Cardiac output and Venous Return Faisal I Mohammed









- Slides: 45
Cardiac output and Venous Return Faisal I. Mohammed, MD, Ph. D 1
Objectives Define cardiac output and venous return Describe the methods of measurement of CO Outline the factors that regulate cardiac output Follow up the cardiac output curves at different physiological states l Define venous return and describe venous return curve l Outline the factors that regulate venous return curve at different physiological states l Inter-relate Cardiac output and venous return curves l l 2
Important Concepts About Cardiac Output (CO) Control • Cardiac Output is the sum of all tissue flows and is affected by their regulation (CO = 5 L/min, cardiac index = 3 L/min/m 2). • CO is proportional to tissue O 2. use. • CO is proportional to 1/TPR when AP is constant. • F= P/R (Ohm’s law) • CO = (MAP - RAP) / TPR, (RAP=0) then • CO=MAP/TPR ; MAP=CO*TPR 3
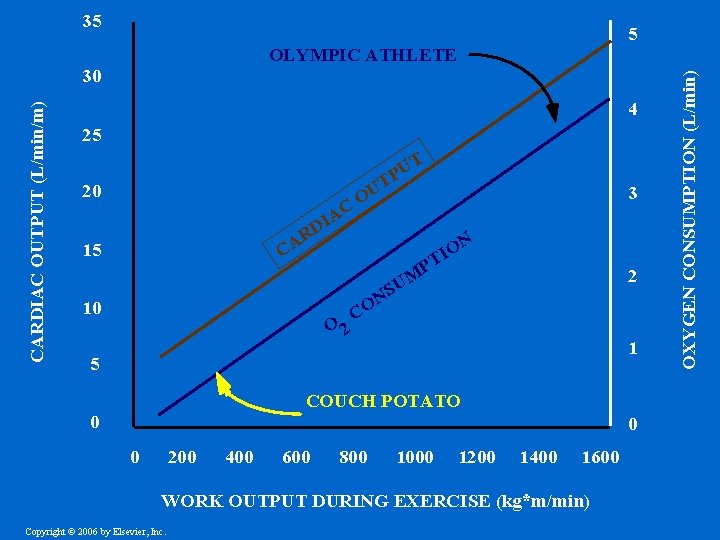
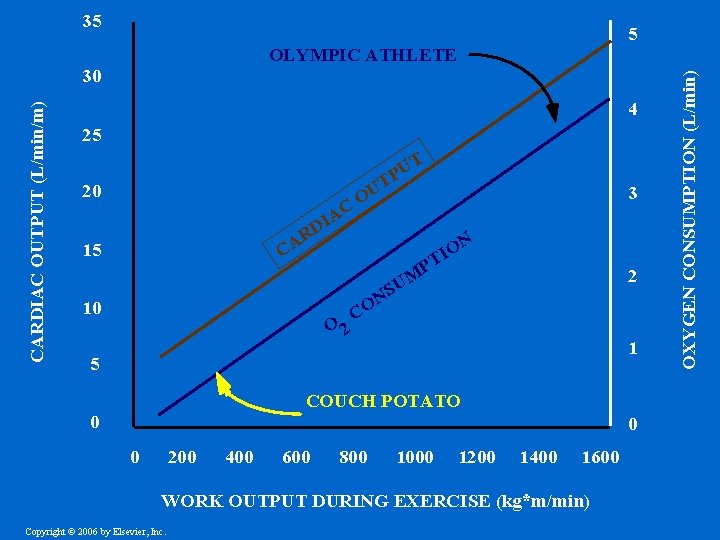
35 4 25 T U P 20 C A DI T U O R A C 15 10 3 N O I PT O 2 2 M U S N CO 1 5 COUCH POTATO 0 0 0 200 400 600 800 1000 1200 1400 1600 WORK OUTPUT DURING EXERCISE (kg*m/min) Copyright © 2006 by Elsevier, Inc. OXYGEN CONSUMPTION (L/min) OLYMPIC ATHLETE 30 CARDIAC OUTPUT (L/min/m) 5
