Care of client with musculoskeletal injury or disorder



- Slides: 42
Care of client with musculoskeletal injury or disorder http: //www. scribd. com/doc/9378673/musculoskeletaldishttp: //www. scribd. com/doc/9378673/musculoskeletal-disorders-careof-client-with-fall-2005 orders-care-of-client-with-fall 2005. scribd. com/doc/9378673/musculoskeletal-disorders-care-of-clientwith-fall-2005
What can go wrong Fractures Hip Mandible Degenerative joint disease Osteoporosis Herniated disc Amputation
CONCEPTS: FRACTURES Reduction/Realignment Immobilization Nursing care Prevention and early detection: complication

Realignment=Reduction Correct bone alignment goal: restore injured part to normal or near-normal function Closed vs. open reduction Open reduction = surgery
Immobilization: to maintain alignment Cast Traction External fixation Internal fixation
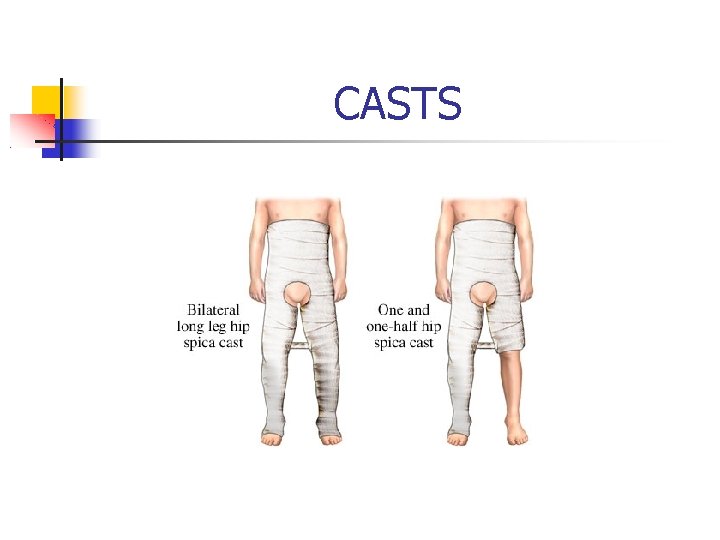
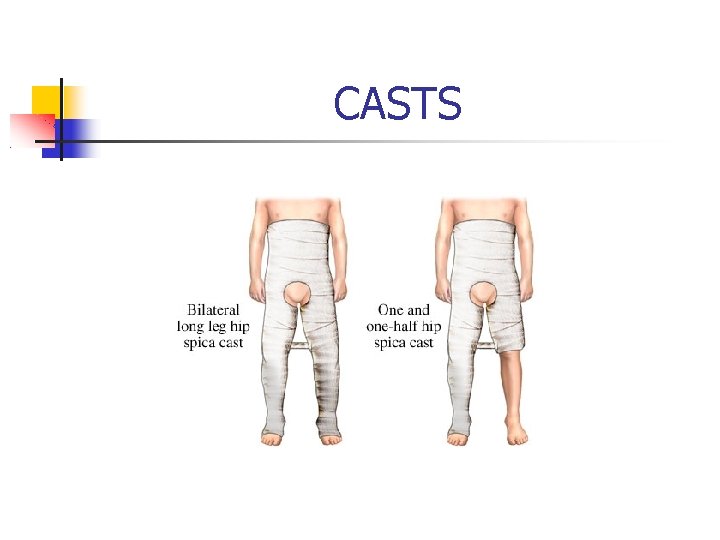
CASTS
Casts External, circumferential Thermochemical reaction = warmth Nursing care: No weight bearing 24 -72 hours “flat hands” Elevate Neuro-vascular checks
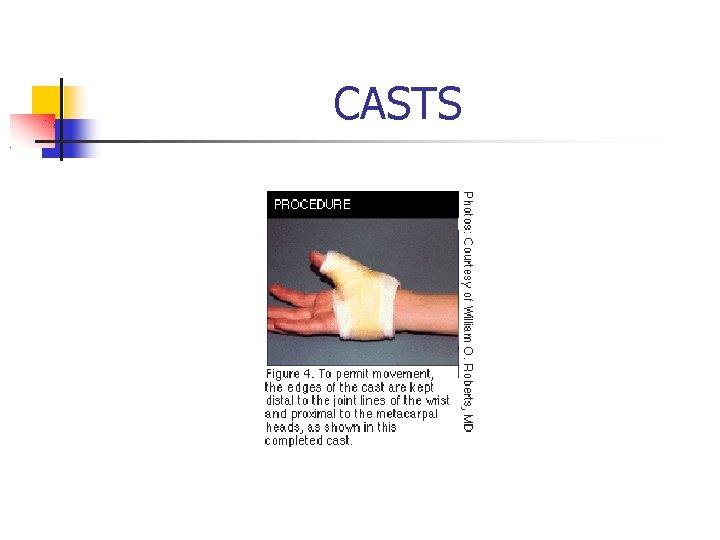
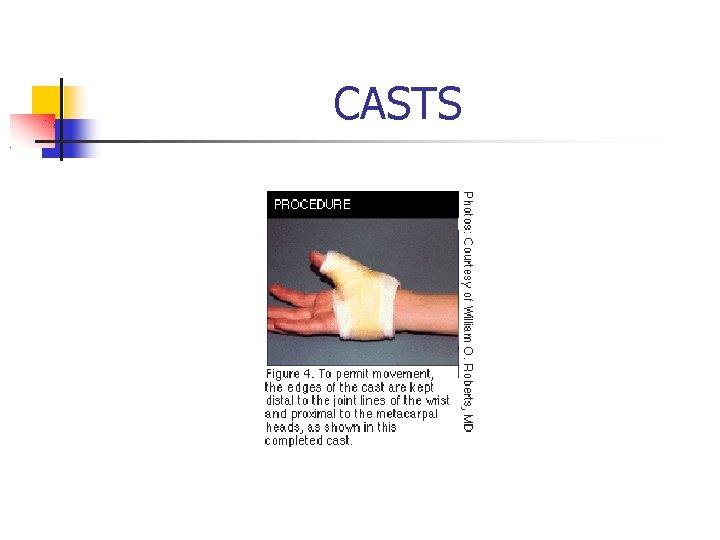
CASTS
Cast: Client/Family Teaching Keep dry No foreign objects in cast No weight bearing until MD order (at least 48 hour) Elevate above heart (48 hours) Signs of problems to report Pain, tingling, burning Sores, odor
