Care of Tracheostomy Tube Prepared by IMRAN IQBAL
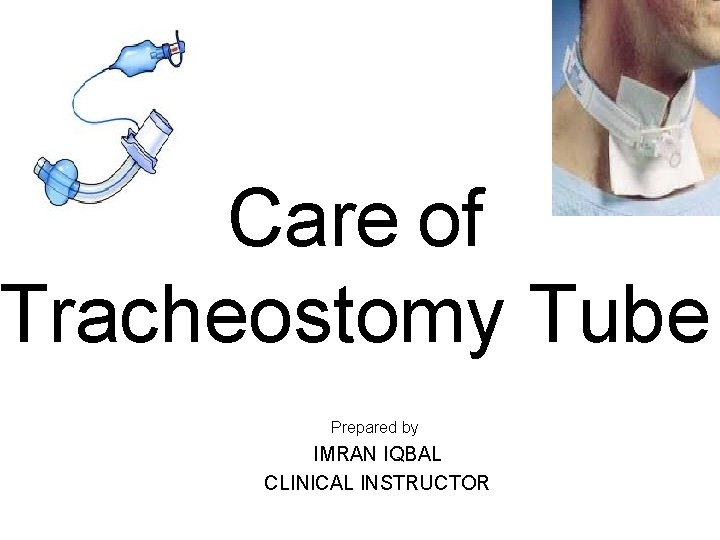
Care of Tracheostomy Tube Prepared by IMRAN IQBAL CLINICAL INSTRUCTOR
OBJECTIVES q Review of Evidenced-Based Guidelines in the Care & Maintenance q Review Definition, Types of Tracheostomies & their uses q Potential Complications q Nursing Care Guidelines Ø Assessment. Ø Suctioning. Ø Dressing changes Ø Inner cannula changes. Ø Other nursing considerations Ø Documentation
OBJECTIVES q Review of Evidenced-Based Guidelines in the Care & Maintenance q Review Definition, Types of Tracheostomies & their uses q Potential Complications q Nursing Care Guidelines Ø Assessment. Ø Suctioning. Ø Dressing changes Ø Inner cannula changes. Ø Other nursing considerations. Ø Documentation
DEFINITIONS q Tracheotomy: Incision made below the cricoid cartilage through the 2 nd -4 th tracheal rings q Tracheostomy: the opening or stoma made by this incision q Tracheostomy Tube: Artificial airway inserted into trachea
INDICATIONS q. To maintain a patent airway when the ability to do this is temporarily or permanently compromised q Bypass Obstructed airway • • • Tumor Laryngeal edema Foreign body obstruction q Facilitate removal of secretions q Permit long-term ventilation/prevent aspiration with prolonged coma q Decrease work of breathing---severe COPD
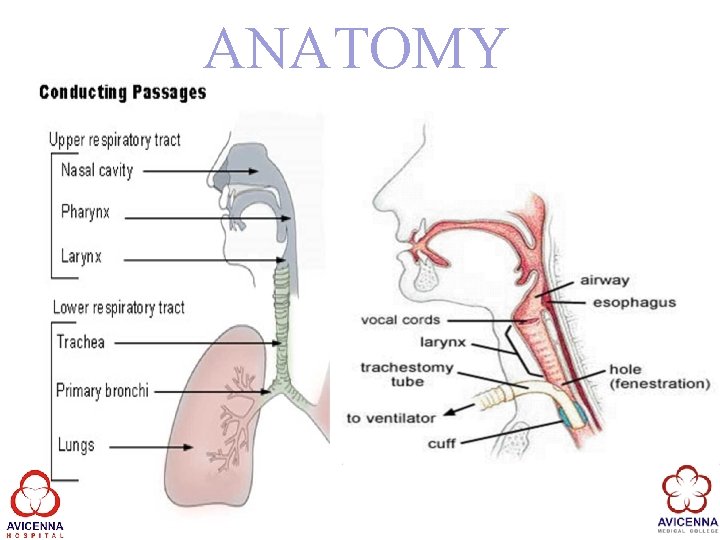
ANATOMY
TYPES OF TRACHEOSTOMY q Cuffed or Un-cuffed q Fenestrated or Non-fenestrated q Disposable or Non-disposable inner cannula.

