Cardiovascular System The Heart 1 Functions of the
- Slides: 38
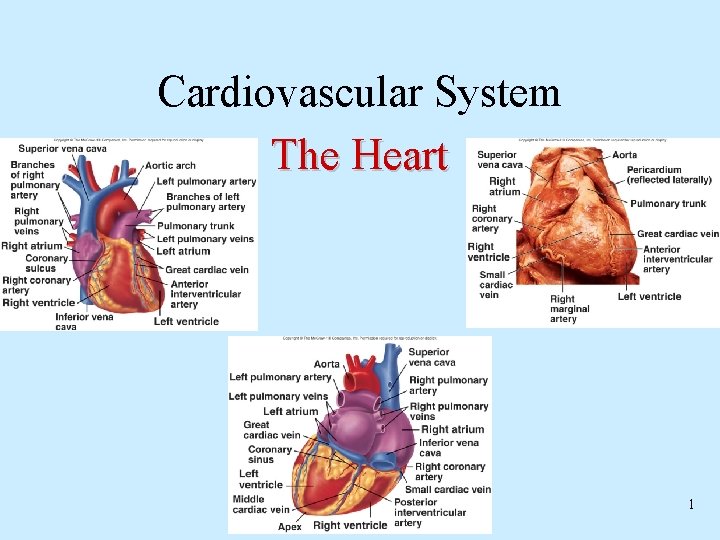
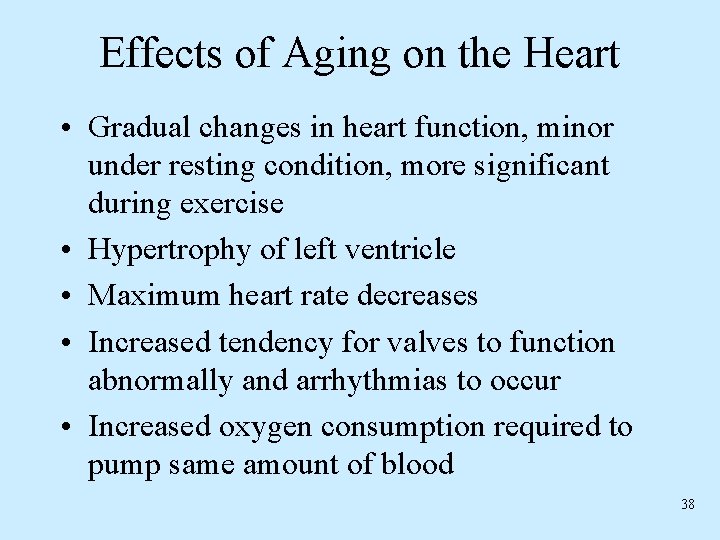
Cardiovascular System The Heart 1
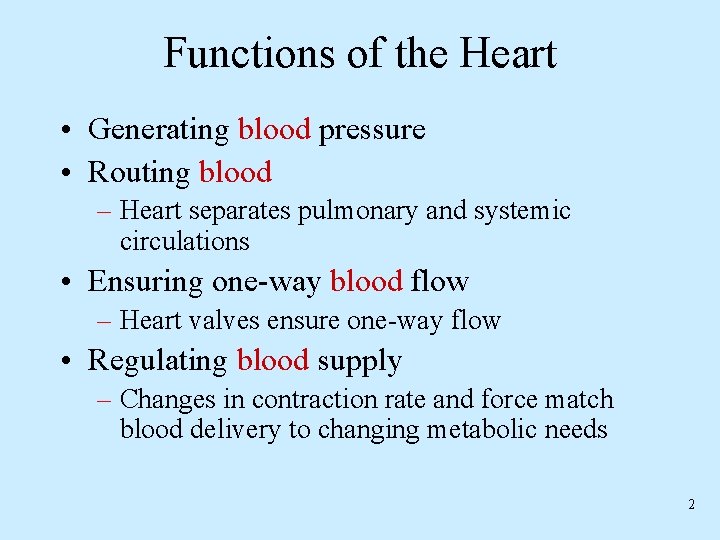
Functions of the Heart • Generating blood pressure • Routing blood – Heart separates pulmonary and systemic circulations • Ensuring one-way blood flow – Heart valves ensure one-way flow • Regulating blood supply – Changes in contraction rate and force match blood delivery to changing metabolic needs 2
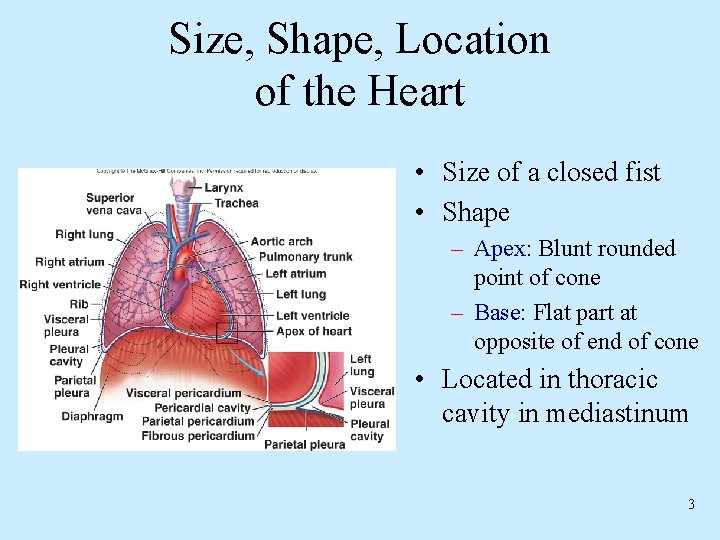
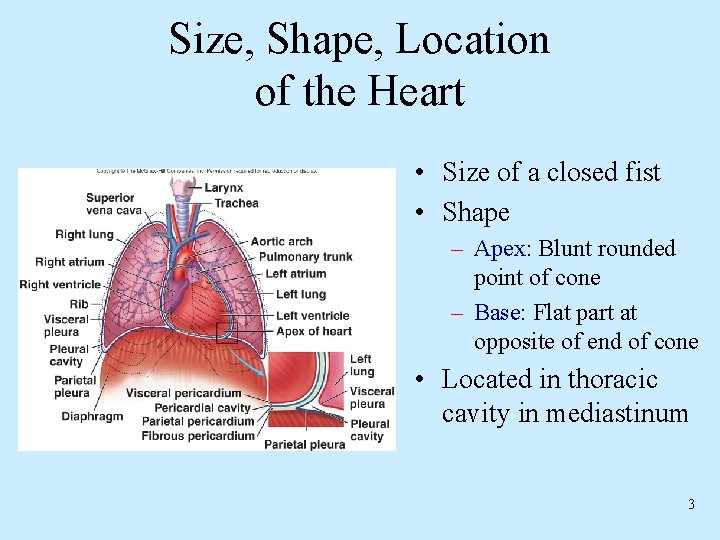
Size, Shape, Location of the Heart • Size of a closed fist • Shape – Apex: Blunt rounded point of cone – Base: Flat part at opposite of end of cone • Located in thoracic cavity in mediastinum 3
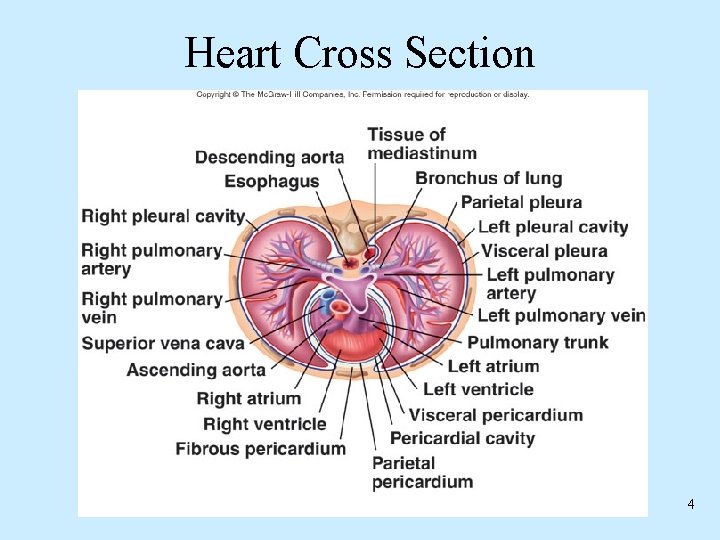
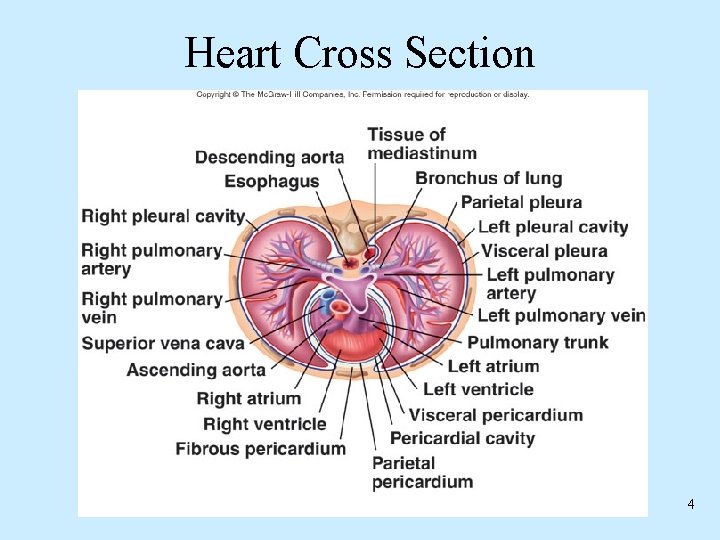
Heart Cross Section 4
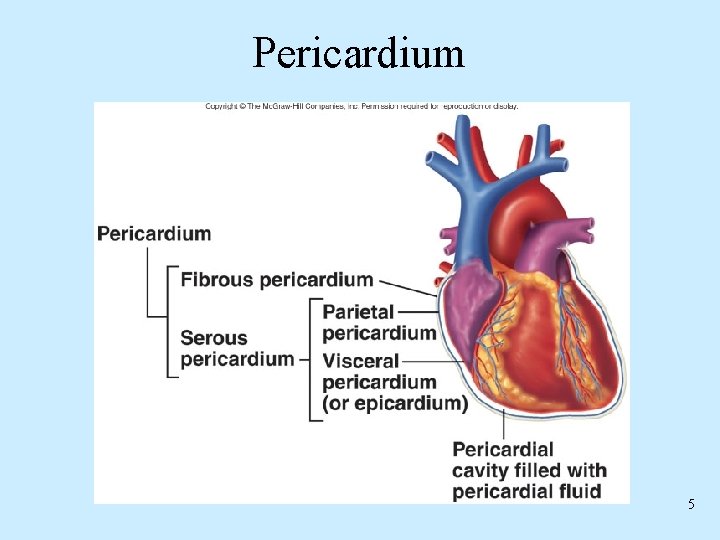
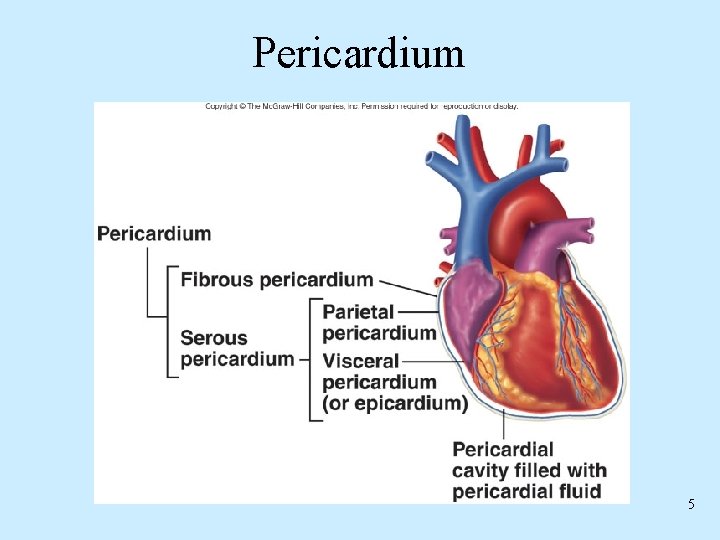
Pericardium 5
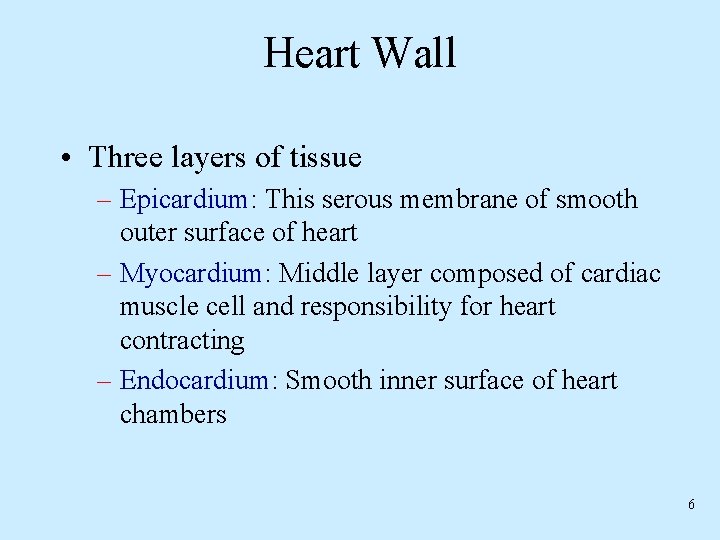
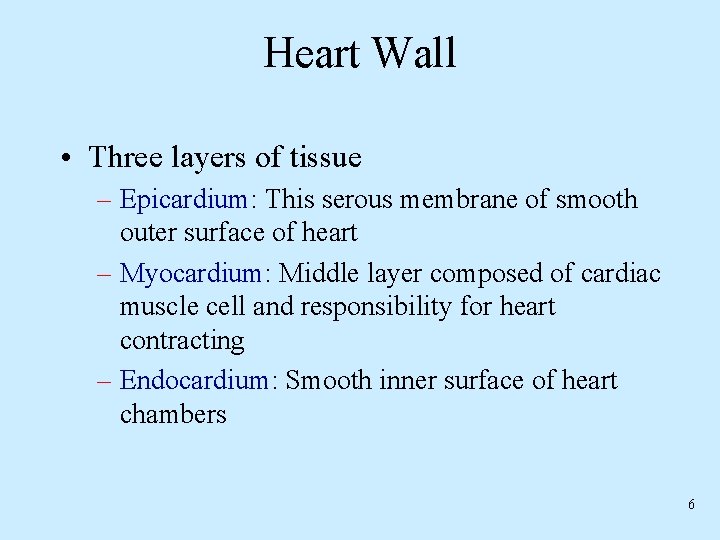
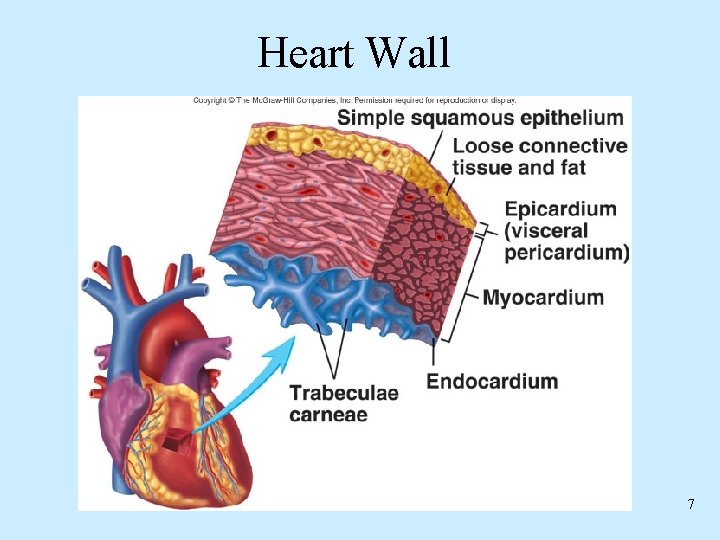
Heart Wall • Three layers of tissue – Epicardium: This serous membrane of smooth outer surface of heart – Myocardium: Middle layer composed of cardiac muscle cell and responsibility for heart contracting – Endocardium: Smooth inner surface of heart chambers 6
