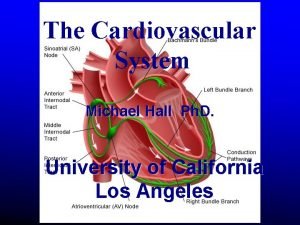
Cardiovascular System Heart cardiac muscle physiology Cardiac conduction

- Slides: 35
Cardiovascular System • Heart – cardiac muscle physiology – Cardiac conduction system – Heart structures • Vessels- arteries and veins • Blood – WBC, RBC and Platelets, =Formed elements plus the plasma (the fluid)
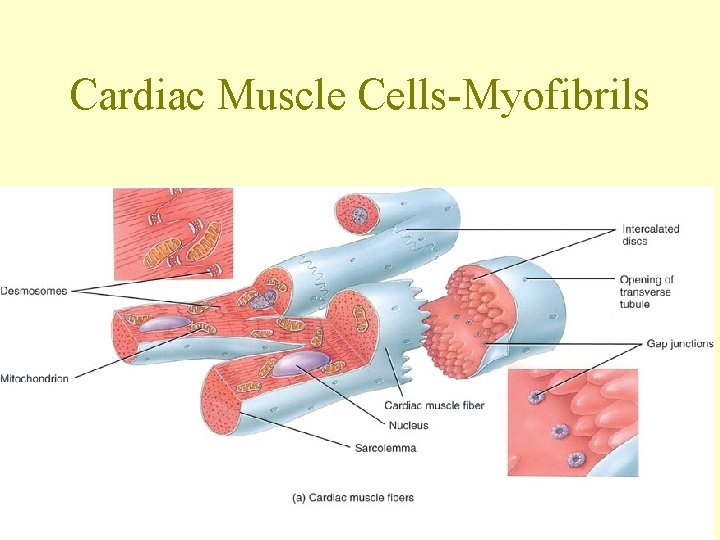
Types of Cardiac Cells • Auto-rhythmic cells = pacemaker cells (depolarize spontaneously) • Contractile cells – myofibrils –connected well together to form “functional Syncitium” for myocardium contraction Ease of movement between cells (conductivity)
Mechanical and Electrical • Critical to remember that there is mechanical aspects to heart function=myofibrils and electrical aspect – Pacemaker cells and – Resulting AP from these cells to working muscle cells causes depolarization and repolarization
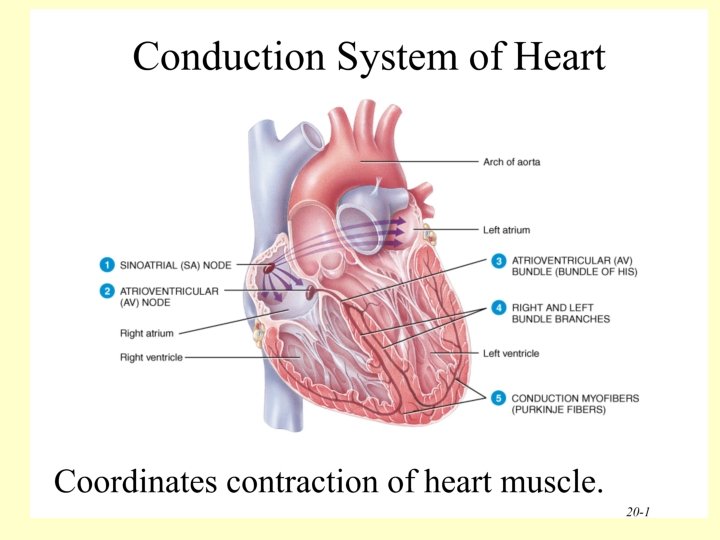
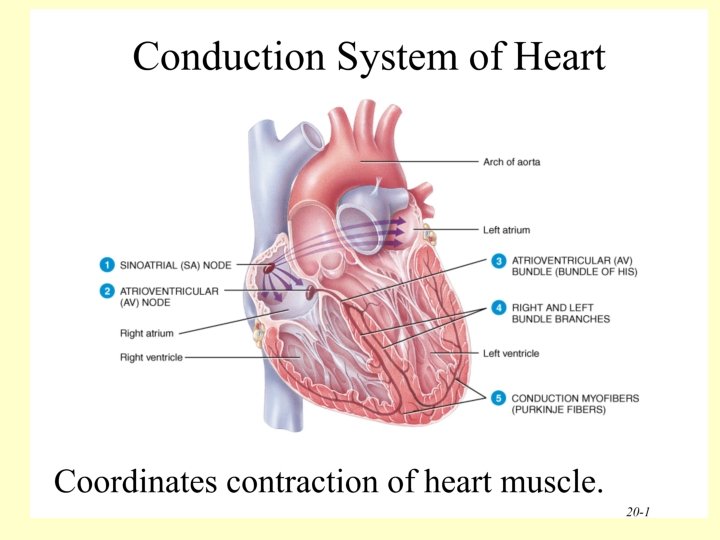
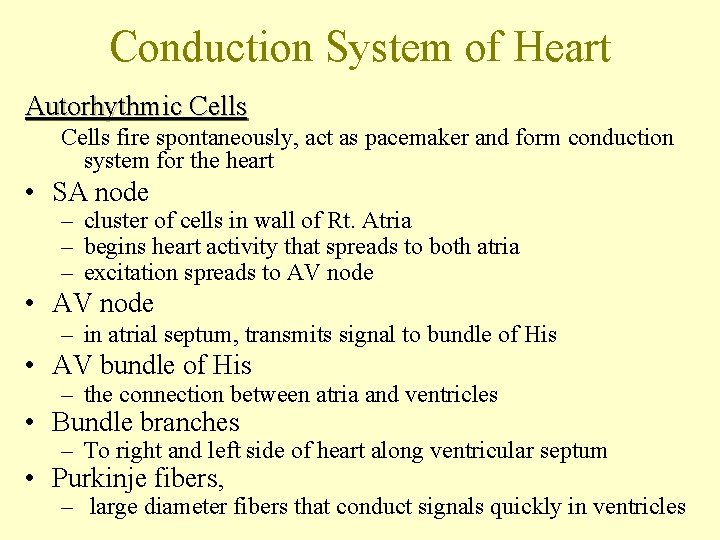
Conduction System of Heart Autorhythmic Cells fire spontaneously, act as pacemaker and form conduction system for the heart • SA node – cluster of cells in wall of Rt. Atria – begins heart activity that spreads to both atria – excitation spreads to AV node • AV node – in atrial septum, transmits signal to bundle of His • AV bundle of His – the connection between atria and ventricles • Bundle branches – To right and left side of heart along ventricular septum • Purkinje fibers, – large diameter fibers that conduct signals quickly in ventricles
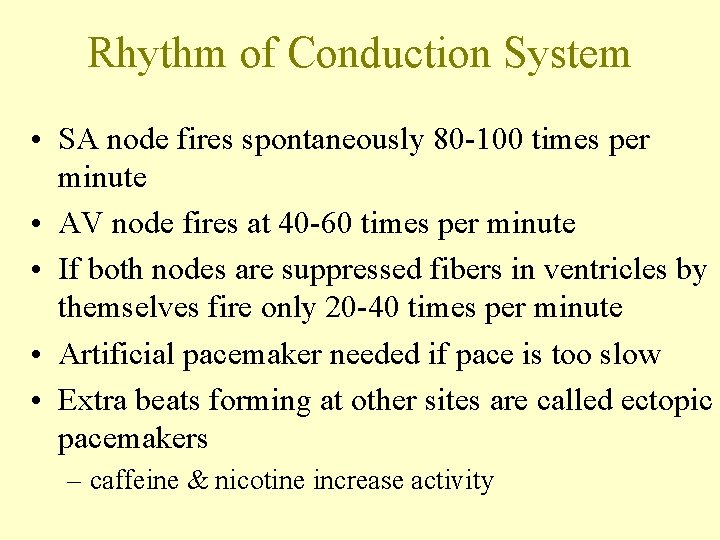
Rhythm of Conduction System • SA node fires spontaneously 80 -100 times per minute • AV node fires at 40 -60 times per minute • If both nodes are suppressed fibers in ventricles by themselves fire only 20 -40 times per minute • Artificial pacemaker needed if pace is too slow • Extra beats forming at other sites are called ectopic pacemakers – caffeine & nicotine increase activity
How does these cells automatically fire? ?
