CARDIOPULMONARY SYSTEMS CLINICAL ANATOMY AND PHYSIOLOGY NOTE Thorough
- Slides: 31
CARDIO-PULMONARY SYSTEMS CLINICAL ANATOMY AND PHYSIOLOGY NOTE Thorough knowledge of anatomy and physiology is an vital pre-requisite for efficient evaluation and interventions. 1
O₂ O₂ O₂ RESPIRATION O₂ O₂ O₂ ₂ CO CO₂ C O₂ ₂ CO CO ₂ CO₂ • The goals of respiration are to provide oxygen to the tissues and to remove carbon dioxide. Respiration can be divided into: (1)Pulmonary ventilation. (2) Diffusion of oxygen and carbon dioxide between the alveoli and the blood (3) Transport of oxygen and carbon dioxide in the blood and body fluids (4) Regulation of ventilation and other facets of respiration. 2
Functions of the Respiratory System • Provides oxygen. • Eliminates carbon dioxide. • Regulates the blood’s hydrogen-ion concentration (p. H conc). • Forms speech sounds (phonation). • Defends against microbes. • Influences arterial concentrations of chemical messengers by removing some from pulmonary capillary blood and producing and adding others to this blood. • Traps and dissolves blood clots. 3
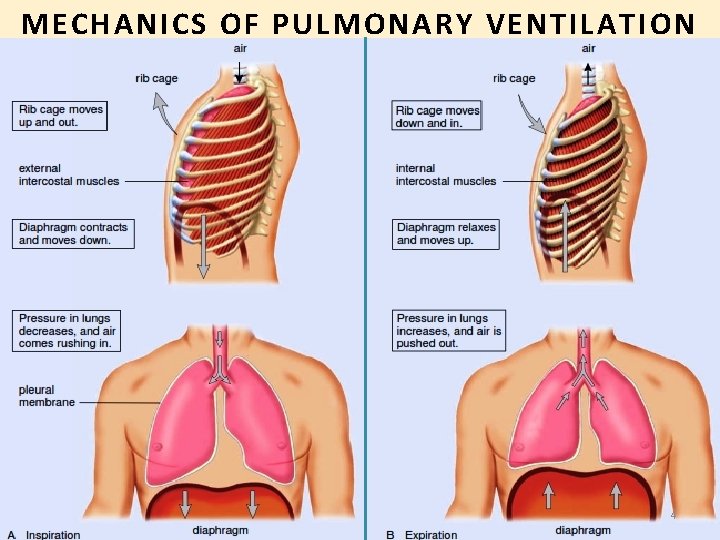
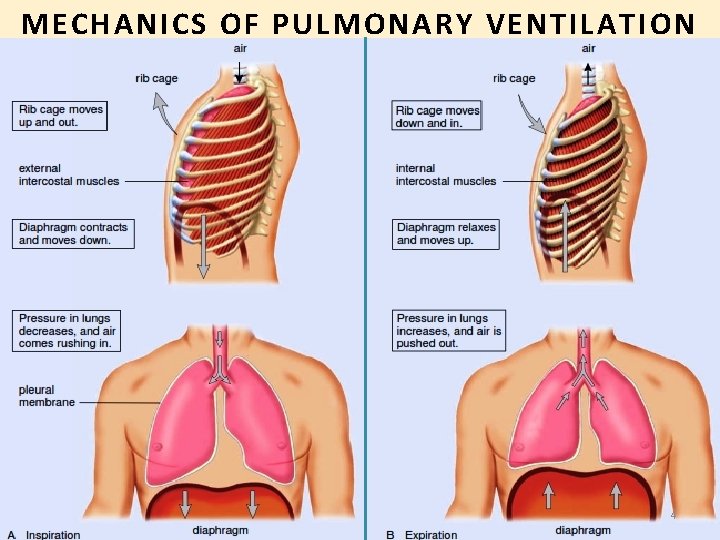
MECHANICS OF PULMONARY VENTILATION 4
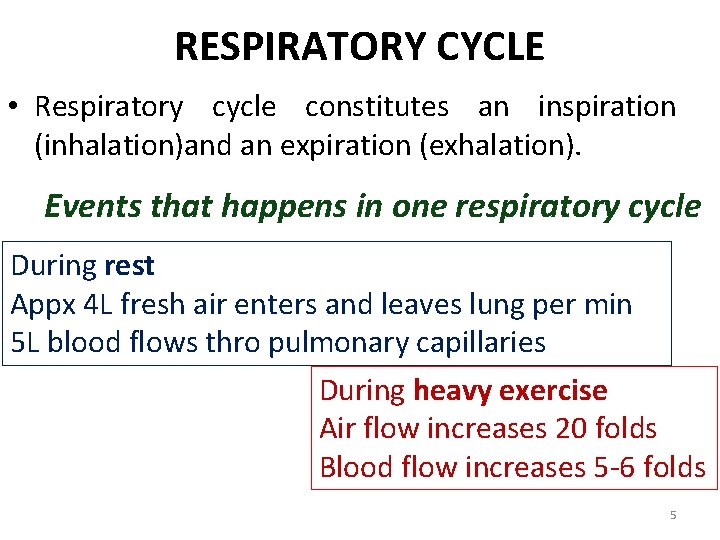
RESPIRATORY CYCLE • Respiratory cycle constitutes an inspiration (inhalation)and an expiration (exhalation). Events that happens in one respiratory cycle During rest Appx 4 L fresh air enters and leaves lung per min 5 L blood flows thro pulmonary capillaries During heavy exercise Air flow increases 20 folds Blood flow increases 5 -6 folds 5
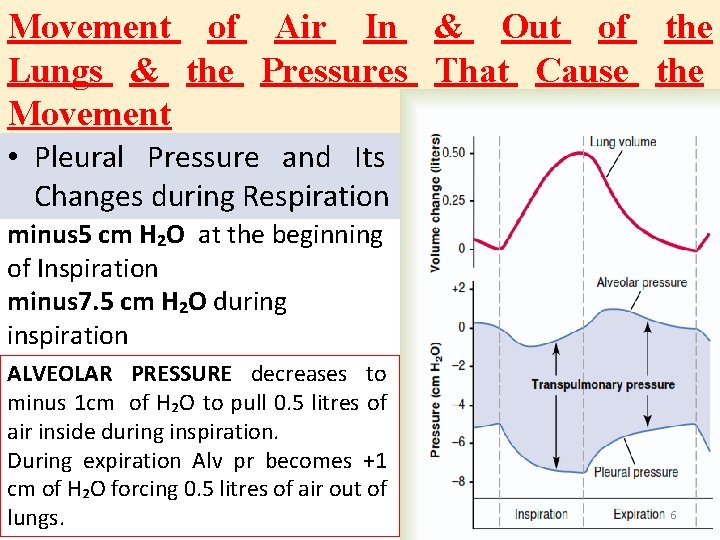
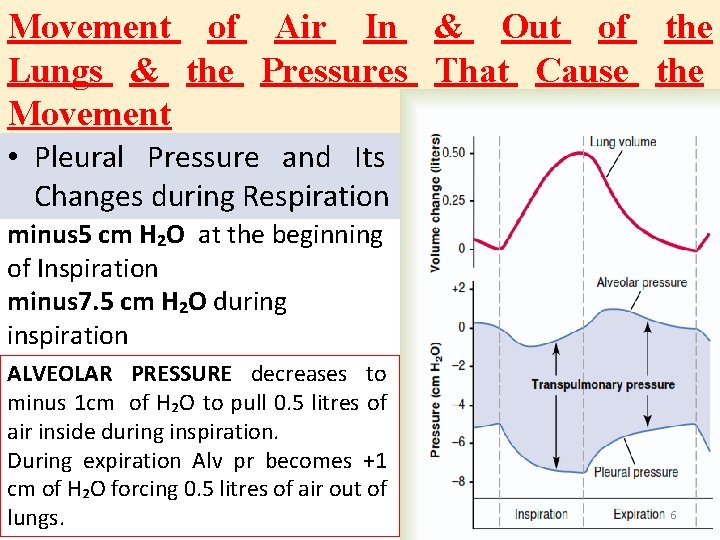
