CARE OF THE OLDER ADULT CHARISSE REED MSN
- Slides: 58
CARE OF THE OLDER ADULT CHARISSE REED, MSN, RN
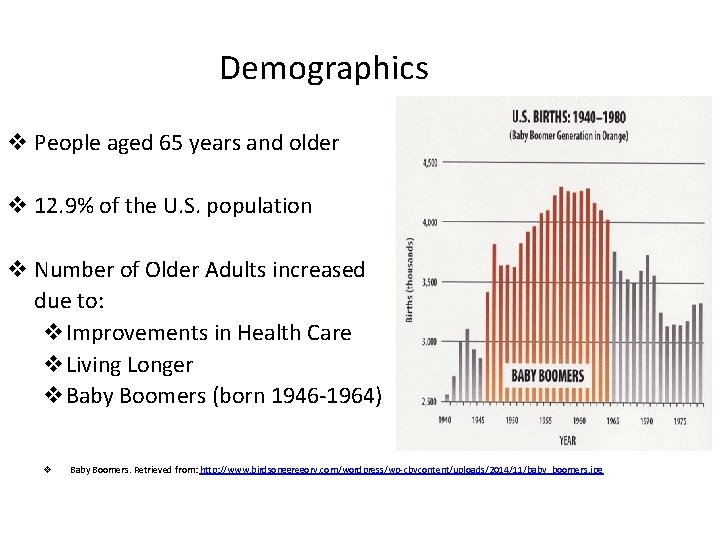
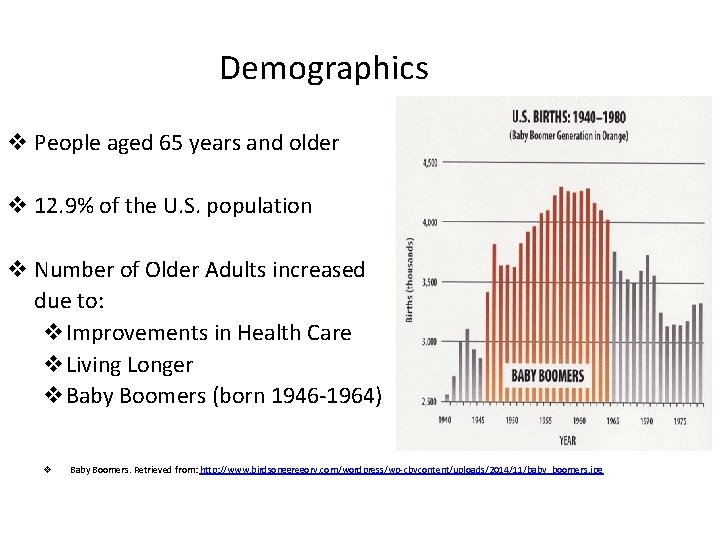
Demographics v People aged 65 years and older v 12. 9% of the U. S. population v Number of Older Adults increased due to: v. Improvements in Health Care v. Living Longer v. Baby Boomers (born 1946 -1964) v Baby Boomers. Retrieved from: http: //www. birdsonggregory. com/wordpress/wp-cbycontent/uploads/2014/11/baby_boomers. jpg
COMMON MYTHS & STEREOTYPES • Older adults are ill, disabled, physically unattractive, and not interested in sex • They are forgetful and unable to understand learn new information • Older adults live below the poverty level & are institutionalized • Myths & stereotypes lead to the undervaluing of older adults
Developmental Tasks • According to Erickson- “Ego Integrity vs Despair” • Older adults often engage in a retrospective appraisal of their lives and see it as a meaningful whole or experience regret of goals not achieved • No two individuals age in the same way
Developmental Tasks (con’t) • Adaptation & adjustment can be easy for some but other need the assistance of family, friends, and health care professionals • Nurses should be sensitive to the effect a loss can have on an older adult and offer support
Physiological Changes • Skin- Integumentary System 1. Thinning of all 3 layers of the skin 2. Drier skin because the decreased number of sebaceous glands results in reduced oil production 3. Less efficient thermoregulation of heat because of fewer sweat glands 4. Reduced sensory input, decreased elasticity
Physiological Changes (con’t) • Interventions for skin-integumentary system 1. Avoid excessive use of soap 2. Skin evaluation & lubrication are necessary to prevent breakdown 3. Avoid direct application of extreme heat & cold 4. Avoid extreme temperatures, proper clothing, etc. 5. Proper positioning and prevention of pressure ulcers
Physiological Changes (con’t) • Head and Neck 1. Facial features appear asymmetrical because of missing teeth or improper fitting dentures 2. Visual acuity decrease with age 3. Presbyopia (farsightedness) due to decreased visual accommodation from loss of lens elasticity 4. Decreased color discrimination, blues & greens hard to see (due to yellowing of the lens) 5. Decreased tears
Physiological Changes • Head & neck (Con’t) 6. More light is needed for reading 7. Hearing loss is often compensated by increasing TV and radio volumes 8. Hearing loss is a combined problem. Majority of loss due to auditory nerve changes or deterioration of the structures of the ear. 9. Taste buds and sense of smell decreases
Physiological Changes (con’t) • Interventions for head & neck 1. Encourage eye exams 2. Encourage the use of hearing aids, if they have them 3. Eliminate unnecessary background noise 4. Face the older client & speak in a clear, low tone. Do not yell. 5. Use short simple sentences
