CARE OF MECHANICALLY VENTILATED PATIENT Dr Kondamudi Sai





- Slides: 39
CARE OF MECHANICALLY VENTILATED PATIENT Dr. Kondamudi Sai Kiran Internal Medicine & Critical Care 10 May 2016, CNE, HICC (Aware Global Hospital)


PATIENT SAFETY PATIENT COMFORT
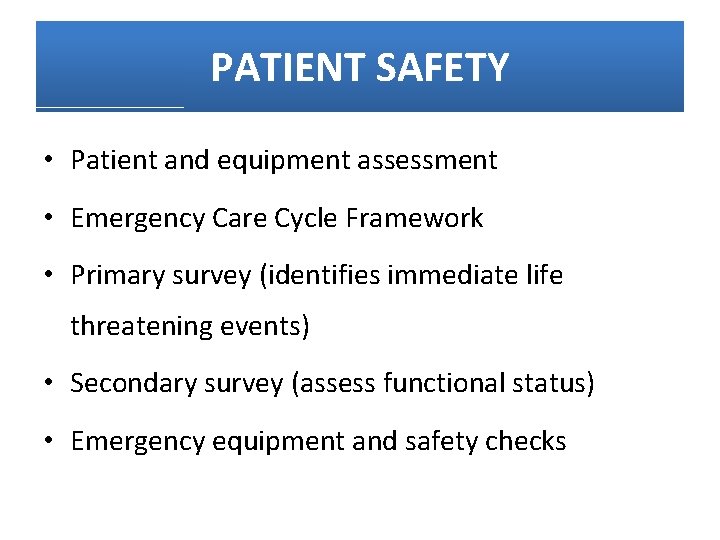
PATIENT SAFETY • Patient and equipment assessment • Emergency Care Cycle Framework • Primary survey (identifies immediate life threatening events) • Secondary survey (assess functional status) • Emergency equipment and safety checks
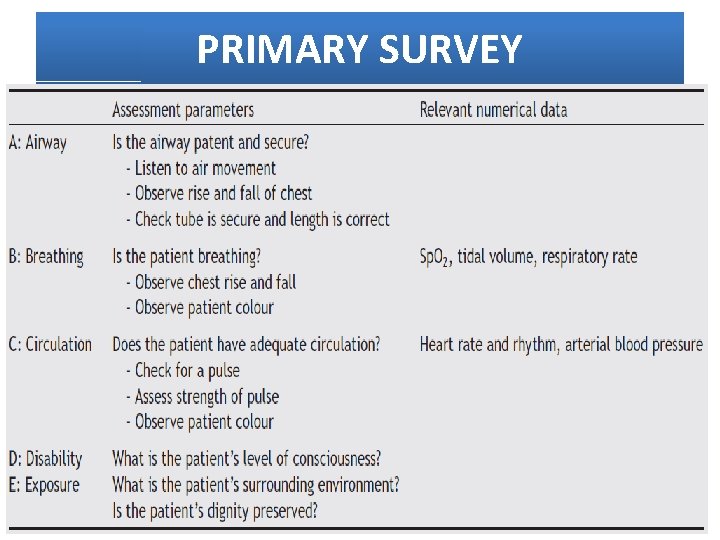
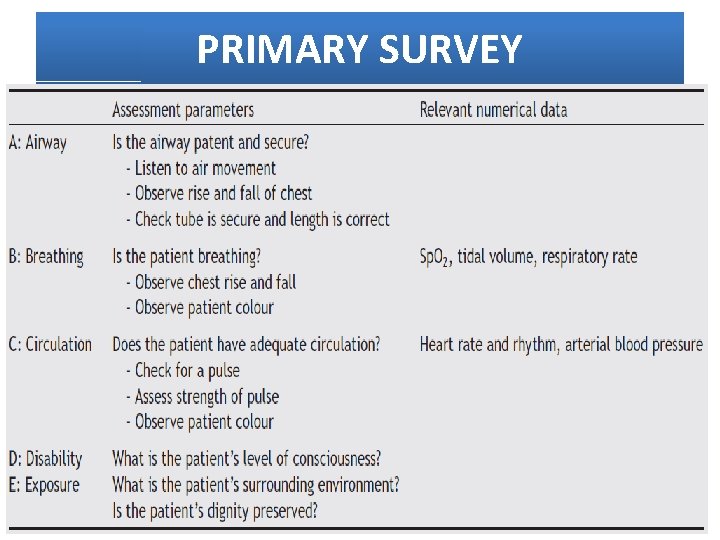
PRIMARY SURVEY
SECONDARY SURVEY • Assess all body systems (head to toe) • Enables early identification of issues and appropriate intervention to minimise or prevent complications
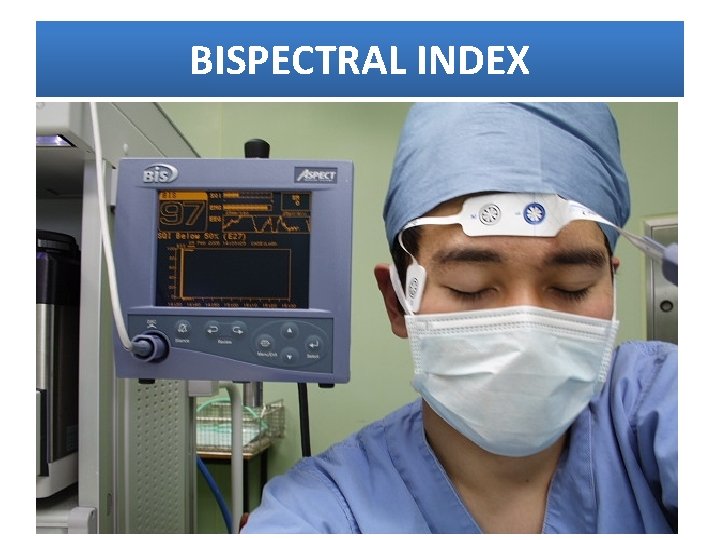
NEUROLOGICAL SYSTEM • GCS o Assess level of consciousness • Communication scoring systems o letter boards, writing notes, mouthing words • Pupil size and reaction • Sedation score: titrate accordingly • Degree of neuromuscular