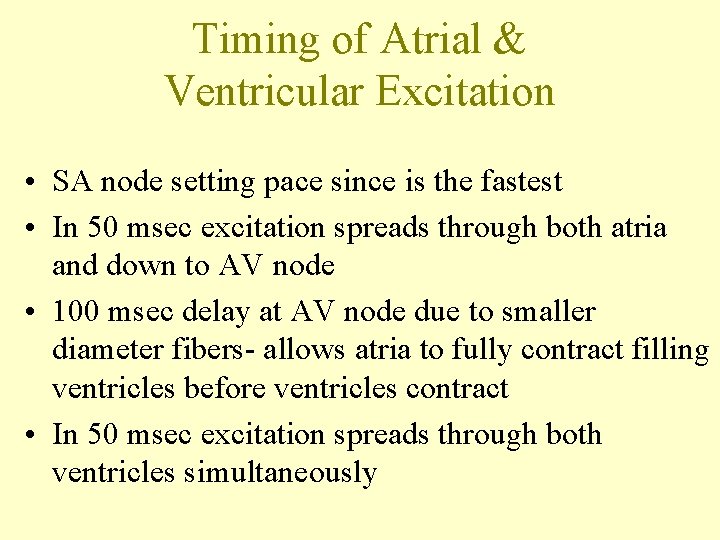
Timing of Atrial & Ventricular Excitation • SA node setting pace since is the fastest • In 50 msec excitation spreads through both atria and down to AV node • 100 msec delay at AV node due to smaller diameter fibers- allows atria to fully contract filling ventricles before ventricles contract • In 50 msec excitation spreads through both ventricles simultaneously
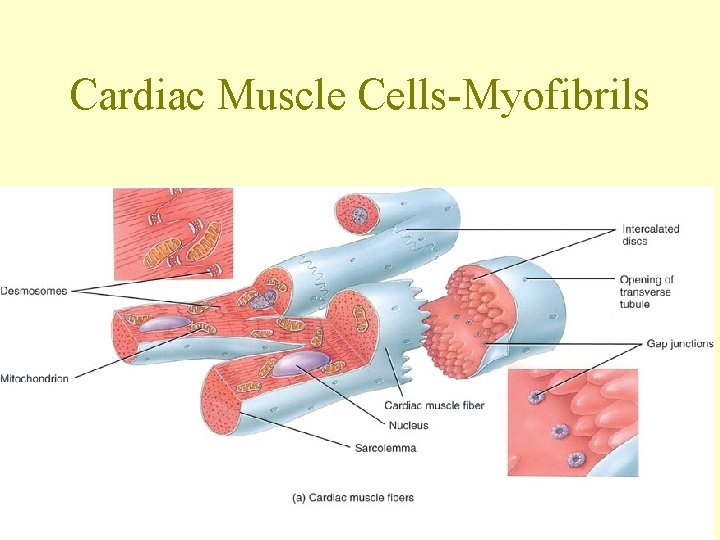
Cardiac Muscle Cells-Myofibrils
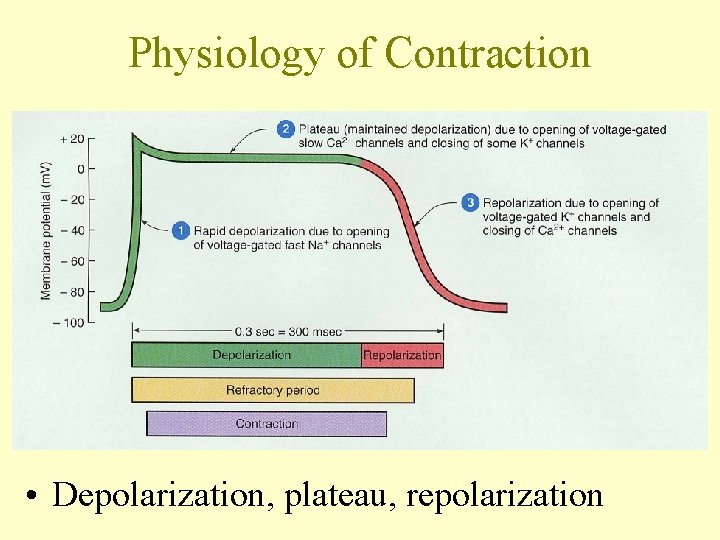
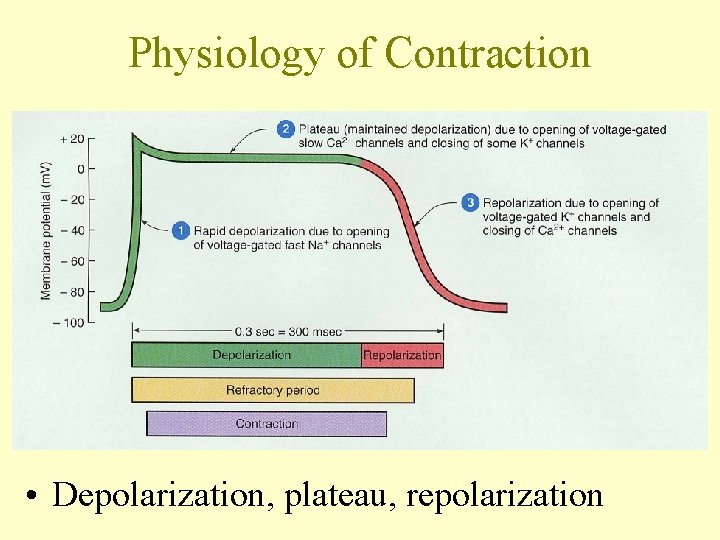
Physiology of Contraction • Depolarization, plateau, repolarization

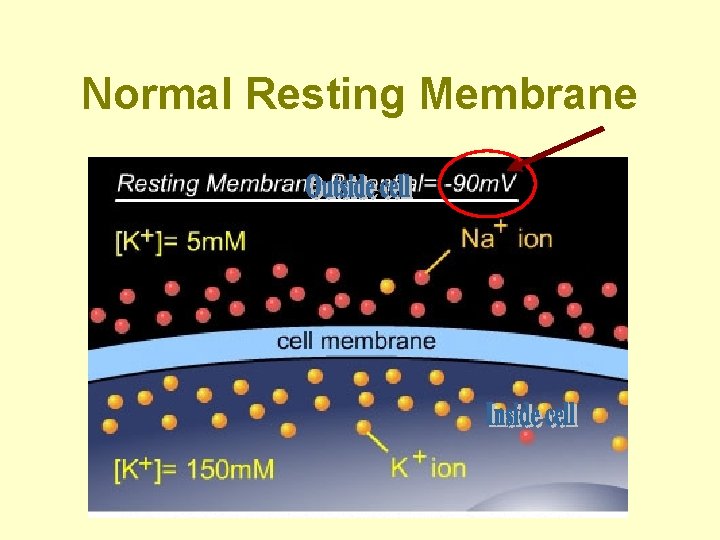
Important Electrolytes • Sodium – major extracellular ion • Potassium - major intracellular ion • Chloride - negative ion • Calcium - very important for muscle contraction
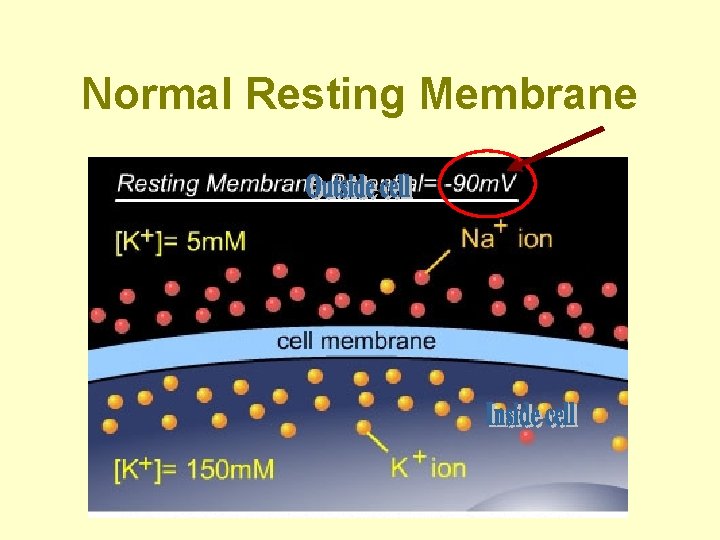
Normal Resting Membrane
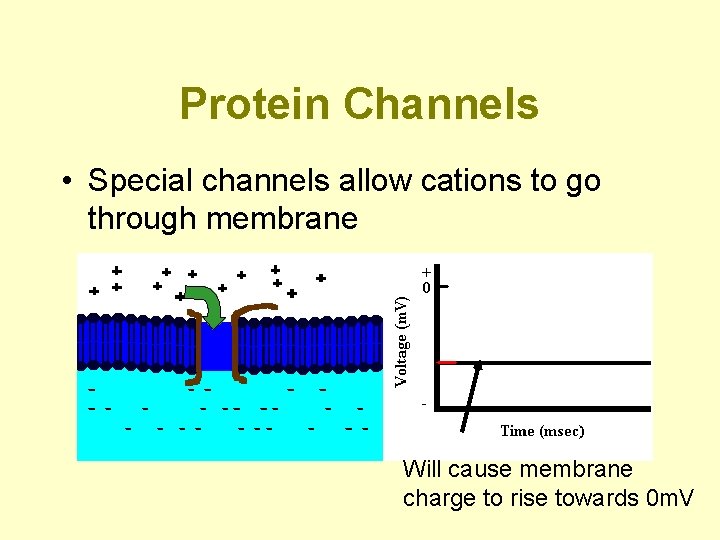
