Cardiovascular System Blood Chapter 17 Blood the only
Cardiovascular System - Blood Chapter 17
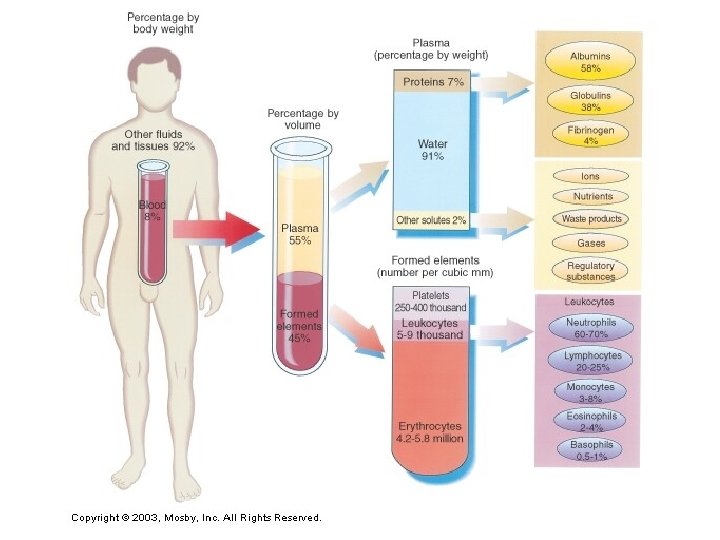
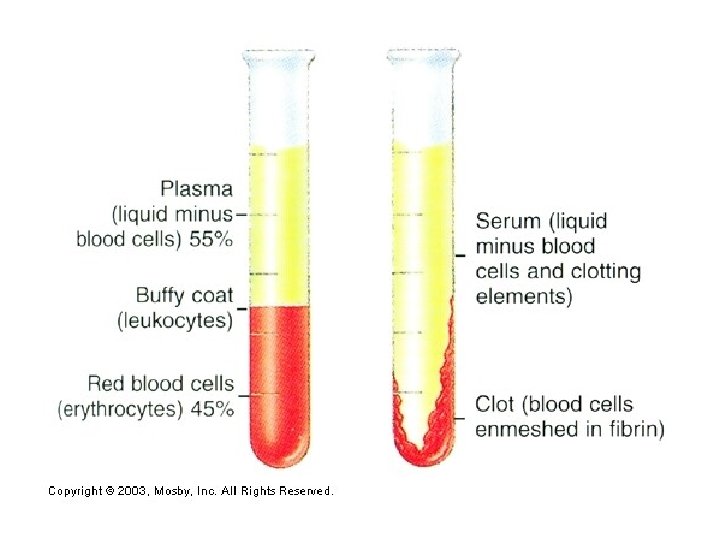
Blood - the only fluid tissue Average adult has approximately 5 L of blood Composed of formed elements and plasma Ø Formed elements are cells and cell fragments Ø Plasma is liquid portion of blood Ø Hematocrit – separating blood by centrifugation into its formed elements and liquid components Ø Erythrocytes (red blood cells) = 45% Ø Plasma = nearly 55% Ø Other cells and platelets = less than 1%
Functions of blood 1. Distribution A. delivery system for oxygen from the lungs and nutrients from the digestive system to all body cells. B. Transporting metabolic waste products from cells to elimination sites. C. Transporting hormones from endocrine glands to target organs. 2. Regulation A. Helps maintain proper body temperature and distributes heat throughout the body. B. Maintains proper p. H in body tissues. C. Maintains adequate fluid volume in the circulatory system.
3. Protection A. Preventing blood loss. B. Prevents infection with antibodies and leukocytes (white blood cells). Plasma Straw-colored sticky fluid that makes-up about 55% of blood volume. ☺ 90% water ☺ Also contains over 100 dissolved solutes including: nutrients, gases, hormones, waste products, ions, and plasma proteins. ☺Plasma proteins are most abundant solutes and are mostly produced by the liver ☺They are not taken up by cells ☺Maintain osmotic pressure of fluids, help to carry some nutrients, serve as clotting factors, etc. ☺Contents constantly adjusted to help maintain homeostasis.
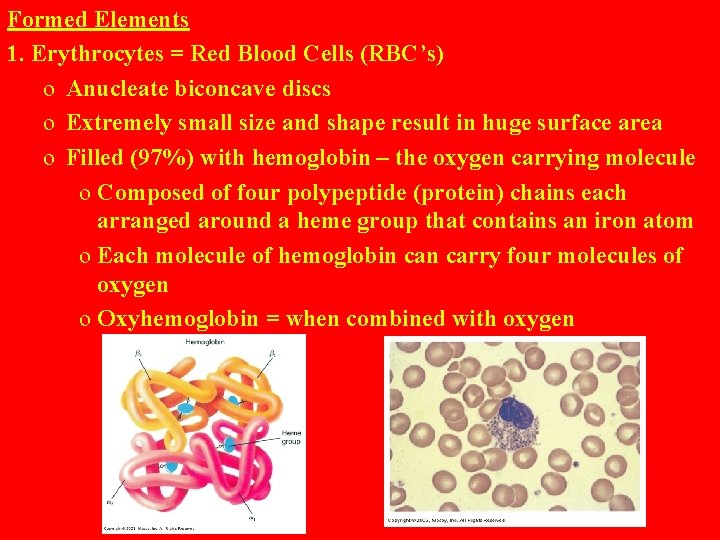
Formed Elements 1. Erythrocytes = Red Blood Cells (RBC’s) o Anucleate biconcave discs o Extremely small size and shape result in huge surface area o Filled (97%) with hemoglobin – the oxygen carrying molecule o Composed of four polypeptide (protein) chains each arranged around a heme group that contains an iron atom o Each molecule of hemoglobin carry four molecules of oxygen o Oxyhemoglobin = when combined with oxygen
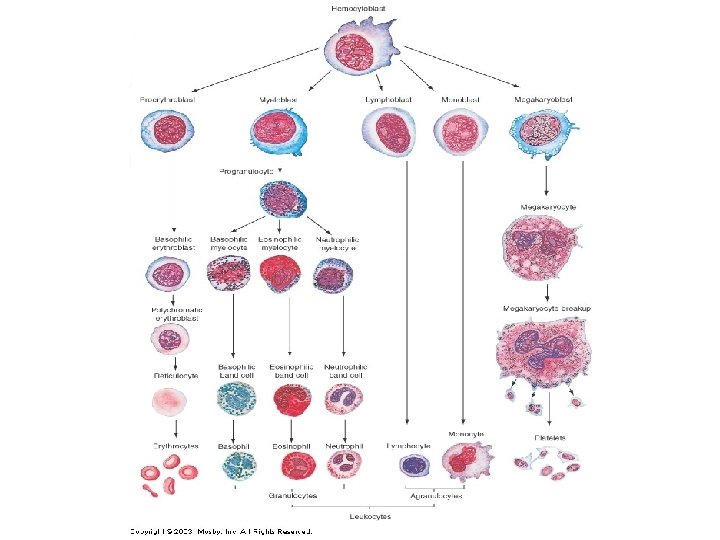
o o o o o Lack mitochondria and thus do not use any oxygen Useful lifespan is 100 -120 days – 100 million die/minute Production of erythrocytes General blood cell formation is hematopoiesis or hemopoiesis Occurs in red bone marrow All formed elements arise from hemocytoblasts, but they develop differently in response to specific hormones and growth factors. Erythrocytes are first released into the blood stream as reticulocytes (count these to estimate RBC production) Balance is maintained within narrow limits as too few lead to tissue hypoxia while too many make the blood too viscous. Erythropoietin is the primary hormone (from liver and kidneys) that stimulates RBC production in response to low oxygen delivery to tissues Iron and B-complex vitamins required
Disorders due to erythrocytes: A. Anemias - when blood has abnormally low oxygen-carrying capacity - hemorrhagic, hemolytic, aplastic, iron-deficiency, pernicious, abnormal hemoglobin (thalassemias and sickle-cell) B. Polycythemia - abnormal excess of RBC’s leading to thick blood 2. Leukocytes = White blood cells (WBC’s) - only formed elements that are complete cells - # vary with health - crucial in fighting disease - can leave circulatory system (diapedesis), move by ameboid movement, and use chemotaxis to find areas of tissue damage or infection.