PARTS OF TRACHEOSTOMY q 1. Flange- secured with trach ties, stabilizes the trach q 2. Outer Cannula-tube connected to flange q 3. Inner Cannula- removable for cleaning q 4. Obturator-a plastic guide with a smooth rounded tip that is used to guide the outer cannula during insertion q 5. Cuff-Soft balloon around the end of the trach that can be inflated to allow for mechanical ventilation

CUFFED TUBES Purpose: q Increase or improve ventilation/oxygenation q Prevent aspiration with feeding tubes, decreased gag reflex, gastro-esophageal reflux Cuff Complications: q Pressure from the cuff can cause damage the trachea q Necrosis To inflate/deflate and monitor pressure
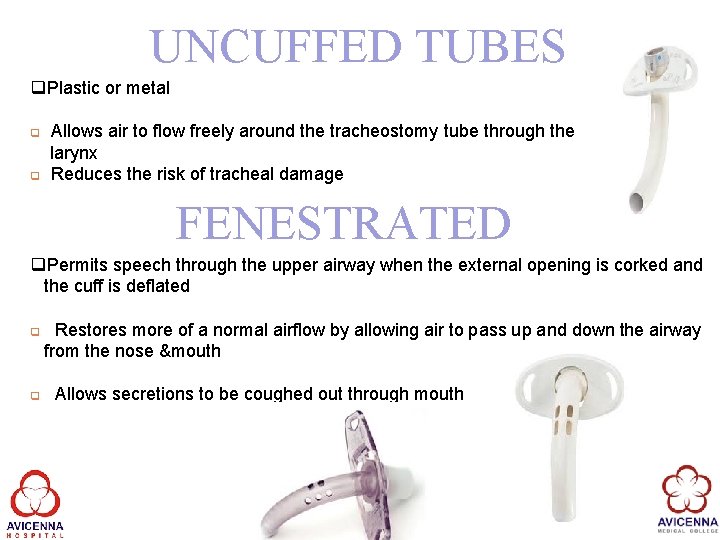
UNCUFFED TUBES q. Plastic or metal q q Allows air to flow freely around the tracheostomy tube through the larynx Reduces the risk of tracheal damage FENESTRATED q. Permits speech through the upper airway when the external opening is corked and the cuff is deflated q q Restores more of a normal airflow by allowing air to pass up and down the airway from the nose &mouth Allows secretions to be coughed out through mouth
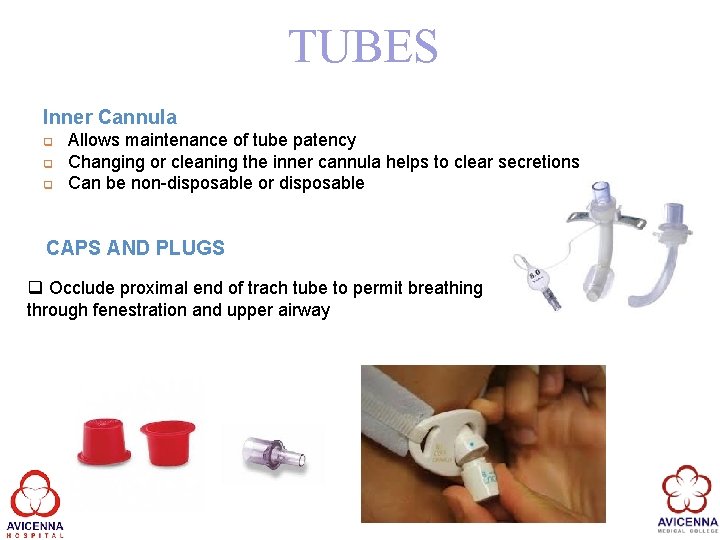
TUBES Inner Cannula q q q Allows maintenance of tube patency Changing or cleaning the inner cannula helps to clear secretions Can be non-disposable or disposable CAPS AND PLUGS q Occlude proximal end of trach tube to permit breathing through fenestration and upper airway
COMPLICATIONS Potential Complications § Hemorrhage § Pneumothorax § Subcutaneous emphysema § Dislodged tube § Airway obstructions § Infection § Aspiration § Tracheal damage
OBSTRUCTION Obstruction § Clinical Presentation: § Skin color— pallor, cyanotic § Increase respiratory rate, Pulse, BP, Decreased O 2 Sat § Use of accessory muscles, flared nostrils, inability to lie flat § Labored breathing § Clammy appearance/cyanosis § Decreased LOC or changes to behavior (i. e. )Distress/anxiety/restlessness