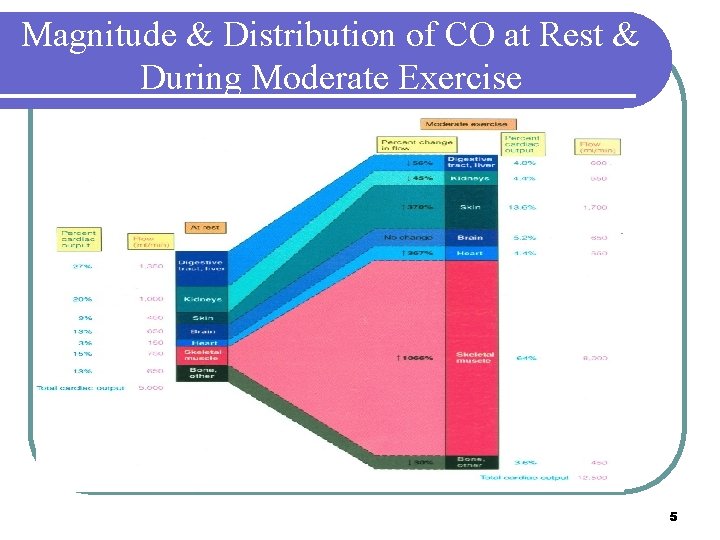
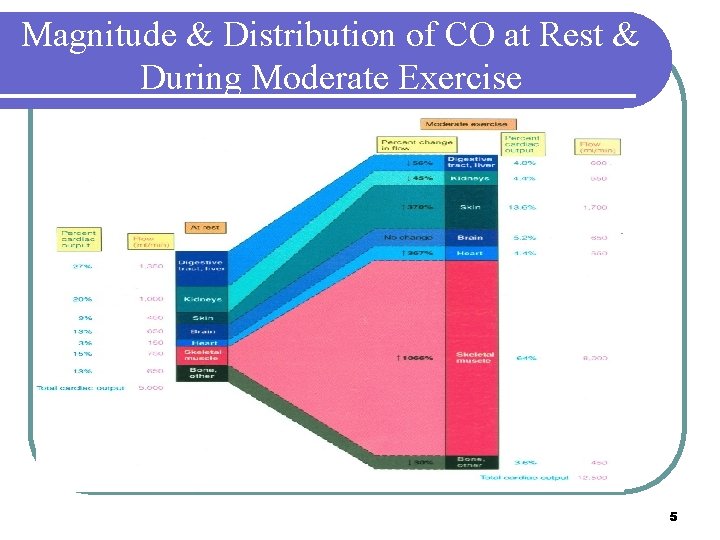
Magnitude & Distribution of CO at Rest & During Moderate Exercise 5
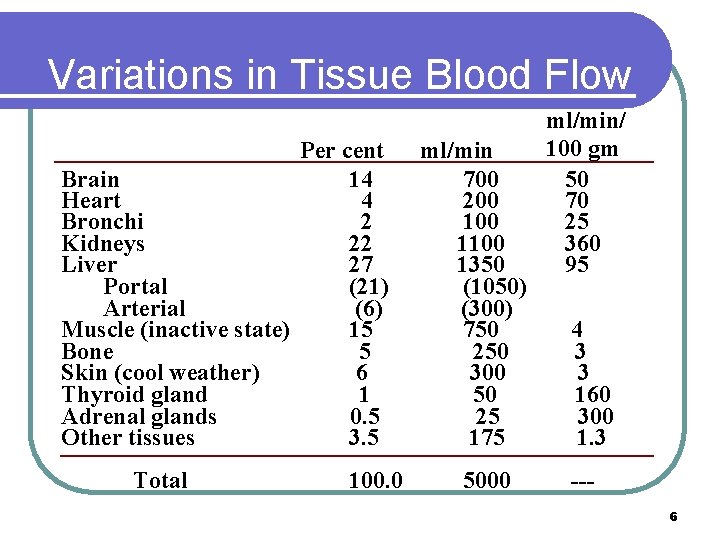
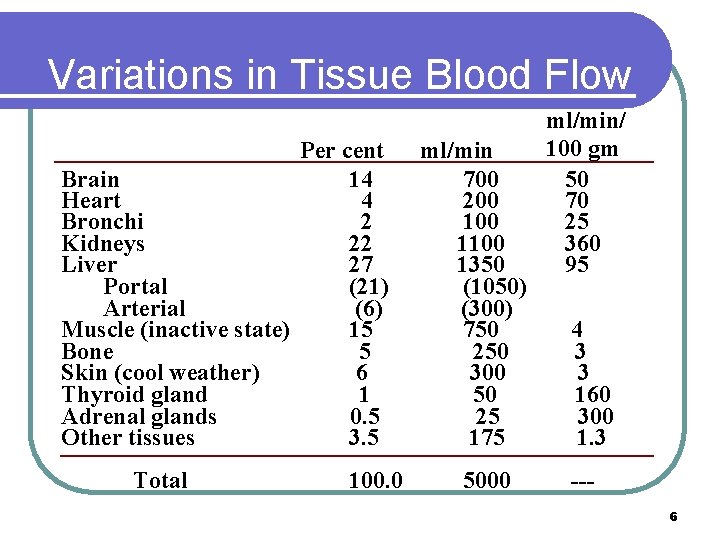
Variations in Tissue Blood Flow Per cent Brain 14 Heart 4 Bronchi 2 Kidneys 22 Liver 27 Portal (21) Arterial (6) Muscle (inactive state) 15 Bone 5 Skin (cool weather) 6 Thyroid gland 1 Adrenal glands 0. 5 Other tissues 3. 5 Total 100. 0 ml/min 700 200 1100 1350 (1050) (300) 750 250 300 50 25 175 5000 ml/min/ 100 gm 50 70 25 360 95 4 3 3 160 300 1. 3 --6
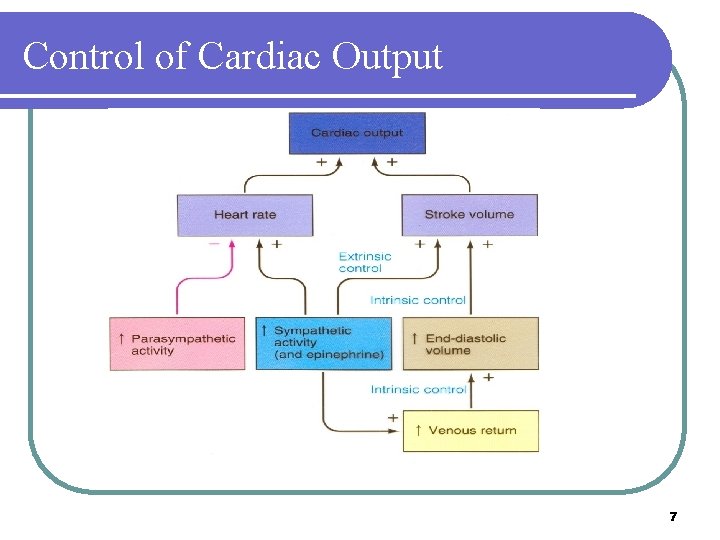
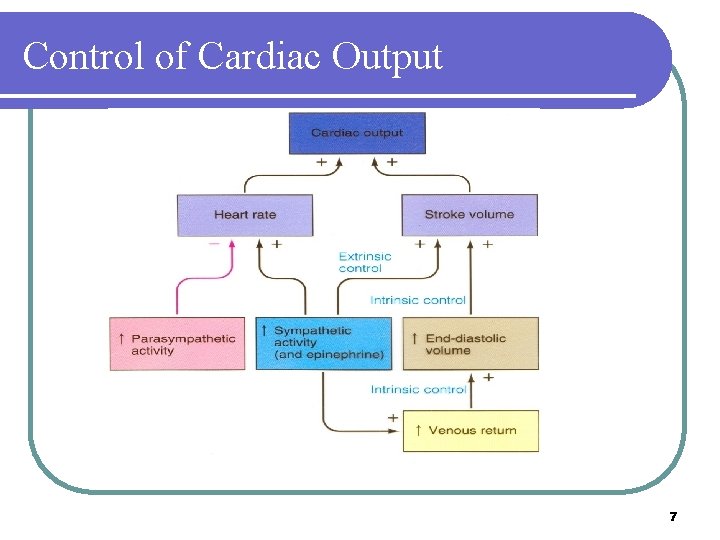
Control of Cardiac Output 7
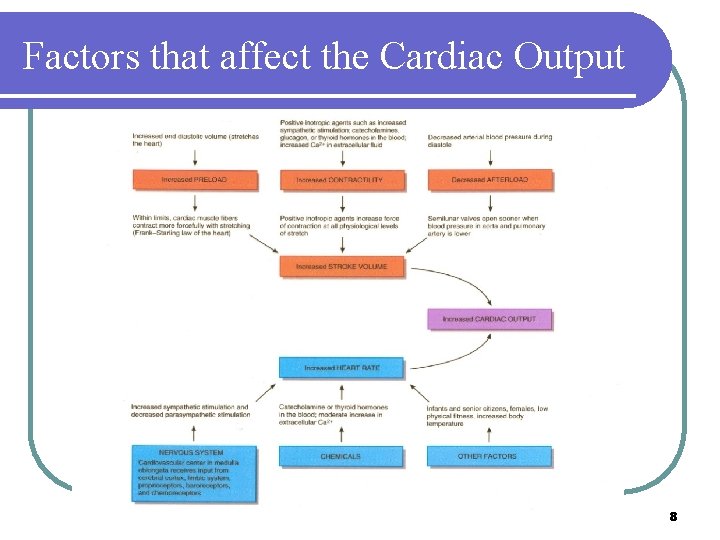
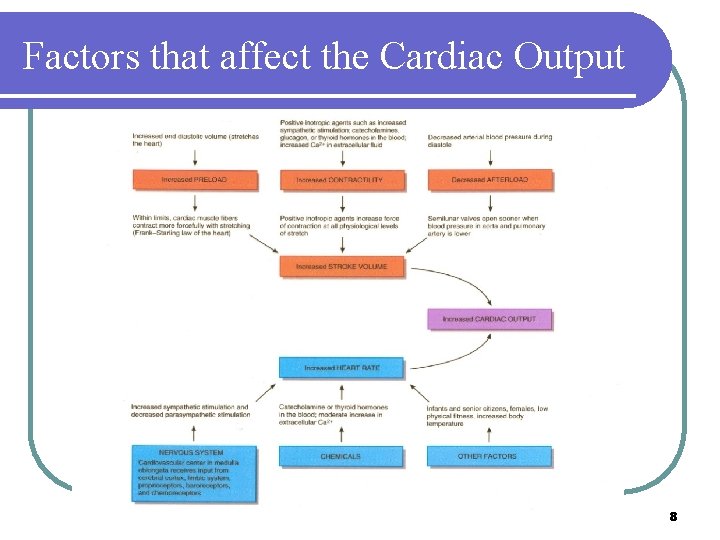
Factors that affect the Cardiac Output 8
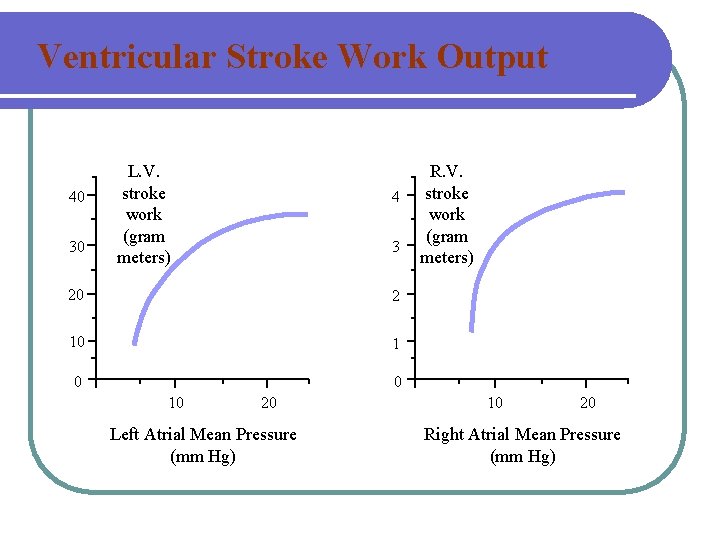
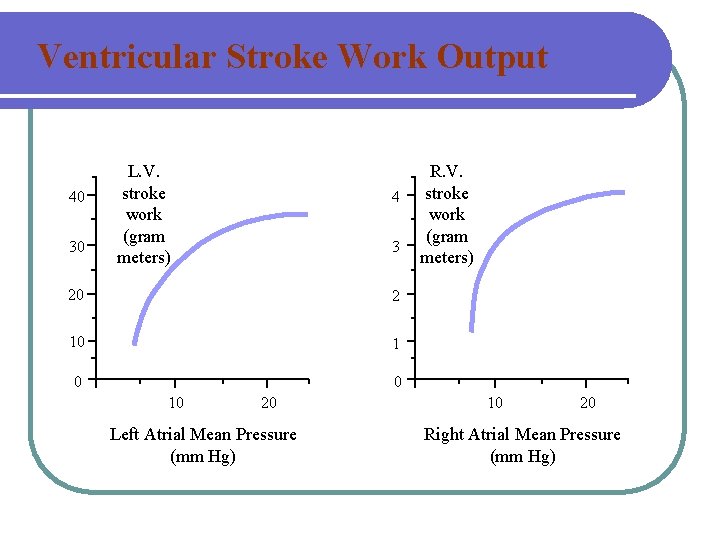
Ventricular Stroke Work Output 40 30 L. V. stroke work (gram meters) 4 3 20 2 10 1 0 0 10 20 Left Atrial Mean Pressure (mm Hg) R. V. stroke work (gram meters) 10 20 Right Atrial Mean Pressure (mm Hg)
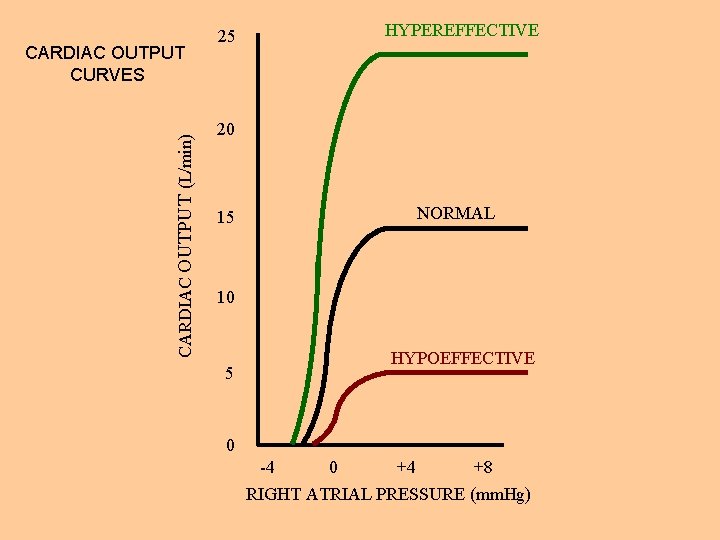
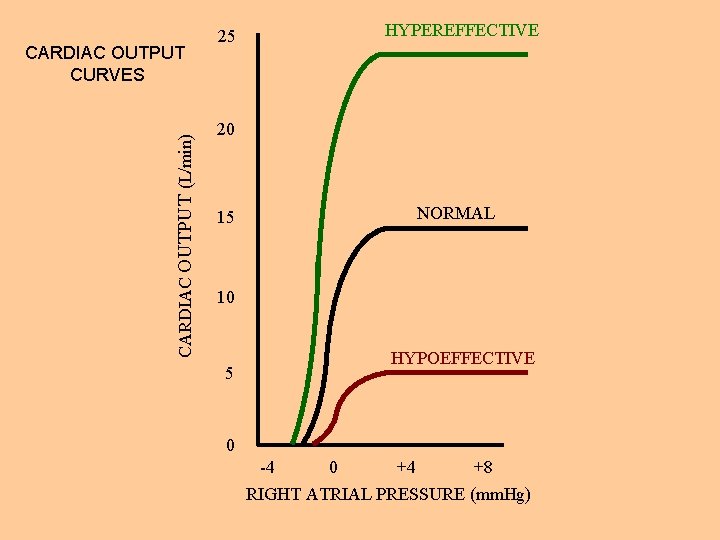