- two main types: - Granulocytes have specialized granules in them - phagocytes - Agranulocytes lack these granules - Lymphocytes – most are located in the lymph tissues - key to immunity - T lymphocytes attack virus-infected cells and tumor cells directly - B lymphocytes produce antibodies - Monocytes – macrophages present w/ chronic infections Disorders due to Leukocytes: A. Leukemias – cancerous condition in which WBC’s proliferate and suppress or impair normal bone marrow infection B. Mononucleosis – viral disease
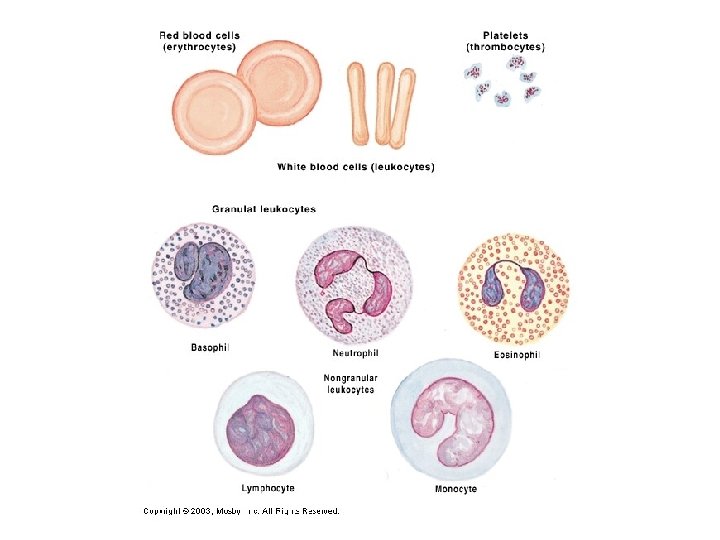

3. Platelets - cell fragments that function in blood clotting - stick to damaged blood vessels and form a temporary plug - release several clotting factors
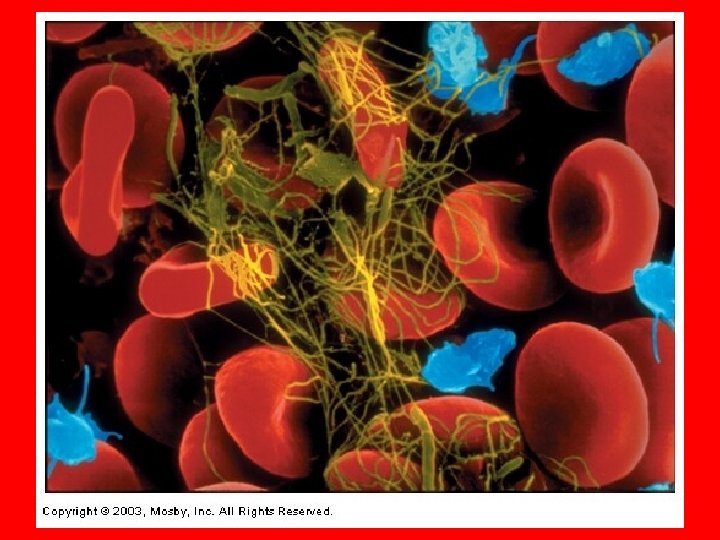
Hemostasis § Stoppage of bleeding § Three steps: 1. Vascular spasms - constriction of the damaged blood vessel 2. Platelet Plug Formation - platelets swell, form spiked processes, and become sticky - stick to exposed fibers of the damaged vessel and begin to release clotting factor chemicals 3. Coagulation – blood clotting - Prothrombin activator is formed from certain plasma proteins and calcium - Prothrombin activator transforms prothrombin to the active enzyme thrombin
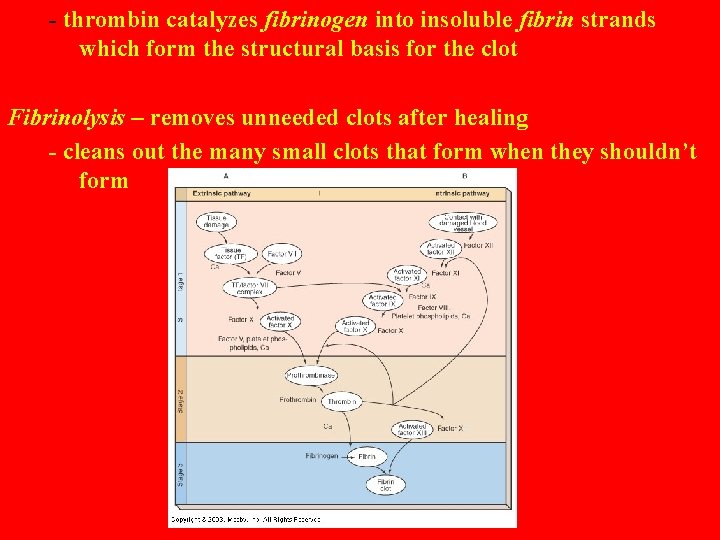
- thrombin catalyzes fibrinogen into insoluble fibrin strands which form the structural basis for the clot Fibrinolysis – removes unneeded clots after healing - cleans out the many small clots that form when they shouldn’t form
Disorders of Hemostasis 1. Thromboembolytic conditions - a clot that forms in an unbroken blood vessel is a thrombus - if a thrombus breaks loose and moves within the bloodstream it is an embolus - cause trouble when they get to a blood vessel that is too small for them to pass through and they block blood flow - caused by conditions which roughen the blood vessel endothelium or by slow blood flow - aspirin and heparin can decrease risk 2. Bleeding disorders - when the normal clotting procedure is interfered with - Platelet deficiency causes spontaneous bleeding from small blood vessels throughout the body - caused by problems in the bone marrow
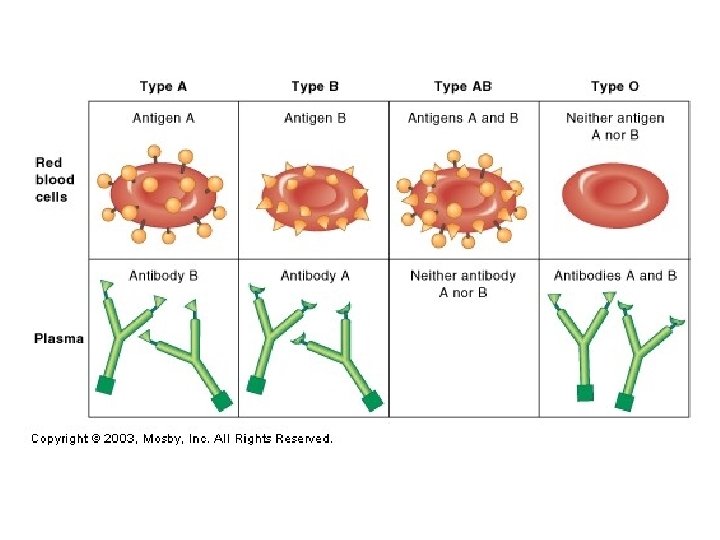
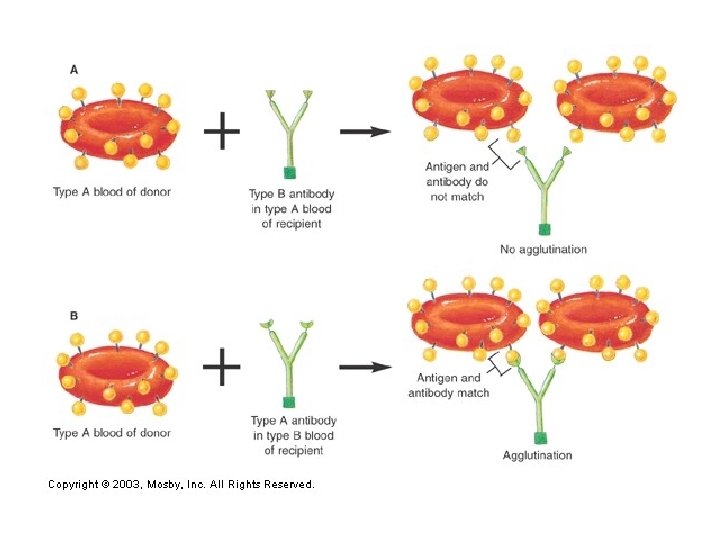
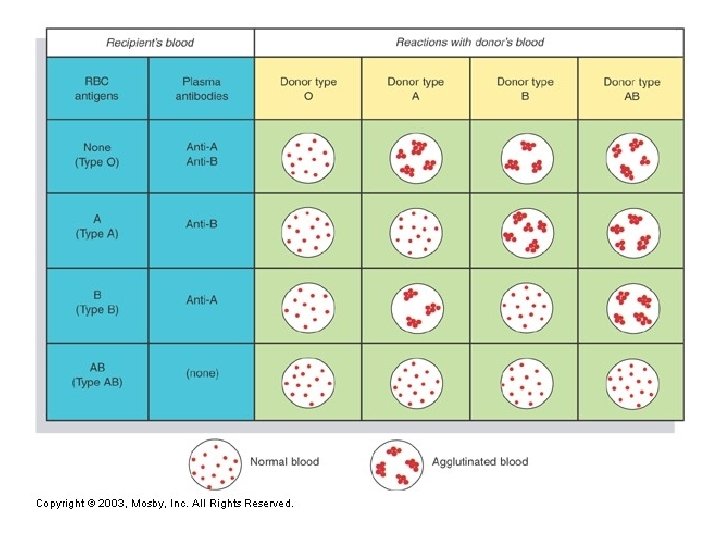
- Impaired liver function – can cause excessive bleeding because many of the clotting factors are produced by the liver - Hemophilias – genetic bleeding disorders - often sex-linked and more common in males - treat with injections of the missing factor Transfusions - when blood loss is severe whole blood transfusions are given - Human Blood Groups - Genetically determined - Result from certain antigens (proteins) on the surface of RBC’s - ABO and Rh blood groups cause strong transfusion reactions and are always matched in transfusions - Agglutination (clumping) of RBC’s occurs when RBC’s with the wrong antigen are transfused into another person
