Cardiovascular System Chapter 13 Cardiovascular System At rest
- Slides: 28
Cardiovascular System Chapter 13
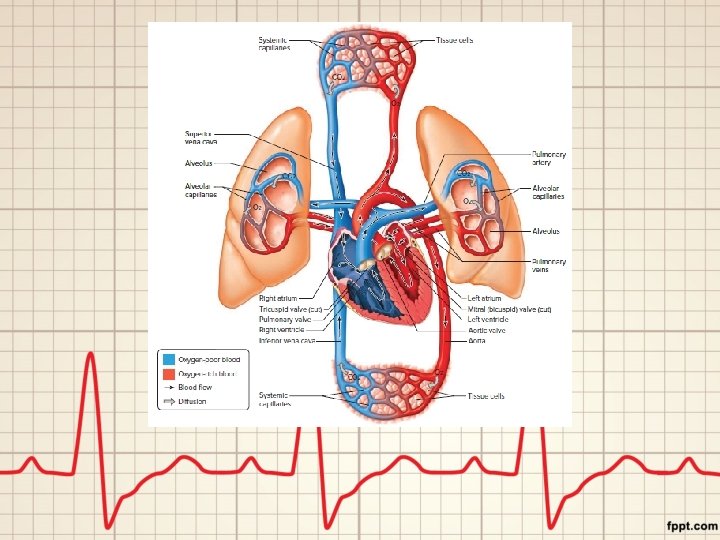
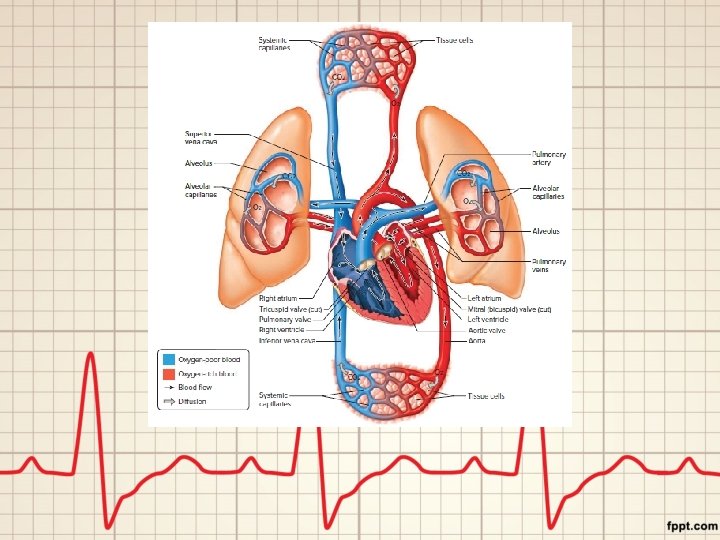
Cardiovascular System • At rest, the heart pumps about 7, 000 liters of blood through the body each day (contracting about 2. 5 million times in the average lifetime) – 1850 gallons = 925 gallons of milk • 3 parts: – Heart – Blood vessels – Blood – 2 closed pathways: • Pulmonary circuit: sends oxygen-poor blood to the lungs to pick up oxygen and unload carbon dioxide • Systemic circuit: sends oxygen-rich blood to all body cells and removes waste
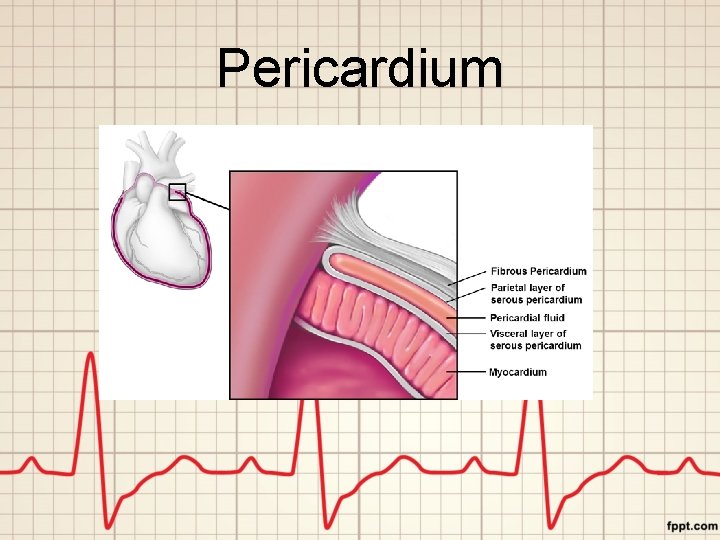
Structure of the Heart • Average adult heart— 14 cm long and 9 cm wide • Bordered by the lungs, lies anterior to the vertebral column and posterior to the sternum • Pericardium: membranous sac that encloses the heart – Innermost layer called the visceral pericardium (covers the heart) – Middle layer called the parietal pericardium – Between the two is called the pericardial cavity (contains fluid that reduces friction between the membrane and the heart)
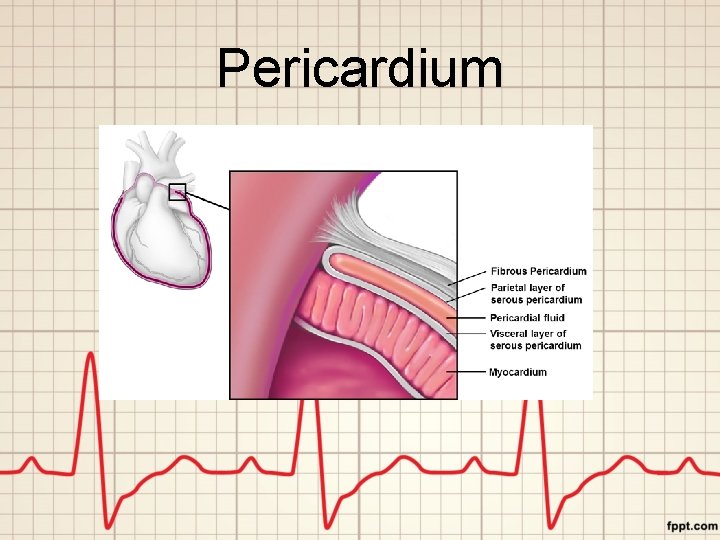
Pericardium
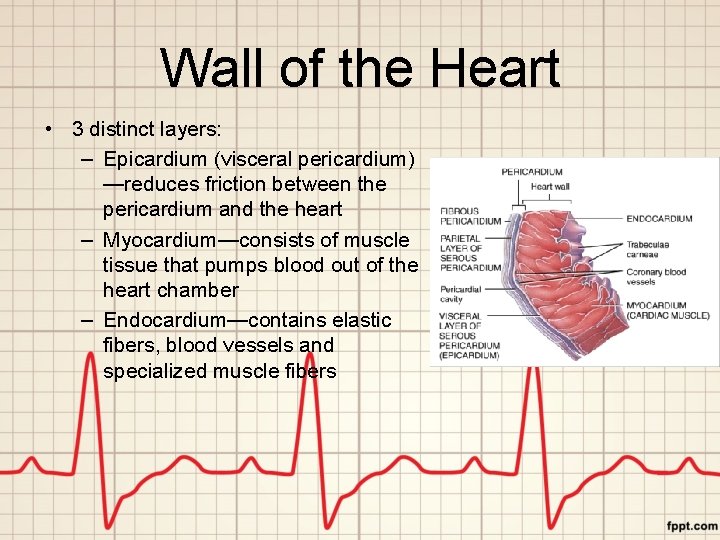
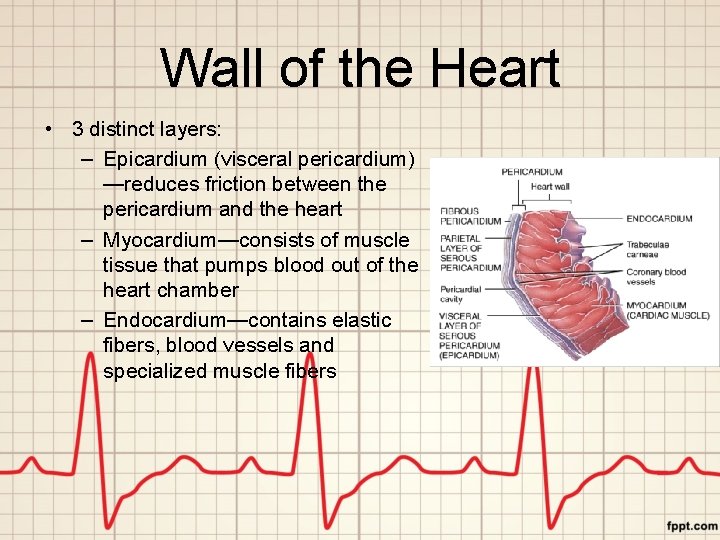
Wall of the Heart • 3 distinct layers: – Epicardium (visceral pericardium) —reduces friction between the pericardium and the heart – Myocardium—consists of muscle tissue that pumps blood out of the heart chamber – Endocardium—contains elastic fibers, blood vessels and specialized muscle fibers
