Cardiomyopathies Denisa Jindrov Definition Cardio heart Myo muscle



- Slides: 59

Cardiomyopathies Denisa Jindrová
Definition Cardio – (heart) Myo – (muscle) Pathy (disease) Heterogeneous group of diseases assosiated with a mechanical or electrical dysfunction with a different etiology, clinical course and therapy
Definition • Myocardial disorder, in which heart muscle is structurally and functionally abnormal • In the primary absence of • coronary artery disease • hypertension • valvular and congenital heart diseases ………sufficient to explain the observed abnormality
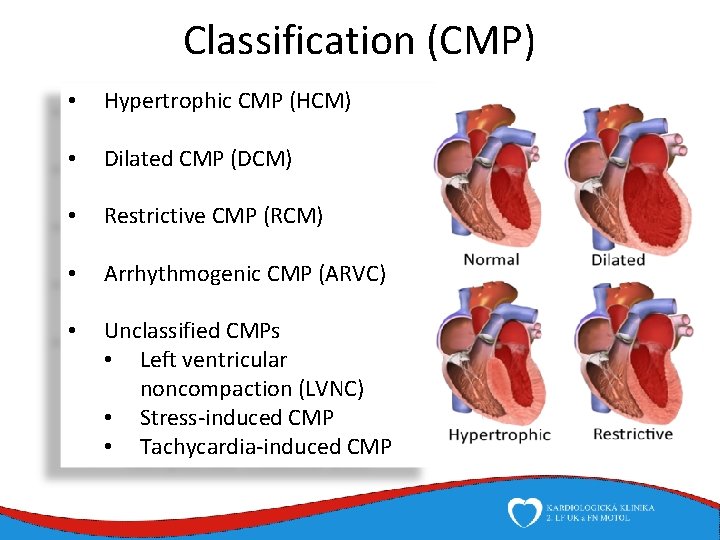
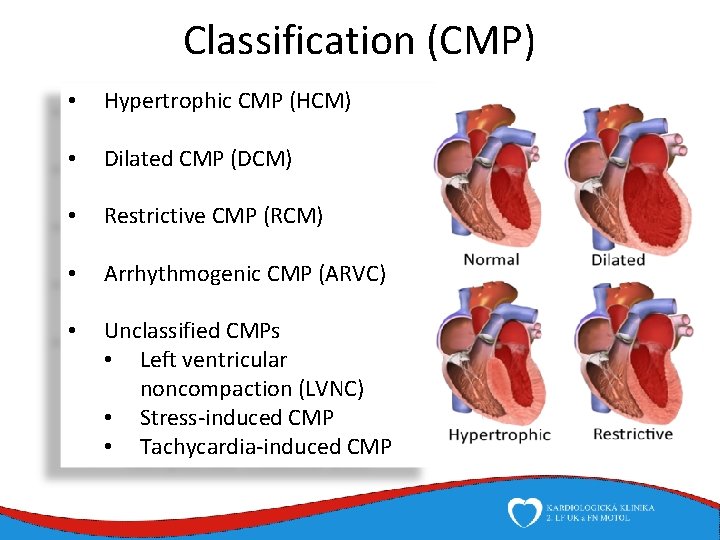
Classification (CMP) • Hypertrophic CMP (HCM) • Dilated CMP (DCM) • Restrictive CMP (RCM) • Arrhythmogenic CMP (ARVC) • Unclassified CMPs • Left ventricular noncompaction (LVNC) • Stress-induced CMP • Tachycardia-induced CMP
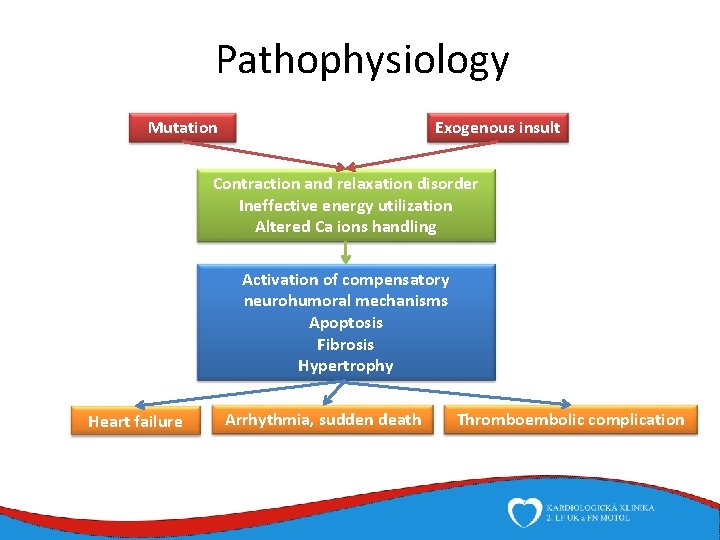
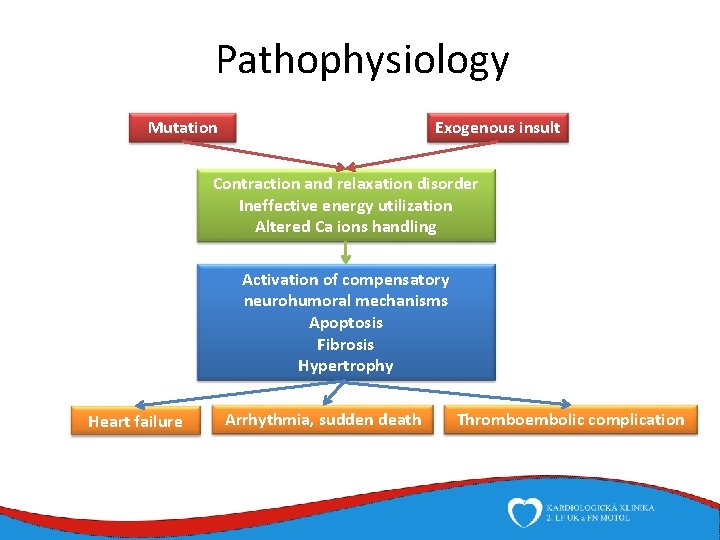
Pathophysiology Mutation Exogenous insult Contraction and relaxation disorder Ineffective energy utilization Altered Ca ions handling Activation of compensatory neurohumoral mechanisms Apoptosis Fibrosis Hypertrophy Heart failure Arrhythmia, sudden death Thromboembolic complication
Etiology Primary dysfunction of cardiomyocytes (by genetic or exogenous insult) Insult leads to disorder of contraction or relaxation Long-standing activation of compensatory neurohumoral mechanisms (eventually accentuates heart failure) Oxidative stress, hypertrophy, fibrosis, apoptosis
Genetics Some cardiomyopathies are monogenic disorders Primary genetic – HCM, ARVC, LVNC Mixed etiology – DCM (20 -40 %), RCM (rare) Great variability of genotype and phenotype Hundreds and thousands of mutations Many genes Various types of inheritence Different phenotypes in identical mutations