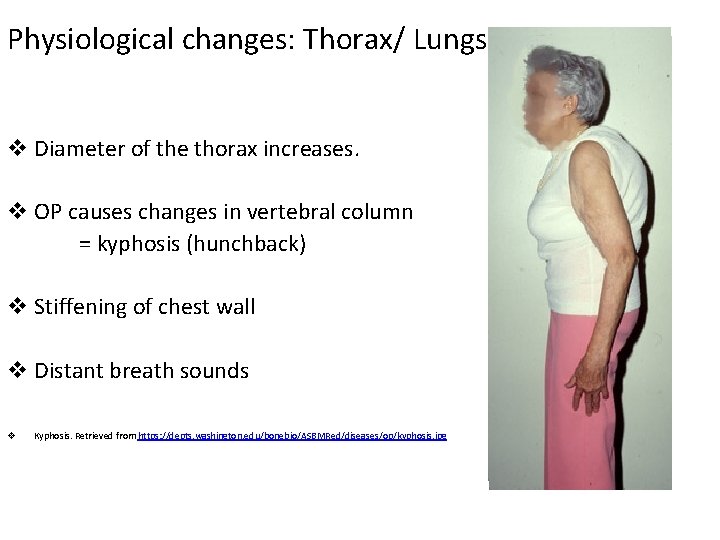
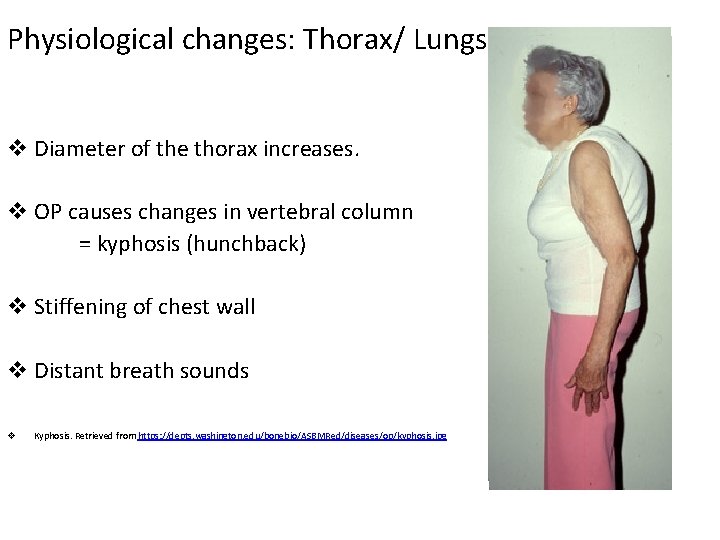
Physiological changes: Thorax/ Lungs v Diameter of the thorax increases. v OP causes changes in vertebral column = kyphosis (hunchback) v Stiffening of chest wall v Distant breath sounds v Kyphosis. Retrieved from https: //depts. washington. edu/bonebio/ASBMRed/diseases/op/kyphosis. jpg
Interventions for thorax/lungs v Turn patients Q 2 H - Decreases secretion build-up. v Elevate the HOB to 30 degrees -promotes drainage of secretions. v Assess breath sounds and O 2 Saturation. v Give O 2 at 2 L BNC as ordered to promote oxygenation. v Elevated HOB. Retrieved from http: //emupdates. com/wp-content/uploads/2011/08/credit-http___goo. gl_yn 2 pq. jpg
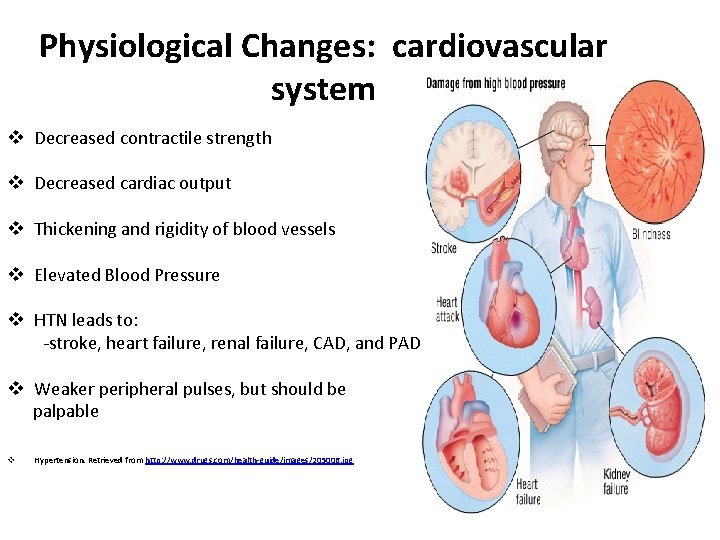
Physiological Changes: cardiovascular system v Decreased contractile strength v Decreased cardiac output v Thickening and rigidity of blood vessels v Elevated Blood Pressure v HTN leads to: -stroke, heart failure, renal failure, CAD, and PAD. v Weaker peripheral pulses, but should be palpable v Hypertension. Retrieved from http: //www. drugs. com/health-guide/images/205006. jpg
Interventions : cardiovascular system v Minimize physical exertion, anxiety, and prolonged inactivity v Protect from decreases in circulation. v Protect feet from injury and provide foot care. v Assess BP; monitor for orthostatic hypotension -(fall prevention) v Instruct patients to change positions slowly. v Orthostatic hypotension. Retrieved from hypotensionclinic. blogspot. com
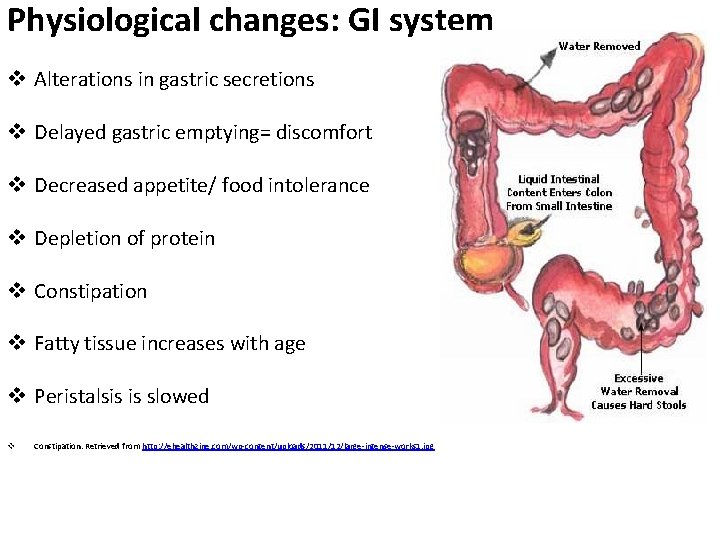
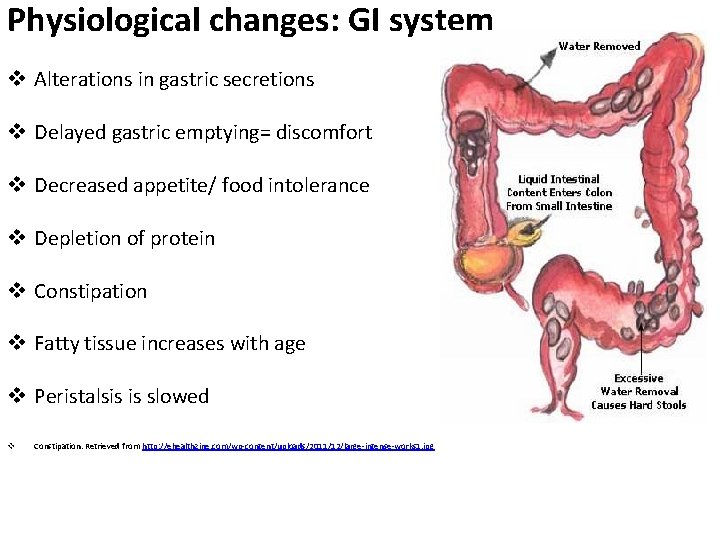
Physiological changes: GI system v Alterations in gastric secretions v Delayed gastric emptying= discomfort v Decreased appetite/ food intolerance v Depletion of protein v Constipation v Fatty tissue increases with age v Peristalsis is slowed v Constipation. Retrieved from http: //ehealthzine. com/wp-content/uploads/2011/12/large-intense-works 1. jpg
Interventions: GI System v Encourage regular exercise/ mobility v Appropriate fiber intake v Do not ignore urges to defecate. v Nutritional assessment with patient specific interventions v Encourage po fluids, especially water v v High fiber diet. Retrieved from www. healthtap. com Hydration. Retrieved from http: //www. easyhealthtips. org/wp-content/uploads/2014/07/man-drinking-water. jpg
Physiological Changes (con’t) • Reproductive System 1. Structural & functional changes occur as a result of hormonal alterations 2. In women, menopause leads to decreases in the size of the ovaries, and hormone production. This results in uterine involution, vaginal atrophy, & loss of breast mass 3. In men, testosterone production & secretion decrease with age and sperm count. Cessation of fertility is not definite with aging.