Heart Chambers • Internally, the heart is divided into four chambers: – Two upper atria (plural for atrium) – Two lower ventricles – Solid, wall-like septum separates the left side of the heart and the right side of the heart • Blood from one side of the heart never mixes with blood from the other side • Atrioventricular valve (AV valve) on the right and left of the heart ensure one-way blood flow between the atrium and ventricle on each side
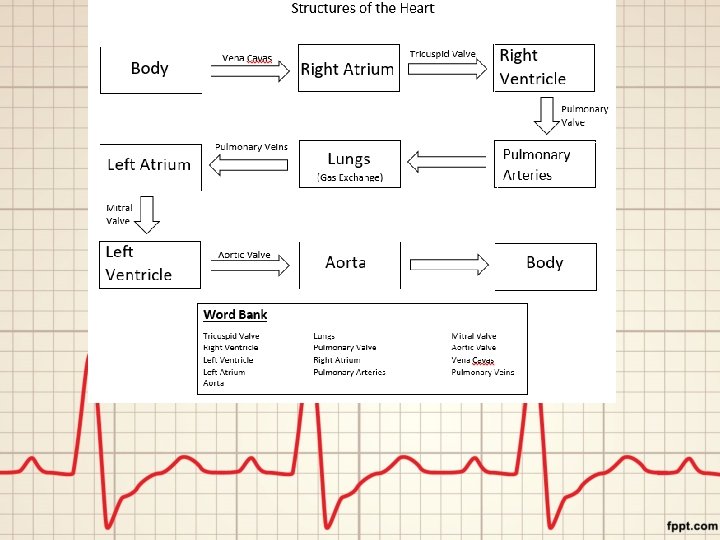
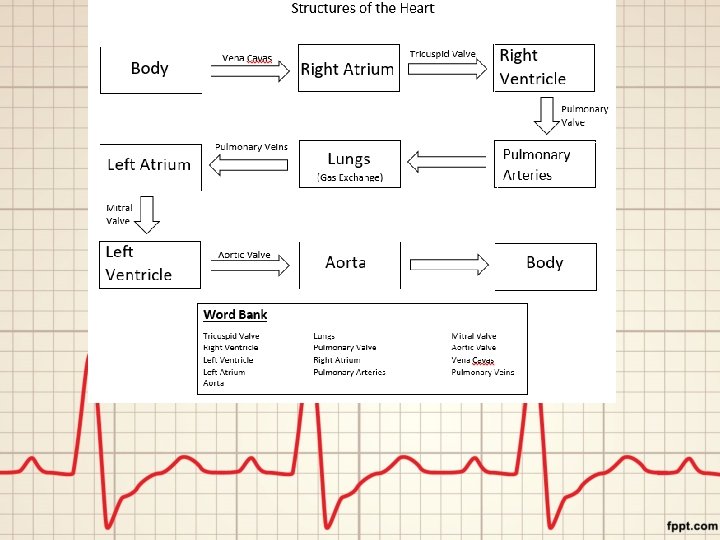
Heart Valves • Vena cavas (superior and inferior) bring deoxygenated blood to the right atrium • Tricuspid valve lies between the right atrium and right ventricle • Pulmonary valve lies between the right ventricle and pulmonary trunk • Pulmonary trunk receives blood from the right ventricle, separates into pulmonary arteries that lead to the lungs
Heart valves • Pulmonary veins deliver blood to the left atrium from the lungs (2 from the right and 2 from the left) • Mitral valve lies between the left atrium and left ventricle (also called the bicuspid valve) • Aortic valve lies between the left ventricle and the aorta • Aorta large artery that receives blood from the left ventricle
Heart Actions • Functions in a coordinated fashion – While the atria contract, the ventricles relax – While the ventricles contract, the atria relax – Both atria and ventricles relax for a brief time • This series of events constitutes a complete heartbeat, or cardiac cycle
Heart Actions • Pressure changes in the heart chambers open and close the valves • Pressure within the heart fluxuates depending on which valves should be open for blood flow
Heart Sounds • The sound of a heart beat are due to vibrations in the heart tissues when the valves close • First part—when ventricles contract & AV valves close • Second part—when ventricles relax & pulmonary and aortic valves close
