Caring for children and young people with Type

- Slides: 31
Caring for children and young people with Type 1 diabetes in school. Kelly Rowe, Alison Murray, Julie Stonehouse and Christine Mc. Partland Diabetes Specialist Nurses Ruth Weatherall/Hue Flannigan Paediatric Dietitian

Our Team Children’s Diabetes Nurses Dietitian’s Consultant Paediatricians Psychologist Support Workers
Clinic Appointments • MDT Clinic 4 x per year • Additional appointments for education and support may be required • School clinics
What is diabetes? Type 1 diabetes or Type 2 diabetes Type 1 – dependent on insulin. Goal: A fine balance of insulin, food and activity Target blood glucose: 4 – 7 mmol/l
Blood glucose testing: Most children test their blood glucose level regularly, a minimum of 5 times per day. This involves pricking their finger with a special device to obtain a small drop of blood which is placed on a strip and into a small electronic blood glucose meter.
Insulin Current treatments include: - • MDI (Multiple Daily Injections) • CSII (Continuous Subcutaneous Insulin Infusion)
Pen Therapy • Short acting insulin can be given every 2 hours if necessary • Long acting insulin is given once daily to maintain blood glucose
Insulin Pump Therapy Many children wear an insulin pump which delivers insulin 24 hours/day Basal insulin is pre-determined and should only be adjusted by diabetes team or parents Bolus insulin is given for the amount of carbohydrate consumed and/or if blood glucose is not within range
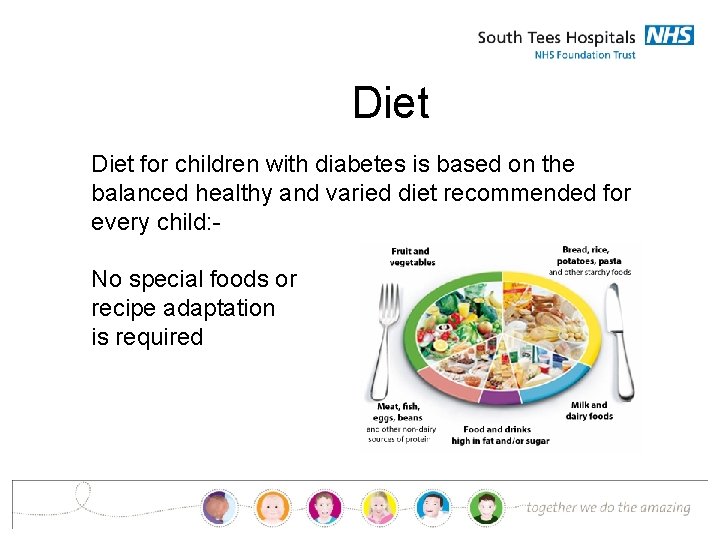
Diet for children with diabetes is based on the balanced healthy and varied diet recommended for every child: No special foods or recipe adaptation is required
Carbohydrate counting • What is carb counting? • What the children need to do at lunch time: Blood glucose test Count carb Inject Eat
Issues • Food not eaten • Young children may need support at meal times to ensure their meal contains carbohydrate • Treats in school
Hypoglycaemia (hypo) This is the most common short term complication and occurs when the blood glucose level falls too low. They are especially likely to happen before meals or during and after exercise. • Too much insulin • Not enough food to fuel an activity • A missed or delayed meal or snack • Hot weather • The child vomiting • Alcohol • No Reason
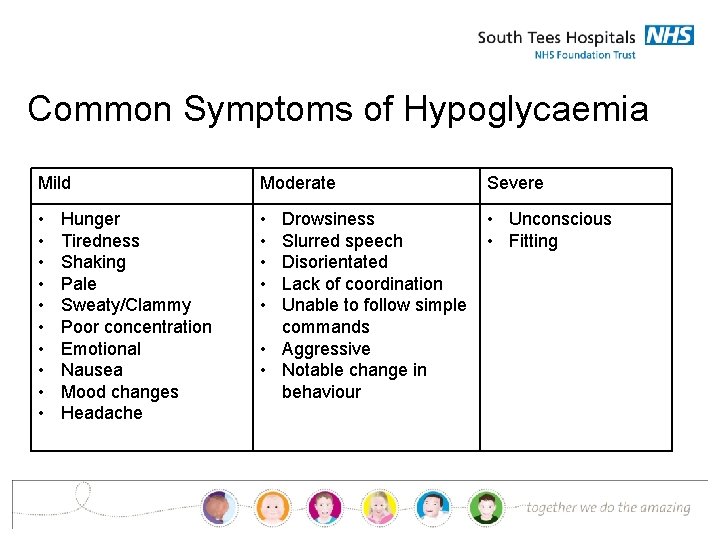
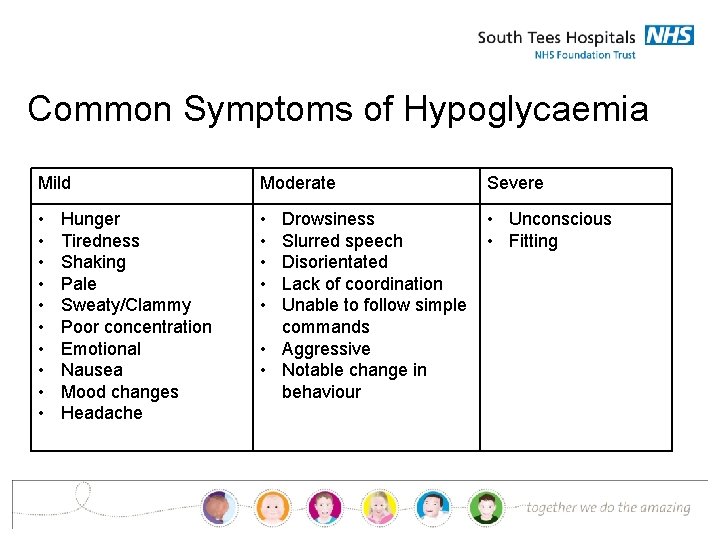
Common Symptoms of Hypoglycaemia Mild Moderate Severe • • • • Unconscious • Fitting Hunger Tiredness Shaking Pale Sweaty/Clammy Poor concentration Emotional Nausea Mood changes Headache Drowsiness Slurred speech Disorientated Lack of coordination Unable to follow simple commands • Aggressive • Notable change in behaviour
Treating a hypo It is very important to treat a hypo quickly If it is left untreated, the blood glucose level will continue to fall and the child could become unconscious THE CHILD SHOULD NOT BE LEFT ALONE – NOR BE SENT OFF TO GET FOOD TO TREAT IT BY THEMSELVES
What to do: Immediately : give approximately 10 grams of something sugary to eat or drink – e. g. 60 ml Lucozade, 100 ml full-sugar coke or 3 glucose tablets If the child is too drowsy to take anything themselves, massage Glucogel into the inside of their cheek Check blood glucose again 15 minutes later