blockade: o Partial rather than complete o Assess using peripheral nerve stimulator • BIS monitoring (Bispectral Index score) o Statistically estimates level of sedation
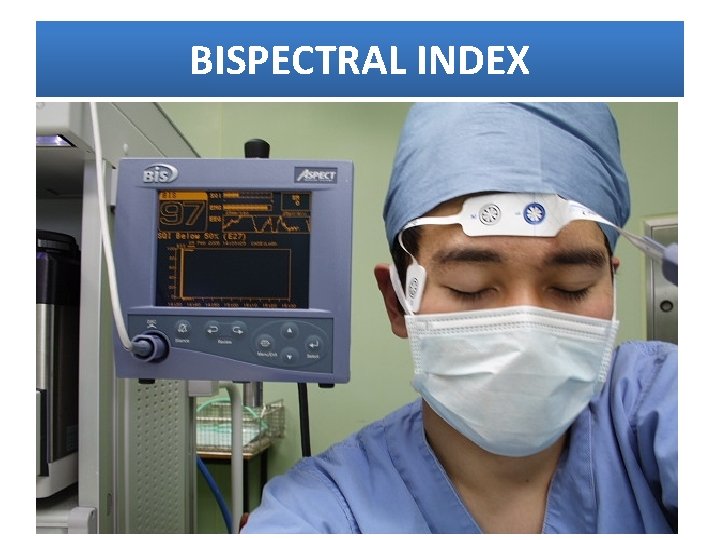
BISPECTRAL INDEX
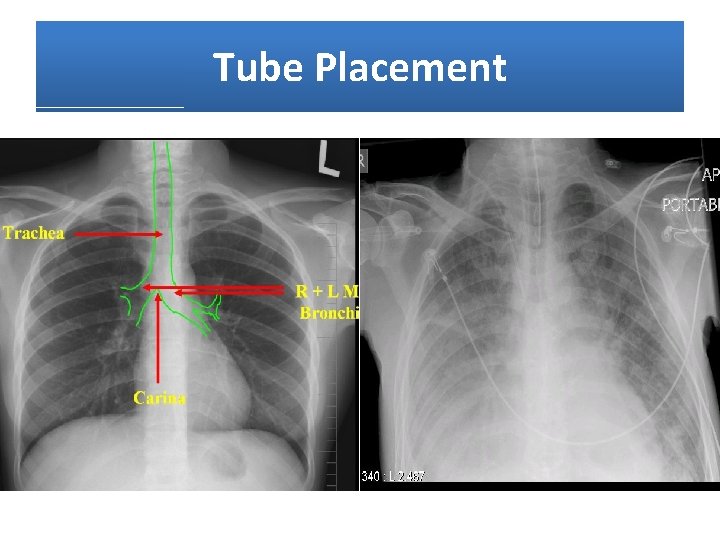
RESPIRATORY SYSTEM • Artificial airway o Tube placement o Tube security o Cuff status • Airway patency o Assessment of lung secretions o Adequacy of humidification • Breathing o Respiratory rate, volume and pressure o ABG analysis o Pulse oximetry o Capnometry
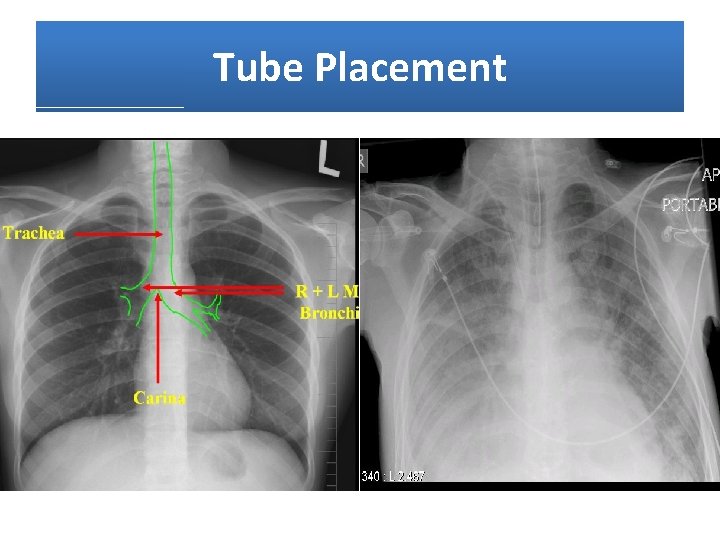
Tube Placement

Tube Security
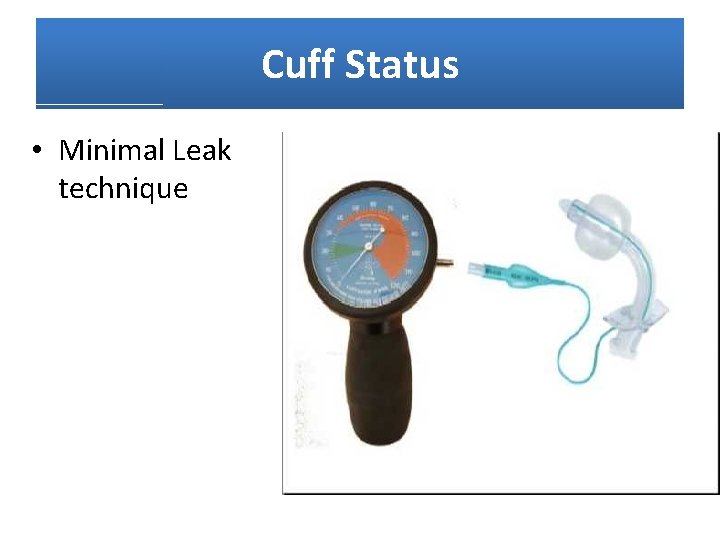
Cuff Status • Minimal Leak technique
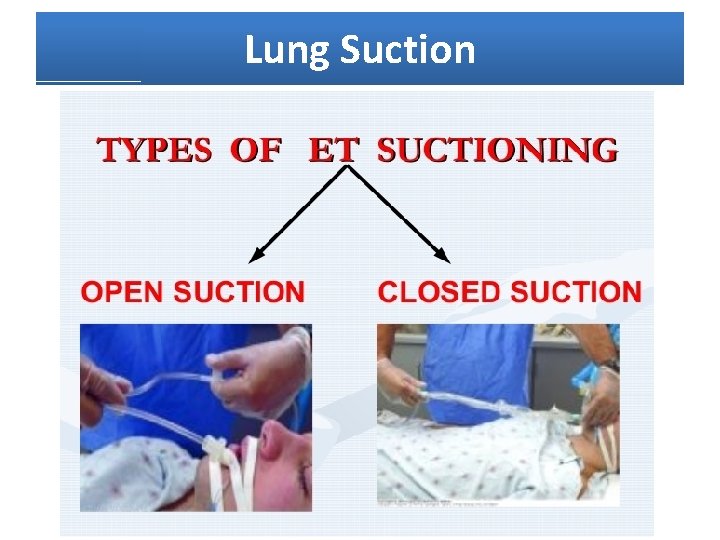
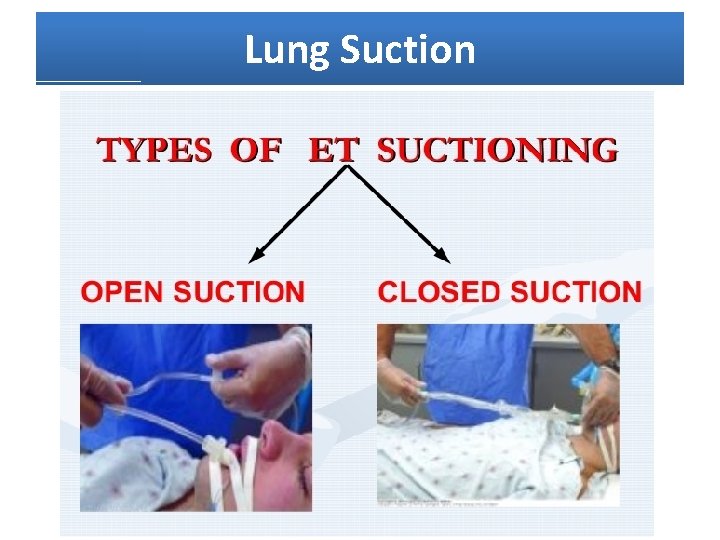
Lung Suction
Humidifcation • Heat and Moisture Exchangers (HME) • Heat Humidifiers (HH)
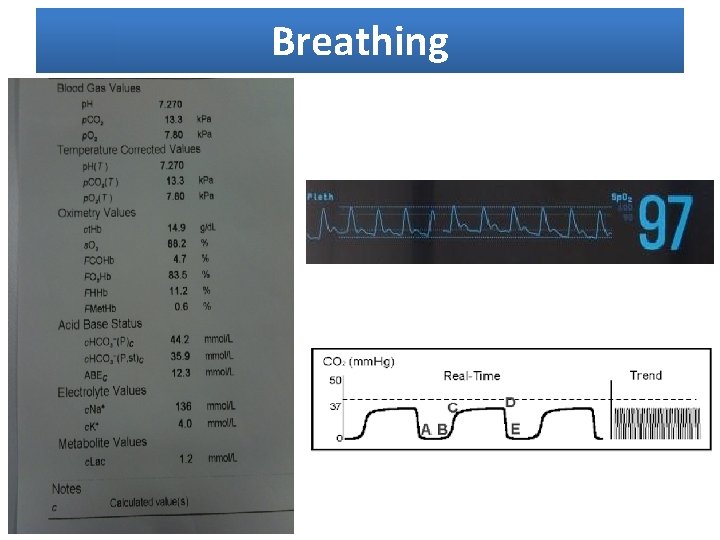
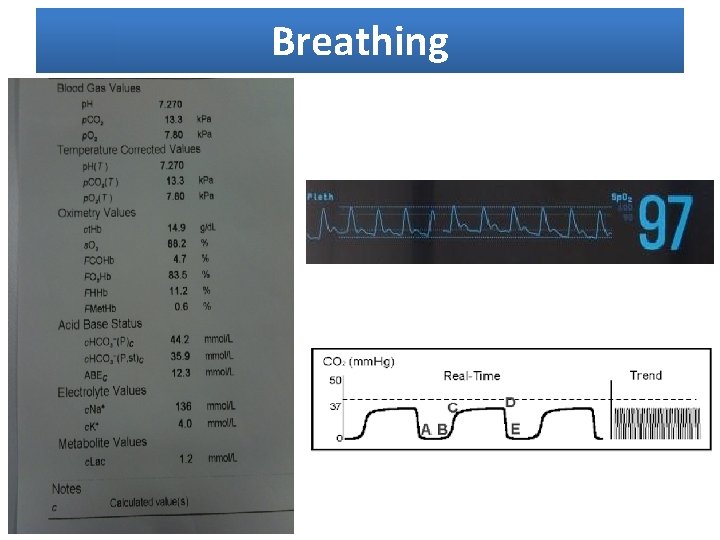
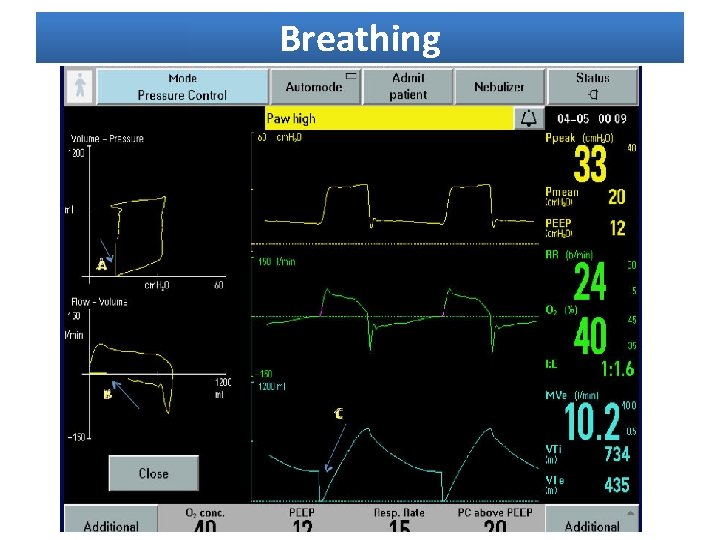
Breathing
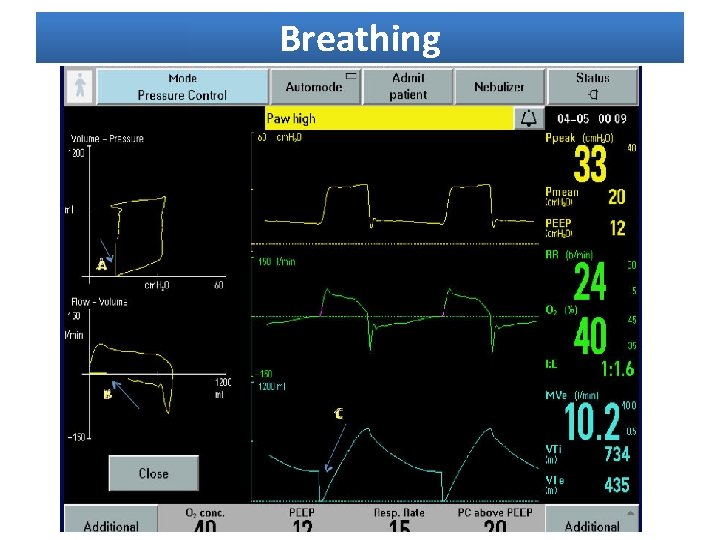
Breathing