CARDIAC OUTPUT (L/min) CARDIAC OUTPUT CURVES 25 HYPEREFFECTIVE 20 15 NORMAL 10 5 HYPOEFFECTIVE 0 -4 0 +4 +8 RIGHT ATRIAL PRESSURE (mm. Hg)

Effect of Sympathetic and Parasympathetic Stimulation on Cardiac Output Maximum sympathetic stimulation Cardiac Output (L/min) 25 20 Normal sympathetic stimulation 15 Zero sympathetic stimulation 10 (Parasympathetic stimulation) 5 0 -4 0 +4 +8 Right Atrial Pressure (mm. Hg)

IPP = INTRAPLEURAL PRESSURE DE C IA CARD = 2 m m. H g ONA P M A T IPP= -5. 5 5 -2 m m. Hg mm Hg -4 m m. H g 10 IPP= CARDIAC OUTPUT (L/min) 15 0 -4 0 4 8 RIGHT ATRIAL PRESSURE (mm. Hg) 12
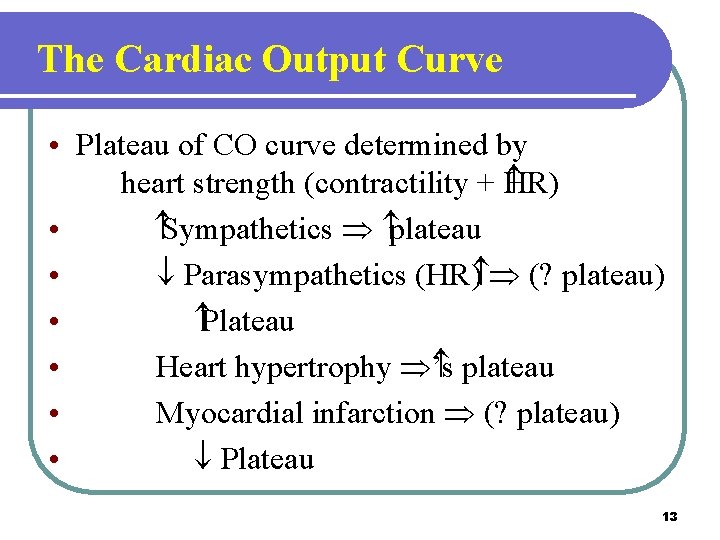
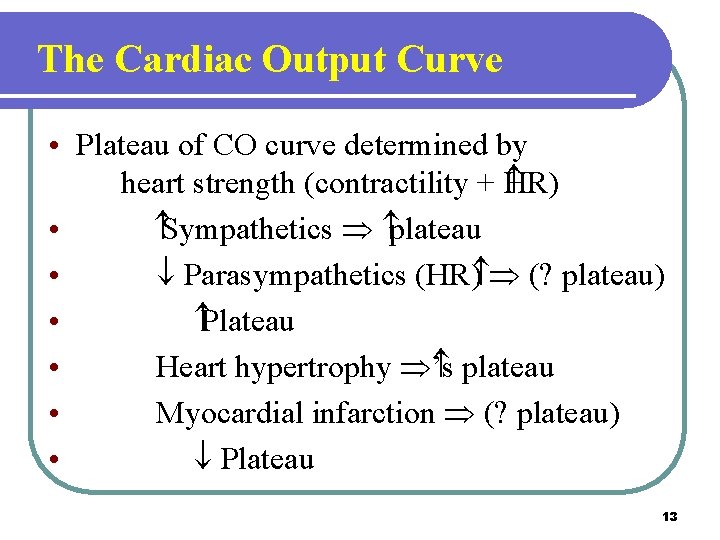
The Cardiac Output Curve • Plateau of CO curve determined by heart strength (contractility + HR) • Sympathetics Þ plateau • ¯ Parasympathetics (HR ) Þ (? plateau) • Plateau • Heart hypertrophy Þ ’s plateau • Myocardial infarction Þ (? plateau) • ¯ Plateau 13

The Cardiac Output Curve (cont’d) • Valvular disease Þ ¯ plateau (stenosis or regurgitation) • Myocarditis Þ ¯ plateau • Cardiac tamponade Þ (? plateau) • ¯ Plateau • Metabolic damage Þ ¯ plateau 14

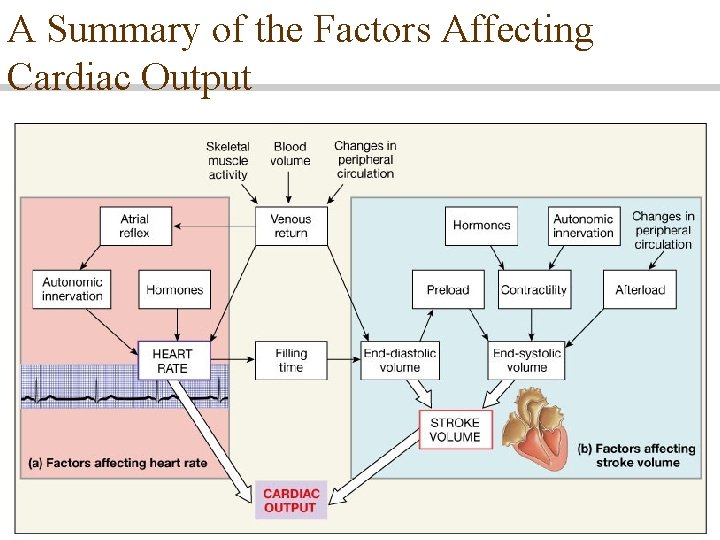
Factors Affecting Cardiac Output
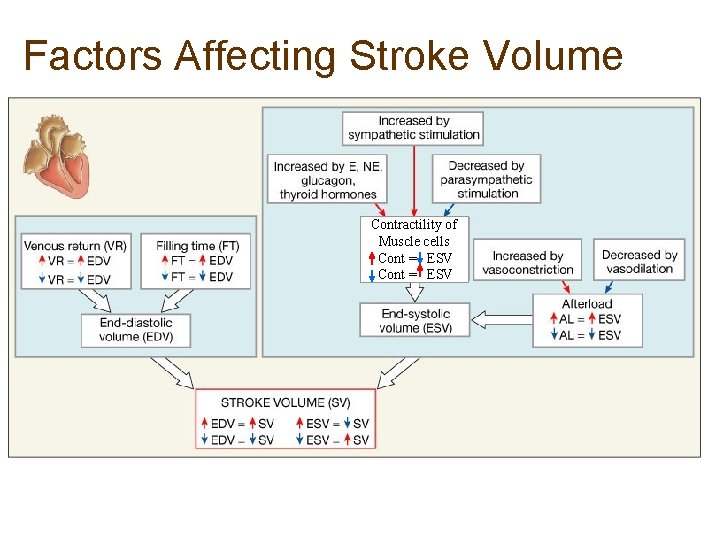
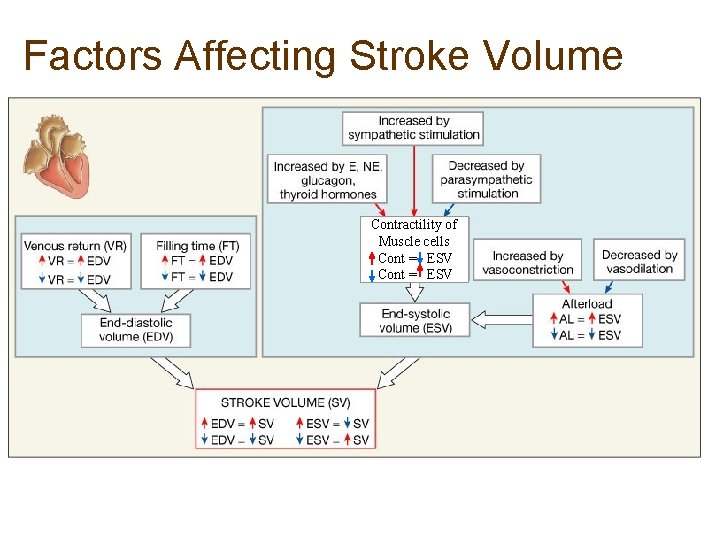
