Cardiac output Cardiac output CO is the volume

- Slides: 43
Cardiac output
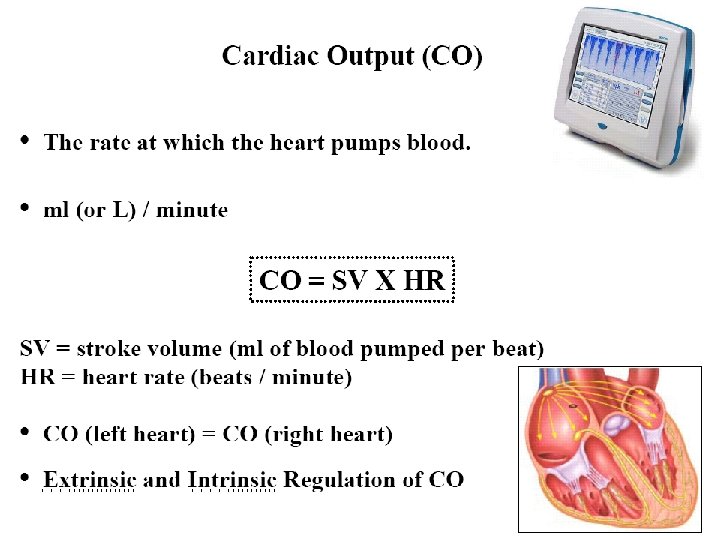
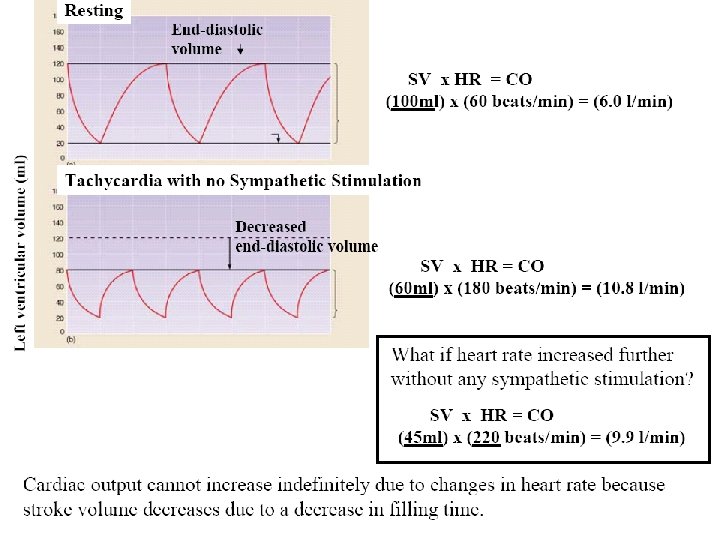
Cardiac output (CO) is the volume of blood being pumped by a ventricle in a minute. Cardiac output is the product of stroke volume and heart rate (CO = HR X SV).
• Cardiac output is equal to the stroke volume (SV) multiplied by the heart rate (HR). • SV is the volume pumped per beat • HR is the number of beats per minute. • Therefore, if there are 70 beats per minute, and 70 ml blood is ejected with each beat, (SV), the cardiac output (CO) is 4900 ml/minute. • This value is typical for an average adult at rest, although CO may reach up to 30 litres/minute during extreme exercise by elite athletes.
