Cardiac Rehabilitation Matthew N Bartels MD MPH Department
Cardiac Rehabilitation Matthew N. Bartels, MD, MPH Department of Rehabilitation Medicine Montefiore Medical Center Albert Einstein College of Medicine
Learning Objectives • Learn the basic terminology of exercise physiology • Learn basic principles of Cardiac Rehabilitation (CR) • Learn needed testing to allow for cardiac rehabilitation • Learn the conditions that are treated as an outpatient • Learn the application of cardiac rehabilitation services in the acute and inpatient rehabilitation settings
Learning Objectives • Identify common neurological, musculoskeletal and orthopedic limitations seen with Cardiac Rehabilitation. • Learn appropriate adaptations to allow for completion of a cardiac rehabilitation program in patients with Learn simple adaptations for safe exercise with co-morbidities.
Basic Terms • • • Aerobic Capacity Cardiac Output Heart Rate Stroke Volume Myocardial Oxygen Consumption
Assessment of Demands of Cardiac Activities • Typically described in terms of metabolic equivalents – 1 MET = 3. 5 m. L O 2/Kg weight/min • Use of standardized MET tables can help assess independence AND GOALS • Help to establish disability and support needs
Role of Exercise Tolerance Testing • Functional versus diagnostic exercise tests • Diagnostic testing for cardiac risk assessment and evaluation of cardiac risk • Functional testing to determine: – Exercise capacity – Safety – Maximum heart rate • Can be estimated by 220 -age • Baseline functional stress testing to obtain individualized maximum heart rate
Functional ETT Protocols • Numerous protocols – Balke-Ware, Naughton, Bruce, others • Can be done with ramped/staged Cycle Ergometry • Basic principles – Staged levels – Done in controlled setting – Treadmill most common – Evaluate for heart rate and safety guidelines
Diagnostic ETT Testing • Goal is to provoke a positive response for plan of further interventions. – Pharmacologic Stress • Dobutamine/adenosine/persantine tests – Alternate diagnostic criteria • Echocardiography • Nuclear Imaging • MRI, and others • Often done off or on limited meds to provoke events/ischemia • Often of limited use for exercise prescription with no clear heart rate targets or not done with actual exercise (phamacologic)
Pros/Cons of Diagnostic ETT for Cardiac Rehab • Benefits: – Can assess cardiac risk – Help diagnose issues to be treated • However: – Often not useful for setting heart rate guidelines – Can’t assess functional response to exercise – Unless done on medications, can’t asses status for cardiac therapy program – Does not allow for evaluation of recovery from exercise and post exercise risks
Other diagnostic studies for CR • Baseline cardiogram • Assessment of ischemia for those with coronary disease (CAD) • Arrhythmia risk assessment • Consideration of Peripheral Vascular Disease (PVD) – Can seriously limit progress in a conditioning program • Management of Heart Failure (HF)
Question 1: • All patients who start a program of cardiac rehabilitation should have consideration of all of the following tests except: – A. Electrocardiogram – B. Cardiac stress test – C. Non invasive flow studies of the legs – D. Echocardiogram – E. Chest computed tomography Scan
Principles of Aerobic Training Basic principles to follow in most individuals • Intensity – 85% Max HR is a target in normal individuals – 60% Max HR is a target in diseased individuals • Duration – 20 -30 minutes of aerobic exercise • Frequency – 3 to 5 times/week • Specificity – Should be task specific (i. e. do walking to improve walking, stairs to improve stair climbing)
Effects of Aerobic Training • Increased – Aerobic Capacity – Cardiac Output – Stroke Volume • Decreased – Heart Rate – Myocardial Oxygen Consumption
Benefits of Aerobic Training • • Angina decreases Reversal of lesions Blood pressure decreases Exercise tolerance increases Decreased depression/anxiety Resting heart rate decreases Improved quality of life
Question 2: • For patients with coronary disease, aerobic training does all of the following except: – A. lower blood pressure – B. increase peripheral resistance – C. lower cholesterol – D. improve exercise tolerance – E. decrease resting heart rate
Classical Rehabilitation Post MI • Classical program designed by Wenger – Historically important, as a radical new approach in the 1970’s, no longer used – 14 day in hospital program after acute infarction – Current in hospital programs shorter - 3 -5 days • Overall program divided into four phases – Acute - I – Convalescent - II – Training - III – Maintenance - IV
Wenger Classical Program of Cardiac Rehabilitation • Phase I – Acute phase - 14 days in hospital form bed to about 4 -5 MET’s activity • Phase II – Convalescent phase - 5 -6 weeks (to allowe infarct healing to prevent myocardial rupture) • Phase III – Training phase - program for 3 times a week for 12 weeks, total of 36 sessions • Phase IV – Maintenance phase – patient to be on a self directed exercise program.

