CARE OF CHILD WITH HIRSCHSPRUNGS DISEASE Introduction Hirschsprung




- Slides: 56
CARE OF CHILD WITH HIRSCHSPRUNG’S DISEASE
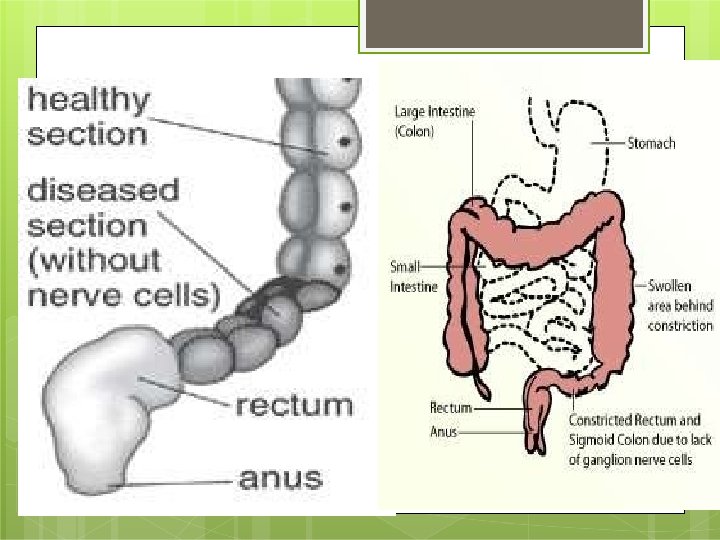
Introduction �Hirschsprung disease, congenital aganglionic megacolon is a developmental disorder of the enteric nervous system and is characterized by an absence of ganglion cells in the distal colon resulting in a functional obstruction. �Enlargement of the colon, caused by bowel obstruction that starts at the anus and progresses upwards.
Introduction �Described by Ruysch in 1691 �Popularized by Hirschsprung in 1886, �Pathophysiology, Whitehouse & Kernohan, the aganglionosis of the distal intestine as the cause of obstruction, the middle of the 20 th century.
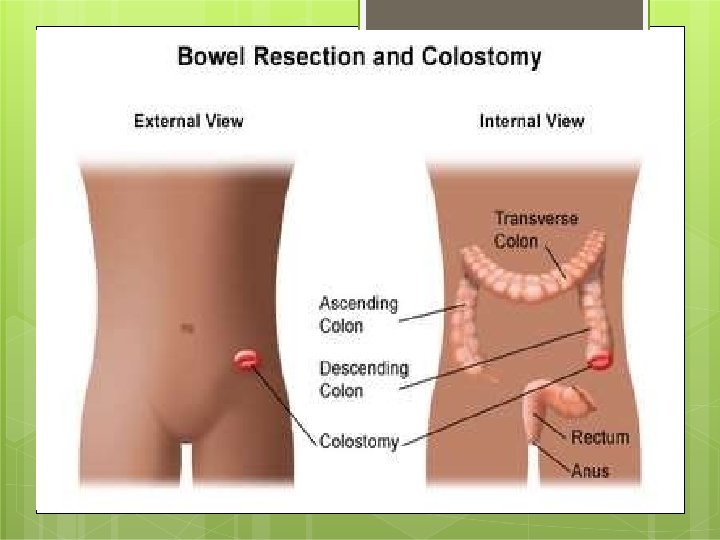
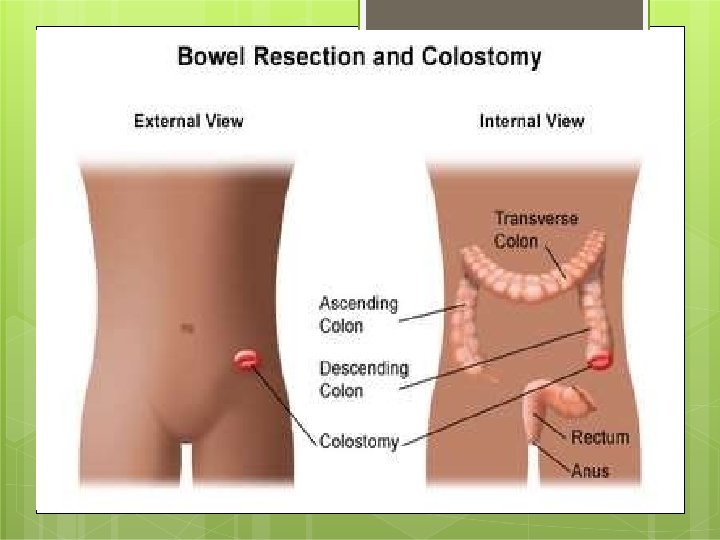
Related Anatomy �Ascending colon � � On the right side of the abdomen, 25 cm. Cecum to the hepatic flexure. Parasympathetic fibers of Vagus nerve (CN X), Ileocolic artery and right colic artery, both branches of the Superior Mesenteric Artery. �Transverse colon � � � Part of the colon from the hepatic flexure to the splenic flexure. The proximal two-thirds : -the middle colic artery, branch of superior mesenteric artery, the latter third: - branches of inferior mesenteric artery.