Cardiac output typically about 5, 500 milliliters (or 5. 5 liters) per minute (which is about equal to total blood volume; so, each ventricle pumps the equivalent of total blood volume each minute under resting conditions) BUT maximum may be as high as 25 - 35 liters per minute Cardiac reserve: the difference between cardiac output at rest & the maximum volume of blood the heart is capable of pumping per minute permits cardiac output to increase dramatically during periods of physical activity
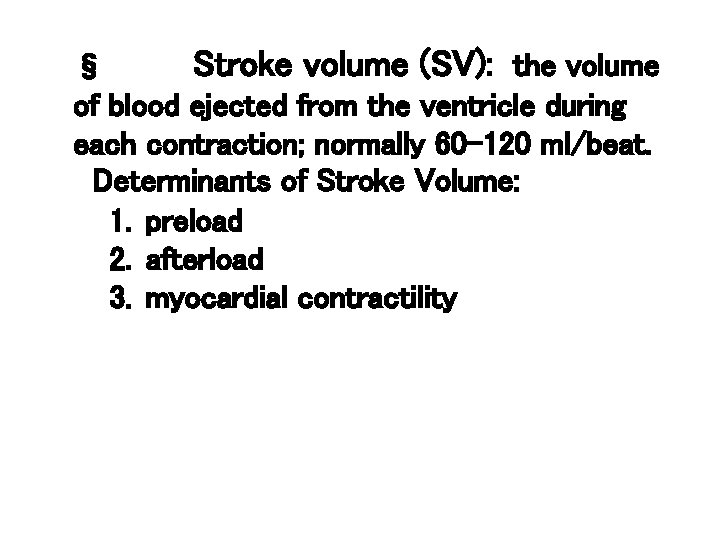
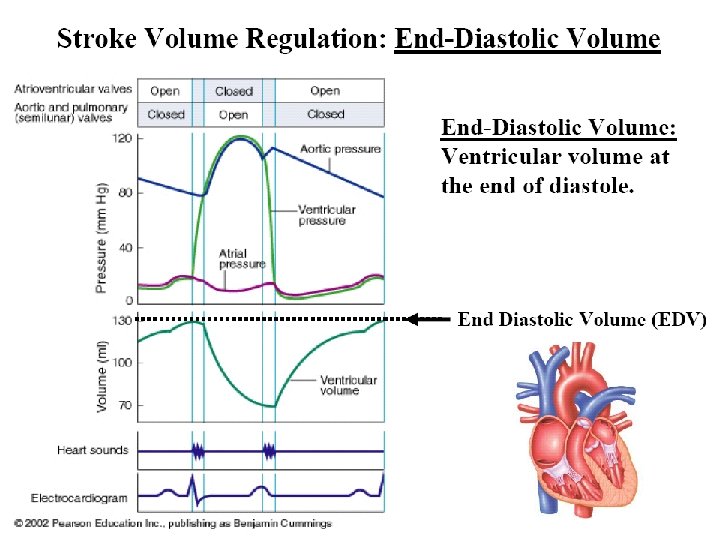
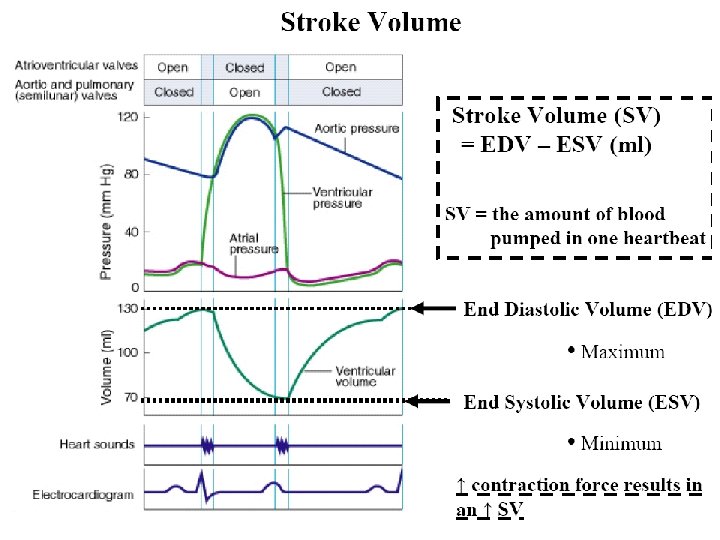
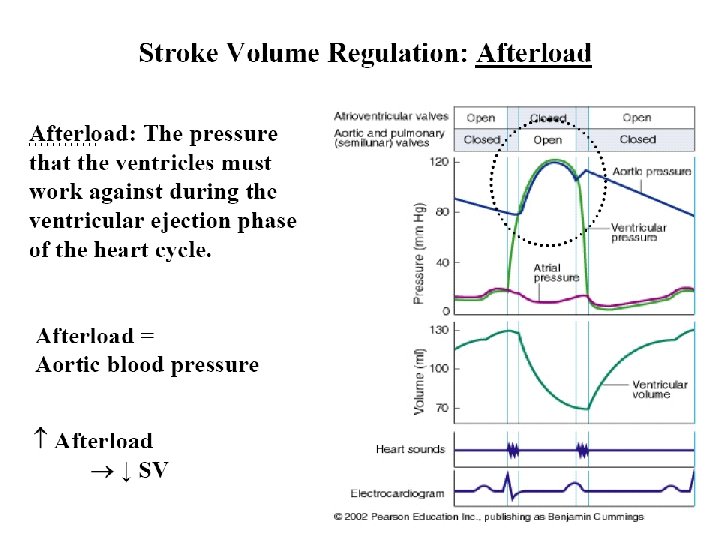
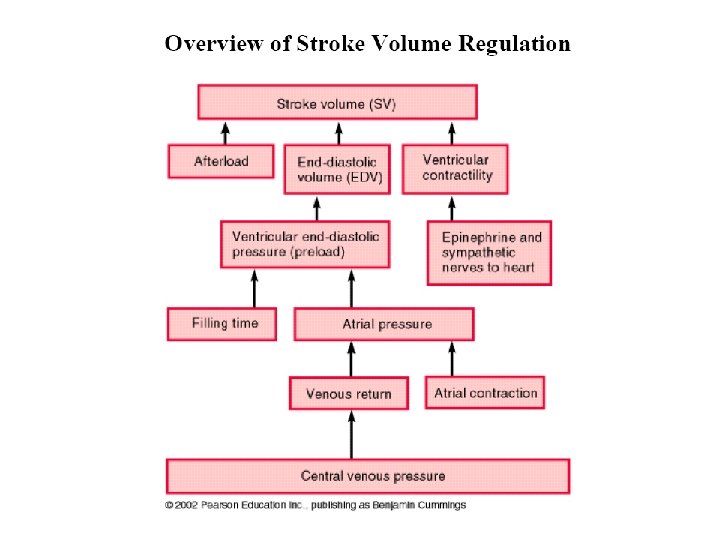
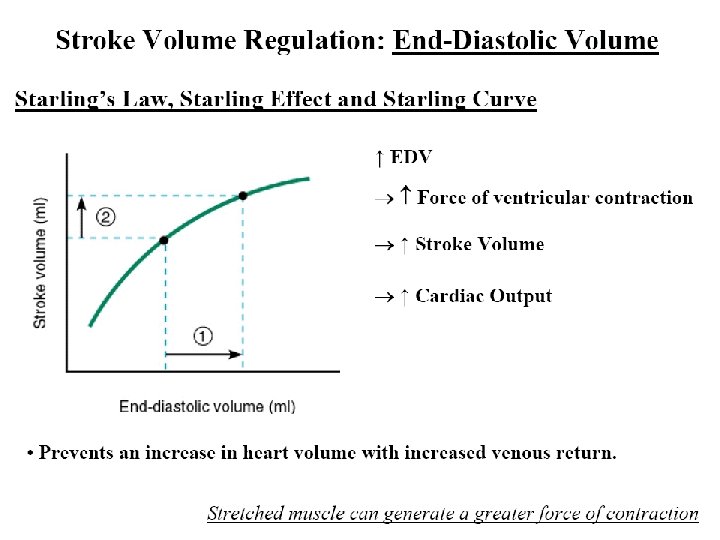
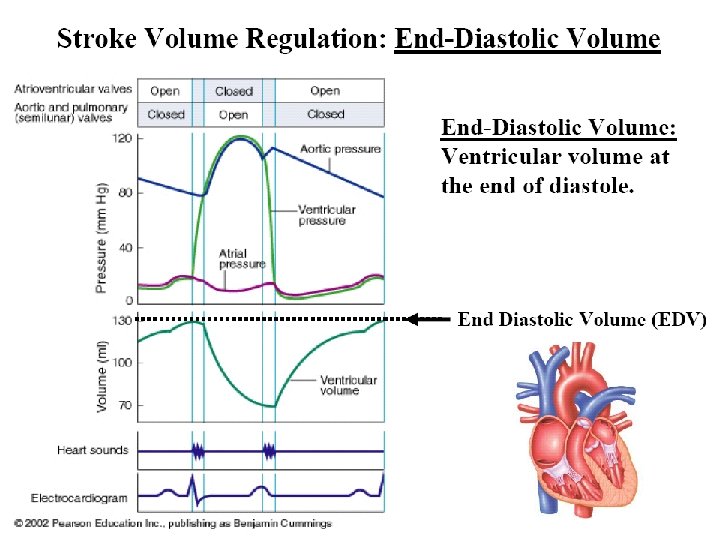
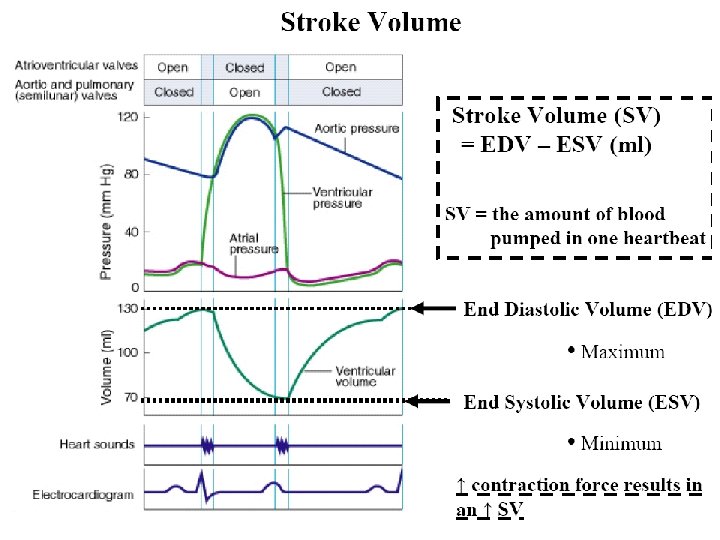
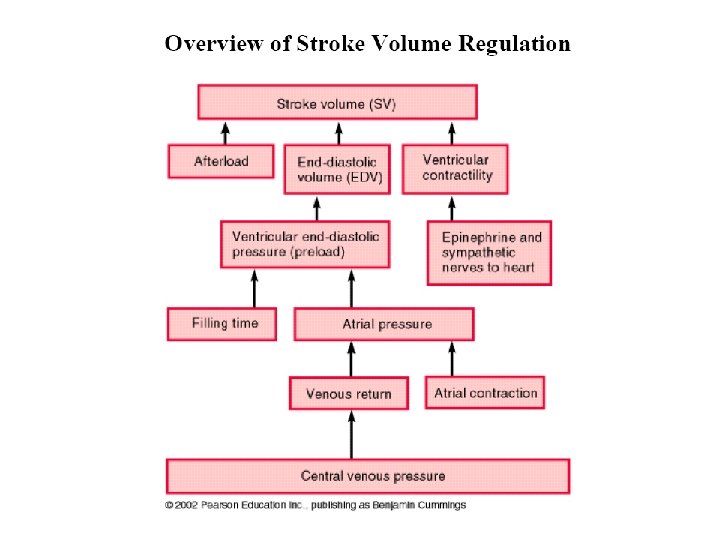