Therapy Exogenous insult prevention Sudden death prevention Primary Secondary Heart failure therapy Symptomatic Life prolonging Prevention of thromboembolic complications
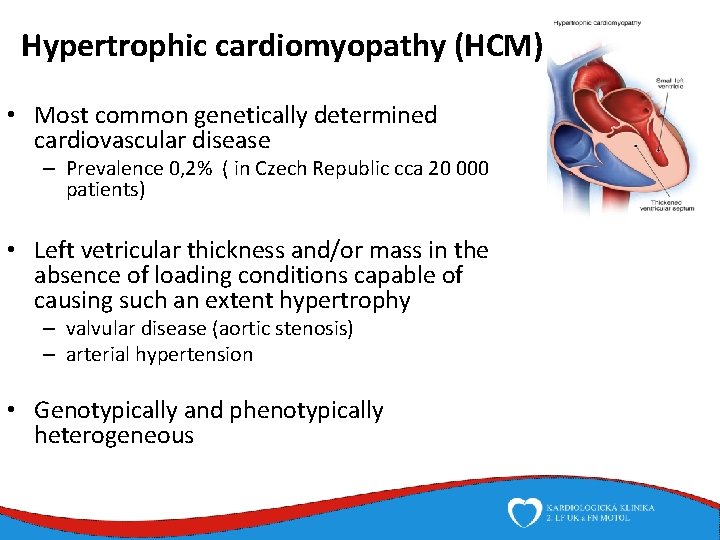
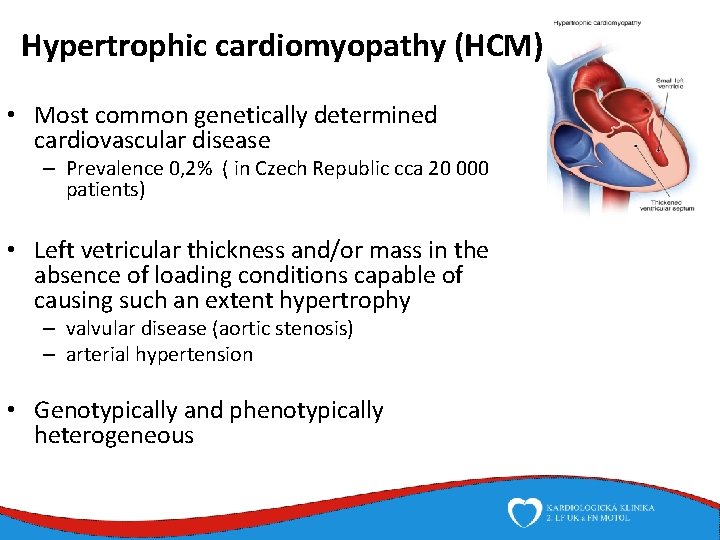
Hypertrophic cardiomyopathy (HCM) • Most common genetically determined cardiovascular disease – Prevalence 0, 2% ( in Czech Republic cca 20 000 patients) • Left vetricular thickness and/or mass in the absence of loading conditions capable of causing such an extent hypertrophy – valvular disease (aortic stenosis) – arterial hypertension • Genotypically and phenotypically heterogeneous
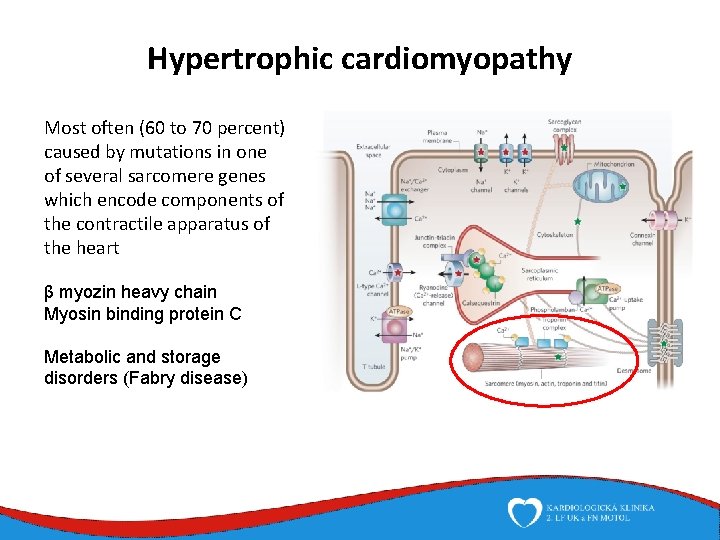
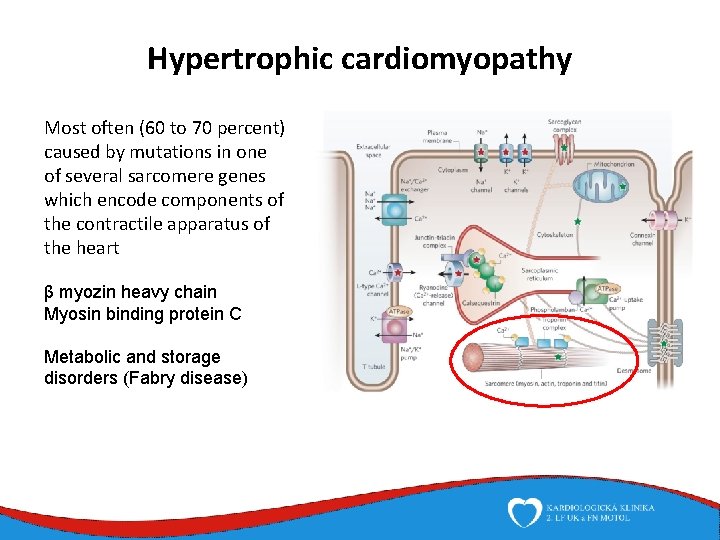
Hypertrophic cardiomyopathy Most often (60 to 70 percent) caused by mutations in one of several sarcomere genes which encode components of the contractile apparatus of the heart β myozin heavy chain Myosin binding protein C Metabolic and storage disorders (Fabry disease)
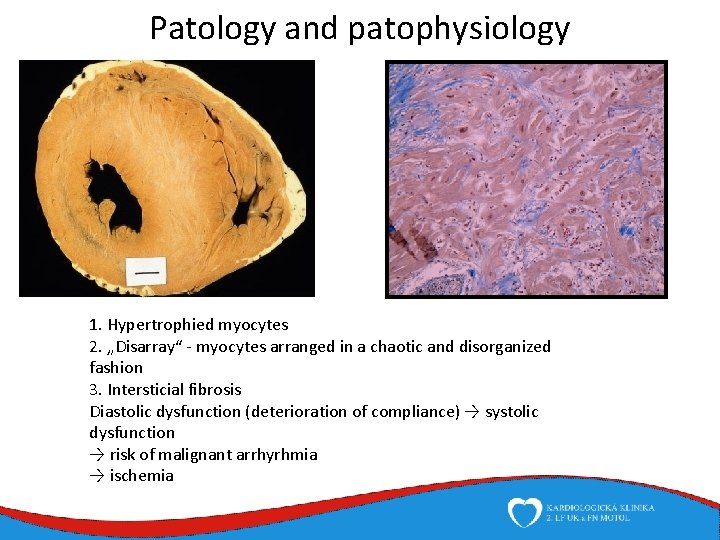
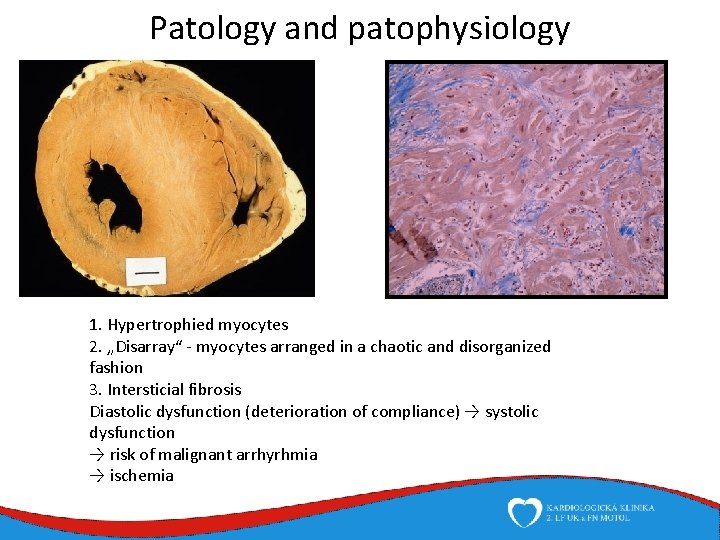
Patology and patophysiology 1. Hypertrophied myocytes 2. „Disarray“ - myocytes arranged in a chaotic and disorganized fashion 3. Intersticial fibrosis Diastolic dysfunction (deterioration of compliance) → systolic dysfunction → risk of malignant arrhyrhmia → ischemia
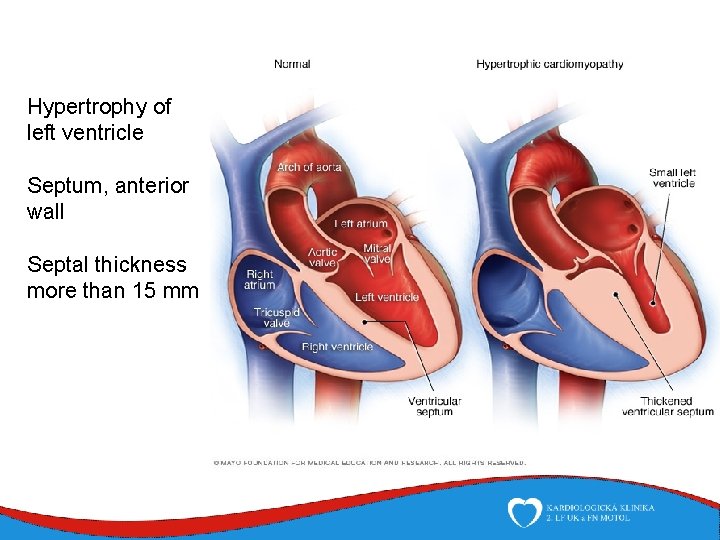
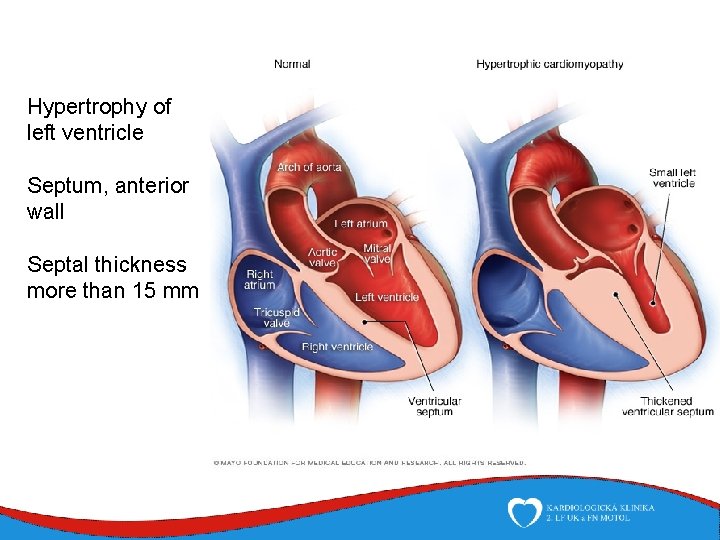
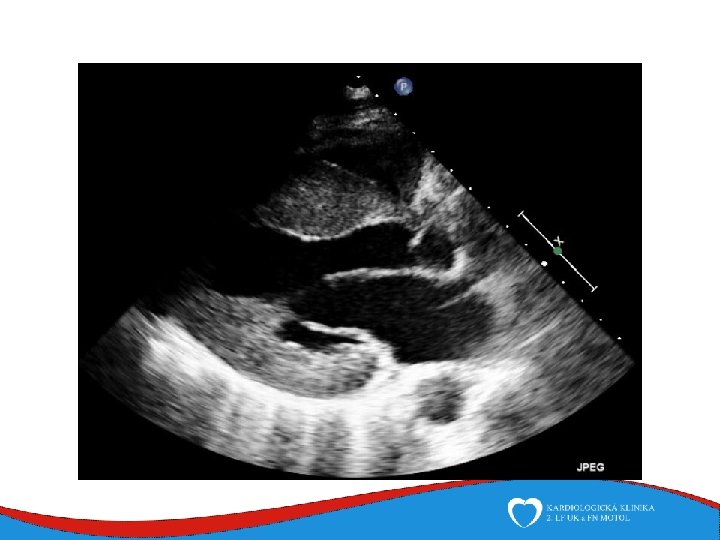
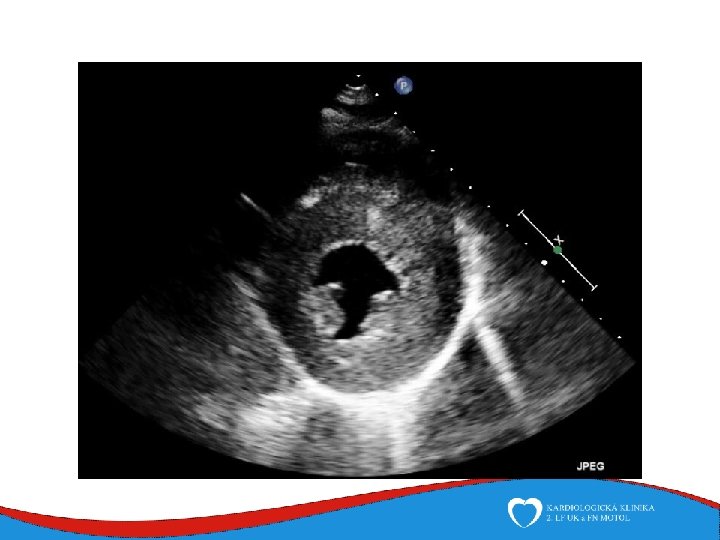
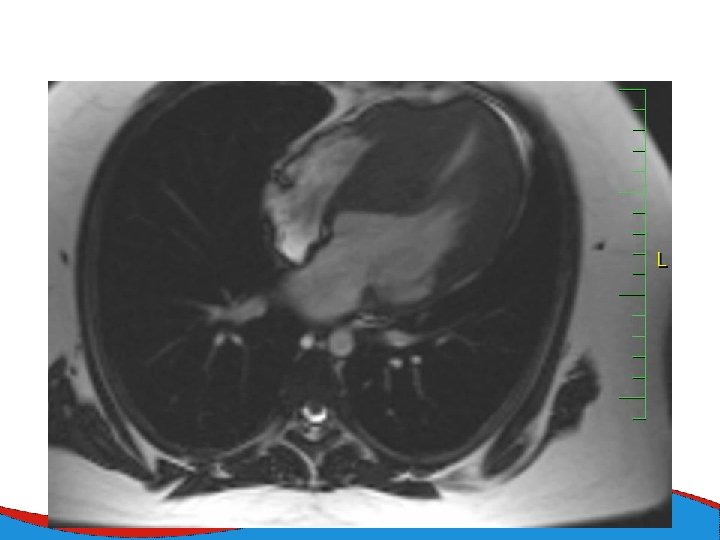
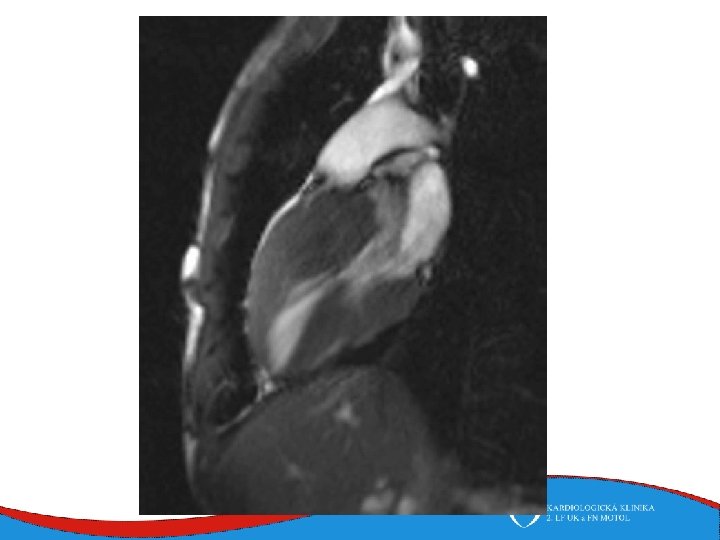
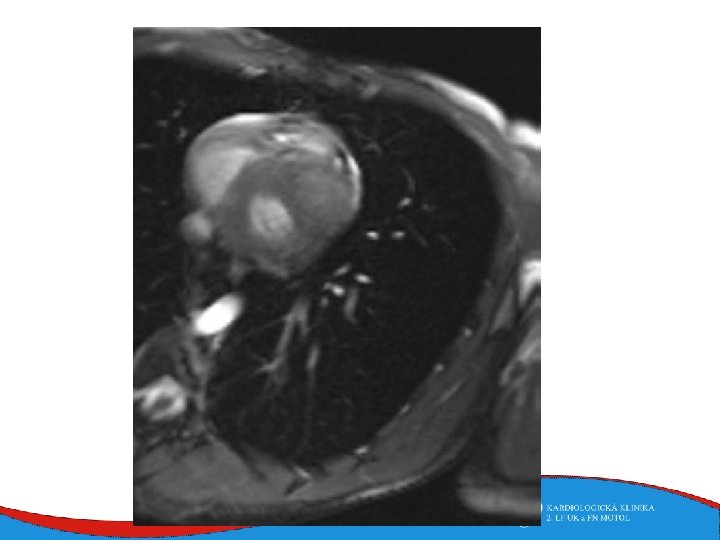
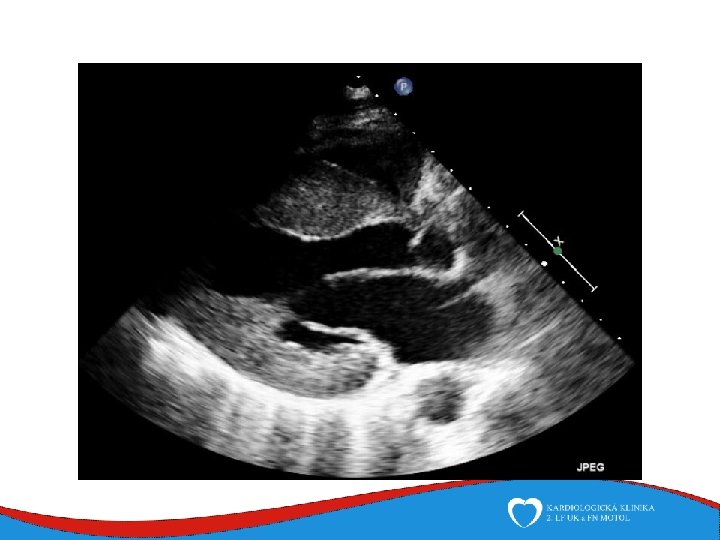
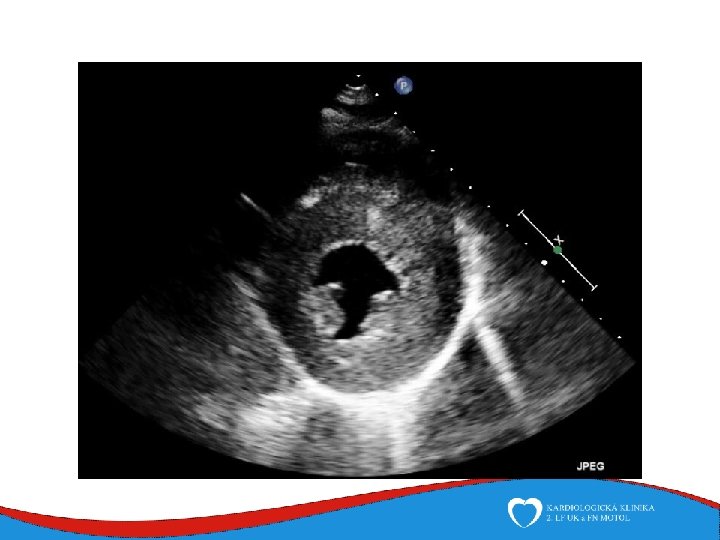
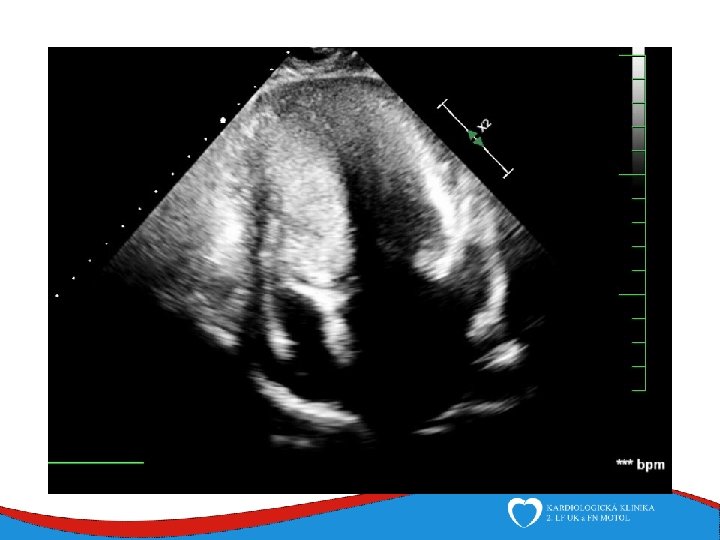
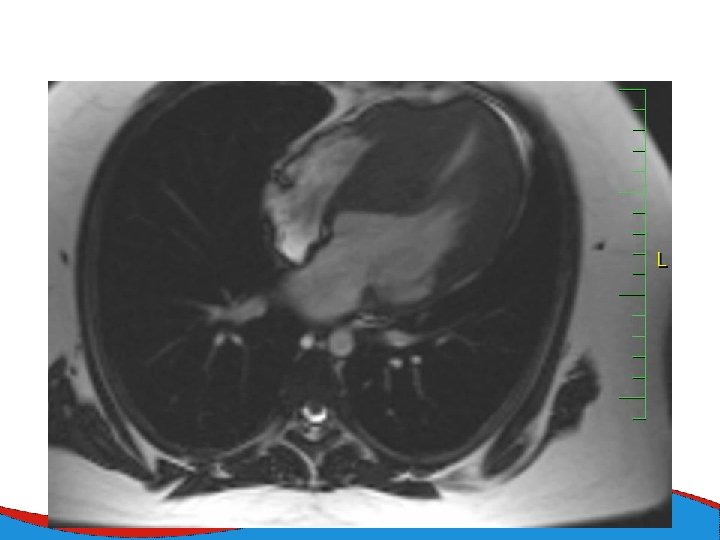
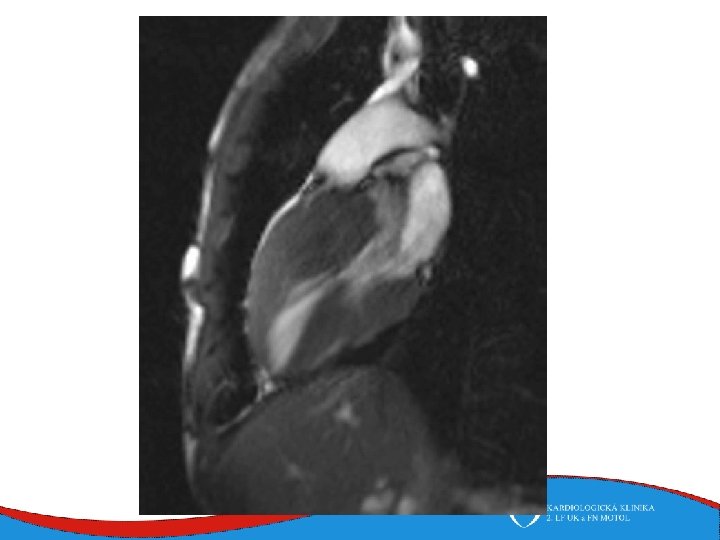
