Cardiovascular Aging Dorothy D Sherwood M D Health




- Slides: 42
Cardiovascular Aging Dorothy D. Sherwood, M. D. Health Core Physician Group Presbyterian Hospital of Dallas Division of Geriatrics July 26 th, 2006
Epidemiology • Currently, 12 % of the population is >65 years of age – 35 million people. • In 2030, 20% of the population will be >65 years of age – 71 million people – one in five. • Half of the people > 65 years of age have after tax incomes at the poverty level.
Epidemiology • Cardiovascular disease is the leading cause of death in the population >65 years. • One half to two thirds of the population > 65 years have hypertension. • The leading discharge diagnosis for> 65 years is congestive heart failure.
Epidemiology • Compelling data indicates that aggressive treatment of hypertension, heart failure, coronary artery disease, and hyperlipidemia in those between the ages of 65 and 74 reduces morbidity and mortality. • Few trials have enrolled those over 75 or those with co-morbid conditions.
Pathophysiology • Hallmarks of cardiovascular aging include – Increase in systolic blood pressure – Increase in pulse pressure and pulse wave velocity (PWV) – Increase in left ventricular mass – Increase in CAD – Increase in Atrial fibrillation

Pathophysiology • Aging is associated with a: – Decrease in early left ventricular diastolic filling. – Decrease in maximal heart rate – Decrease in maximal cardiac output – Decrease in maximal aerobic capacity – Decreased exercise induced augmentation of LVEF and heart rate – Decreased vasodilatation in response to beta adrenergic stimulation or endothelial mediated vasodilatation.
Pathophysiology • Cellular, enzymatic, and molecular alterations in the arterial vessel: – Smooth muscle cells (SMC) migrate to the intima, causing intimal thickening. – Metalloproteinases, angiotensin II, transforming growth factor beta, intracellular cell adhesion molecules, result in increased production of collagen, collagen cross linking, fibronectin, calcification, in the media with decrease in elastin in the media – leading to stiff vessel. – Reduced endothelial function due to apoptosis and senescence results in decreased NO – Decreased vasodilatory response to beta adrenergic agonists and alpha adrenergic antagonist
Pathophysiology • This results in arterial dilation with increased arterial stiffness and decreased NO induced vasodilatation.
Pathophysiology • Cellular, enzymatic, and molecular alterations in the Heart: – Similar to those in the arterial wall – with similar enzymatic changes resulting in increased collagen cross linking, increased fibronectin, decrease in elastin – In the atria, decrease in sinus node cells, and alterations in the extracellular matrix results in sinus node dysfunction leading to atrial fibrillation; similar changes occur in the AV node.
Pathophysiology • Reduced, but hypertrophied myocytes result in alteration in calcium channels, leading to – Prolongation of contraction and relaxation of the myocardium with aging.
Pathophysiology • Changes in the intravascular environment with age: – Increase in prothrombotic factors s such as V, VIII, IX, plasminogen, resulting in impaired fibrinolyisis – Increased pro-thrombotic cytokines – especially interleukin 6 – All of these potentiate the development of atherosclerosis
Pathophysiology • Autonomic nervous system – Decreased number of alpha and beta adrenergic cells and decreased function of the cells with aging. – Decreased dopaminergic responsiveness with aging – Decreased vascular response to cholinergics, but increased central nervous system response

Pathophysiology • The combined effect of the changes in the autonomic nervous system results in a decreased baroreceptor response in the elderly and decreased ability to respond to stress.
Pathophysiology • We can impact some of the age related changes: – Exercise increases endothelial function – Exercise decreases arterial wall stiffness – ACEI, ARB, Aldosterone inhibitors, Beta blockers may influence remodeling of the vessels and the myocardium.
Pharmacodynamic effects of aging • Suffice it to say, that elderly are highly sensitive to: – The therapeutic effects of a drug: i. e. a direct vasodilator such a prazocin; the rate effects of beta blockers – The toxic effects of the drug: i. e. digoxin toxicity occurs at a much lower dose in the elderly – The drug-drug interactions: ACEI and NSAID for example –

