Care of Chest tubes Closed Chest Drainage System
Care of Chest tubes Closed Chest Drainage System VN 255 1
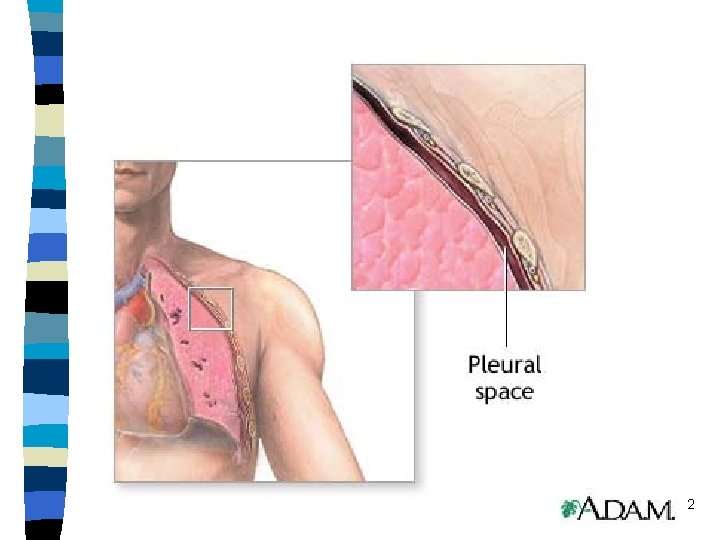
2
Thora-centesis: “chest-puncture ” n Insertion of a needle into the pleural space to aspirate fluid (pleural effusion=fluid trapped pleural space) aspirate/or drain fluid, blood, air, or to inject medication. May be for (diagnosticreasons), or for therapeutic reasons to “reduce respiratory distress” n If a continuous drainage is required use a chest drainage system like a “Pleur-Evac” closed chest drainage system. 3
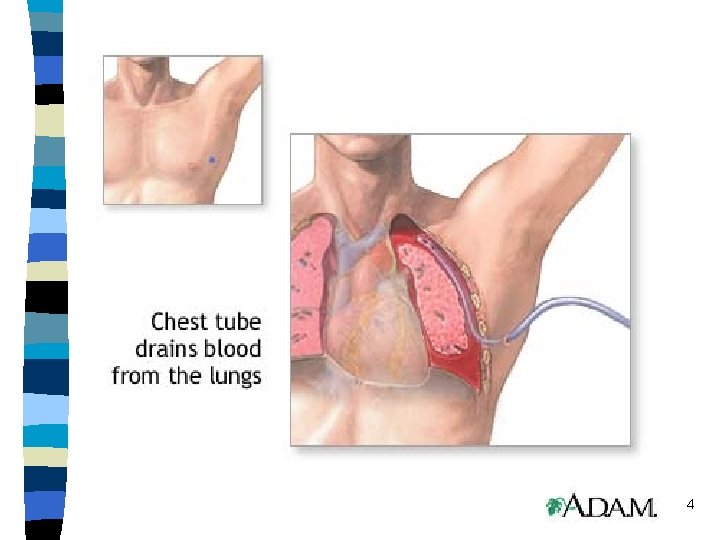
4
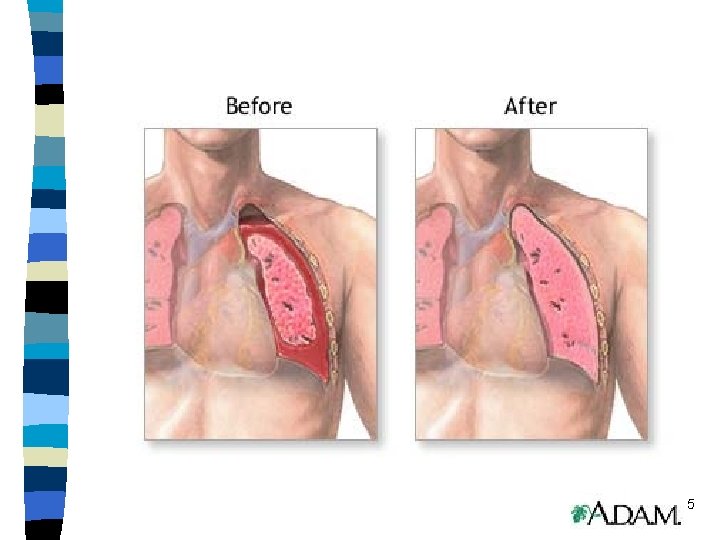
5
Thoracentesis: n After this procedure: Physician applies petroleum-jelly based gauze over the insertion site and forms a tight occlusive dressing. Monitor VS, changes in respirations/SOB and a CXR post procedure to be sure the lung was not punctured during the procedure causing a “pneumo-thorax” or collection of air or gas trapped in pleural space=lungs to collapse! 6
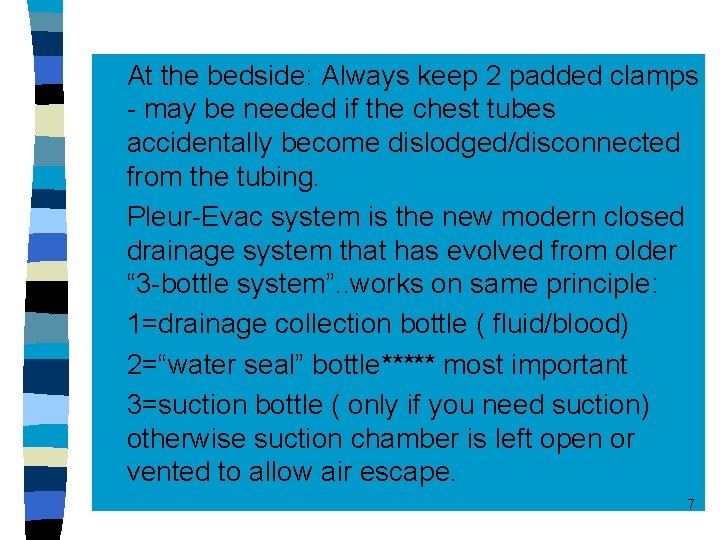
n n n At the bedside: Always keep 2 padded clamps - may be needed if the chest tubes accidentally become dislodged/disconnected from the tubing. Pleur-Evac system is the new modern closed drainage system that has evolved from older “ 3 -bottle system”. . works on same principle: 1=drainage collection bottle ( fluid/blood) 2=“water seal” bottle***** most important 3=suction bottle ( only if you need suction) otherwise suction chamber is left open or vented to allow air escape. 7