§ Stroke volume (SV): the volume of blood ejected from the ventricle during each contraction; normally 60 -120 ml/beat. Determinants of Stroke Volume: 1. preload 2. afterload 3. myocardial contractility
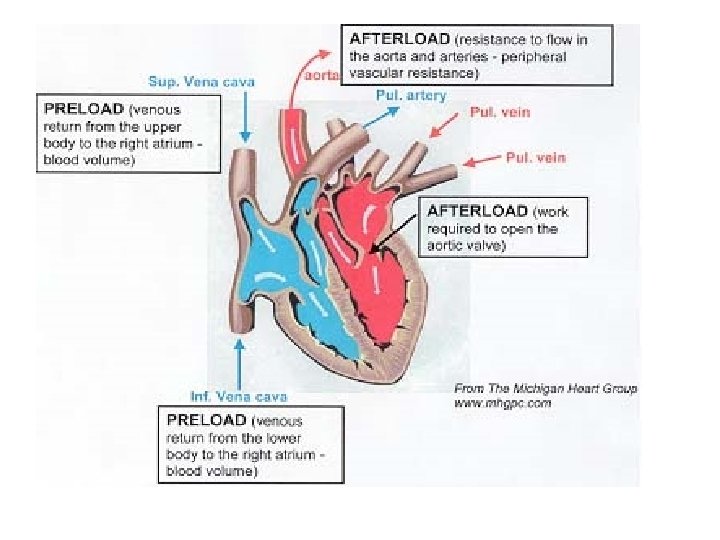
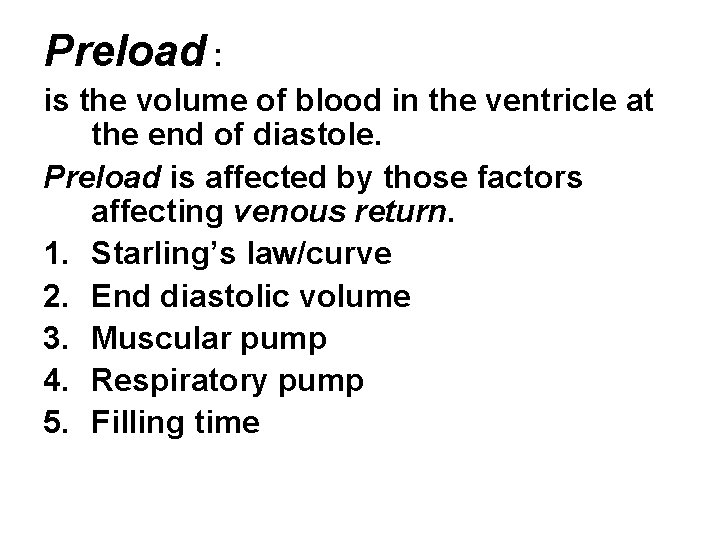
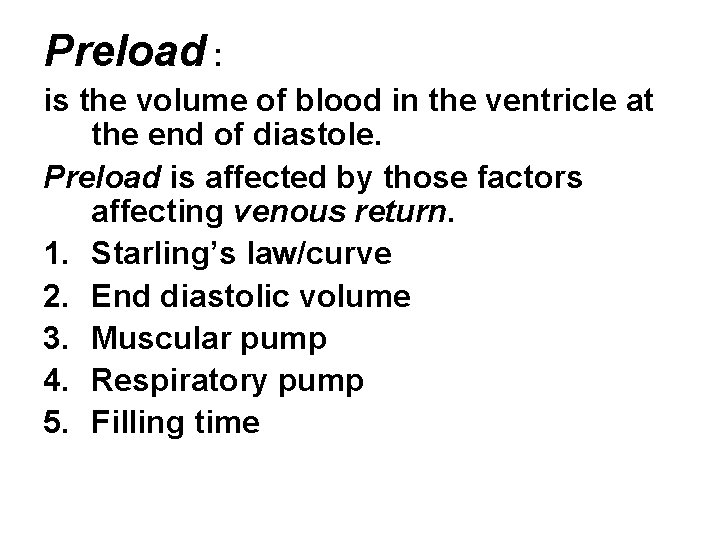
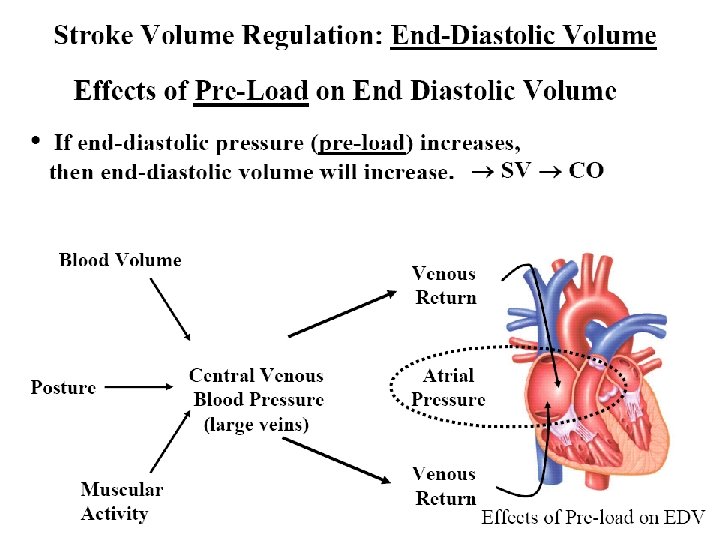
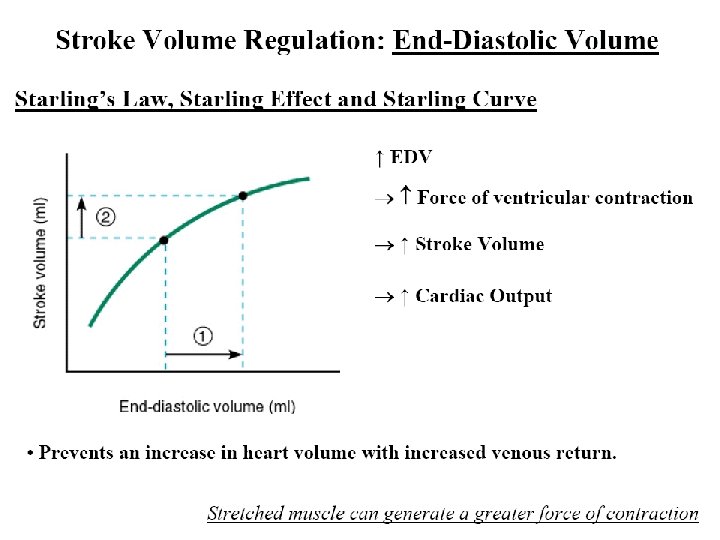
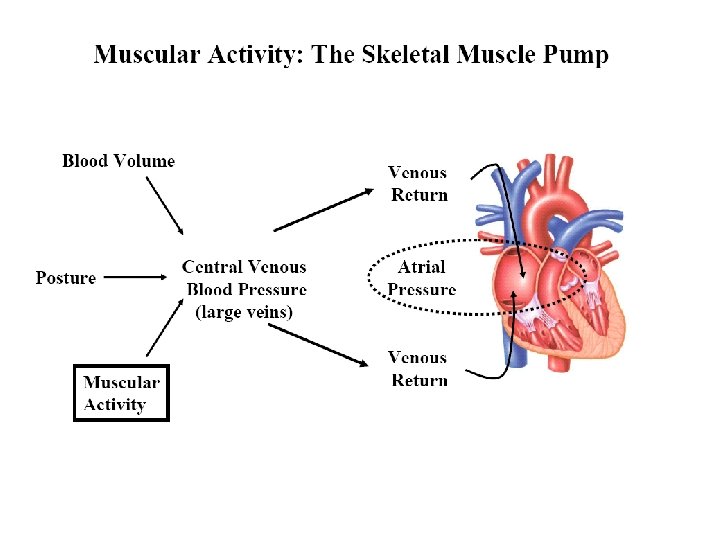
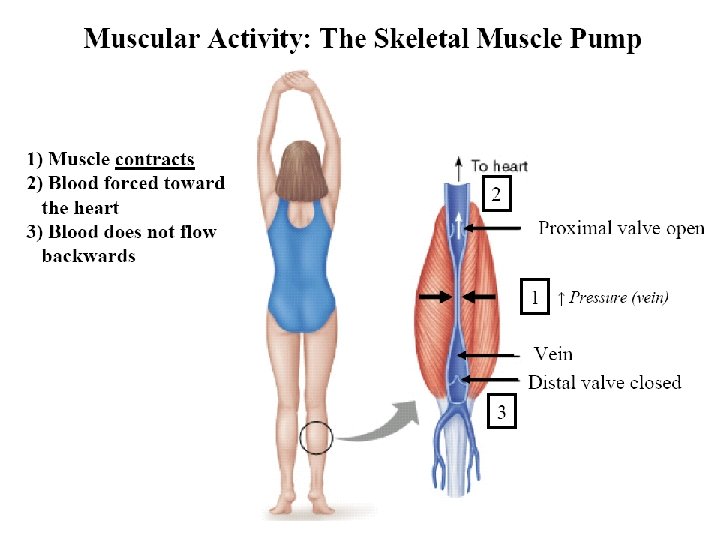
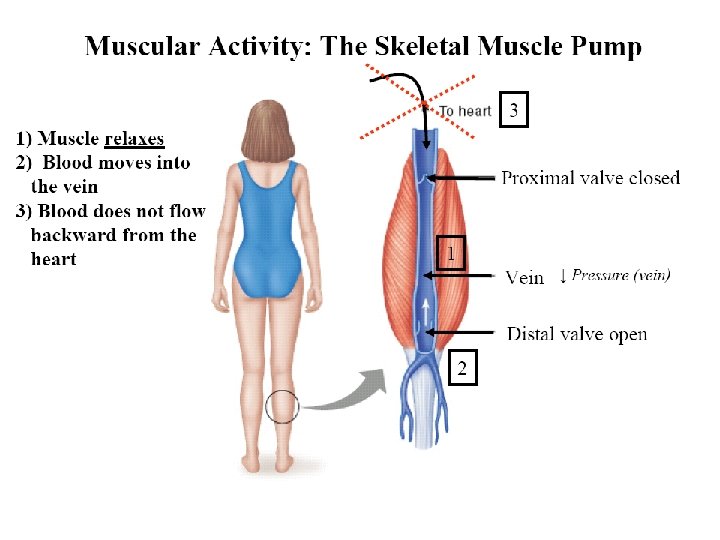
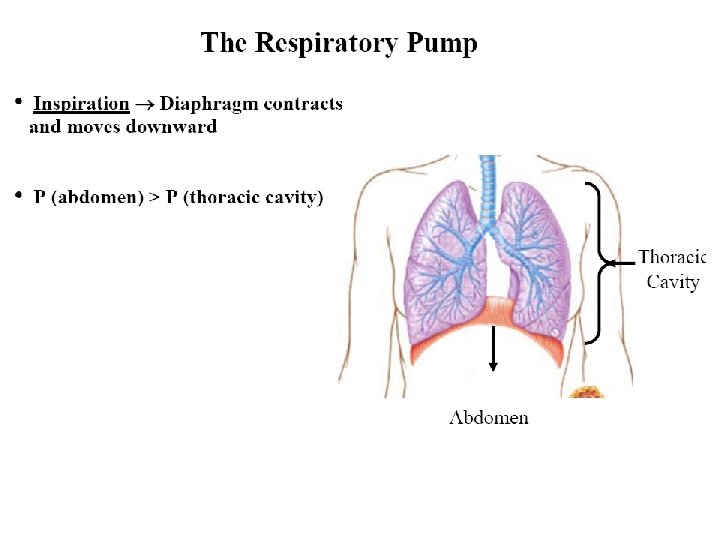
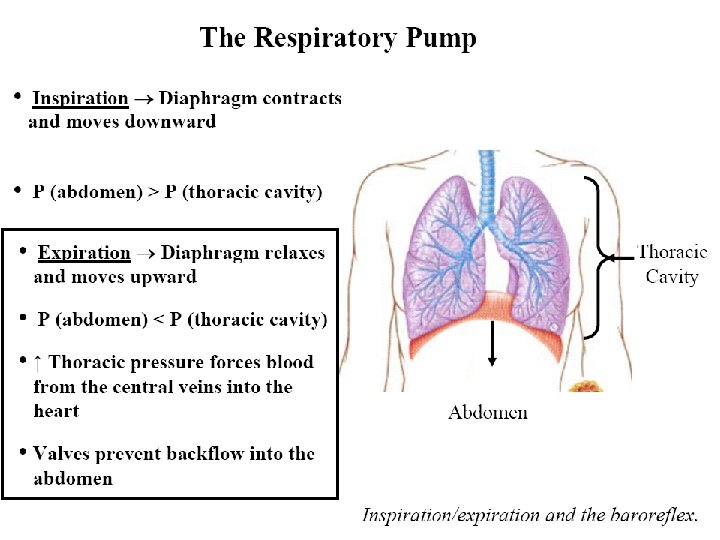
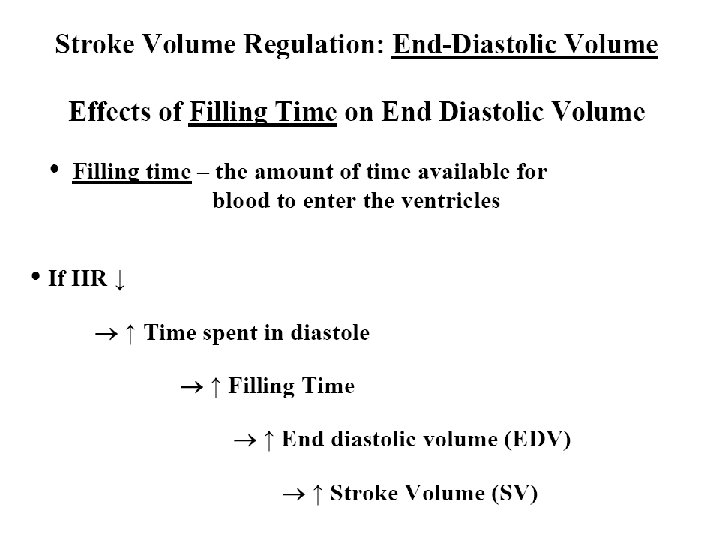
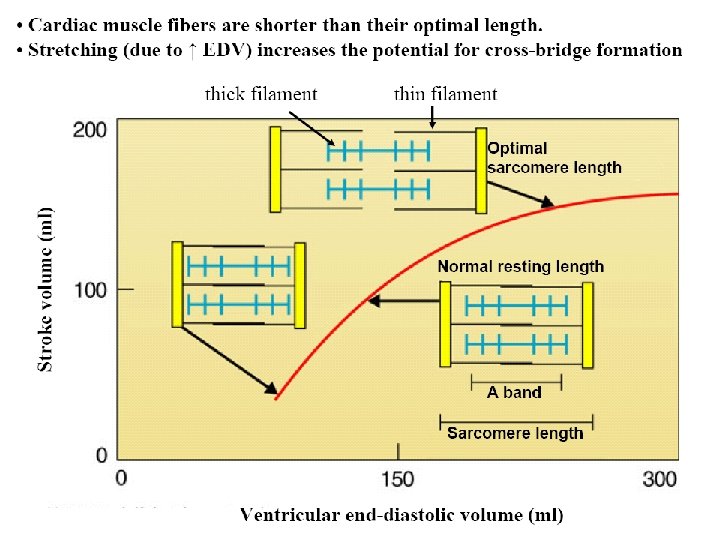
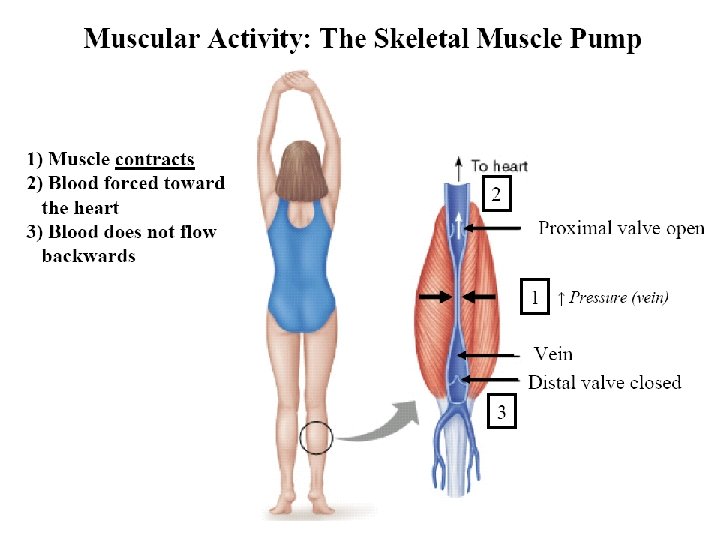
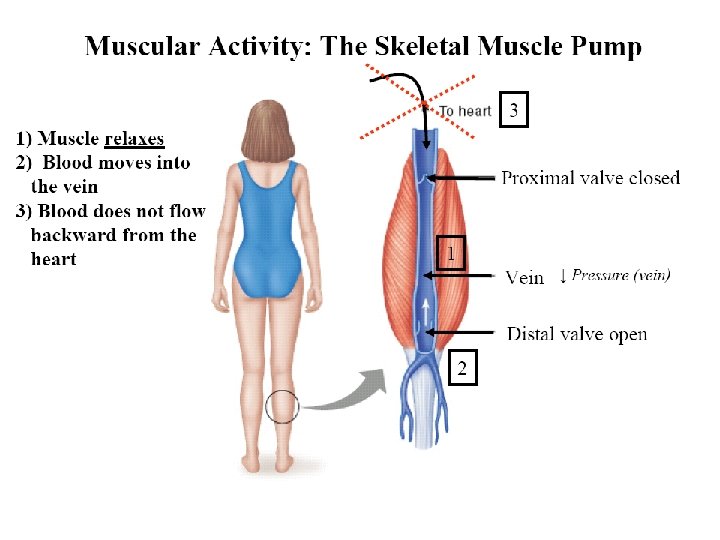
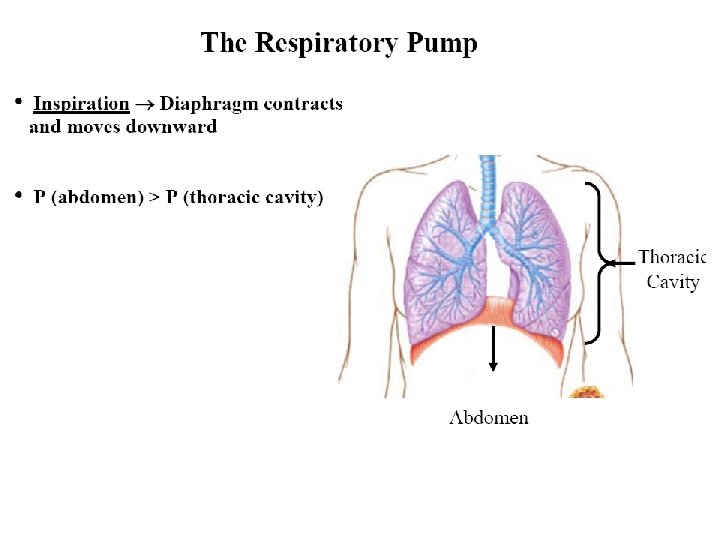
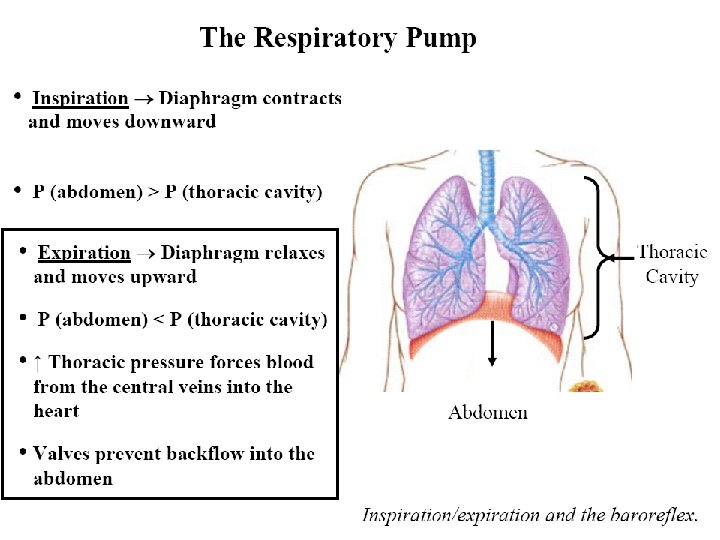
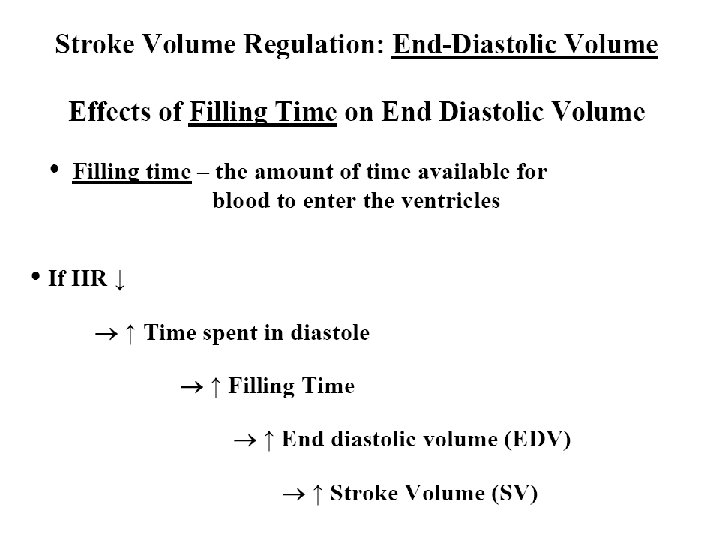