Pharmacodynamic effects of aging • Elderly patients can not take a joke! – Look up every drug before you give it – If renally cleared – adjust the dose – i. e. beta blockers are renally cleared. – Know the drug-drug interactions – Know the complications – Start low – go slow, and re-address need for drug at every visit.
Hypertension • Measure BP in both arms, supine, sitting, and standing. – Elderly patients are very susceptible to orthostatic hypotension. • The risk of hypertension is greater in the elderly, at least up to age 80, than in the younger population, and the reduction in CAD and heart failure is greater in the elderly with treatment than in the young.
Hypertension • Limited data from placebo controlled trials reveals a decrease in strokes and heart failure in patients over the age of 80 with treated hypertension, but no difference in mortality.
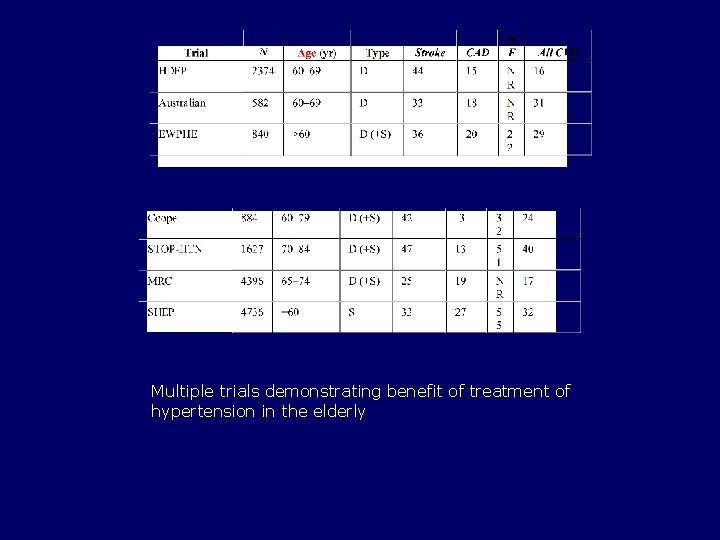
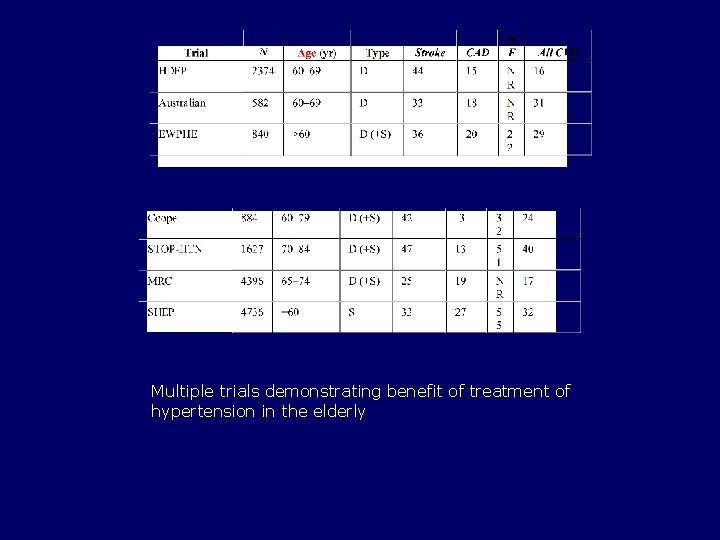
Multiple trials demonstrating benefit of treatment of hypertension in the elderly
Hypertension • Thiazides are as effective as any other drug for first line treatment. – Risk of hyponatremia – Risk of incontinence – Risk of hypokalemia – Never go above 25 mg, start at 6. 25 mg
Hypertension • To evaluate the best second line therapy for each patient, take into account their co-morbid conditions, and the drug-drug interactions that will occur. Use www. geriatricsatyourfingertips. com. • Or JNC 7 to determine the best choice
Hypertension • Postural Hypotension – a fall of 20 mm Hg with standing is associated with a marked increase in falls. – Increases the risk associated with antidepressants, anti-psychotics, and antiparkinsonian medications – Increases the risk associated with postprandiol hypotension • Greatest fall in BP is 1 hour after eating, returning to normal 3 to 4 hours after eating
CAD • Autopsy studies show that > 50% of the men over the age of 60 have significant CAD with increase in the incidence of multi-vessel disease and left main disease • The life time risk for developing CAD is estimated to be 1 in 3 for men and 1 in 4 for women
CAD • By the age of 80, 20 to 30% of men and women have symptomatic CAD. • History is atypical: epigastric discomfort; shoulder pain; back pain; SOB; nausea or no symptoms at all • Symptoms not necessarily related to exertion.
CAD • Testing: – Exercise stress testing has about an 80% sensitivity and 75% specificity – The addition of an echocardiogram or nuclear study improves the validity of the test – In men and women who can not exercise, dobutamine or adenosine can be used. – Due to high levels of calcification in the arteries, CT may not be useful in the elderly.
CAD • Treatment: the same as the younger population, unless there is less than a 2 year life expectancy. – Heart Protection Study showed benefit in patients with disease treated with statins – There is no data regarding statins and primary prevention in patients over the age of 75
CAD • Age is a risk factor for myopathy with statin therapy. Therefore, the lowest effective dose should be used in this population. • Beta blockers, ACEI, and long-acting nitrates should be used. – Avoid Beta blockers in SA or AV nodal disease – Avoid Calcium Channel Blockers
CAD • Revascularization: – BARI study – 109 patients ages 65 to 83. – CABG vs. PTCA – CABG associated with increased early mortality and morbidity, but less angina and less repeat procedures – Stroke was more common after CABG and heart failure after PTCA – 5 year survival was 86% for CABG and 81 % for PTCA – In hospital mortality for CABG in patients over 75 is 6 to 8% and stroke is 3 to 6%
CAD • TIME trial compared re-vasularization to optimal medical therapy. At 6 months, revascularization was favored, but a 1 year there was no difference in outcomes • Data is limited in the use of drug eluting stents and off pump bypass.