Physiological Changes (con’t) • Interventions for reproductive system 1. Refer to physician for hormonal replacements and prescription meds
Physiological Changes (con’t) • Urinary System 1. Hypertrophy of the prostate develops in men causing urinary retention, frequency, incontinence and UTI’s. 2. Decreased muscle tone contributes to incontinence & incomplete emptying of the bladder 3. Bladder capacity decreases
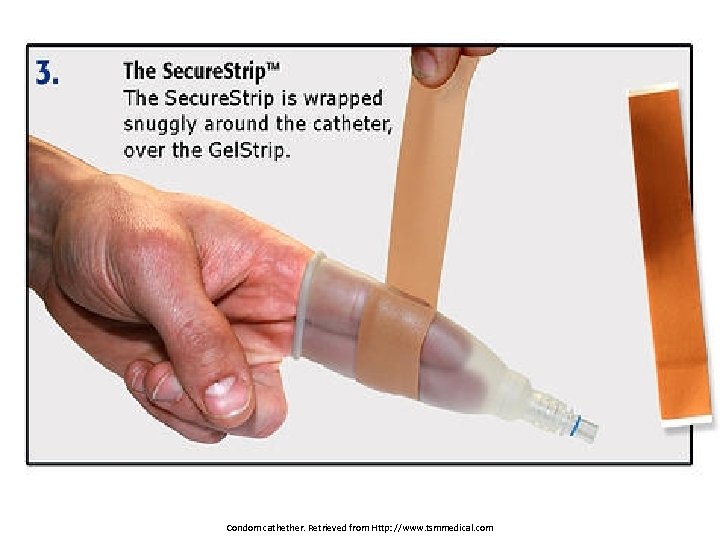
Interventions: Urinary System v Assist older adults to toilet to immediately when they ask to void. v Monitor and record accurate I & O. v Developing a voiding schedule may help. v Bladder training v Use of external catheters, medications, protective pants v v Bedside Commode. Retrieved from http: //www. galaxymedical. net/images/bedside-commode. jpg Incontinence briefs. Retrieved from http: //www. biorelief. com/media/catalog/product/cache/1/thumbnail/9 df 78 eab 33525 d 08 d 6 e 5 fb 8 d 27136 e 95/a/t/attends_shaped_front. jpg
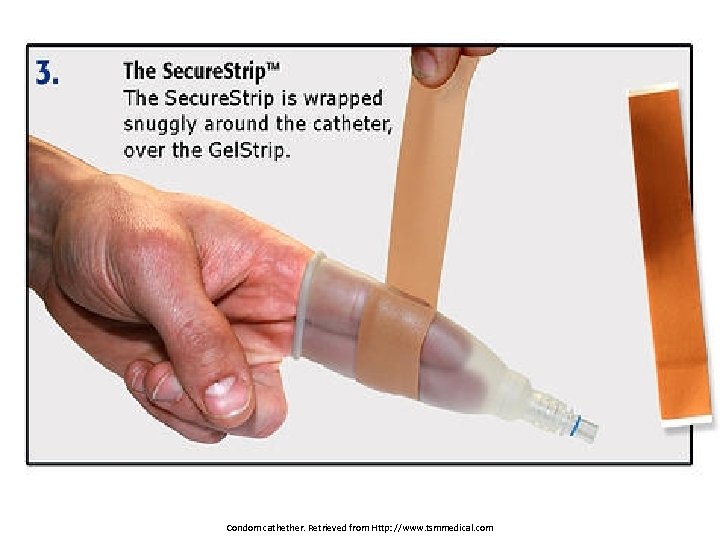
Condom cathether. Retrieved from Http: //www. tsmmedical. com
Physiological Changes: Musculoskeletal System 1. Decrease in muscle tone and strength with age 2. Decrease bone density, less so in men than women 3. Osteoporosis major threat to older adults 4. Arthritis, gait and balance disorders 5. Impairments: hemiparesis, ataxia, spasticity, coordination or balance problems
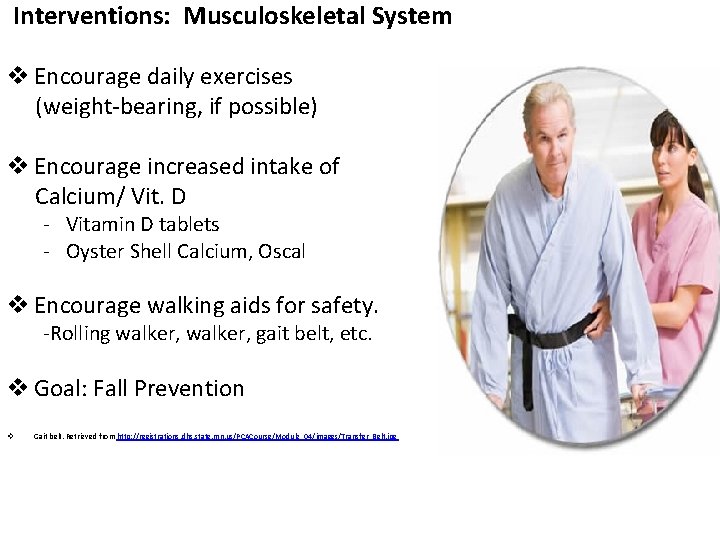
Interventions: Musculoskeletal System v Encourage daily exercises (weight-bearing, if possible) v Encourage increased intake of Calcium/ Vit. D - Vitamin D tablets - Oyster Shell Calcium, Oscal v Encourage walking aids for safety. -Rolling walker, gait belt, etc. v Goal: Fall Prevention v Gait belt. Retrieved from http: //registrations. dhs. state. mn. us/PCACourse/Module_04/images/Transfer_Belt. jpg
Physiological Changes: Neurological System 1. Gradual loss in the number of neurons with age, but no major change in neurotransmitter levels 2. All voluntary reflexes are slower Interventions: Neurological System 1. Adapt to their pace 2. Allow more time to complete task, eating, bathing, dressing, learning a new skill
Psychosocial changes: cognition v Cognitive Changes include: -Disorientation -Poor Judgment -Loss of Language Skills -These symptoms are NOT normal v 3 Common Conditions That Affect Cognition - Delirium - Dementia - Depression. Retrieved from http: //blogs. psychcentral. com/depression/files/2012/04/depressedsenior_cr pd. jpg