Hypertrophy of left ventricle Septum, anterior wall Septal thickness more than 15 mm

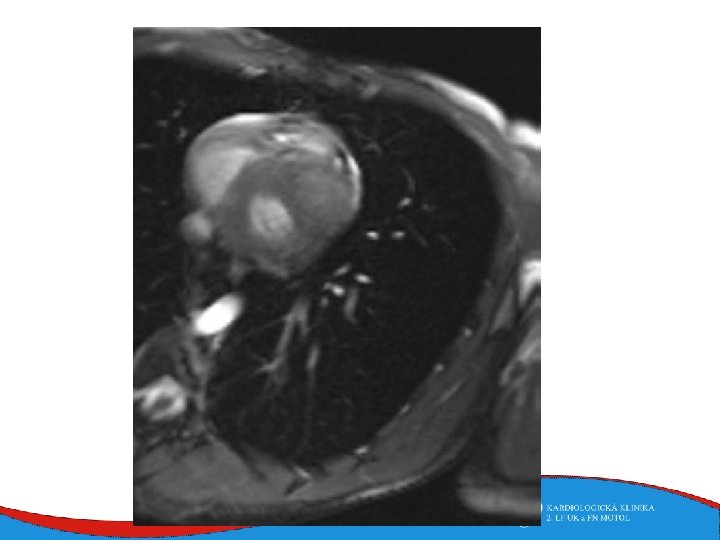
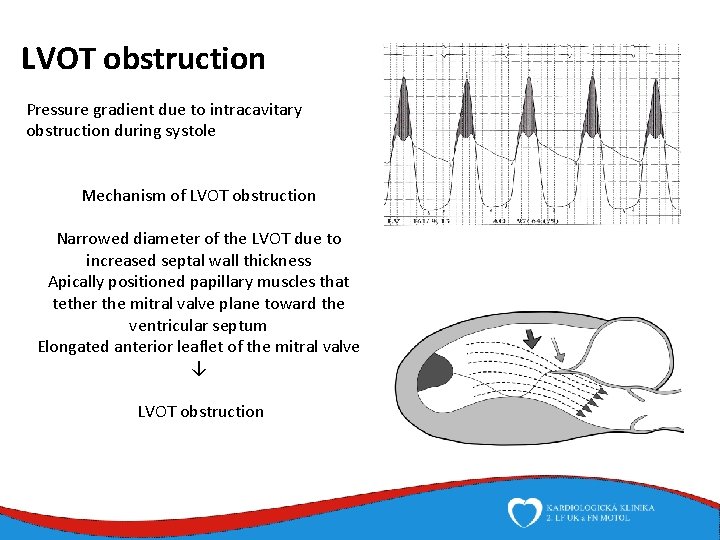
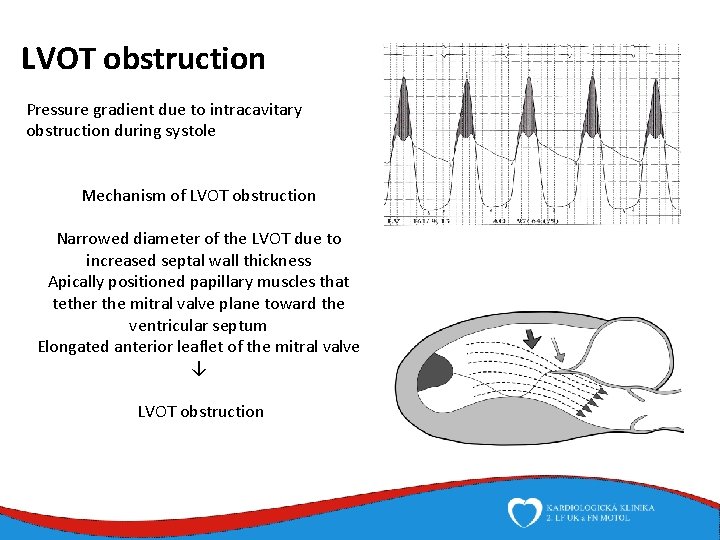
LVOT obstruction Pressure gradient due to intracavitary obstruction during systole Mechanism of LVOT obstruction Narrowed diameter of the LVOT due to increased septal wall thickness Apically positioned papillary muscles that tether the mitral valve plane toward the ventricular septum Elongated anterior leaflet of the mitral valve ↓ LVOT obstruction
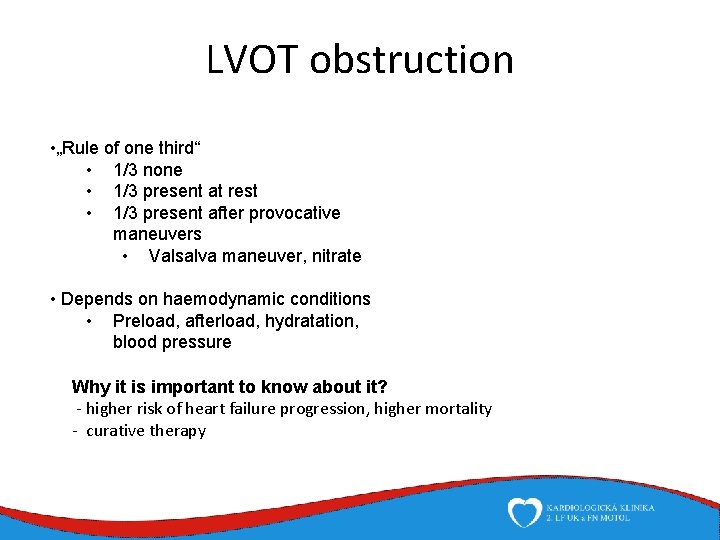
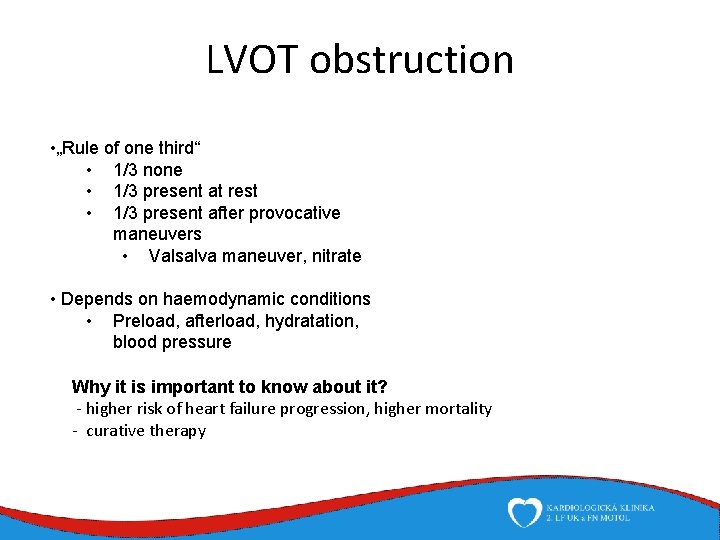
LVOT obstruction • „Rule of one third“ • 1/3 none • 1/3 present at rest • 1/3 present after provocative maneuvers • Valsalva maneuver, nitrate • Depends on haemodynamic conditions • Preload, afterload, hydratation, blood pressure Why it is important to know about it? - higher risk of heart failure progression, higher mortality - curative therapy
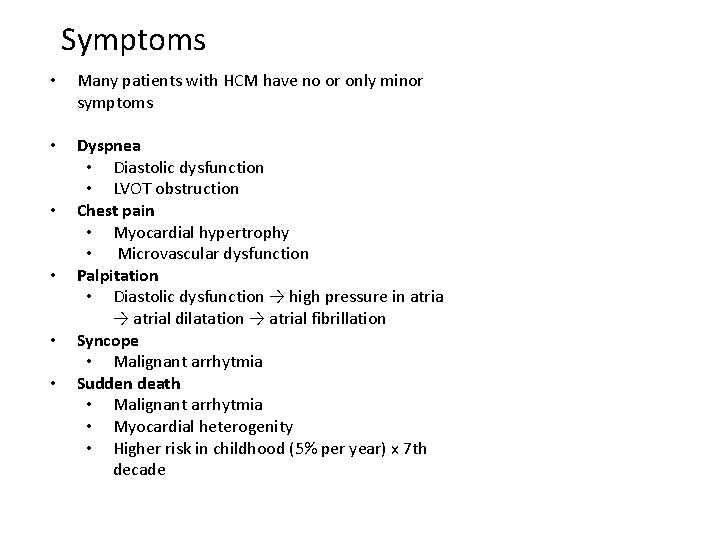
Symptoms • Many patients with HCM have no or only minor symptoms • Dyspnea • Diastolic dysfunction • LVOT obstruction Chest pain • Myocardial hypertrophy • Microvascular dysfunction Palpitation • Diastolic dysfunction → high pressure in atria → atrial dilatation → atrial fibrillation Syncope • Malignant arrhytmia Sudden death • Malignant arrhytmia • Myocardial heterogenity • Higher risk in childhood (5% per year) x 7 th decade • •
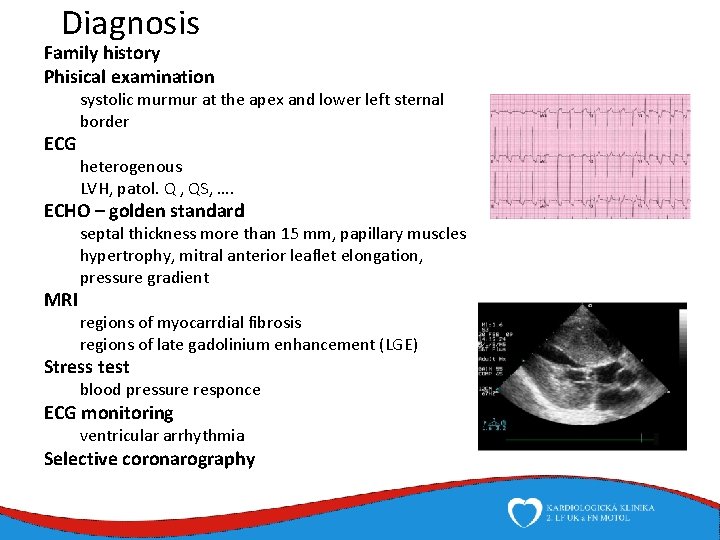
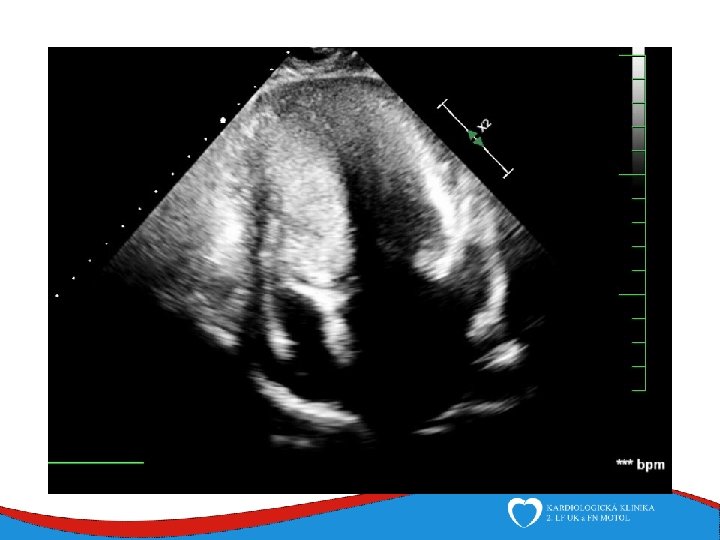
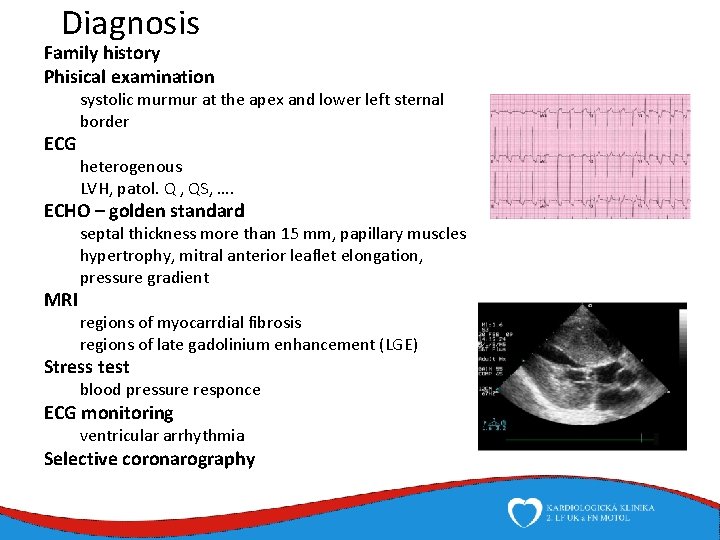
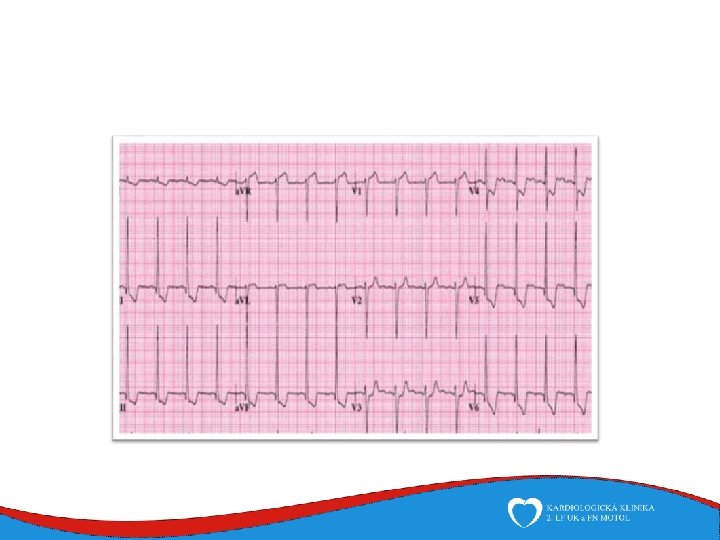
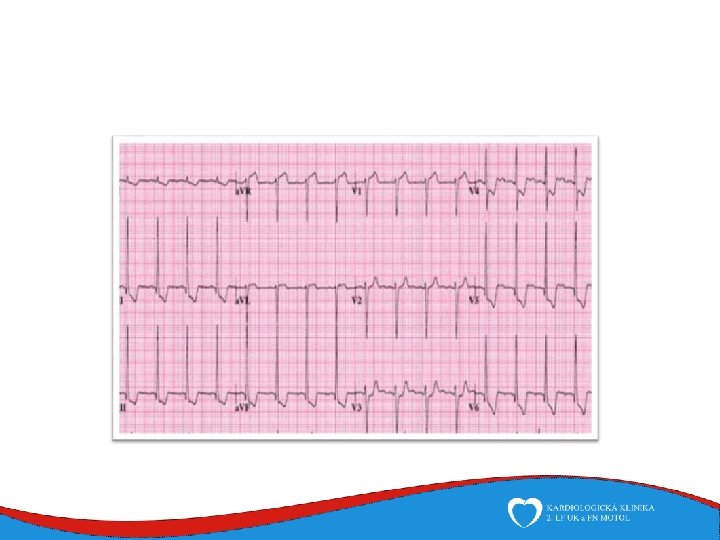
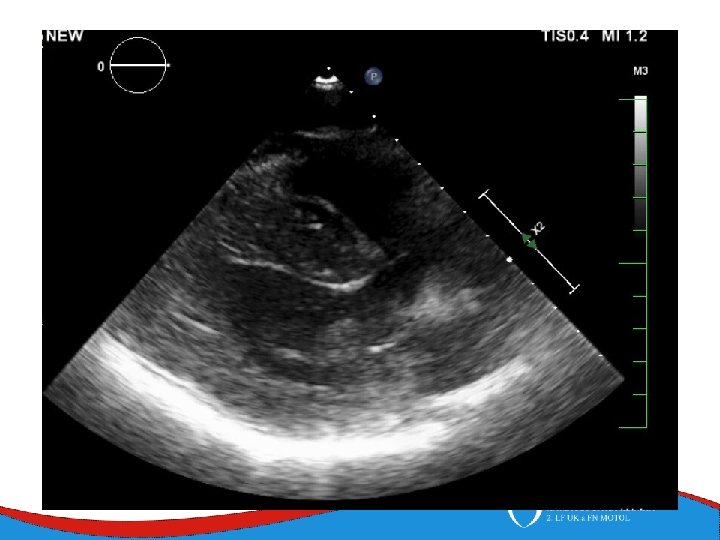