Current Cardiac Rehab Schema • Since revascularization and better acute heart attack care, convalescence is usually no longer needed. So now 3 phase approach in most cases • Overall program divided into three phases – Phase 1: Acute - 2 -3 days in hospital, up to 4 -5 METs – (one to two flights of stairs) – Phase 2: Training - classical outpatient 36 sessions of cardiac rehab over 12 weeks – Phase 3: Maintenance – Home and/or center based maintenance exercise program
Phase 1: Acute • Begins in coronary care unit (Coronary Care Unit) • Early Mobilization – CCU to 2 flights of stairs in 2 -3 days • Telemetry monitoring at each stage of increased activity, can avoid telemetry if stable at a given level of activity • Begin patient education at this time – This is a “teachable moment” • Ends at discharge from hospital • Low level stress test prior to discharge
Newer Views on Acute Cardiac Rehabilitation (Phase 1) • Patients now often have procedures post MI – Ischemia is “fixed” => can be more vigorous • Multiple co-morbidities may exist => PVD, etc. • Survivors of major events with severe debility – Long ICU stays – Critical illness complications – Severe CHF/low EF • Phase 1 may be prolonged in these settings – New concept of prolonged institutional phase 1 rehabilitation: Phase 1 B Rehabilitation
Phase 1 B Cardiac Rehabilitation • Continued Inpatient hospitalization for rehab • Can be in an Acute (hospital) or subacute (rehabilitation facility) setting • Usually in patients with advanced needs – Pateints with complicated courses, advanced age, multiple co-morbidities, stroke, etc. • Goals – Safe independent function at home – Achieve 4 -5 MET safe exercise tolerance – Preparation for Phase 2 rehab program
Medical Indications for Phase 1 B Cardiac Rehabilitation • Comorbidity – Stroke – either preceding or from the cardiac event – Amputation/Vascular Disease – Advanced Age – Severe Deconditioning • Prolonged ICU Stay and Recovery • Inability to Progress to Ambulation • Infection or other complications
Medical Indications for Phase 1 B Cardiac Rehabilitation • Complex Patient Populations – Post Transplantation – Complex Cardiac Surgical Patients • Severe Heart Failure, decompensation – Start Phase 1 B when on Stable Regimen • Severe Cardiac Arrhythmias – Only after adequate control is achieved – After automatic internal cardiac defibrillator (AICD) or medical management
Prescription Writing for Phase 1 B Cardiac Rehabilitation • Standard Prescription Rules Apply – Diagnosis – include cardiac and other issues – Precautions – Heart rate, Blood pressure, and other parameters – Goals – Intensity and duration of exercises – Exercises • Aerobic Conditioning • Strengthening of Upper and Lower Extremities • Stretching Program – Monitoring Guidelines – need for telemetry, pulse oximetry, other issues
Goals for Phase 1 B Cardiac Rehabilitation • • Improve Function Improve Fitness Improve Exercise response Improve Self-Image Return to Normal Activities Decrease Morbidity Prevent Complications Education about cardiac disease and risk factor modification • Lifestyle modification to start
Overview of Phase 1 B Programs • Can Safely Establish a Phase 1 B Program in Existing Rehabilitation Facilities • Coordinate in a Multidisciplinary Approach • Basic Principles of Rehabilitation Apply • Must have Close Monitoring and Tightly Written Exercise Prescriptions • Rehabilitation Approach can Treat Multiple Comorbidities in Comprehensive Way • Allows treatment of patients with both cardiac and physical disabilities.