Review of Anatomy � Descending colon � � � Splenic flexure to the beginning of the sigmoid colon. Store matter that will be emptied into the rectum. The left colic artery. �Sigmoid colon � � After the descending colon and before the rectum. S-shaped. Muscular, and contract to increase the pressure inside the colon, causing the stool to move into the rectum. Sigmoid arteries, a branch of the Inferior Mesenteric Artery.
Review of physiology �Enteric ganglion cells are derived from the neural crest. �During normal development, neuroblasts will be found in the small intestine by the 7 th week of gestation and will reach the colon by the 12 th week of gestation.
physiology �Three neuronal plexus �The sub mucosal (ie, Meissner) plexus, �The intermuscular (ie, Auerbach) plexus, �The smaller mucosal plexus. �Normal motility is primarily under the control of intrinsic neurons. �Control both contraction and relaxation of smooth muscle. �Extrinsic control is mainly through the cholinergic and adrenergic fibers. The cholinergic fibers cause contraction, and the adrenergic fibers mainly cause inhibition.
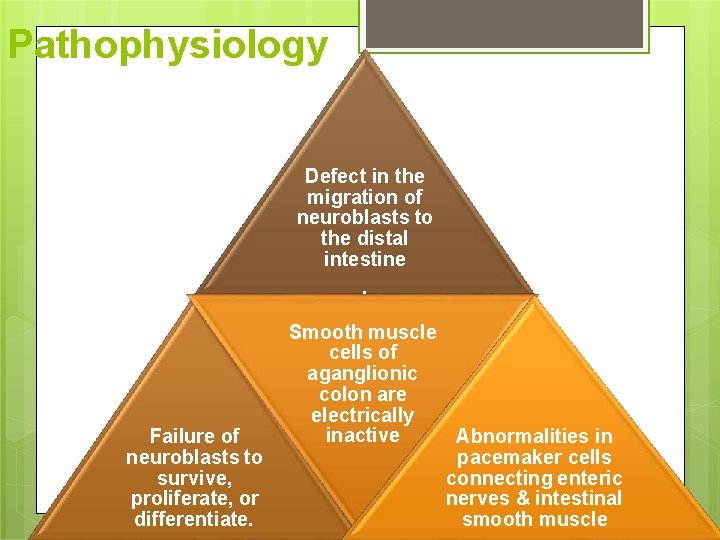
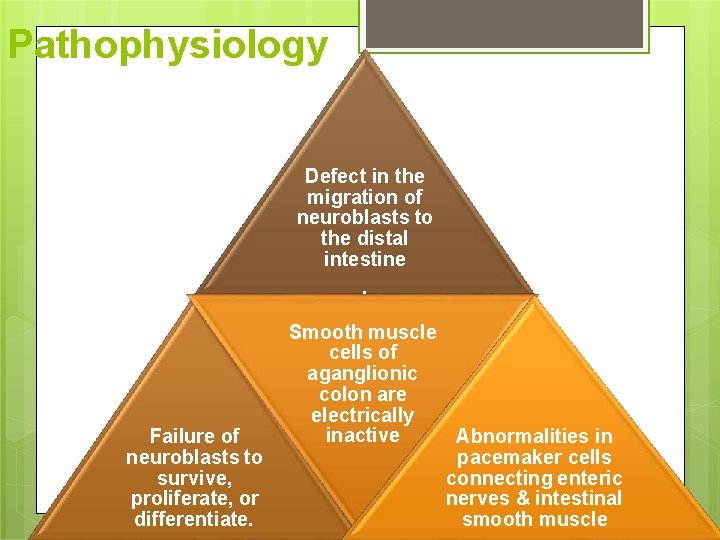
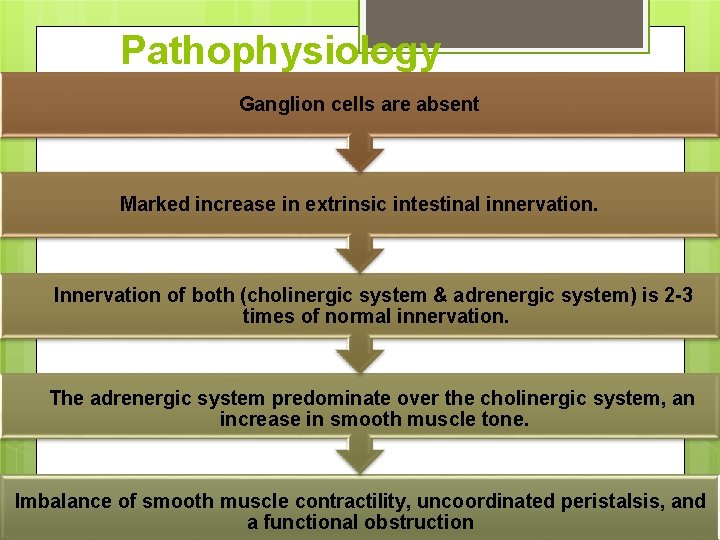
Pathophysiology Defect in the migration of neuroblasts to the distal intestine. Failure of neuroblasts to survive, proliferate, or differentiate. Smooth muscle cells of aganglionic colon are electrically inactive Abnormalities in pacemaker cells connecting enteric nerves & intestinal smooth muscle