- when blood types are mixed incorrectly antibodies in the recipient plasma cause agglutination of the donated RBC’s - Transfusion reactions can block small blood vessels, cause fevers, chills, nausea, vomiting, and in severe cases renal failure which can be lethal - Rh factor is another antigen on the RBC’s + indicates the presence of the antigen
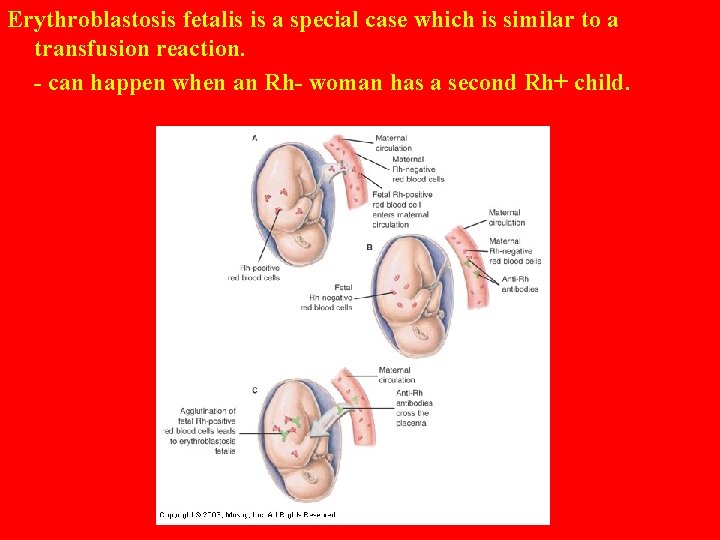
Erythroblastosis fetalis is a special case which is similar to a transfusion reaction. - can happen when an Rh- woman has a second Rh+ child.
THE HEART
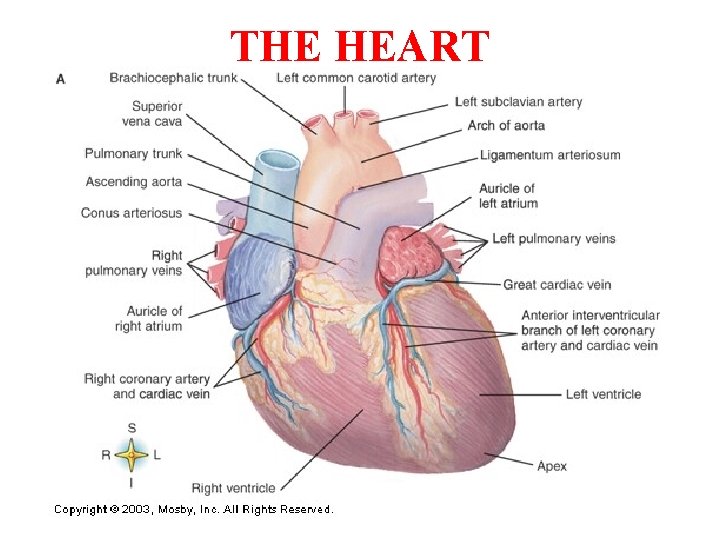
The Heart § Located in the mediastinum of the thoracic cavity. About the size of your fist § Surrounded by the double-layered pericardium which helps protect it and anchors it to other structures § Pericardial space between the layers allows the heart free movement Layers of the heart wall - epicardium – inner layer of the pericardium which is tightly attached to outer layer of the heart - myocardium – composed of cardiac muscle which actually does the contracting of the heart - made of branching fibers which spread the impulse between them - intercalated discs allow flow of ions from fiber to fiber
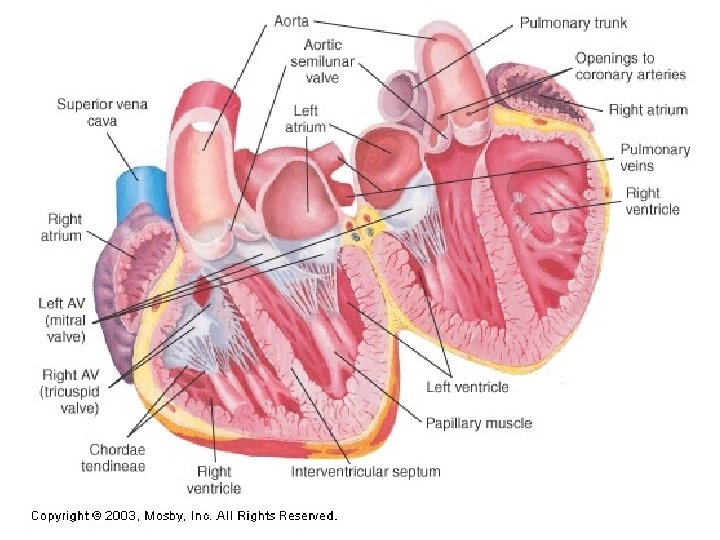
- endocardium – inner covering of the heart chambers Chambers of the heart: 1. Atria = receiving chambers - receive the returning blood from the body circulation - relatively small and thin-walled - Right Atrium - receives blood from the systemic circulation - superior vena cava (precava) from tissues above diaphragm - inferior vena cava (postcava) from tissues below diaphragm - coronary sinus collects blood draining from the myocardium itself - Left Atrium - receives blood from the pulmonary circulation via the pulmonary veins
2. Ventricles = discharging chambers - compose most of the mass of the heart - walls much thicker and more muscular than the atria - Right Ventricle – pumps blood to pulmonary trunk which branches into the pulmonary arteries to the lungs - Left Ventricle – pumps blood to the systemic circulation through the aorta 3. Valves of the heart - unidirectional flaps that impede backflow of blood - open and close due to blood pressure differences on their two sides A. Atrioventricular valves control flow between the atria and the ventricles - chordae tendinae anchor the valve flaps to the ventricles and keep the flaps from reversing up into the atria when the ventricles contract