CARDIOVASCULAR SYSTEM • Marked alteration with PPV • Increased intra thoracic pressure > decreased venous return > decreased pre load > decreased cardiac output • Continuous multi lead ECG monitoring • Assess heart rate/rhythm, blood pressure, CVP, peripheral perfusion, electrolytes, CXR, Hb • Cardiac output monitoring (Pulmonary artery catheter) • Maintain adequate filling pressure (CVP: 10 -12 mm. Hg) • Deep vein thrombosis prophylaxis o TED stockings, compression devices, LMWH
GASTROINTESTINAL SYSTEM • Nutritional status is vital part of care • Early enteral feeding via oro/NG tube recommended • Feeding protocol o Monitoring absorption, increasing rate gradually, prokinetics as needed • Meet caloric requirements (9 – 18 kcal/kg/day) • Assess for abdominal discomfort / distension / bowel sounds / amount & characteristics of gastric aspirate • Assess muscle mass, degree of muscle wasting, physical strength and body weight • Monitor liver function tests and clotting times
METABOLIC SYSTEM • Temperature monitoring • Increased risk of nosocomial infections o TLC / CRP / PCT / IL-6 • Prevention of VAP (ventilator associated pneumonia) • Blood glucose monitoring o GRBS < 170 mg/d. L • Early detection of infection • Monitor electrolytes and phosphate
RENAL SYSTEM • Positive pressure ventilation associated with reduced cardiac output • Neural and hormonal mechanisms o ADH o RAAS • Maintain urine output = 0. 5 ml/kg/hour • Adequate cardiac output and MAP • Renal perfusion pressure
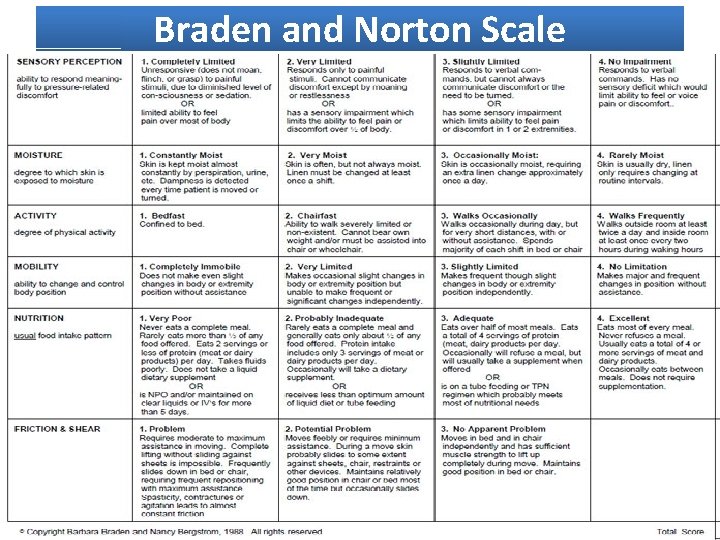
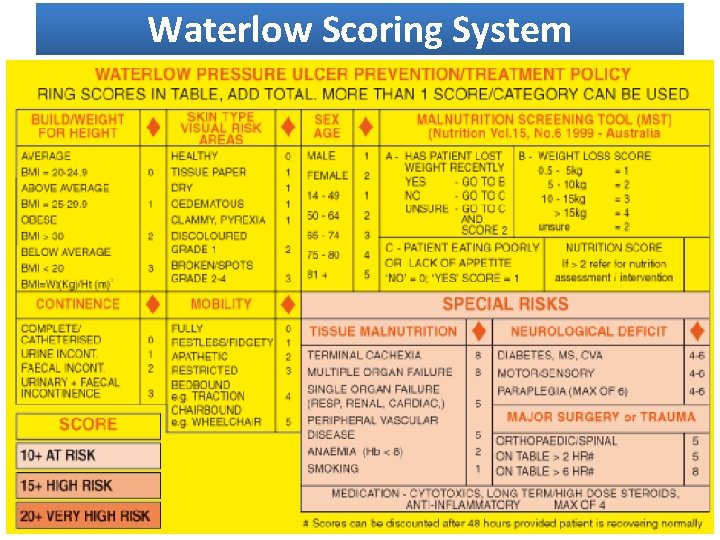
SKIN INTEGRITY AND MOBILITY • Sedation and ventilation risk factors • Effective pressure ulcer prevention is essential o Waterlow scoring system o Braden and Norton scales (best for critically ill) • Semi recumbent positioning rather than supine • Enhance mobility (sitting in chair)
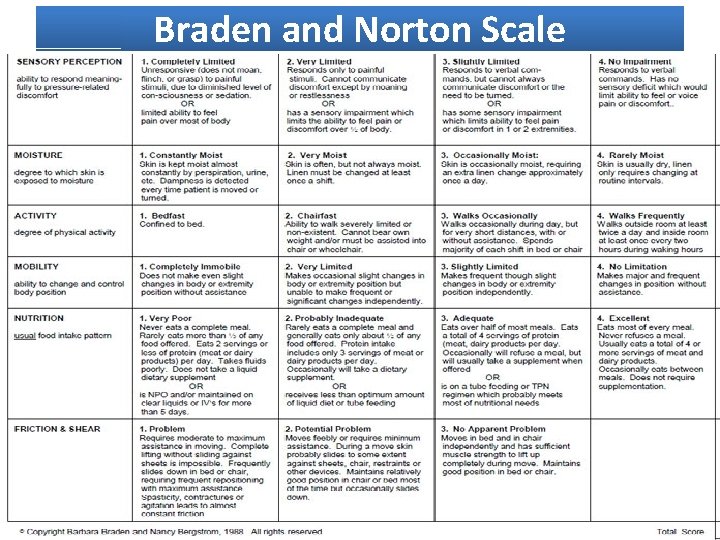
Braden and Norton Scale
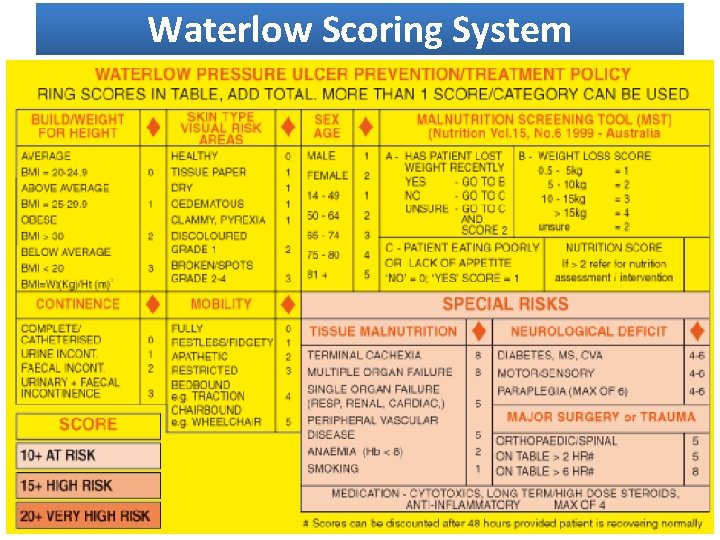
Waterlow Scoring System
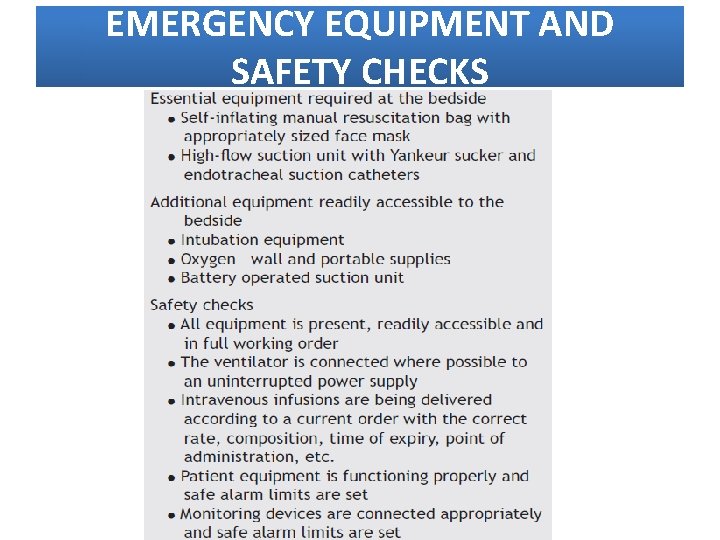
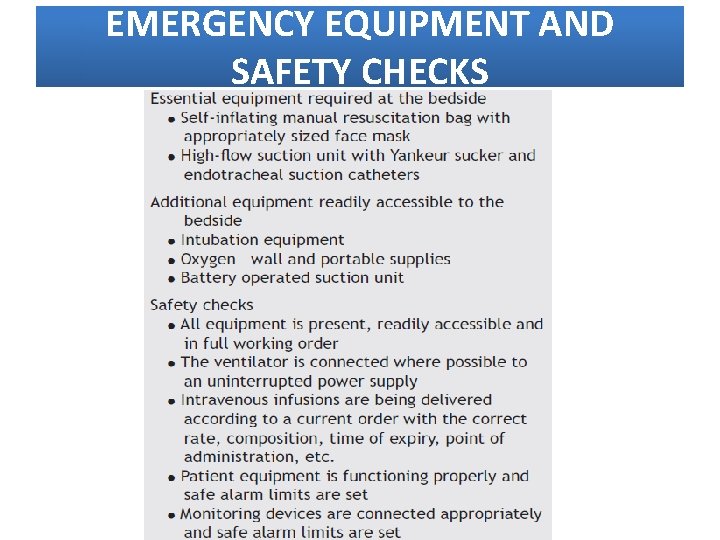
EMERGENCY EQUIPMENT AND SAFETY CHECKS