Preload : is the volume of blood in the ventricle at the end of diastole. Preload is affected by those factors affecting venous return. 1. Starling’s law/curve 2. End diastolic volume 3. Muscular pump 4. Respiratory pump 5. Filling time
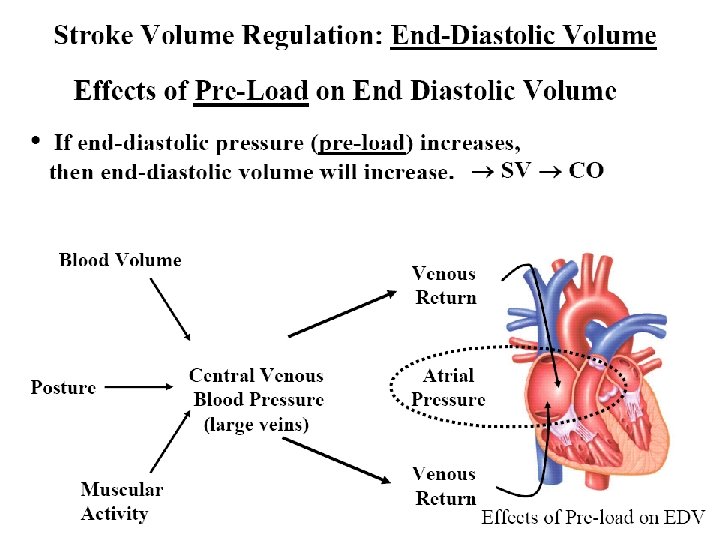
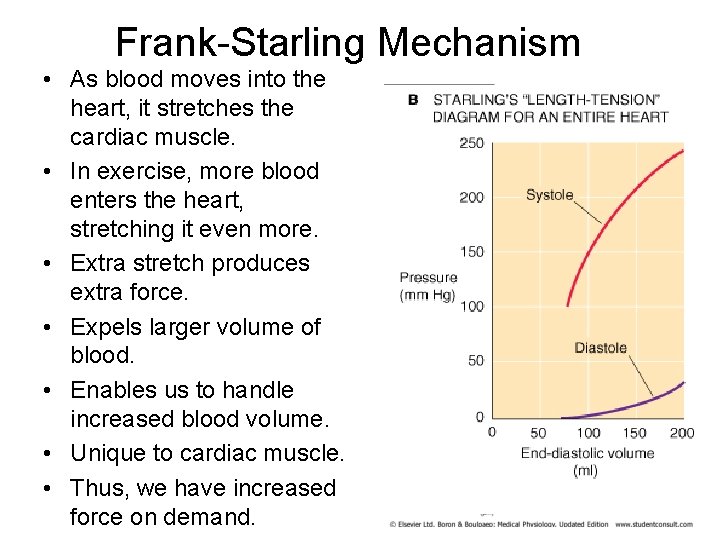
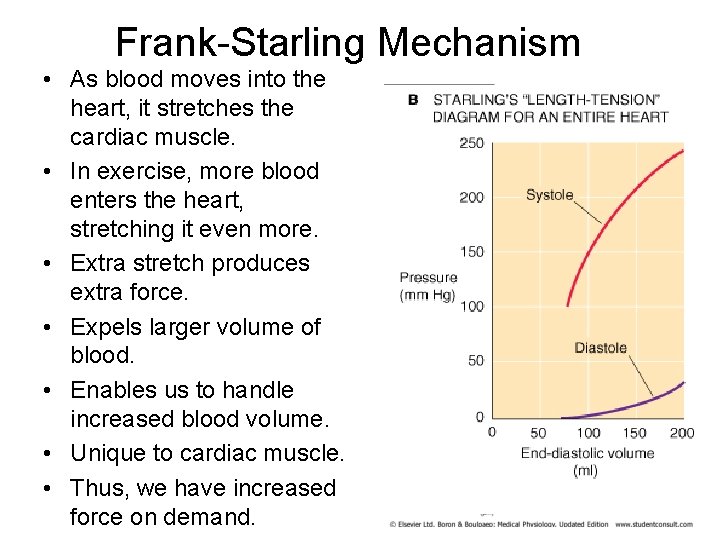
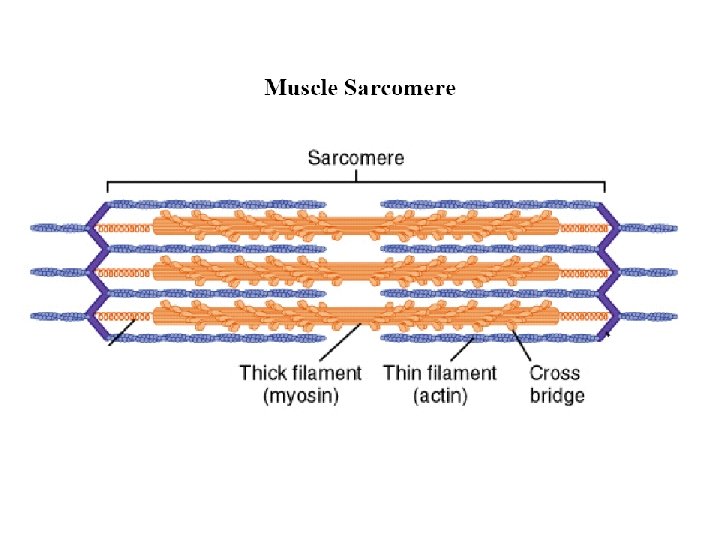
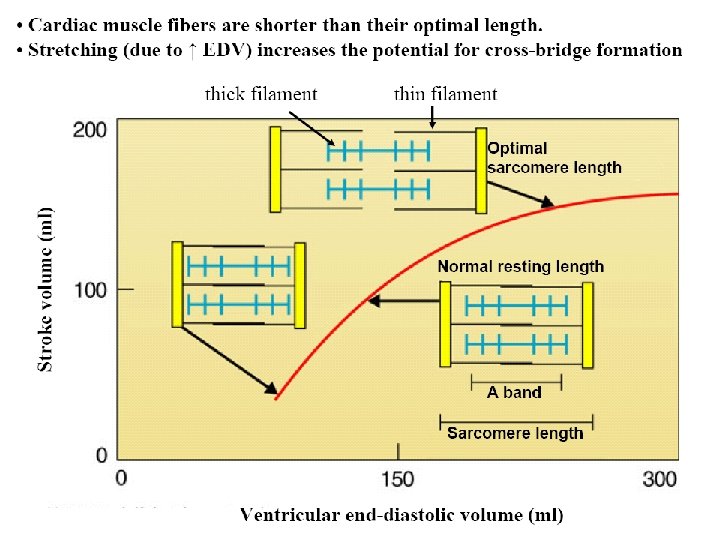
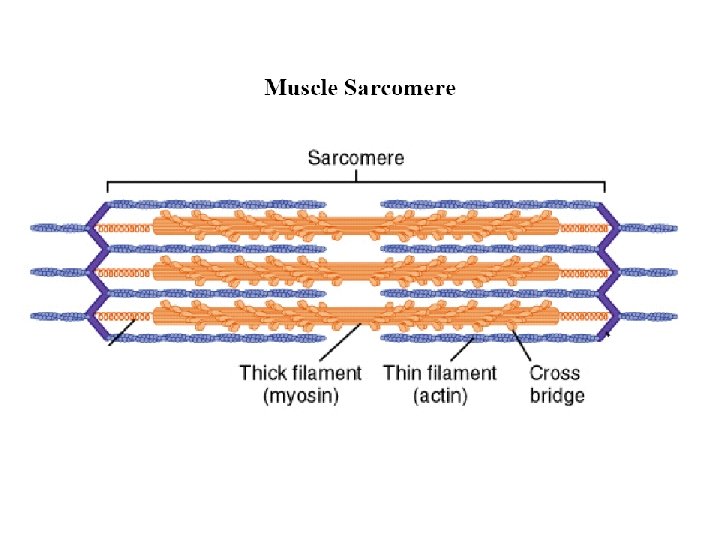
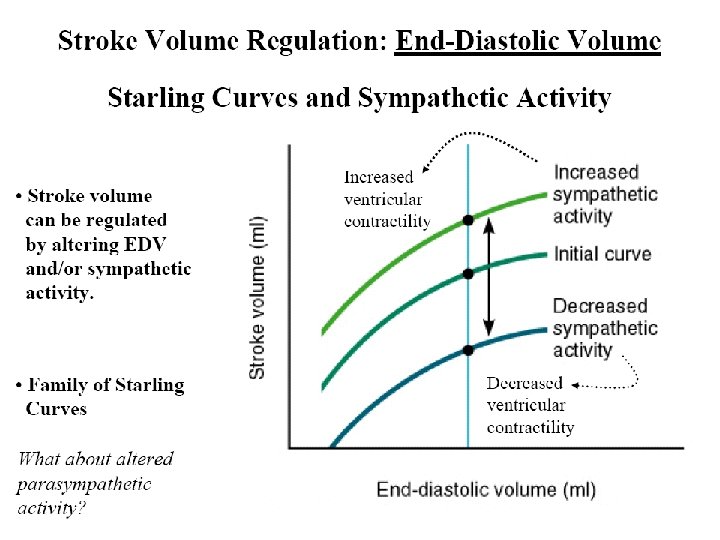
Frank-Starling Mechanism • As blood moves into the heart, it stretches the cardiac muscle. • In exercise, more blood enters the heart, stretching it even more. • Extra stretch produces extra force. • Expels larger volume of blood. • Enables us to handle increased blood volume. • Unique to cardiac muscle. • Thus, we have increased force on demand.