Factors Affecting Stroke Volume Contractility of Muscle cells Cont = ESV
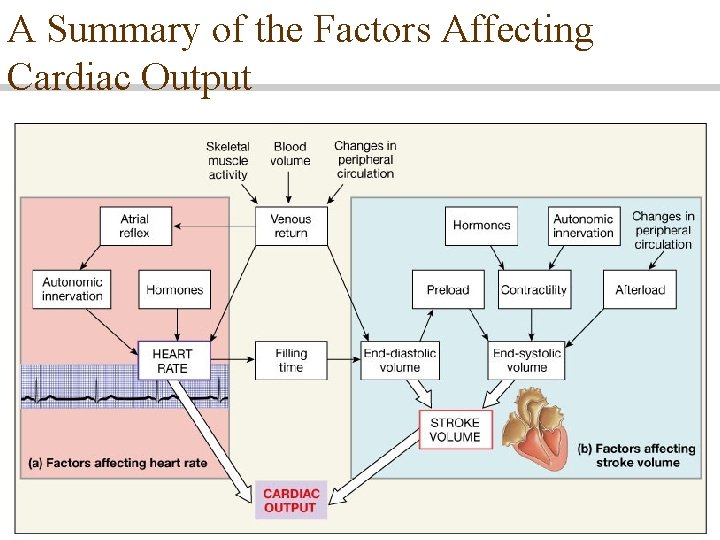
A Summary of the Factors Affecting Cardiac Output
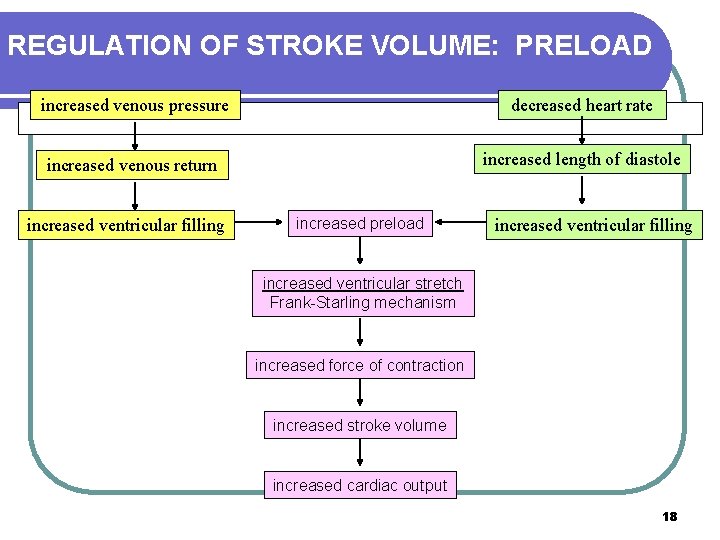
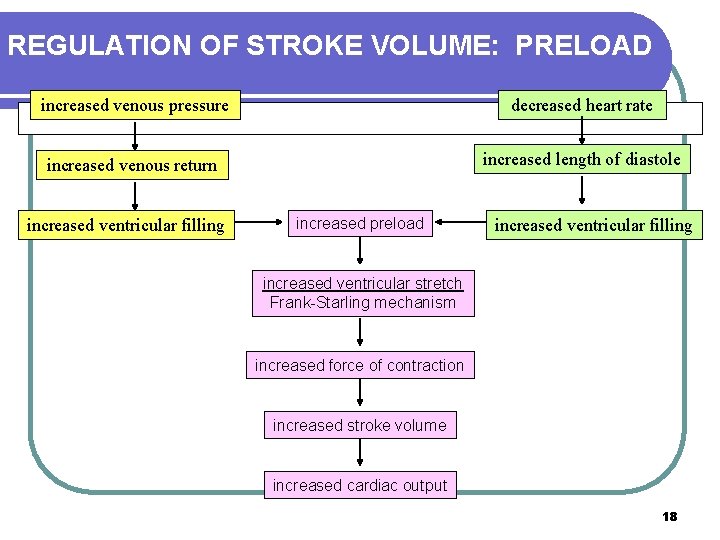
REGULATION OF STROKE VOLUME: PRELOAD increased venous pressure decreased heart rate increased venous return increased length of diastole increased ventricular filling increased preload increased ventricular filling increased ventricular stretch Frank-Starling mechanism increased force of contraction increased stroke volume increased cardiac output 18
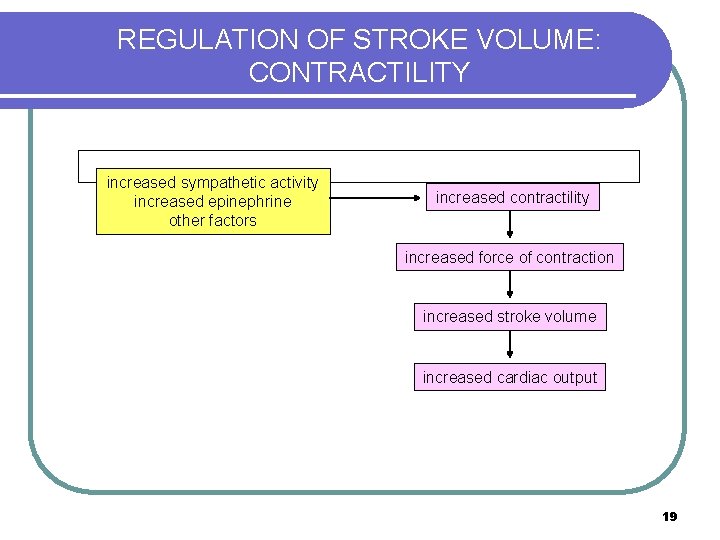
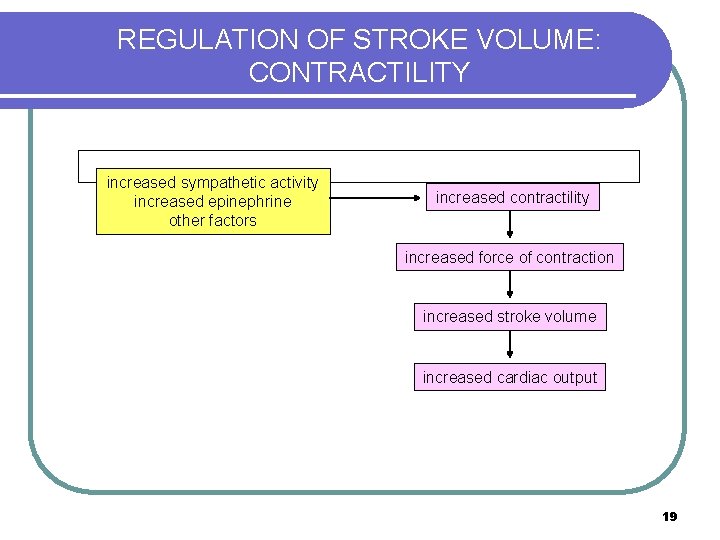
REGULATION OF STROKE VOLUME: CONTRACTILITY increased sympathetic activity increased epinephrine other factors increased contractility increased force of contraction increased stroke volume increased cardiac output 19
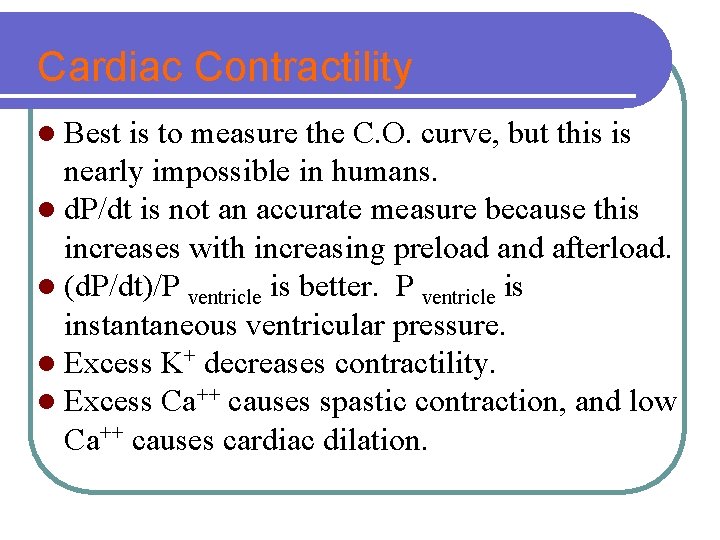
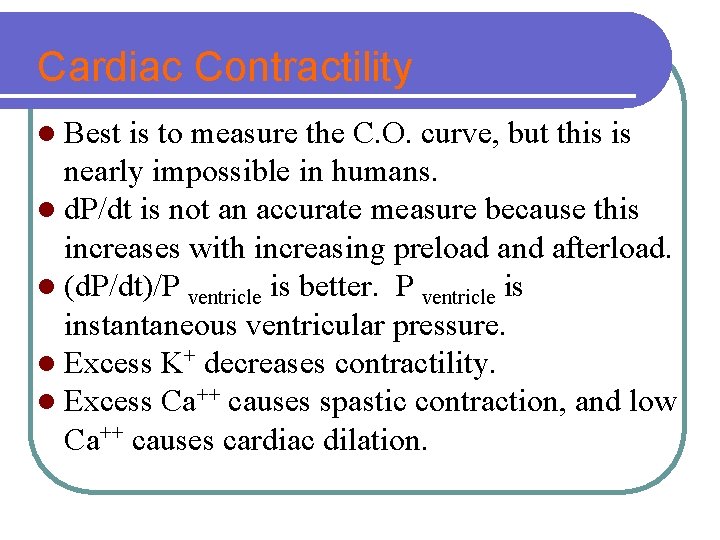
Cardiac Contractility l Best is to measure the C. O. curve, but this is nearly impossible in humans. l d. P/dt is not an accurate measure because this increases with increasing preload and afterload. l (d. P/dt)/P ventricle is better. P ventricle is instantaneous ventricular pressure. l Excess K+ decreases contractility. l Excess Ca++ causes spastic contraction, and low Ca++ causes cardiac dilation.