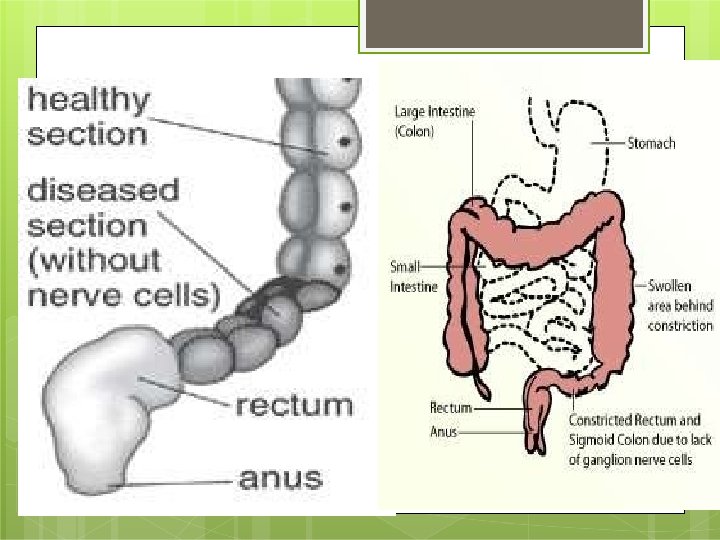
Pathophysiology �Aganglionosis begins with the anus, which is always involved, and continues proximally for a variable distance. �Myenteric (Auerbach) plexus & submucosal (Meissner) plexus are absent, reduced bowel peristalsis & function.
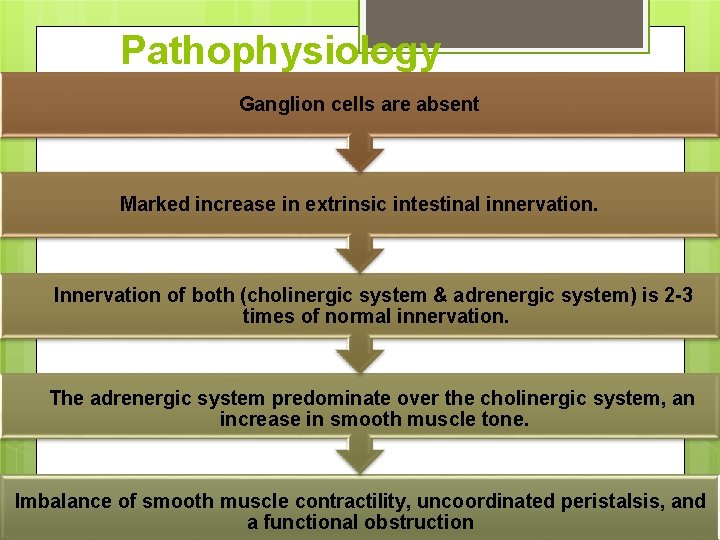
Pathophysiology Ganglion cells are absent Marked increase in extrinsic intestinal innervation. Innervation of both (cholinergic system & adrenergic system) is 2 -3 times of normal innervation. The adrenergic system predominate over the cholinergic system, an increase in smooth muscle tone. Imbalance of smooth muscle contractility, uncoordinated peristalsis, and a functional obstruction
Incidence � 1 case per 1500 newborns to 1 case per 7000 newborns.
epidemiology �Sex �M>F; M: F=4: 1. �However, with long-segment disease, the incidence increases in females. �Age �Uncommon in premature infants. �Approximately 90% of patients with Hirschsprung disease are diagnosed in the newborn period.
Mortality/Morbidity �Approximately 20% of infants have one or more associated abnormality (neurological, cardiovascular, urological, or gastrointestinal system). �Hirschsprung disease has been found to be associated with Down syndrome �Untreated aganglionic megacolon in infancy may result in a mortality rate of as much as 80%. �In cases of treated Hirschsprung disease, the mortality rate may be as high as 30% as a result of enterocolitis.