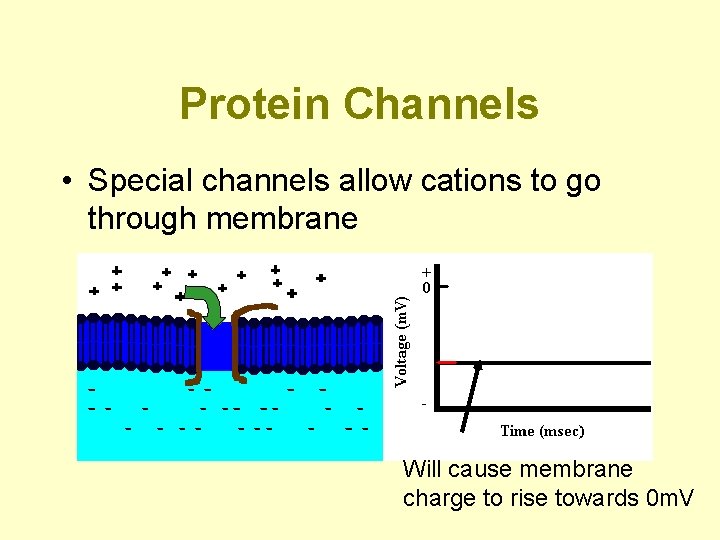
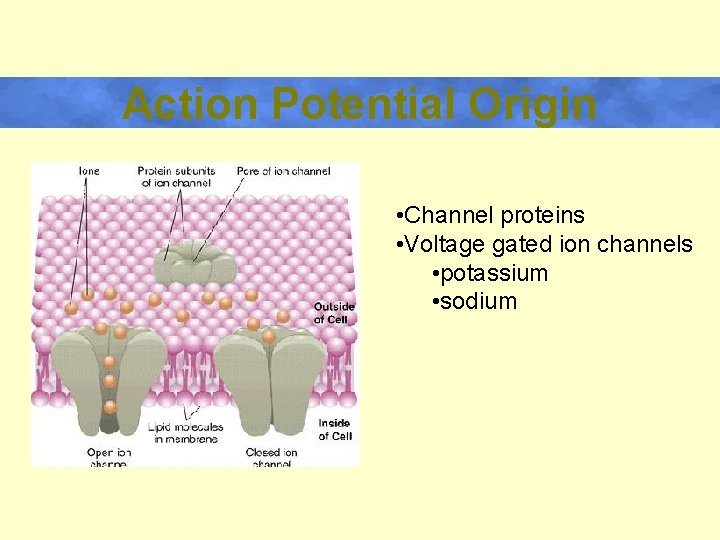
Protein Channels • Special channels allow cations to go through membrane Will cause membrane charge to rise towards 0 m. V
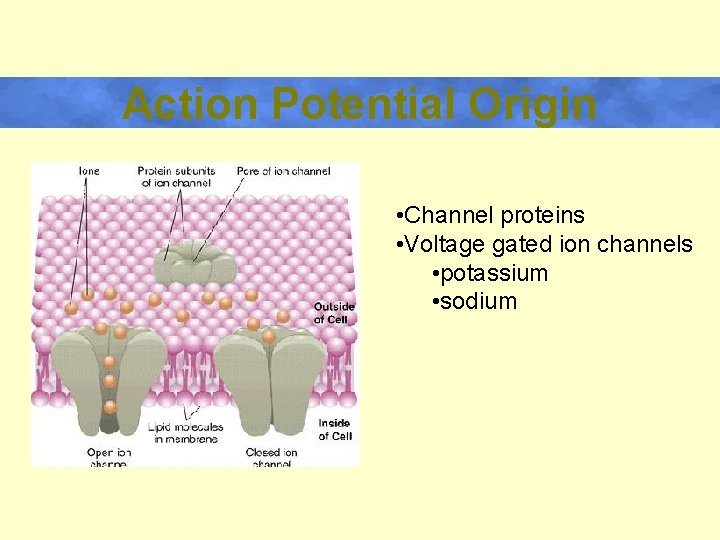
Action Potential Origin • Channel proteins • Voltage gated ion channels • potassium • sodium
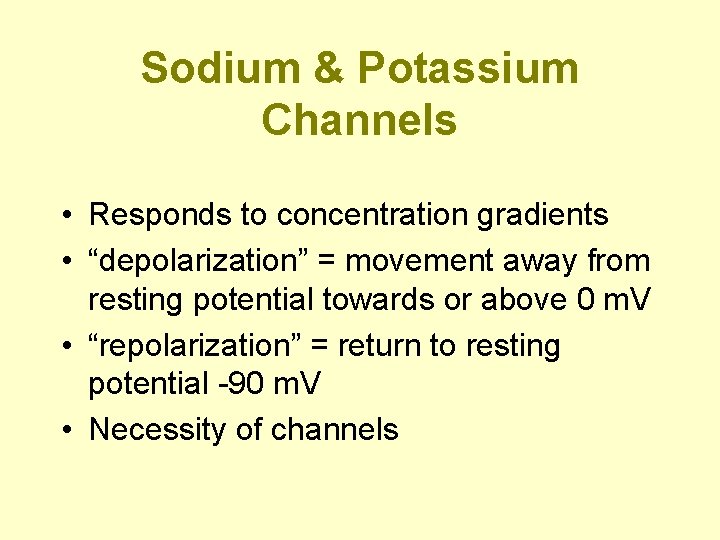
Sodium & Potassium Channels • Responds to concentration gradients • “depolarization” = movement away from resting potential towards or above 0 m. V • “repolarization” = return to resting potential -90 m. V • Necessity of channels
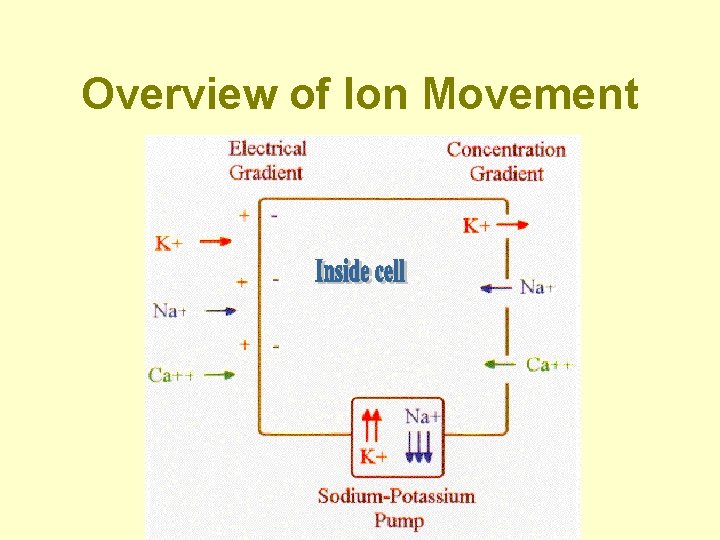
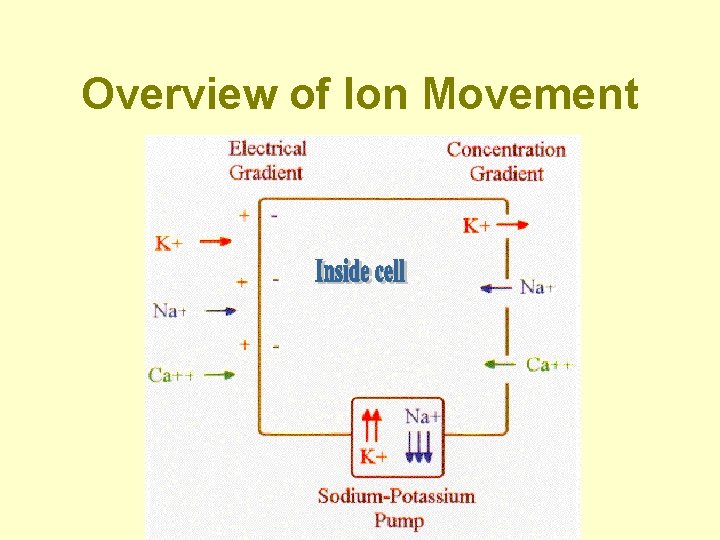
Overview of Ion Movement
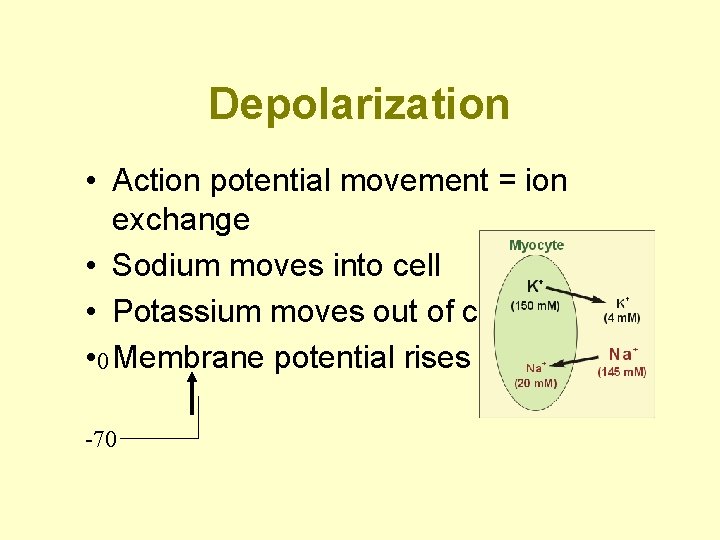
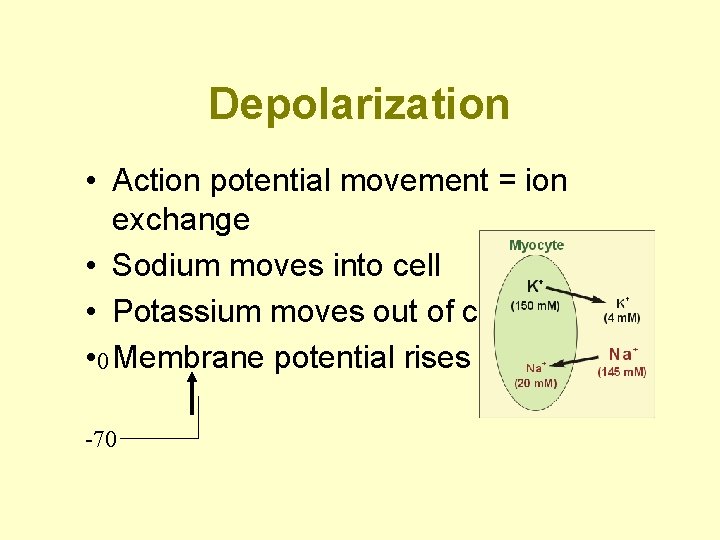
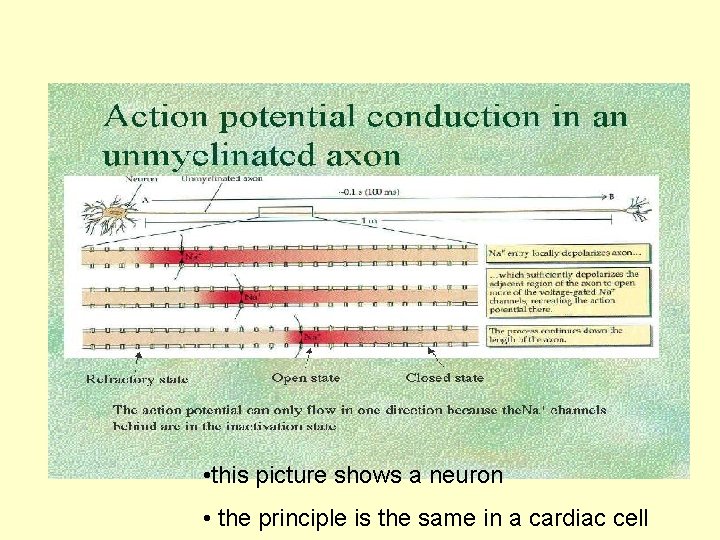
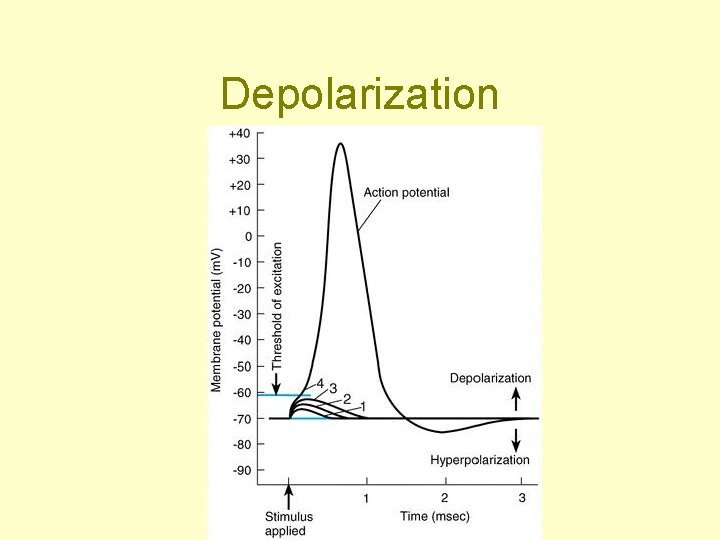