Frank-Starling Law. Increased myocardial stretch = increased force of contraction. ↑ Volume = ↑ Pressure = ↑ Stretch ↓ Volume = ↓ Pressure = ↓ Stretch
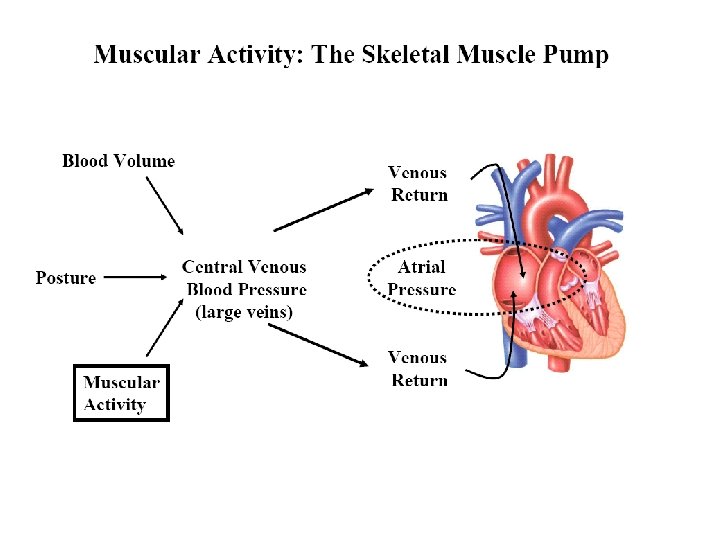
Vasoconstriction will increase venous return/preload, and vasodilation will decrease venous return/preload. § vasoconstriction = preload § vasodilation = preload
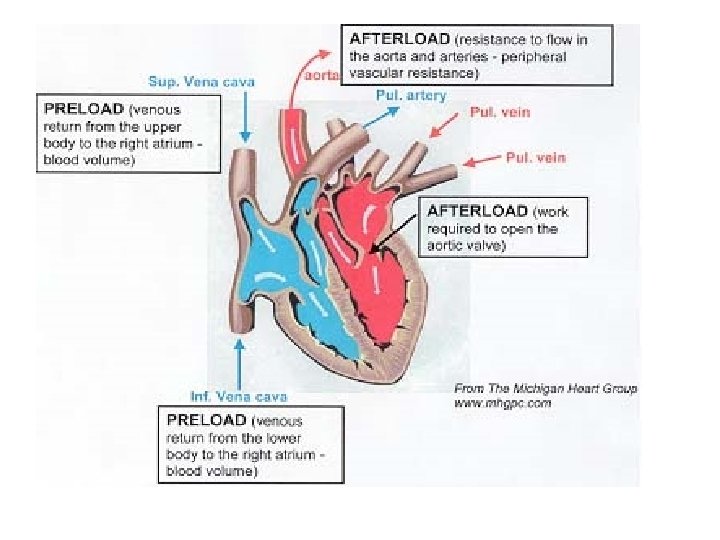
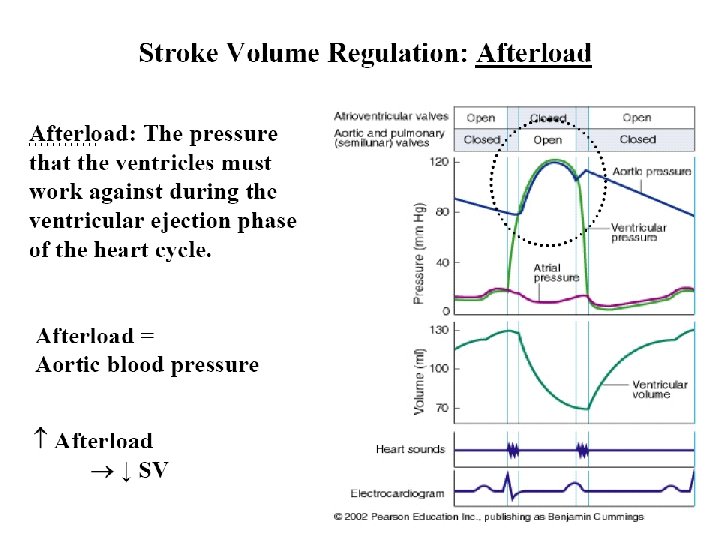
Afterload : is the pressure against which the ventricles must pump - and overcome - in order to open the aortic/pulmonic valves and eject their contents.
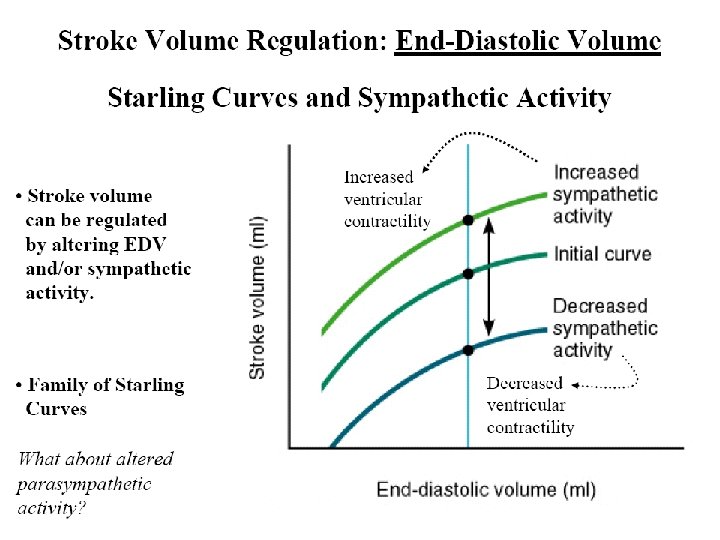
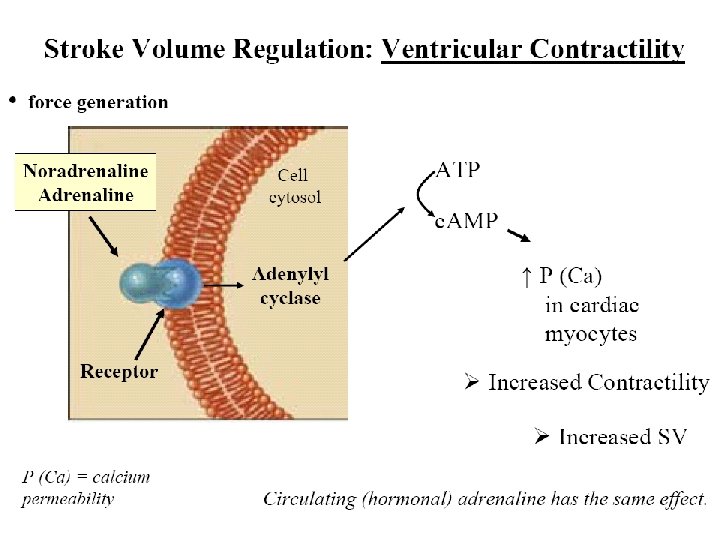
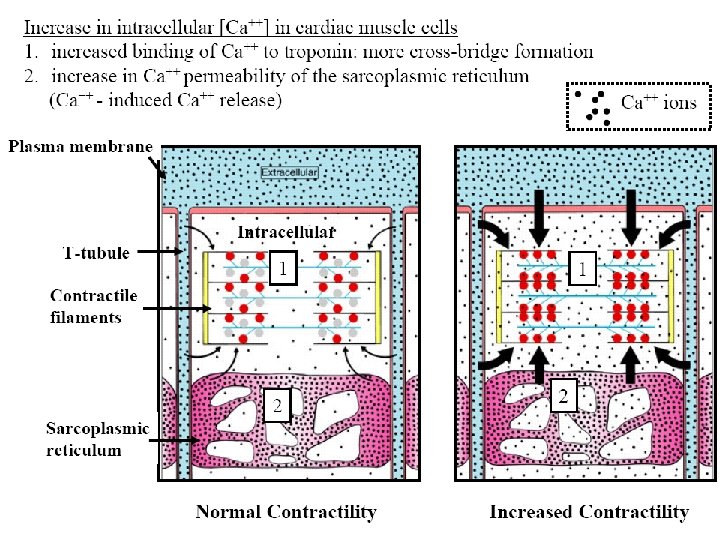
Myocardial contractility Contractility (inotropy): refers to the ability of the heart to contract - independent of preload stretch.