Movement of Air In & Out of the Lungs & the Pressures That Cause the Movement • Pleural Pressure and Its Changes during Respiration minus 5 cm H₂O at the beginning of Inspiration minus 7. 5 cm H₂O during inspiration ALVEOLAR PRESSURE decreases to minus 1 cm of H₂O to pull 0. 5 litres of air inside during inspiration. During expiration Alv pr becomes +1 cm of H₂O forcing 0. 5 litres of air out of lungs. 6
“Work” of Breathing • During inspiration- respiratory muscle contraction. • Expiration is a passive process caused by elastic recoil WORK OF INSPIRATION ü Compliance work or elastic work ü Tissue resistance work ü Airway resistance work. Energy Required for Respiration. In normal quite respiration- 3 to 5 per cent of the total energy is expended by the body. Increases as much as 50 -folds in heavy exercise, increased airway resistance or decreased pulmonary compliance. 7
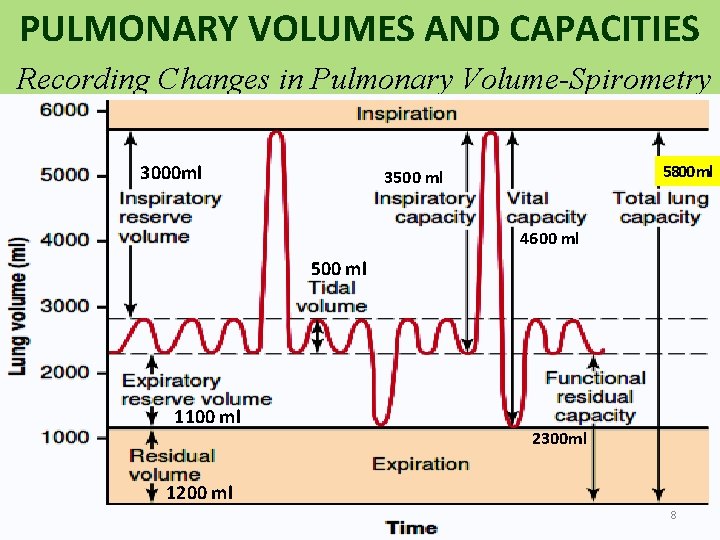
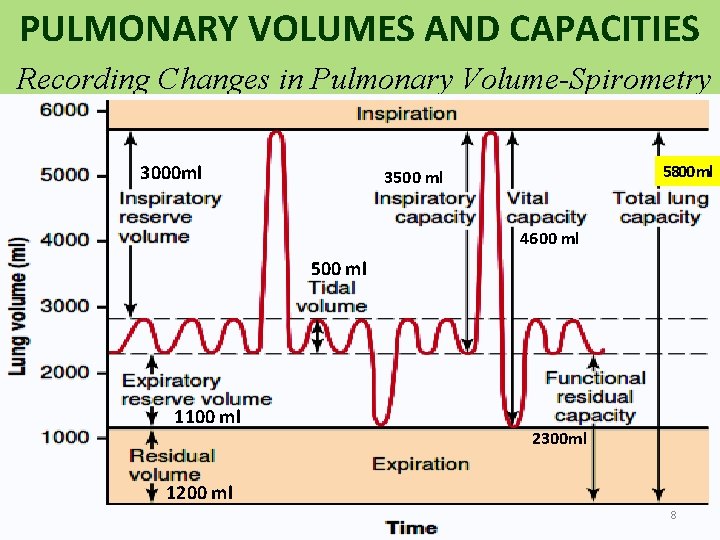
PULMONARY VOLUMES AND CAPACITIES Recording Changes in Pulmonary Volume-Spirometry 3000 ml 5800 ml 3500 ml 4600 ml 500 ml 1100 ml 2300 ml 1200 ml 8
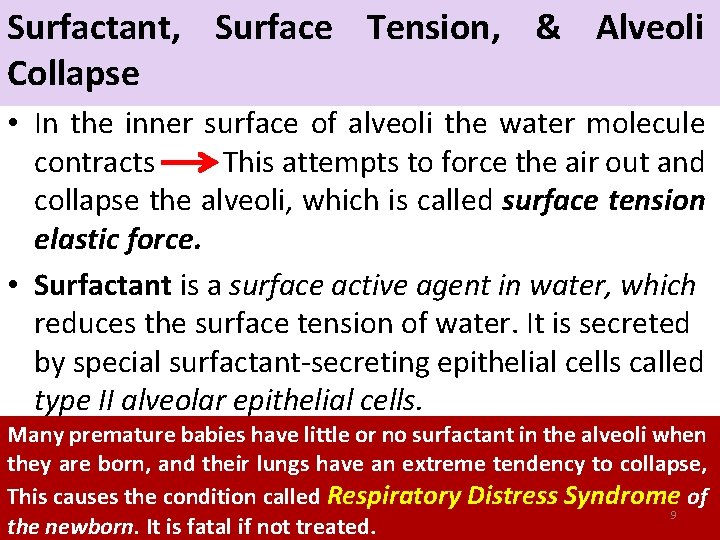
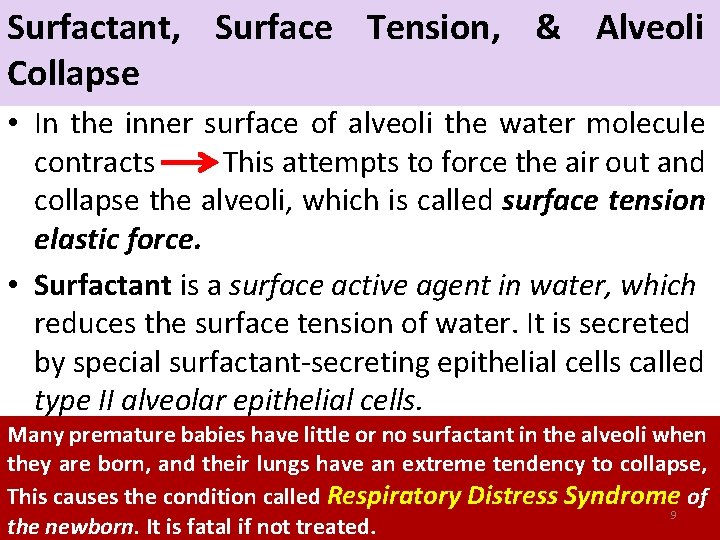
Surfactant, Surface Tension, & Alveoli Collapse • In the inner surface of alveoli the water molecule contracts This attempts to force the air out and collapse the alveoli, which is called surface tension elastic force. • Surfactant is a surface active agent in water, which reduces the surface tension of water. It is secreted by special surfactant-secreting epithelial cells called type II alveolar epithelial cells. Many premature babies have little or no surfactant in the alveoli when they are born, and their lungs have an extreme tendency to collapse, This causes the condition called Respiratory Distress Syndrome of 9 the newborn. It is fatal if not treated.