Clinical presentation �Newborn with delayed passage of meconium �Any child with a history of chronic constipation since birth with �Ribbon like stool �Foul smelly stool. �Bowel obstruction with bilious vomiting, �Abdominal distention, �Poor feeding �Failure to thrive. �About 10% diarrhea caused by enterocolitis �Colonic perforation, �Sepsis �vomiting.
Physical presentation �Distended abdomen �Inability to release flatus �An empty rectum on digital rectal examination �Rectal impaction �Rapid expulsion of feces after rectal examination
Diagnosis: �H/o failure to pass meconium within 24 -48 hours after birth. �Plain abdominal radiographs may show distended bowel loops with a paucity of air in the rectum. �Barium enema �The catheter is placed just inside the anus �Contrast injected into the anus �Radiographs are taken immediately after hand injection of contrast and again 24 hours later. �A narrowed distal colon with proximal dilation is the classic finding of Hirschsprung disease after a barium enema. �Retention of contrast for longer than 24 hours after the barium enema has been performed.

Barium enema
Diagnosis: �Anorectal manometry detects the relaxation reflex of the internal sphincter after distension of the rectal lumen. This normal inhibitory reflex is thought to be absent. �Rectal �The biopsy definitive diagnosis of Hirschsprung disease is confirmed by rectal biopsy, i. e. , findings that indicate an absence of ganglion cells. �Hypertrophied nerves in that area. �Full-thickness rectal biopsy. �The specimen must be obtained at least 1. 5 cm above the dentate line because aganglionosis may normally be present below this level. �Bleeding and scarring and need for GA.
Diagnosis: �Simple suction rectal biopsy �Rectal mucosa and submucosa are sucked into the suction device, and a self-contained cylindrical knife cuts off the tissue. �Can be easily performed at the bedside. �Laboratory Studies �Chemistry panel: dehydration(diarrhea). �CBC count: preoperative hematocrit and platelet count. �Coagulation studies: clotting disorders are corrected before surgery. �Because cardiac malformation (2 -5%) and Trisomy 21 (5 -15%) are associated with congenital aganglionosis, cardiac evaluation and genetic testing may be warranted.
Differential Diagnoses: �Constipation, �Hypothyroidism, �Irritable Bowel Syndrome, �Anorectal malformations �Intestinal atresias or stenosis �Intestinal malrotation �Meconium blockage syndrome �Neuronal intestinal dysplasia �Prematurity �Small left colon syndrome �Micro colon �Sepsis �Cystic fibrosis

TREATMENT
Medical Care �The 1. 2. 3. general goals of medical care 3 -fold To treat the complications of unrecognized or untreated Hirschsprung disease, To institute temporary measures until definitive reconstructive surgery can take place, To manage bowel function after reconstructive surgery.

Medical Care �Management of complications �Reestablishing normal fluid and electrolyte balance, �Preventing bowel over distension, �Managing sepsis. �Intravenous hydration, nasogastric decompression, administration of intravenous antibiotics remain the cornerstones of initial medical management. �Colonic lavage, consisting of mechanical irrigation with a large-bore rectal tube and large volumes of irrigant, may be required. �Balanced salt solutions may help prevent electrolyte imbalances.

Medical Care �Nasogastric decompression, intravenous fluids, antibiotics, and colonic lavage may also need to be used in postoperative patients who develop enterocolitis as a complication. �Sodium cromoglycate �Routine colonic irrigation and prophylactic antibiotic therapy �Injecting the non relaxing internal sphincter mechanism with botulinum toxin has been shown to induce more normal patterns of bowel movements in postoperative patients with enterocolitis.