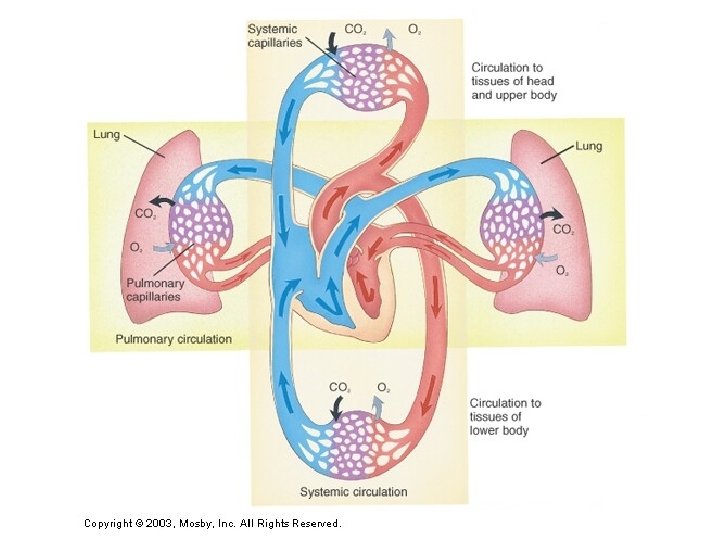
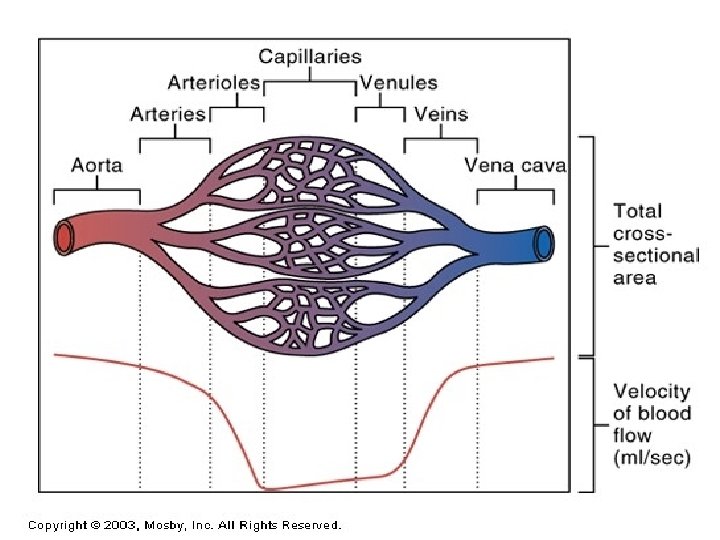
- when ventricles are relaxed these valves are open and blood can flow into the ventricles B. Semilunar valves - prevent backflow of blood into the ventricles when the ventricles relax - leaking valves are not always severely handicapping Blood Flow Through the Heart - heart acts as a double pump system to two distinct circuits - Right side is the pulmonary circuit - receives oxygen-poor blood and carbon dioxide-rich blood - enters right atrium which pumps it through the tricuspid valve (rt. Atrioventricular valve) to the right ventricle which pumps blood through the pulmonary semilunar valve to the lungs where gas exchange takes place
- Left side is the systemic circuit pump - left atrium receives oxygen-rich blood from the pulmonary vein and pumps it through the bicuspid valve (left atrioventricular valve) to the left ventricle which pumps blood through the aortic semilunar valve to the aorta which branches to all parts of the body - left ventricle is the largest and strongest chamber due to work load
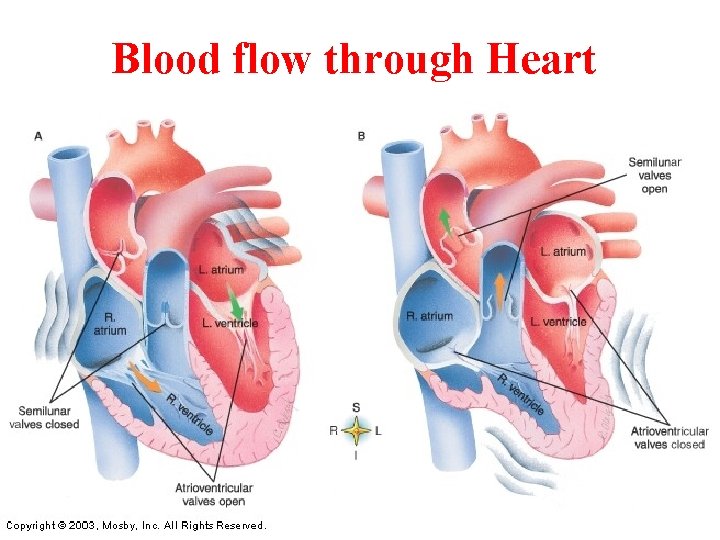
Blood flow through Heart
Blood supply to the heart - blood that flows through the heart chambers supplies very little of the needs of the heart - the two main coronary arteries branch off of the aorta as it leaves the heart. - heart attacks (myocardial infarctions) are caused by occlusion of a coronary artery - heart muscle requires 5% of the body’s blood supply - venous blood returns through the coronary sinus which dumps into the right atrium
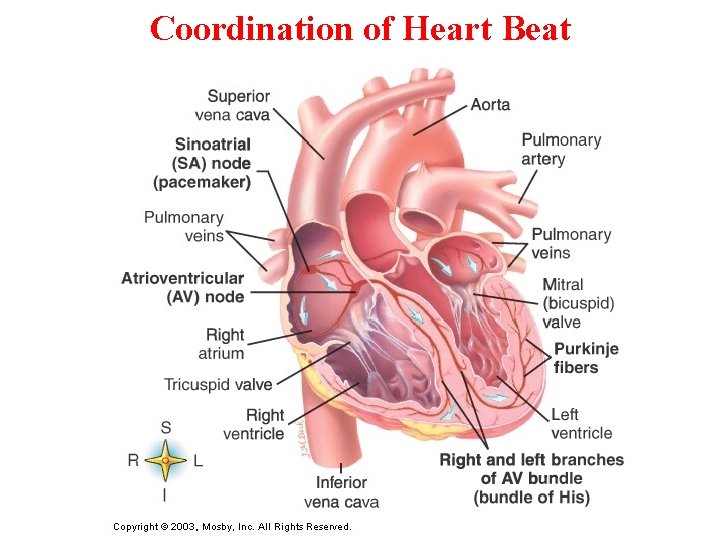
Coordination of Heart Beat
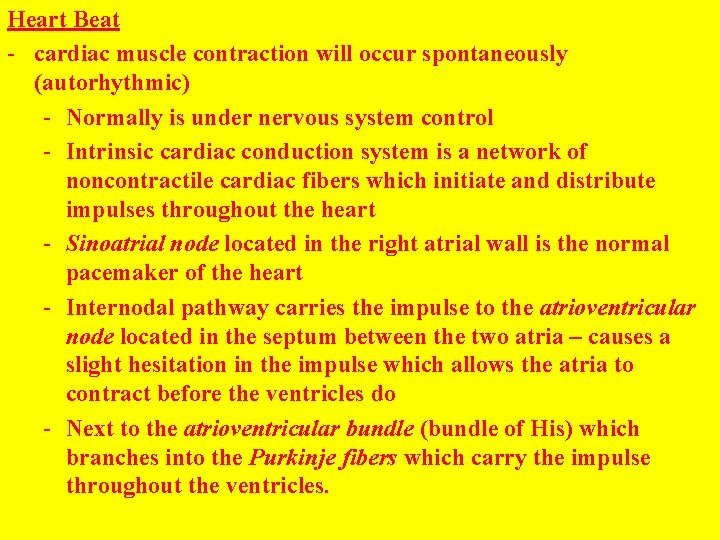
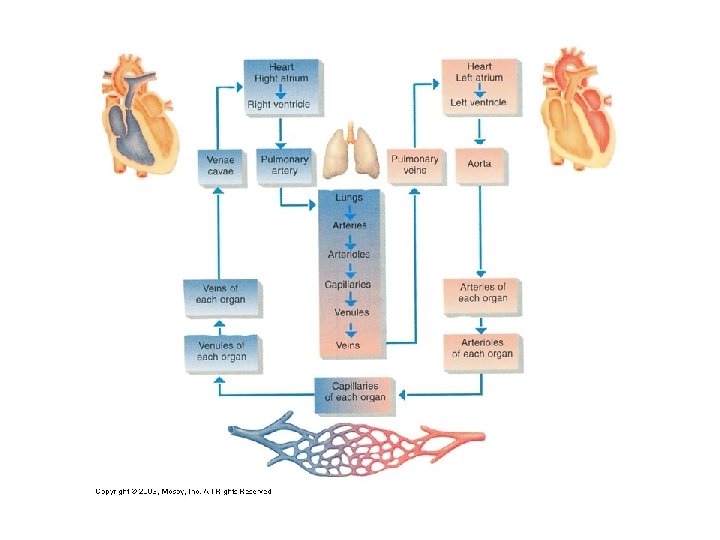
Heart Beat - cardiac muscle contraction will occur spontaneously (autorhythmic) - Normally is under nervous system control - Intrinsic cardiac conduction system is a network of noncontractile cardiac fibers which initiate and distribute impulses throughout the heart - Sinoatrial node located in the right atrial wall is the normal pacemaker of the heart - Internodal pathway carries the impulse to the atrioventricular node located in the septum between the two atria – causes a slight hesitation in the impulse which allows the atria to contract before the ventricles do - Next to the atrioventricular bundle (bundle of His) which branches into the Purkinje fibers which carry the impulse throughout the ventricles.