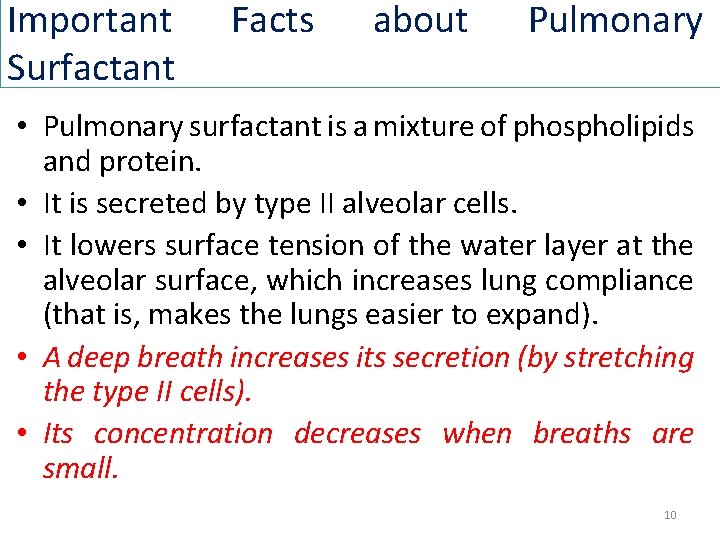
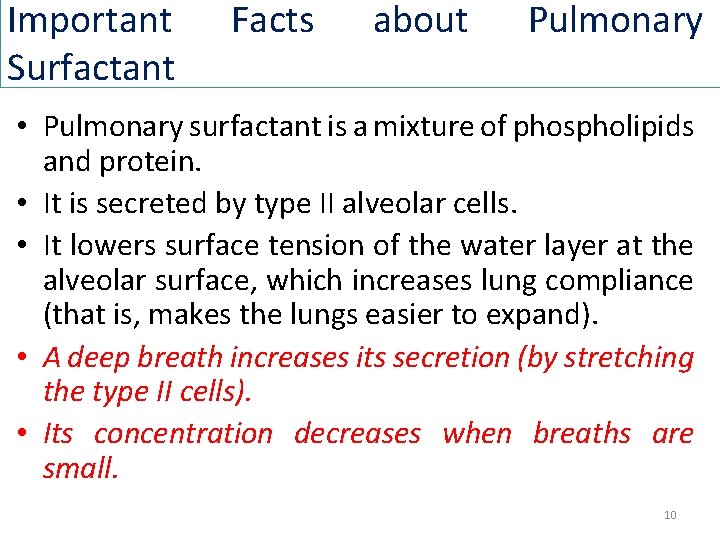
Important Surfactant Facts about Pulmonary • Pulmonary surfactant is a mixture of phospholipids and protein. • It is secreted by type II alveolar cells. • It lowers surface tension of the water layer at the alveolar surface, which increases lung compliance (that is, makes the lungs easier to expand). • A deep breath increases its secretion (by stretching the type II cells). • Its concentration decreases when breaths are small. 10
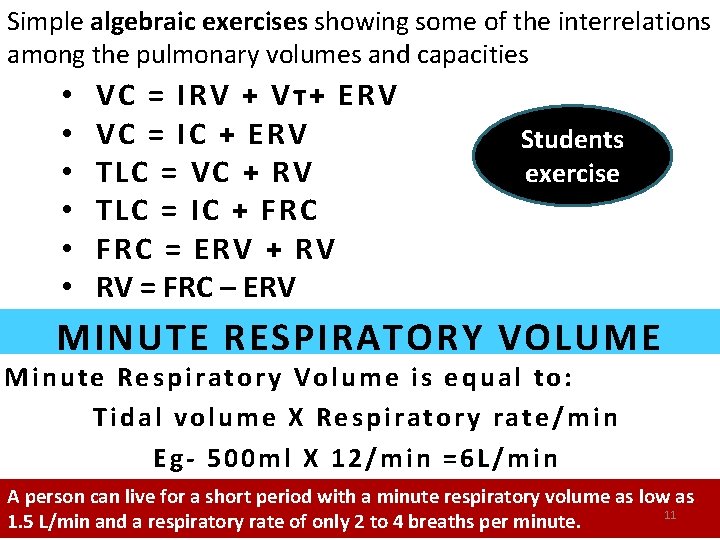
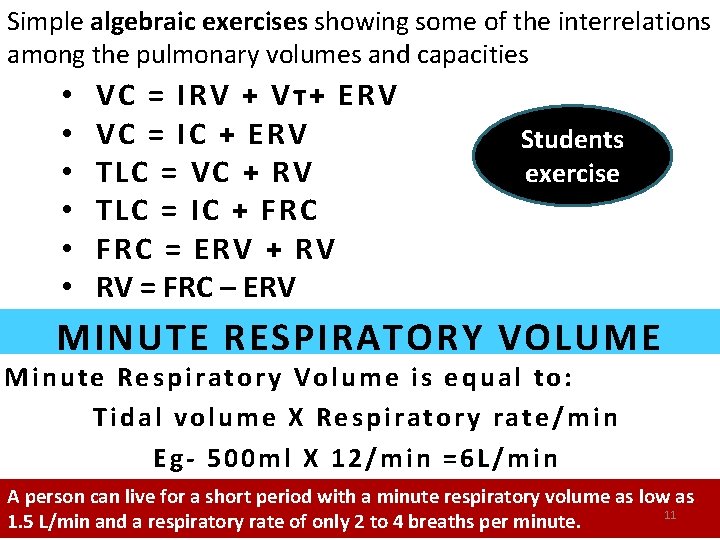
Simple algebraic exercises showing some of the interrelations among the pulmonary volumes and capacities • • • VC = IRV + Vᴛ+ ERV VC = IC + ERV TLC = VC + RV TLC = IC + FRC = ERV + RV RV = FRC – ERV Students exercise MINUTE RESPIRATORY VOLUME Minute Respiratory Volume is equal to: Tidal volume X Respiratory rate/min Eg- 500 ml X 12/min =6 L/min A person can live for a short period with a minute respiratory volume as low as 11 1. 5 L/min and a respiratory rate of only 2 to 4 breaths per minute.
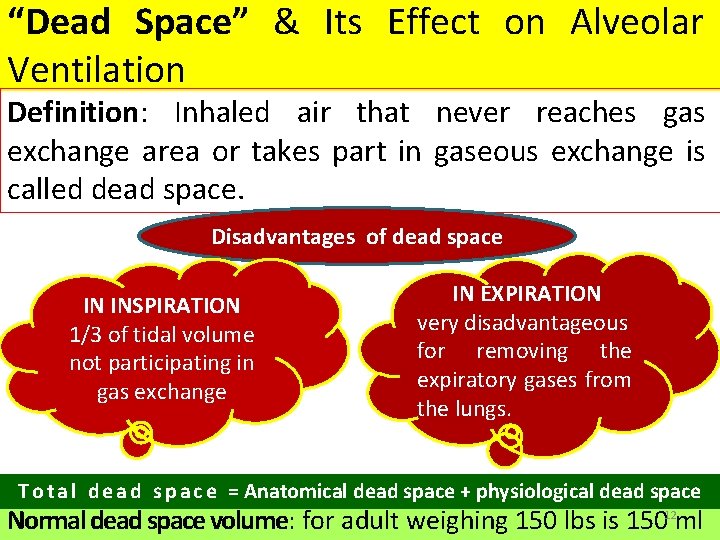
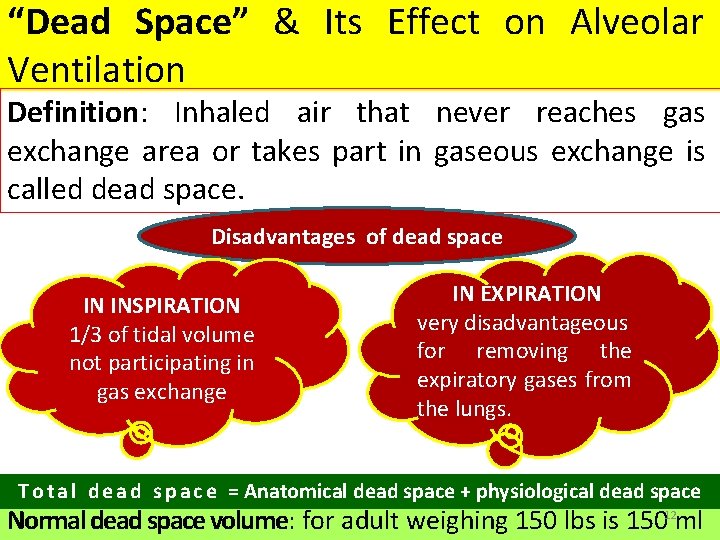
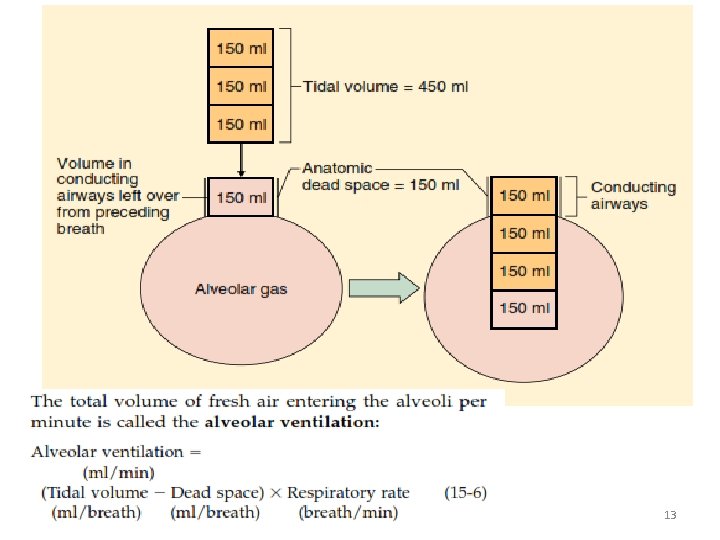
“Dead Space” & Its Effect on Alveolar Ventilation Definition: Inhaled air that never reaches gas exchange area or takes part in gaseous exchange is called dead space. Disadvantages of dead space IN INSPIRATION 1/3 of tidal volume not participating in gas exchange IN EXPIRATION very disadvantageous for removing the expiratory gases from the lungs. T o t a l d e a d s p a c e = Anatomical dead space + physiological dead space Normal dead space volume: for adult weighing 150 lbs is 15012 ml