Cognitive changes: Delirium v State that causes confusion: -Acute (reversible) -Chronic (irreversible) v Causes: - Hypoglycemia Medications Electrolyte imbalances Tumors Infections Cerebral Anoxia v Onset of delirium requires prompt assessment and intervention v Confusion. Retrieved from http: //feedyoursoul. com/wp-content/uploads/2014/08/confused. jpg
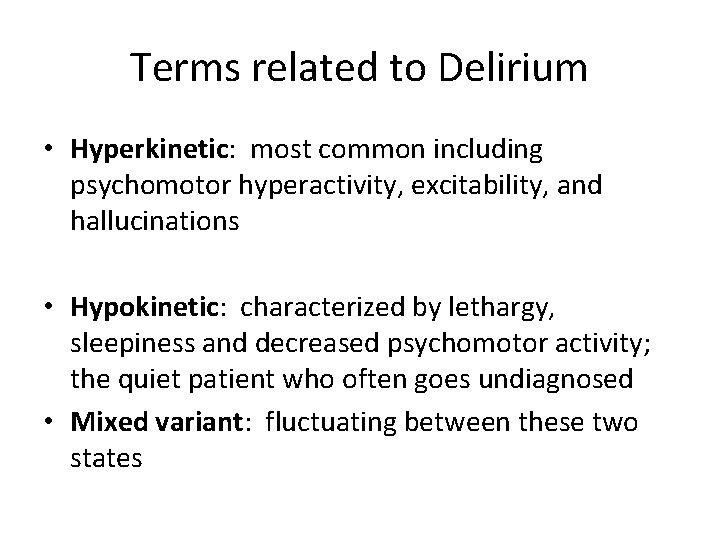
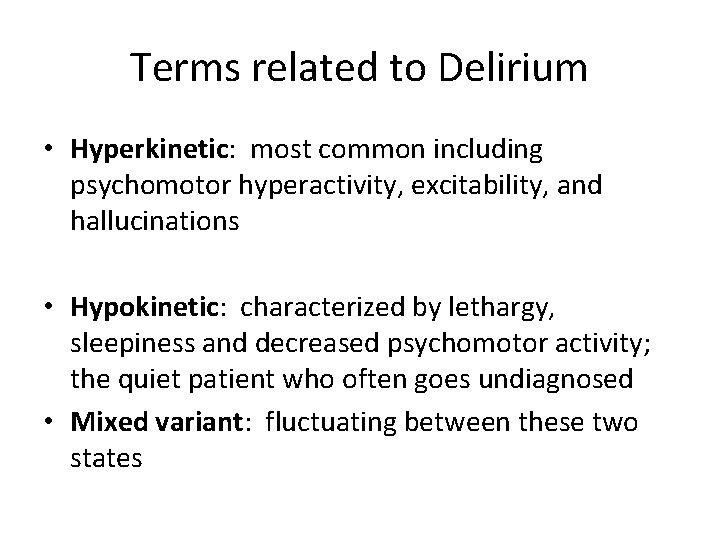
Terms related to Delirium • Hyperkinetic: most common including psychomotor hyperactivity, excitability, and hallucinations • Hypokinetic: characterized by lethargy, sleepiness and decreased psychomotor activity; the quiet patient who often goes undiagnosed • Mixed variant: fluctuating between these two states
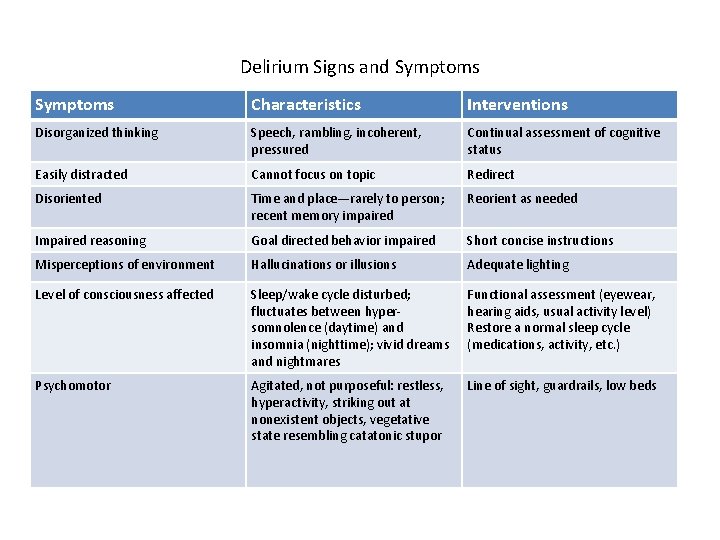
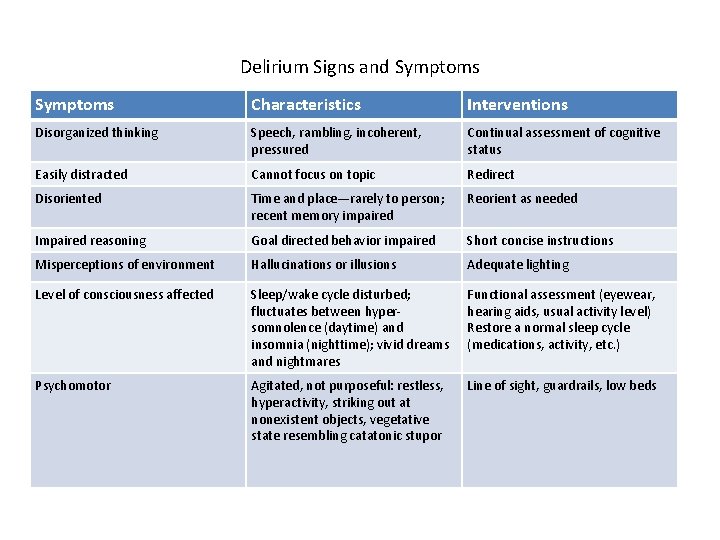
Delirium Signs and Symptoms Characteristics Interventions Disorganized thinking Speech, rambling, incoherent, pressured Continual assessment of cognitive status Easily distracted Cannot focus on topic Redirect Disoriented Time and place—rarely to person; recent memory impaired Reorient as needed Impaired reasoning Goal directed behavior impaired Short concise instructions Misperceptions of environment Hallucinations or illusions Adequate lighting Level of consciousness affected Sleep/wake cycle disturbed; fluctuates between hypersomnolence (daytime) and insomnia (nighttime); vivid dreams and nightmares Functional assessment (eyewear, hearing aids, usual activity level) Restore a normal sleep cycle (medications, activity, etc. ) Psychomotor Agitated, not purposeful: restless, hyperactivity, striking out at nonexistent objects, vegetative state resembling catatonic stupor Line of sight, guardrails, low beds
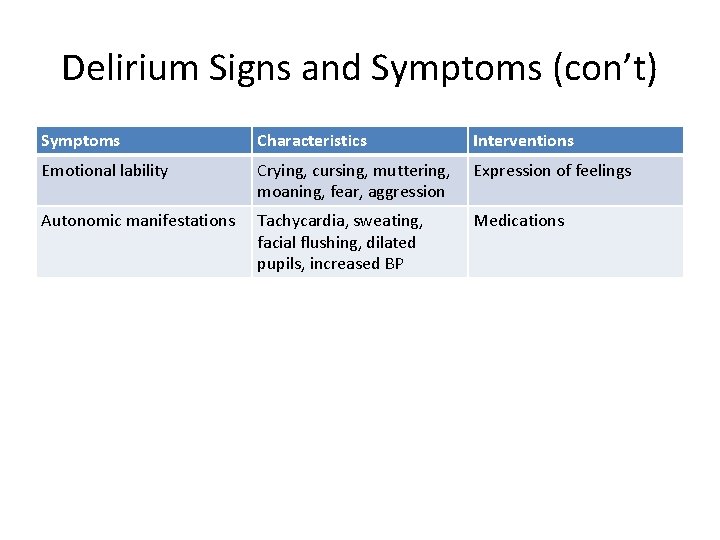
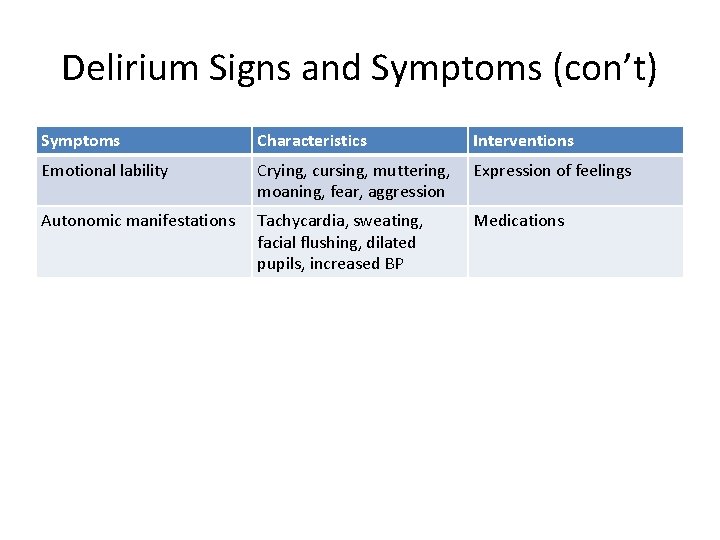
Delirium Signs and Symptoms (con’t) Symptoms Characteristics Interventions Emotional lability Crying, cursing, muttering, moaning, fear, aggression Expression of feelings Autonomic manifestations Tachycardia, sweating, facial flushing, dilated pupils, increased BP Medications
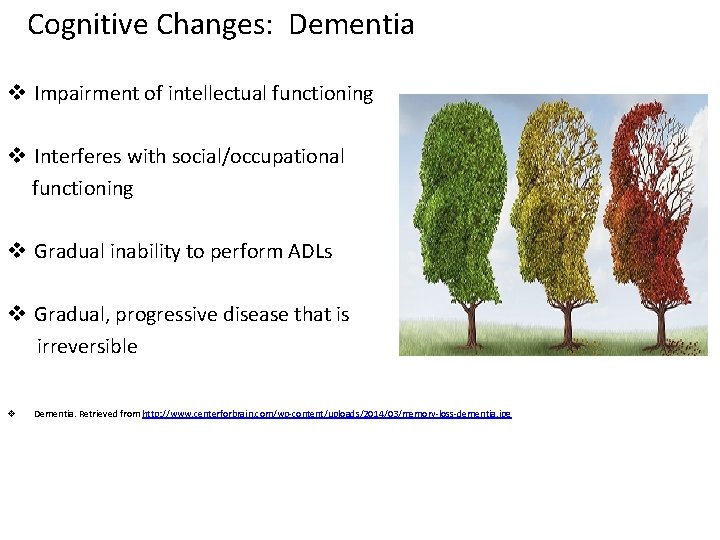
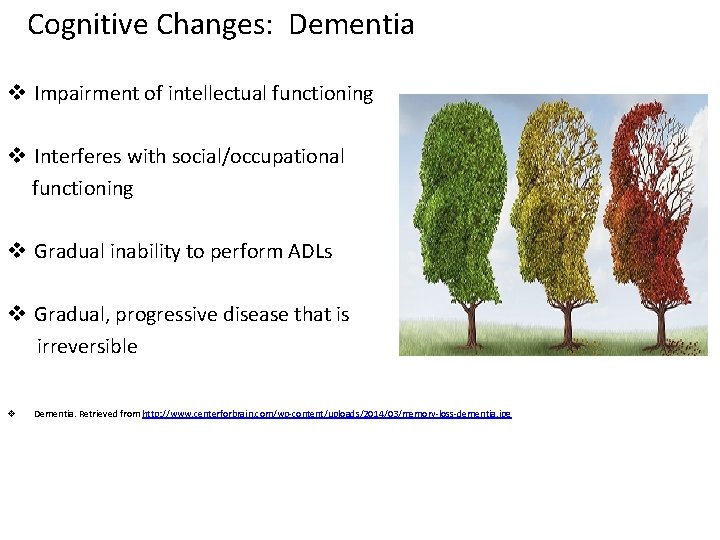
Cognitive Changes: Dementia v Impairment of intellectual functioning v Interferes with social/occupational functioning v Gradual inability to perform ADLs v Gradual, progressive disease that is irreversible v Dementia. Retrieved from http: //www. centerforbrain. com/wp-content/uploads/2014/03/memory-loss-dementia. jpg
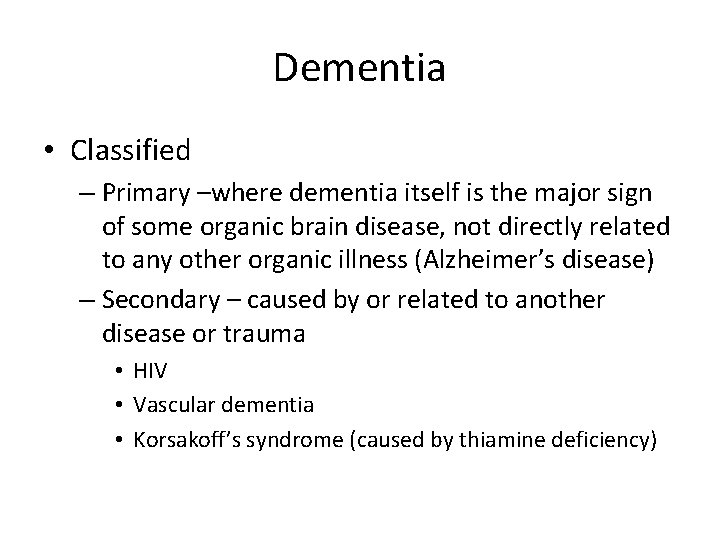