Closed-chest drainage system 8
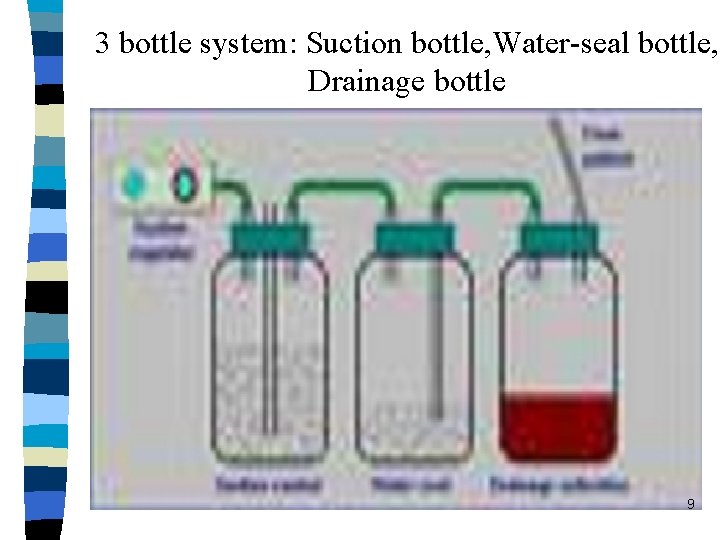
3 bottle system: Suction bottle, Water-seal bottle, Drainage bottle 9
10
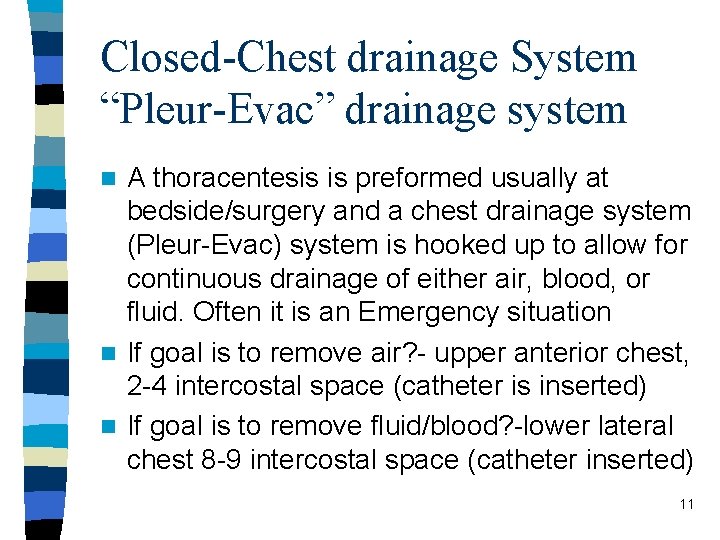
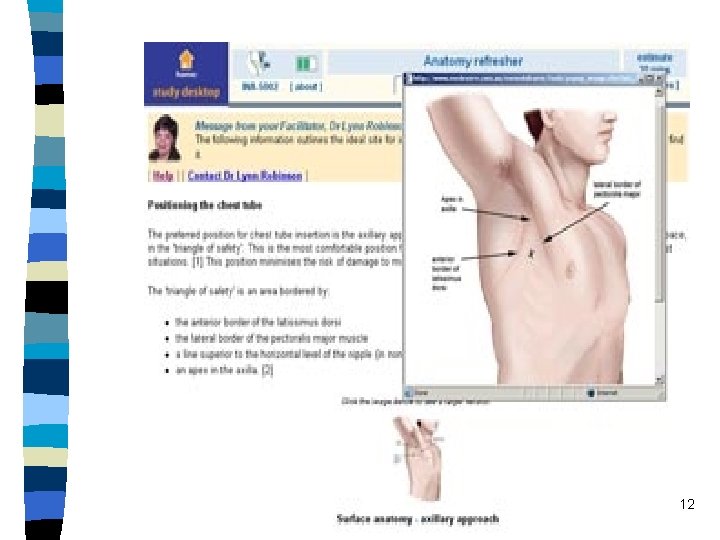
Closed-Chest drainage System “Pleur-Evac” drainage system A thoracentesis is preformed usually at bedside/surgery and a chest drainage system (Pleur-Evac) system is hooked up to allow for continuous drainage of either air, blood, or fluid. Often it is an Emergency situation n If goal is to remove air? - upper anterior chest, 2 -4 intercostal space (catheter is inserted) n If goal is to remove fluid/blood? -lower lateral chest 8 -9 intercostal space (catheter inserted) n 11
12
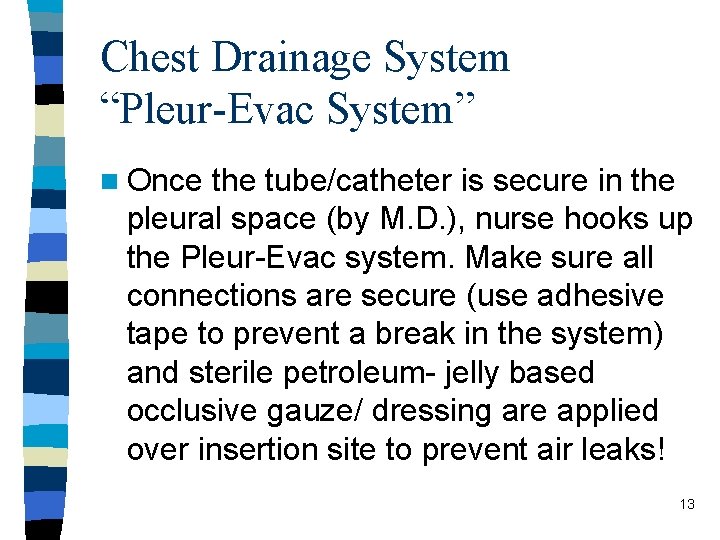
Chest Drainage System “Pleur-Evac System” n Once the tube/catheter is secure in the pleural space (by M. D. ), nurse hooks up the Pleur-Evac system. Make sure all connections are secure (use adhesive tape to prevent a break in the system) and sterile petroleum- jelly based occlusive gauze/ dressing are applied over insertion site to prevent air leaks! 13
Closed Chest Drainage System “Pleur-Evac chest drainage system The whole system is based on maintaining a “Negative intra-thoracic pressure” so we need a water seal bottle/chamber ( bottle # 2) n Each time client exhales=air is trapped in pleural space and it travels down the chest tube to water seal