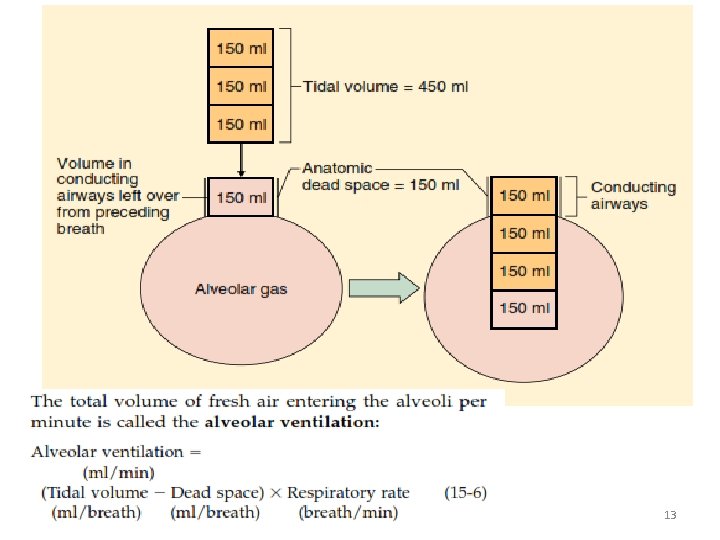
13
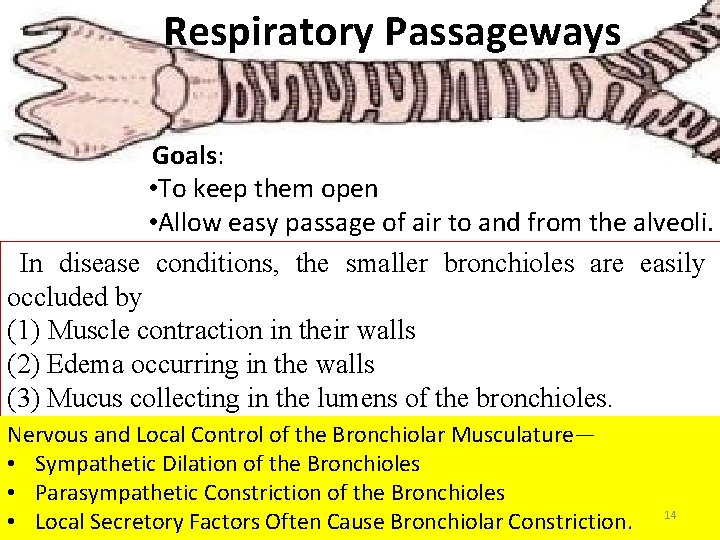
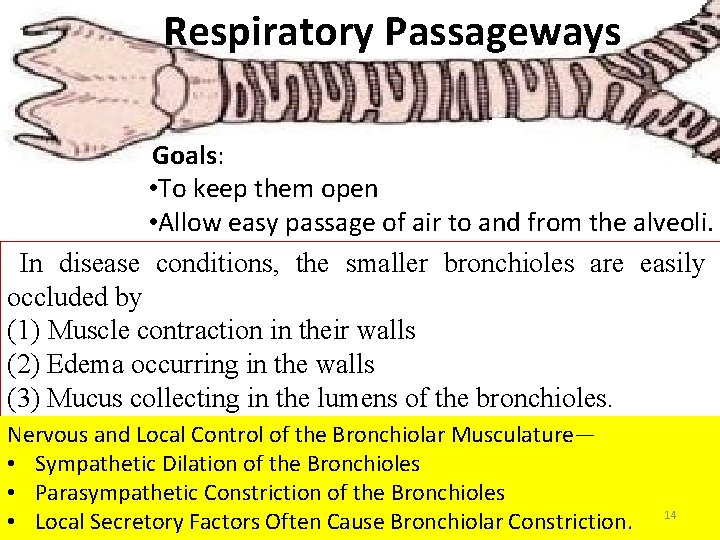
Respiratory Passageways Goals: • To keep them open • Allow easy passage of air to and from the alveoli. In disease conditions, the smaller bronchioles are easily occluded by (1) Muscle contraction in their walls (2) Edema occurring in the walls (3) Mucus collecting in the lumens of the bronchioles. Nervous and Local Control of the Bronchiolar Musculature— • Sympathetic Dilation of the Bronchioles • Parasympathetic Constriction of the Bronchioles • Local Secretory Factors Often Cause Bronchiolar Constriction. 14
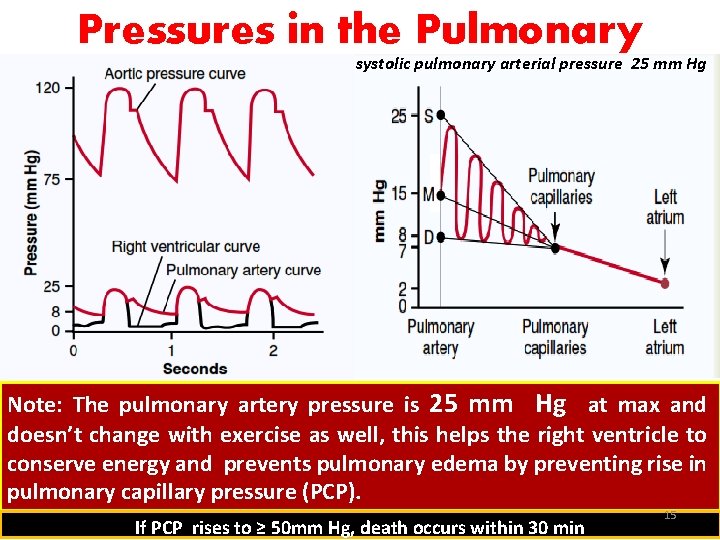
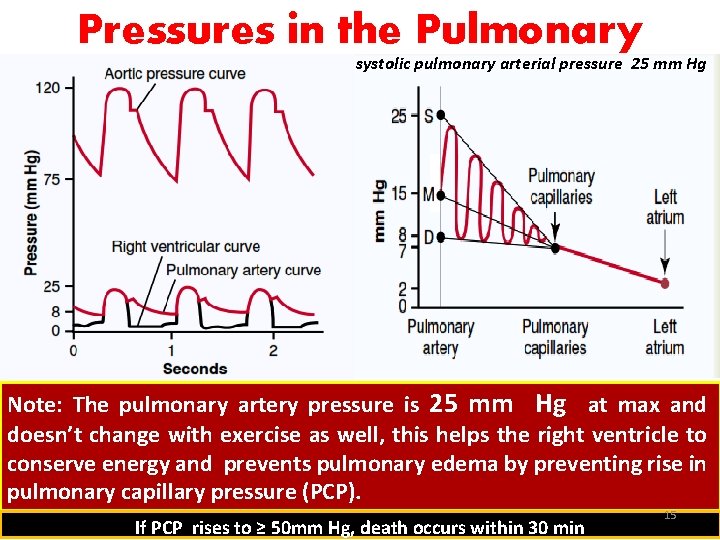
Pressures in the Pulmonary systolic pulmonary arterial pressure 25 mm Hg System Note: The pulmonary artery pressure is 25 mm Hg at max and doesn’t change with exercise as well, this helps the right ventricle to conserve energy and prevents pulmonary edema by preventing rise in pulmonary capillary pressure (PCP). If PCP rises to ≥ 50 mm Hg, death occurs within 30 min 15
Answer the following questions 1. How will you calculate trans-pulmonary pressure? 2. What will be the Pleural pressure at the beginning of inspiration? 3. In normal quiet respiration how many percentage of total energy of body is utilized? 4. What is the normal value of IRV in spirometer? 