CAD • Treatment of acute MI in the elderly with thrombolysis or primary angioplasty is associated with better outcomes, but also, with increased risk of complications including hemorrhage and stroke. – Thin, black, female, prior cva, Bp >160 associated with increased risk of ICH
CAD • Post MI treatment – Beta Blockers, ACEI, ASA, Statins all have been shown to be of benefit in the elderly. • Start with lower doses and titrate carefully
CHF • Five year mortality is 50% for patients with systolic impairment and 25% for patients with diastolic HF • There is a 4 fold increase in mortality in patients with diastolic dysfunction compared to those without HF. • Age is associated with HF with preserved systolic function
CHF • Exercise intolerance is the mark of heart failure • Nocturnal cough, PND, DOE are common signs of heart failure, but may not be recognized – Less than 50% of patients with moderate diastolic HF by doppler had the diagnosis of Hf
CHF • Physical exam in the elderly is not easy – they all have edema; their neck veins are always distended or appear to be; S 3 and rales are only present when decompensated. • One must rely on ECHO and BNP to diagnose heart failure at times.
CHF • Treatment – Not good data in the elderly – most CHF studies are with patients with systolic dysfunction. Women and the frail elderly are not included at all.
CHF • Treatment of Systolic Failure – Control BP – Diurese – Control heart rate if in A fib. – ACEI or ARB gently – Beta blocker gently – Exercise
CHF • Diastolic Dysfunction – Diuretics – ACEI or ARB gently – Beta blockers gently – Exercise
Arrhythmia • Up to 90 % of the sinus node cells are lost by the age of 75! • Resting heart rate is not effected by age, but maximal heart rate and beat to beat variability are both reduced. • SN response to beta adrenergic and parasympathetic stimulation is reduced.
Arrhythmia • EKG shows prolonged PR and LAD • Arrhythmias requiring treatment – Bradycardia due to SA or AV nodal dysfunction – A Fib – 8 to 10% of 80 year olds have A fib. • 50% of patients with A fib are > 75 years old
Arrhythmia • A fib – Focus should be on anticoagulation for stroke prevention and rate control. Rarely is rhythm control needed or possible. • Warfarin – INR 2 to 2. 5 – Don’t forget – associated with osteoporosis • ASA 325 mg in very elderly or very debilitated.
Summary • CV aging is associated with – Decreased arterial compliance – Decreased cardiac compliance – Decreased maximal heart rate and EF with exercise/stress – Decreased adrenergic sensitivity – Increased systolic hypertension – Increased LV mass – Increased CAD – Increased arrhythmias
Summary • Treatment • Encourage Exercise and: – Monitor orthostatic BP. – Start low, go slow. – Avoid vasodilators if possible. – May have increased sensitivity to bradycardia from beta blockers, calcium channel blockers. – Watch for drug/drug interactions. – Monitor frequently, be careful.
 Halimbawa ng cardiovascular endurance
Halimbawa ng cardiovascular endurance Sherwood receiver test
Sherwood receiver test Sherwood parkdale
Sherwood parkdale Marking
Marking Rivers passing through sherwood forest
Rivers passing through sherwood forest Sherwood transceiver ratings
Sherwood transceiver ratings Bw contest
Bw contest Community midwife nottingham
Community midwife nottingham The egg sherwood anderson summary
The egg sherwood anderson summary Switch light os
Switch light os Sherwood parkdale skating club
Sherwood parkdale skating club Newark and sherwood homes bidding
Newark and sherwood homes bidding Dhl business park
Dhl business park William carey dorothy plackett
William carey dorothy plackett Genie wiley nature vs nurture
Genie wiley nature vs nurture Dorothy stringer term dates
Dorothy stringer term dates Behavioral system model by dorothy johnson
Behavioral system model by dorothy johnson Dorothy height sorority
Dorothy height sorority A telephone call dorothy parker
A telephone call dorothy parker Dorothea puente serial killer
Dorothea puente serial killer Dorothy jacks cfa aas
Dorothy jacks cfa aas Dorothy edgers pearl harbor
Dorothy edgers pearl harbor Eaton arc flash handbook
Eaton arc flash handbook Subsystem in nursing
Subsystem in nursing Dorothy johnson nursing theory
Dorothy johnson nursing theory Penelope dorothy parker
Penelope dorothy parker Dorothy chun
Dorothy chun Dorothy wilding
Dorothy wilding The richer the poorer by dorothy west
The richer the poorer by dorothy west Definicija zdravstvene njege po virginiji henderson
Definicija zdravstvene njege po virginiji henderson Dr dorothy serna
Dr dorothy serna Dorothy stubbe
Dorothy stubbe Dorothy f schmidt college of arts and letters
Dorothy f schmidt college of arts and letters Dorothy johnson center
Dorothy johnson center Dorothy stringer slg
Dorothy stringer slg The wizard of oz and populism
The wizard of oz and populism Dorothy perkins stockists
Dorothy perkins stockists Dorothy koch
Dorothy koch Capillary bed labeled
Capillary bed labeled Riesgo cardiovascular por perimetro abdominal
Riesgo cardiovascular por perimetro abdominal Maniobra de azoulay
Maniobra de azoulay What makes up the circulatory system
What makes up the circulatory system Rias cardiovascular
Rias cardiovascular