Diagnosis Family history Phisical examination ECG systolic murmur at the apex and lower left sternal border heterogenous LVH, patol. Q , QS, …. ECHO – golden standard MRI septal thickness more than 15 mm, papillary muscles hypertrophy, mitral anterior leaflet elongation, pressure gradient regions of myocarrdial fibrosis regions of late gadolinium enhancement (LGE) Stress test blood pressure responce ECG monitoring ventricular arrhythmia Selective coronarography
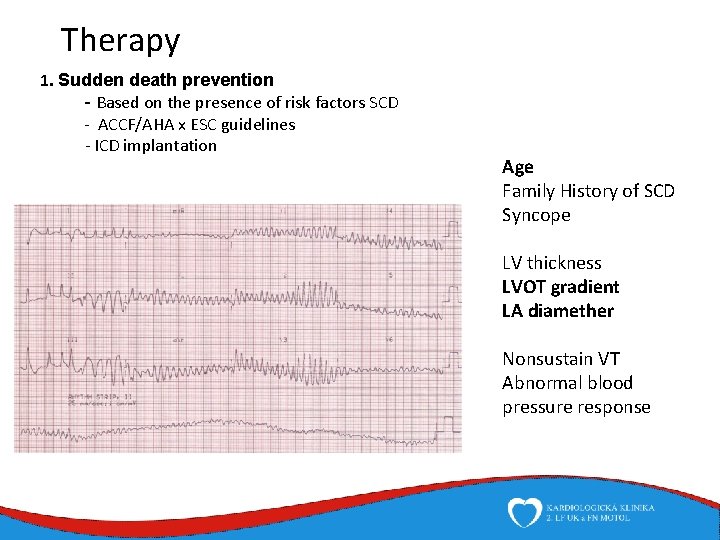
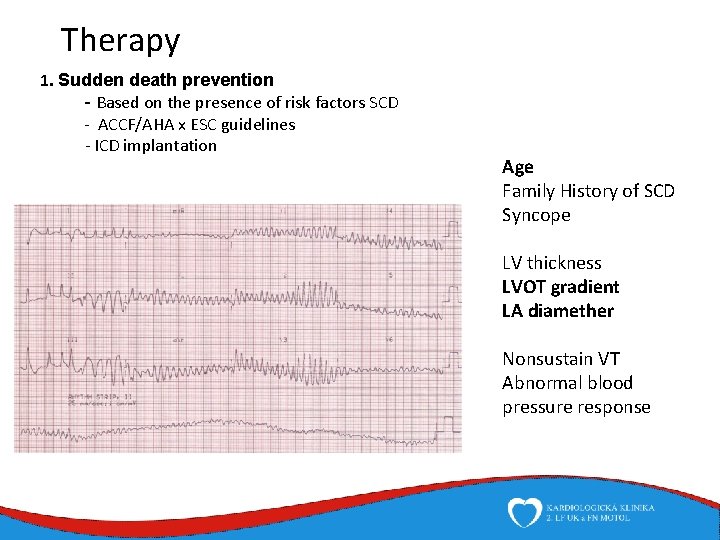
Therapy 1. Sudden death prevention - Based on the presence of risk factors SCD - ACCF/AHA x ESC guidelines - ICD implantation Age Family History of SCD Syncope LV thickness LVOT gradient LA diamether Nonsustain VT Abnormal blood pressure response
Medical therapy Heart failure therapy BB Diuretics ACEi, sartans (systolic dysfunction) Aldosterone receptors blockers (systolic dysfunction) Obstruction BB Verapamil Prevention of thromboembolic complications of atrial fibrillation amiodaron, dronedaron, sotalol warfarin, NOACs
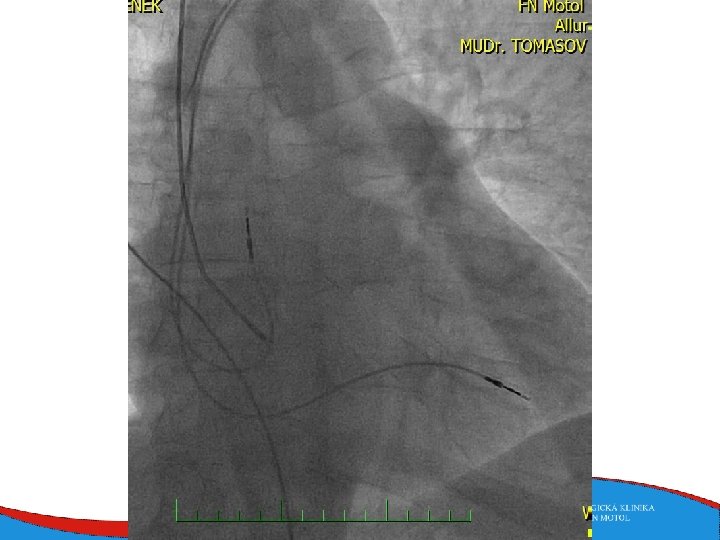
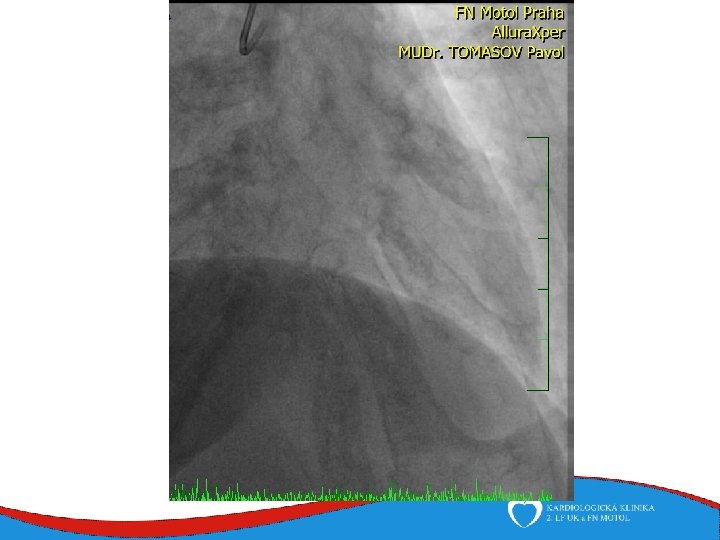
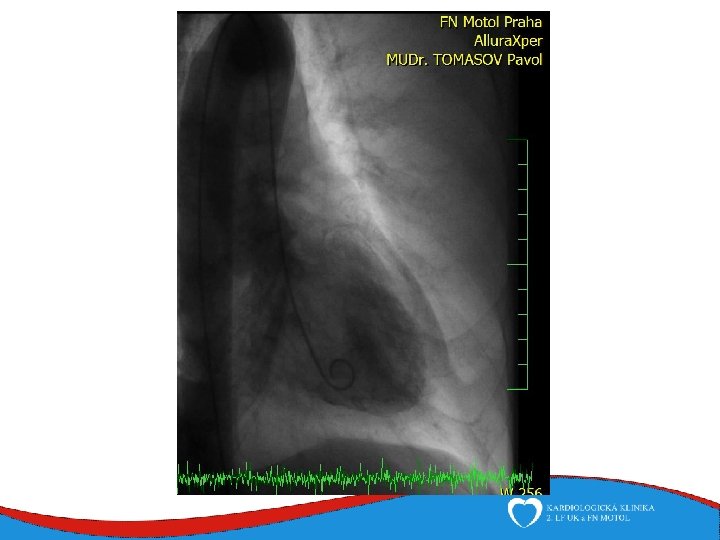
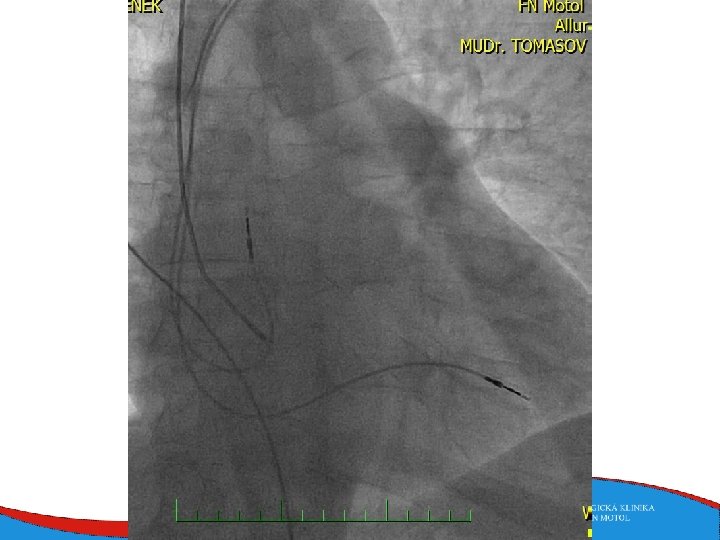
Septal reduction therapy (for ventricular obstruction) • Surgical myectomy • Septal ablation • Symptomatic patients despite the optimal medical therapy • A small amount of alcohol is induced into a septal branch • Myocardial scar and subsequent reduction in the diameter of the basal septum
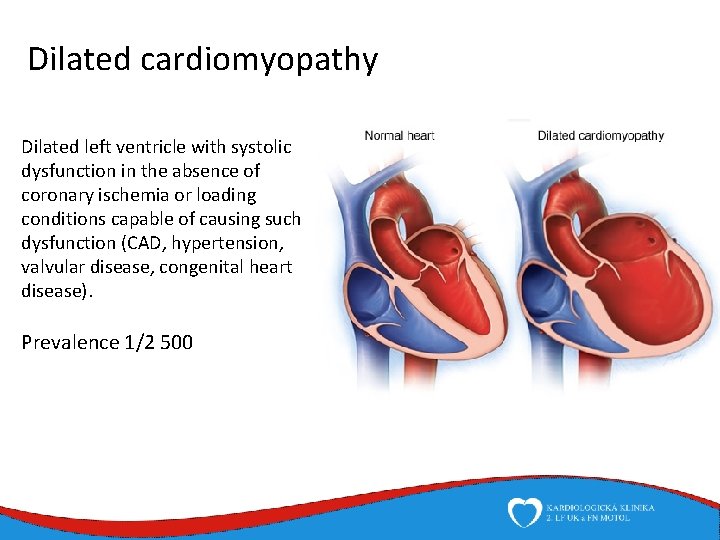
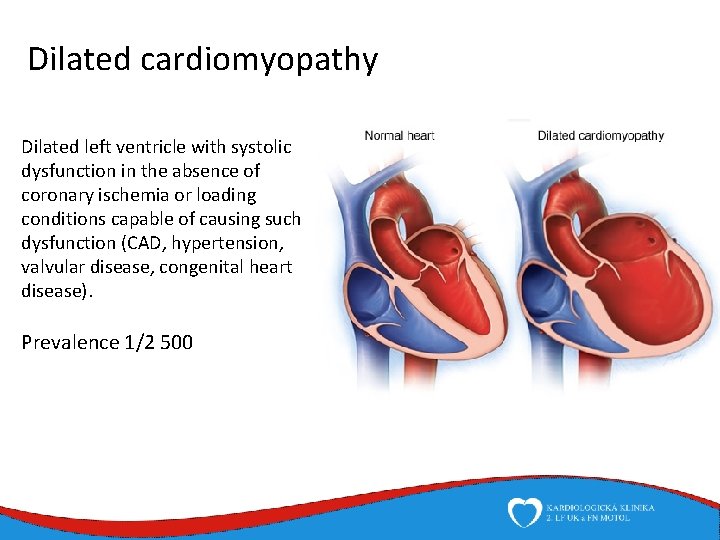
Dilated cardiomyopathy Dilated left ventricle with systolic dysfunction in the absence of coronary ischemia or loading conditions capable of causing such dysfunction (CAD, hypertension, valvular disease, congenital heart disease). Prevalence 1/2 500