End of Phase 1 and 1 B: Discharge • Maintain early mobilization – Gradually increase endurance • Maximum heart rate as previously determined by low level ETT (can be 6 minute walk test, stair climb test, shuttle walk test) • In Classic Program (phase II) a six week program to allow for scar formation – Now only after cardiac surgery with a sternotomy (allows for healing) – Exercise 3 -5 times per week at 4 -5 METs maximum – 20 -30 minute sessions at target HR set by d/c ETT – 5 minute warm up/cool down sessions
Phase 2: Training • Classical Program (phase III) 6 weeks post MI, full level ETT performed – Screen out arrhythmias, ischemia – Set target heart rate • With revascularization, start as soon as possible • Monitoring with each increase in level • Patient self monitoring taught – Borg Scale – Heart rate • Education is critical her – Lifestyle modification – Disease specific teaching (Diabetes, hypertension) – Medication education
Phase 2: Training • Usual program as outpatient – 3 sessions a week minimum – Minimum 6 -8 weeks in duration, can be longer – Up to 4 hours per session – Cross training (use treadmill, cycle, stair climber) – Always start with a 5 minute warm up/cool down – 20 -30 minutes on each piece of apparatus – Include a strengthening program • low weight (<50% one repetition maximum) • high repetition (3 sets of ten with a few minutes between sets)
Phase 3: Maintenance • Most important phase • Benefits of training can be lost in a few weeks of being sedentary • Regular exercise necessary – Minimum of 2 to 3 times a week – At least 30 minutes of exercise per session excluding warm up and cool down – Alternate with strengthening sessions – Role for maintenance/wellness program
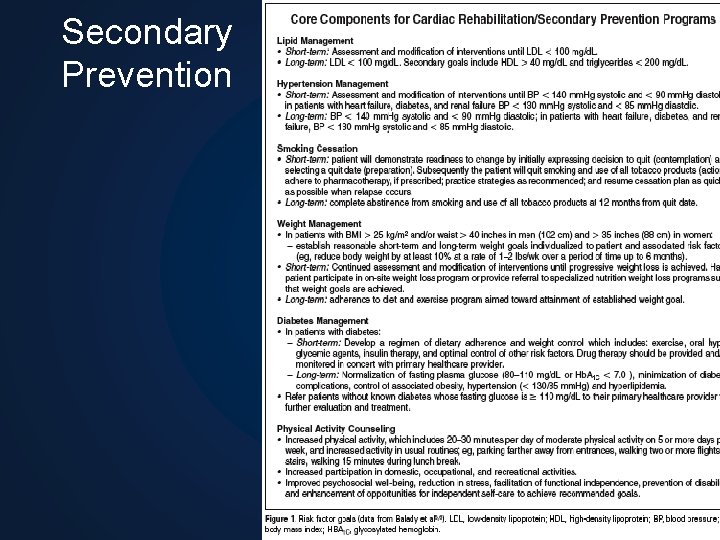
Secondary prevention goals in CR • Tobacco cessation – this is critical!!! • BP - <140/90 mm. Hg or <130/80 in DM or renal disease • Lipid control: LDL-C <100 mg/Dl for TG >200, non HDL-C <130 mg/Dl. These targets are being modified so need to keep up with recent guidelines • Physical activity 30+ minutes for at least 5 days a week • Stress relief: Relaxation techniques
Secondary Prevention Goals in CR • Weight management: BMI 18. 5 to 24. 9 – and waist <40 in men and <35 in women • DM: Hgb. A 1 c <7% • Depression/anxiety: Evaluate for depression/anxiety – If present => treat • Exercise capacity: Assess with ETT if possible – Develop individual training program • Encourage healthy lifestyle and lifestyle choices
Secondary Prevention Goals in CR • Medications: Assess current medications – Assure beta blockade – Assure antiplatelet agent – Assure cholesterol lowering agent – Assess BP control medications • Assess medication adherence and knowledge • Assess ability to manage diabetes – Self monitoring – Dietary and insulin management
Practical Issues • Be more aggressive after revascularization • Patients now with smaller initial MI – Shorter recovery – Revascularized at presentation • CR needs to be available to all post MI patients, only offered to about 10 -20% of patients – Need to refer patients – CR more effective than any single medication intervention in lowering morbidity and mortality • Limitations of access and referral need to be addressed.
Question 3: • A primary goal of Secondary Prevention in cardiac rehabilitation includes: – A. Financial counseling – B. Weight management – C. Arthritis management – D. Breathing control – E. Postural control
Basic Needs for Outpatient Services • Ideally a physician supervised program with trained physical therapists, nurses, exercise physiologists providing care • Consider cardiac rehabilitation in: – Post Myocardial Infarction – Post bypass surgery, Post Valve surgery – Stable Angina – Heart failure – Post transplant – Stable arrhythmias
Elements in an Outpatient Program • Medical supervision – Can be internist, rehabilitation physician, cardiologist • Trained staff – Exercise physiologists, nurse, physical therapists – Training available with the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR) • Mixed strength/endurance/flexibility training • Education components must be present – – Nutritional counseling, medication management Smoking cessation Support groups Maintenance support
Secondary Prevention
Basic Observations on Exercise If exercise was a medication, it would be the highest selling pharmaceutical of all time However, since exercise is work, it is grossly underutilized for almost every condition for which it would be appropriate
Rehabilitation in Special Situations • Angina Pectoris – Begin once medical management optional – Includes training and maintenance phases – Exercise at just below anginal threshold (heart rate) • Cardiac arrhythmias – Use limits set by ETT, continuous telemetry – Proceed normally in patients with AICD • Avoid AICD firing rate with stress testing and exercise program (keep heart rate at least 10 beats per minute below AICD ventricular tachycardia firing rate with exertion)
Rehabilitation After Bypass Surgery • Immediate post operative period – Mobilize starting POD #1 – Progressive mobilization POD 2 -5 – Discharge planning and exercise prescription • Consider a symptom limited ETT 3 to 4 weeks post surgery, should exercise at 4 -5 METs until rehab starts • For sternotomy patients, no upper limb exercise over 10 pounds until sternum healed (bone healing time) • Phase 2 as in Post MI patients • Maintenance Phase is essential to prevent recurrence – Three types of programs • Low, moderate, high intensity
Cardiomyopathy and Heart Failure: Physiology • Patients with ejection fraction < 30% • Multiple medical problems – High risk of sudden death – Deconditioned – Depressed – Low endurance – Fatigue • Still can have marked benefits with cardiac rehabilitation.