External fixation Metal pins inserted into bone Pins attach to external rods Nursing care: Assess for s/s infection Teach pin care: ½ H 2 O 2+ ½ H 2 o Open reduction: assess incision Elevate Neurovascular checks

EXTERNAL FIXATION
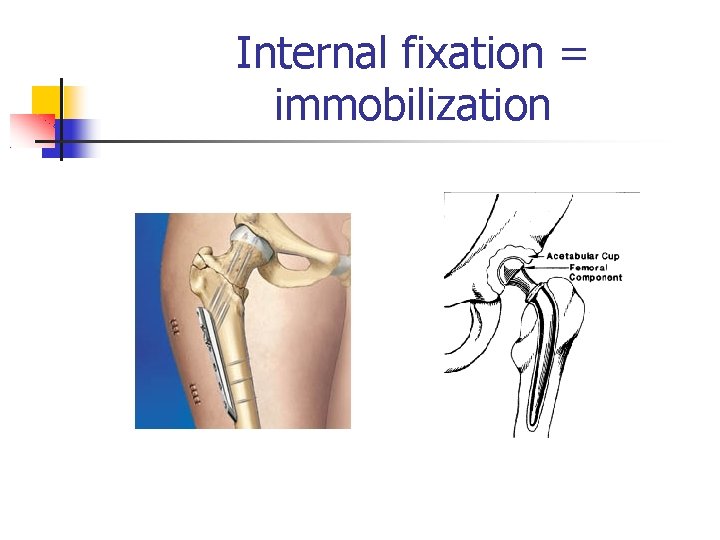
Internal Fixation Pins, plates, screws surgically inserted Nursing care: Assess incision site MD orders: activity, weight bearing, ROM, Assess s/s infection; temp. q 2 -4 hours Neurovascular checks: 5 “P’s”

INTERNAL FIXATION
Traction Pulling forces: traction + countertraction Purpose(s): Prevent or reduce muscle spasm Immobilization Reduce a fracture Treat certain joint conditions
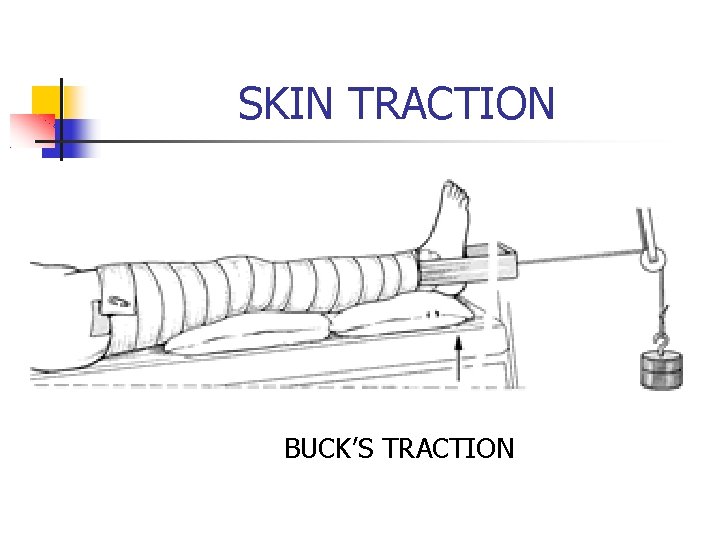
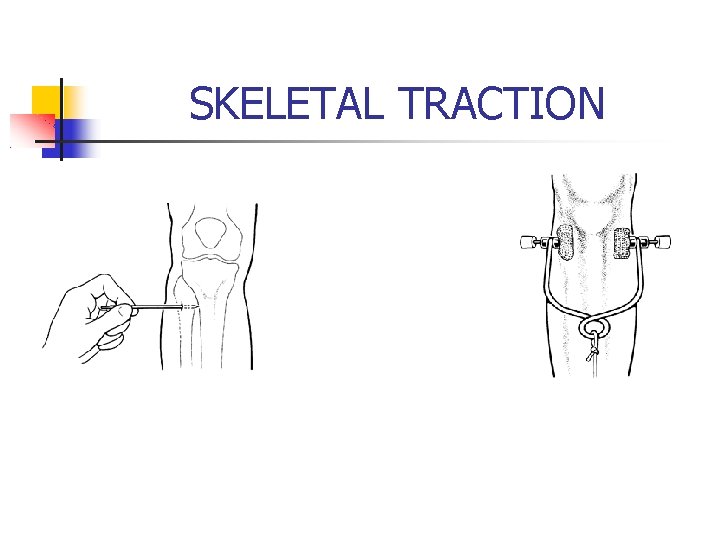
Types of Traction Skin Buck’s Russell’s Bryant’s (“babies cry with Bry”) Skeletal Balanced suspension (Lewis, 1660 -1661)
Nursing Concerns/Interventions Assess neurovascular status Assess skin (bony prominences, under elastic wraps, etc. ) Assess pin sites (skeletal tx) Maintain correct body alignment Weights hang freely Hazards of immobility
TRACTION
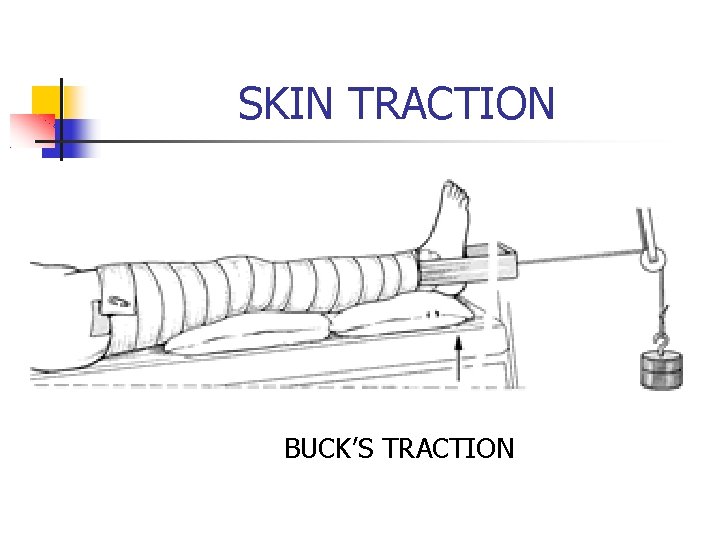
SKIN TRACTION BUCK’S TRACTION
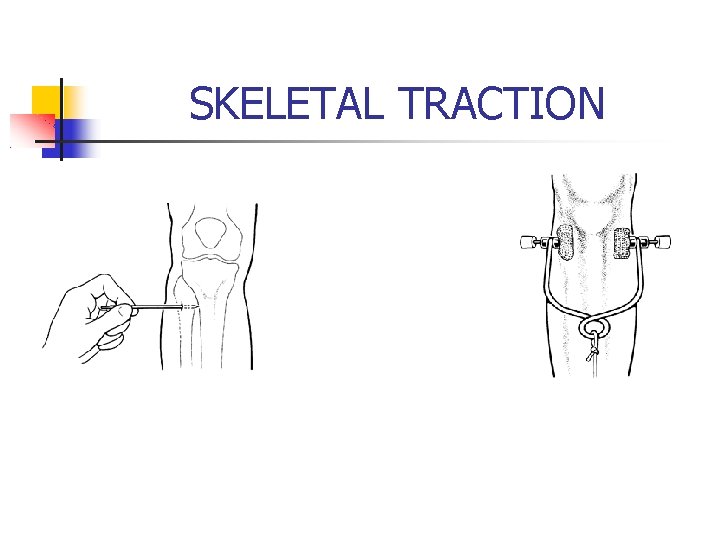
SKELETAL TRACTION