Dilated cardiomyopathy • Specific causes • Inflammatory • History of myocarditis • Viral aetiology+ predisposition • Toxic • Alhohol induced • 90 g alcolol/day 5 years + predisposition • Cocain induced • Drug induced • Peripartal • 1/2000 birth, unknown patophysiology • Muscular dystrophias • Duchen and Becker • Familiar DCM • 1/3 predisposition • sarcomeric, cytoskeletal , nuclear membrane genes • DCM of unknown etilogy
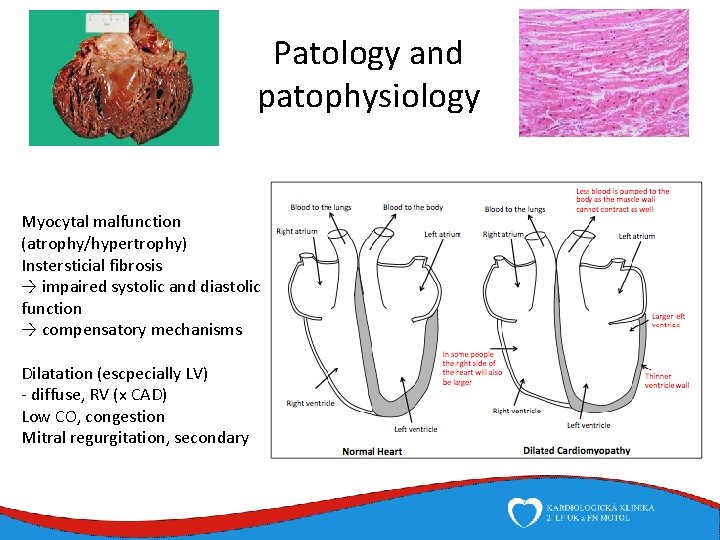
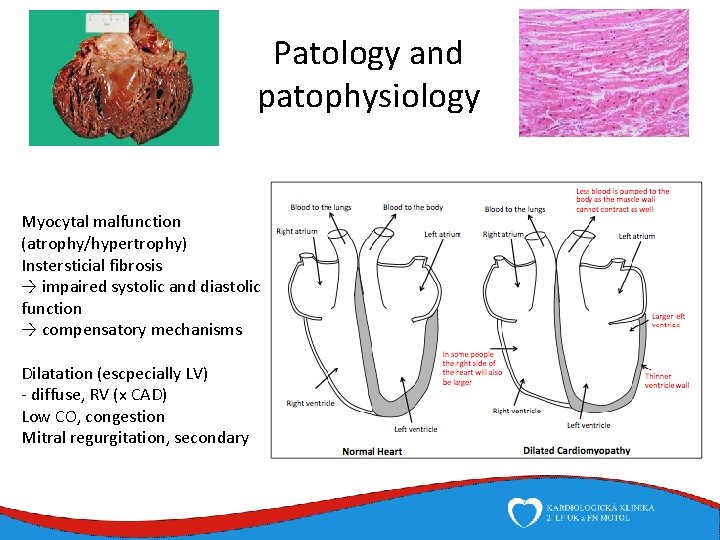
Patology and patophysiology Myocytal malfunction (atrophy/hypertrophy) Instersticial fibrosis → impaired systolic and diastolic function → compensatory mechanisms Dilatation (escpecially LV) - diffuse, RV (x CAD) Low CO, congestion Mitral regurgitation, secondary
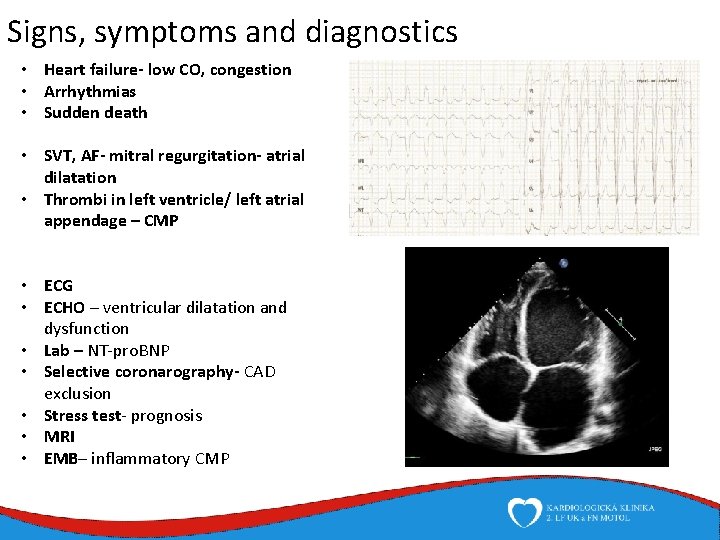
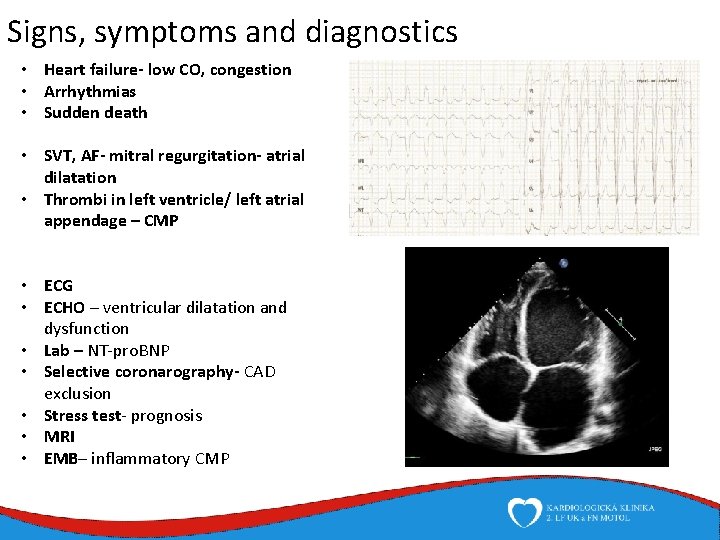
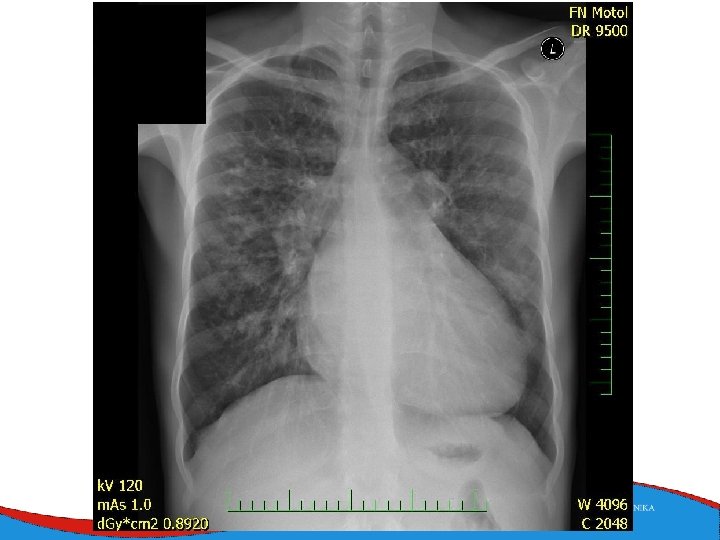
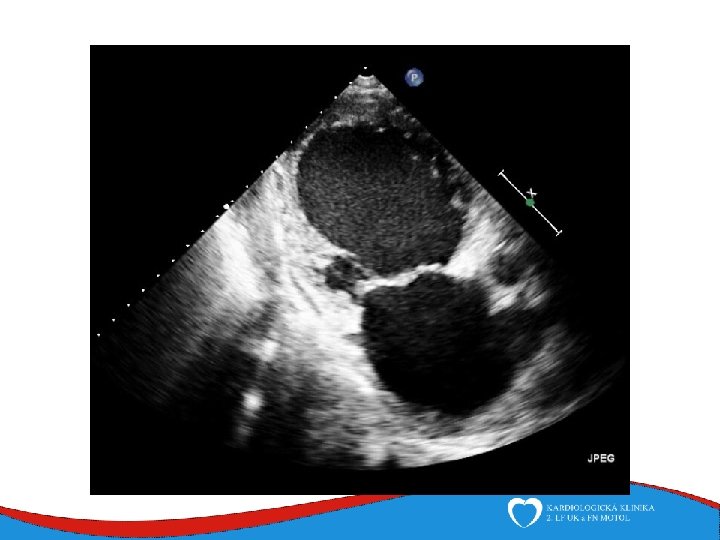
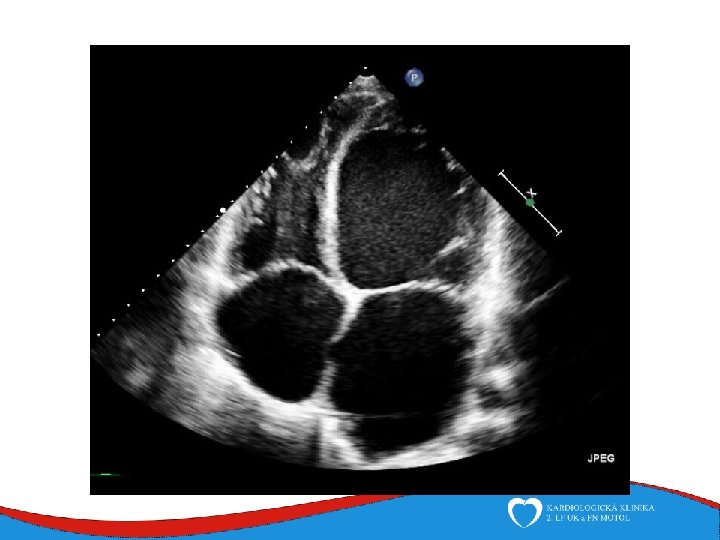
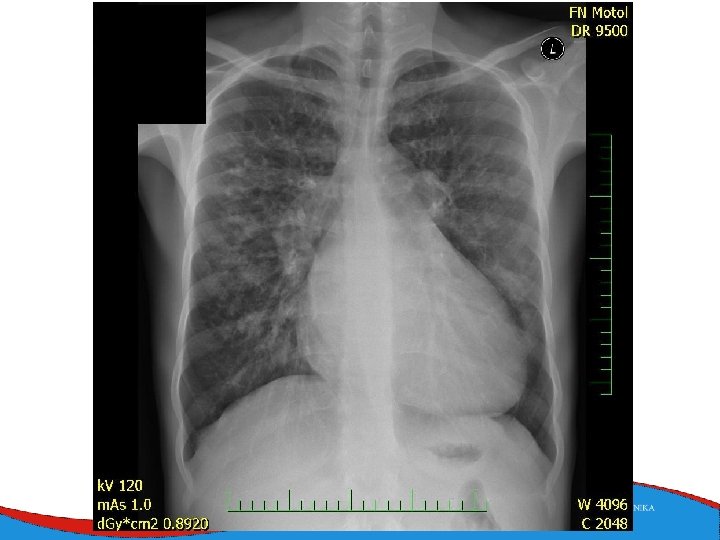
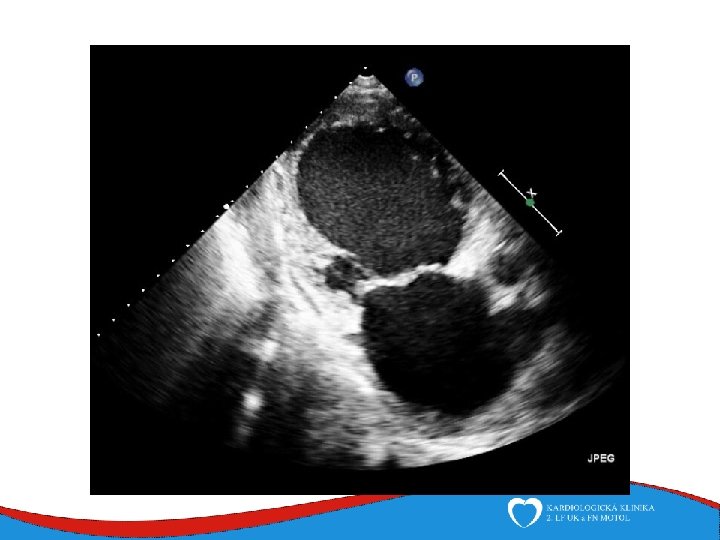
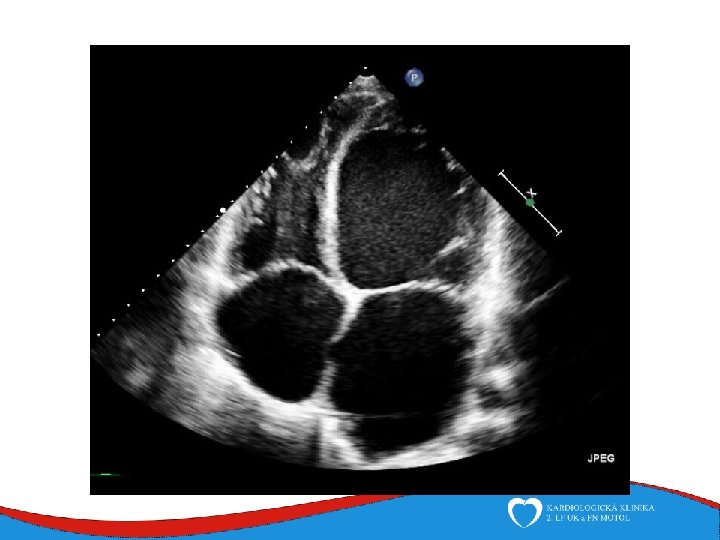
Signs, symptoms and diagnostics • Heart failure- low CO, congestion • Arrhythmias • Sudden death • SVT, AF- mitral regurgitation- atrial dilatation • Thrombi in left ventricle/ left atrial appendage – CMP • ECG • ECHO – ventricular dilatation and dysfunction • Lab – NT-pro. BNP • Selective coronarography- CAD exclusion • Stress test- prognosis • MRI • EMB– inflammatory CMP
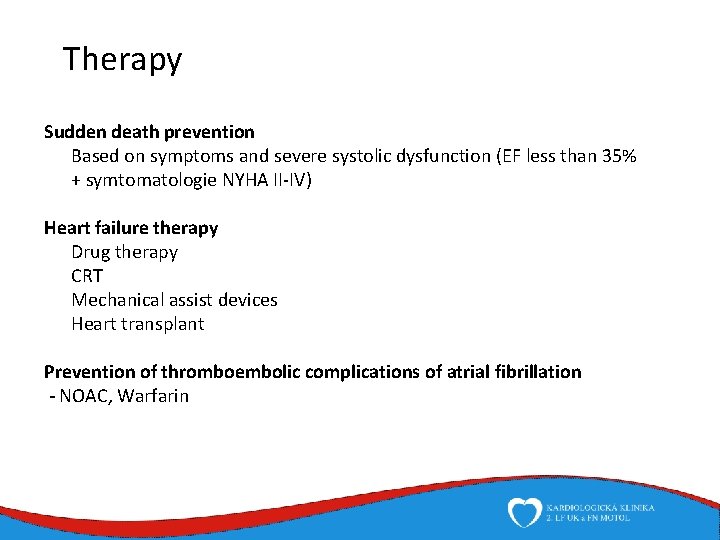
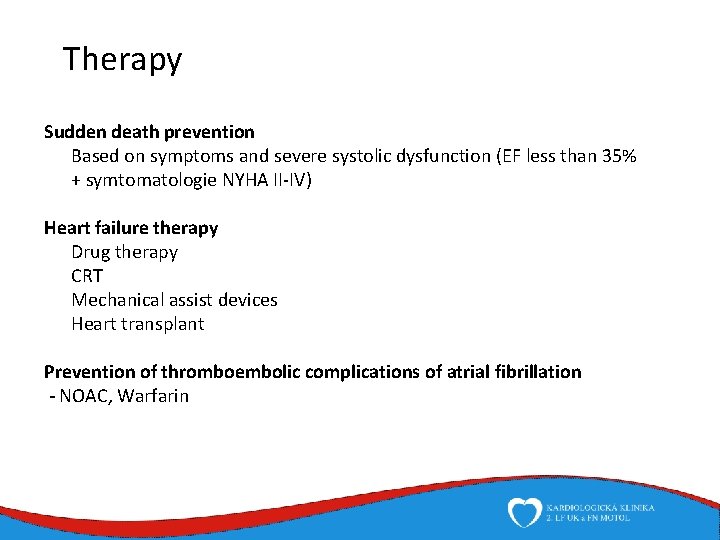
Therapy Sudden death prevention Based on symptoms and severe systolic dysfunction (EF less than 35% + symtomatologie NYHA II-IV) Heart failure therapy Drug therapy CRT Mechanical assist devices Heart transplant Prevention of thromboembolic complications of atrial fibrillation - NOAC, Warfarin
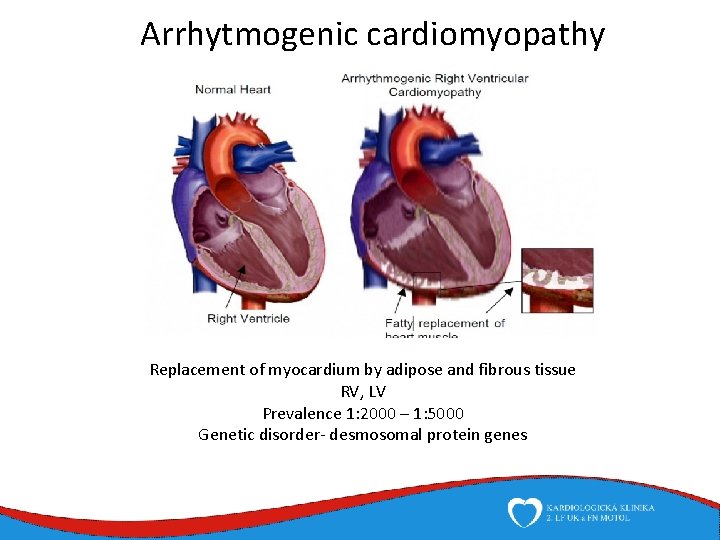
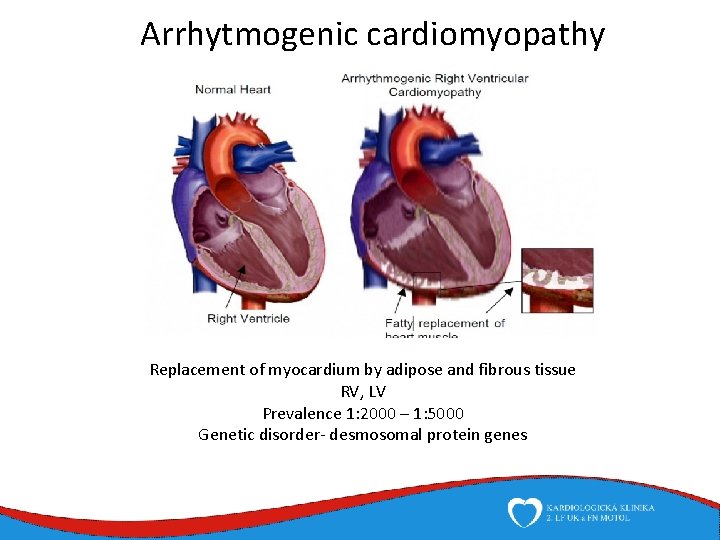
Arrhytmogenic cardiomyopathy Replacement of myocardium by adipose and fibrous tissue RV, LV Prevalence 1: 2000 – 1: 5000 Genetic disorder- desmosomal protein genes