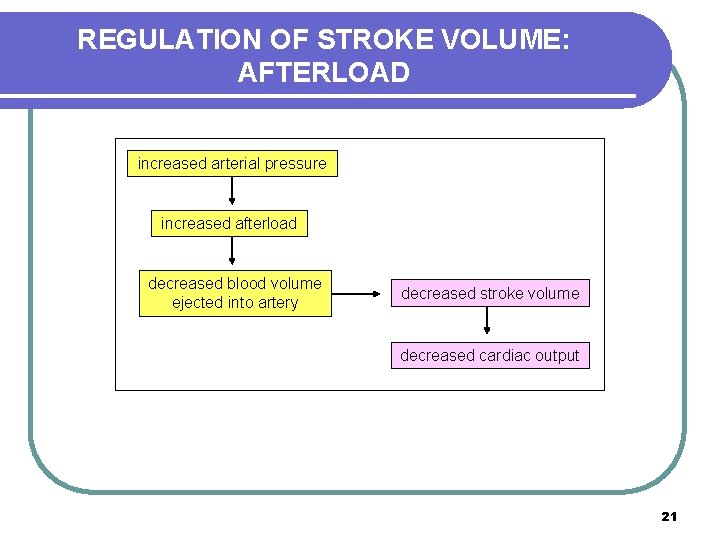
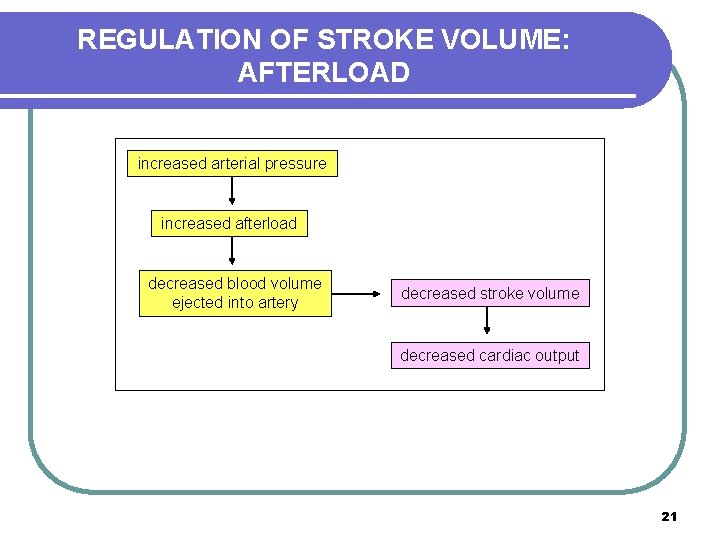
REGULATION OF STROKE VOLUME: AFTERLOAD increased arterial pressure increased afterload decreased blood volume ejected into artery decreased stroke volume decreased cardiac output 21
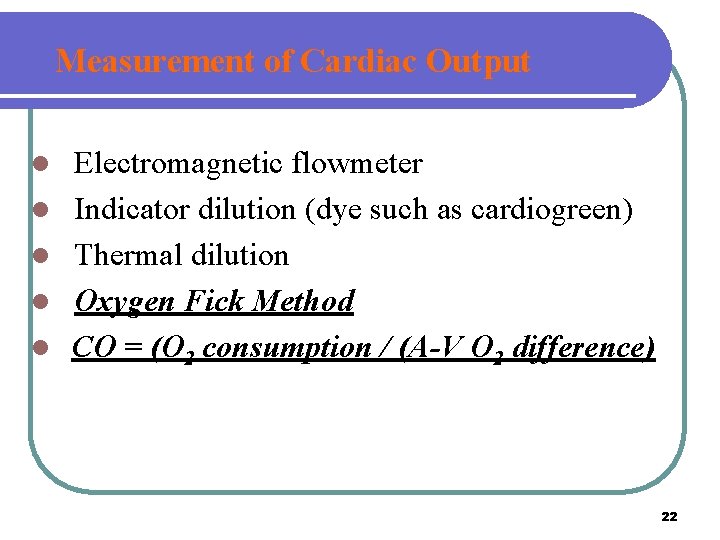
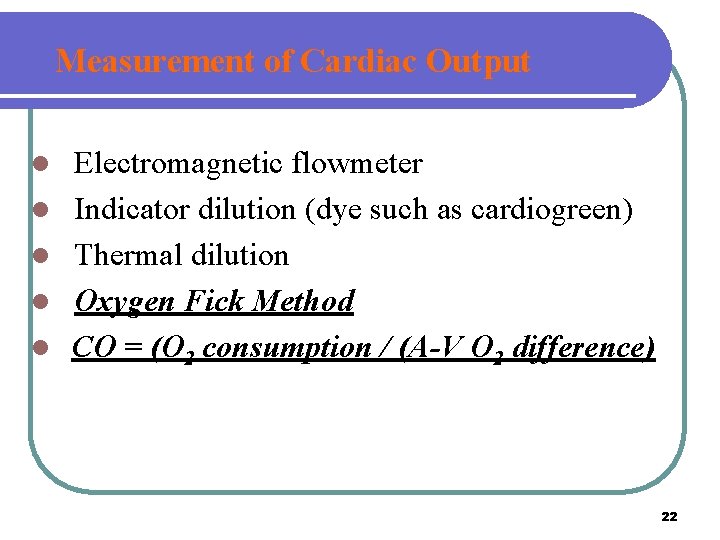
Measurement of Cardiac Output l l l Electromagnetic flowmeter Indicator dilution (dye such as cardiogreen) Thermal dilution Oxygen Fick Method CO = (O 2 consumption / (A-V O 2 difference) 22
Electromagnetic flowmeter 23
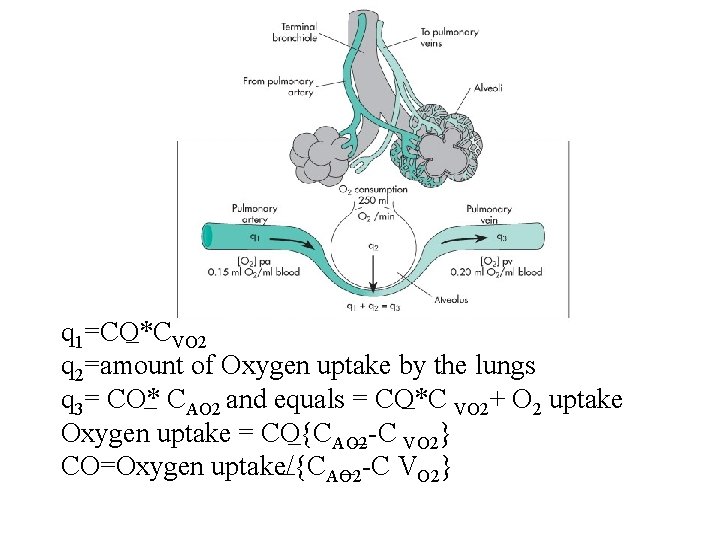
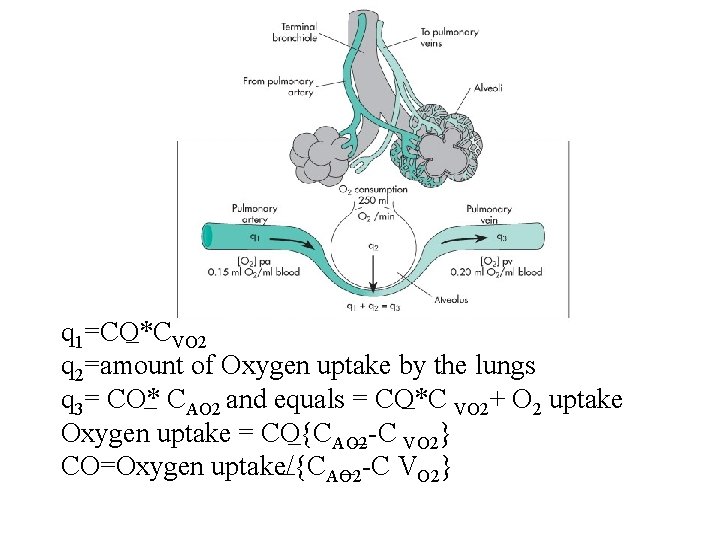
q 1=CO*CVO 2 q 2=amount of Oxygen uptake by the lungs q 3= CO* CAO 2 and equals = CO*C VO 2+ O 2 uptake Oxygen uptake = CO{CAO 2 -C VO 2} CO=Oxygen uptake/{CAO 2 -C VO 2}
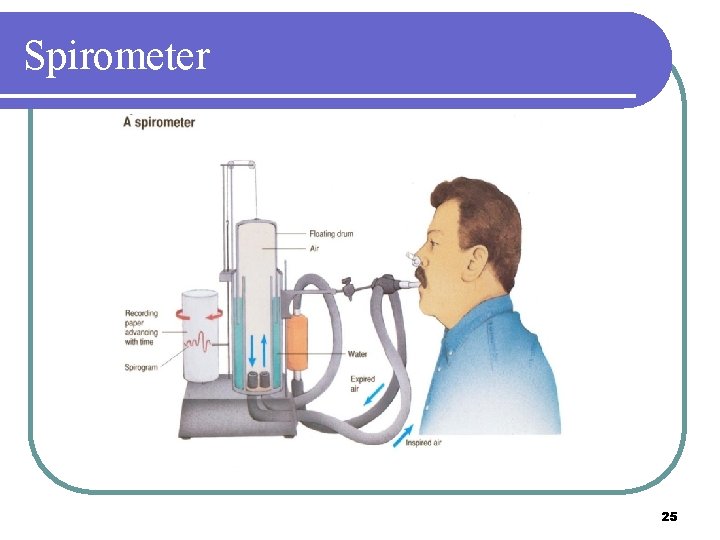
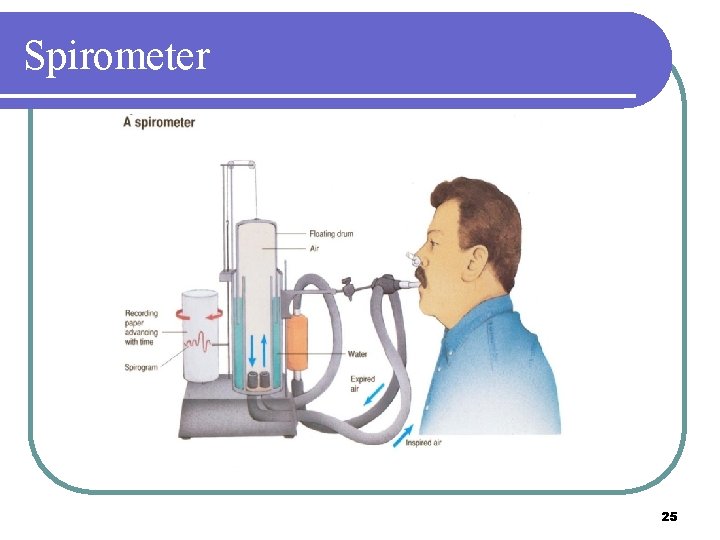
Spirometer 25

Swan-Ganz catheter 26
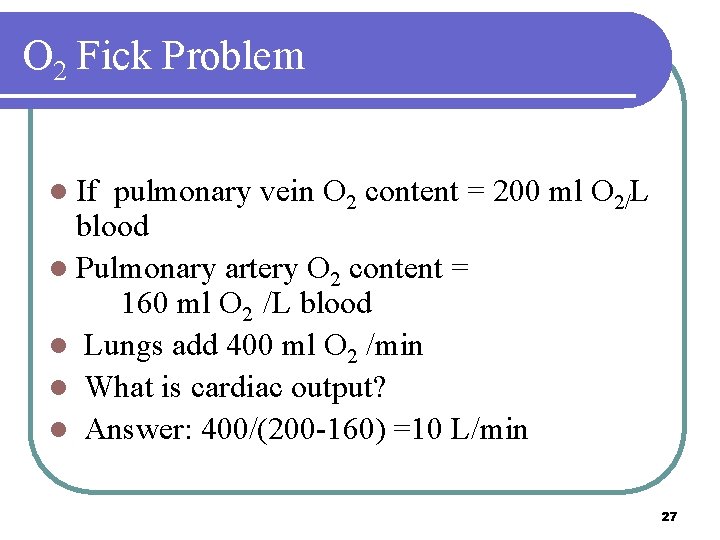
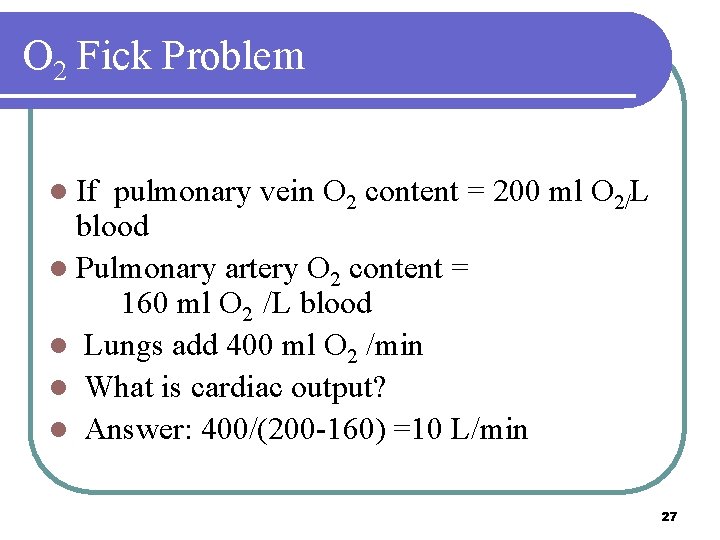
O 2 Fick Problem l If pulmonary vein O 2 content = 200 ml O 2/L blood l Pulmonary artery O 2 content = 160 ml O 2 /L blood l Lungs add 400 ml O 2 /min l What is cardiac output? l Answer: 400/(200 -160) =10 L/min 27