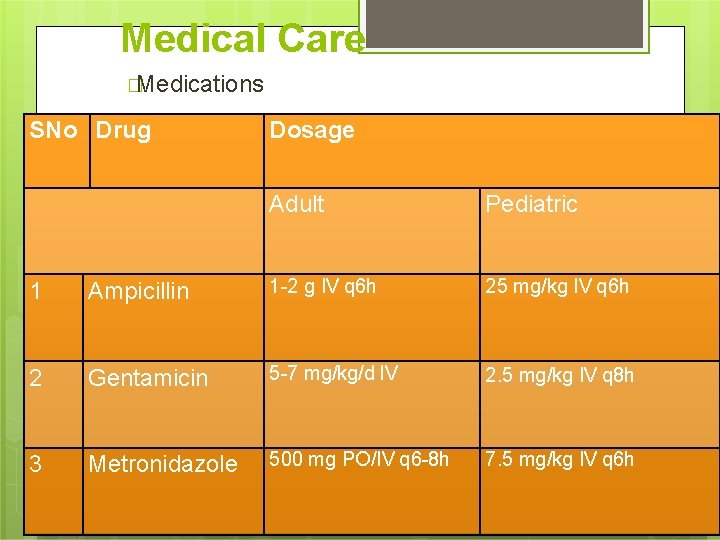
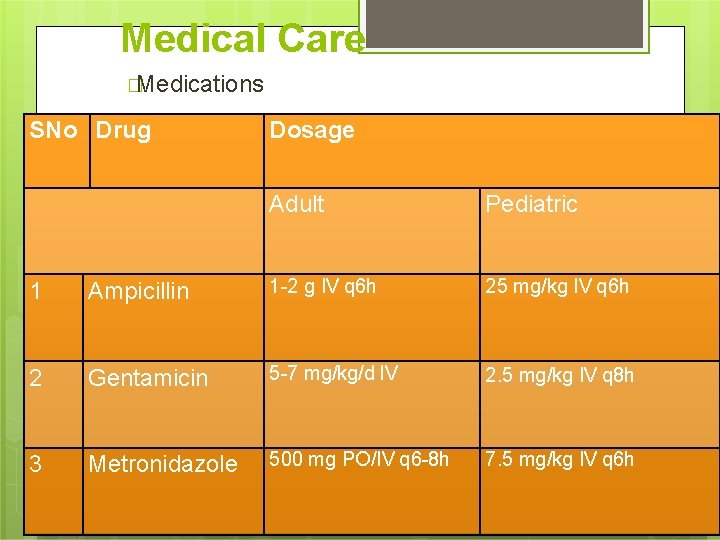
Medical Care �Medications SNo Drug Dosage Adult Pediatric 1 Ampicillin 1 -2 g IV q 6 h 25 mg/kg IV q 6 h 2 Gentamicin 5 -7 mg/kg/d IV 2. 5 mg/kg IV q 8 h 3 Metronidazole 500 mg PO/IV q 6 -8 h 7. 5 mg/kg IV q 6 h
Medical Care �Toxins �Induce more normal patterns of bowel movements in postoperative patients with enterocolitis. �Botulinum toxin type A: - Binds to receptor sites on motor nerve terminals and inhibits release of acetylcholine, which in turn inhibits transmission of impulses in neuromuscular tissue. �Adult � 1. 25 -2. 5 U IM; may repeat after 3 -4 month �Pediatric �>12 years: Administer as in adults <12 years: 0. 25 -1 U IM; may repeat after 3 -4 month
Surgical Care Diverting colostomy at the time of diagnosis Once the child grows and weighs more than 10 kg, the definitive repair is performed. 1. 2. �In 1949, Swenson described the first consistent definitive procedure for Hirschsprung disease, rectosigmoidectomy with coloanal anastomosis. Since then, other operations have been described, including the Duhamel and Soave techniques.
Surgical Care �For neonates who are first treated with a diverting colostomy, the transition zone is identified and the colostomy is placed proximal to this area. The presence of ganglion cells at the colostomy site confirmed by a frozen-section biopsy. �The 3 most commonly performed definitive repairs are the Swenson, Duhamel, and Soave procedures (The Pull-through Procedure).
Pull Through
Swenson’s operation
Surgical Care �Swenson �The procedure Swenson procedure was the original pullthrough procedure used to treat Hirschsprung disease. �The aganglionic segment is resected down to the sigmoid colon and the remaining rectum, and an oblique anastomosis is performed between the normal colon and the low rectum.