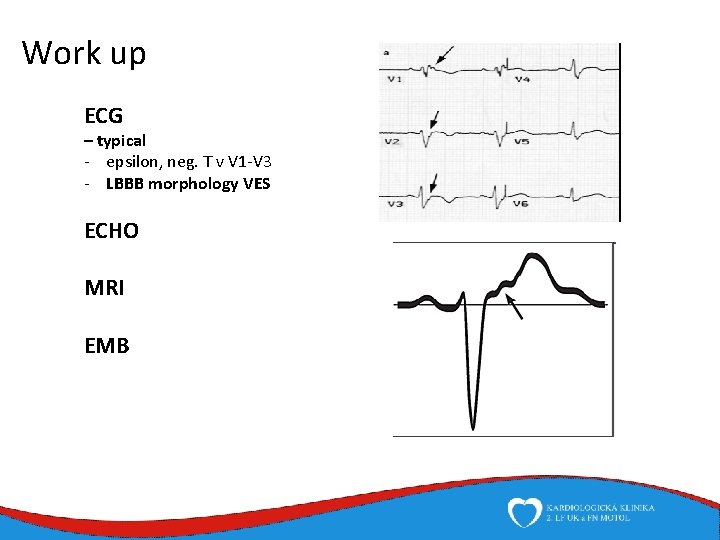
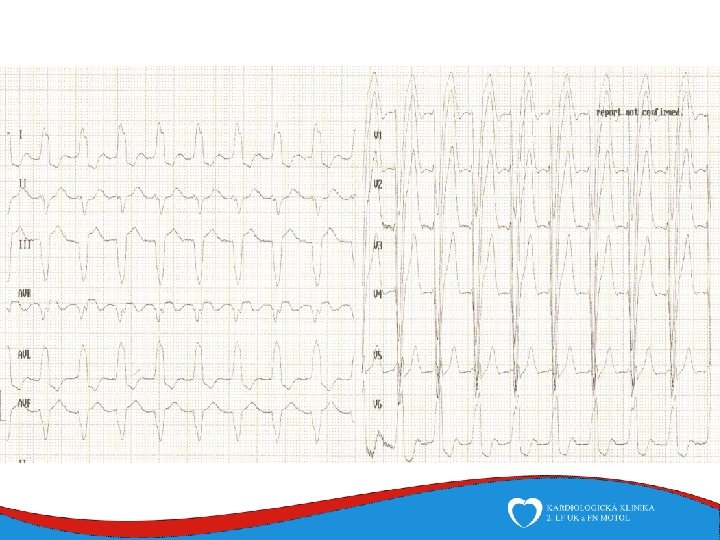
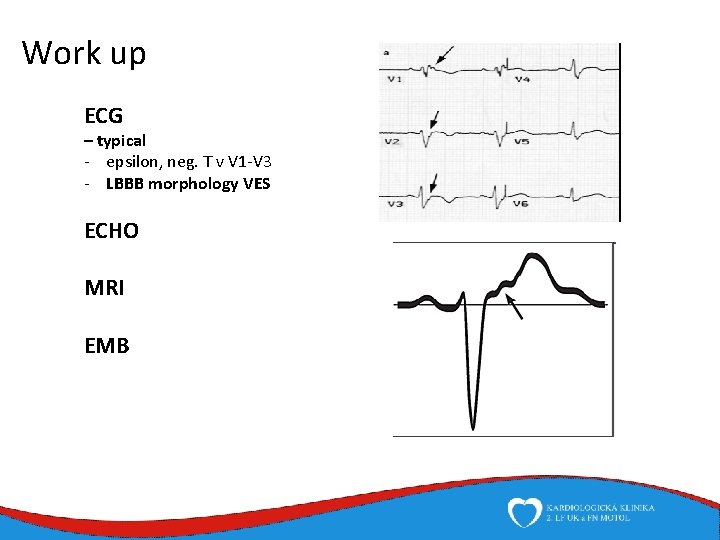
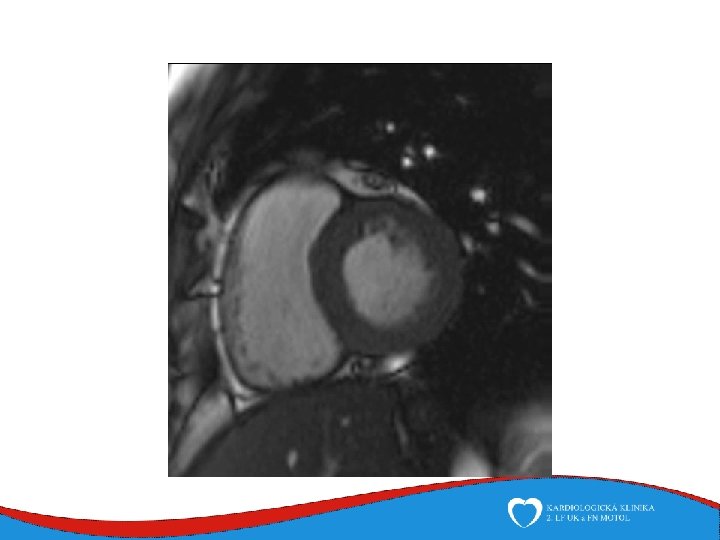
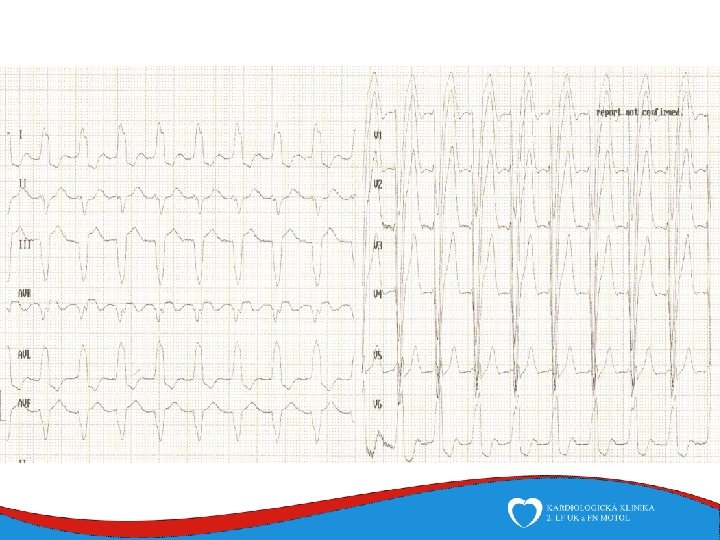
Work up ECG – typical - epsilon, neg. T v V 1 -V 3 - LBBB morphology VES ECHO MRI EMB
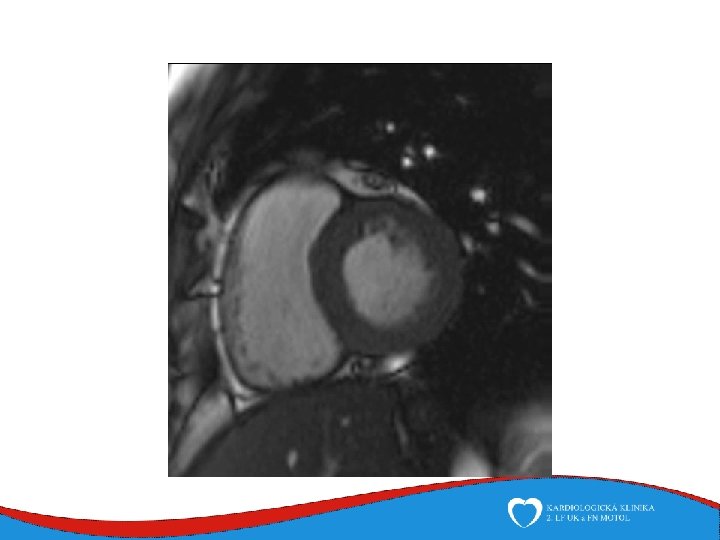
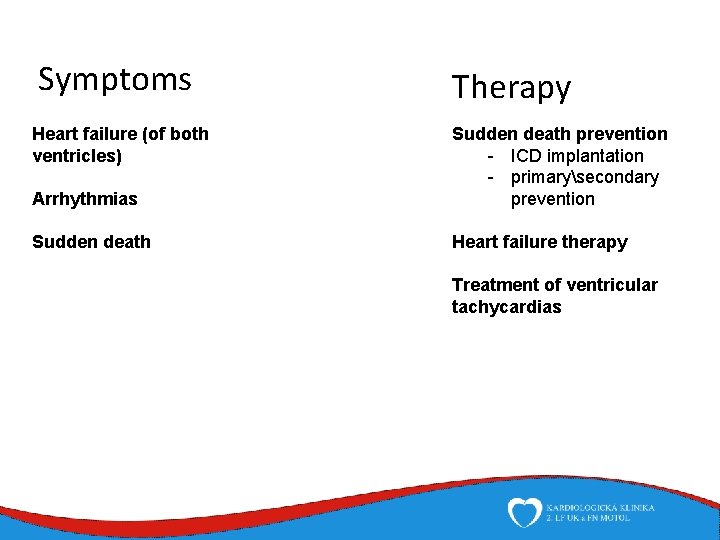
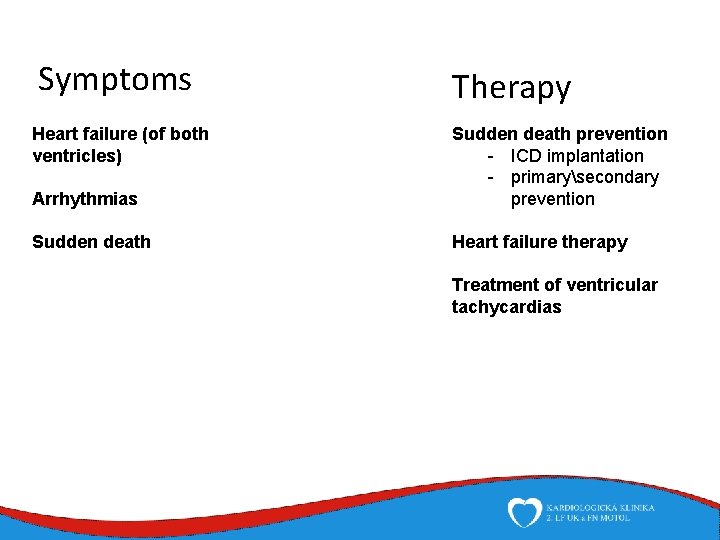
Symptoms Heart failure (of both ventricles) Therapy Arrhythmias Sudden death prevention - ICD implantation - primarysecondary prevention Sudden death Heart failure therapy Treatment of ventricular tachycardias
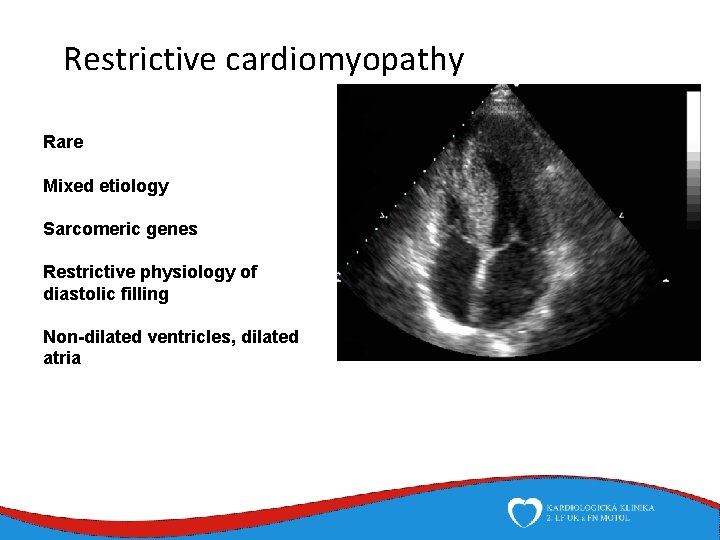
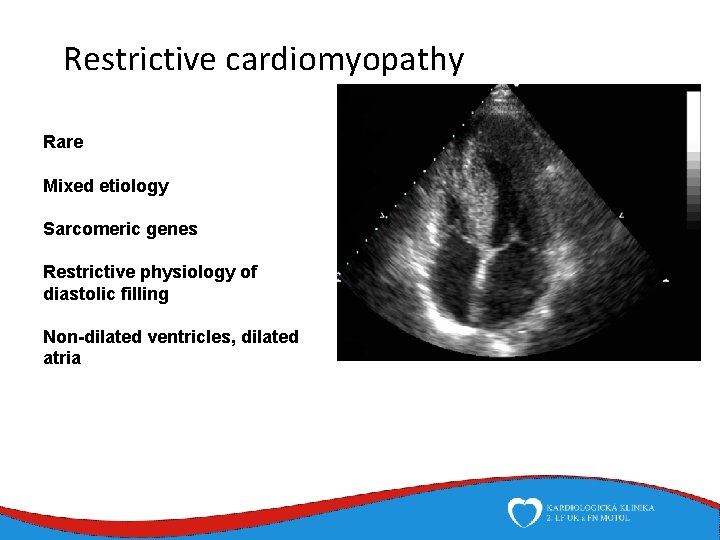
Restrictive cardiomyopathy Rare Mixed etiology Sarcomeric genes Restrictive physiology of diastolic filling Non-dilated ventricles, dilated atria
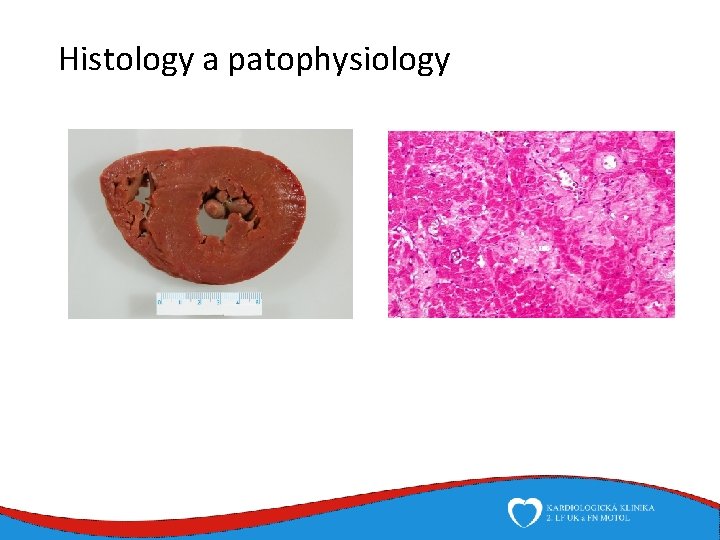
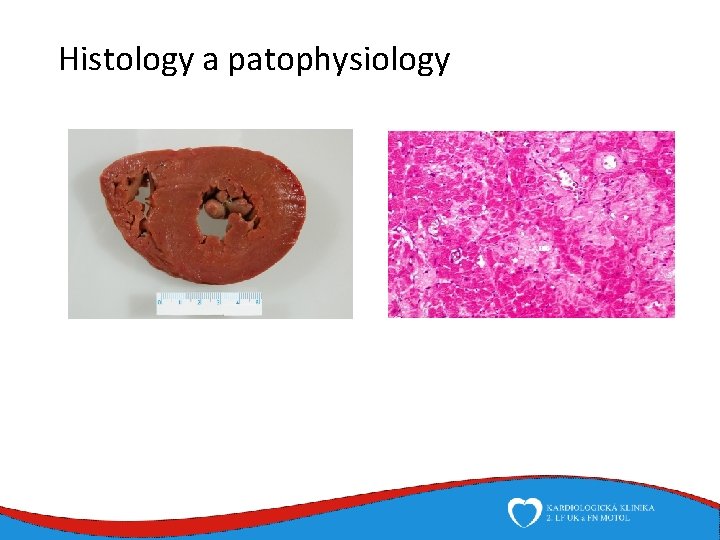
Histology a patophysiology
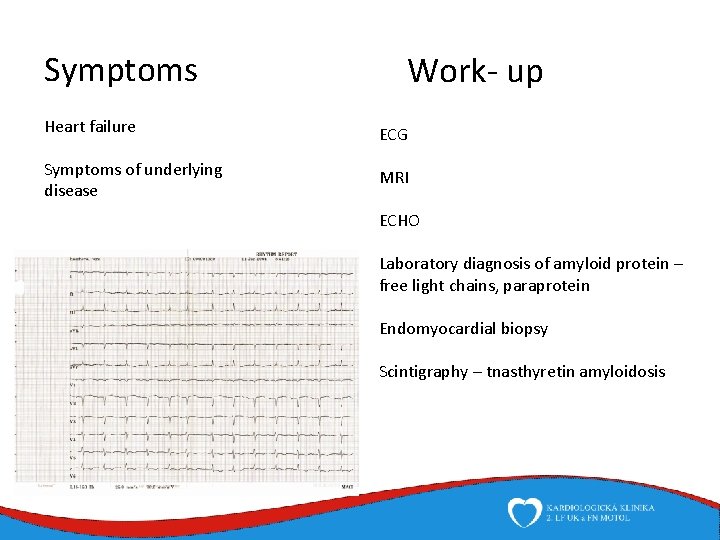
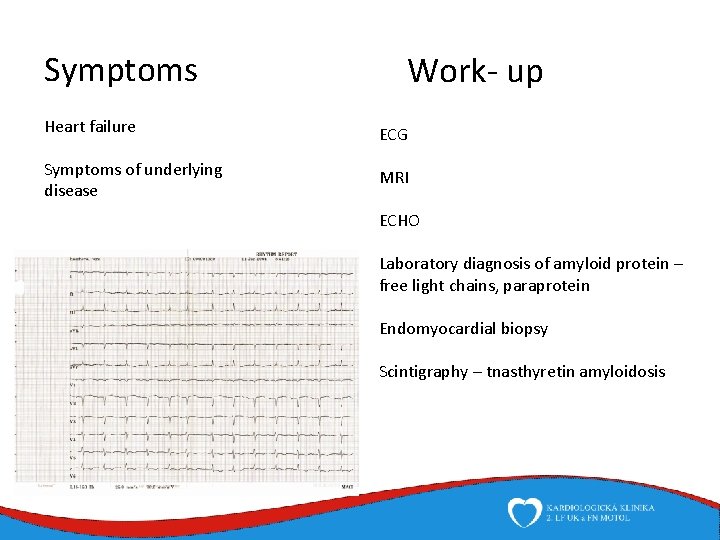
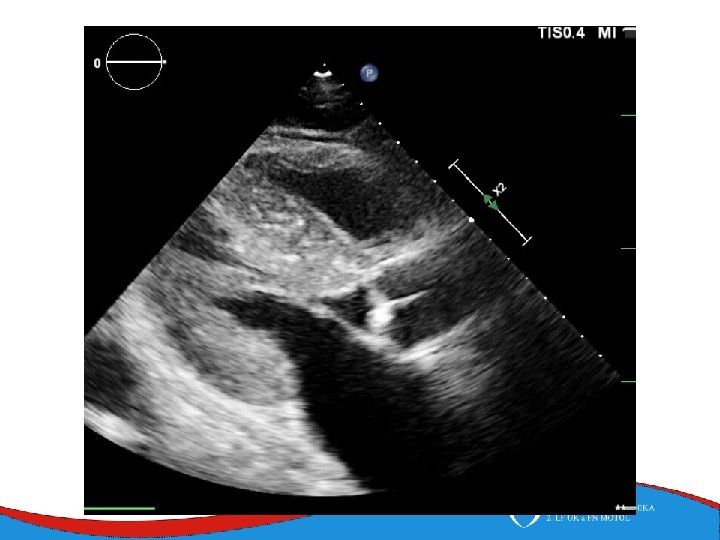
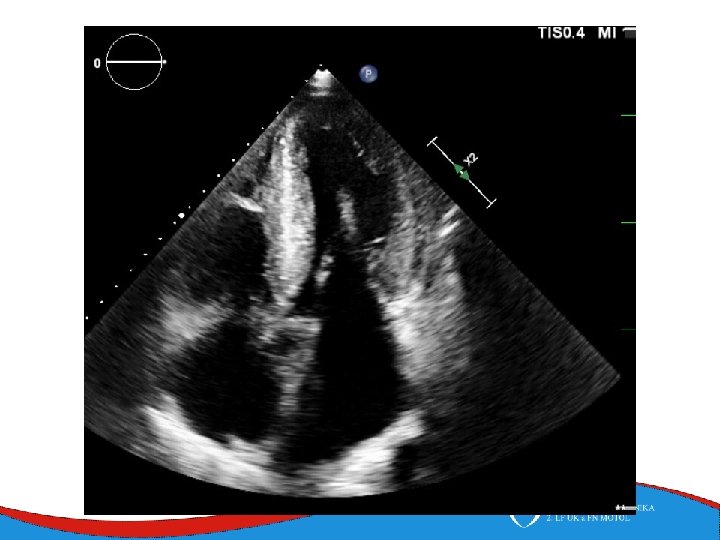
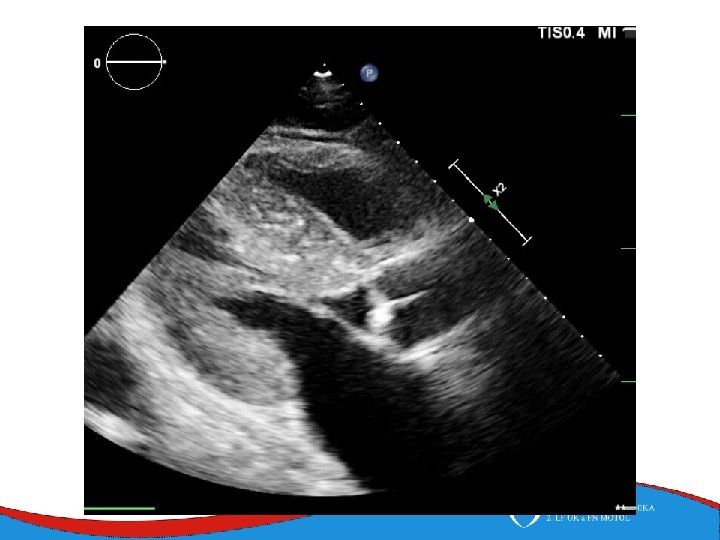
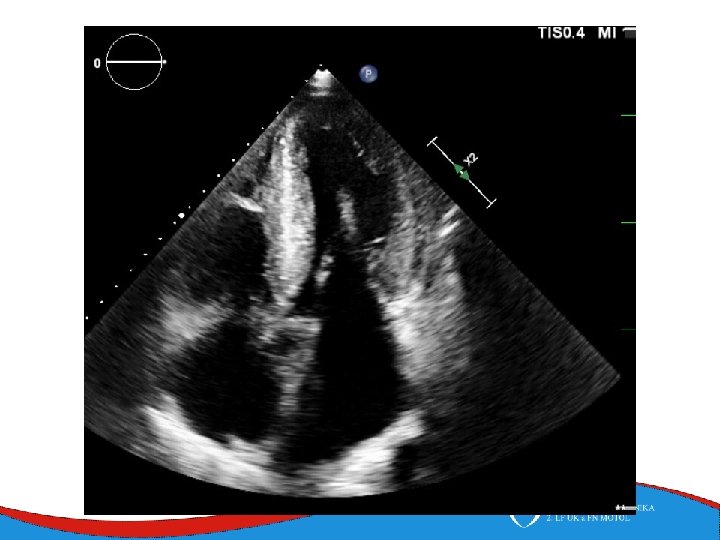
Symptoms Work- up Heart failure ECG Symptoms of underlying disease MRI ECHO Laboratory diagnosis of amyloid protein – free light chains, paraprotein Endomyocardial biopsy Scintigraphy – tnasthyretin amyloidosis
Therapy Heart failure therapy (including heart transplant) Liver transplant Hematology Specific therapy against amyloid protein
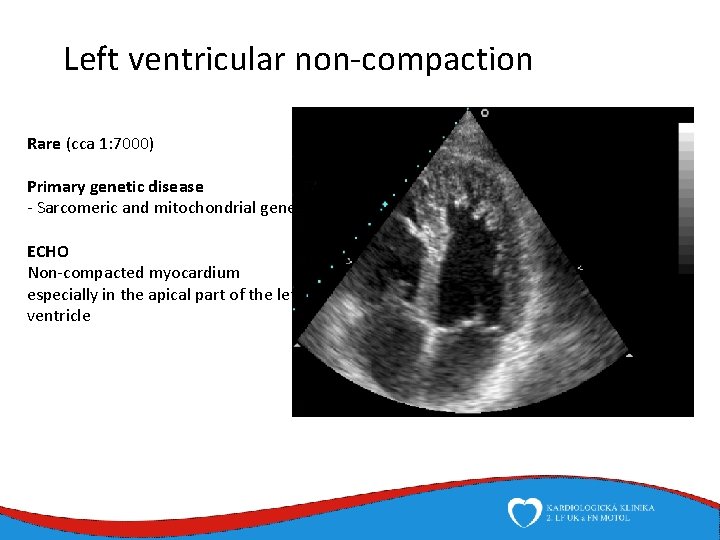
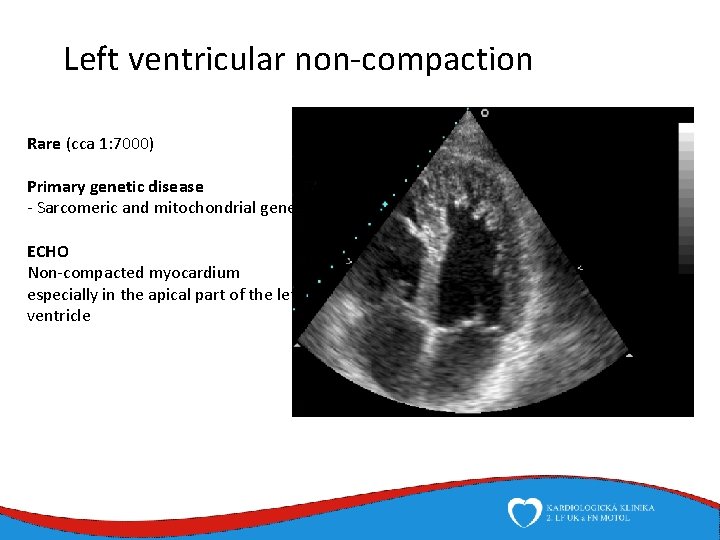
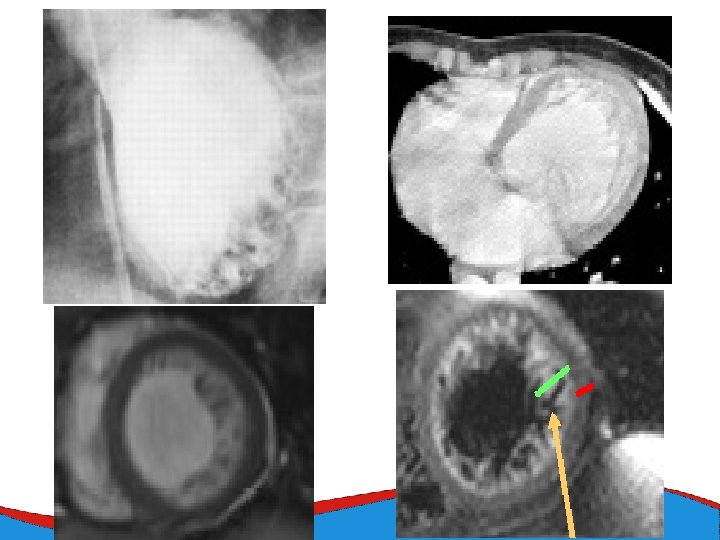
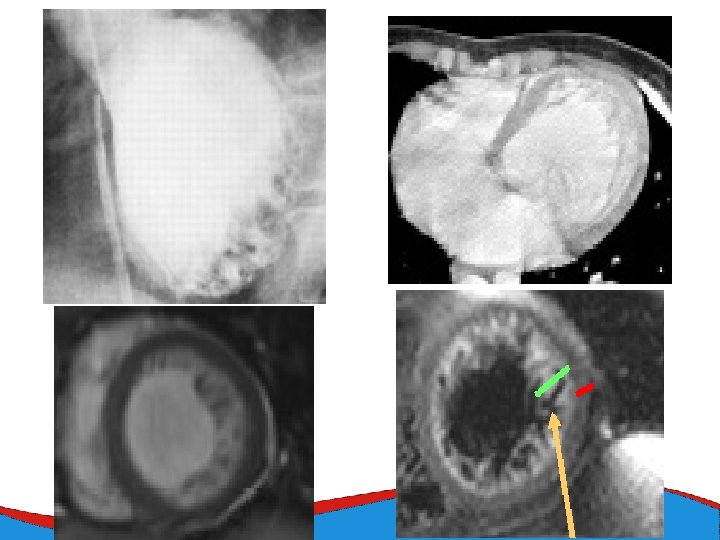