Depolarization • Action potential movement = ion exchange • Sodium moves into cell • Potassium moves out of cell • 0 Membrane potential rises -70
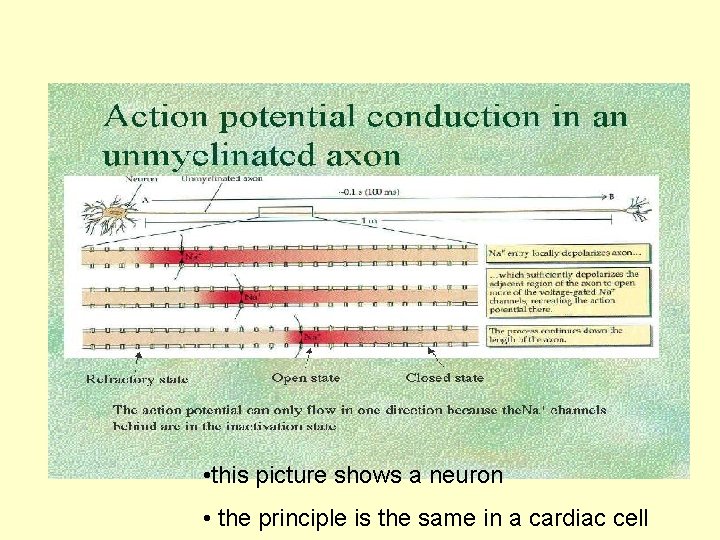
• this picture shows a neuron • the principle is the same in a cardiac cell
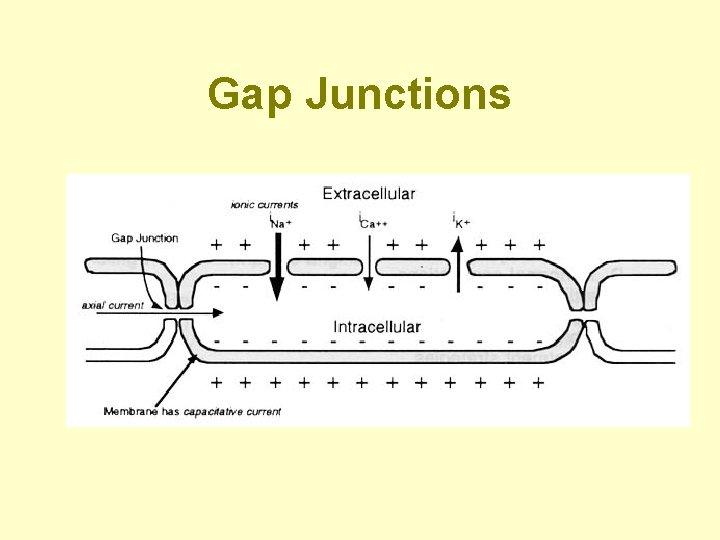
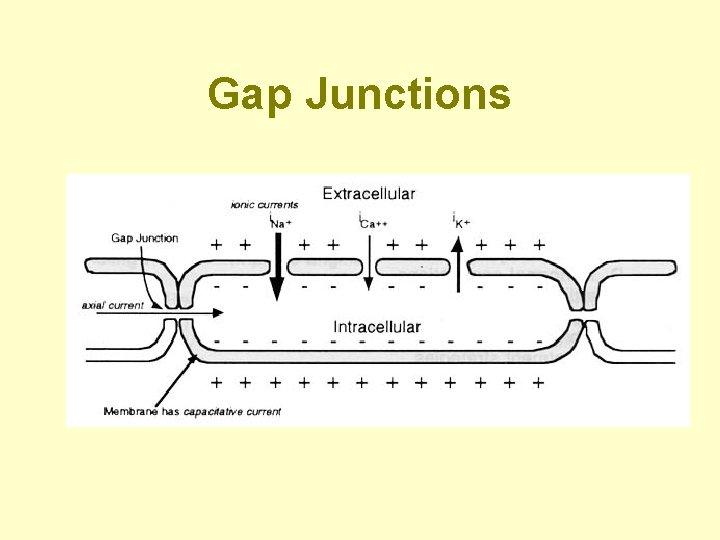
Gap Junctions
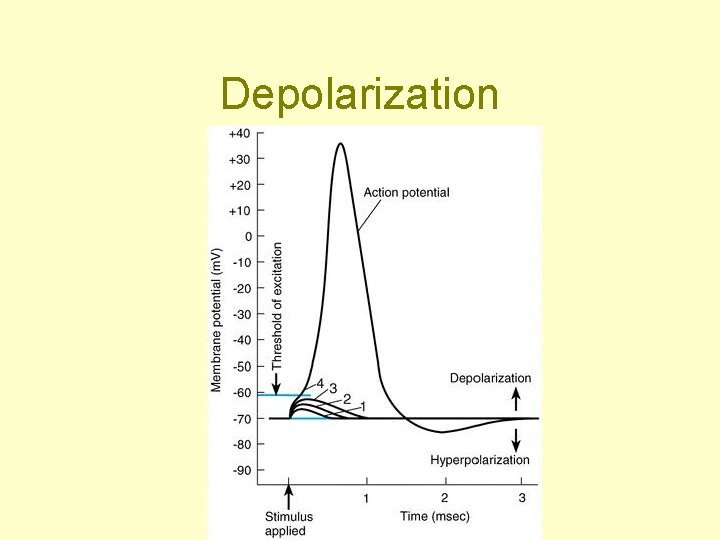
Depolarization
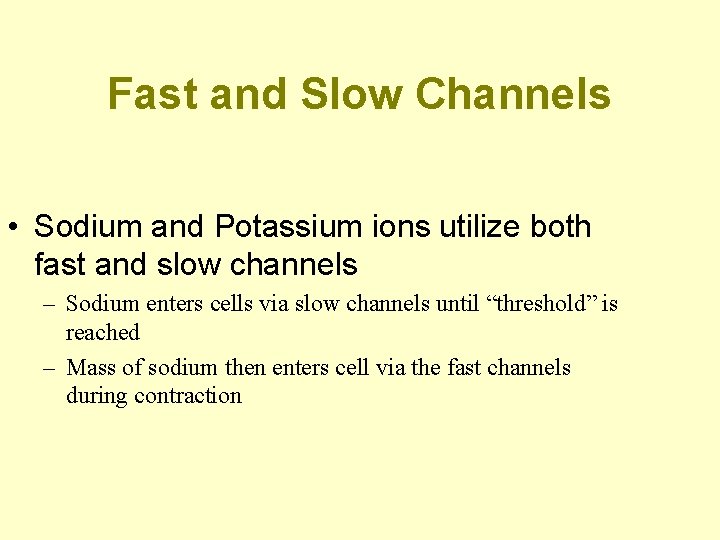
Fast and Slow Channels • Sodium and Potassium ions utilize both fast and slow channels – Sodium enters cells via slow channels until “threshold” is reached – Mass of sodium then enters cell via the fast channels during contraction
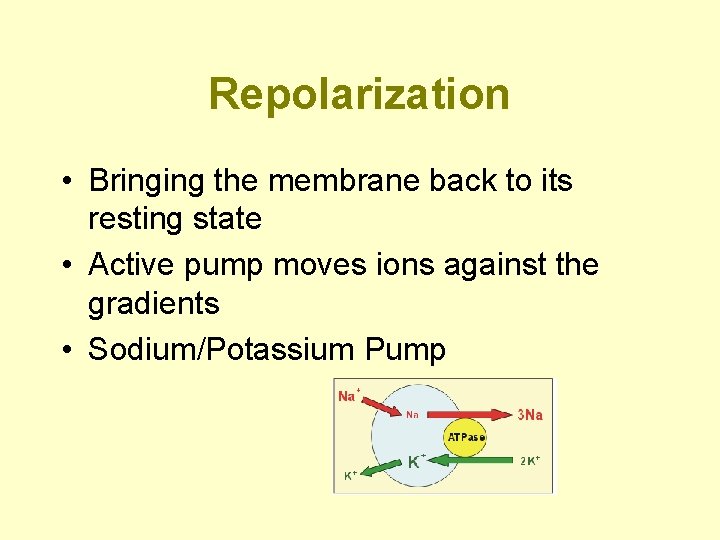
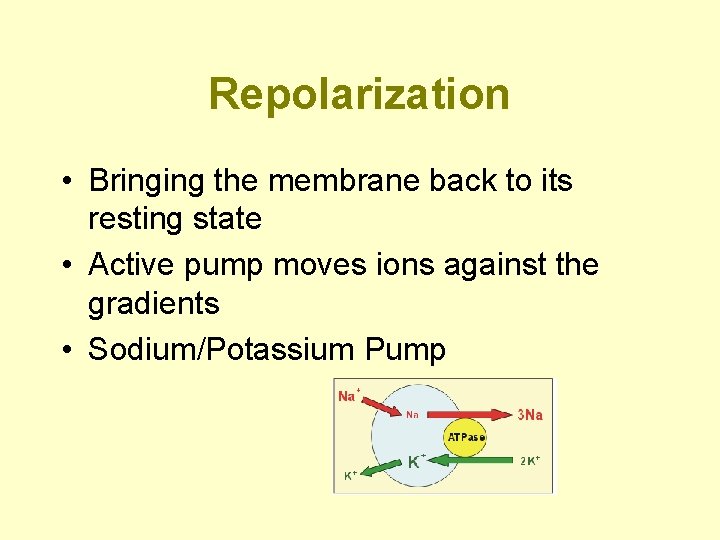
Repolarization • Bringing the membrane back to its resting state • Active pump moves ions against the gradients • Sodium/Potassium Pump
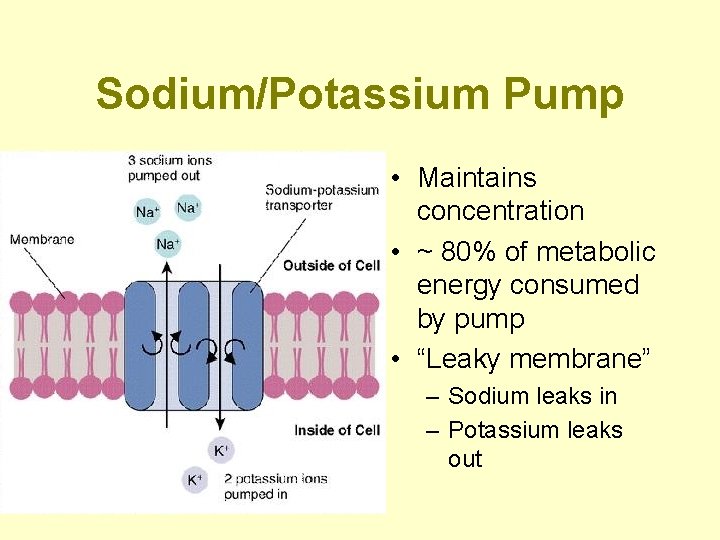