Once blood glucose is above 4 mmol/l and young person is on MDI: Give 10 grams of starchy food i. e; - • 1 Digestive biscuit, • 2 Rich Tea biscuits • A piece of fruit To prevent the blood glucose from dropping again. • If about to have lunch this is not required and insulin should be given for the carbohydrates within the meal.
Once blood glucose is above 4 mmol/l and young person is on Insulin Pump: • Consider giving 10 grams of starchy carbohydrate (depending on activity level) • If about to have lunch this is not required and insulin should be given for the carbohydrates within the meal.
IF THE CHILD IS UNCONSCIOUS • DO NOT GIVE THEM ANYTHING ORALLY • LAY THEM ON THEIR SIDE IN THE RECOVERY POSITION • IF ON INSULIN PUMP DISCONNECT PUMP • PHONE 999 FOR AN AMBULANCE • INFORM PARENTS
Hyperglycaemia When blood glucose is consistently above 14 mmol/l, possible causes: • Not enough insulin • Too much carbohydrate • Missed insulin dose • Less exercise than usual • Stress • Puberty • Illness/Infection
• High glucose levels may cause the child to be thirsty and need to go to the toilet more often. • If levels are consistently high please inform their parents who can adjust their insulin appropriately • Please contact the diabetes team if you have any concerns
Common Symptoms of Hyperglycaemia • • • Excessive Thirst Frequent trips to the toilet Tiredness/Lethargy Mood changes Aggressive, boisterous behaviour
Severe Symptoms of Hyperglycaemia • • Headache Severe tummy ache Nausea Vomiting Drowsiness Rapid breathing Ketones 1. 5 mmol/l and above
What to do • Check child has washed and dried hands thoroughly and repeat test • Check when insulin was last given • If more than 2 hrs since last bolus give correction dose as advised by the meter • Check for ketones if on an insulin pump or if unwell • Repeat blood glucose in 2 hrs and if still above 14 mmol/l contact parents for advice • Encourage to drink water
High Blood Glucose + Ketones + feeling Unwell = DANGER • Phone 999 and contact parents
Illness: • If the child is very unwell they are unlikely to be in school • However if they have a mild illness such as cough or cold they may still attend • Please be aware illness may cause blood glucose to be elevated • Encourage fluids and regular BG monitoring • Contact parents if concerned
Physical activity Does the young person check regularly before P. E? Do they act upon their reading? Low OR high? ? If blood glucose is above 14 mmol/l and they have ketones they should not exercise.
School trips: Day trips should not cause any real problem as the routine will be much the same as a normal school day Necessary equipment, insulin and extra starchy food should be taken along in case of any delays as well as emergency hypo supplies Extra support can be given to school if holidays are planned.
Care Plans • All children and young people should have a care plan in school. • This needs to be reviewed annually by a designated person within school. • All schools should have diabetes related literature to support staff education. • Do all children/YP in school have a care plan? • Who is your dedicated person? • Does your dedicated person know how to contact us for support?
Diabetes is EVERYONE’S responsibility. However, if you need support Tel: 01642 854660 JCUH 01609 763718 FHN (Tues/Thurs)
Check out our new “children’s diabetes website” http: //southtees. nhs. uk/services/paediatric-diabetes/ Lots of useful information on managing diabetes Accu-chek School Information Infopad https: //kids. accu-chek. co. uk/documents/School_Info. Pad. pdf
Thank you Any questions?