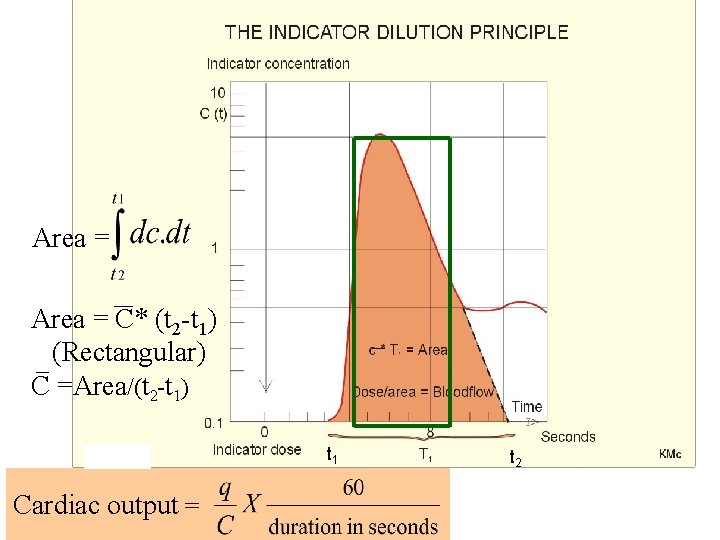
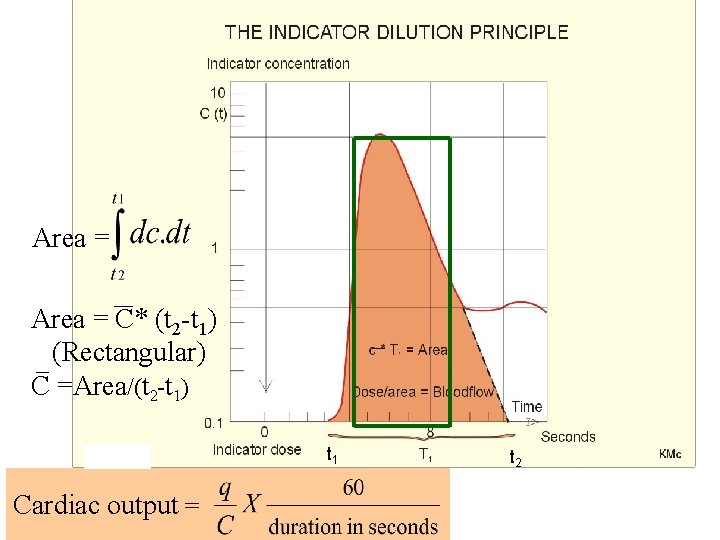
Area = C* (t 2 -t 1) (Rectangular) C =Area/(t 2 -t 1) t 1 Cardiac output = t 2
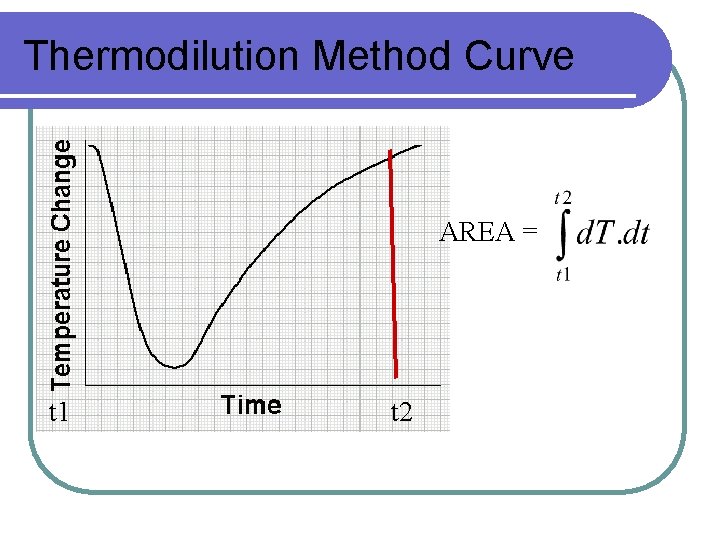
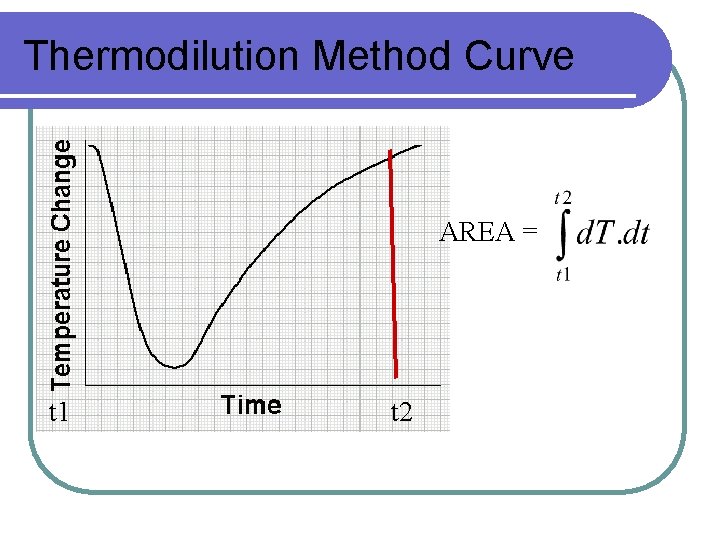
Thermodilution Method Curve AREA = t 1 t 2
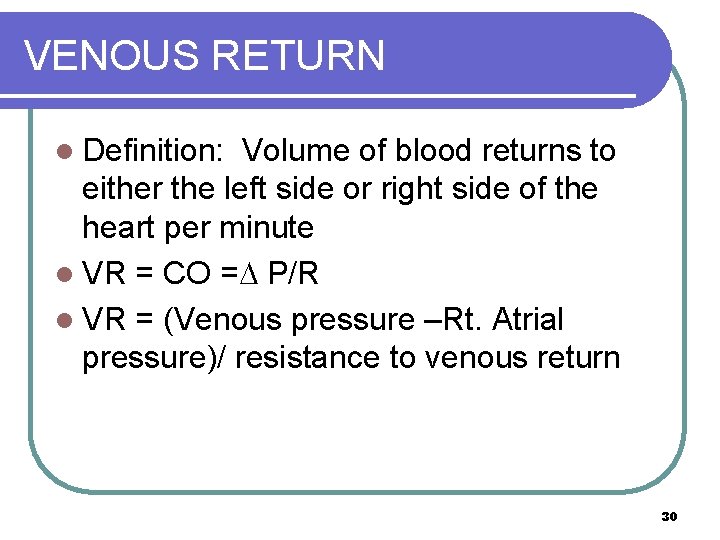
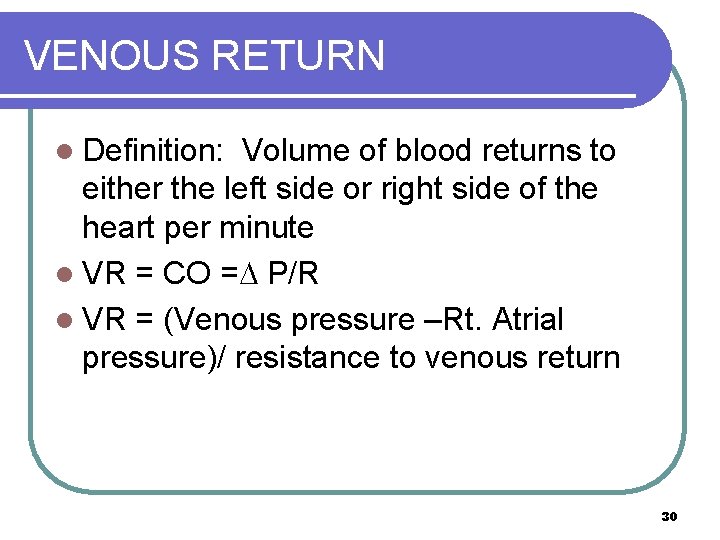
VENOUS RETURN l Definition: Volume of blood returns to either the left side or right side of the heart per minute l VR = CO = P/R l VR = (Venous pressure –Rt. Atrial pressure)/ resistance to venous return 30
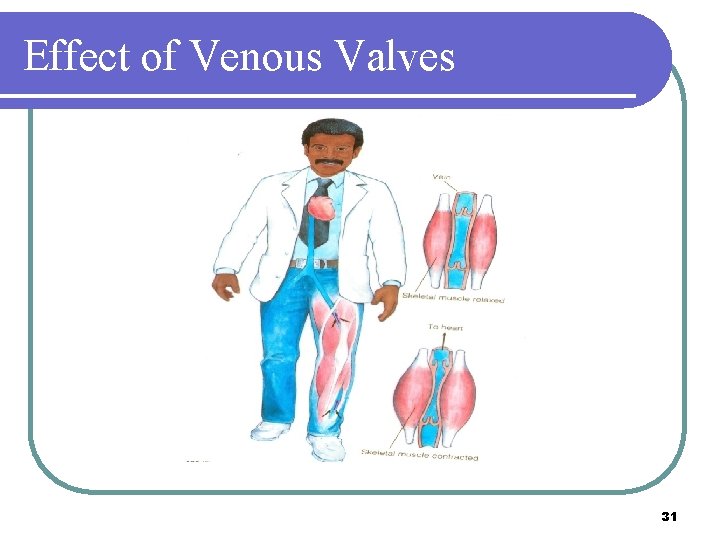
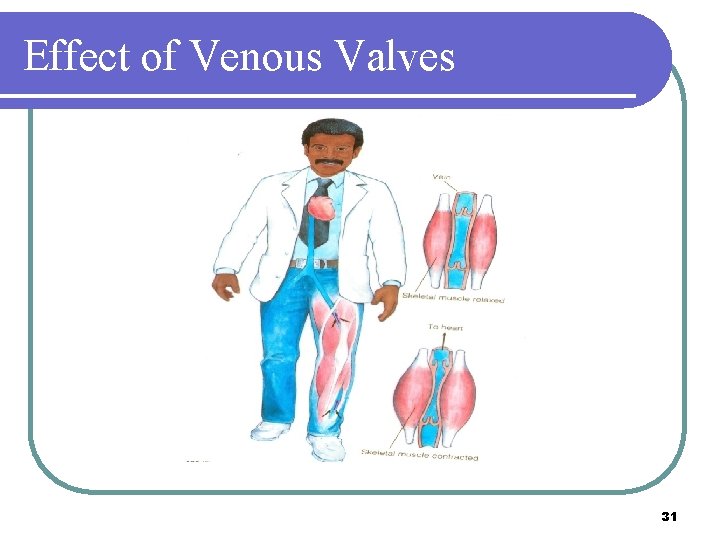
Effect of Venous Valves 31
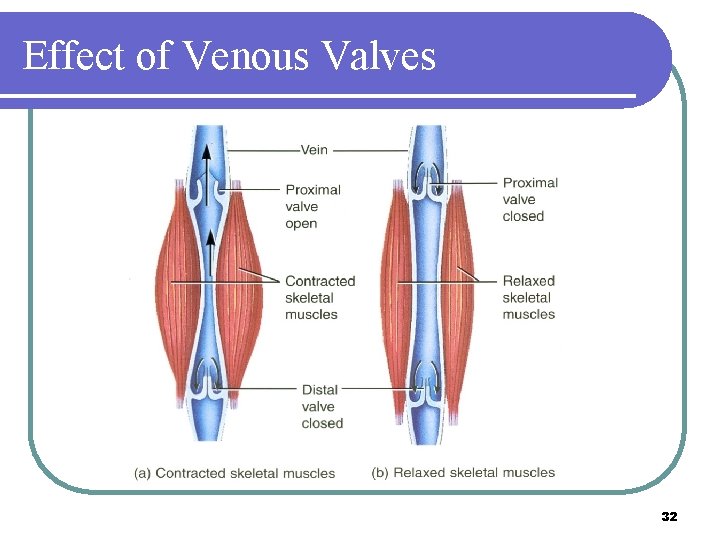
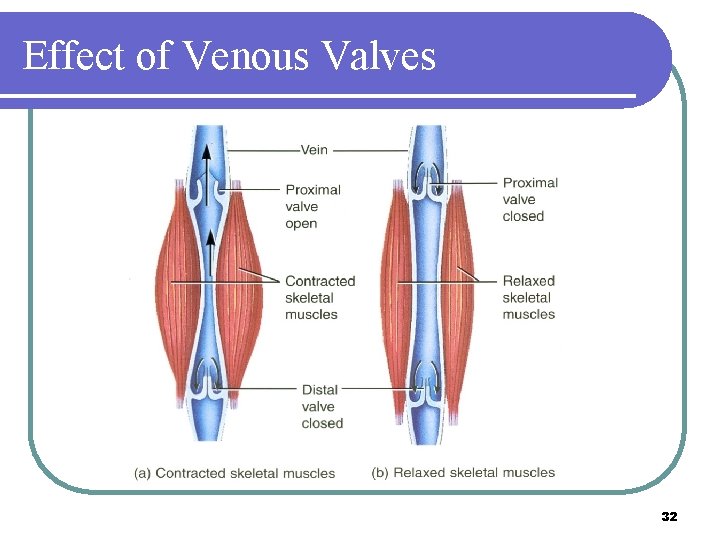
Effect of Venous Valves 32
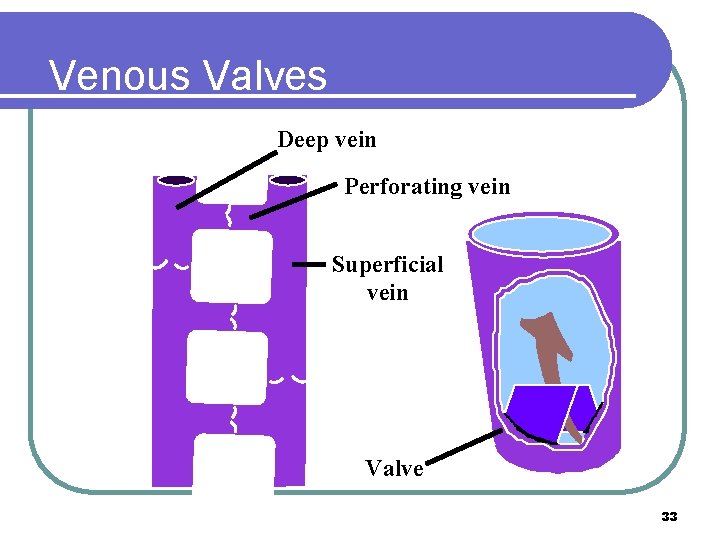
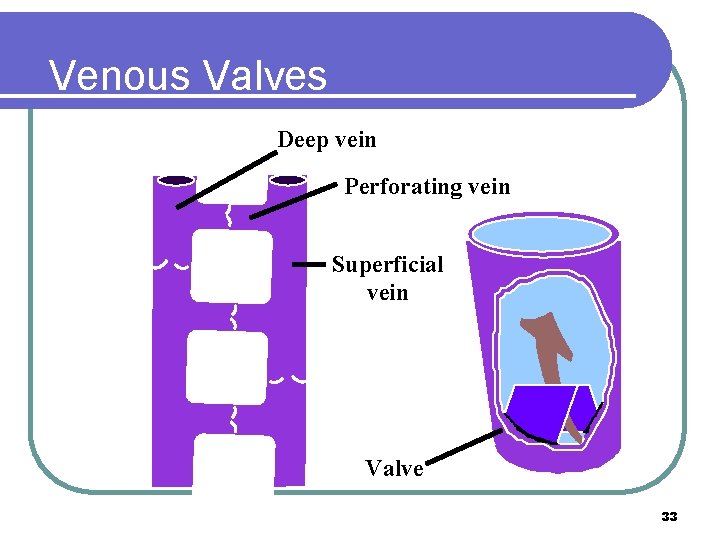
Venous Valves Deep vein Perforating vein Superficial vein Valve 33
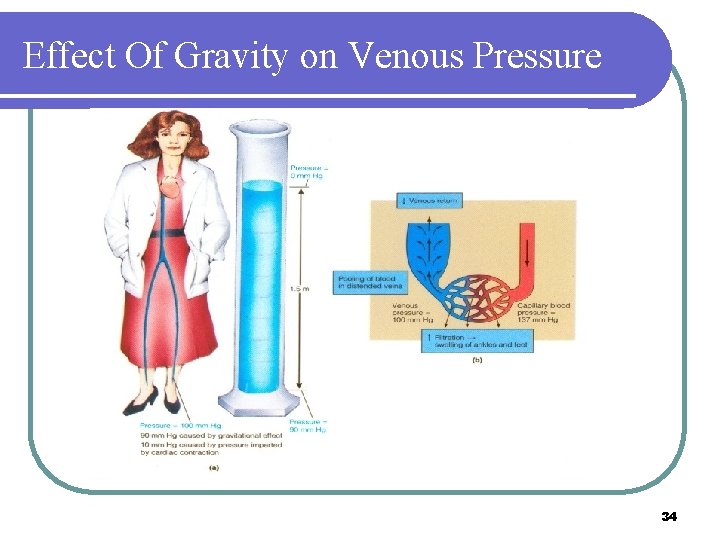
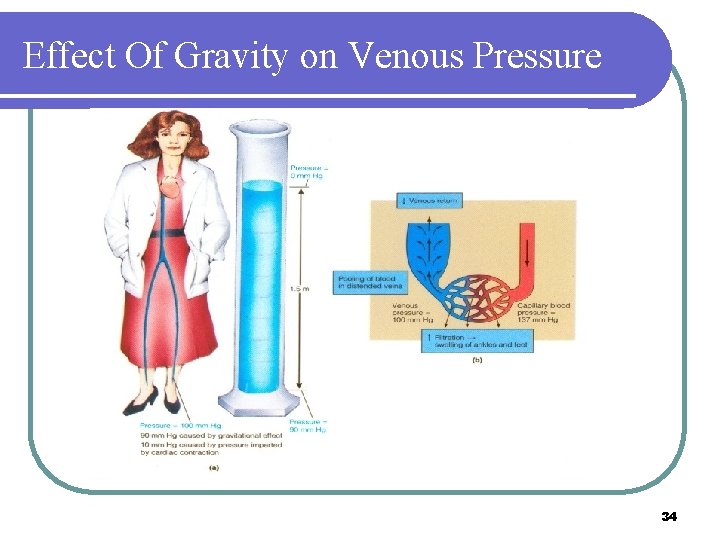
Effect Of Gravity on Venous Pressure 34