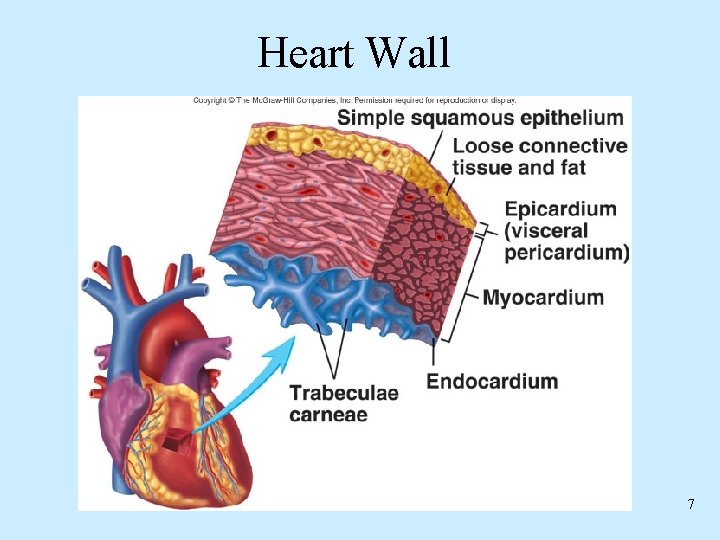
Heart Wall 7
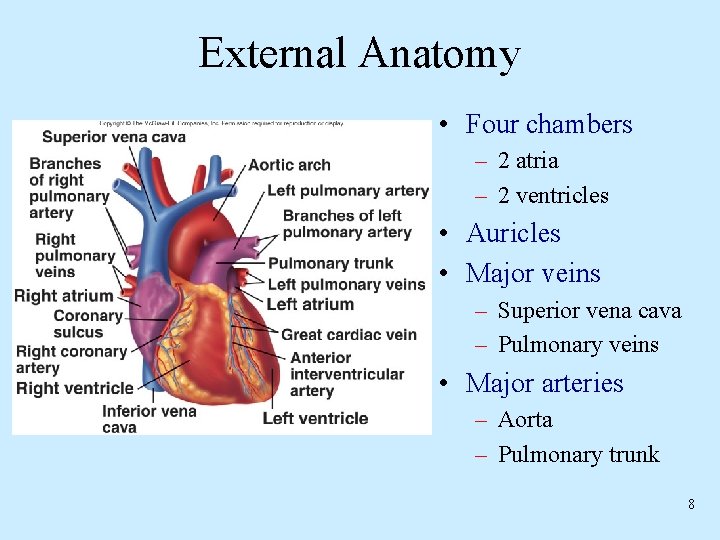
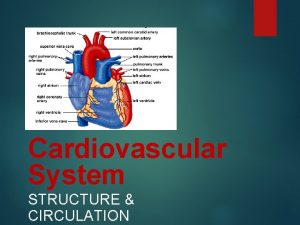
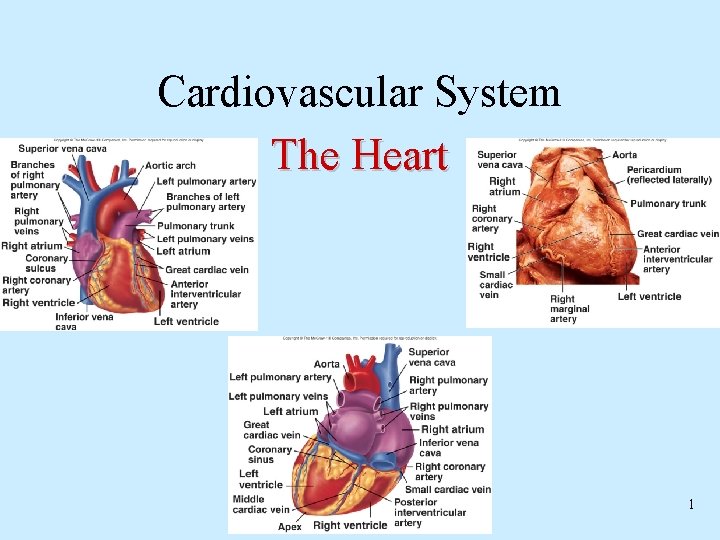
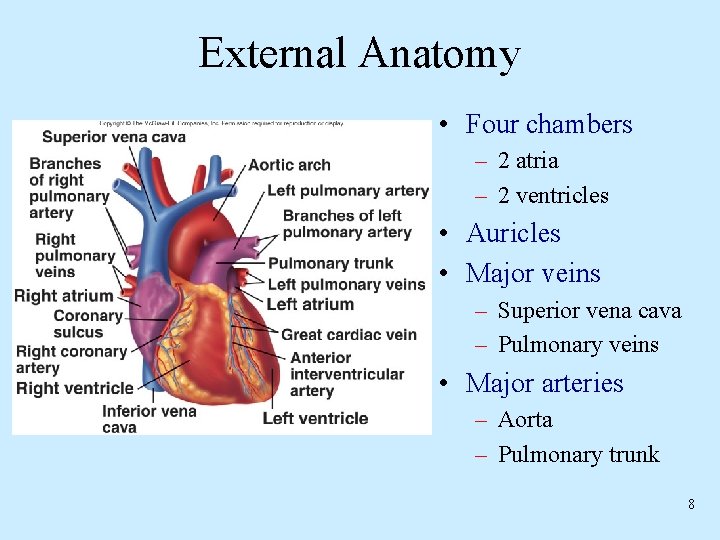
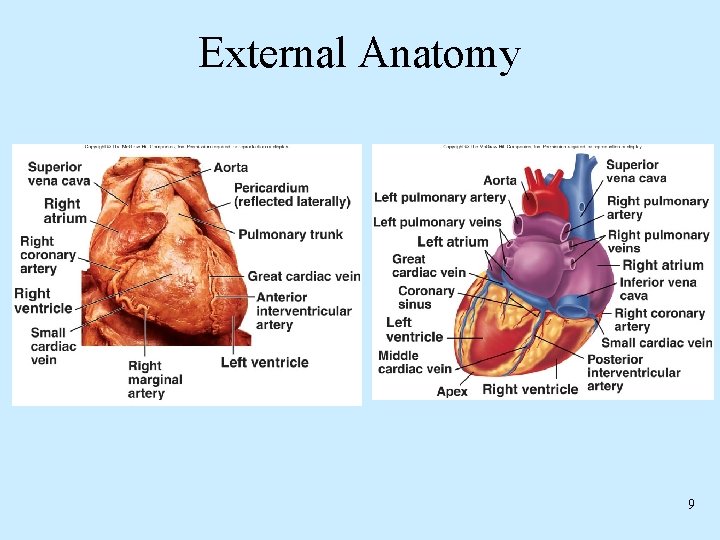
External Anatomy • Four chambers – 2 atria – 2 ventricles • Auricles • Major veins – Superior vena cava – Pulmonary veins • Major arteries – Aorta – Pulmonary trunk 8
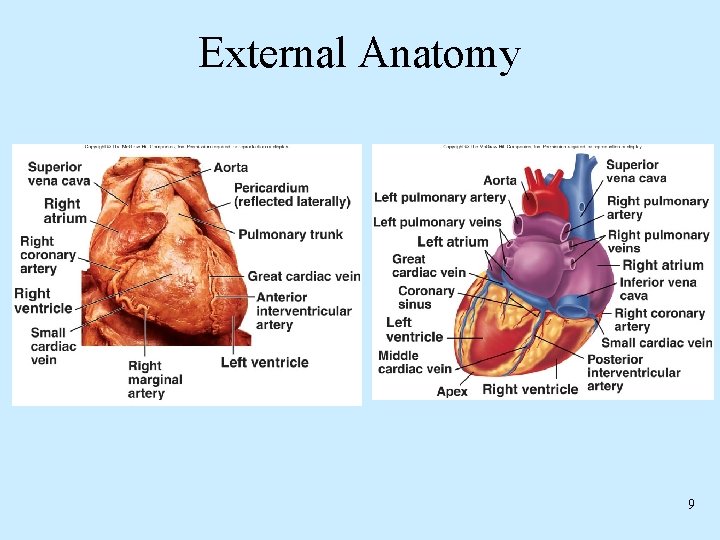
External Anatomy 9
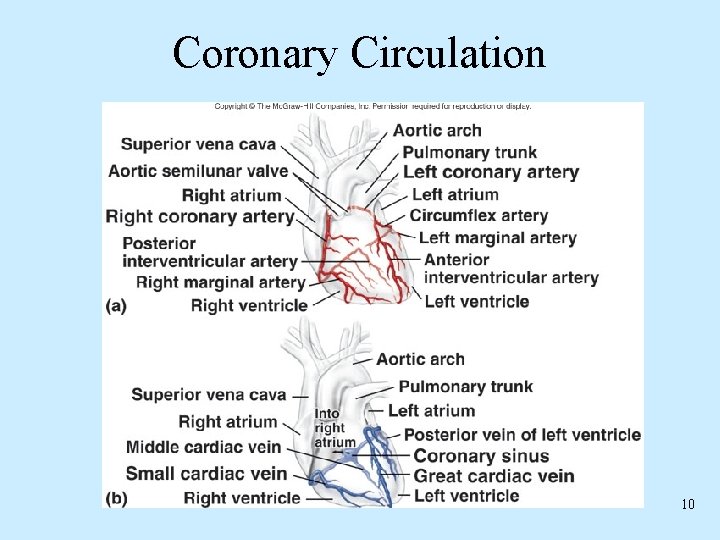
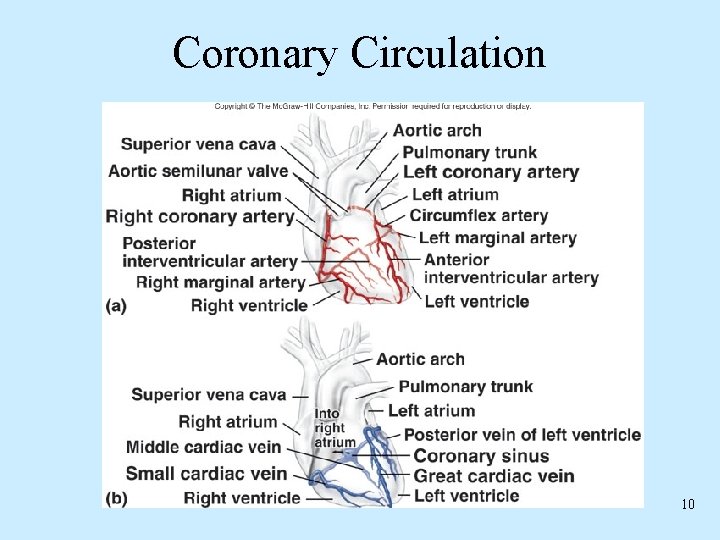
Coronary Circulation 10
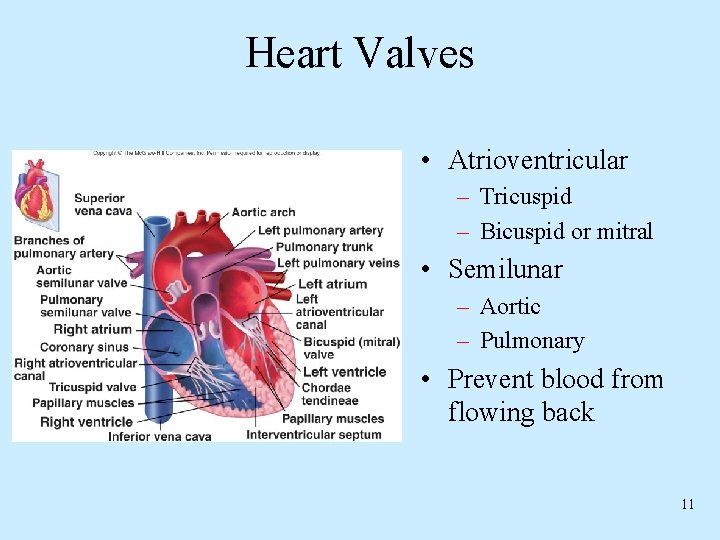
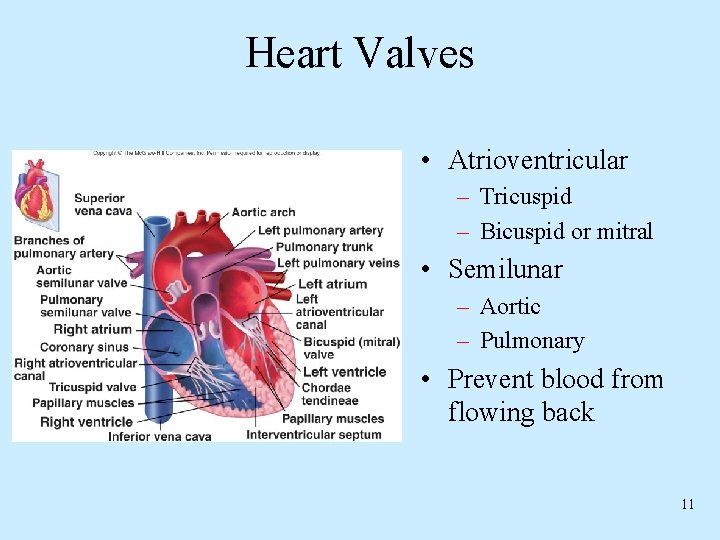
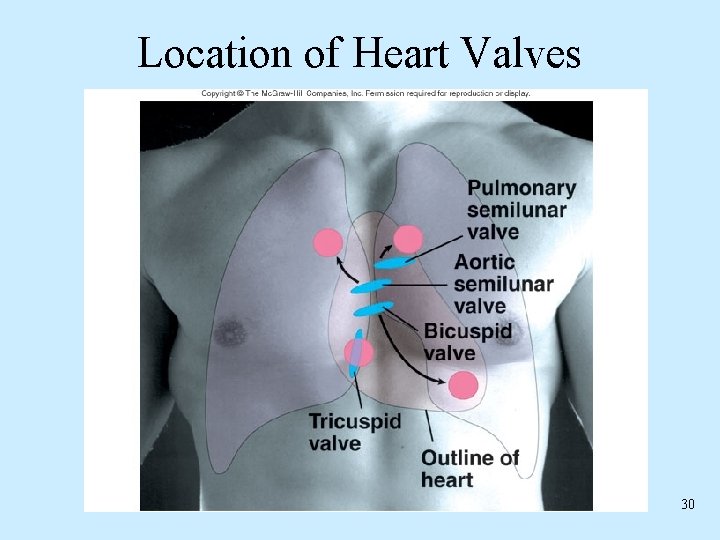
Heart Valves • Atrioventricular – Tricuspid – Bicuspid or mitral • Semilunar – Aortic – Pulmonary • Prevent blood from flowing back 11
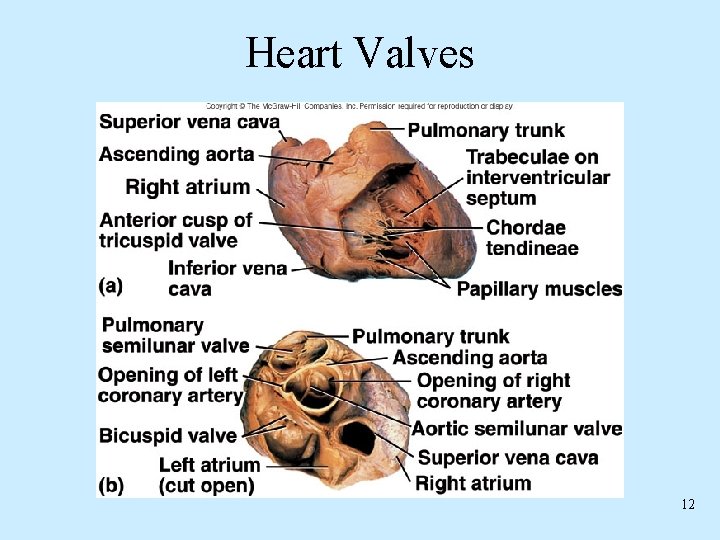
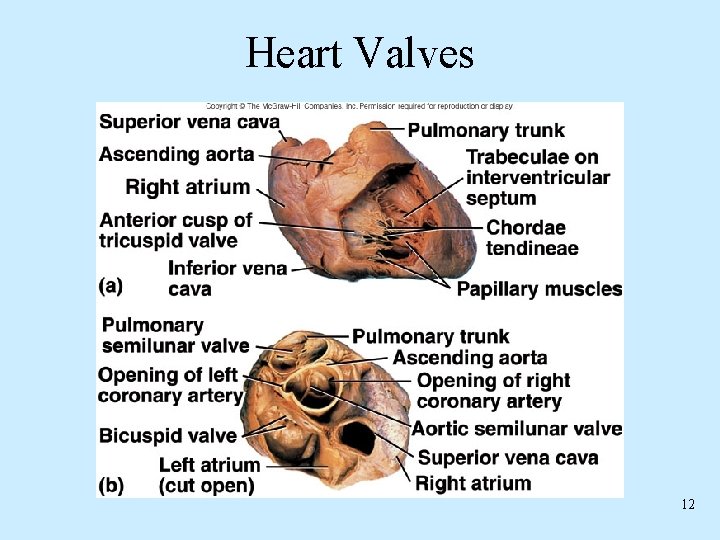
Heart Valves 12
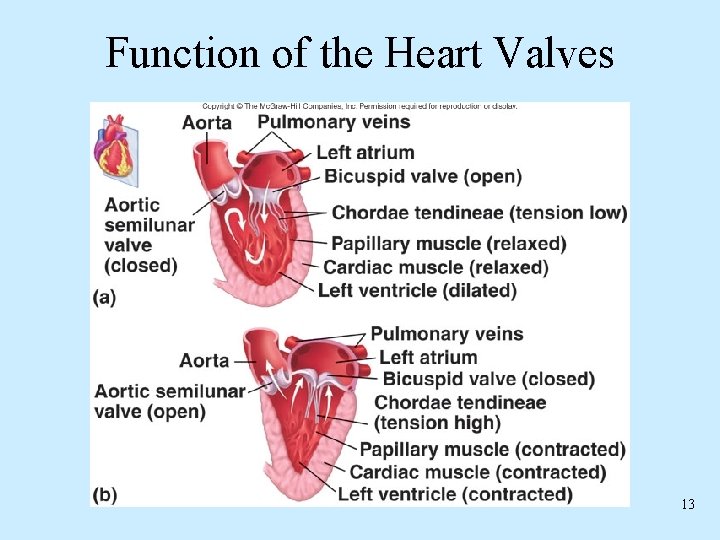
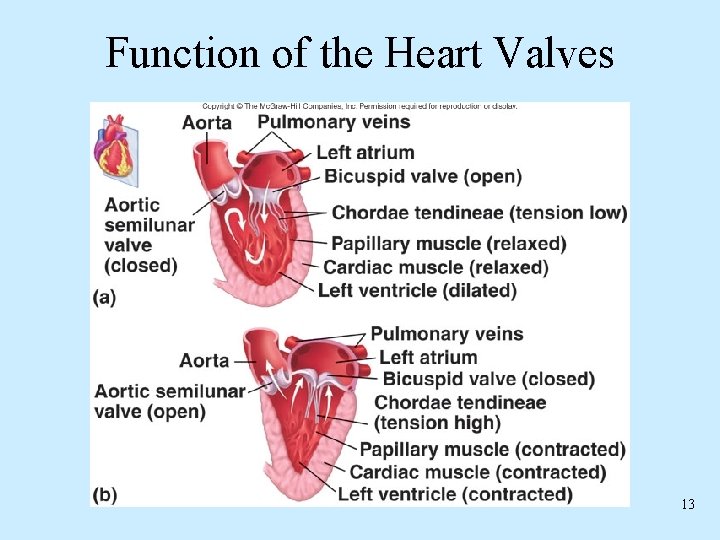
Function of the Heart Valves 13
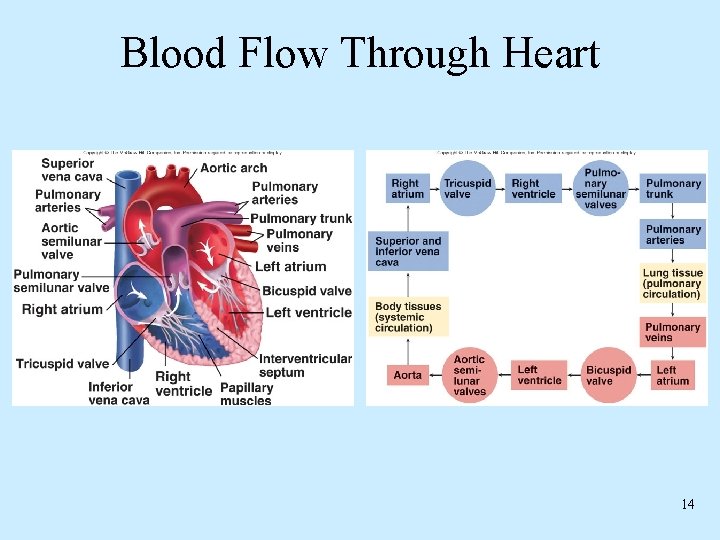
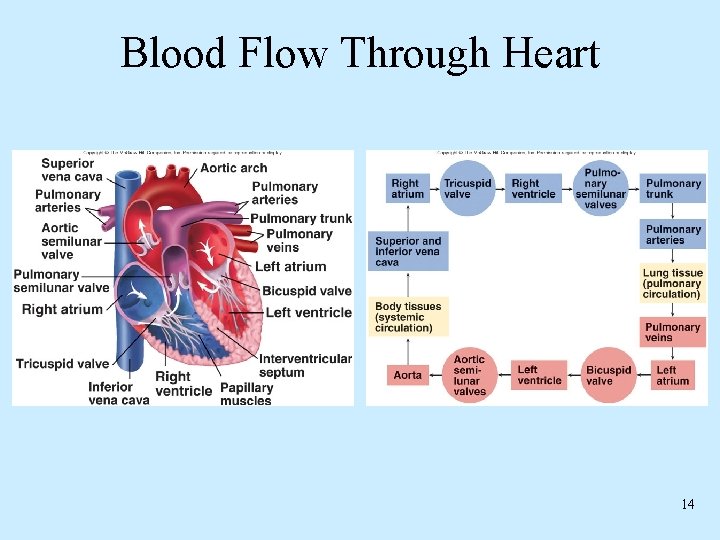
Blood Flow Through Heart 14
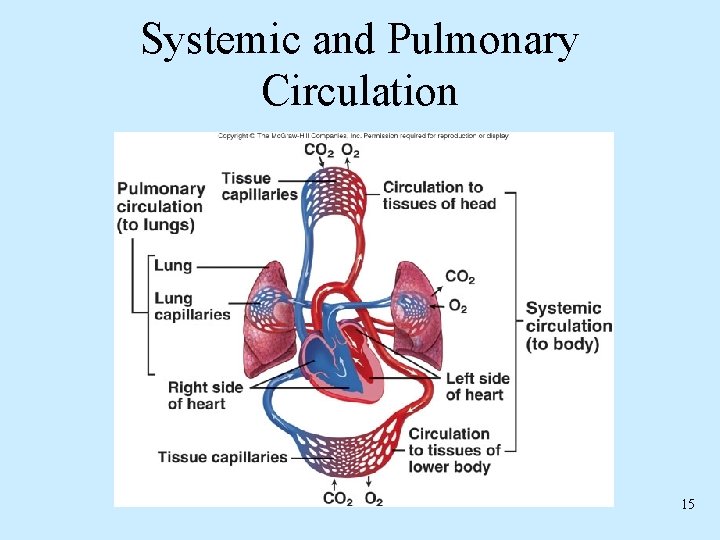
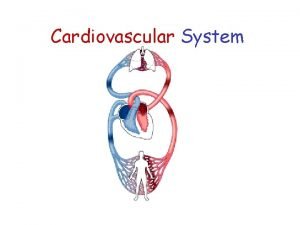
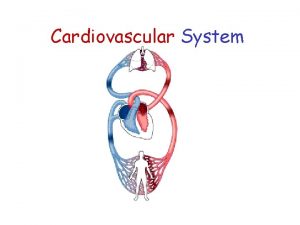
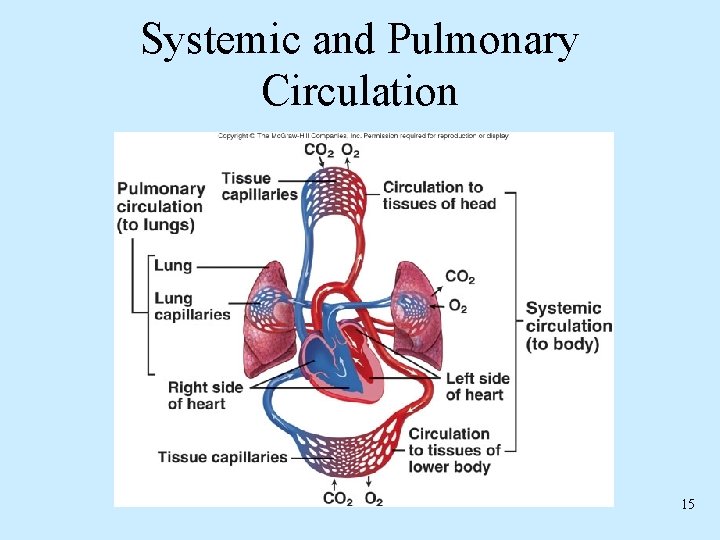
Systemic and Pulmonary Circulation 15
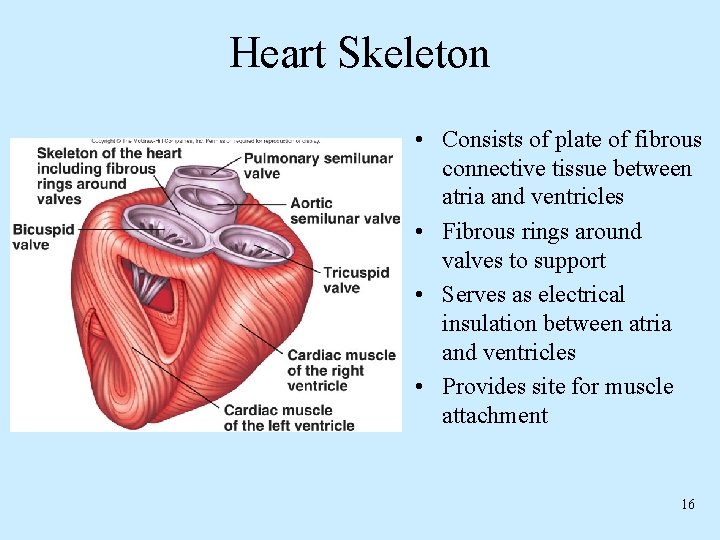