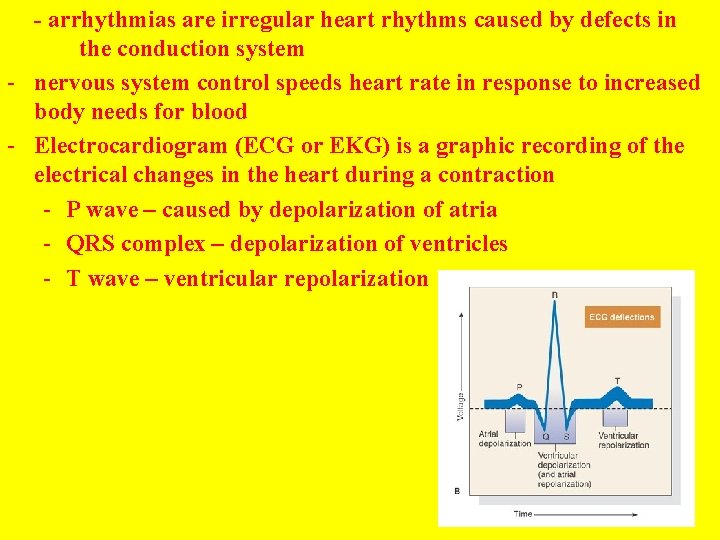
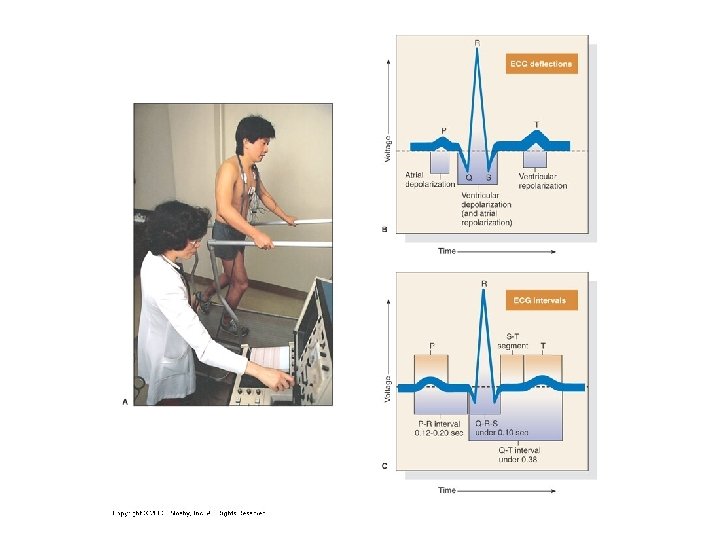
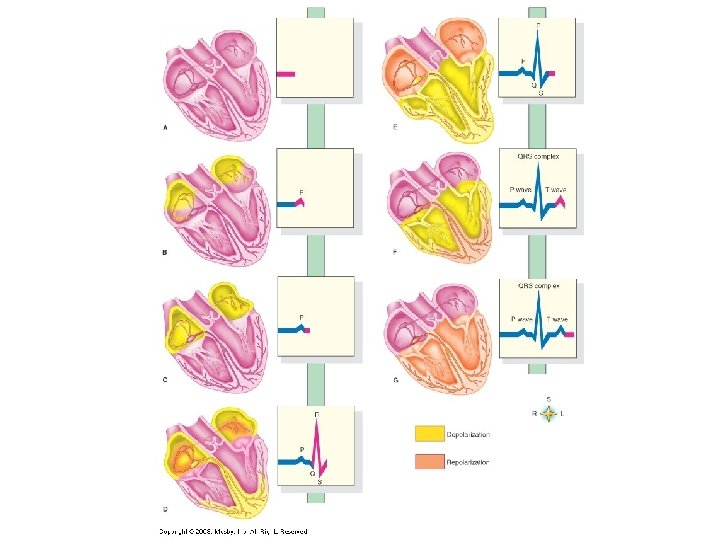
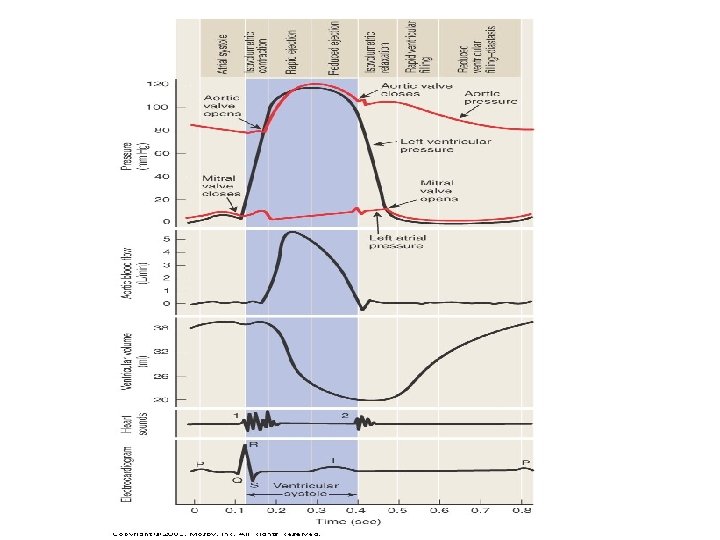
- arrhythmias are irregular heart rhythms caused by defects in the conduction system - nervous system control speeds heart rate in response to increased body needs for blood - Electrocardiogram (ECG or EKG) is a graphic recording of the electrical changes in the heart during a contraction - P wave – caused by depolarization of atria - QRS complex – depolarization of ventricles - T wave – ventricular repolarization
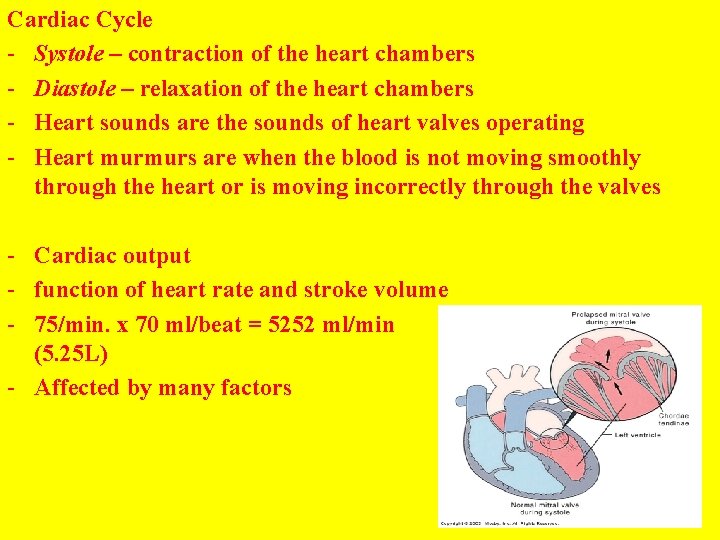
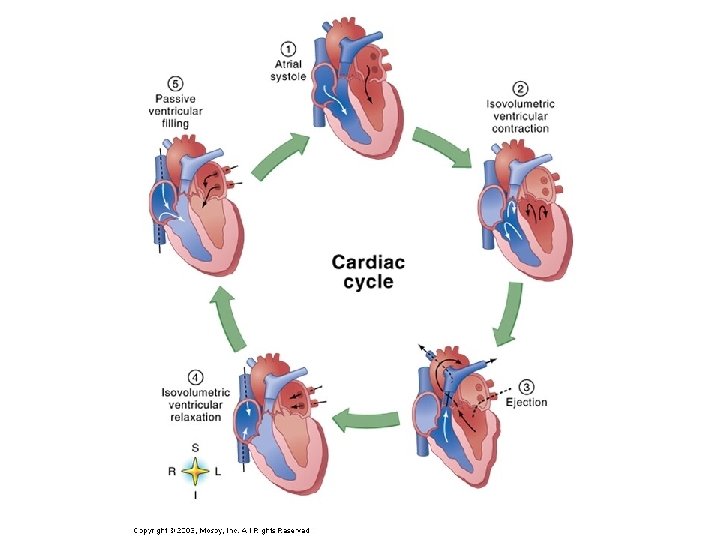
Cardiac Cycle - Systole – contraction of the heart chambers - Diastole – relaxation of the heart chambers - Heart sounds are the sounds of heart valves operating - Heart murmurs are when the blood is not moving smoothly through the heart or is moving incorrectly through the valves - Cardiac output - function of heart rate and stroke volume - 75/min. x 70 ml/beat = 5252 ml/min (5. 25 L) - Affected by many factors
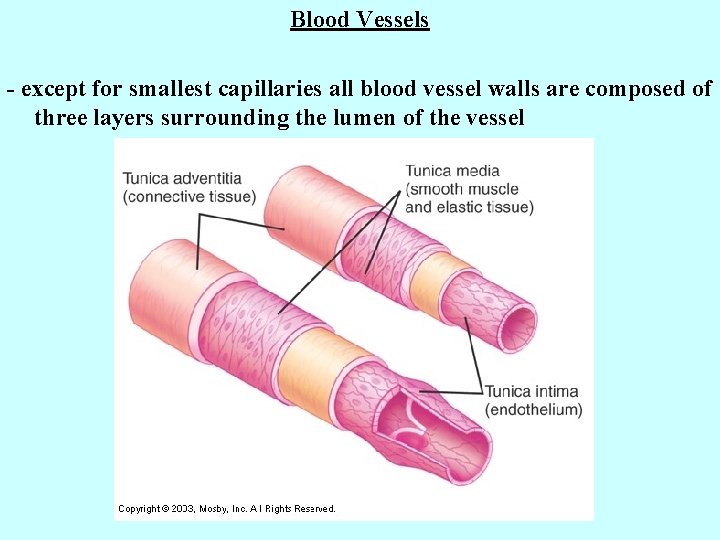
Blood Vessels - except for smallest capillaries all blood vessel walls are composed of three layers surrounding the lumen of the vessel
1. Tunica intima - innermost layer which is in contact with the blood - composed of simple squamous epithelium with closely fitting cells which form a slick surface with little friction on the blood 2. Tunica media - layer of circular muscles - controlled by sympathetic division of the autonomic nervous system - vasoconstriction – contraction of these muscles decreases vessel diameter - vasodilation – relaxation increases vessel diameter - very important in control of blood pressure 3. Tunica adventitia - tough outer layer that protects the blood vessel and helps to anchor it to surrounding tissues