Left ventricular non-compaction Rare (cca 1: 7000) Primary genetic disease - Sarcomeric and mitochondrial genes ECHO Non-compacted myocardium especially in the apical part of the left ventricle
Left ventricular non-compaction • Signs and symptoms • Heart failure • Thromboembolic complications • LV trabecularization- predisposition • Anticoagulation therapy (systolic dysfunction) • DG – echo, MRI • Therapy – heart failure therapy, anticoagulation therapy
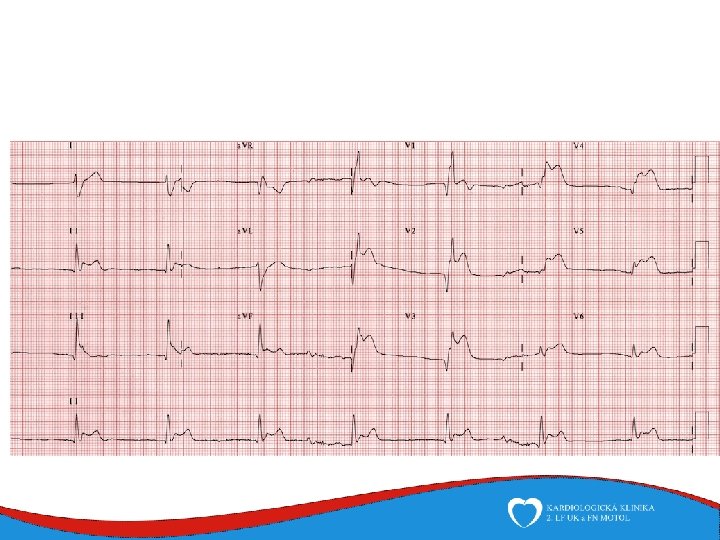
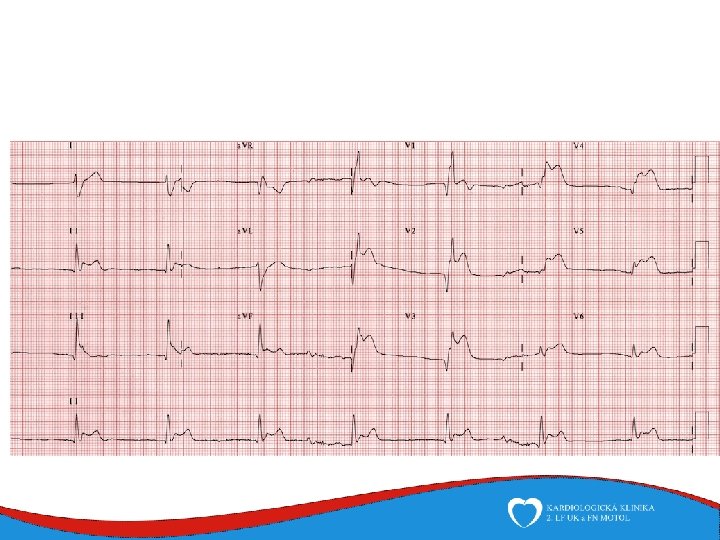
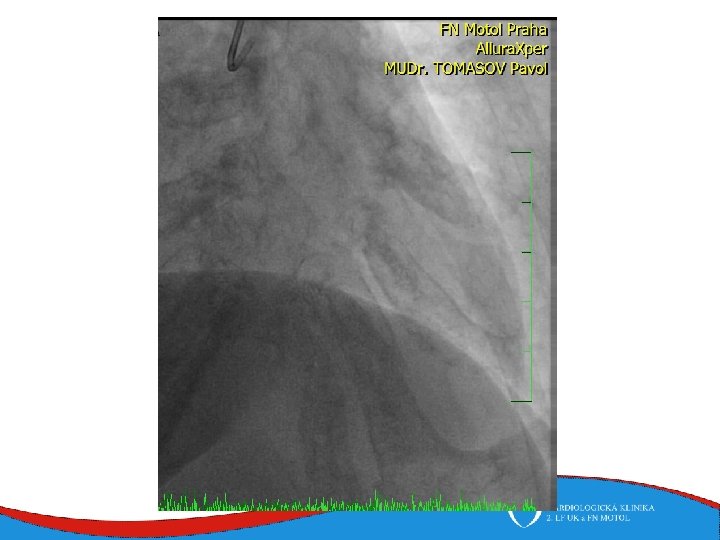
Case report Woman, 75 years Comes to ED for new-onset chest pain and weakness History: hyperthyreosis Drugs: Thyrozol Family history: no cardiovascular diseases Physical: BP 105/70, HR 92/min, RR 20 breaths/min, sat O 2 94%
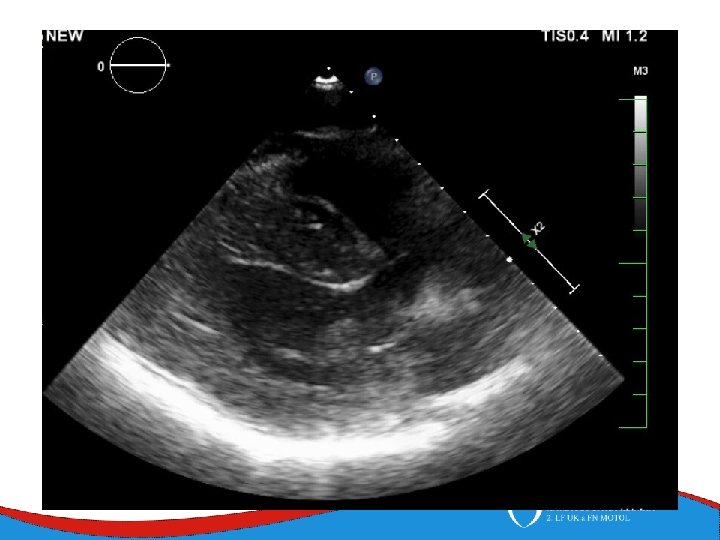
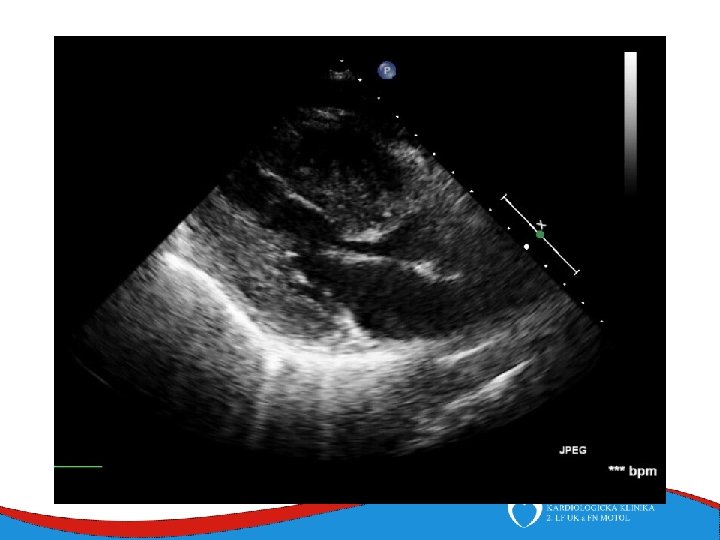
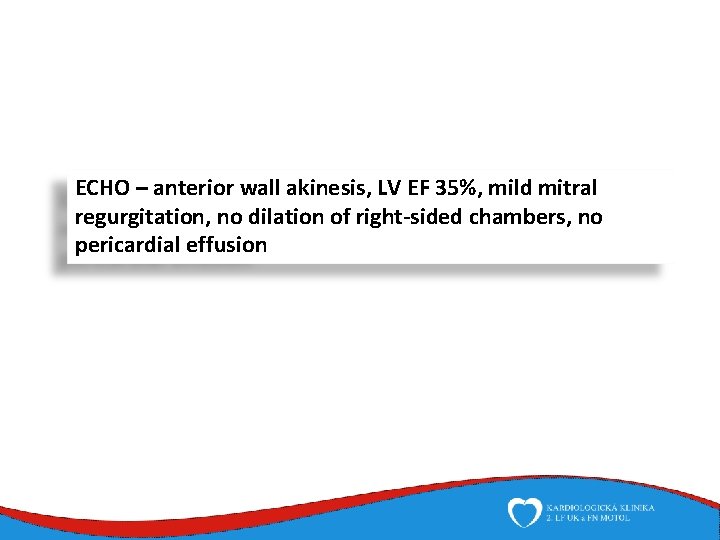
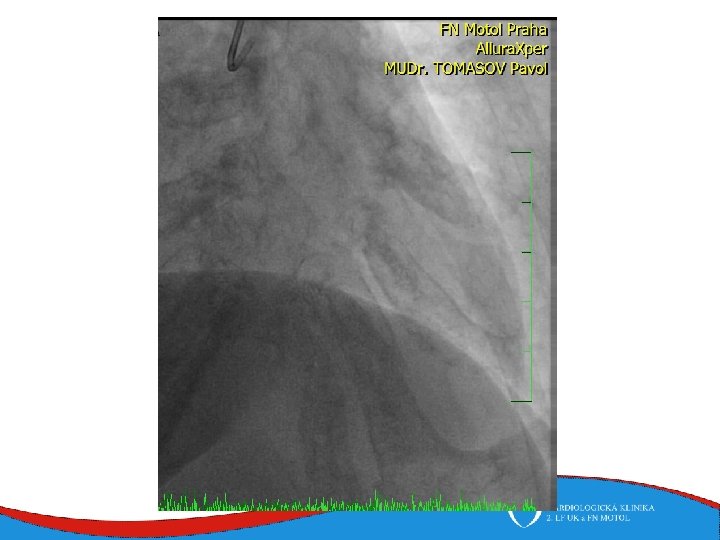
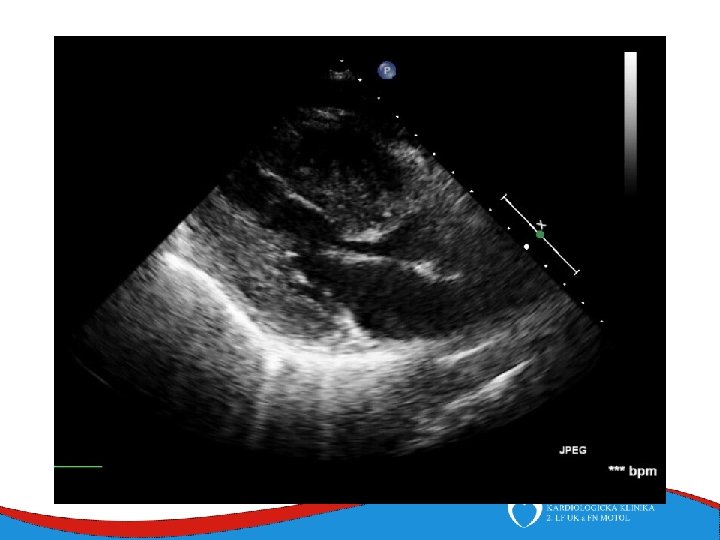
ECHO – anterior wall akinesis, LV EF 35%, mild mitral regurgitation, no dilation of right-sided chambers, no pericardial effusion
1
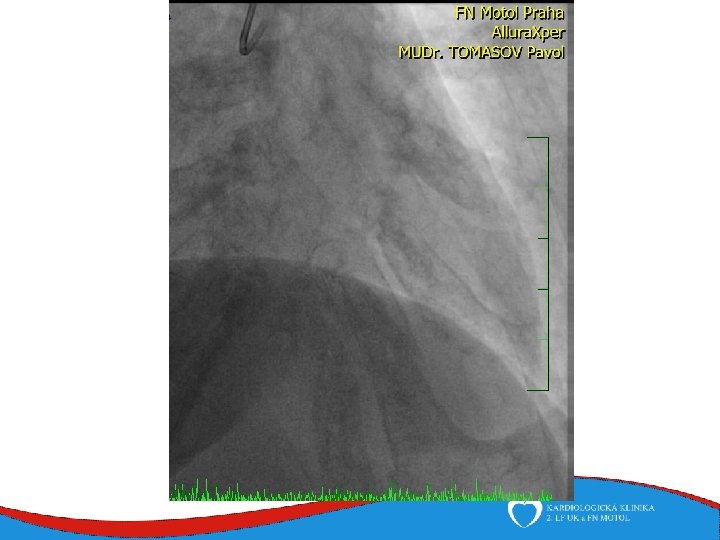
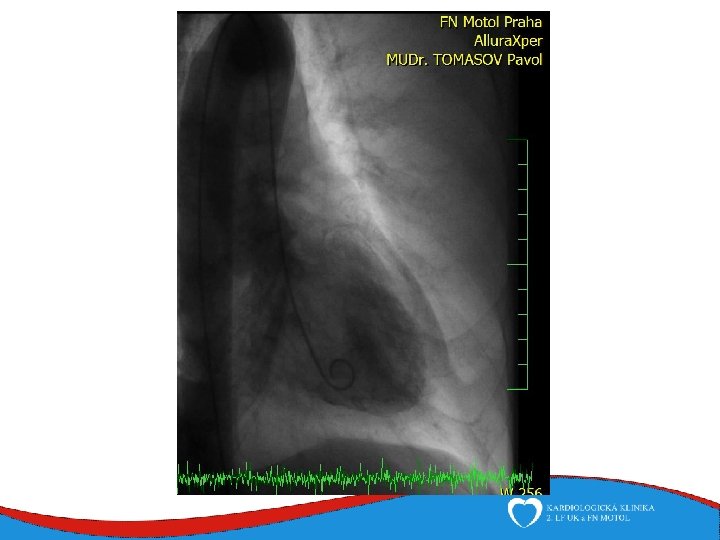

Tako-tsubo
 Myo muscle
Myo muscle Cmp
Cmp Bafra turizm myo
Bafra turizm myo Mkp myo
Mkp myo ısparta uluborlu selahattin karasoy meslek yüksekokulu
ısparta uluborlu selahattin karasoy meslek yüksekokulu Muscle root word
Muscle root word Fin smart ring
Fin smart ring Mkp myo
Mkp myo Oculus rift tutorial
Oculus rift tutorial Root word ase
Root word ase Araklı myo
Araklı myo Prutie vzor
Prutie vzor Denisa predeteanu
Denisa predeteanu Mudr denisa osinova
Mudr denisa osinova Denisa vinanska
Denisa vinanska Mudr denisa osinova
Mudr denisa osinova Denisa vinanska
Denisa vinanska Denisa predeteanu
Denisa predeteanu Tamara ionescu
Tamara ionescu Paobrazy
Paobrazy Denisa červenková
Denisa červenková Pic of smooth muscle