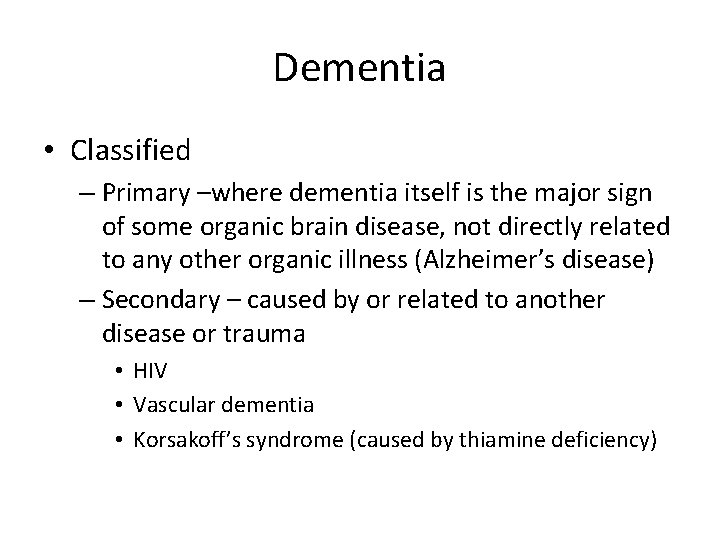
Dementia • Classified – Primary –where dementia itself is the major sign of some organic brain disease, not directly related to any other organic illness (Alzheimer’s disease) – Secondary – caused by or related to another disease or trauma • HIV • Vascular dementia • Korsakoff’s syndrome (caused by thiamine deficiency)
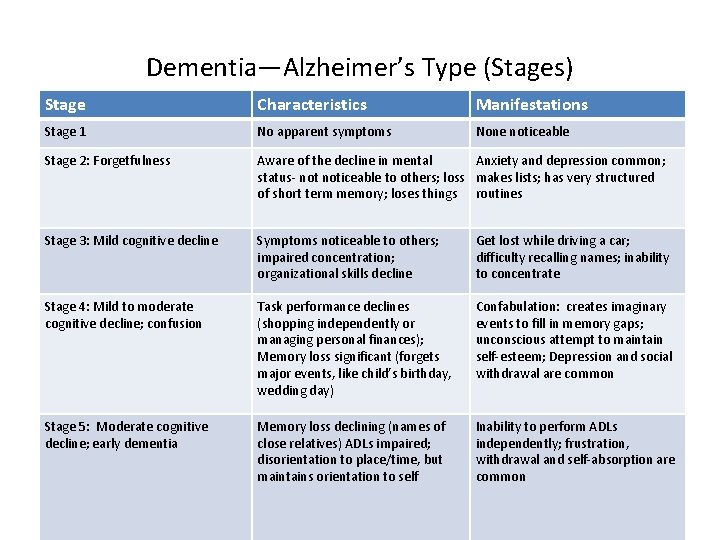
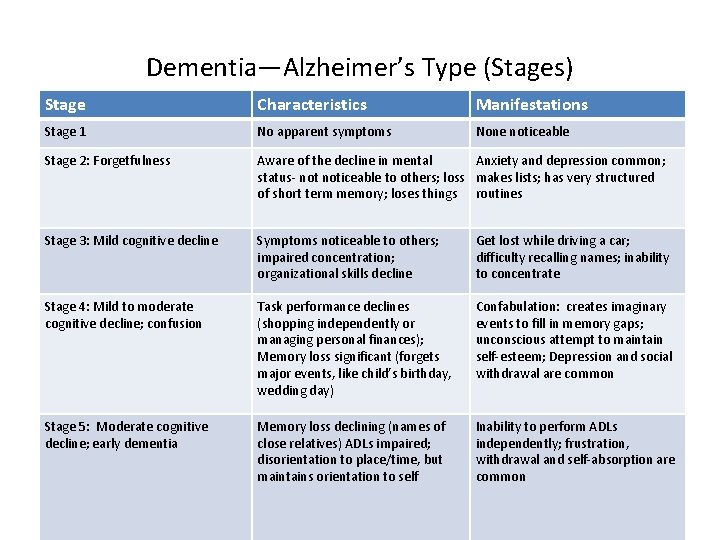
Dementia—Alzheimer’s Type (Stages) Stage Characteristics Manifestations Stage 1 No apparent symptoms None noticeable Stage 2: Forgetfulness Aware of the decline in mental Anxiety and depression common; status- noticeable to others; loss makes lists; has very structured of short term memory; loses things routines Stage 3: Mild cognitive decline Symptoms noticeable to others; impaired concentration; organizational skills decline Get lost while driving a car; difficulty recalling names; inability to concentrate Stage 4: Mild to moderate cognitive decline; confusion Task performance declines (shopping independently or managing personal finances); Memory loss significant (forgets major events, like child’s birthday, wedding day) Confabulation: creates imaginary events to fill in memory gaps; unconscious attempt to maintain self-esteem; Depression and social withdrawal are common Stage 5: Moderate cognitive decline; early dementia Memory loss declining (names of close relatives) ADLs impaired; disorientation to place/time, but maintains orientation to self Inability to perform ADLs independently; frustration, withdrawal and self-absorption are common
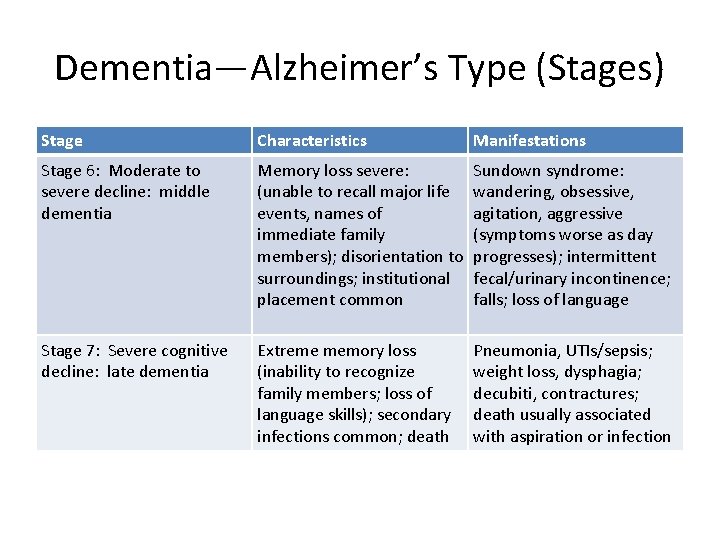
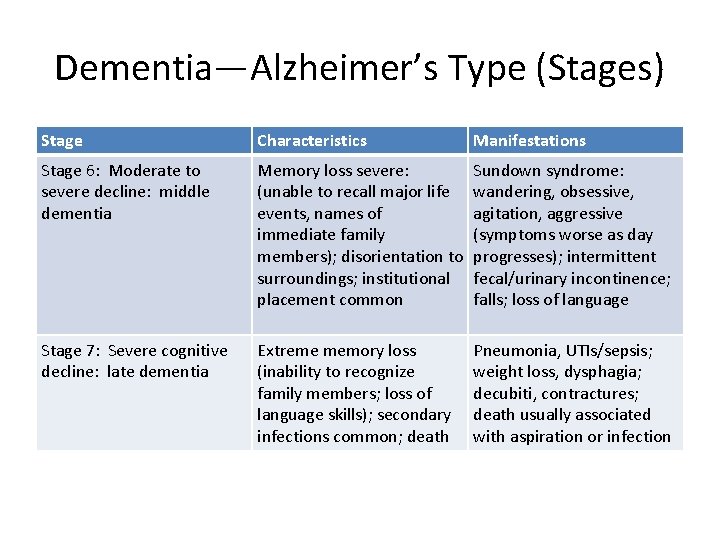
Dementia—Alzheimer’s Type (Stages) Stage Characteristics Manifestations Stage 6: Moderate to severe decline: middle dementia Memory loss severe: (unable to recall major life events, names of immediate family members); disorientation to surroundings; institutional placement common Sundown syndrome: wandering, obsessive, agitation, aggressive (symptoms worse as day progresses); intermittent fecal/urinary incontinence; falls; loss of language Stage 7: Severe cognitive decline: late dementia Extreme memory loss (inability to recognize family members; loss of language skills); secondary infections common; death Pneumonia, UTIs/sepsis; weight loss, dysphagia; decubiti, contractures; death usually associated with aspiration or infection
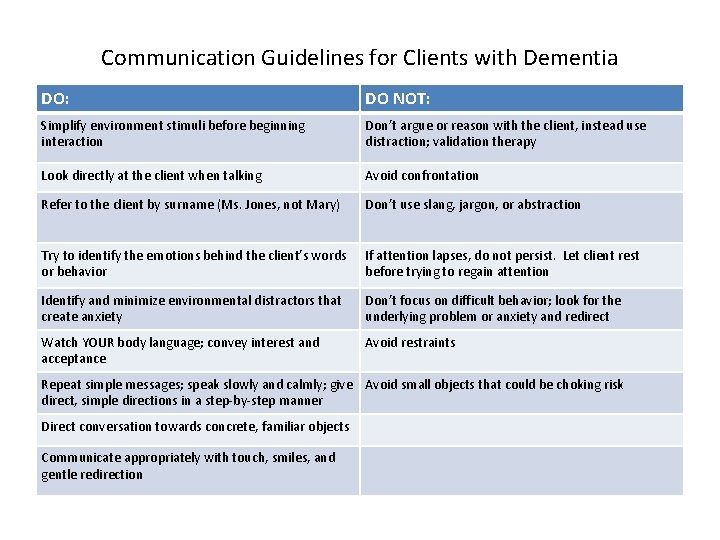
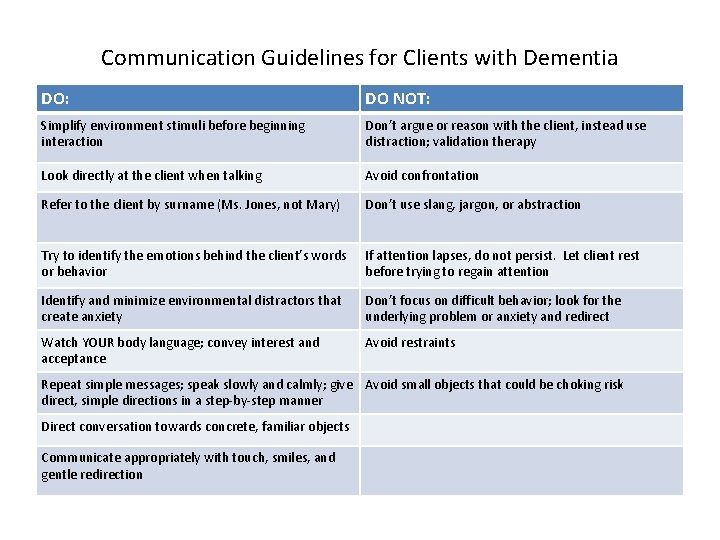