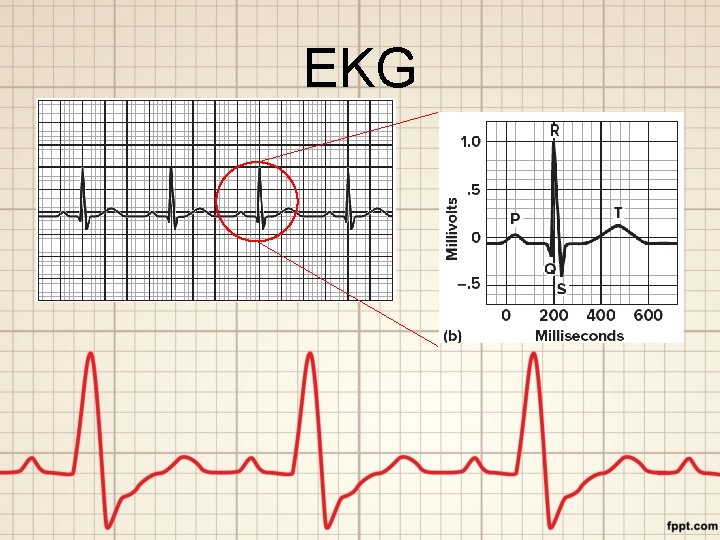
Electrocardiogram • An electrocardiogram (ECG/EKG) is a recording of the electrical changes in the myocardium (muscle layer of the wall of the heart) • The pattern is generated as action potentials stimulate cardiac muscle cells to contract
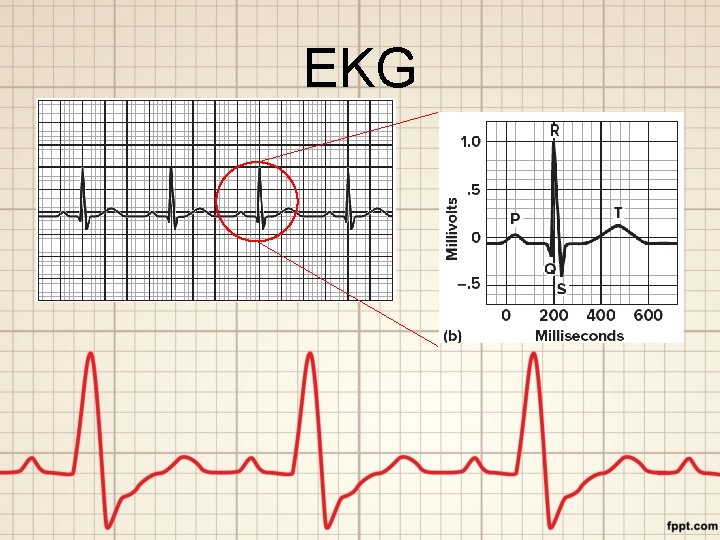
EKG
Heart Rates • Tachycardia is an abnormally fast heartbeat (more than 100 beats per minute) • Bradycardia is a slow heart rate (less than 60 per minute); may occur during sleep • Body temperature, certain drugs, heart disease can all affect heart rate
Blood Vessels • Closed circuit of tubes that carries blood from the heart to the body cells and back • Vessels include: – Arteries—strong, elastic vessels adapted for transporting blood away from the heart under relatively high pressure
Blood Vessels • Vessels include: – Arterioles—small branch of an artery that communicates with a capillary network – Capillaries—smallest blood vessels that connect to arterioles and allow for exchange of nutrients and waste
Blood Vessels • Vessels include: – Venules—vessel that transports blood from capillaries to veins – Veins—transport blood back to the atria and follow pathways that roughly parallel those of arteries
Blood Pressure • Force blood exerts against the inner walls of the blood vessels • Commonly refers to the pressure in arteries supplied by branches of the aorta
Arterial Blood Pressure • Rises and falls in a pattern corresponding to the phases of the cardiac cycle – Contraction of the ventricles squeezes blood out and into the pulmonary trunk and aorta which increases the pressure in these arteries • Maximum pressure during ventricular contraction is called the systolic pressure