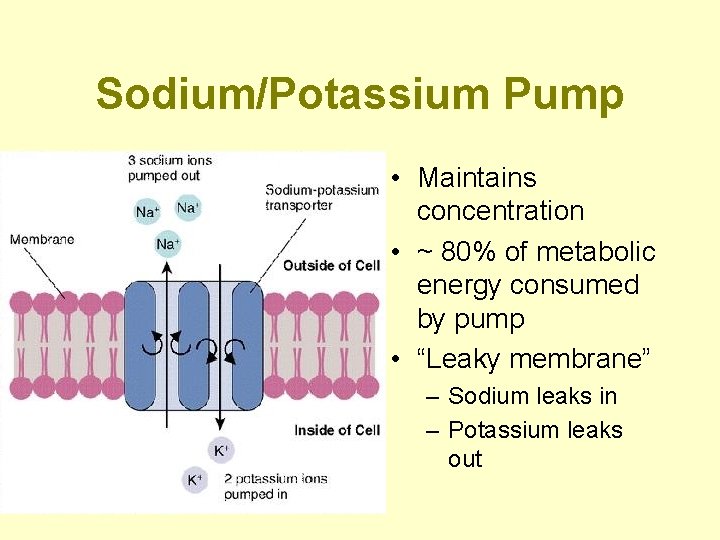
Sodium/Potassium Pump • Maintains concentration • ~ 80% of metabolic energy consumed by pump • “Leaky membrane” – Sodium leaks in – Potassium leaks out
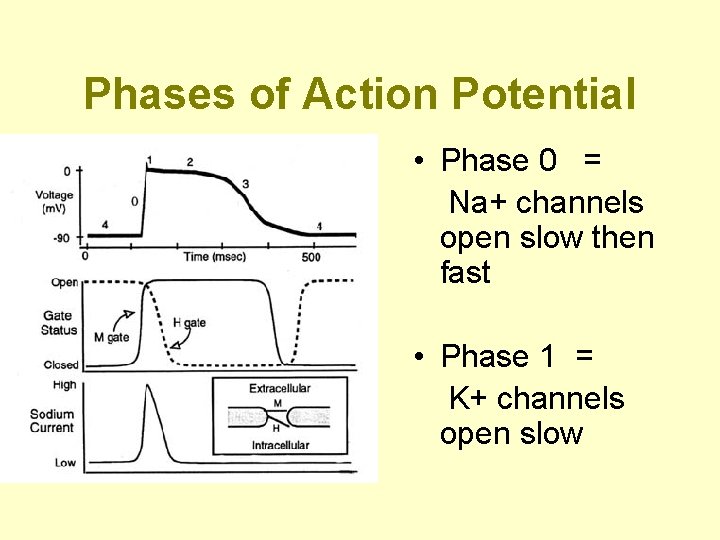
Phases of the Action Potential • Specific sequence of events • Phases 0 through 4 • Important to know what happens in each phase – Comprehension of pathology and pharmacotherapy
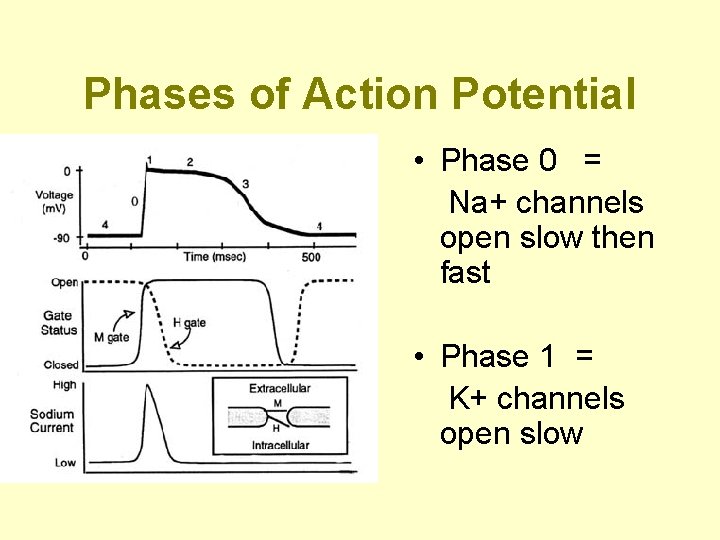
Phases of Action Potential • Phase 0 = Na+ channels open slow then fast • Phase 1 = K+ channels open slow
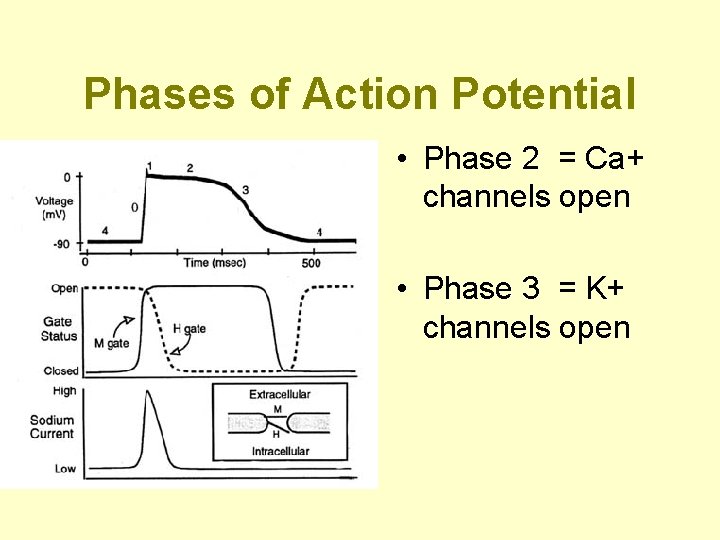
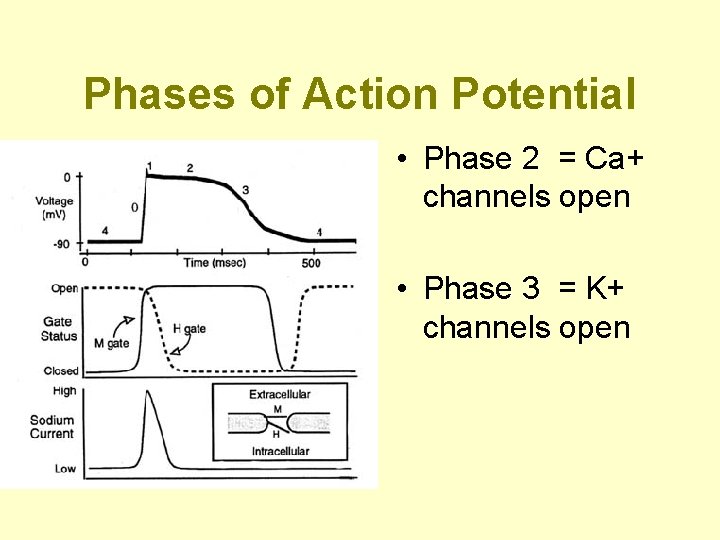
Phases of Action Potential • Phase 2 = Ca+ channels open • Phase 3 = K+ channels open
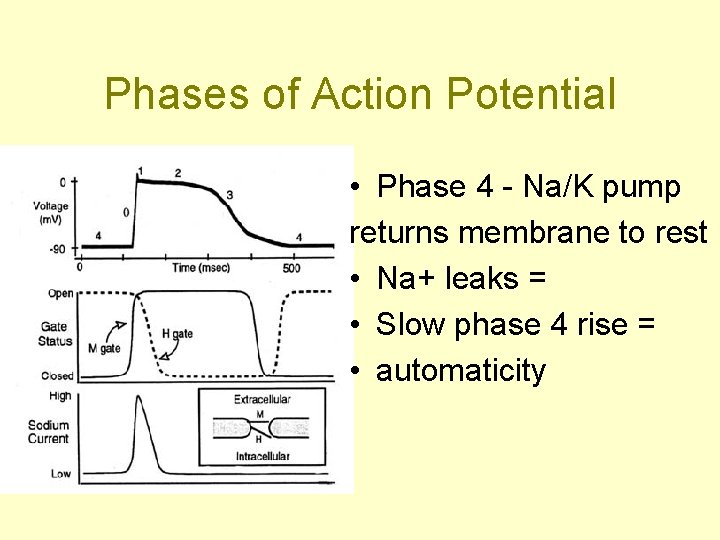
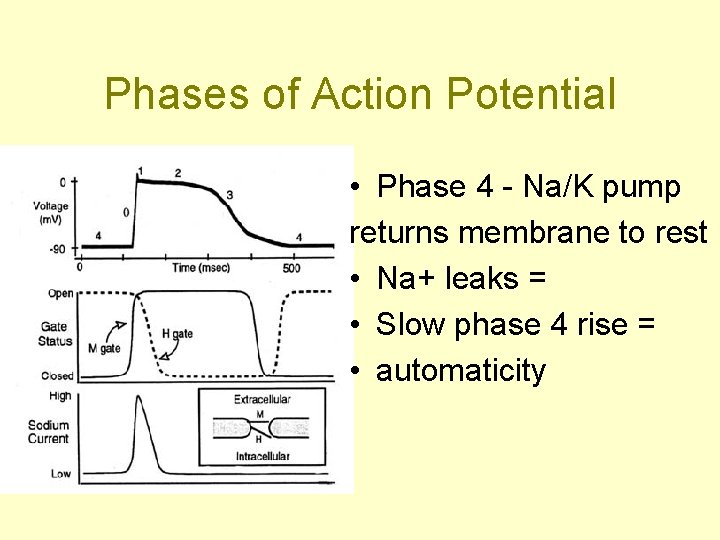
Phases of Action Potential • Phase 4 - Na/K pump returns membrane to rest • Na+ leaks = • Slow phase 4 rise = • automaticity