Venous Pressure in the Body • Compressional factors tend to cause resistance to flow in large peripheral veins. • Increases in right atrial pressure causes blood to back up into the venous system thereby increasing venous pressures. • Abdominal pressures tend to increase venous pressures in the legs. 35
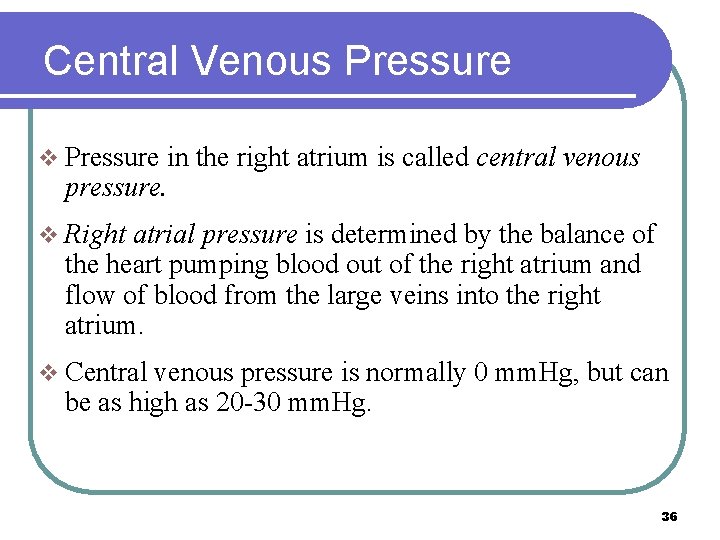
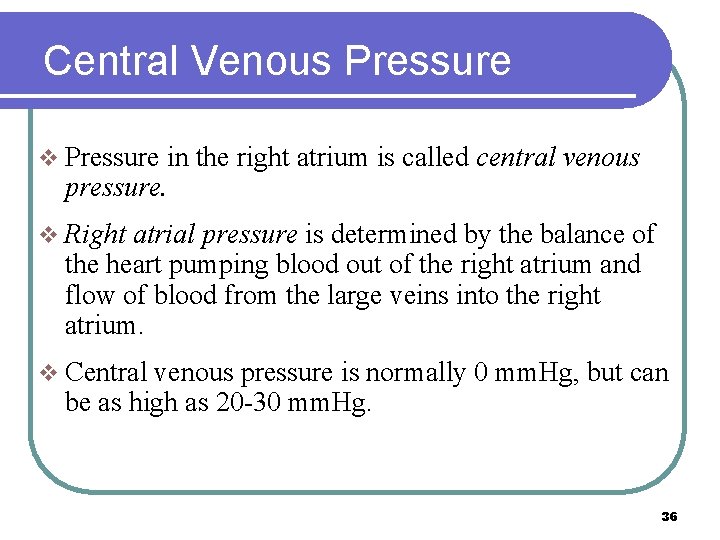
Central Venous Pressure v Pressure in the right atrium is called central venous pressure. v Right atrial pressure is determined by the balance of the heart pumping blood out of the right atrium and flow of blood from the large veins into the right atrium. v Central venous pressure is normally 0 mm. Hg, but can be as high as 20 -30 mm. Hg. 36
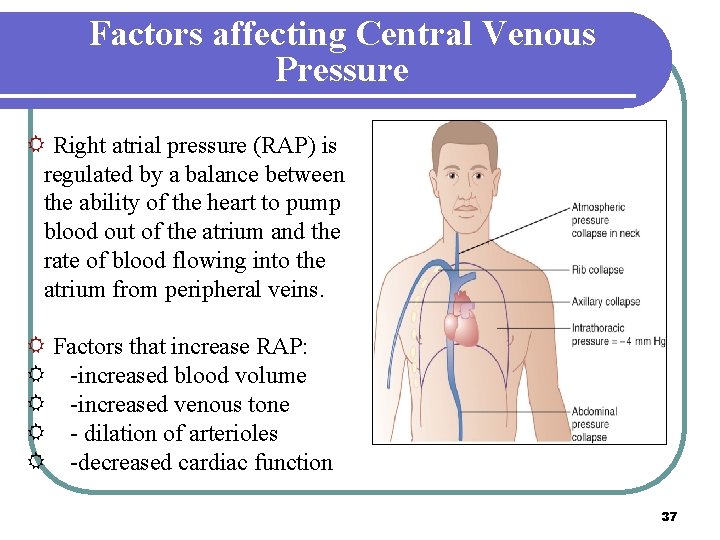
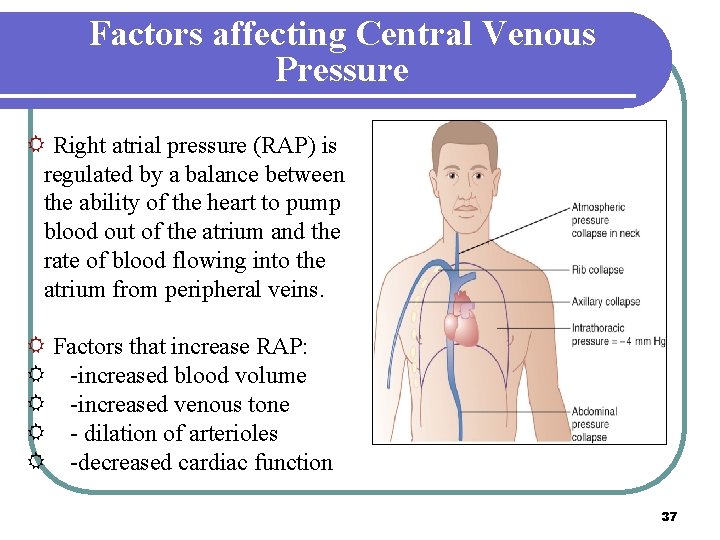
Factors affecting Central Venous Pressure R Right atrial pressure (RAP) is regulated by a balance between the ability of the heart to pump blood out of the atrium and the rate of blood flowing into the atrium from peripheral veins. R Factors that increase RAP: R -increased blood volume R -increased venous tone R - dilation of arterioles R -decreased cardiac function 37

Factors that Facilitate Venous Return 38
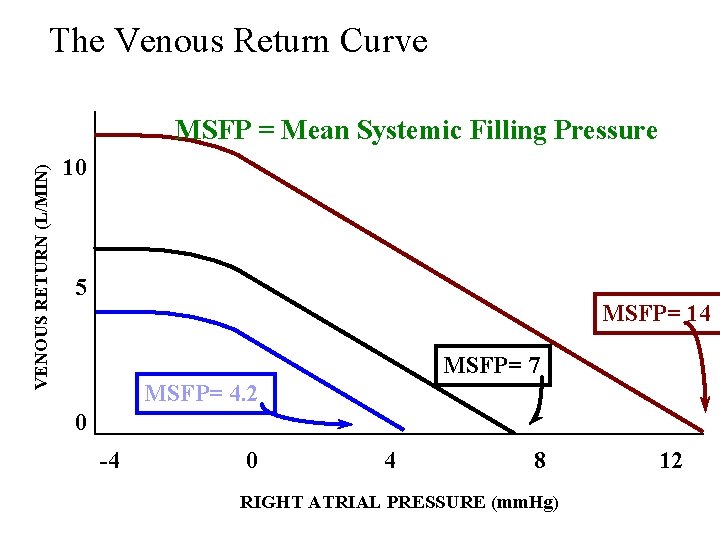
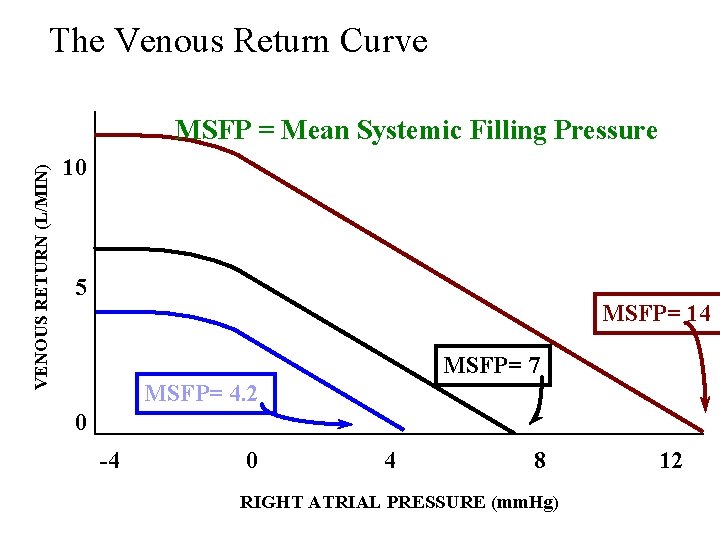