5. What is the value of normal RV of lungs? 6. How will you calculate a persons IC value? 7. What is the abbreviation of RDS? 8. What is the normal value of ERV? 9. How will you calculate a persons VC? 10. A persons TV is 450 ml and BR is 12/min, calculate his minute respiratory volume? 16
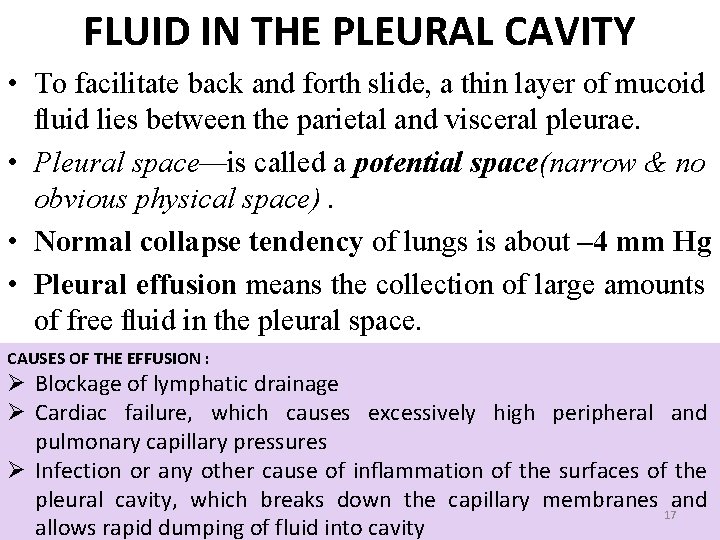
FLUID IN THE PLEURAL CAVITY • To facilitate back and forth slide, a thin layer of mucoid fluid lies between the parietal and visceral pleurae. • Pleural space—is called a potential space(narrow & no obvious physical space). • Normal collapse tendency of lungs is about – 4 mm Hg • Pleural effusion means the collection of large amounts of free fluid in the pleural space. CAUSES OF THE EFFUSION : Ø Blockage of lymphatic drainage Ø Cardiac failure, which causes excessively high peripheral and pulmonary capillary pressures Ø Infection or any other cause of inflammation of the surfaces of the pleural cavity, which breaks down the capillary membranes and 17 allows rapid dumping of fluid into cavity
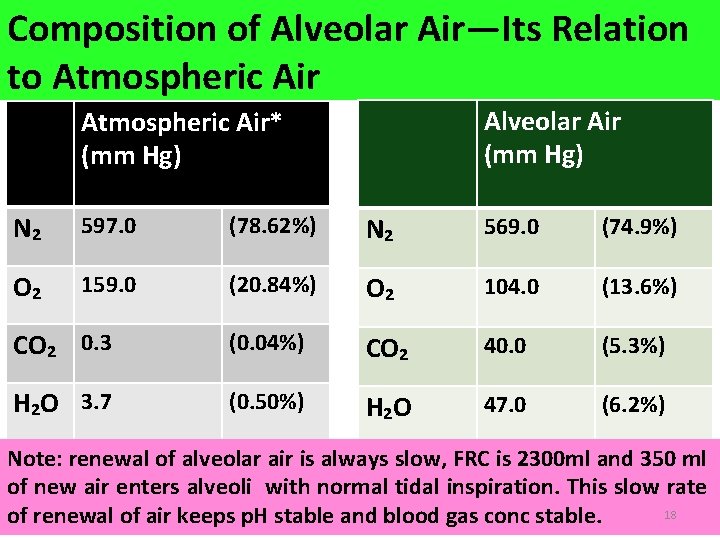
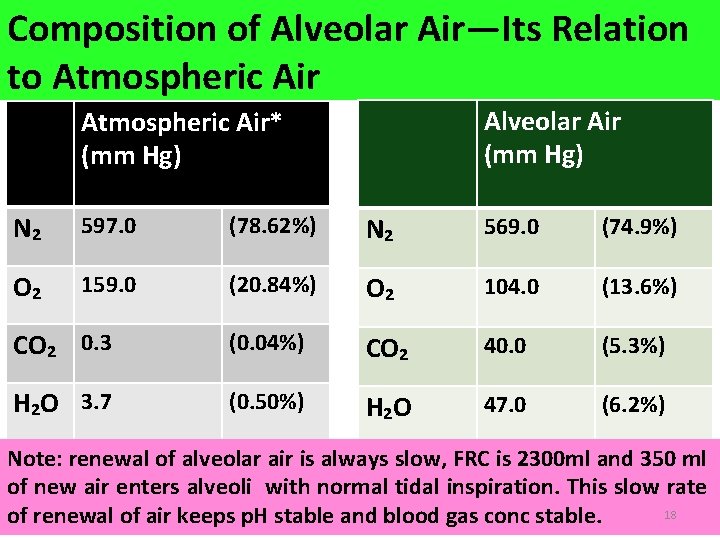
Composition of Alveolar Air—Its Relation to Atmospheric Air Alveolar Air (mm Hg) Atmospheric Air* (mm Hg) N₂ 597. 0 (78. 62%) N₂ 569. 0 (74. 9%) O₂ 159. 0 (20. 84%) O₂ 104. 0 (13. 6%) CO₂ 0. 3 (0. 04%) CO₂ 40. 0 (5. 3%) H₂O 3. 7 (0. 50%) H₂O 47. 0 (6. 2%) Note: renewal of alveolar air is always slow, FRC is 2300 ml and 350 ml of new air enters alveoli with normal tidal inspiration. This slow rate 18 of renewal of air keeps p. H stable and blood gas conc stable.