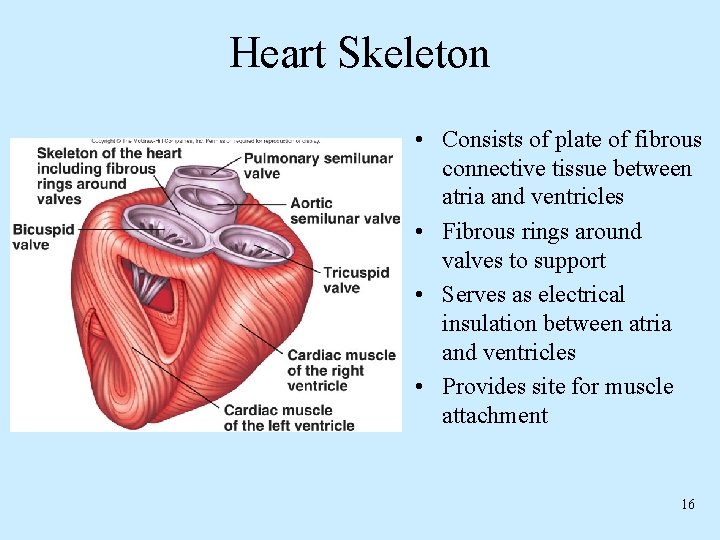
Heart Skeleton • Consists of plate of fibrous connective tissue between atria and ventricles • Fibrous rings around valves to support • Serves as electrical insulation between atria and ventricles • Provides site for muscle attachment 16
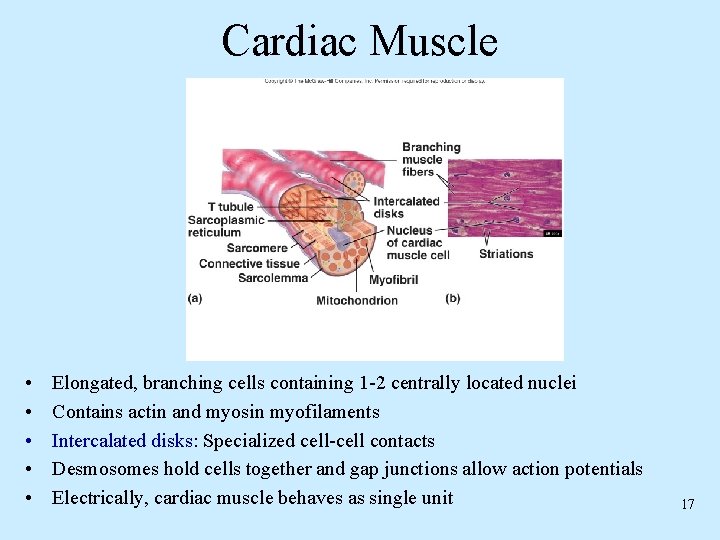
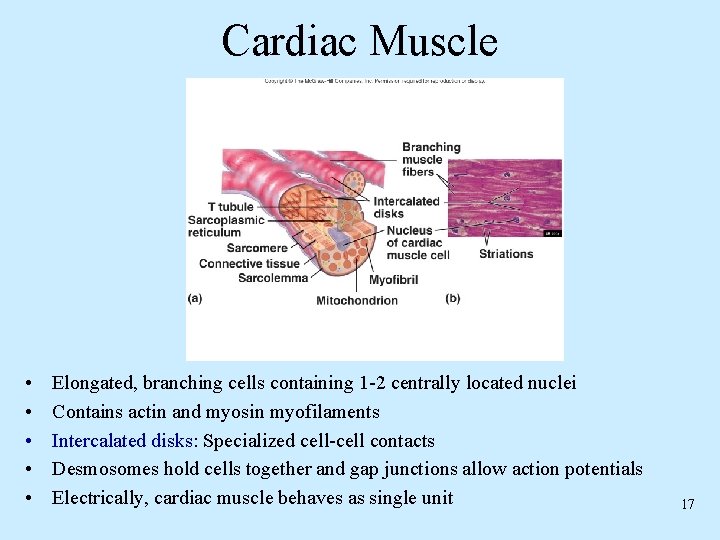
Cardiac Muscle • • • Elongated, branching cells containing 1 -2 centrally located nuclei Contains actin and myosin myofilaments Intercalated disks: Specialized cell-cell contacts Desmosomes hold cells together and gap junctions allow action potentials Electrically, cardiac muscle behaves as single unit 17
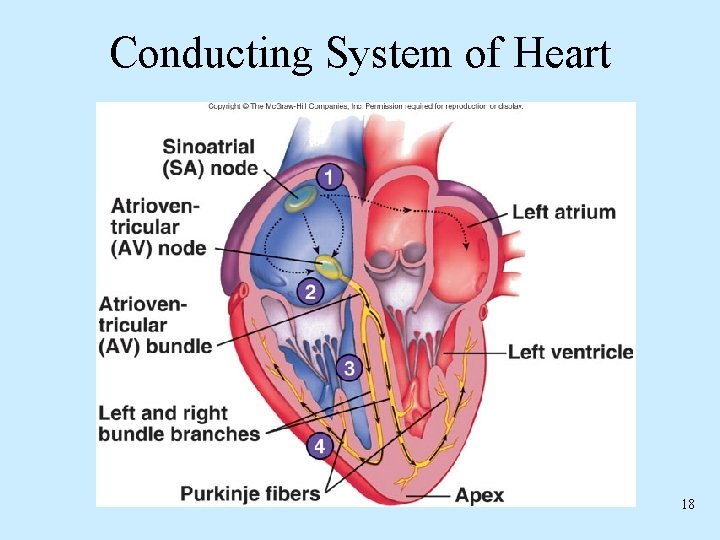
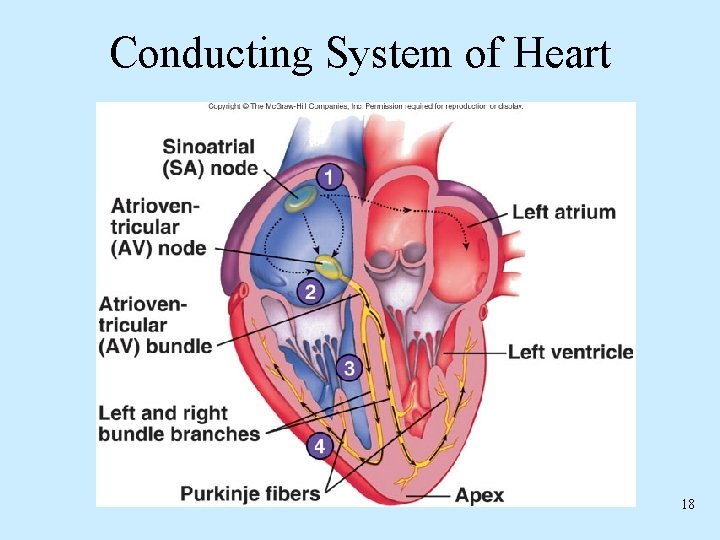
Conducting System of Heart 18
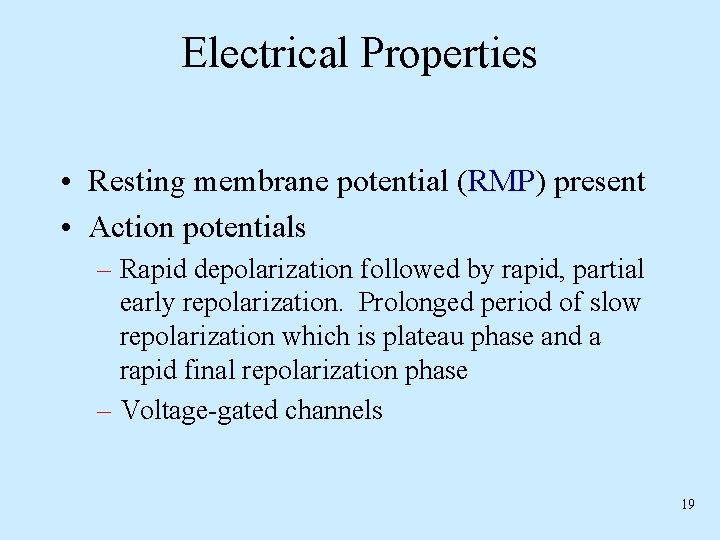
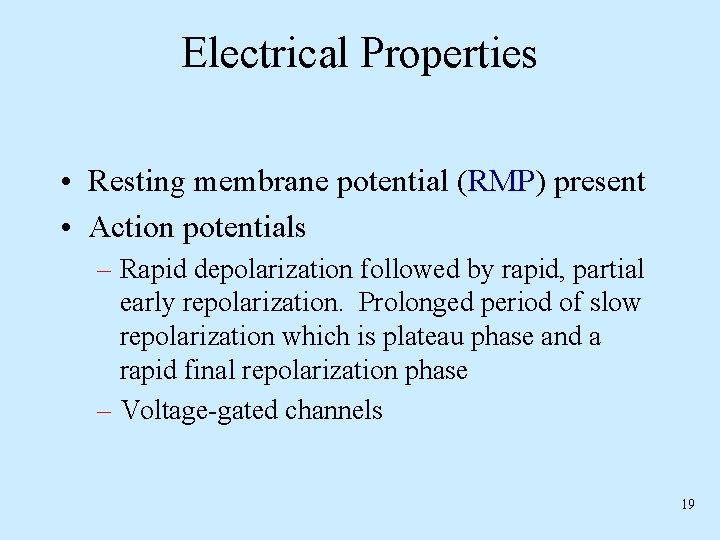
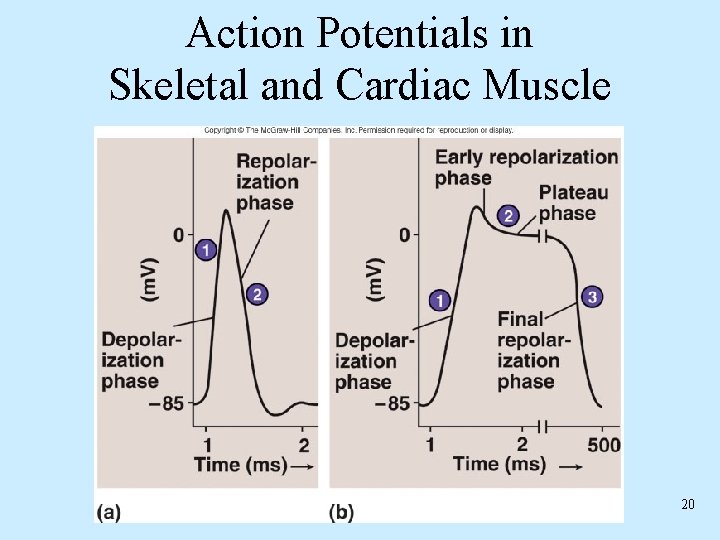
Electrical Properties • Resting membrane potential (RMP) present • Action potentials – Rapid depolarization followed by rapid, partial early repolarization. Prolonged period of slow repolarization which is plateau phase and a rapid final repolarization phase – Voltage-gated channels 19
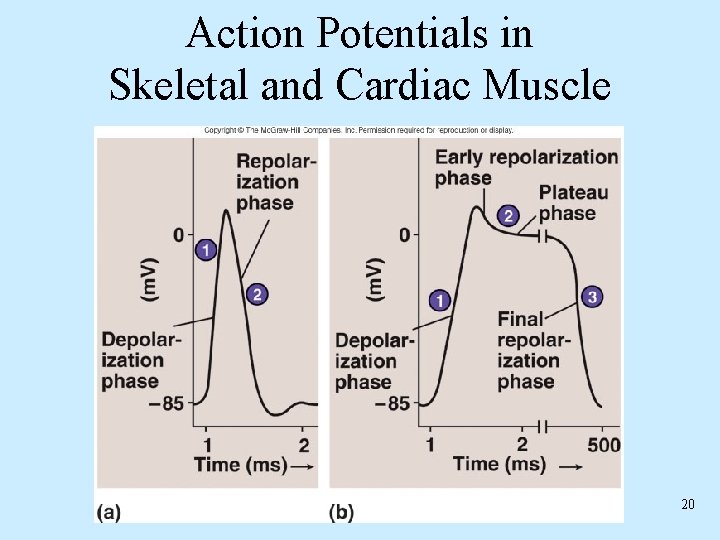
Action Potentials in Skeletal and Cardiac Muscle 20
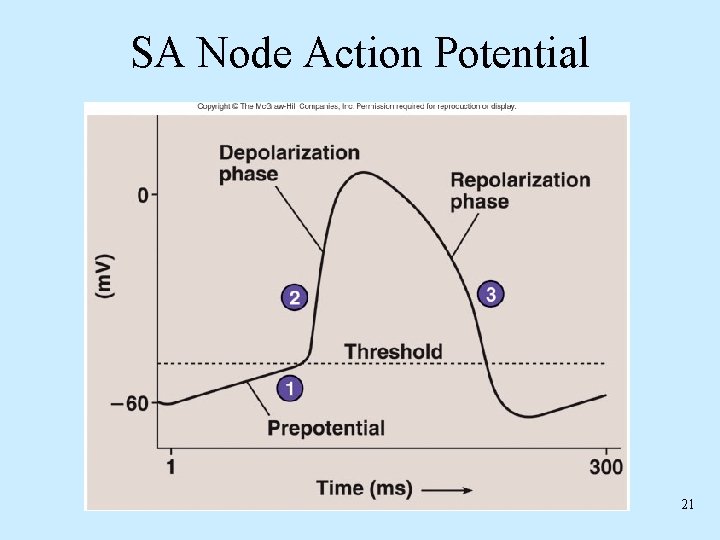
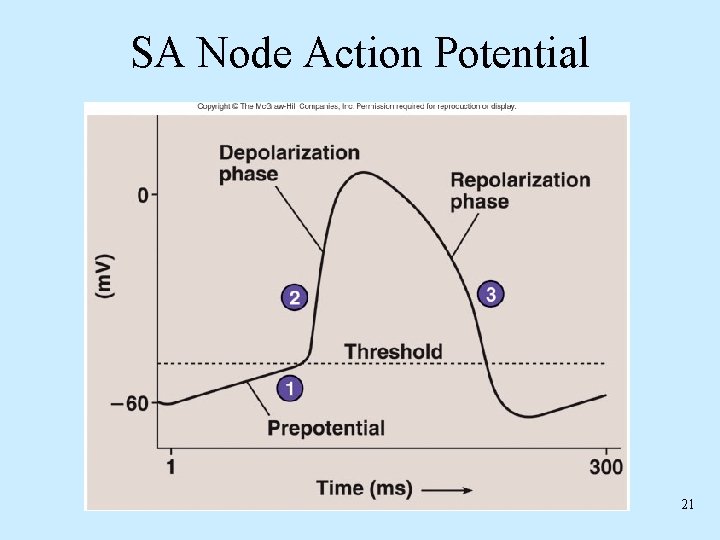