The Venous Return Curve VENOUS RETURN (L/MIN) MSFP = Mean Systemic Filling Pressure 10 5 MSFP= 14 MSFP= 7 MSFP= 4. 2 0 -4 0 4 8 RIGHT ATRIAL PRESSURE (mm. Hg) 12
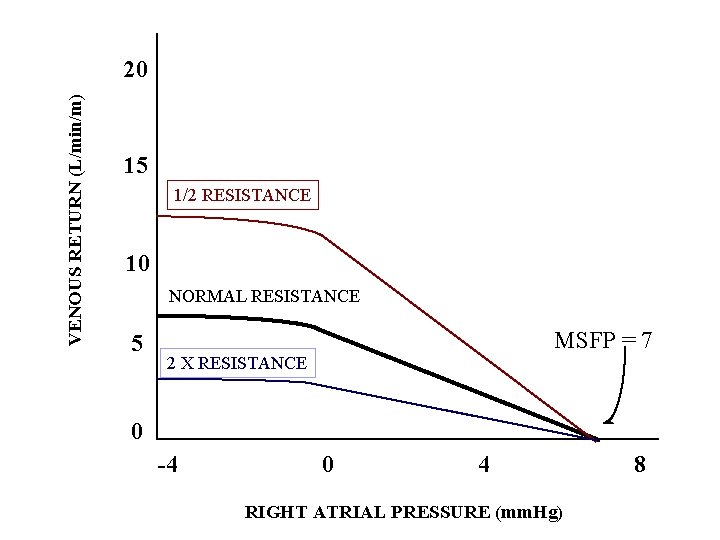
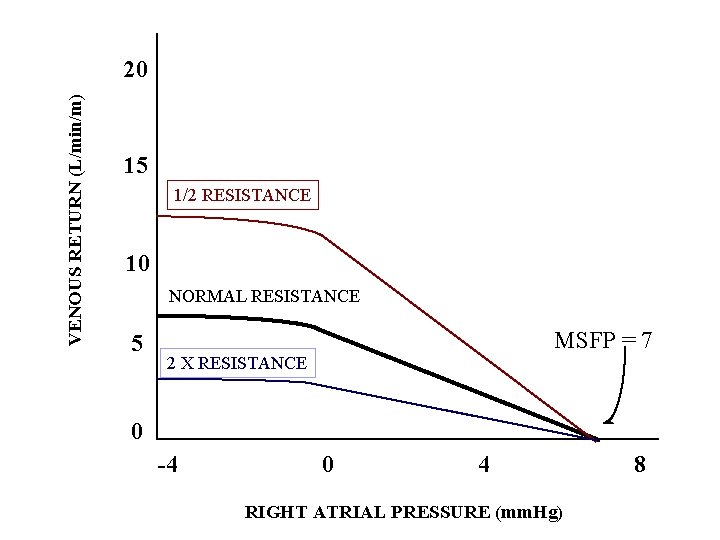
VENOUS RETURN (L/min/m) 20 15 1/2 RESISTANCE 10 NORMAL RESISTANCE 5 MSFP = 7 2 X RESISTANCE 0 -4 0 4 RIGHT ATRIAL PRESSURE (mm. Hg) 8
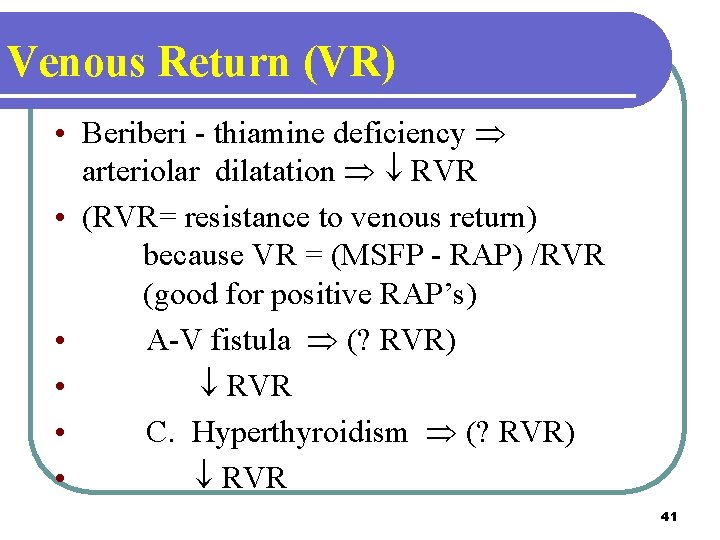
Venous Return (VR) • Beriberi - thiamine deficiency Þ arteriolar dilatation Þ ¯ RVR • (RVR= resistance to venous return) because VR = (MSFP - RAP) /RVR (good for positive RAP’s) • A-V fistula Þ (? RVR) • ¯ RVR • C. Hyperthyroidism Þ (? RVR) • ¯ RVR 41

Venous Return (VR) (cont’d) • • • Anemia Þ ¯ RVR (why? ) Sympathetics Þ MSFP Blood volume Þ MSFP + small ¯ in RVR ¯ Venous compliance (muscle contraction or venous constriction) Þ (? MSFP) MSFP 42
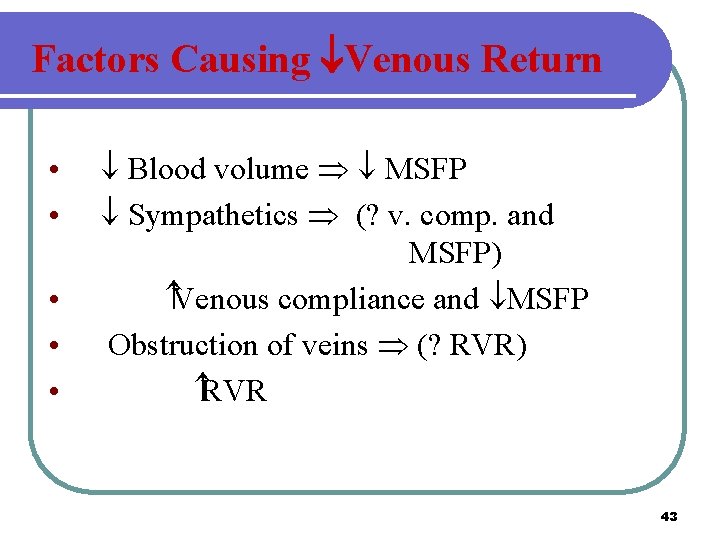
Factors Causing Venous Return • • • ¯ Blood volume Þ ¯ MSFP ¯ Sympathetics Þ (? v. comp. and MSFP) Venous compliance and ¯MSFP Obstruction of veins Þ (? RVR) RVR 43

CARDIAC OUTPUT AND VENOUS RETURN (L/min/m) 25 MAXIMAL SYMPATHETIC STIMULATION 20 15 10 5 NORMAL CARDIAC SPINAL ANESTHESIA MAX SYM SPINAL VR AN CU R VE ES T HE S IA 0 -4 0 4 NO PAT HET RM AL 8 IC S TIM ULA TIO N 12 RIGHT ATRIAL PRESSURE (mm. Hg) 16
Thank You