The Condensed Version • Maintenance of membranes resting potential • External force (stimulus) • Slow rise brings it to threshold at - 70 m. V • Ion exchange begins • Na+, then Ca+ into cell • K+ out of cell
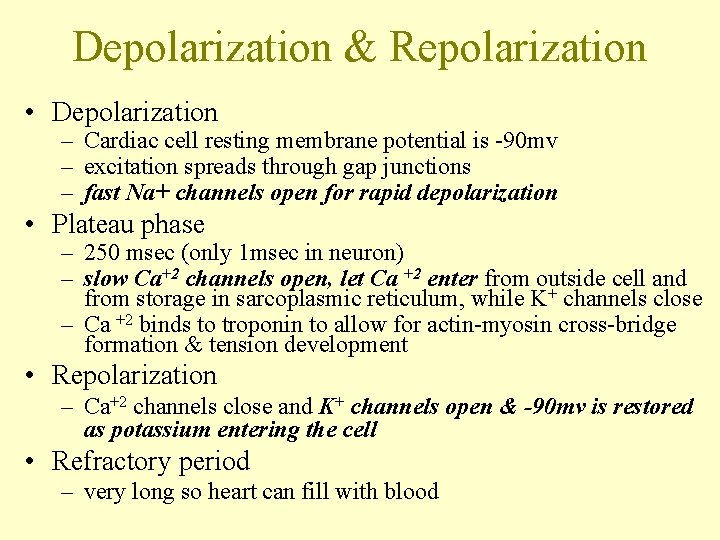
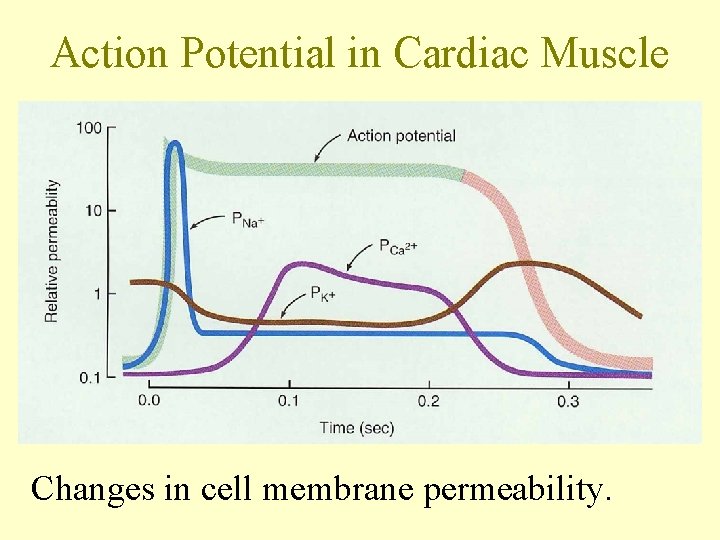
Depolarization & Repolarization • Depolarization – Cardiac cell resting membrane potential is -90 mv – excitation spreads through gap junctions – fast Na+ channels open for rapid depolarization • Plateau phase – 250 msec (only 1 msec in neuron) – slow Ca+2 channels open, let Ca +2 enter from outside cell and from storage in sarcoplasmic reticulum, while K+ channels close – Ca +2 binds to troponin to allow for actin-myosin cross-bridge formation & tension development • Repolarization – Ca+2 channels close and K+ channels open & -90 mv is restored as potassium entering the cell • Refractory period – very long so heart can fill with blood