SA Node Action Potential 21
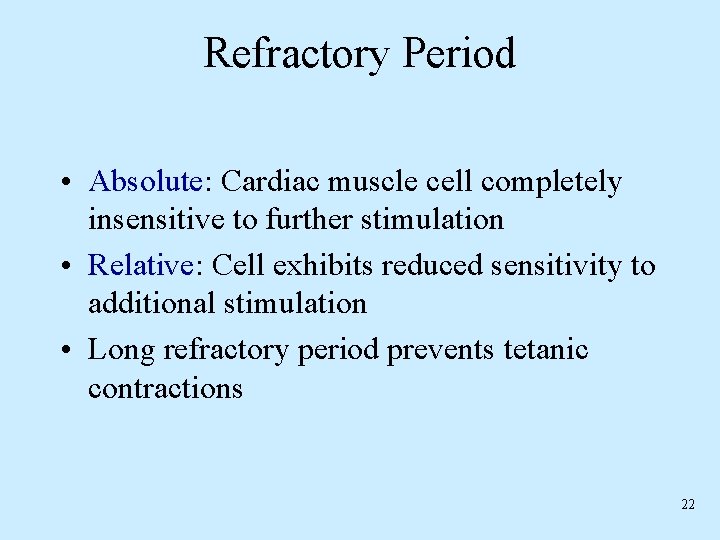
Refractory Period • Absolute: Cardiac muscle cell completely insensitive to further stimulation • Relative: Cell exhibits reduced sensitivity to additional stimulation • Long refractory period prevents tetanic contractions 22
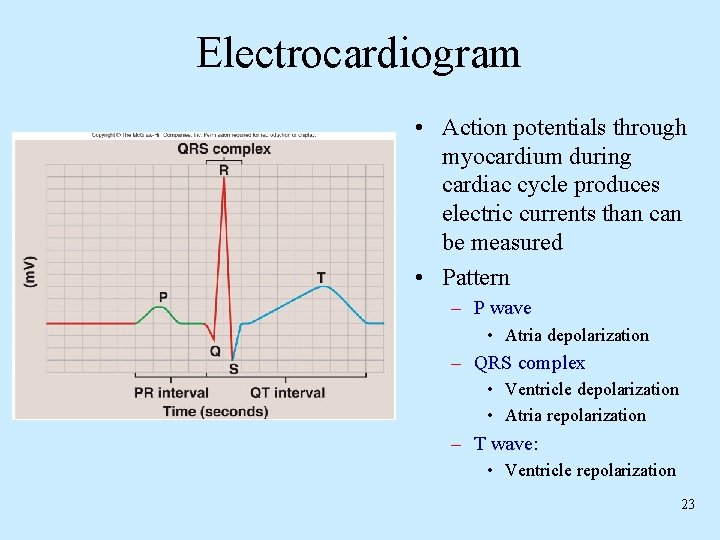
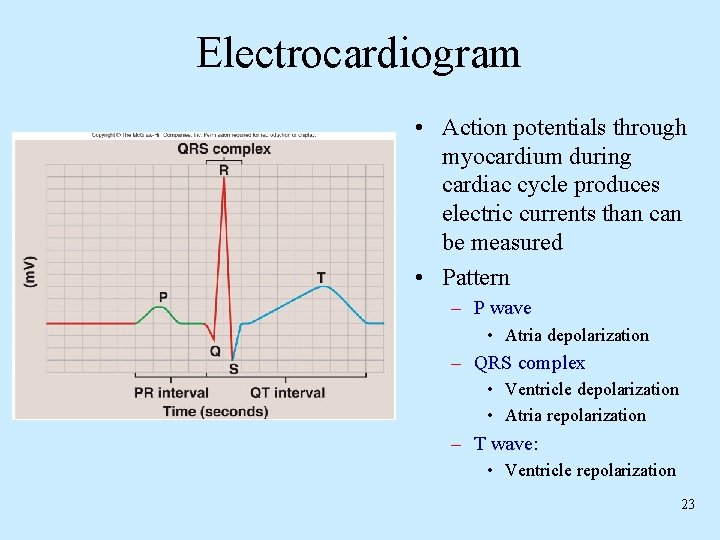
Electrocardiogram • Action potentials through myocardium during cardiac cycle produces electric currents than can be measured • Pattern – P wave • Atria depolarization – QRS complex • Ventricle depolarization • Atria repolarization – T wave: • Ventricle repolarization 23
Cardiac Arrhythmias • Tachycardia: Heart rate in excess of 100 bpm • Bradycardia: Heart rate less than 60 bpm • Sinus arrhythmia: Heart rate varies 5% during respiratory cycle and up to 30% during deep respiration • Premature atrial contractions: Occasional shortened intervals between one contraction and succeeding, frequently occurs in healthy people 24
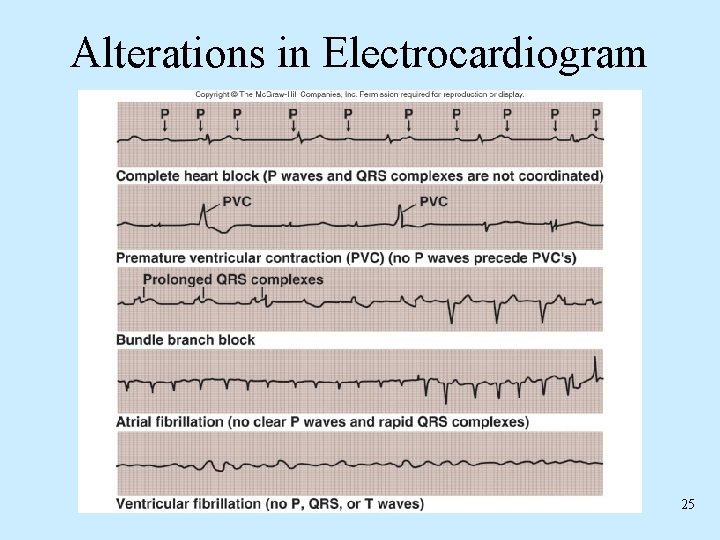
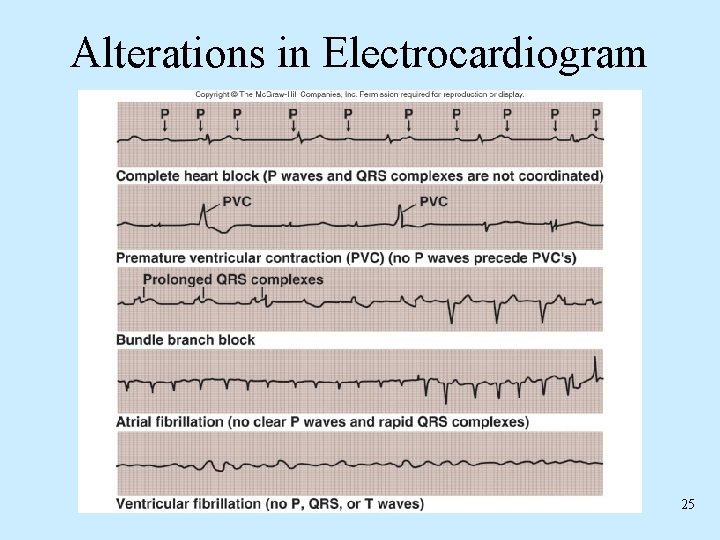
Alterations in Electrocardiogram 25
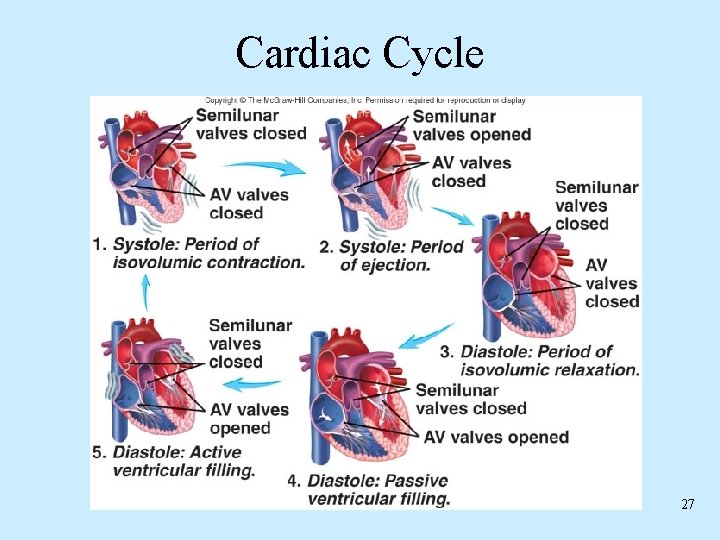
Cardiac Cycle • Heart is two pumps that work together, right and left half • Repetitive contraction (systole) and relaxation (diastole) of heart chambers • Blood moves through circulatory system from areas of higher to lower pressure. – Contraction of heart produces the pressure 26