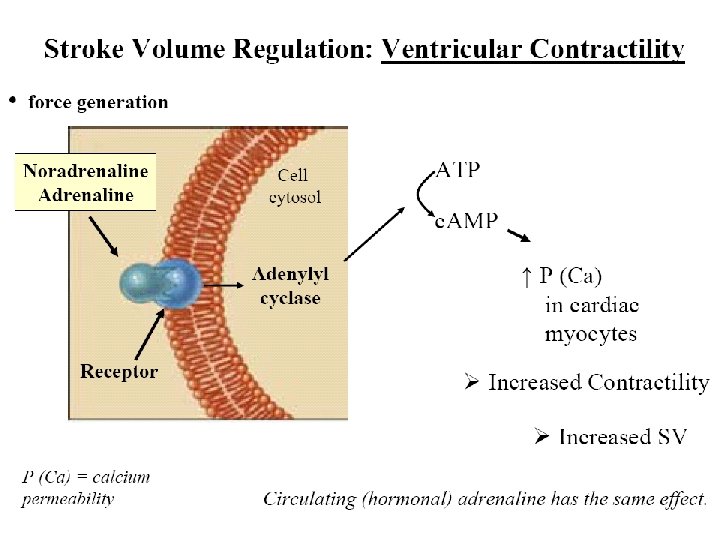
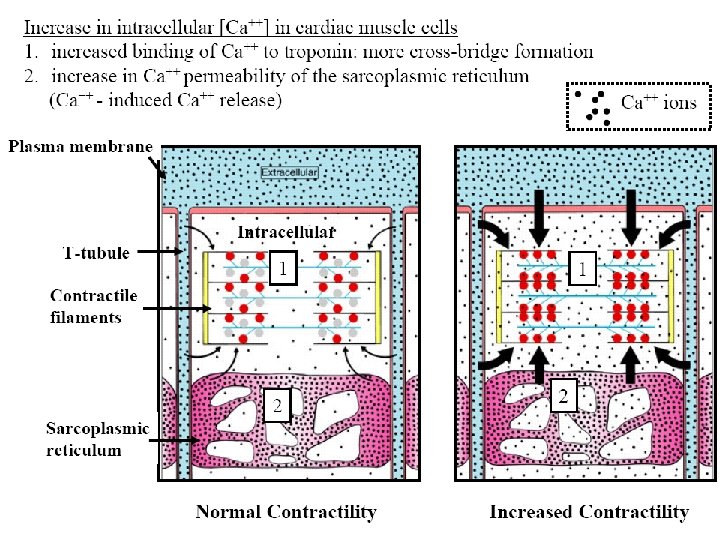
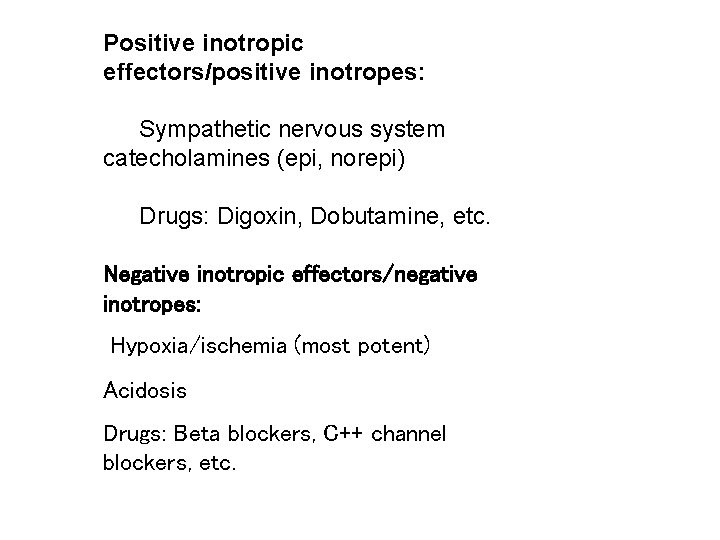
Positive inotropic effectors/positive inotropes: Sympathetic nervous system catecholamines (epi, norepi) Drugs: Digoxin, Dobutamine, etc. Negative inotropic effectors/negative inotropes: Hypoxia/ischemia (most potent) Acidosis Drugs: Beta blockers, C++ channel blockers, etc.
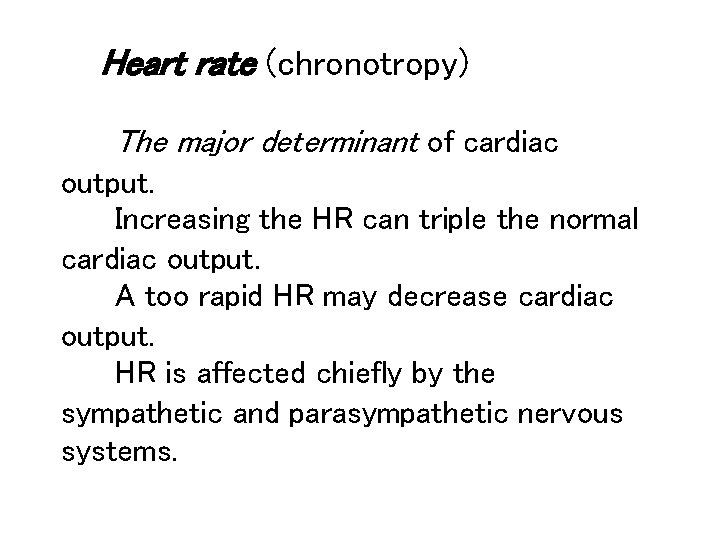
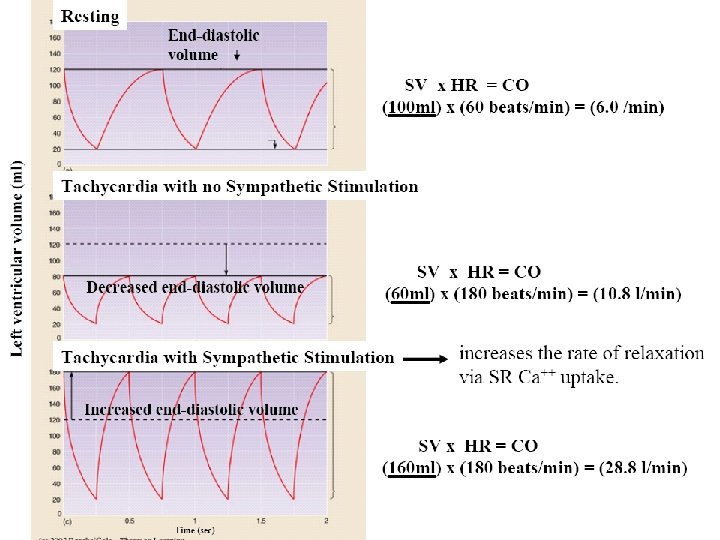
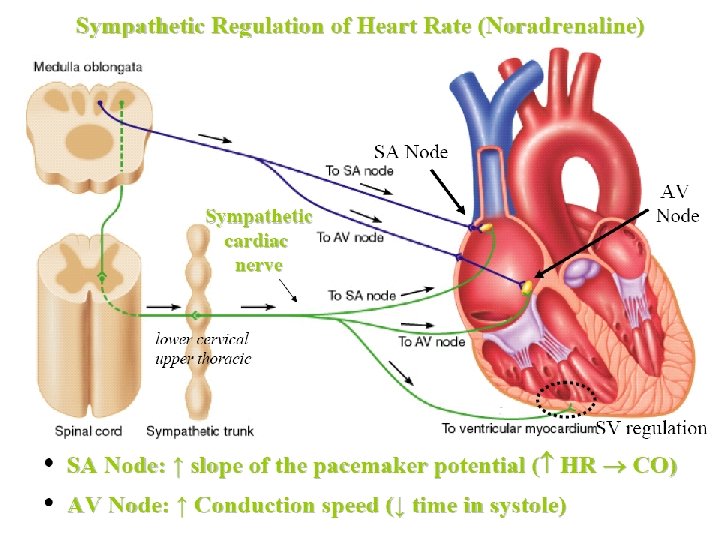
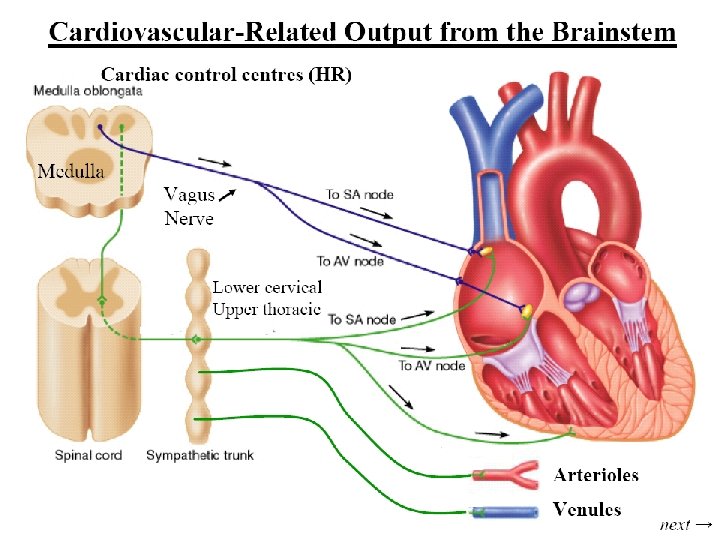
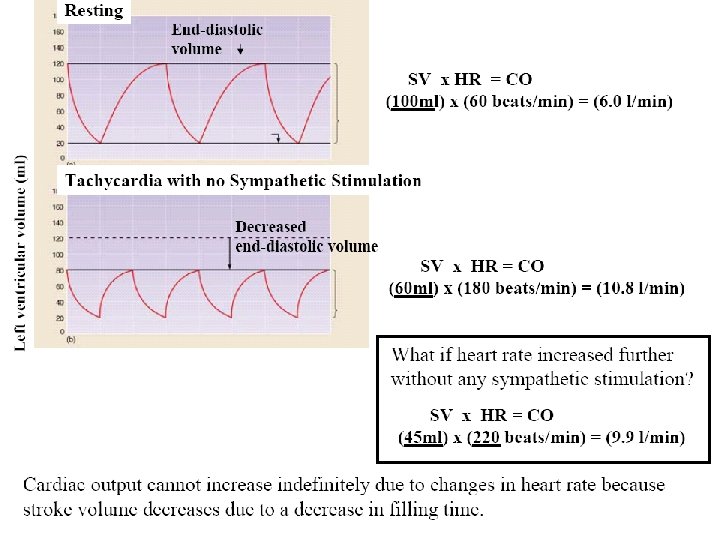
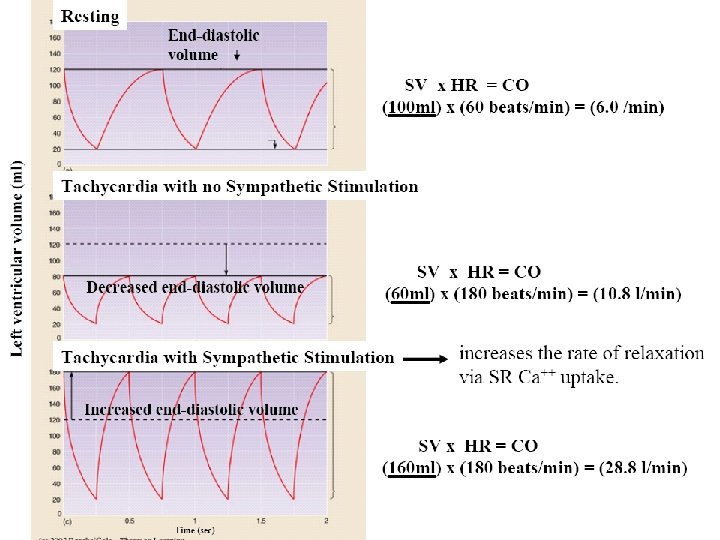
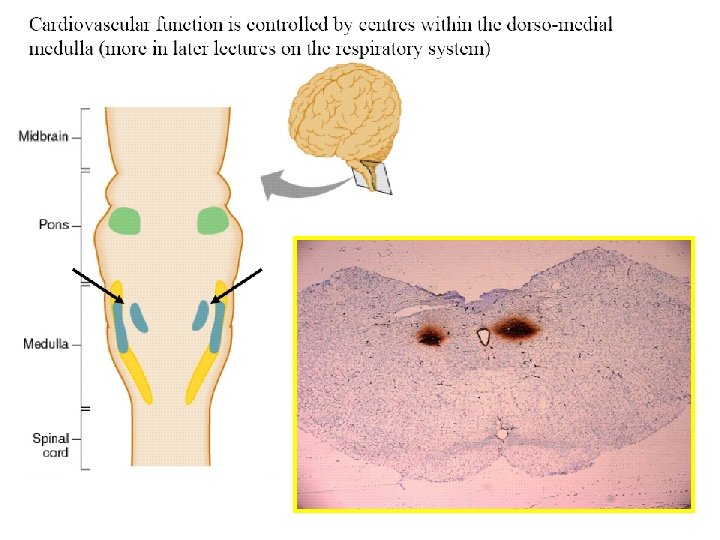
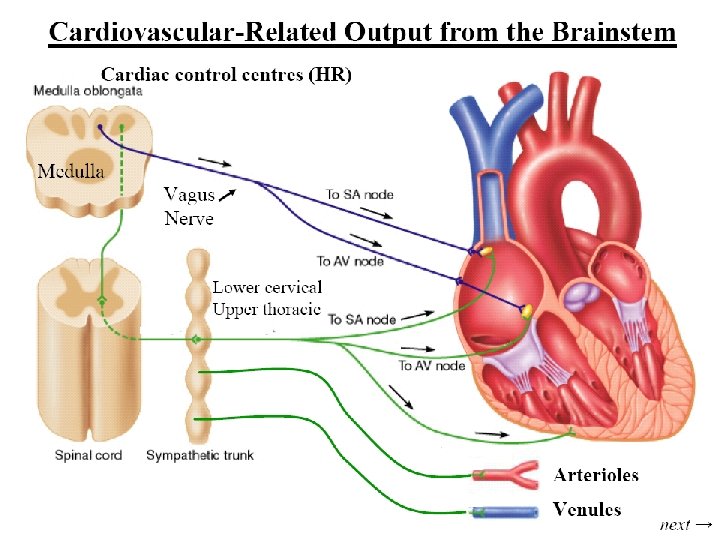