PATIENT COMFORT • Positioning • Hygiene • Stressors o Communication o Sleep disturbance o Isolation • Pain management • Sedation
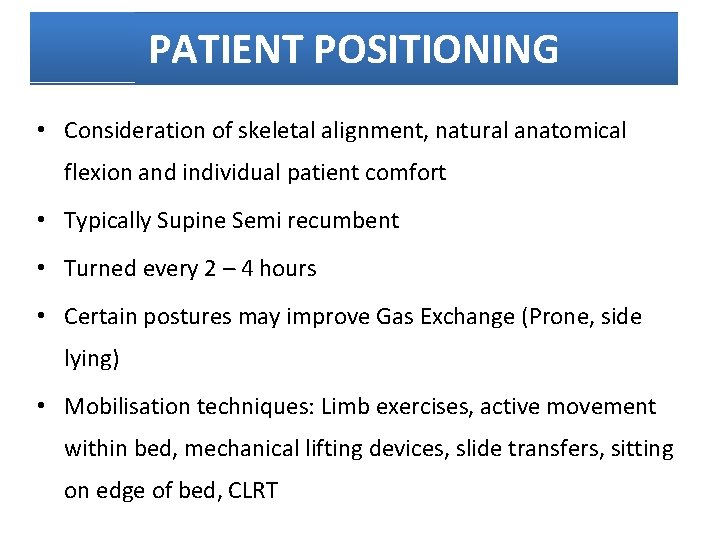
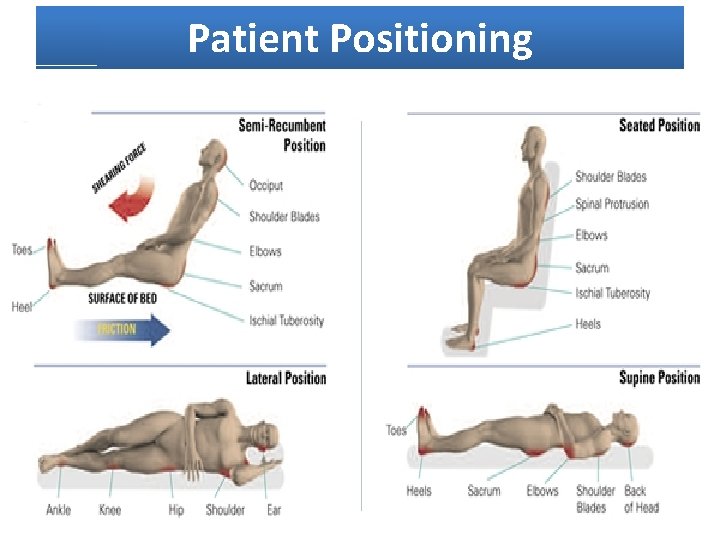
PATIENT POSITIONING • Consideration of skeletal alignment, natural anatomical flexion and individual patient comfort • Typically Supine Semi recumbent • Turned every 2 – 4 hours • Certain postures may improve Gas Exchange (Prone, side lying) • Mobilisation techniques: Limb exercises, active movement within bed, mechanical lifting devices, slide transfers, sitting on edge of bed, CLRT
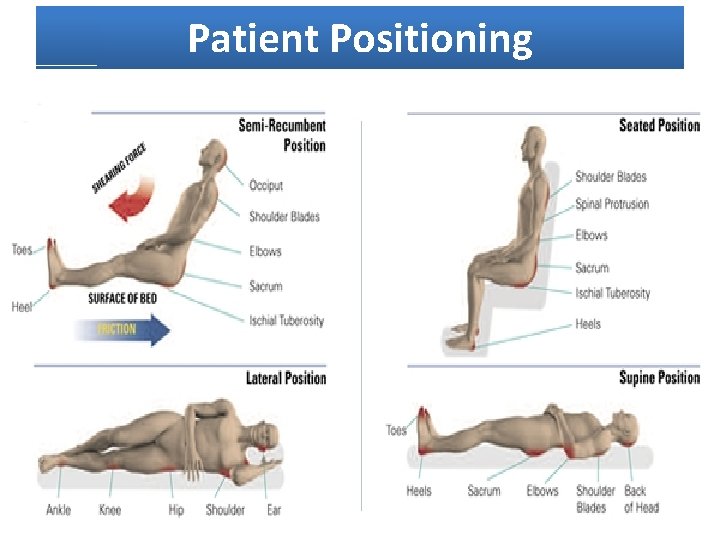
Patient Positioning
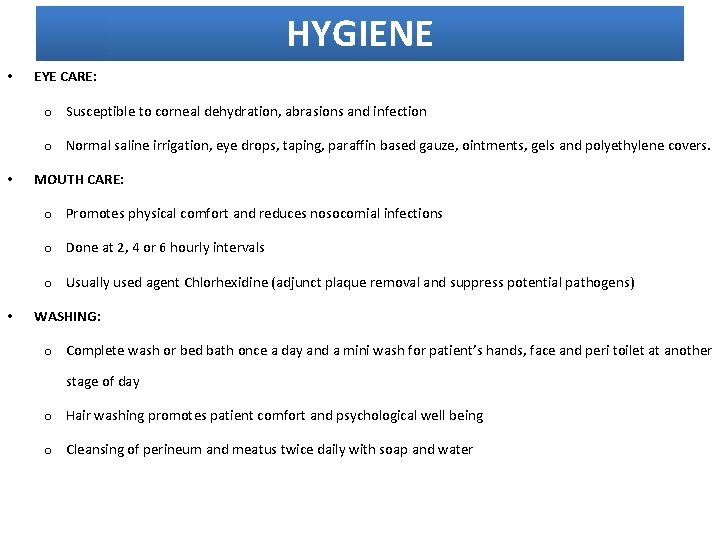
HYGIENE • EYE CARE: o Susceptible to corneal dehydration, abrasions and infection o Normal saline irrigation, eye drops, taping, paraffin based gauze, ointments, gels and polyethylene covers. • MOUTH CARE: o Promotes physical comfort and reduces nosocomial infections o Done at 2, 4 or 6 hourly intervals o Usually used agent Chlorhexidine (adjunct