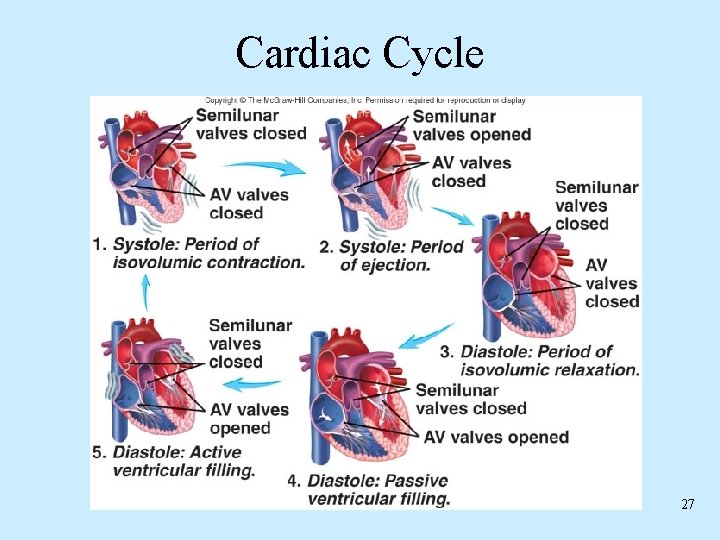
Cardiac Cycle 27
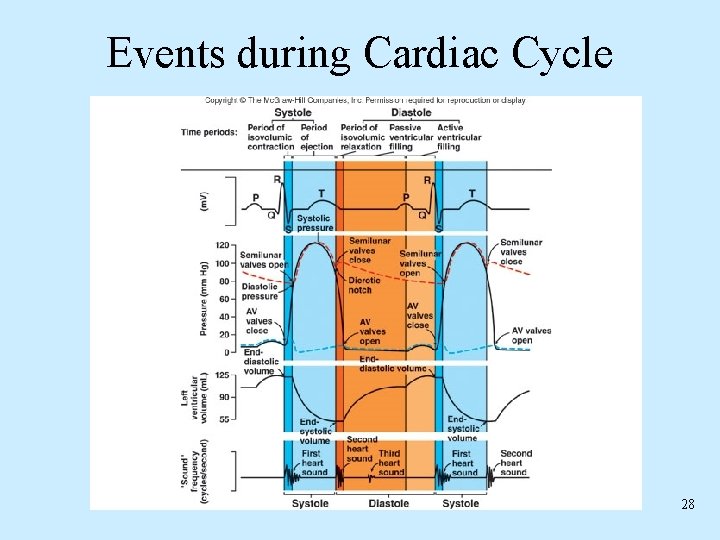
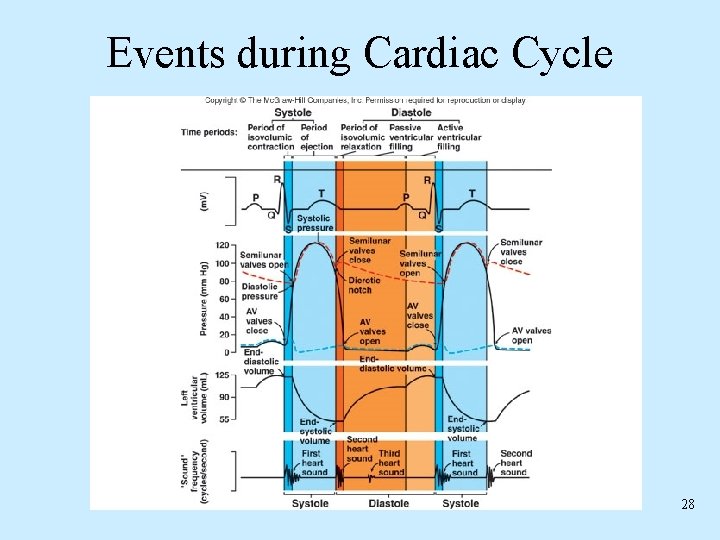
Events during Cardiac Cycle 28
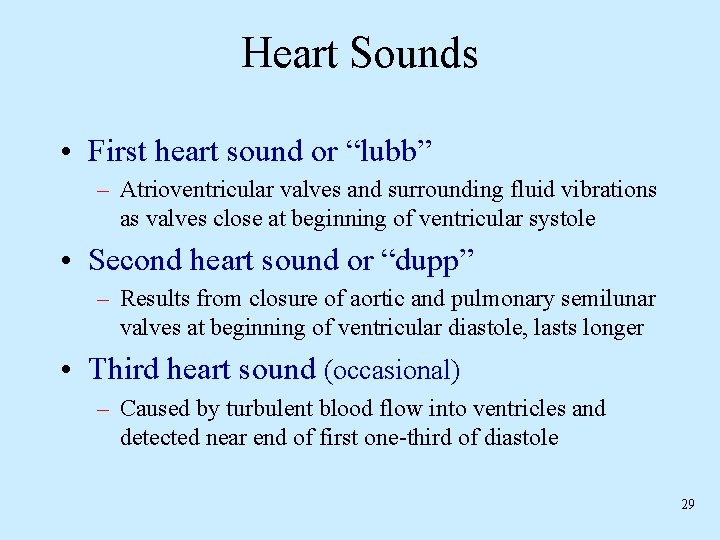
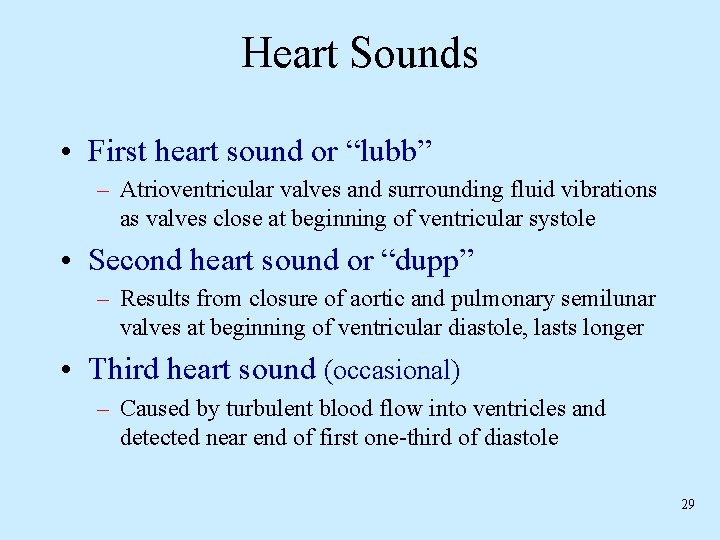
Heart Sounds • First heart sound or “lubb” – Atrioventricular valves and surrounding fluid vibrations as valves close at beginning of ventricular systole • Second heart sound or “dupp” – Results from closure of aortic and pulmonary semilunar valves at beginning of ventricular diastole, lasts longer • Third heart sound (occasional) – Caused by turbulent blood flow into ventricles and detected near end of first one-third of diastole 29
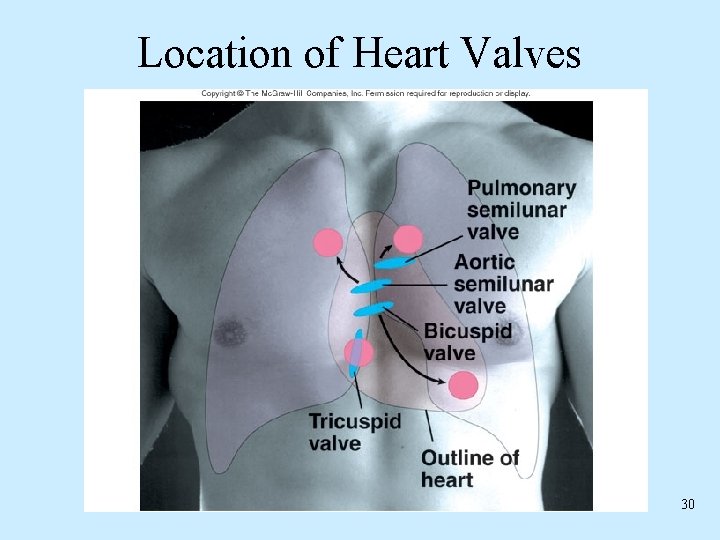
Location of Heart Valves 30
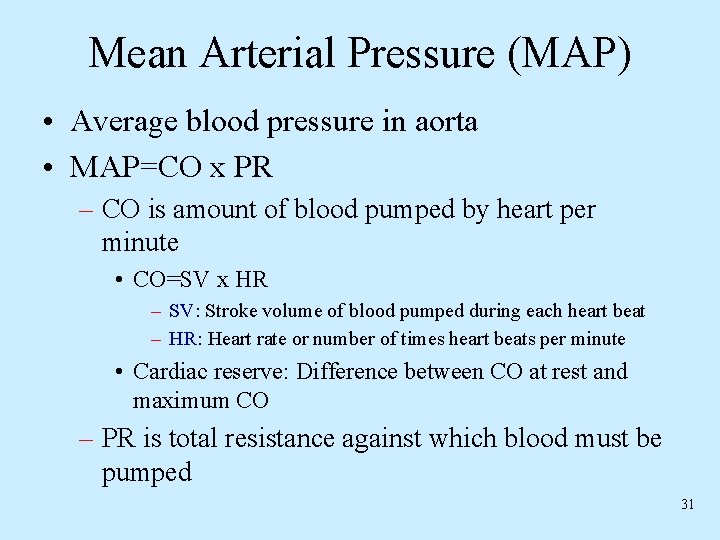
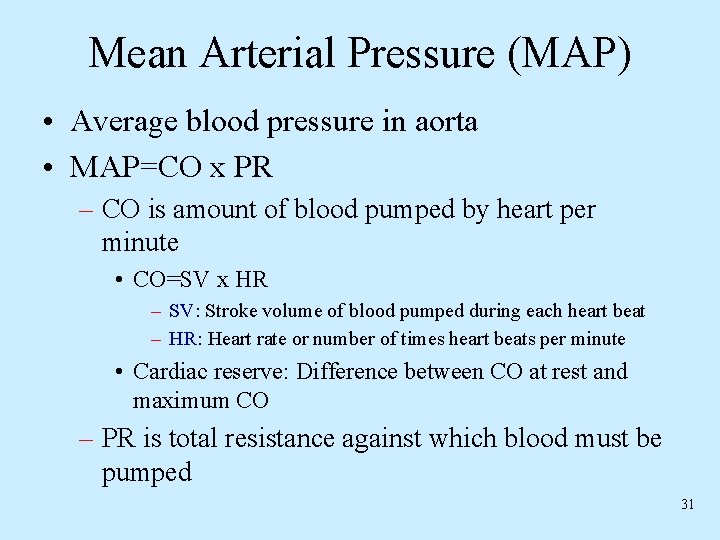
Mean Arterial Pressure (MAP) • Average blood pressure in aorta • MAP=CO x PR – CO is amount of blood pumped by heart per minute • CO=SV x HR – SV: Stroke volume of blood pumped during each heart beat – HR: Heart rate or number of times heart beats per minute • Cardiac reserve: Difference between CO at rest and maximum CO – PR is total resistance against which blood must be pumped 31
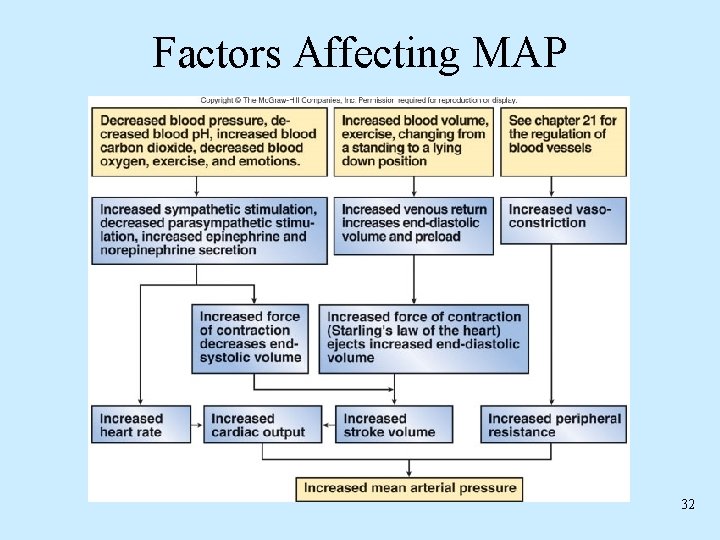
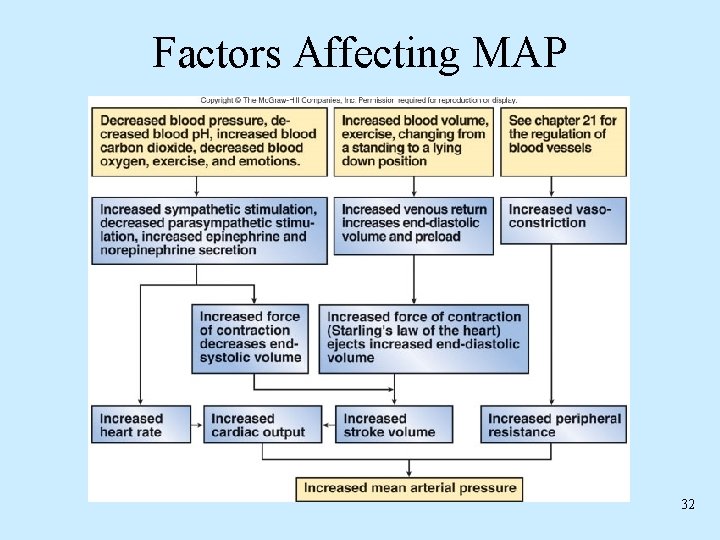
Factors Affecting MAP 32