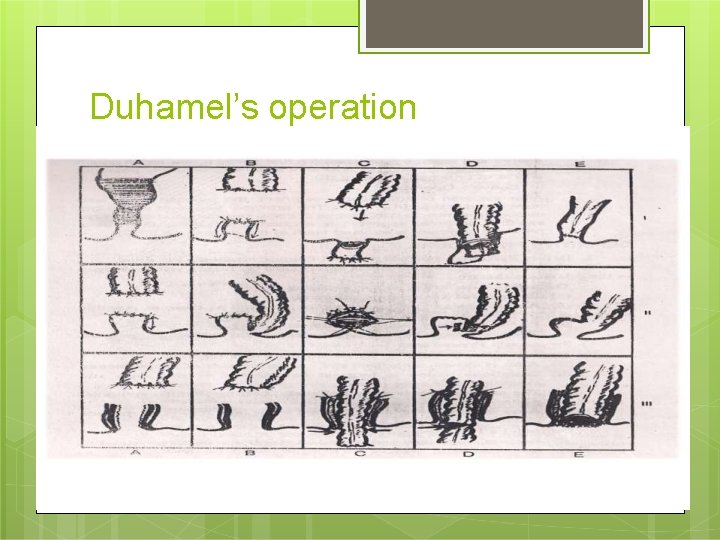
Duhamel’s operation
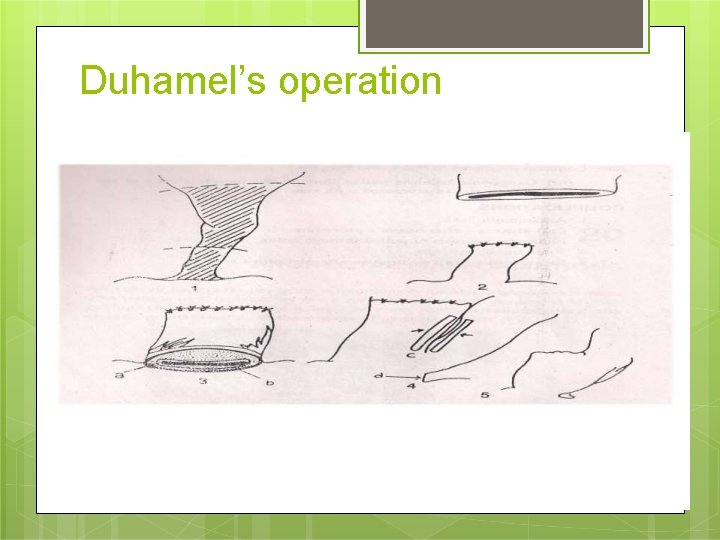
Duhamel’s operation
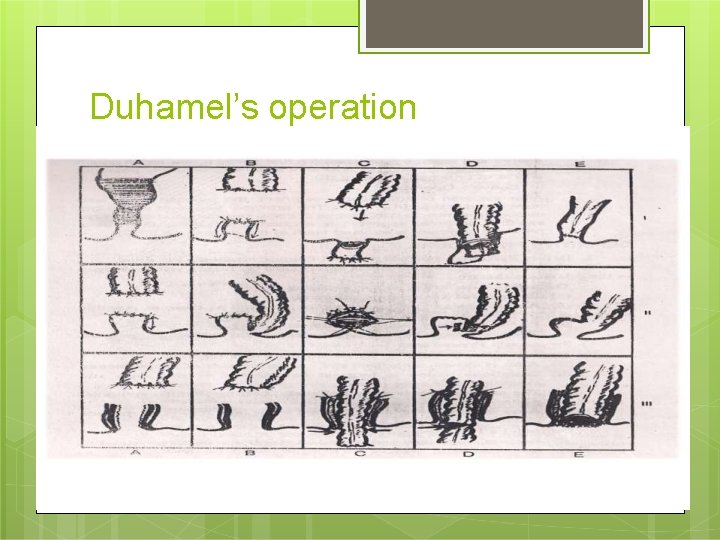
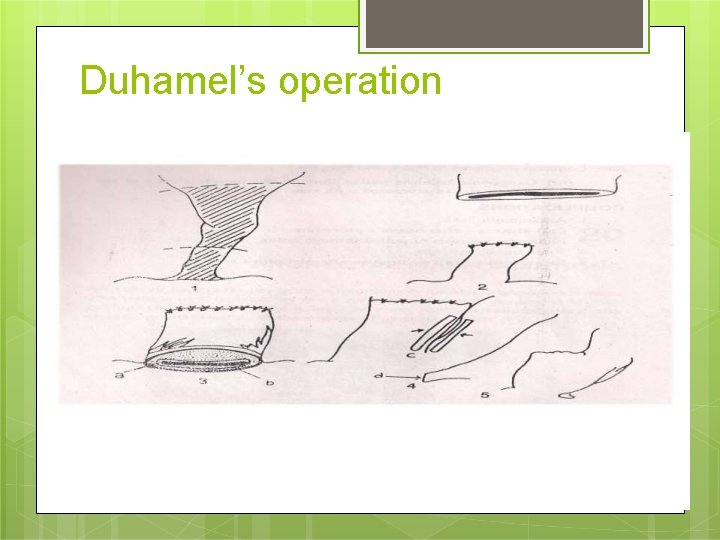
Surgical Care �Duhamel procedure �The Duhamel procedure was first described in 1956 as a modification to the Swenson procedure. �Key points are that a retrorectal approach is used and a significant portion of aganglionic rectum is retained. �The aganglionic bowel is resected down to the rectum, and the rectum is over sewn. The proximal bowel is then brought through the retrorectal space (between the rectum and sacrum), and an end-toside anastomosis is performed on the remaining rectum.