PREVENTION IS THE KEY q. Trach patients are at high risk for airway obstructions, impaired ventilation, and infection as well as other complications q. Altered body image, requiring emotional/psychological support q. Skilled and timely nursing assessment and care can prevent these complications Goals in care will include maintaining a patent airway as well as ventilation/oxygenation: q Suctioning q Humidity q Trach care & maintenance
NURSING ASSESSMENT q. Tracheostomy assessment to be done every 2 hourly/PRN q. Look and listen q. Vital signs & Sp. O 2 – pulse oximetry q. Oxygen/Humidity q. Respiratory assessment breath sounds q. Secretions- amount, color, consistency q. Cough, ability to clear own secretions q. Trach site
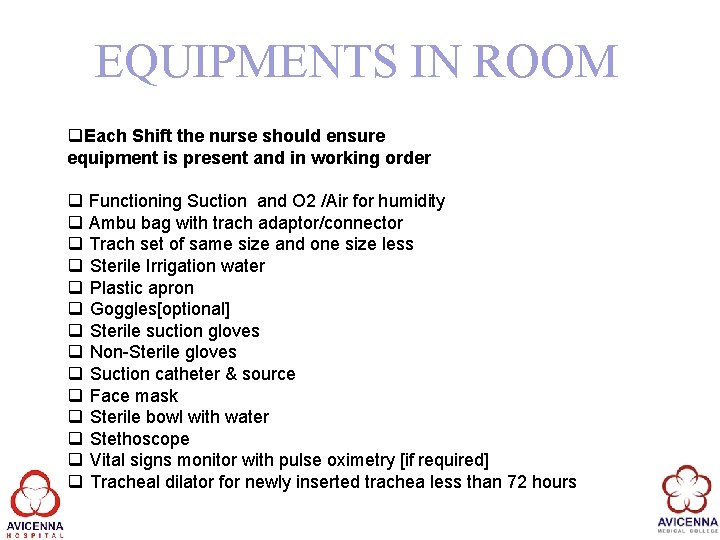
EQUIPMENTS IN ROOM q. Each Shift the nurse should ensure equipment is present and in working order q Functioning Suction and O 2 /Air for humidity q Ambu bag with trach adaptor/connector q Trach set of same size and one size less q Sterile Irrigation water q Plastic apron q Goggles[optional] q Sterile suction gloves q Non-Sterile gloves q Suction catheter & source q Face mask q Sterile bowl with water q Stethoscope q Vital signs monitor with pulse oximetry [if required] q Tracheal dilator for newly inserted trachea less than 72 hours
CHANGING/CLEANING INNER CANNULA q Tracheostomy tubes removable inner cannula will be cleaned /changed at least once a day/PRN q White inner cannula will be insitu while suctioning and eating q The red inner cannula insitu while speaking Cleaning : q Clean inner cannula with sterile water and dry with sterile gauze Trach ties-are changed only when wet or soiled and once a day, two people should assist with this procedure
SUCTIONING OF TRACHEOSTOMY TUBE
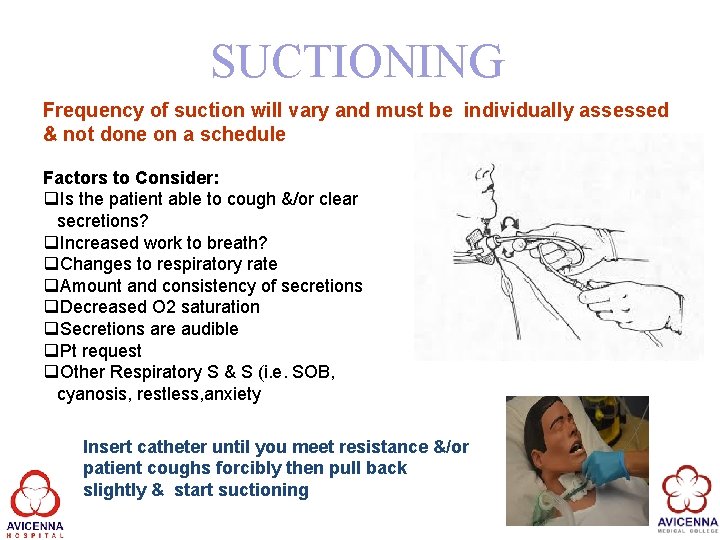
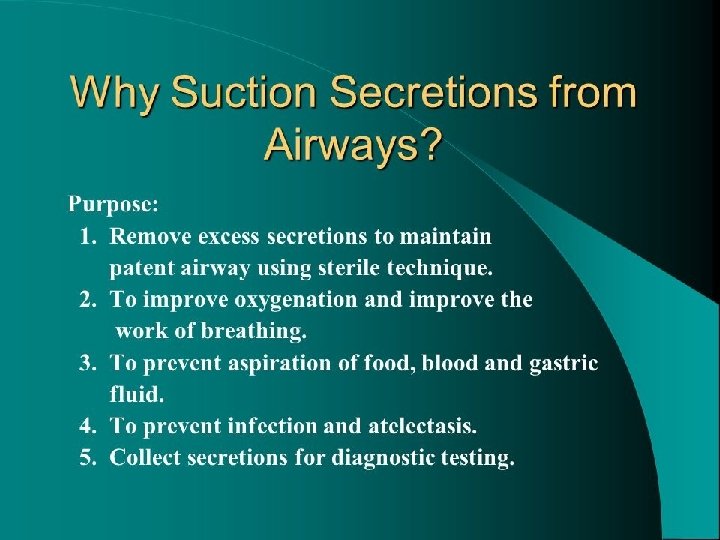