Cardiomyopathy and HF: Physiology • Altered physiology in Heart Failure • Lack of normal response to exercise – Possible decrease in ejection fraction with increased afterload, possible decrease in stroke volume and blood pressure – Cardiac output may not increase sufficiently to generate a dynamic exercise response – Can have prolonged fatigue post exertion – May be more prone to arrhythmias
Heart Failure: Benefits of Rehabilitation • Unlike Classic rehabilitation, little effect on the heart muscle, does not usually increase stroke volume • Most improvements are peripheral changes that allow for better exercise tolerance – Increased peripheral oxygen extraction • Improved oxygen carrying capacity • Better release of oxygen by red blood cells – Lower heart rate at submaximal exercise – Lower systemic vascular resistance – Increased maximum workload – Can improve New York Heart Association functional level by one level
Question 4: • For patients with Heart Failure, the chance of sudden death is less than patients with angina or ischemic heart disease. – A. True – B. False
Heart Failure: Rehabilitation Program Specifics • Prolonged warm ups and cool downs – Improves safety, allows for accommodation to exercise, prevents rapid blood pressure changes • Dynamic exercise preferred over isometrics – Prevents increased afterload • Target heart rate 10 bpm below any significant endpoint • Start and advance under close supervision • Continuous telemetry for severe left ventricular dysfunction

Rehabilitation in Heart Failure • Graded exercise tolerance test for all patients before starting exercise program is suggested – Rule out arrhythmias, angina, or atypical exercise response – Establish safe guidelines for heart rate, blood pressure and level of exercise. • Contraindications to cardiac rehabilitation in HF – Unstable angina – Decompensated HF – Unstable arrhythmias
Rehabilitation in Valvular Heart Disease • Treat patients with valve disease as those patients in heart failure • In presence of anticoagulation use low impact exercises • Critical Aortic Stenosis (AS) is the only contraindicated condition. – Severe AS is allowed, but needs exercise test to assure safety. • After valve replacement surgery – Program is similar to post bypass surgery patient – Training can increase work capacity by up to 60%, rate pressure product by up to 15%
Scope of Issue of Dual Disability in Cardiac Rehabilitation • Most common comorbidities are in “vasculopaths” and come with aging • Orthopedic limitations are extremely common – Lower limb arthritis and back pain • Vascular disease travels in common - so CAD often seen with stroke and PVD
Cardiac Disease in Patients with Primary Disability • Spinal cord injury: – Primary cause of death is now cardiac disease. – There is an accelerated rate of development of CAD (more and earlier than normal controls). – Exercise can case improvements • But peak exercise levels are not equal to normal
Cardiac Disease in Patients with Primary Disability • Amputee/PVD: – Serious co-existence of disease – Many issues in common with CAD • Stroke/Neurological Disease – Common to see stroke and CAD – Benefits of treatment extend to stroke as well as the CAD
Coincidence of Coronary and Peripheral Vascular Disease • • High correlation of CAD with PVD affects up to 5% of patients age < 50 years PVD affects over 20% of patients age >70 years PVD common in patients undergoing bypass surgery • Need to control rate, best would be cardioversion - needs telemetry only if in paroxysmal a-fib or rate control an issue • Normal HR/BP limits • No pulse oximetry • Most like a stroke with no Cardiac Issues.