Heart rate (chronotropy) The major determinant of cardiac output. Increasing the HR can triple the normal cardiac output. A too rapid HR may decrease cardiac output. HR is affected chiefly by the sympathetic and parasympathetic nervous systems.
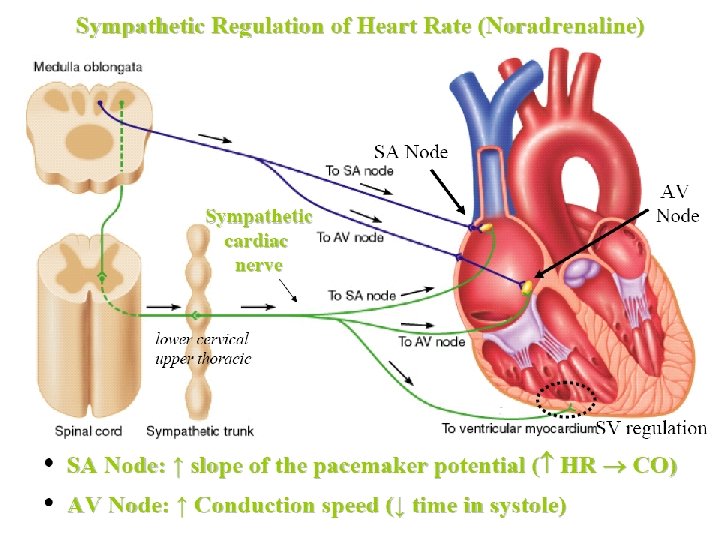
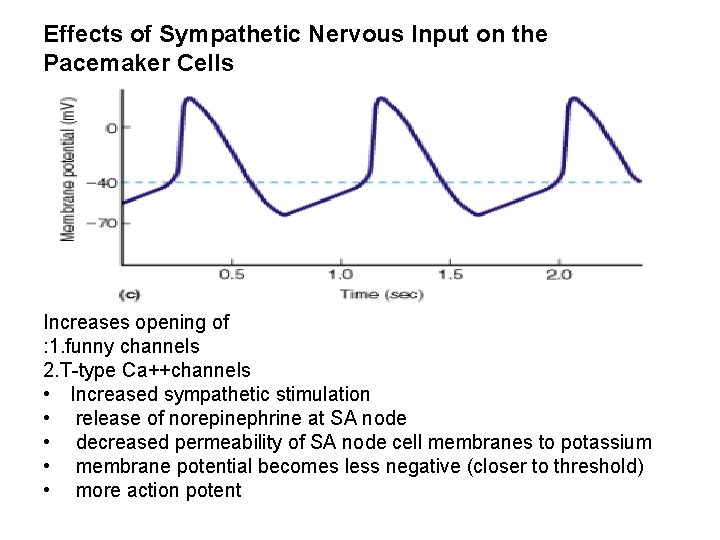
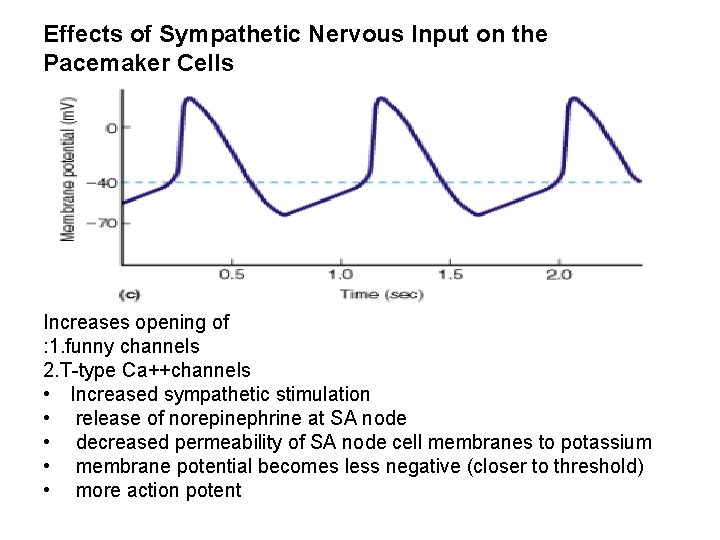
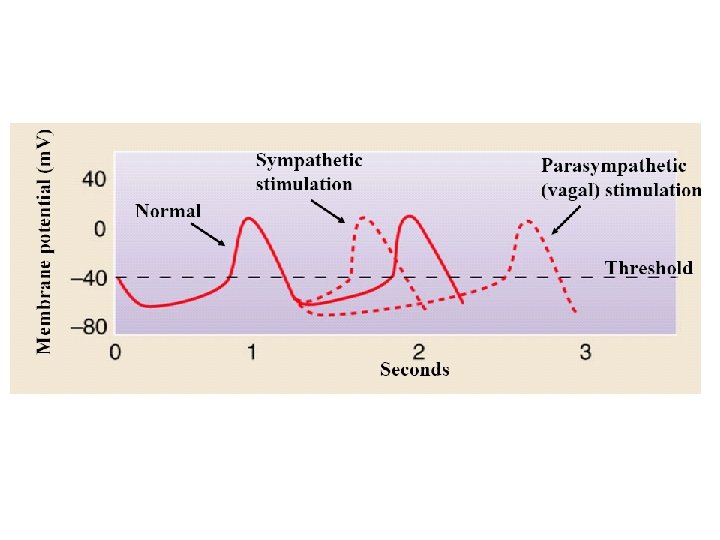
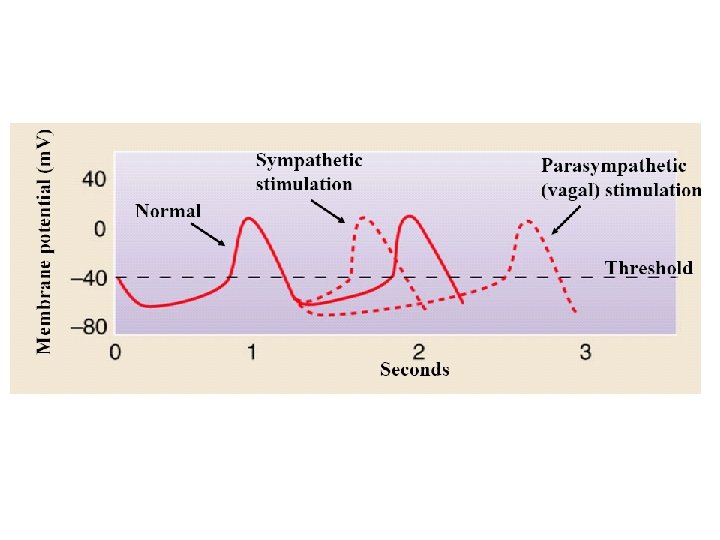
Effects of Sympathetic Nervous Input on the Pacemaker Cells . Increases opening of : 1. funny channels 2. T-type Ca++channels • Increased sympathetic stimulation • release of norepinephrine at SA node • decreased permeability of SA node cell membranes to potassium • membrane potential becomes less negative (closer to threshold) • more action potent
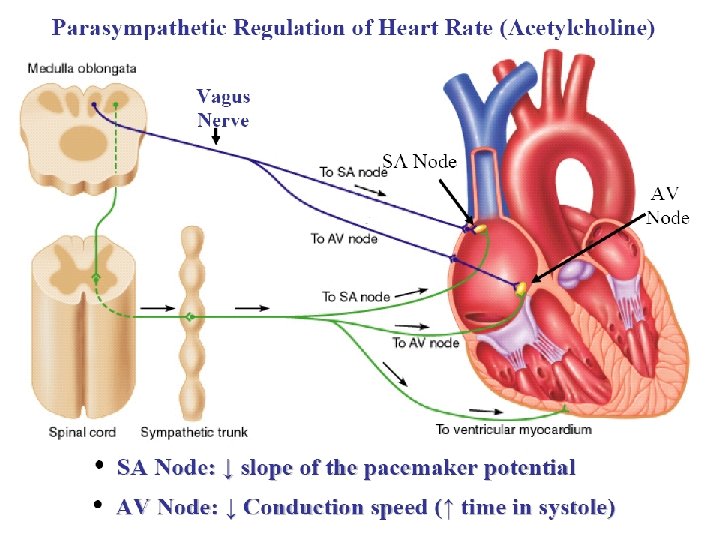
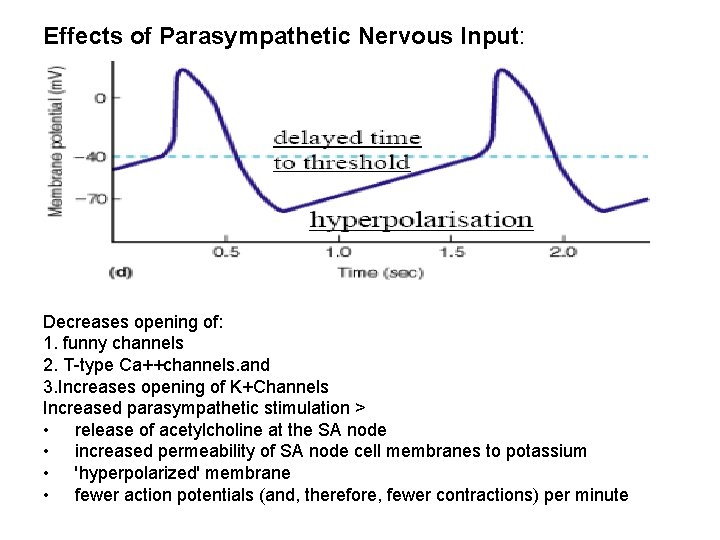