SUCTIONING Frequency of suction will vary and must be individually assessed & not done on a schedule Factors to Consider: q. Is the patient able to cough &/or clear secretions? q. Increased work to breath? q. Changes to respiratory rate q. Amount and consistency of secretions q. Decreased O 2 saturation q. Secretions are audible q. Pt request q. Other Respiratory S & S (i. e. SOB, cyanosis, restless, anxiety Insert catheter until you meet resistance &/or patient coughs forcibly then pull back slightly & start suctioning
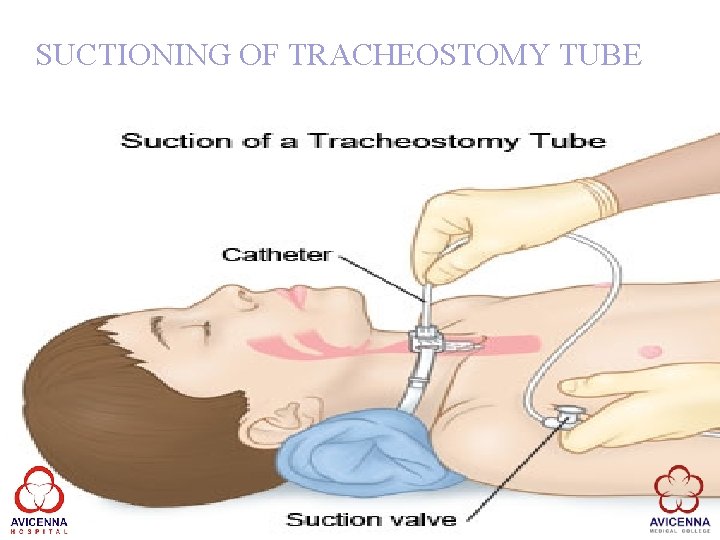
SUCTIONING OF TRACHEOSTOMY TUBE
![COMPLICATIONS WITH SUCTIONING q Hypoxemia [_Sp. O 2, _RR] q Hypoxia [Cyanosis, respiratory distress] COMPLICATIONS WITH SUCTIONING q Hypoxemia [_Sp. O 2, _RR] q Hypoxia [Cyanosis, respiratory distress]](http://slidetodoc.com/presentation_image_h2/60ef8e21ef57e39a61192a1c294cd7ea/image-21.jpg)
COMPLICATIONS WITH SUCTIONING q Hypoxemia [_Sp. O 2, _RR] q Hypoxia [Cyanosis, respiratory distress] q Tachycardia and hypertension [Due to hypoxemia] q Bradycardia and hypotension[Due to stimulation of the vagus nerve] q Increased intracranial pressure [Due to hypertension] q Bleeding [Due to trauma to the tracheal and/or bronchial mucosa] q Cardiac Arrhythmias q Bronchospasm q Infection q Pain
SUCTIONING TIME q Continue suctioning the patient until the airway is clear of secretions. No more than four [4] suction attempts should be made per suction episode. q It is recommended that the episode of suctioning (including passing the catheter and suctioning the tracheostomy tube) is completed within 5 -10 seconds
HUMIDIFICATION q. Unless otherwise ordered all patients with a tracheostomy who requires oxygen must have humidification applied. q. Humidification is applied through a thermal humidifier. e. g. Thermovent

COMMUNICATION Alteration in communication q. Lip reading q. Communication Board q. Corking for speech

- Slides: 25