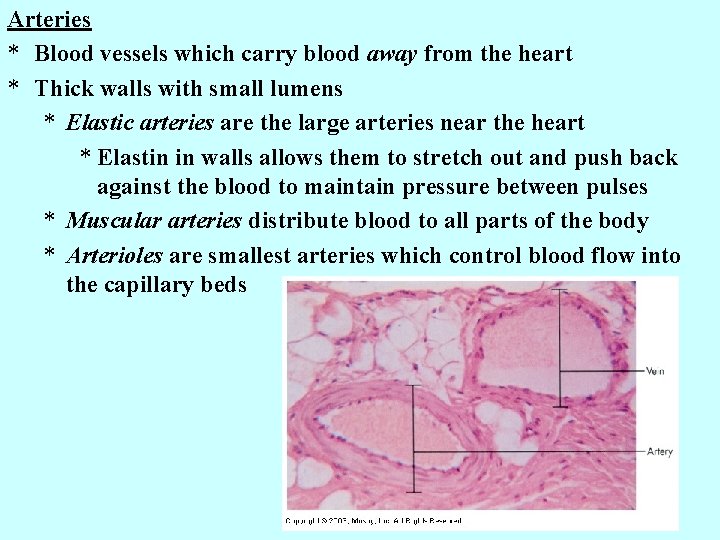
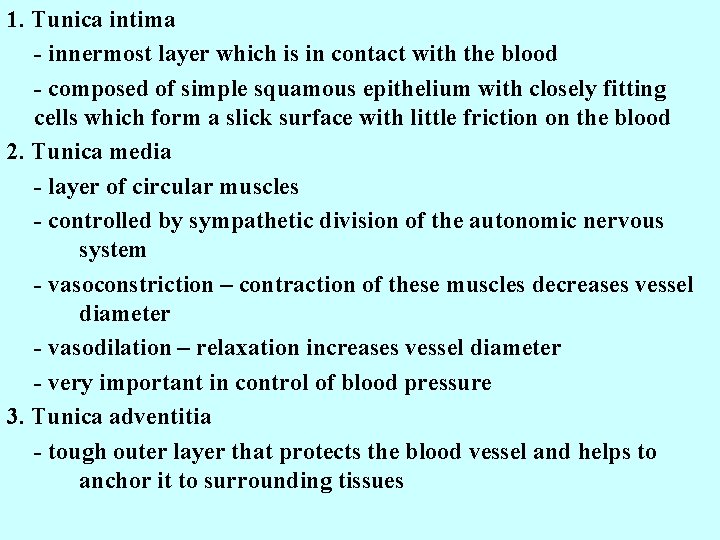
Arteries * Blood vessels which carry blood away from the heart * Thick walls with small lumens * Elastic arteries are the large arteries near the heart * Elastin in walls allows them to stretch out and push back against the blood to maintain pressure between pulses * Muscular arteries distribute blood to all parts of the body * Arterioles are smallest arteries which control blood flow into the capillary beds
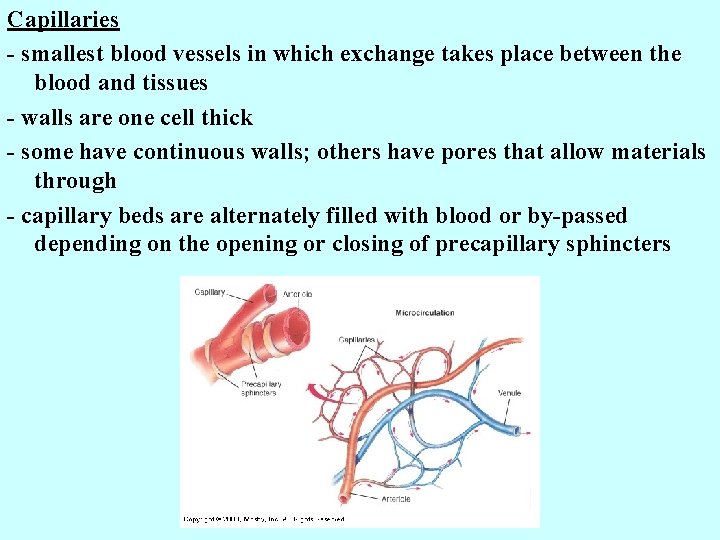
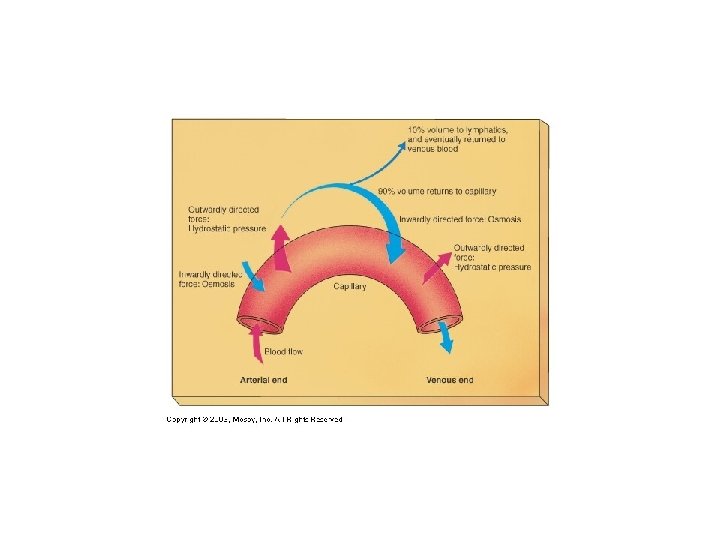
Capillaries - smallest blood vessels in which exchange takes place between the blood and tissues - walls are one cell thick - some have continuous walls; others have pores that allow materials through - capillary beds are alternately filled with blood or by-passed depending on the opening or closing of precapillary sphincters
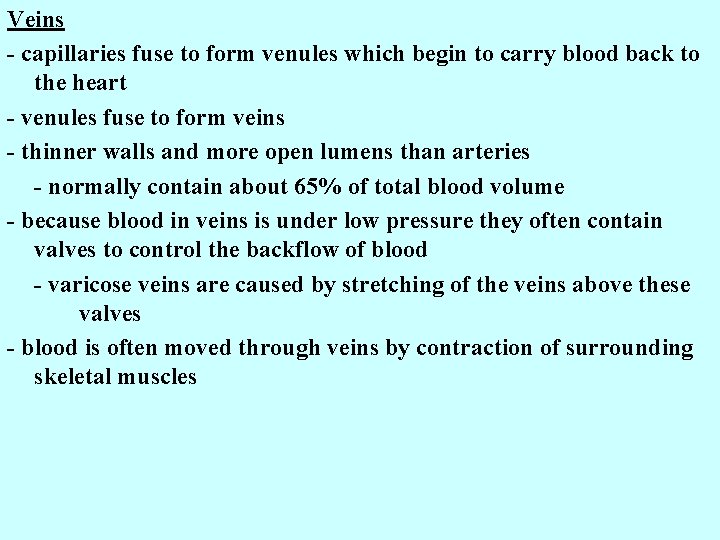
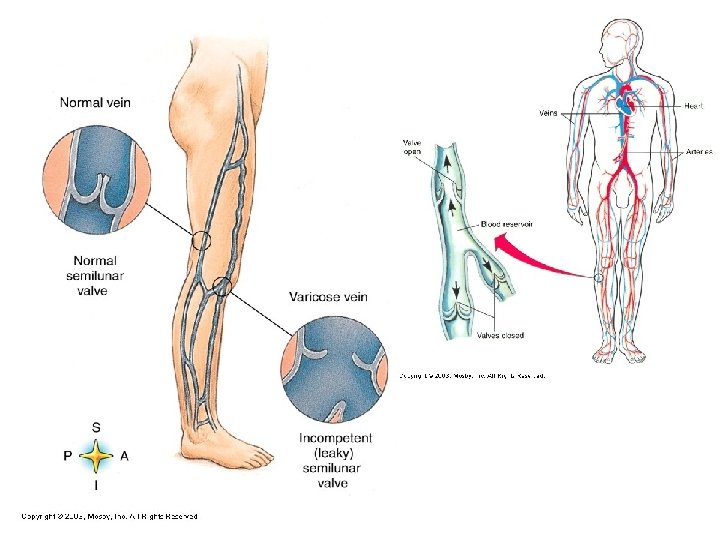
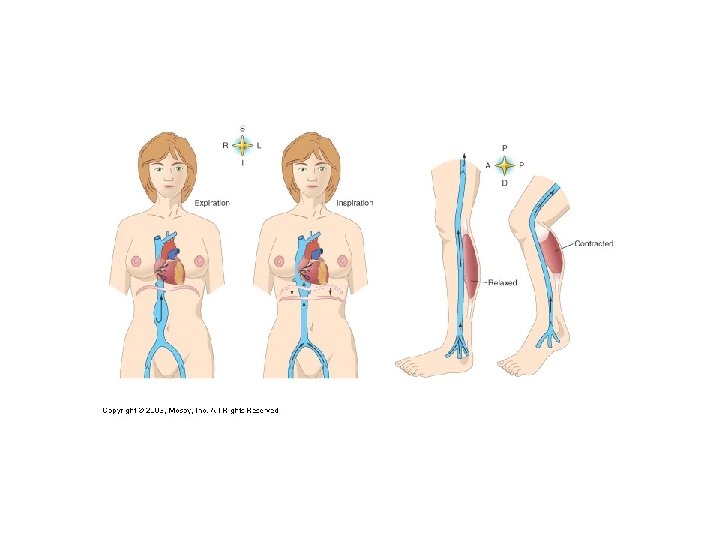
Veins - capillaries fuse to form venules which begin to carry blood back to the heart - venules fuse to form veins - thinner walls and more open lumens than arteries - normally contain about 65% of total blood volume - because blood in veins is under low pressure they often contain valves to control the backflow of blood - varicose veins are caused by stretching of the veins above these valves - blood is often moved through veins by contraction of surrounding skeletal muscles
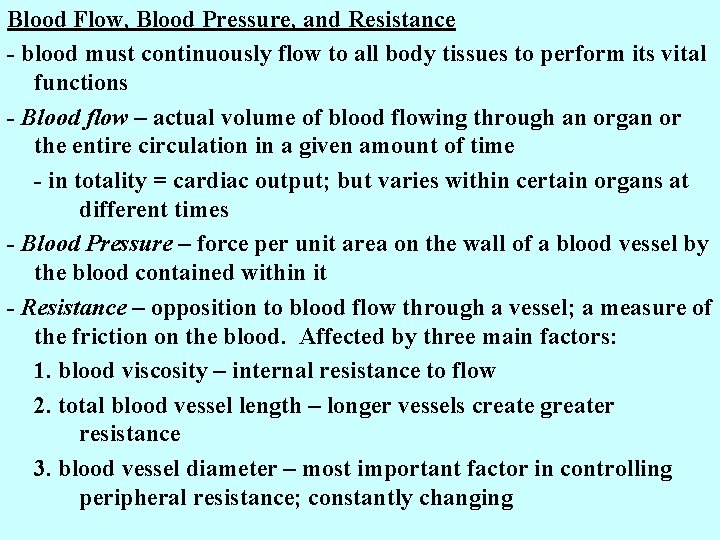