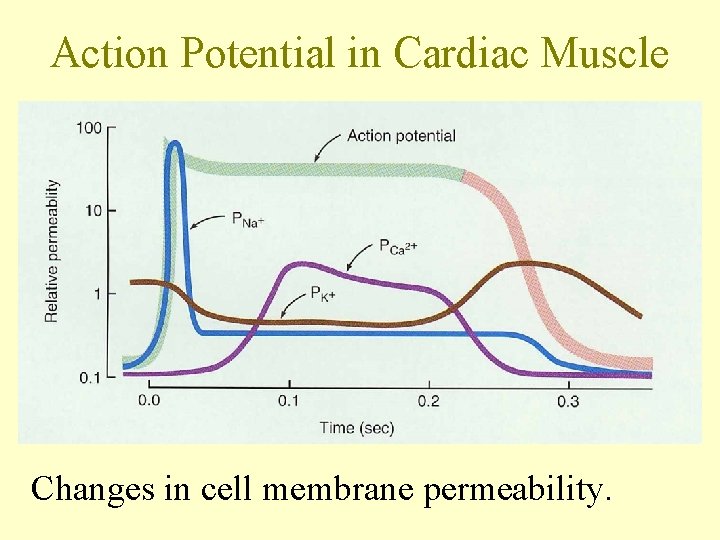
Action Potential in Cardiac Muscle Changes in cell membrane permeability.
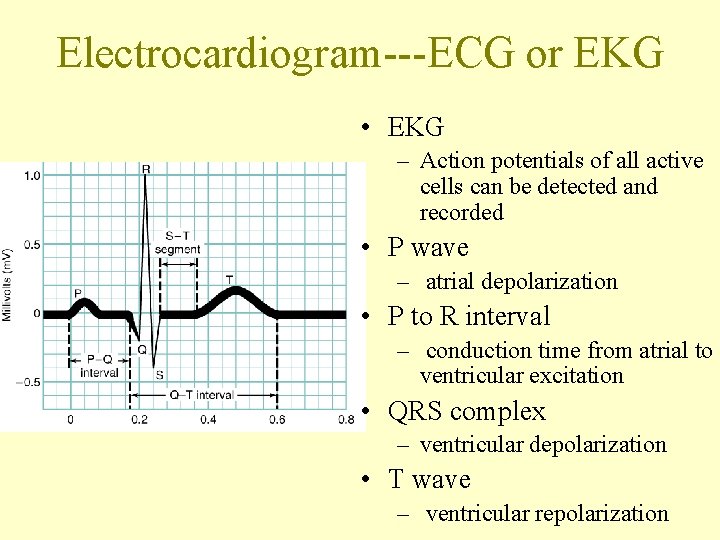
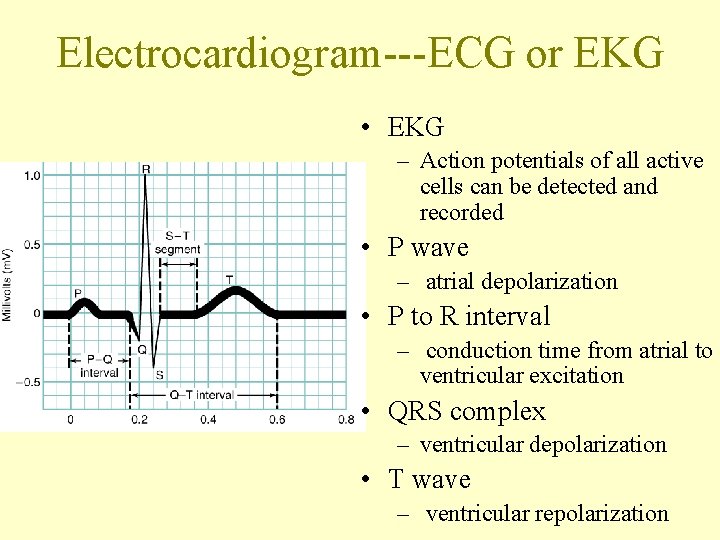
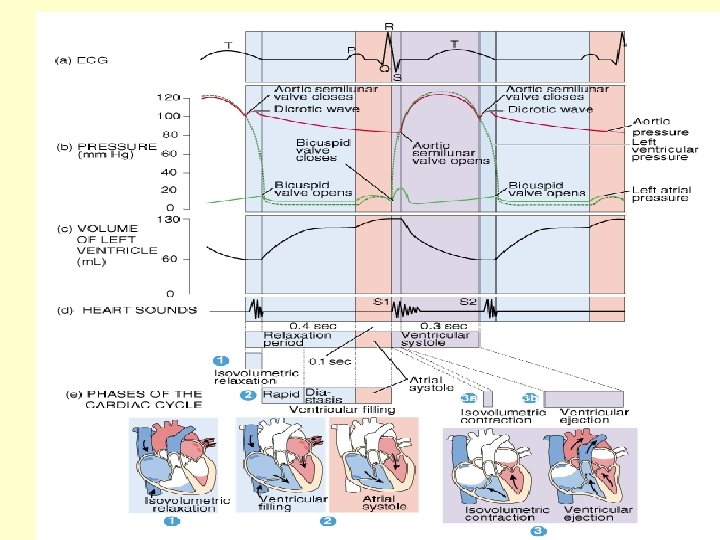
Electrocardiogram---ECG or EKG • EKG – Action potentials of all active cells can be detected and recorded • P wave – atrial depolarization • P to R interval – conduction time from atrial to ventricular excitation • QRS complex – ventricular depolarization • T wave – ventricular repolarization
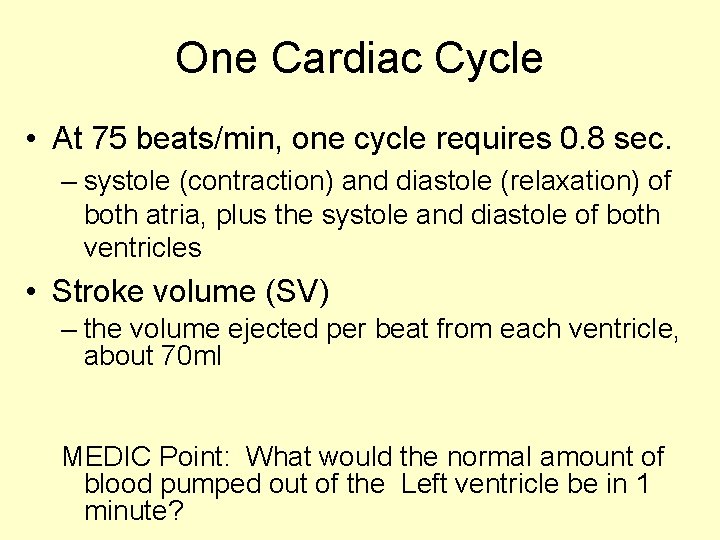
One Cardiac Cycle • At 75 beats/min, one cycle requires 0. 8 sec. – systole (contraction) and diastole (relaxation) of both atria, plus the systole and diastole of both ventricles • Stroke volume (SV) – the volume ejected per beat from each ventricle, about 70 ml MEDIC Point: What would the normal amount of blood pumped out of the Left ventricle be in 1 minute?