Pic of smooth muscle Toe dancers muscle a two bellied muscle of the calf
Toe dancers muscle a two bellied muscle of the calf Vddi cardio
Vddi cardio Stopul cardio respirator definitie
Stopul cardio respirator definitie Cristina skrypnyk
Cristina skrypnyk Index cardio thoracique
Index cardio thoracique Culmen poumon
Culmen poumon Gr chest 2 projections
Gr chest 2 projections Cardiovision
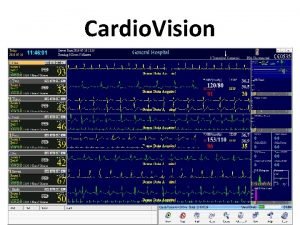
Cardiovision Champs pulmonaires clairs
Champs pulmonaires clairs Cauze reversibile de stop cardio-respirator
Cauze reversibile de stop cardio-respirator Ingurgitación yugular
Ingurgitación yugular Nssttc
Nssttc Cardio sense
Cardio sense Calcul index cardio thoracique
Calcul index cardio thoracique Ejemplos de prefijo auto
Ejemplos de prefijo auto Signe de cruveilhier baumgarten
Signe de cruveilhier baumgarten Cardiomems video
Cardiomems video Tonus cardio moderateur
Tonus cardio moderateur Softecg
Softecg Cardio map
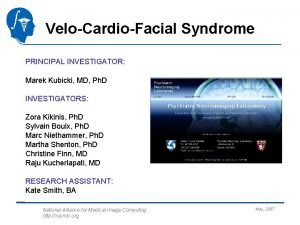
Cardio map Velo cardio facial syndrome
Velo cardio facial syndrome Trusight cardio
Trusight cardio 4tech cardio
4tech cardio Discovery cardio care programme
Discovery cardio care programme Velo-cardio-facial syndrome pictures
Velo-cardio-facial syndrome pictures Electro cardio gram
Electro cardio gram Atl cardio
Atl cardio Cardio alex
Cardio alex Inferior wall heart blood supply
Inferior wall heart blood supply Heart muscle
Heart muscle How is the heart muscle nourished
How is the heart muscle nourished Define autorhythmicity
Define autorhythmicity Function of smooth muscle
Function of smooth muscle Dullness to percussion
Dullness to percussion Sheep heart facts
Sheep heart facts Hart to hart merrylands
Hart to hart merrylands Muscle re education definition
Muscle re education definition Bipennate muscle definition
Bipennate muscle definition