Blood Flow, Blood Pressure, and Resistance - blood must continuously flow to all body tissues to perform its vital functions - Blood flow – actual volume of blood flowing through an organ or the entire circulation in a given amount of time - in totality = cardiac output; but varies within certain organs at different times - Blood Pressure – force per unit area on the wall of a blood vessel by the blood contained within it - Resistance – opposition to blood flow through a vessel; a measure of the friction on the blood. Affected by three main factors: 1. blood viscosity – internal resistance to flow 2. total blood vessel length – longer vessels create greater resistance 3. blood vessel diameter – most important factor in controlling peripheral resistance; constantly changing
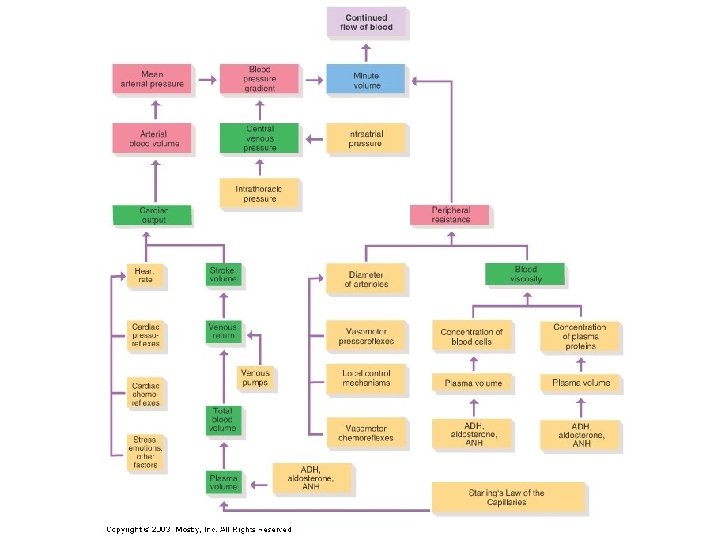
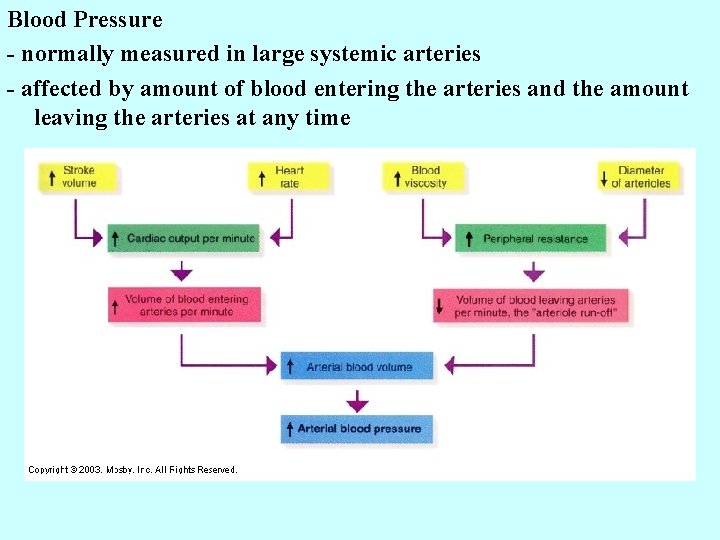
Blood Pressure - normally measured in large systemic arteries - affected by amount of blood entering the arteries and the amount leaving the arteries at any time
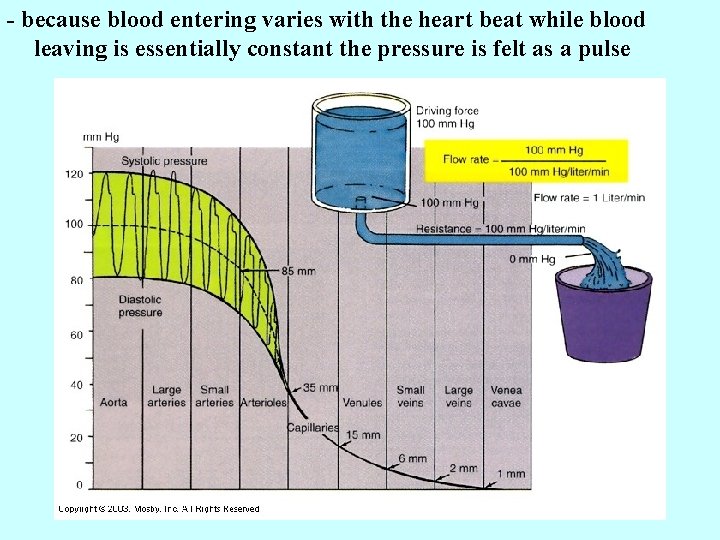
- because blood entering varies with the heart beat while blood leaving is essentially constant the pressure is felt as a pulse
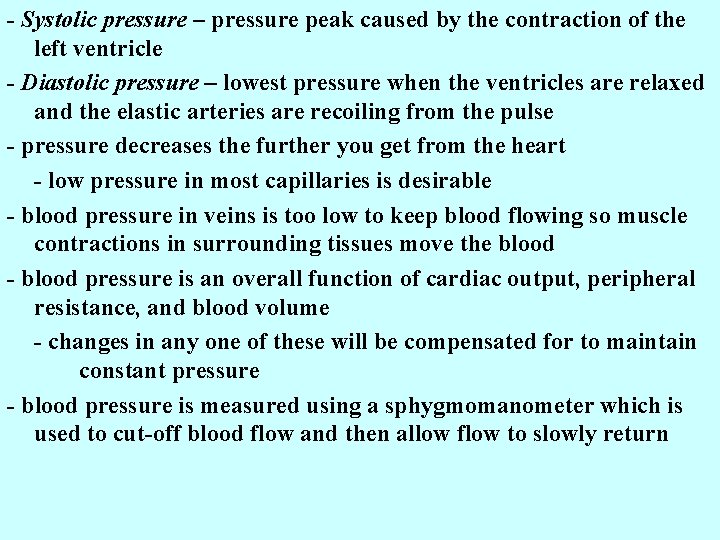
- Systolic pressure – pressure peak caused by the contraction of the left ventricle - Diastolic pressure – lowest pressure when the ventricles are relaxed and the elastic arteries are recoiling from the pulse - pressure decreases the further you get from the heart - low pressure in most capillaries is desirable - blood pressure in veins is too low to keep blood flowing so muscle contractions in surrounding tissues move the blood - blood pressure is an overall function of cardiac output, peripheral resistance, and blood volume - changes in any one of these will be compensated for to maintain constant pressure - blood pressure is measured using a sphygmomanometer which is used to cut-off blood flow and then allow flow to slowly return