plaque removal and suppress potential pathogens) • WASHING: o Complete wash or bed bath once a day and a mini wash for patient’s hands, face and peri toilet at another stage of day o Hair washing promotes patient comfort and psychological well being o Cleansing of perineum and meatus twice daily with soap and water
COMMUNICATION STRESSORS • Integral component of high quality nursing care • Certain behaviours and devices • Nurse’s use of positive body language, friendly facial expression, eye contact, questions with Yes/No response reduces patient distress • Involvement of family and familiar staff • Lip reading, pen & paper, word or picture charts, alphabet boards and rewritable magnetic boards • Electronic voice output communication aids
SLEEP DISTURBANCE • High levels of fragmented sleep reported • Environmental noise, lighting, stress and pain • Suppresses immune system, weakened upper airway muscles • Visual hallucinations and delirium may result • Timely silencing of alarms, dimmed lighting, comfortable positioning , ICU room temperature, clustering of care
ISOLATION AND LONELINESS • Negative impact on patient perception of safety • Orientation to day and time • Personalise ICU environment • Trips to the outside • Family focused care • Relaxation, massage, music therapy, therapeutic touch and empathetic physical contact • Spiritual comfort
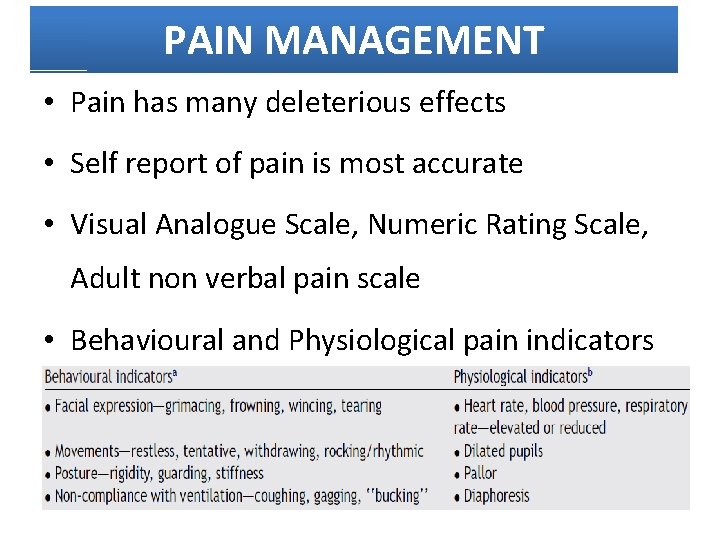
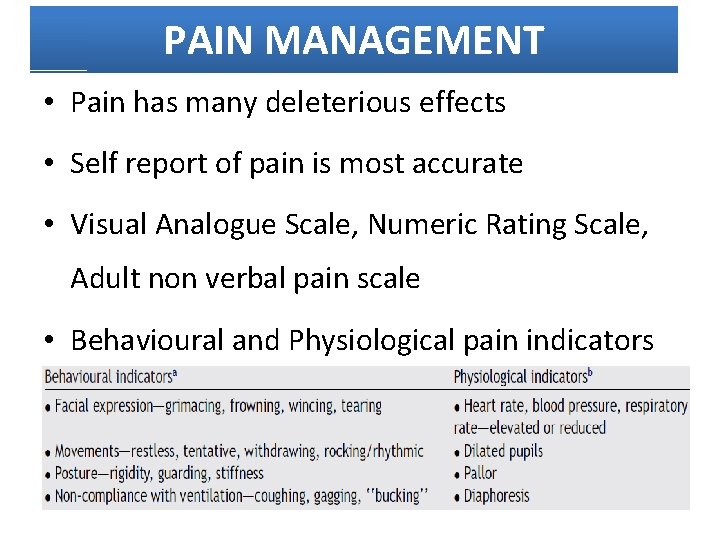
PAIN MANAGEMENT • Pain has many deleterious effects • Self report of pain is most accurate • Visual Analogue Scale, Numeric Rating Scale, Adult non verbal pain scale • Behavioural and Physiological pain indicators
PHARMACOLOGICAL PAIN MANAGEMENT • Intravenous opiods • Fentanyl or morphine • Continuous administration preferred over intermittent doses • Risk of withdrawal symptoms if used for more than 7 days • Gradual weaning needed
NON PHARMACOLOGICAL PAIN MANAGEMENT • Provision of information prior to procedures • Distraction • Relaxation techniques • Heat and cold treatments • Massage • Transcutaneous electric nerve stimulation (TENS) • Music