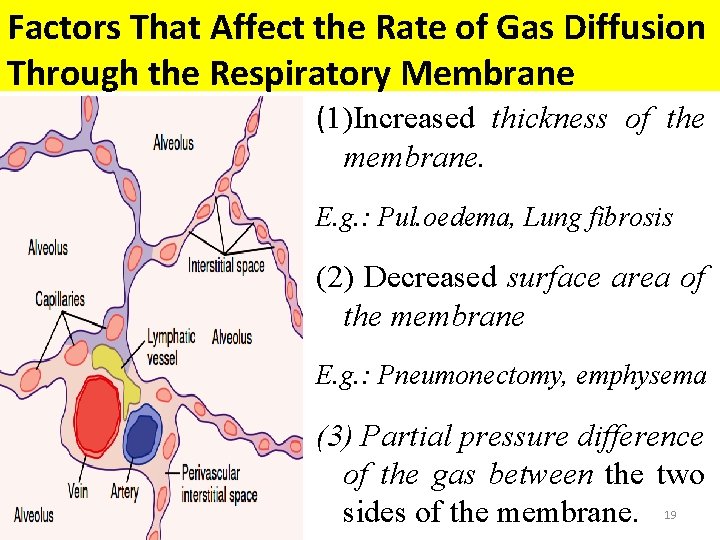
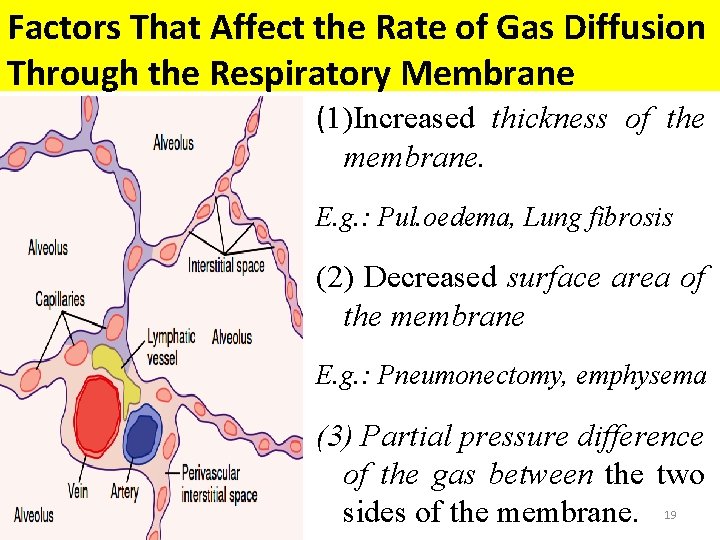
Factors That Affect the Rate of Gas Diffusion Through the Respiratory Membrane (1)Increased thickness of the membrane. E. g. : Pul. oedema, Lung fibrosis (2) Decreased surface area of the membrane E. g. : Pneumonectomy, emphysema (3) Partial pressure difference of the gas between the two sides of the membrane. 19
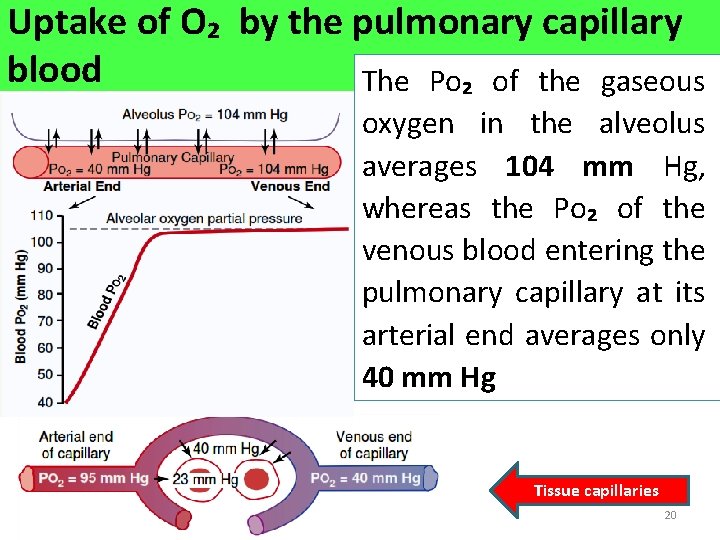
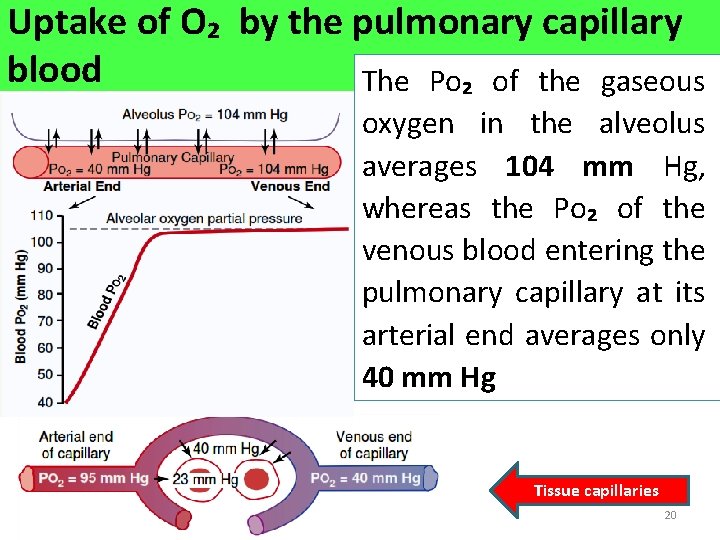
Uptake of O₂ by the pulmonary capillary blood The Po₂ of the gaseous oxygen in the alveolus averages 104 mm Hg, whereas the Po₂ of the venous blood entering the pulmonary capillary at its arterial end averages only 40 mm Hg Tissue capillaries 20
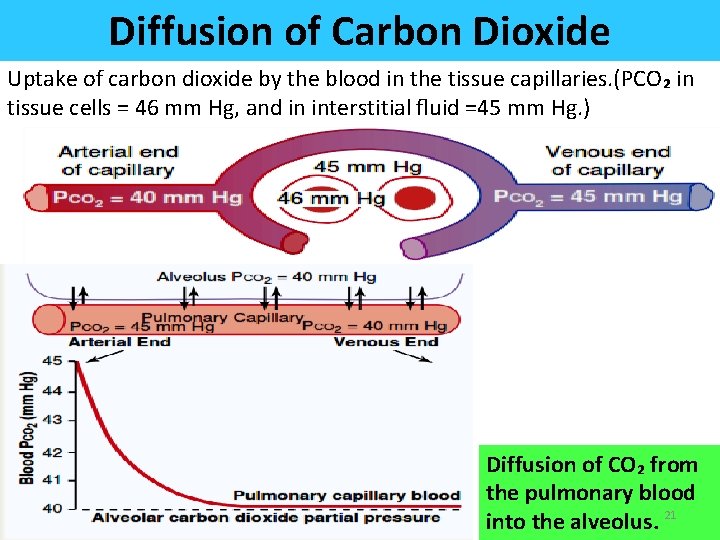
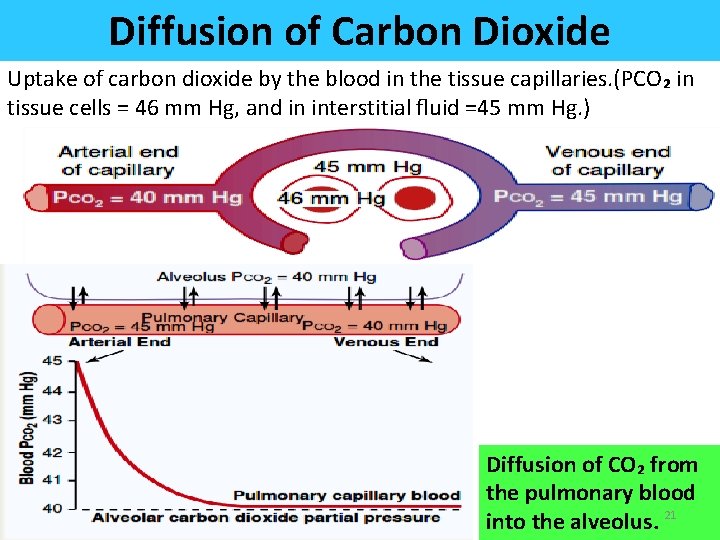
Diffusion of Carbon Dioxide Uptake of carbon dioxide by the blood in the tissue capillaries. (PCO₂ in tissue cells = 46 mm Hg, and in interstitial fluid =45 mm Hg. ) Diffusion of CO₂ from the pulmonary blood into the alveolus. 21
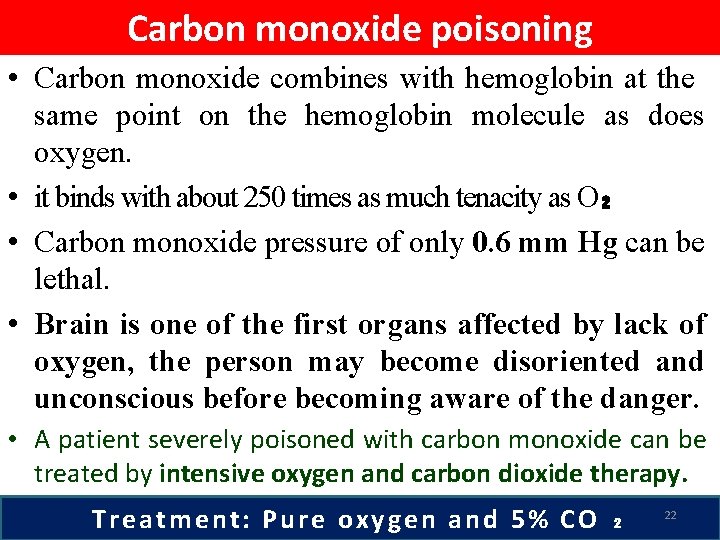
Carbon monoxide poisoning • Carbon monoxide combines with hemoglobin at the same point on the hemoglobin molecule as does oxygen. • it binds with about 250 times as much tenacity as O₂ • Carbon monoxide pressure of only 0. 6 mm Hg can be lethal. • Brain is one of the first organs affected by lack of oxygen, the person may become disoriented and unconscious before becoming aware of the danger. • A patient severely poisoned with carbon monoxide can be treated by intensive oxygen and carbon dioxide therapy. Treatment: Pure oxygen and 5% CO ₂ 22