Communication Guidelines for Clients with Dementia DO: DO NOT: Simplify environment stimuli before beginning interaction Don’t argue or reason with the client, instead use distraction; validation therapy Look directly at the client when talking Avoid confrontation Refer to the client by surname (Ms. Jones, not Mary) Don’t use slang, jargon, or abstraction Try to identify the emotions behind the client’s words or behavior If attention lapses, do not persist. Let client rest before trying to regain attention Identify and minimize environmental distractors that create anxiety Don’t focus on difficult behavior; look for the underlying problem or anxiety and redirect Watch YOUR body language; convey interest and acceptance Avoid restraints Repeat simple messages; speak slowly and calmly; give Avoid small objects that could be choking risk direct, simple directions in a step-by-step manner Direct conversation towards concrete, familiar objects Communicate appropriately with touch, smiles, and gentle redirection
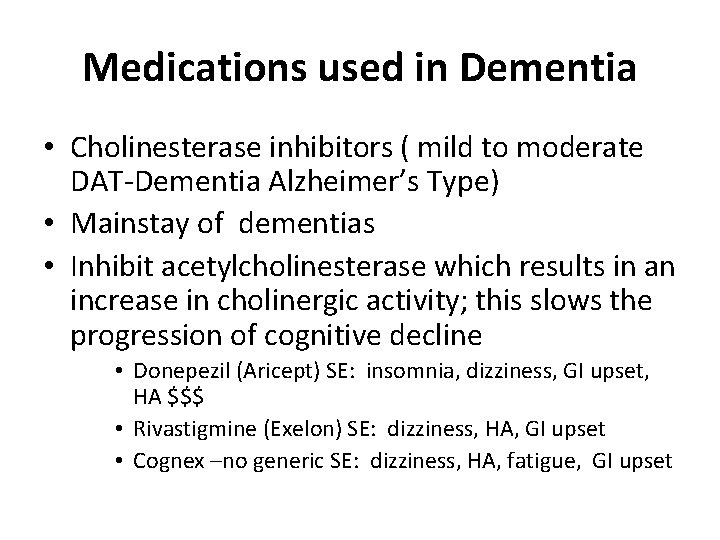
Medications used in Dementia • Cholinesterase inhibitors ( mild to moderate DAT-Dementia Alzheimer’s Type) • Mainstay of dementias • Inhibit acetylcholinesterase which results in an increase in cholinergic activity; this slows the progression of cognitive decline • Donepezil (Aricept) SE: insomnia, dizziness, GI upset, HA $$$ • Rivastigmine (Exelon) SE: dizziness, HA, GI upset • Cognex –no generic SE: dizziness, HA, fatigue, GI upset
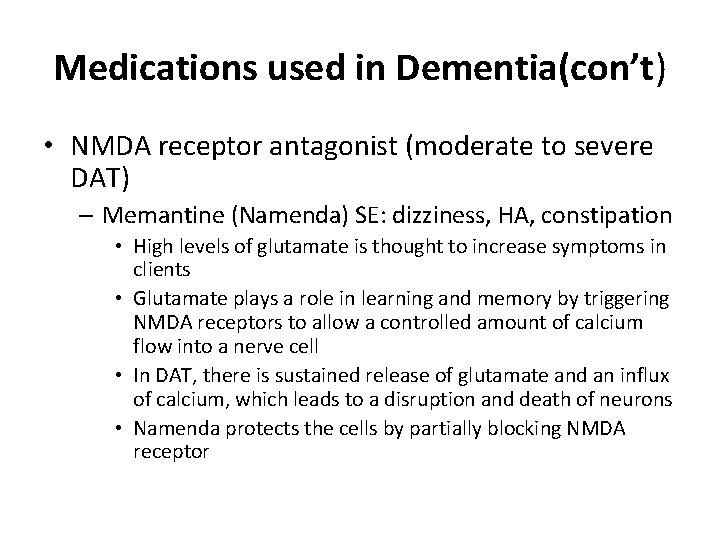
Medications used in Dementia(con’t) • NMDA receptor antagonist (moderate to severe DAT) – Memantine (Namenda) SE: dizziness, HA, constipation • High levels of glutamate is thought to increase symptoms in clients • Glutamate plays a role in learning and memory by triggering NMDA receptors to allow a controlled amount of calcium flow into a nerve cell • In DAT, there is sustained release of glutamate and an influx of calcium, which leads to a disruption and death of neurons • Namenda protects the cells by partially blocking NMDA receptor
Medications used in Dementia (con’t) • • Antipsychotics SSRIs (Selective Serotonin Reuptake Inhibitors) Anti-anxiety Sedative-hypnotic (benzodiazepine)
Outcomes for Dementia • Client: – No physical injury – No harm to self or others – Ability to communicate individual needs with consistent caregiver – Fulfills ADLs with assistance • Caregiver – Verbalized understanding of disease process • Realistic expression/expectation of disease process