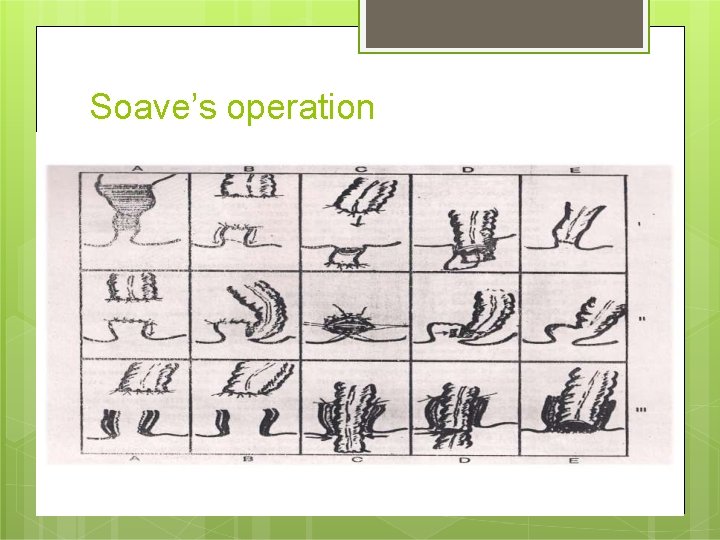
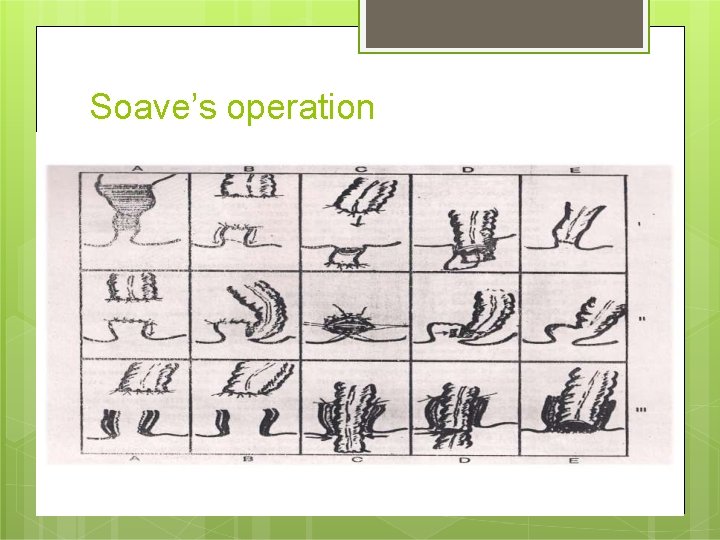
Soave’s operation
Surgical Care �Soave �The (endorectal) procedure Soave procedure was introduced in the 1960 s and consists of removing the mucosa and submucosa of the rectum and pulling the ganglionic bowel through the aganglionic muscular cuff of the rectum. �The original operation did not include a formal anastomosis, relying on scar tissue formation between the pull-through segment and the surrounding aganglionic bowel. The procedure has since been modified by Boley to include a primary anastomosis at the anus.
Surgical Care �Anorectal myomectomy �For children (and occasionally adults) with ultra short-segment Hirschsprung disease, removing a strip of posterior midline rectal wall is an alternative surgical option. �The procedure removes a 1 -cm wide strip of extra mucosal rectal wall beginning immediately proximal to the dentate line and extending to the normal ganglionic rectum proximally. �The mucosa and submucosa are preserved and closed.
Complications �Postoperative enterocolitis with the Swenson procedure, �Constipation following the Duhamel repair, �Diarrhea and incontinence with the Soave pullthrough procedure. �Anastomosis leakage and stricture formation (515%), �Intestinal obstruction (5%), �Pelvic abscess (5%), �Wound infection (10%), �Wound dehiscence and incomplete resection requiring re-operation (5%).
Complications �Stomal complications, such as prolapse or stricture. �Rectovesical fistulas �Mechanical obstruction �Persistent aganglionosis �Motility disorders �Internal sphincter achalasia may result in persistent obstruction. This can be treated with internal sphincterotomy, intrasphincteric botulinum toxin, or nitroglycerin paste. Most cases will resolve by the age of 5 years.
Complications �Functional megacolon may be present due to stool-holding behavior. �Incontinence may be the result of abnormal sphincter function, decreased sensation, or overflow incontinence secondary to constipation.
Prognosis �As expected, patients with associated trisomy 21 tend to have poorer clinical outcomes. � In general, more than 90% of patients with Hirschsprung disease have satisfactory outcomes �Although many patients may have disturbances of bowel function for several years before developing normal continence.