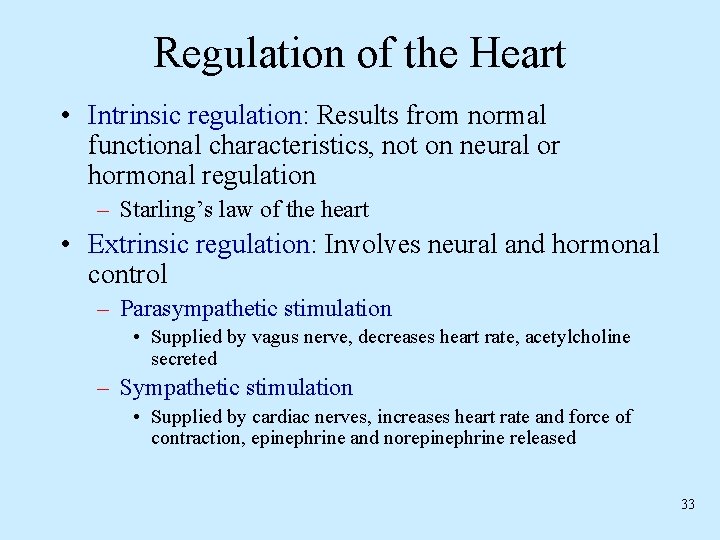
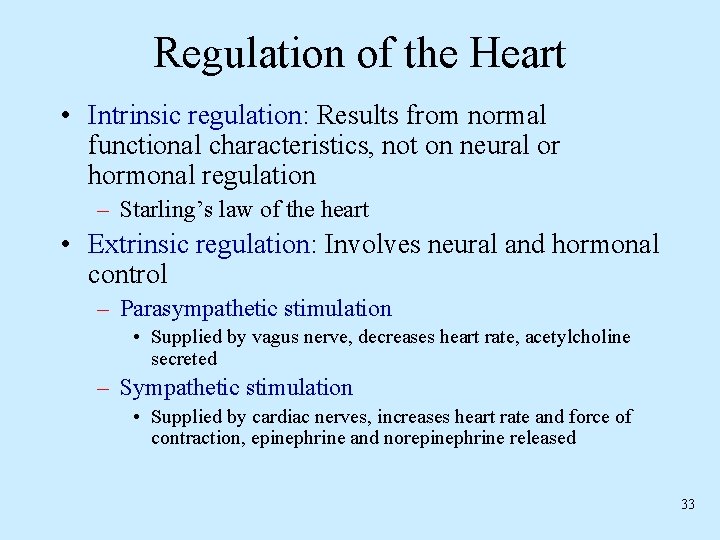
Regulation of the Heart • Intrinsic regulation: Results from normal functional characteristics, not on neural or hormonal regulation – Starling’s law of the heart • Extrinsic regulation: Involves neural and hormonal control – Parasympathetic stimulation • Supplied by vagus nerve, decreases heart rate, acetylcholine secreted – Sympathetic stimulation • Supplied by cardiac nerves, increases heart rate and force of contraction, epinephrine and norepinephrine released 33
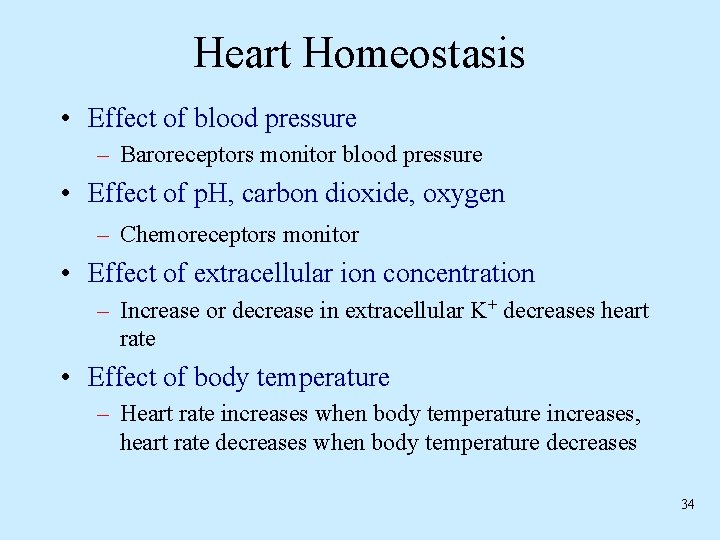
Heart Homeostasis • Effect of blood pressure – Baroreceptors monitor blood pressure • Effect of p. H, carbon dioxide, oxygen – Chemoreceptors monitor • Effect of extracellular ion concentration – Increase or decrease in extracellular K+ decreases heart rate • Effect of body temperature – Heart rate increases when body temperature increases, heart rate decreases when body temperature decreases 34
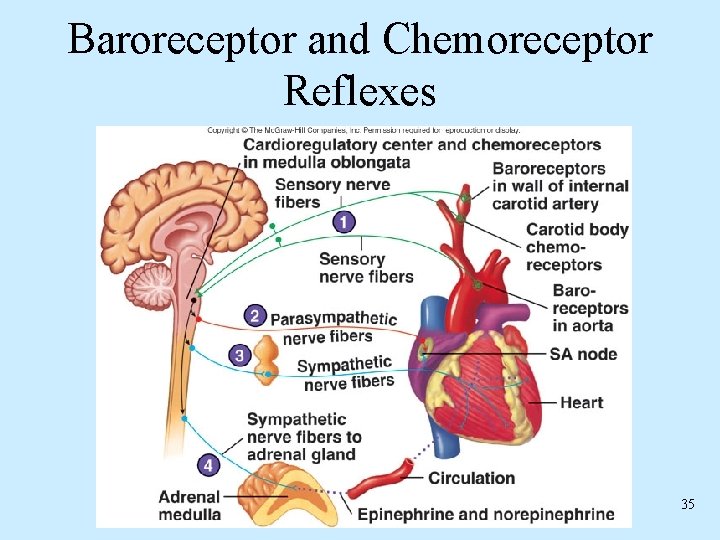
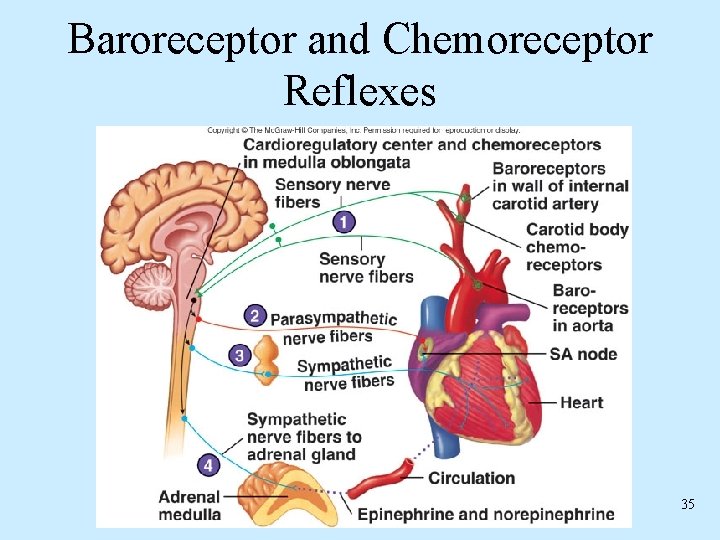
Baroreceptor and Chemoreceptor Reflexes 35
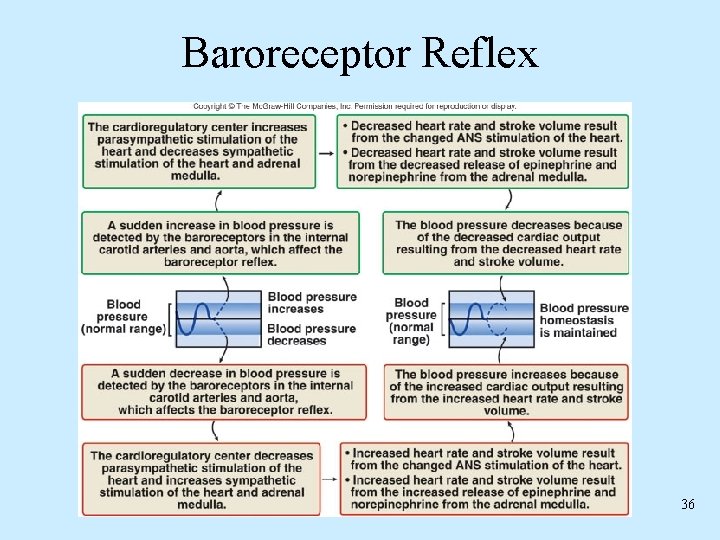
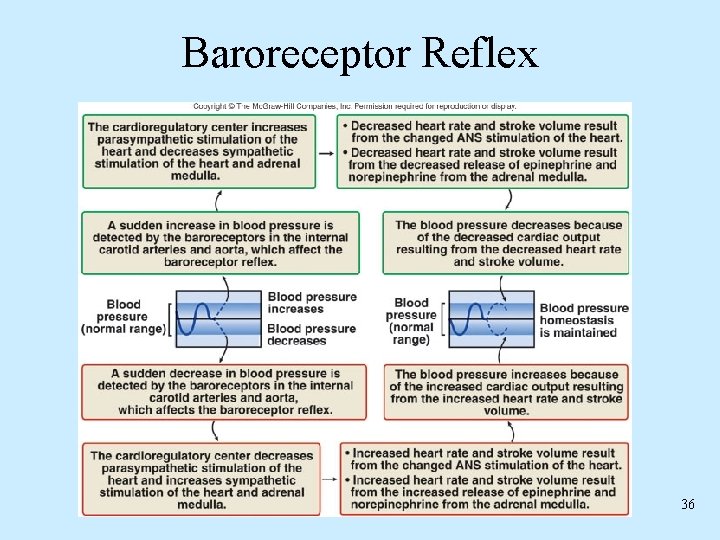
Baroreceptor Reflex 36
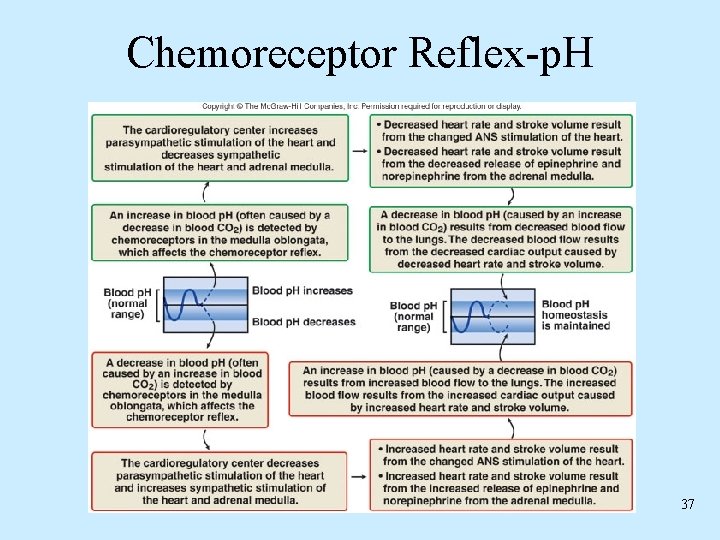
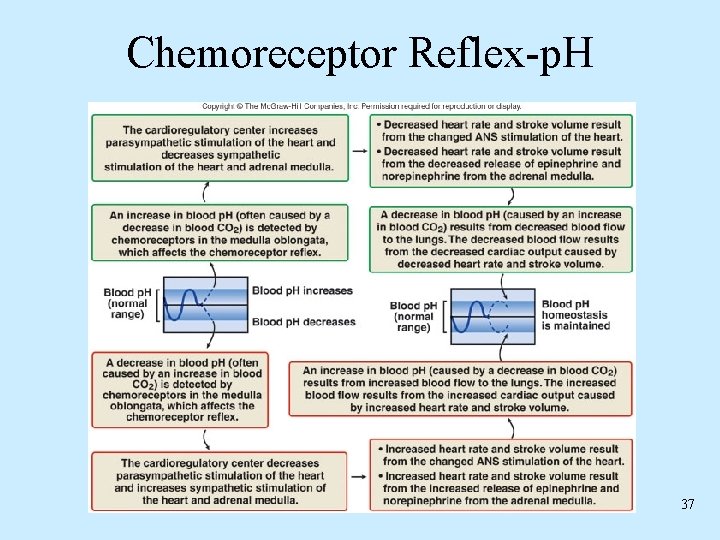
Chemoreceptor Reflex-p. H 37