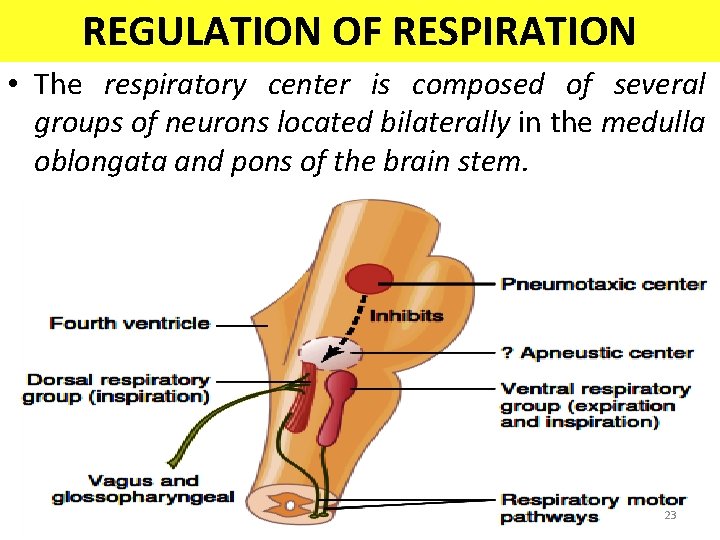
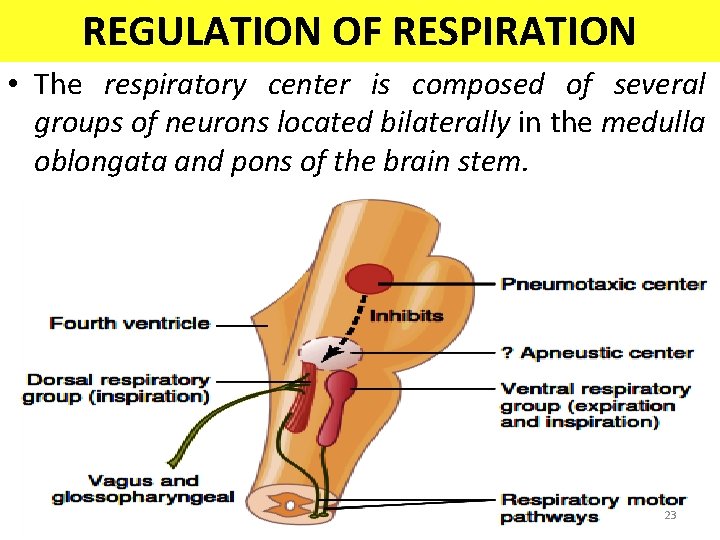
REGULATION OF RESPIRATION • The respiratory center is composed of several groups of neurons located bilaterally in the medulla oblongata and pons of the brain stem. 23
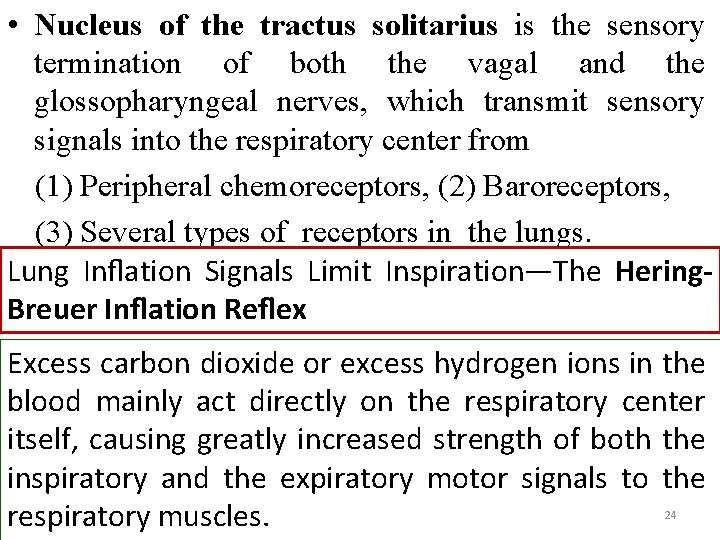
• Nucleus of the tractus solitarius is the sensory termination of both the vagal and the glossopharyngeal nerves, which transmit sensory signals into the respiratory center from (1) Peripheral chemoreceptors, (2) Baroreceptors, (3) Several types of receptors in the lungs. Lung Inflation Signals Limit Inspiration—The Hering. Breuer Inflation Reflex Excess carbon dioxide or excess hydrogen ions in the blood mainly act directly on the respiratory center itself, causing greatly increased strength of both the inspiratory and the expiratory motor signals to the respiratory muscles. 24
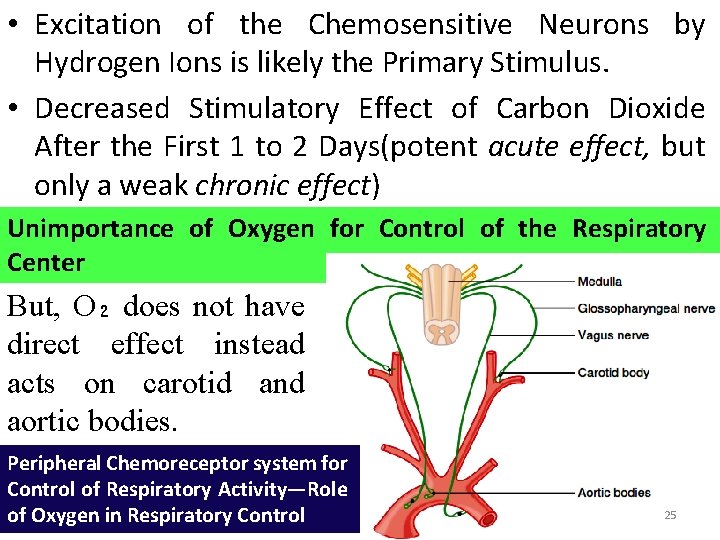
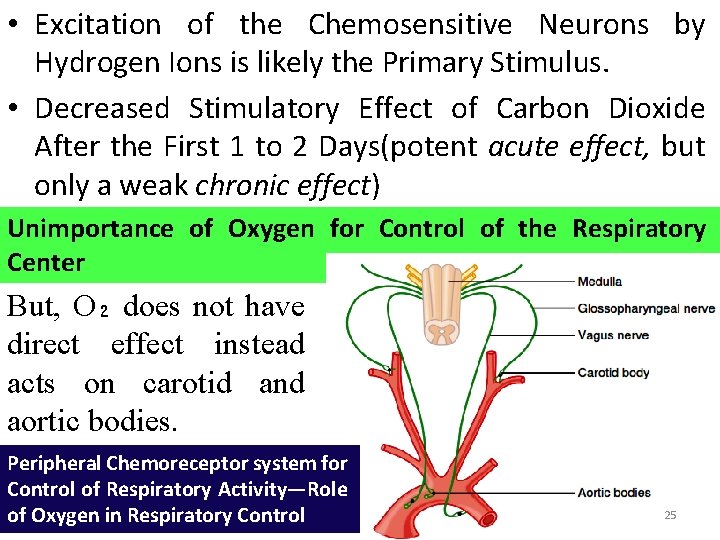
• Excitation of the Chemosensitive Neurons by Hydrogen Ions is likely the Primary Stimulus. • Decreased Stimulatory Effect of Carbon Dioxide After the First 1 to 2 Days(potent acute effect, but only a weak chronic effect) Unimportance of Oxygen for Control of the Respiratory Center But, O₂ does not have direct effect instead acts on carotid and aortic bodies. Peripheral Chemoreceptor system for Control of Respiratory Activity—Role of Oxygen in Respiratory Control 25