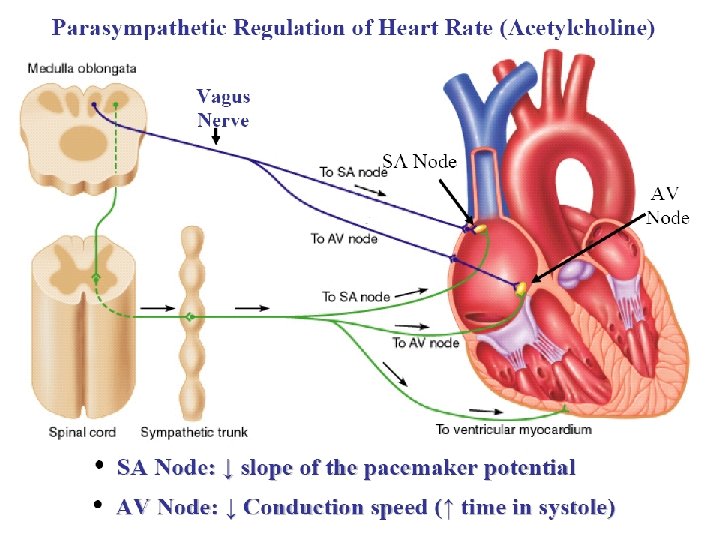
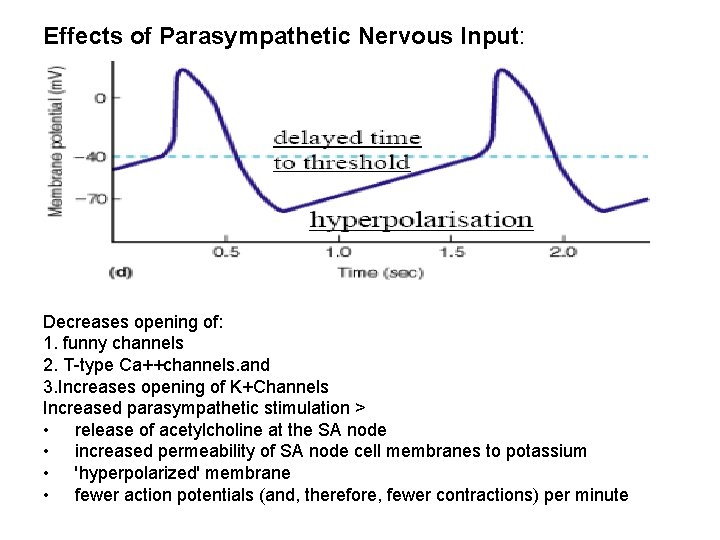
Effects of Parasympathetic Nervous Input: Decreases opening of: 1. funny channels 2. T-type Ca++channels. and 3. Increases opening of K+Channels Increased parasympathetic stimulation > • release of acetylcholine at the SA node • increased permeability of SA node cell membranes to potassium • 'hyperpolarized' membrane • fewer action potentials (and, therefore, fewer contractions) per minute
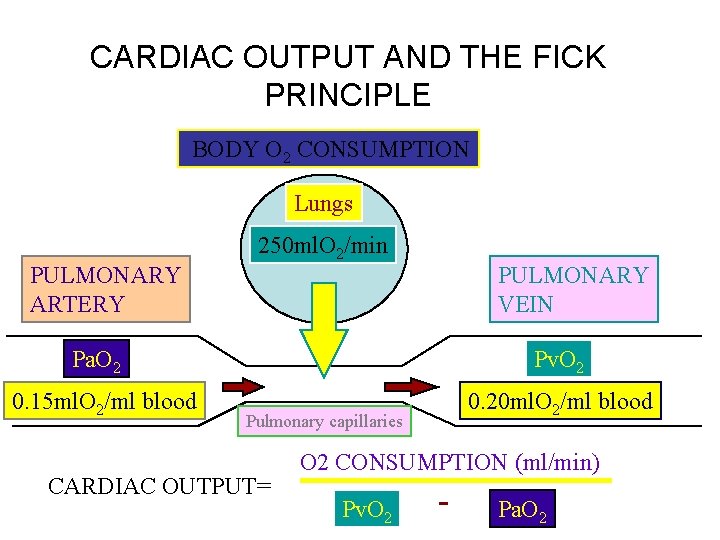
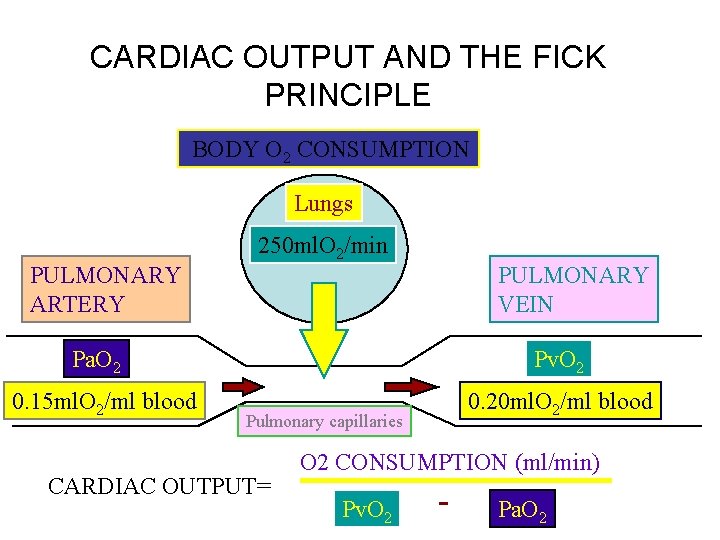
CARDIAC OUTPUT AND THE FICK PRINCIPLE BODY O 2 CONSUMPTION Lungs PULMONARY ARTERY 250 ml. O 2/min PULMONARY VEIN Pa. O 2 0. 15 ml. O 2/ml blood Pv. O 2 0. 20 ml. O 2/ml blood Pulmonary capillaries CARDIAC OUTPUT= O 2 CONSUMPTION (ml/min) Pv. O 2 - Pa. O 2