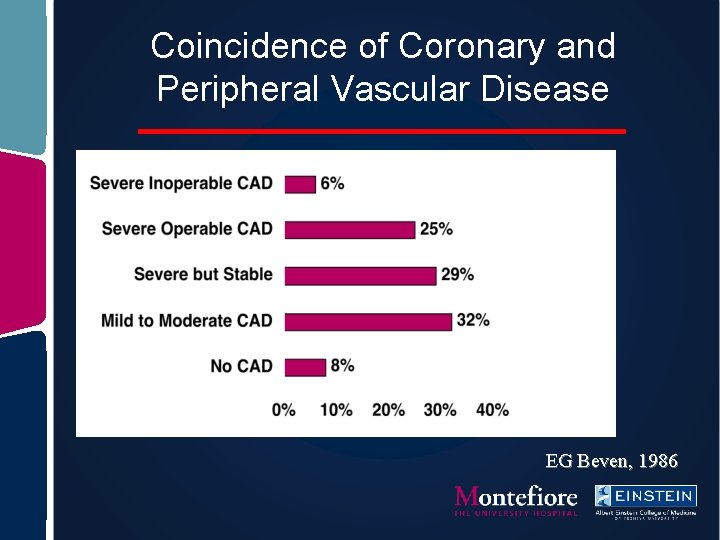
Coincidence of Coronary and Peripheral Vascular Disease EG Beven, 1986
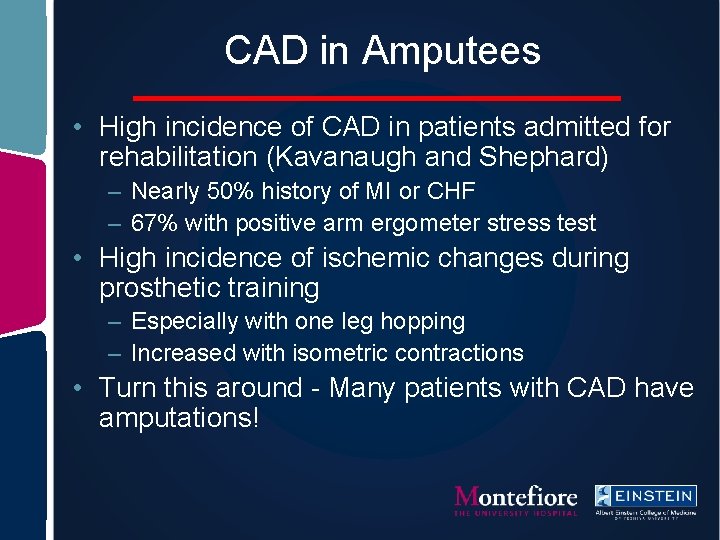
CAD in Amputees • High incidence of CAD in patients admitted for rehabilitation (Kavanaugh and Shephard) – Nearly 50% history of MI or CHF – 67% with positive arm ergometer stress test • High incidence of ischemic changes during prosthetic training – Especially with one leg hopping – Increased with isometric contractions • Turn this around - Many patients with CAD have amputations!

Risk Factors for PVD • Risk factors overlap with Coronary Disease – Smoking is the major risk factor – Hypertriglyceridemia – Diabetes Mellitus – Elevated cholesterol – Treatment is similar • Similar secondary prevention • Similar benefits with exercise conditioning
Exercise Prescription for Amputees with CAD • Upper extremity ergometry testing useful • Protocols and testing are established – Exercise induced ECG changes at <50 watts positive (Kavanaugh, Cruts, Davidoff, others) – Chest pain often not present during testing – Arm/general fatigue most common symptom – Can determine maximum safe heart rates – Can determine general exercise guidelines
Exercise Training in PVD • Guidelines published by the American College of Sports Medicine – 20 -30 minutes of interval exercise – Increase to 40 -60 minutes over 4 to 6 weeks – Maximum heart rate as determined by exercise testing – Airdyne arm-leg ergometry, arm ergometry, water aerobic exercises are alternative exercises • Full program through the American Association of Cardiovascular and Pulmonary Rehabilitation.
Exercise Training in Patients with Leg Amputation • Aerobic conditioning does occur • Arm ergometry protocols exist – Exercise with three minute stages – Begin at 5 watts resistance, increase by 5 watts per stage – Exercise occurs at 50 -70% maximum – Goal is 15 minutes of exercise at target – 5 minute warm up/cool down periods
Home Exercise Programs in PVD • Patients can monitor exertion at home – Use rating of perceived exertion through the Borg scale – Can do self pulse monitoring – Ambulation exercises can be used in patients after amputation in those who are proficient prosthetic ambulators
Cardiac Assessment in PVD • Standard treadmill and bicycle stress testing not possible if claudication limiting • Upper extremity ergometry possible • Risk stratification can be done with pharmacologic stress testing • Cardiac catheterization in patients at high risk or with positive stress test