Arterial Blood Pressure • When the ventricles relax: – Arterial pressure drops – Lowest pressure that remains in the arteries before the next ventricular contraction is called diastolic pressure
Pulse • The surge of blood entering the arteries during ventricular contraction expands the arterial walls • Pressure begins to drop almost immediately as contraction ends, and the arterial walls recoil • The alternating expanding and recoiling of arteries can be felt as a pulse
Factors the Influence Blood Pressure • Cardiac Output – The volume of blood pushed out from the ventricle per minute – If volume or heart rate increases, cardiac output increases = blood pressure increases
Factors the Influence Blood Pressure • Blood Volume – The sum of the formed elements and plasma in the vascular system – Blood pressure is directly proportional to blood volume in the system
Factors the Influence Blood Pressure • Peripheral Resistance – Force of friction between blood and the walls of the blood vessels – Blood pressure must overcome peripheral resistance if the blood is to continue flowing
Factors that Influence Blood Pressure • Blood Viscosity: – Difficulty with which the molecules of a fluid flow past one another – The greater the viscosity, the greater the resistance to flow
Control of Blood Pressure Blood pressure = Cardiac Output x Peripheral Resistance • Both cardiac output and peripheral resistance are controlled in part by baroreceptor reflexes • Baroreceptors are receptors that sense changes in blood pressure – If arterial pressure increases, baroreceptors send impulses to the brain to decrease heart rate