NURSING MANAGEMENT
Assessment: History: �Family history �General �Feeding habits (poor) �Fussiness �Irritability �Distended abdomen �Signs of under nutrition (pallor, muscle weakness, fatigue) �Bowel habits of the neonate or child �Frequency �Character of the bowel movement of stool �Onset of constipation (ribbon like, foul smelly) �Medical history �Clinical presentation
NURSING DIAGNOSIS �Fluid electrolyte imbalance �Impaired bowel pattern �imbalanced nutritional less than body requirement �Disturbed self body image related to the colostomy �Knowledge deficit of the parent related to the disease condition �Feeding modifications related to GI surgery �Abdominal distension related to obstruction
NURSING INTERVENTIONS Preoperative preparation �Informed consent �Consent to be taken from the parents of the infant or the legal guardians �Nutritional status: �A child who is malnourished may not be able to withstand the surgery until the physical status improves. �Low-fiber, high-calories & high protein diet is given �In severe cases of malnutrition, total parental nutrition can be given
NURSING INTERVENTIONS Psychological preparation �Explain the disease properly to the parents �Use charts, diagrams & models to explain the problem in the working of the bowel �Demonstrate pictorially the surgical procedure �Older child is to be prepared emotionally for a colostomy �Because the colostomy represents a change in the body function, the nurse should investigate the care giver’s previous knowledge of the procedure �Family members may have misconceptions regarding the colostomy. �Temporary colostomy also indicates that a future surgery will be done to close it. So the capabilities of the parent to afford it at that time need to be seen.
NURSING INTERVENTIONS Bowel preparation �No need to prepare bowel in newborn as the gut is sterile �Patient is kept on NG to administer Go. LYTELY to empty the bowel & to administration of systemic antibiotics & rectal irrigation �The rule of 8 -6 -4 -2 is followed that is nothing solid 8 hr before surgery, no formula 6 hr before surgery, no breastfeeding 4 hr before surgery & nothing at all 2 hr before surgery.
NURSING INTERVENTIONS Diet �The patient should have nothing by mouth before the operation. �Institute tube feeding or formula/breast milk once bowel function resumes. �High-fiber diets and diets containing fresh fruits and vegetables may optimize postoperative bowel function in certain patients.
NURSING INTERVENTIONS Ongoing management �Because progressive distension of the abdomen is a serious sign, abdominal circumference is measured with a paper tape measure at the largest diameter, usually at the level of the umbilicus. �The point of measurement is marked with pen to ensure its reliability
NURSING INTERVENTIONS Postoperative management: �The infant is given nothing by mouth & have NG tube to suction. �Intake & output, including NG tube lose & stool from the ostomy are measured. �To prevent contamination of the wound with urine of the baby, the diaper must be pinned below the dressing or urethral catheterization can be done. �IV fluids are given to maintain adequate hydration & electrolyte balance �An abdominal assessment, including monitoring of return of bowel sounds & passage of stool, will indicate when oral feeding can be started.
NURSING INTERVENTIONS Postoperative management : �Regular colostomy care to be done following aseptic guidelines. �Ongoing education of the older child & care givers regarding ostomy care begins with preparation for their discharge. �The nurse should explain the function of each piece of equipment, stressing features that permit the child to be safely moved & handled, such as length of tubing, use of arm boards & IV site & tape to secure NG tube to the nose. �Parents should be encouraged & assisted in holding & comforting their child. �Involve the child & the parents in the dressing change, as this will increase their confidence & will also help in the acceptance of the ostomy by the child & parents
NURSING INTERVENTIONS Postoperative management: �Explain them about the procedure of skin care & change of appliance & the frequency of care, control of order, sign of complications (ribbon like stool, excessive diarrhea, bleeding, prolapsed, failure to pass flatus or stool) �If enterostomal therapist is available, then refer the parents to him for expert assistance in planning home care �Sometimes families require financial assistance & additional psychological support. So refer the parents to social worker �A referral to home health care agency for home nursing visits can meet the need of additional supervision of care, reinforcement of child & parent’s education & support.
NURSING INTERVENTIONS Activity �Limit physical activity for about 6 weeks to allow the wound to heal properly (applies more to older children). Follow-up Further Inpatient Care �If a diverting colostomy is created in a newborn, he or she must remain in the hospital until the ostomy is functioning and feeding goals are obtained. Feedings are usually initiated 24 -48 hours after the creation of the colostomy. �After the definitive pull-through procedure is performed, the patient is hospitalized until full feedings are possible and evidence of the return of bowel function is obtained. Patients are to take nothing by mouth, with intravenous fluid hydration until they pass flatus or have a bowel movement. Once this occurs, clear liquids may be started, and the diet may be advanced until feeding goals are obtained. Intravenous antibiotics are also continued until evidence of proper bowel function is observed.
NURSING INTERVENTIONS Further Outpatient Care �After a definitive pull-through procedure is performed, normal growth and development should ensue. �Patients should be monitored for normal bowel habits. Patients with no other underlying disorders and no postoperative complications should develop normal bowel habits. However, such habits may not develop until the patient is older.