Question 5: • It is uncommon to see patients with ischemic heart disease and stroke or peripheral vascular disease. – A. True – B. False
Outcomes of Exercise in PVD • Studies demonstrate – Average increase in pain free walking distance of 134% , range from 44 -290% – Average increase in peak walking time of 96%, range from 25 -183% – Graded treadmill exercises show increases in maximum oxygen consumption and maximum exercise performance
Effect of Cardiac Rehabilitation in Amputees • Increased energy costs of ambulation are well documented • The presence of cardiac disease in amputation decreases the likelihood of independent gait • Patients demonstrate increased work capacity and peak oxygen consumption after cardiac rehabilitation
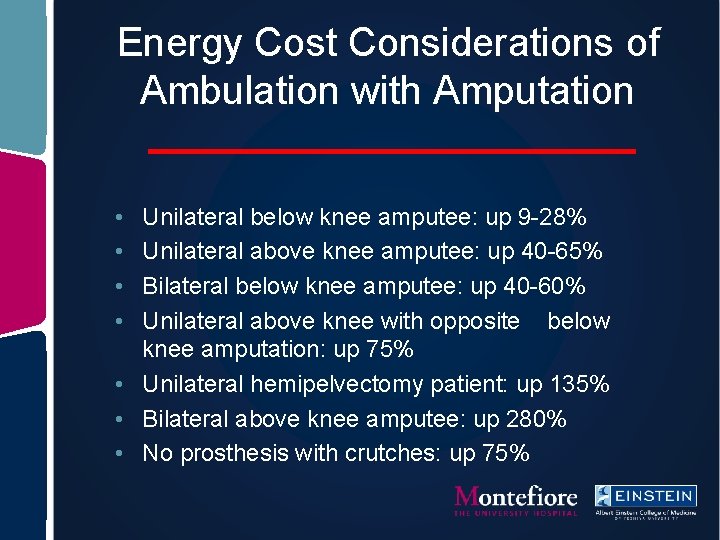
Energy Cost Considerations of Ambulation with Amputation • • Unilateral below knee amputee: up 9 -28% Unilateral above knee amputee: up 40 -65% Bilateral below knee amputee: up 40 -60% Unilateral above knee with opposite below knee amputation: up 75% • Unilateral hemipelvectomy patient: up 135% • Bilateral above knee amputee: up 280% • No prosthesis with crutches: up 75%
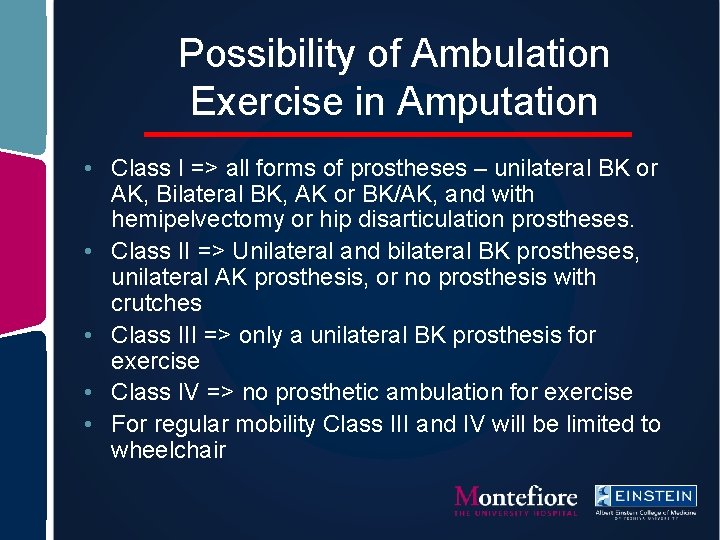
Possibility of Ambulation Exercise in Amputation • Class I => all forms of prostheses – unilateral BK or AK, Bilateral BK, AK or BK/AK, and with hemipelvectomy or hip disarticulation prostheses. • Class II => Unilateral and bilateral BK prostheses, unilateral AK prosthesis, or no prosthesis with crutches • Class III => only a unilateral BK prosthesis for exercise • Class IV => no prosthetic ambulation for exercise • For regular mobility Class III and IV will be limited to wheelchair
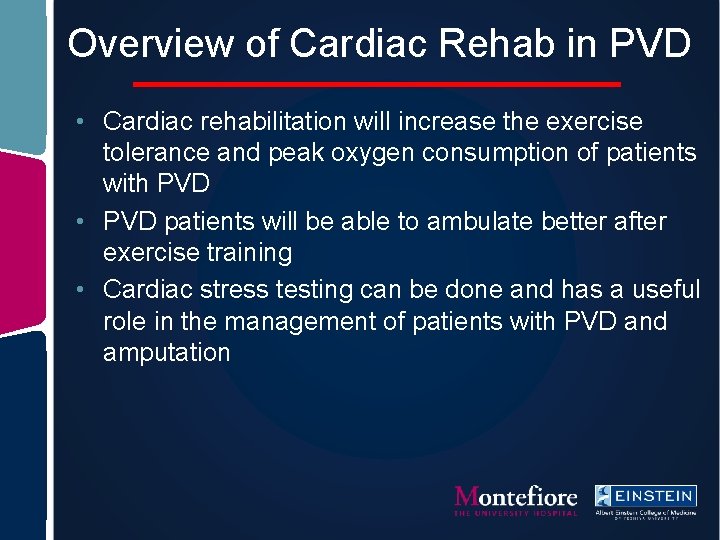
Overview of Cardiac Rehab in PVD • Cardiac rehabilitation will increase the exercise tolerance and peak oxygen consumption of patients with PVD • PVD patients will be able to ambulate better after exercise training • Cardiac stress testing can be done and has a useful role in the management of patients with PVD and amputation
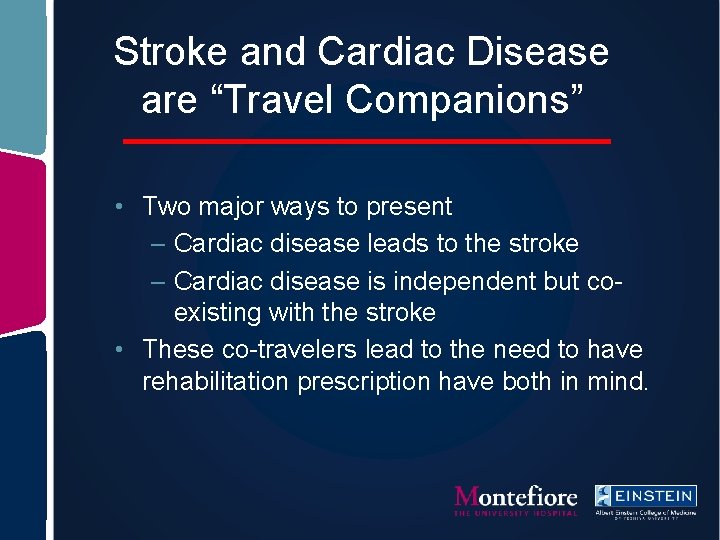
Stroke and Cardiac Disease are “Travel Companions” • Two major ways to present – Cardiac disease leads to the stroke – Cardiac disease is independent but coexisting with the stroke • These co-travelers lead to the need to have rehabilitation prescription have both in mind.