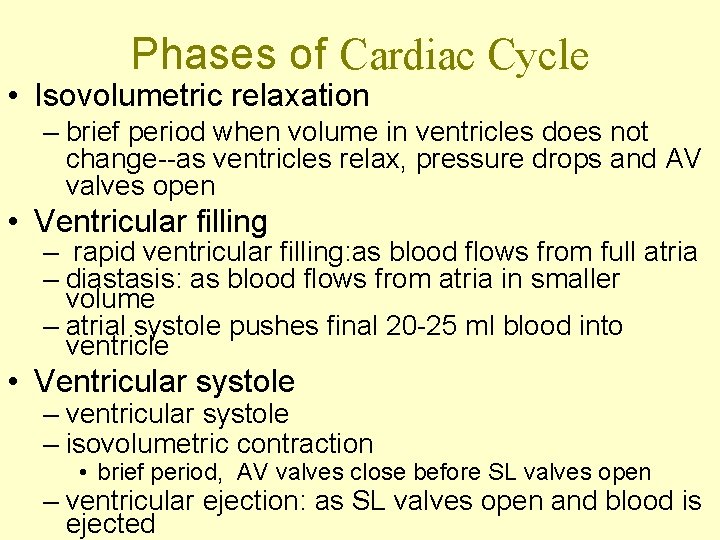
Phases of Cardiac Cycle • Isovolumetric relaxation – brief period when volume in ventricles does not change--as ventricles relax, pressure drops and AV valves open • Ventricular filling – rapid ventricular filling: as blood flows from full atria – diastasis: as blood flows from atria in smaller volume – atrial systole pushes final 20 -25 ml blood into ventricle • Ventricular systole – ventricular systole – isovolumetric contraction • brief period, AV valves close before SL valves open – ventricular ejection: as SL valves open and blood is ejected
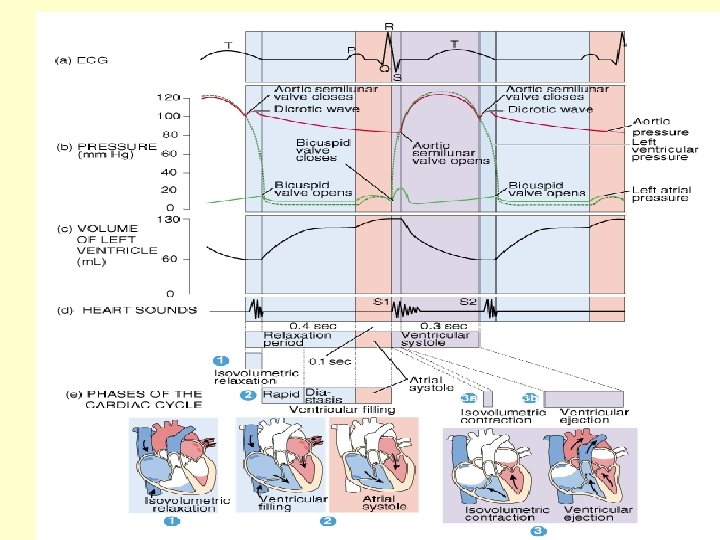
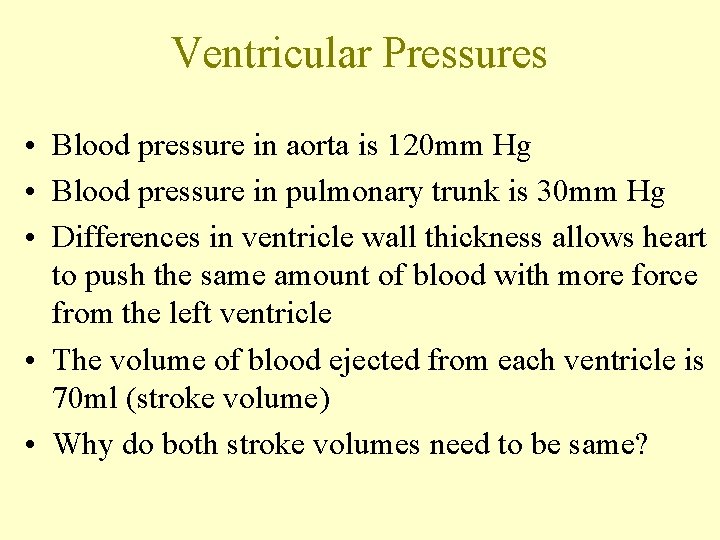
Ventricular Pressures • Blood pressure in aorta is 120 mm Hg • Blood pressure in pulmonary trunk is 30 mm Hg • Differences in ventricle wall thickness allows heart to push the same amount of blood with more force from the left ventricle • The volume of blood ejected from each ventricle is 70 ml (stroke volume) • Why do both stroke volumes need to be same?
 Anatomy and physiology unit 7 cardiovascular system
Anatomy and physiology unit 7 cardiovascular system Intrinsic cardiac conduction system
Intrinsic cardiac conduction system Figure 11-4
Figure 11-4 Refractory period cardiac
Refractory period cardiac Right ventricle failure
Right ventricle failure Conduction system of heart
Conduction system of heart Conduction system of the heart
Conduction system of the heart Internodal pathway
Internodal pathway Cardiac conduction
Cardiac conduction Actin and myosin
Actin and myosin Contraction
Contraction Muscle physiology
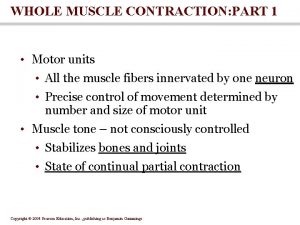
Muscle physiology Treppe
Treppe Actin and myosin cross bridges
Actin and myosin cross bridges Nerve muscle physiology
Nerve muscle physiology Sarcoplasmic
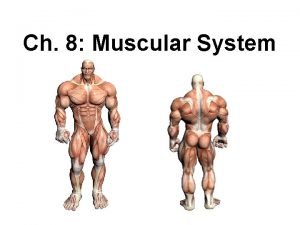
Sarcoplasmic Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Simple cardiac cycle flow chart
Simple cardiac cycle flow chart Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Cardiac muscle tissue labeled
Cardiac muscle tissue labeled Comparison of skeletal cardiac and smooth muscle
Comparison of skeletal cardiac and smooth muscle Cardiac muscle mitochondria
Cardiac muscle mitochondria Cardiac muscle
Cardiac muscle Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Characteristic of cardiac muscle
Characteristic of cardiac muscle L
L Characteristics of skeletal smooth and cardiac muscle
Characteristics of skeletal smooth and cardiac muscle Tissue type
Tissue type Cardiac muscle histology labeled
Cardiac muscle histology labeled Cardiac muscle
Cardiac muscle Skeletal muscle longitudinal section labeled
Skeletal muscle longitudinal section labeled Inner quads
Inner quads Smooth muscle under the microscope
Smooth muscle under the microscope Cardiac muscle striations
Cardiac muscle striations Cardiac muscle striations
Cardiac muscle striations Cardiac muscle striations
Cardiac muscle striations