Nursing Diagnoses Neurovascular dysfunction, risk for Acute pain, R/T edema, muscle spasms, movement of bones Infection, risk for Impaired skin integrity, risk for Impaired physical mobility
Complications of Fractures Compartment syndrome Fat embolism Venous thrombosis Infection
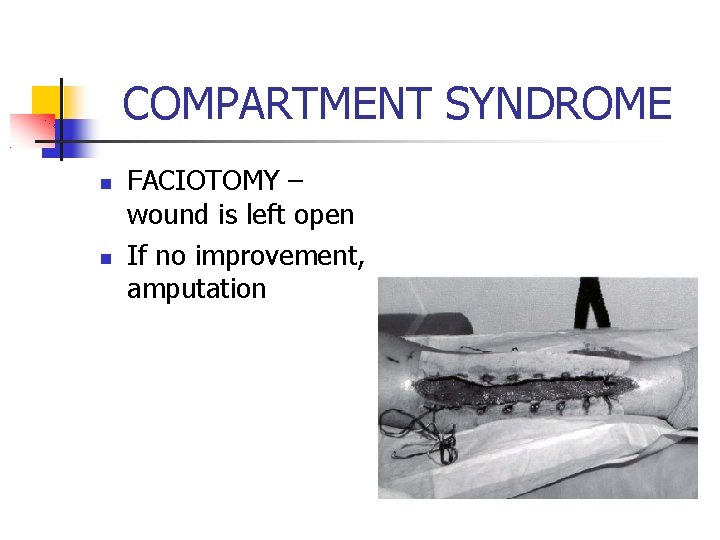
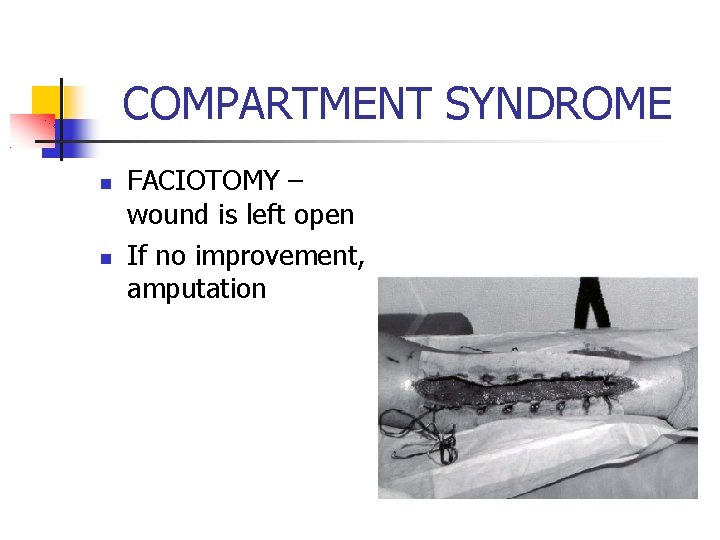
COMPARTMENT SYNDROME FACIOTOMY – wound is left open If no improvement, amputation
Hip Fracture In 1999 (USA) hip fractures resulted in approximately 338, 000 hospital admissions Up to 25% of community-dwelling older adults who sustain hip fractures remain institutionalized for at least a year
Hip Fractures One-third of older women who fracture their hip will die within a year because of lengthy convalescence that makes them susceptible to complications, like lung and bladder infections. The Lancet 1999; 353: 878 -82
Fracture of hip Types of hip fractures (Lewis pg. 1675): Intracapsular Capital Subcapital Transcervical Extracapsular Intertrochanteric Subtrochanteric
ORIF vs “Total Hip” Open reduction/internal fixation: pins, screws, plate(s) Total hip: endoprosthesis – replace femoral head
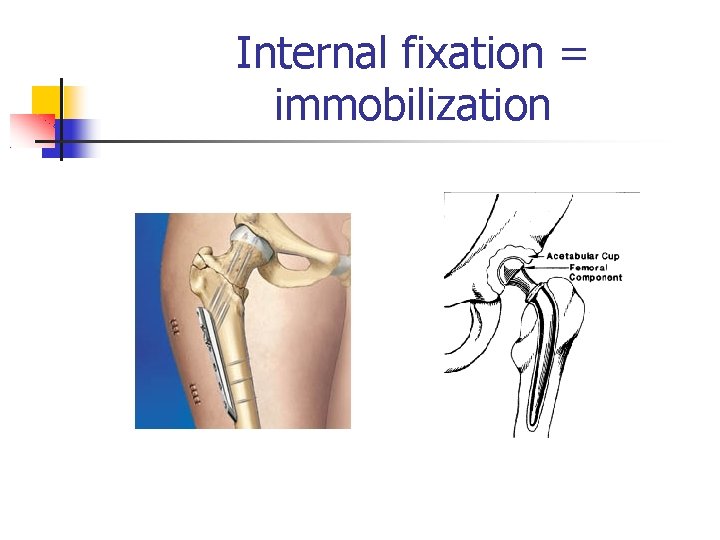
Internal fixation = immobilization
Nursing Care Risk for peripheral neurovascular dysfunction Pain Impaired mobility: Prevent thrombus Safety Constipation Risk for impaired skin integrity: Immobility Incision