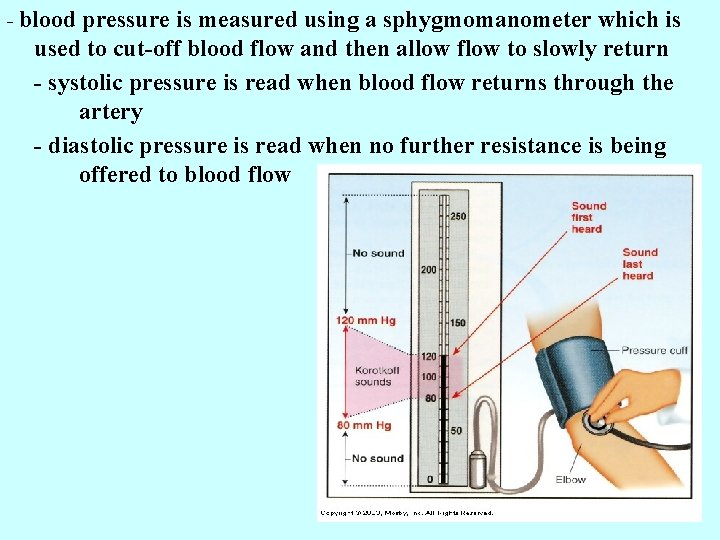
- blood pressure is measured using a sphygmomanometer which is used to cut-off blood flow and then allow flow to slowly return - systolic pressure is read when blood flow returns through the artery - diastolic pressure is read when no further resistance is being offered to blood flow
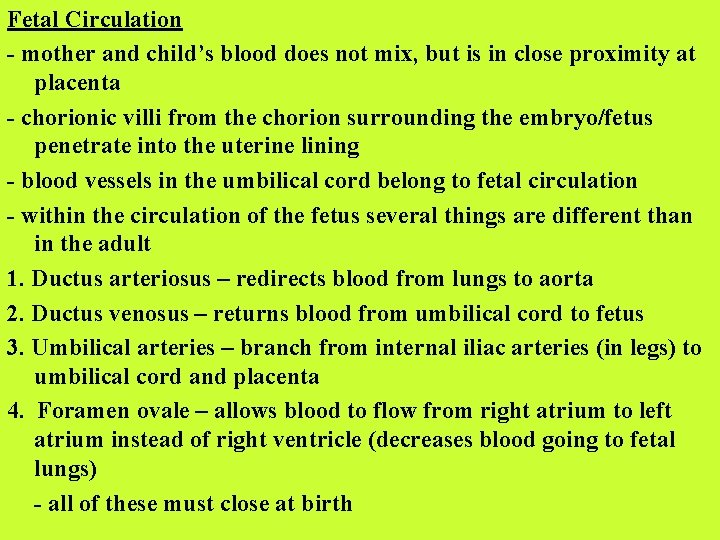
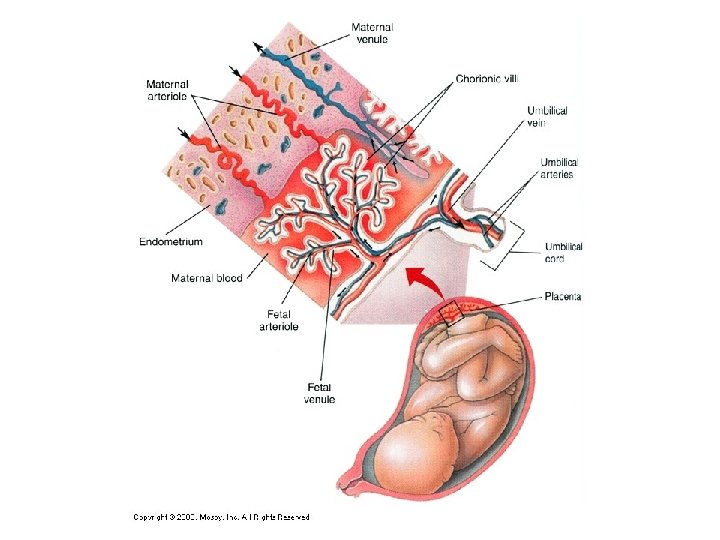
Fetal Circulation - mother and child’s blood does not mix, but is in close proximity at placenta - chorionic villi from the chorion surrounding the embryo/fetus penetrate into the uterine lining - blood vessels in the umbilical cord belong to fetal circulation - within the circulation of the fetus several things are different than in the adult 1. Ductus arteriosus – redirects blood from lungs to aorta 2. Ductus venosus – returns blood from umbilical cord to fetus 3. Umbilical arteries – branch from internal iliac arteries (in legs) to umbilical cord and placenta 4. Foramen ovale – allows blood to flow from right atrium to left atrium instead of right ventricle (decreases blood going to fetal lungs) - all of these must close at birth
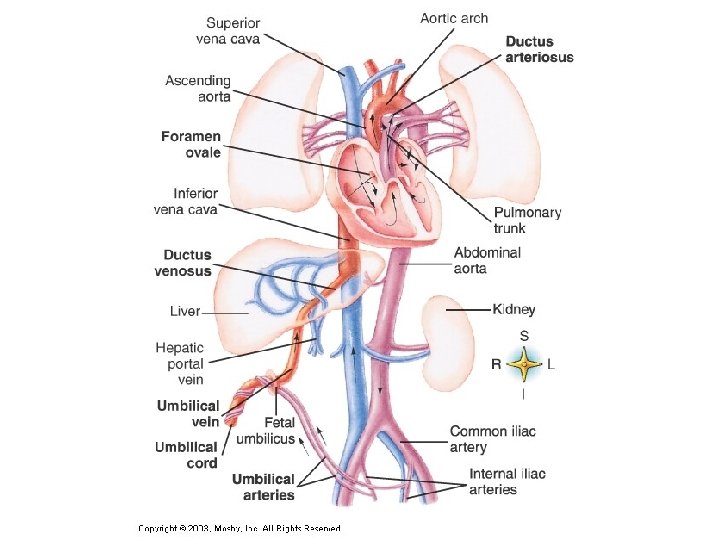
Diseases and disorders of the Cardiovascular System 1. Hypotension – low blood pressure 2. Hypertension – high blood pressure - common in obese people due to greater total length of blood vessels - chronic hypertension is often a result of increased peripheral resistance - often caused by atherosclerosis - primary hypertension has no discernable cause but is affected by: diet, obesity, age, race, heredity, stress, smoking
3. Circulatory Shock - most often caused by blood loss 4. Heart attack - caused by blockage of the coronary arteries
- Slides: 62