Outcomes for Dementia • Caregiver (con’t) – Verbalizes management of the illness • • • Ensuring safety Maintaining orientation Nutritional information Difficult behaviors (aggression, wandering, pacing) Hygiene and toileting – Verbalizes available resources • Professional counseling • Home Health
Outcomes for Dementia • Caregiver (con’t) – Verbalizes available resources (con’t) • Respite Care • Referrals – – – Alzheimer’s Association http: //www. alz. org http: //nimh. gov/publicat/medicate. html http: //www. aarp. org Day care centers Legal/financial services
Psychological Changes (con’t) • Cognitive Changes (con’t) **Depression Reduce overall happiness & contibutes to physical & social limitations It complicates the treatment of other medical conditions & increases the risk of suicide Late life depression is not a normal part of aging Due to lifestyle transitions and loss
Psychosocial Changes (con’t) • Retirement 1. Causes stressors such as economic, relationship, and financial 2. Affect spouses, adult children, & grandchildren 3. Planning for retirement allows a smoother transition into retirement
Psychosocial Changes (con’t) • Social Isolation 1. The degree of social isolation increases with age 2. Isolation can be by choice or due to a response to a condition that inhibits the ability to interact with others. It may arise for attitudinal, presentational, behavioral, or geographical factors. 3. Attitudinal occurs due to personal or cultural values
Psychosocial Changes (con’t) • Social isolation(con’t) 4. Presentational results from a persons unacceptable appearance 5. Behavioral result for the persons unacceptable behaviors 6. Geographical occurs from institutional barriers, distance from family & friends, and environmental crime
Elder Abuse • 10 % over the age of 65 are victims to abuse or neglect • Often a relative who lives with the elderly person or may be an assigned caregiver • Types of abuse: Psychological, neglect, physical, financial, sexual
Contributing Factors to Elder Abuse • • Longer Life Dependency Stress Learned violence
Identifying & Recognizing Elder Abuse • • • Psychological Abuse Physical Abuse Neglect Sexual Abuse Financial Abuse
Elder Victims Response to Abuse • Often minimize/deny the abuse • Unwilling to disclose information – fear of retaliation • Protective toward a family member or unwilling to institute legal action due to fear of retaliation. • Often isolated so their mistreatment is less likely to be noticed by those who might be alert to symptoms of abuse.