Effects of Aging on the Heart • Gradual changes in heart function, minor under resting condition, more significant during exercise • Hypertrophy of left ventricle • Maximum heart rate decreases • Increased tendency for valves to function abnormally and arrhythmias to occur • Increased oxygen consumption required to pump same amount of blood 38
 Capillary bed
Capillary bed What makes up the cardiovascular system
What makes up the cardiovascular system Rat cardiovascular system simulation
Rat cardiovascular system simulation Cardiovascular/lymphatic system it's totally tubular
Cardiovascular/lymphatic system it's totally tubular Blood vessels crash course
Blood vessels crash course Chapter 5 learning exercises medical terminology
Chapter 5 learning exercises medical terminology Figure 11-8 arteries
Figure 11-8 arteries Chapter 11 the cardiovascular system figure 11-3
Chapter 11 the cardiovascular system figure 11-3 Chapter 11 the cardiovascular system
Chapter 11 the cardiovascular system Lesson 11 cardiovascular system
Lesson 11 cardiovascular system Circulatory system tissue
Circulatory system tissue Anatomy blood vessels
Anatomy blood vessels Introduction of heart
Introduction of heart Cardiovascular system
Cardiovascular system Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Chapter 13 cardiovascular system
Chapter 13 cardiovascular system Chapter 11 the cardiovascular system figure 11-2