Femoral head prosthesis (total hip) Prevent dislocation: Do not flex > 90 degrees No internal rotation (toes to ceiling) Maintain abduction Do not position on operative side Patient teaching: Precautions for 6 -8 weeks Notify dentist: prophylactic antibiotics Lewis: pg. 1678
Fracture of mandible Trauma vs. Therapeutic Immobilization: wiring, screws, plate(s) Nursing care: Airway (Cutter with client) Oral hygiene Nutrition Communication
What can go wrong Fractures Hip Mandible Degenerative joint disease Osteoporosis Herniated disc Amputation
Degenerative Joint Disease: Osteoarthritis Not normal part of aging process Cartilage destruction: Trauma Repetitive physical activities Inflammation Certain drugs (corticosteroids) Genetics
Assessment Location, nature, duration of pain Joint swelling/crepitus Joint enlargement Deformities Ability to perform ADL’s Risk factors Weight (history of obesity)
Nursing Interventions Pain management Rest with acute pain; exercise to maintain mobility Splint or brace Moist heat Alternative therapies TENS, acupuncture, therapeutic touch
Surgical management: total joint arthroplasty (replacement) Elbow, shoulder, hip, knee, ankle, etc. Pre-operative teaching: “What to expect” (CPM, abduction pillow, drains, compression dressing, etc. ) Postoperative exercises: quad sets, glute sets, leg raises, abduction exercises Pain management: PCA Use of pain scale
Total Joint Arthroplasty Post-operative care: 5 P’s Observe for bleeding Pain management Knee: CPM Check incision for s/s infection
Total Joint Arthroplasty Postoperative Care Prevent: Dislocation Skin breakdown Venous thrombosis (DVT) TED/Sequential compression Anticoagulants Exercises: plantar flexion, dorsiflexion, circle feet, glute & quad sets
Osteoporosis Primary – often women postmenopause Secondary – corticosteroids, immobility, hyperparathyroidism Bone demineralization = decreased bone density Fractures: Wrist Hip Vertebral column
Silent disease Dowager’s hump (kyphosis) Pain Compression fractures Spontaneous fractures X-ray can not detect until > 25% calcium in bone is lost Diagnosis: bone density ultrasound
Interventions Hormone replacement Calcium & vitamin D Calcitonin, Fosamax, Actonel, Evista Avoid alcohol and smoking Daily weight bearing, sustained exercise (walking, bike) Safety in home (throw rugs, pets, etc. )
What can go wrong Fractures Hip Mandible Degenerative joint disease Osteoporosis Herniated disc Amputation
Location of PPT on Web is below http: //www. scribd. com/doc/9378673/m usculoskeletal-disorders-care-of-clientwith-fall-2005