SEDATION • Pain and other correctable causes of distress should be eliminated • Determine patient’s level of anxiety and agitation • Sedation-Agitation-Scale (SAS), Richmond Agitation Sedation Scale (RASS) • In synergy with opiods • DOC – Benzodiazepines (anxiolytic and amnesiac) • Midazolam, Diazepam, Lorazepam • Propofol • Protocols incorporating daily withdrawal of sedation should be utilised
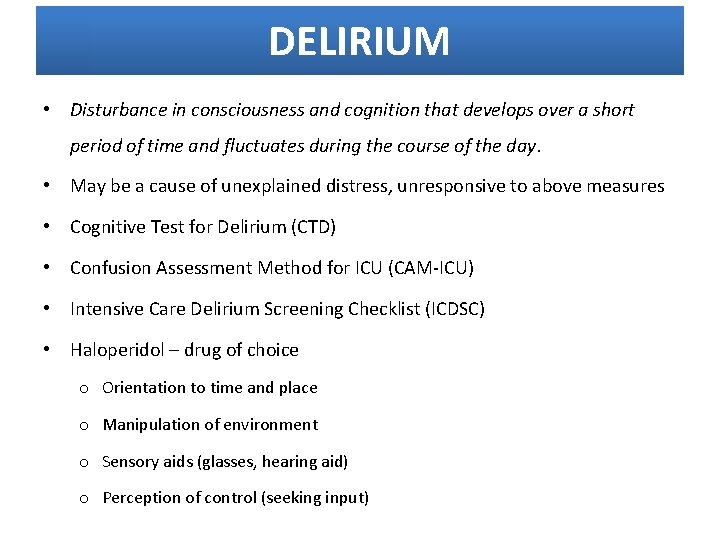
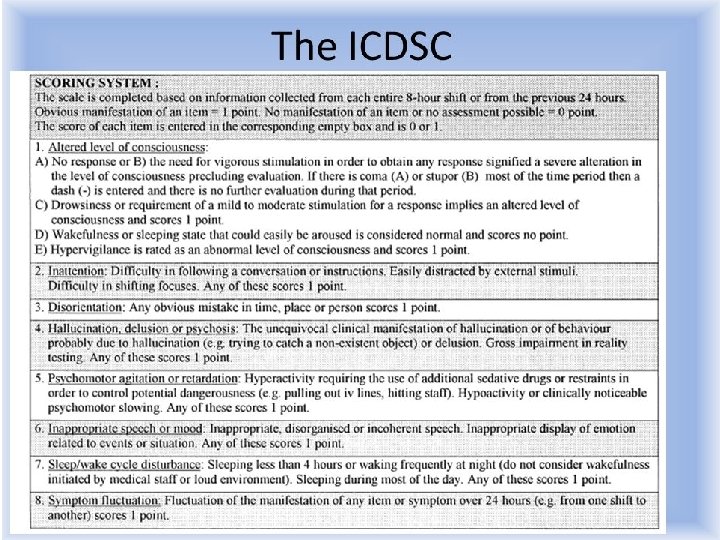
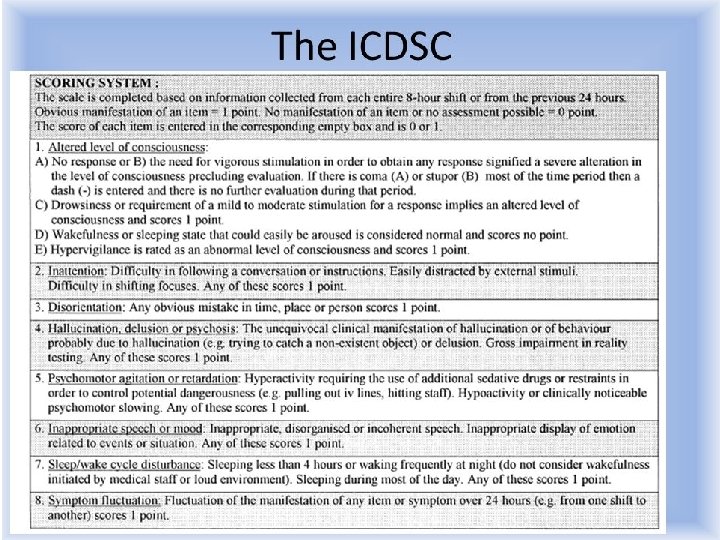
DELIRIUM • Disturbance in consciousness and cognition that develops over a short period of time and fluctuates during the course of the day. • May be a cause of unexplained distress, unresponsive to above measures • Cognitive Test for Delirium (CTD) • Confusion Assessment Method for ICU (CAM-ICU) • Intensive Care Delirium Screening Checklist (ICDSC) • Haloperidol – drug of choice o Orientation to time and place o Manipulation of environment o Sensory aids (glasses, hearing aid) o Perception of control (seeking input)

THANK YOU