Basic Facts About Co-existence of Cardiac Disease and Stroke • 20 -30% of stroke is due to cardiac disease • Atherosclerosis affects both organ systems equally – Cardiac plaque rupture more common – Cerebral blockage more common Kaps M, et. al. Heart and Brain. 73: 698 -710
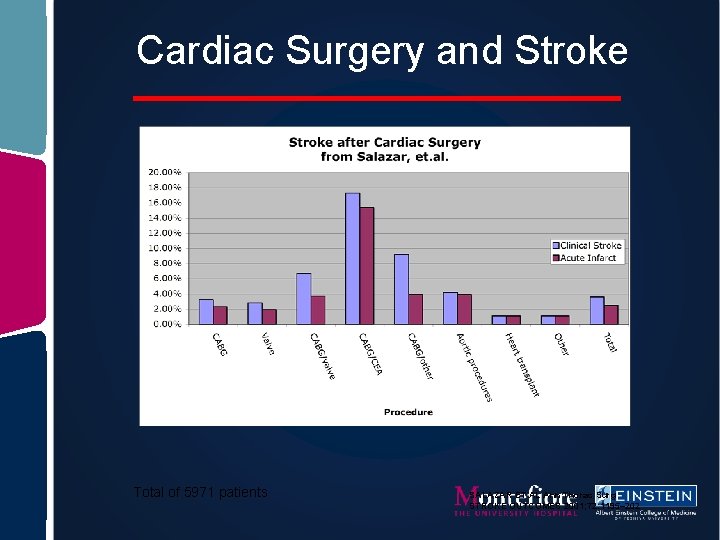
Cardiac Surgery and Stroke Total of 5971 patients SALAZAR ET AL Ann Thorac Surg STROKE OUTCOMES 2001; 72: 1195– 202
Risk Factor Modification Programs Similar for PVD, Stroke, Amputee • • Hypertension Hypercholesterolemia Stress reduction Diabetic management Increased activity Dietary modification Education
Exercise Modifications - Stroke • Exercise in stroke and cardiac disease: – – Leg ergometry Arm ergometry Strengthening Ambulation on a flat surface - if able • Modifications of ambulation with Stroke – Remember: with orthosis and assistive device: • Gait speed decreases 40 -45% • Energy cost of ambulation is 50 -65% higher.
Exercise Modifications - SCI • Multiple changes in physiology – Loss of muscle pump action – less pre load – Hypertension is common in older patients with longer standing SCI – Hypotension on postural change – Decreased vascular distensibility – Often with other morbidity • Renal failure • Depression • Sedentary
Exercise Modifications - SCI • Preferred exercises in SCI and cardiac disease: – Arm ergometry – Wheelchair ergometry – Hybrid arm exercise and functional electrical stimulation for legs
Exercise Modification: Orthopedic Limitations • Certain precautions apply: – Avoid impact exercises – Gliding or seated exercise better • Ergometry is usually well tolerated • Consider recumbent cycle for back pain – treadmill and upright cycle ergometry often painful. • Stair steppers can also be tolerated for back and large joint arthritis – Large joint arthritis and Back Pain • Pre-medicate with pain medication • Avoid extremes of the range of motion • Rhythmic motion better
Orthopedic Limitations • Coordinate care with physicians who are caring for the underlying musculoskeletal diseases. • Learn which precautions apply • Examples: – Avoid back extension in spinal stenosis – Avoid back flexion in lumbar disc disease – Avoid axial loading in osteoporosis
Conclusions • Cardiac rehabilitation can be done in all types of patients who have co-existing cardiac disease. • Modifications for Stroke, Orthopedic, and Neurologic limitations can be easily incorporated. • Do not exclude patients with other disabilities as they have significant benefits and can be enrolled with relatively minor modifications.