bottle/chamber under water and then bubbles up and out of the bottle! The water acts as a seal allowing air to escape from pleural space but preventing air from getting back into the lungs via negative pressure of inspiration! n 14
Water seal bottle/chamber The water level in the water seal bottle/chamber will fluctuate gently up and down with each inspiration/expiration. This is called “tidaling” n Only time tidaling should stop is 1. = when the lung is “re-inflated” and no longer requires a chest tube or n 2. = if a problem occurs with the tubing (kinked, occlusion, breaks in the system) and should be checked ASAP! n 3. =If constant or vigorous “bubbling” occur please check for a “leak” something is wrong 15 n
Closed Chest Drainage System Suction bottle/chamber (bottle #3) used to speedily re-inflate the lungs. Water is added to the bottle/chamber. Suction is applied. (the force of suction is solely dependent on amount of water in bottle not the amount of suction set on suction machine. If water evaporates=add more water to prescribed level of water. n See gentle bubbling in suction bottle n If vigorous bubbling=suction will not be maintained; did the water evaporate? Add prescribed amount. n If suction not used: chamber is then left open to allow air to escape. n 16
Closed Chest Drainage System: Drainage/Collection bottle/chamber (#1) n Only used if drain fluid/blood pleural space. (pleural effusion, chest trauma, surgery). Drainage chamber is not emptied but just marked amount every shift on the bottle/chamber. n Report any marked increases in bloody drainage/fluid. Recorded as “Output” n Often when chamber is full; RN/M. D. will change out the closed chest drainage system (Pleur-Evac) with a new one. n 17

18

19
Closed Chest Drainage System General guidelines: n Check system for any breaks, cracks, kinks in tubing, or broken connections n n Auscultate lung sounds, any sudden SOB, dyspnea, pain, hear any “crepitous sounds= think …SQ emphysema? ” hear & palpate for leakage of air into SQ tissue Tight occlusive dressing intact? Clamps at bedside? n No dependent loops tubing? Is the drainage system below chest level? n Check water seal chamber and or suction chamber for the correct amount of water in chambers? Any vigorous bubbling? leaks? n Record drainage as output n 20
Closed drainage system If client must be transported: suction is usually off and air is vented out. Tubing is not clamped for transport! n If a tube accidentally pulls out=quickly place a tight occlusive dressing over the insertion site on the chest to prevent air from reentering…follow hospital policy n Process of “Milking and Stripping” tubes is controversial…follow hospital policy n If time to D/C’d the Chest tube/closed drainage system= M. D. pulls tube out and tight occlusive petroleum-jelly based gauze is applied over insertion site: CXR done (check for pneumothorax d/t a puncture lung? ), Monitor respirations & for crepitous? n 21
- Slides: 21