Voluntary Control of Respiration • For short periods of time, respiration can be controlled voluntarily and that one can hyperventilate or hypoventilate to such an extent that serious derangements in Pco₂, p. H, and Po₂ can occur in the blood. EFFECT OF BRAIN EDEMA The activity of the respiratory center may be depressed or even inactivated by acute brain edema resulting from brain concussion. 26
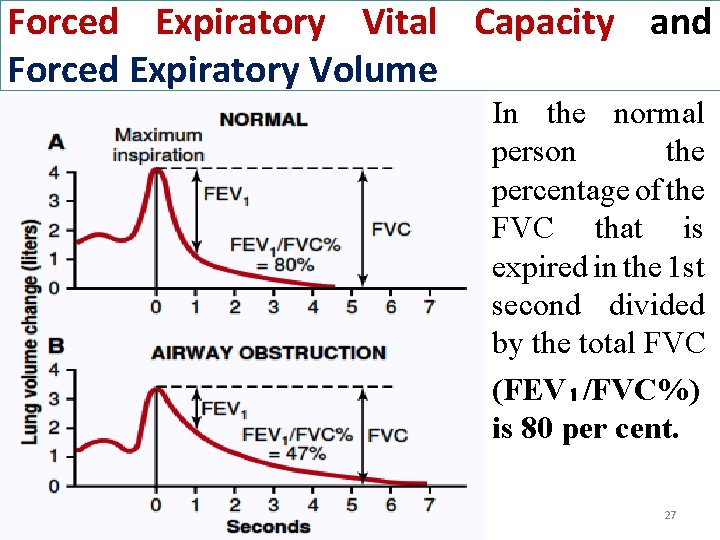
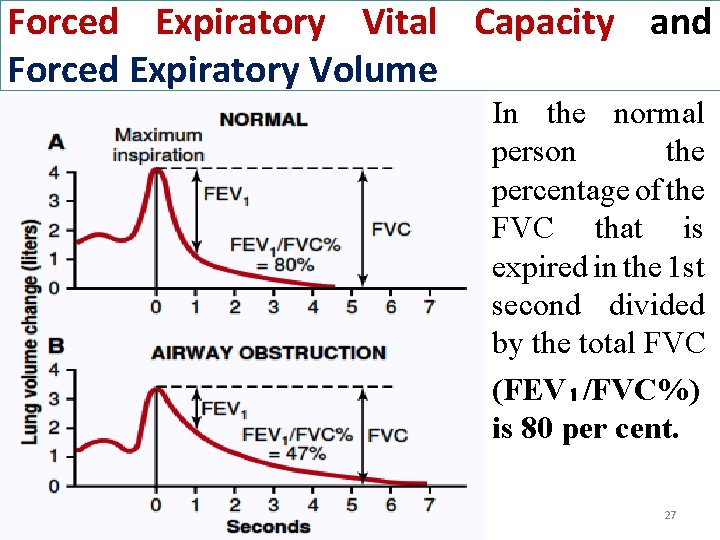
Forced Expiratory Vital Capacity and Forced Expiratory Volume In the normal person the percentage of the FVC that is expired in the 1 st second divided by the total FVC (FEV₁/FVC%) is 80 per cent. 27
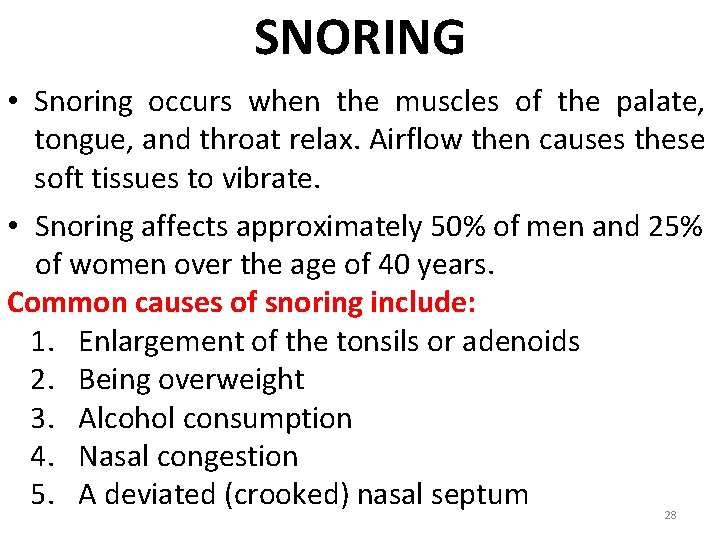
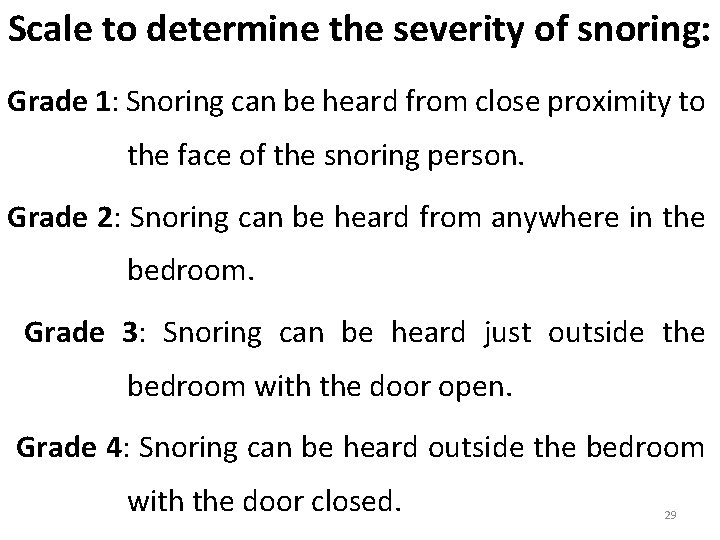
SNORING • Snoring occurs when the muscles of the palate, tongue, and throat relax. Airflow then causes these soft tissues to vibrate. • Snoring affects approximately 50% of men and 25% of women over the age of 40 years. Common causes of snoring include: 1. Enlargement of the tonsils or adenoids 2. Being overweight 3. Alcohol consumption 4. Nasal congestion 5. A deviated (crooked) nasal septum 28
Scale to determine the severity of snoring: Grade 1: Snoring can be heard from close proximity to the face of the snoring person. Grade 2: Snoring can be heard from anywhere in the bedroom. Grade 3: Snoring can be heard just outside the bedroom with the door open. Grade 4: Snoring can be heard outside the bedroom with the door closed. 29
Pulmonary Abnormalities • • • Chronic Pulmonary Emphysema Pneumonia Atelectasis Asthma Tuberculosis Bronchitis Lung cancer Pneumothorax Pulmonary edema Severe acute respiratory syndrome (SARS) Sudden infant death syndrome (SIDS) Pulmonary embolism 30
s ’ t a Th d n e the s i h of t r e t p a h c 31