Chapter 11 the cardiovascular system figure 11-2 The cardiovascular system includes the
The cardiovascular system includes the Chapter 19 cardiovascular system blood
Chapter 19 cardiovascular system blood Chapter 19 the cardiovascular system blood vessels
Chapter 19 the cardiovascular system blood vessels Percussion of right border of heart
Percussion of right border of heart Left atrium sheep heart
Left atrium sheep heart Stars plowhorses puzzles dogs
Stars plowhorses puzzles dogs Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Soplo protosistolico
Soplo protosistolico Rias cardiovascular
Rias cardiovascular National cardiovascular partners
National cardiovascular partners When does stroke volume increase
When does stroke volume increase Chapter 46 the child with a cardiovascular alteration
Chapter 46 the child with a cardiovascular alteration The child with a cardiovascular disorder chapter 26
The child with a cardiovascular disorder chapter 26 Chapter 25 assessment of cardiovascular function
Chapter 25 assessment of cardiovascular function American board of cardiovascular medicine
American board of cardiovascular medicine Battiti ectopici ventricolari forum
Battiti ectopici ventricolari forum Neuronas sensoriales
Neuronas sensoriales Sistema digestivo
Sistema digestivo Isgemiese hartsiekte
Isgemiese hartsiekte Fitness components
Fitness components Salud cardiovascular
Salud cardiovascular