Healthcare Workers • Responsibilities of the RN with Abuse – If there is suspicion of abuse/neglect – REPORT IT!!! – If you are uncertain, discuss with another coworker and STILL REPORT IT!!!! – If you feel intimidated when confronted with cases of elder abuse, refer to an individual who has experience in management (Unit Manager, Social Worker, etc. ) of such victims may be the MOST effective approach.
Nursing and Violence-Therapeutic Nursing Care • Explore one’s own attitude toward the survivor • Recognize attitudes and seek to change negative feelings • Gain experience through educational programs or volunteer in programs for survivors assistance
Psychosocial Changes (con’t) • Sexuality 1. Older adults should express sexual feelings 2. Sexuality plays a role in maintaining self-esteem 3. Physical changes & medications affect sexual functioning
Psychosocial Changes (con’t) • Housing and environmental 1. Changes may be necessary because of death of spouse, physical impairments, and health problems 2. Housing arrangement depend on activity level restrictions, financial status, and support systems
Psychosocial changes: Death v Older adults may experience death of spouse, children, friends, or family members. v Grieving Process: Kubler-Ross Stages of Dying -Denial, Anger, Bargaining, Depression, Acceptance v Nurses provide support to pt. v Help patients cope with losses. v Facilitate adjustment to life changes. v Holding Hands. Retrieved from https: //www. michaeljfox. org/files/blog/Patient-Doctor-Hands. jpg
Psychosocial Interventions v Therapeutic Communication is very important. v Must be genuinely concerned for welfare of pt v Never underestimate the power of touch: -Provides sensory stimulation -Provides comfort v Reality orientation v Refer to support groups/ community activities. v Encourage adaptive coping. (Social support, religious faith, counseling/therapy) v Discourage maladaptive coping. (use of alcohol/ drugs to deal with pain)
Sleep and rest v Deficient sleep hours can negatively effect the pt’s functioning in daytime hours. -Negatively effects health v Causes of Sleep Disturbances: -Medications (Beta-blockers, decongestants, anti-psychotics) - Sleep Apnea -Restless Leg Syndrome -Pain -Cardiac/ Pulmonary disorders
Pain Management v Older adults often suffer from Chronic Pain. -Osteoarthritis -Neuropathies -Central/ neuropathic pain following a CVA -Postherpetic neuralgia -Phantom Limb pain v Goal: Maintain acceptable level of comfort Pain. Retrieved from http: //www. cirpd. org
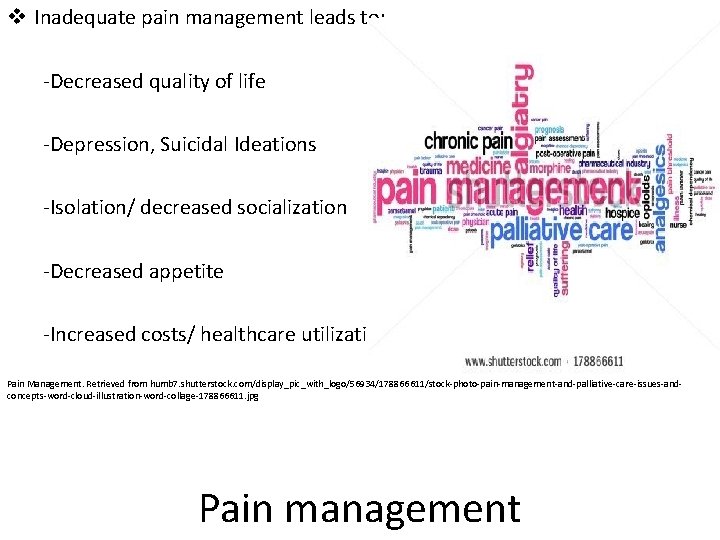
v Inadequate pain management leads to: -Decreased quality of life -Depression, Suicidal Ideations -Isolation/ decreased socialization -Decreased appetite -Increased costs/ healthcare utilization Pain Management. Retrieved from humb 7. shutterstock. com/display_pic_with_logo/56934/178866611/stock-photo-pain-management-and-palliative-care-issues-andconcepts-word-cloud-illustration-word-collage-178866611. jpg Pain management
"Maybe" When I wander don’t tell me to come and sit down. Wander with me. It may be because I am hungry, thirsty, need the toilet. Or maybe I just need to stretch my legs. When I call for my mother (even though I’m ninety!) don’t tell me she has died. Reassure me, cuddle me, ask me about her. It may be that I am looking for the security that my mother once gave me. When I shout please don’t ask me to be quiet…or walk by. I am trying to tell you something, but have difficulty in telling you what. Be patient. Try to find out. I may be in pain. When I become agitated or appear angry, please don’t reach for the drugs first. I am trying to tell you something. It may be too hot, too bright, too noisy. Or maybe it’s because I miss my loved ones. Try to find out first. When I don’t eat my dinner or drink my tea it may be because I’ve forgotten how to. Show me what to do, remind me. It may be that I just need to hold my knife and fork I may know what to do then. When I push you away while you’re trying to help me wash or get dressed, maybe it’s because I have forgotten what you have said. Keep telling me what you are doing over and over. Maybe others will think you’re the one that needs the help! With all my thoughts and maybes, perhaps it will be you who reaches my thoughts, understands my fears, and will make me feel safe. Maybe it will be you who I need to thank. If only I knew how. -Author unknown “Maybe”. Retrieved from http: //www. walking-in-their-shoes. com/-maybe-poem. html