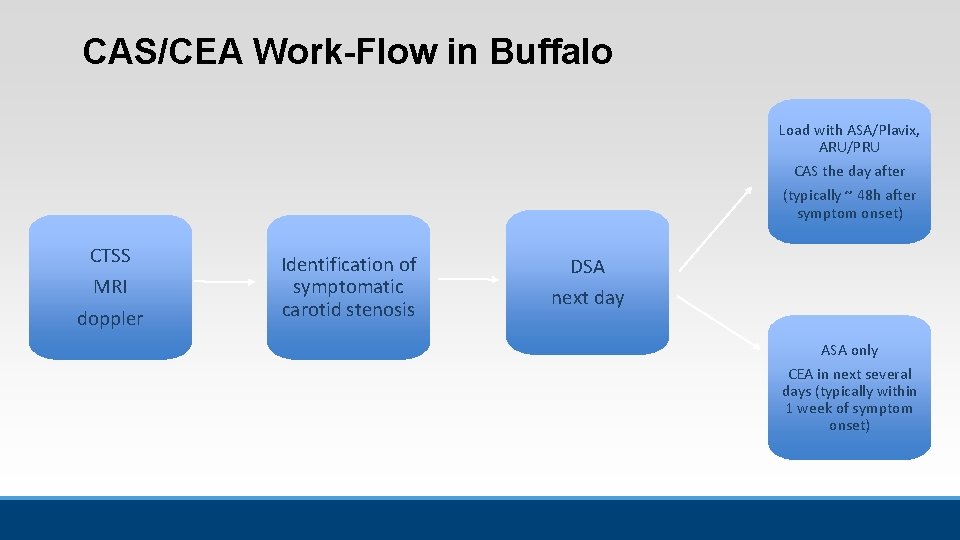
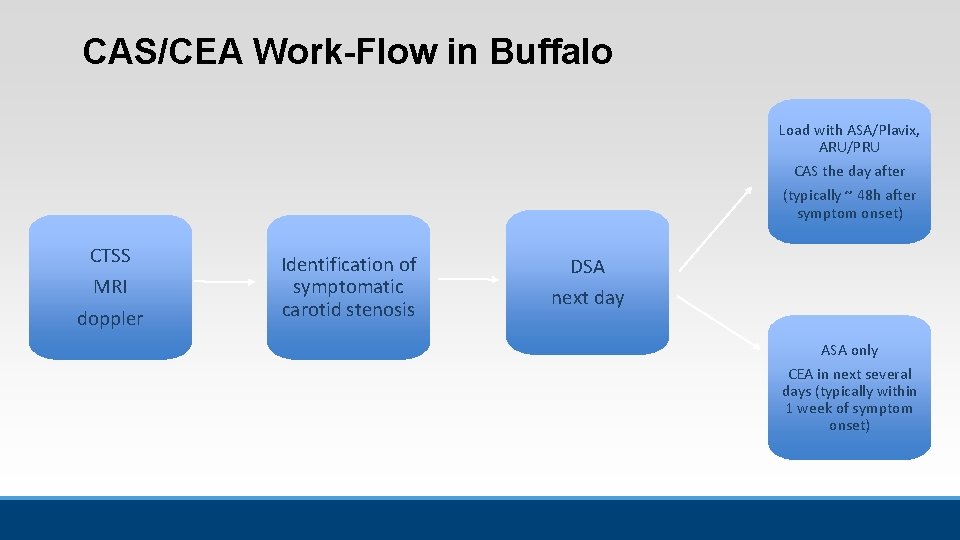
CAS/CEA Work-Flow in Buffalo Load with ASA/Plavix, ARU/PRU CAS the day after (typically ~ 48 h after symptom onset) CTSS MRI doppler Identification of symptomatic carotid stenosis DSA next day ASA only CEA in next several days (typically within 1 week of symptom onset)
Concluding Remarks § Timing of carotid revascularization after symptom onset still a topic of debate § Guidelines suggest CAS/CEA within 2 weeks § Randomized controlled trials are needed to assess specific timing of carotid revascularization within 2 weeks (e. g. < 48 h vs. > 48 h-2 wks)

Neuroendovascular Fellows: Michael Tso, MD Ph. D Gary Rajah, MD Rimal Dossani, MD