Sample Case #1 - Amputation • 65 year old Diabetic man admitted for PVD – Stable operative course for below knee amputation after failed femoral bypass surgery – POD #1 extubation, noted to have altered hemodynamics – ECG changes c/w MI, Echo with EF 35% – Cardiac cath reveals 3 vessle disease – High risk CABG done, patient extubated POD #2 – Rehab medicine is called to evaluate the patient
Question 6: • Patients with Stroke and Peripheral vascular disease have similar programs for secondary prevention compared to patients with ischemic cardiac disease. – A. True – B. False
Question 7: • Patients with significant co-morbidities or other disabilities are unable to participate in cardiac rehabilitation. – A. True – B. False
Treatment Options/Cardiac Prescription - Case #1 • Peri-operative MI, now s/p CABG – Post op precautions - Sternal precautions, wound care – Has been revascularized - less fear about ischemia • Telemetry for activity, especially since post MI and with low EF • Supplemental oxygen use helpful – Possible need for anticoagulation in this case, low EF. • If a-fib contributor - then absolutely yes – a-fib transiently seen in up to 40% of post CABG – 60% of post Valve replacement cases. – Heart rate parameters • 60 -65% predicted max, • or use 20 BPM above baseline for Beta blockers
Sample Case #2 - Stroke • 65 year old man admitted for CABG – – – Stable operative course POD #1 extubation, noted to have right hemiparesis Head CT negative for bleed, MRI with new left MCA stroke TCD negative, Echo unrevealing, other w/u negative Cause unclear, possible emboli from aortic plaque, air Rehab medicine is called to evaluate the patient
Treatment Options/Cardiac Issues in Prescription - Case #2 • Peri-operative stroke – Post op precautions - Sternal precautions, wound care – Has been revascularized - less fear about ischemia • Telemetry for new levels of activity • Supplemental oxygen use helpful – No clear need for anticoagulation in this case • If a-fib contributor - then yes – a-fib transiently seen in up to 40% of post CABG – 60% of post Valve replacement cases. – Heart rate parameters • 60 -65% predicted max, • or use 20 BPM for Beta blockers
Sample Case #3 - Stroke • 82 y. o. woman presents with new onset left HP • Evaluation in the emergency room reveals peripheral edema, and hypertension out of control. • Work up shows an internal capsular bleed, with edema on MRI, and Echocardiogram shows a decreased ejection fraction with a probable hypertensive cardiomyopathy. • Rehab medicine is called to evaluate the patient
Treatment Options/Cardiac Issues in Prescription - Case #3 • Hypertensive stroke – Has co-existing cardiomyopathy • Cardiac precautions as in heart failure • Gentle conditioning with close monitoring for arrhythmias and tight blood pressure control • Aggressive heart failure management in addition to her stroke treatment
Sample Case #4 - Stroke • 34 year old homeless man presents with fever and new left hemiparesis • Evaluation shows multiple enhancing lesions on CT. • Echocardiogram demonstrates probable vegetation on the Mitral Valve • Long term antibiotic therapy is started with eventual plan for mitral valve replacement • Rehab medicine is called to evaluate the patient
Treatment Options/Cardiac Issues in Prescription - Case #4 • Mycotic emboli • Valvular heart disease - CHF issues • Will benefit from rehab intervention before MVR as this allows better surgical outcomes. • Staged rehab may be needed - post mitral valve replacement continue stroke rehab. • Precautions differ pre and post valve replacement: sternotomy after valve replacement may limit ambulation training
Sample Case #5 - Stroke • 45 yo woman admitted with new hemiplegia • ER evaluation shows new frontal and occipital strokes, consistent with emboli, new onset atrial-fibrillation • Echo normal, lab tests reveal marked hyperthyroidism • Treatment is initiated, Rehab consult is called.
Treatment Options/Cardiac Issues in Prescription - Case #5 • • Embolic CVA due to a-fib Falls precautions Heart rate monitoring Standard heart rate and blood pressure precautions • Should tolerate all levels of activity
Areas for Investigation • Precise cardiac effect of exercise training – Cardiac parameters – Cardiovascular risk factors – Functional capacity – Incidence of cardiac events • Precise vascular effect of exercise training – Mechanisms of increased ambulation
Areas for Development • Increased availability of cardiac rehabilitation • Increased coordination of in-patient and outpatient services • Improved community education programs • Improved aftercare and compliance with stage 4 rehabilitation (maintenance of exercsi)
Key References (Circulation. 2007; 115: 2675 -2682. )
Key References (Circulation. 2001; 104: 1694 -1740. )
Key References
- Slides: 93