CARDIAC MUSCLE Atrial muscles Ventricular muscles Specialized conductive

- Slides: 27

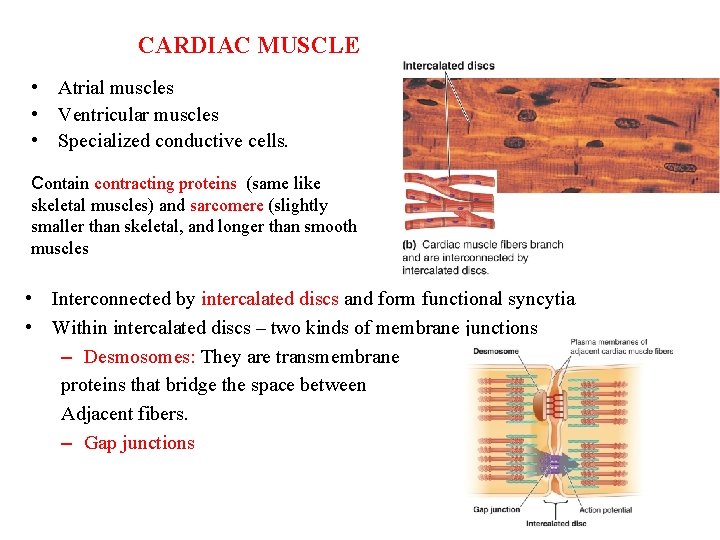
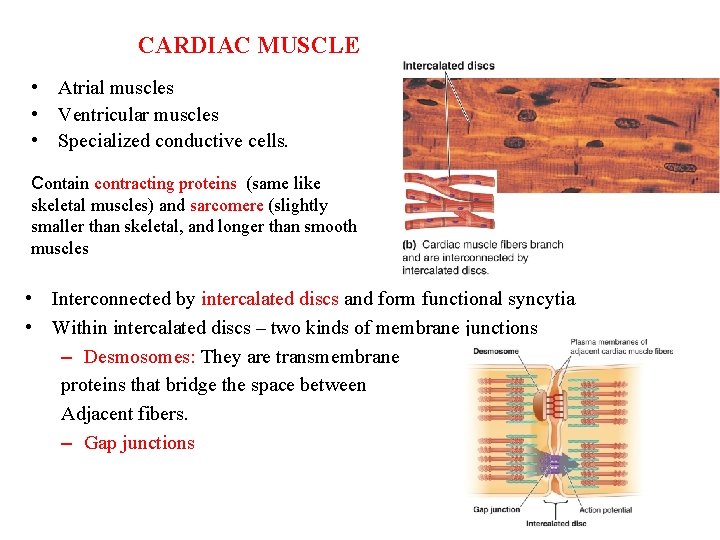
CARDIAC MUSCLE • Atrial muscles • Ventricular muscles • Specialized conductive cells. Contain contracting proteins (same like skeletal muscles) and sarcomere (slightly smaller than skeletal, and longer than smooth muscles • Interconnected by intercalated discs and form functional syncytia • Within intercalated discs – two kinds of membrane junctions – Desmosomes: They are transmembrane proteins that bridge the space between Adjacent fibers. – Gap junctions
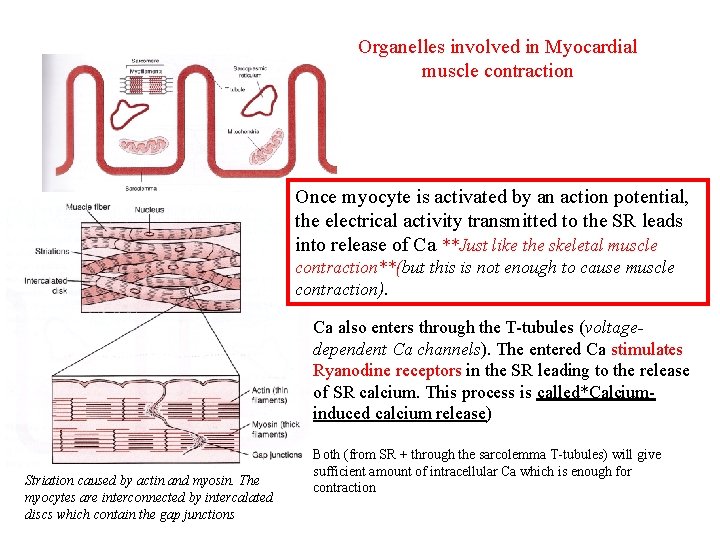
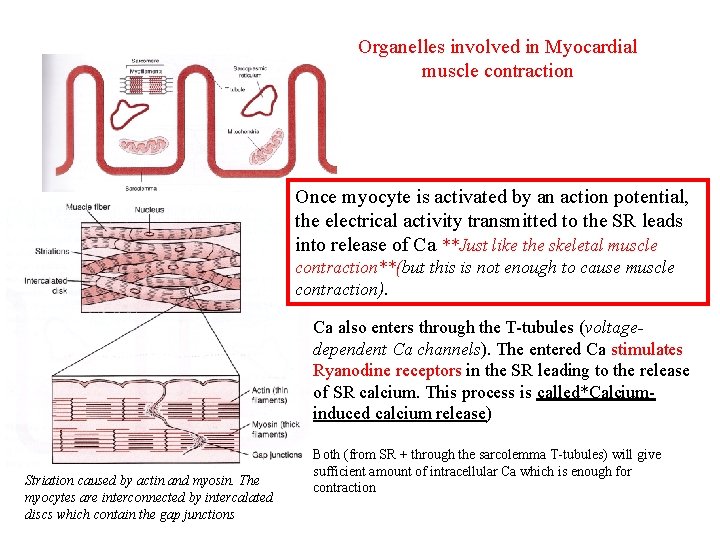
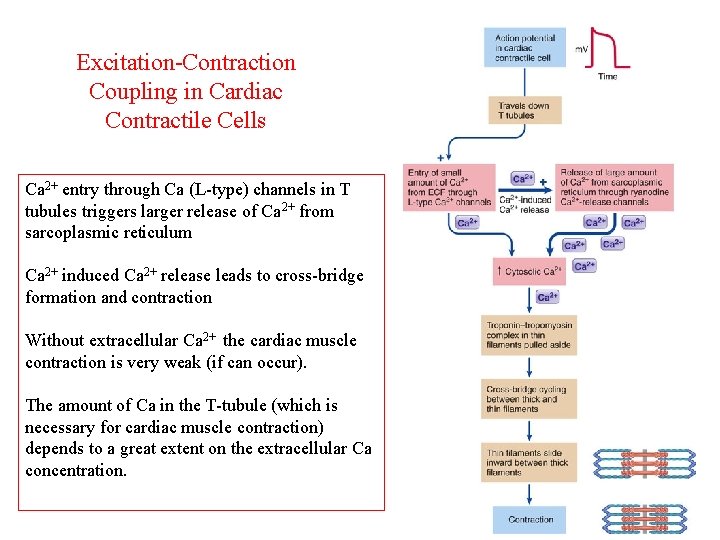
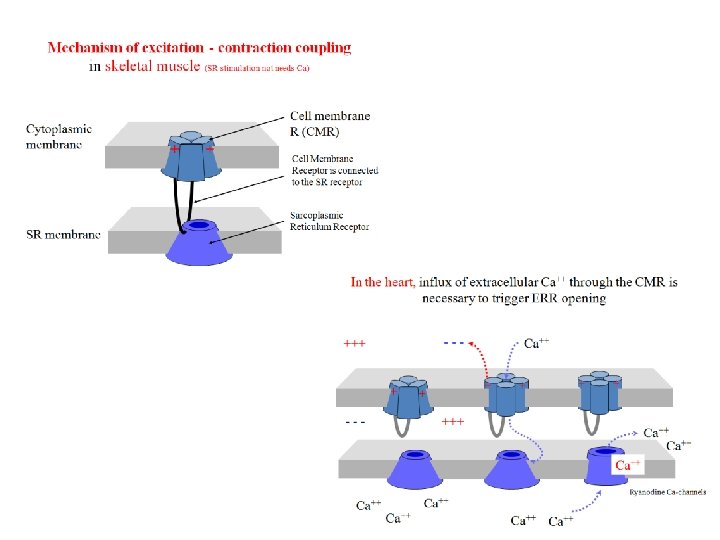
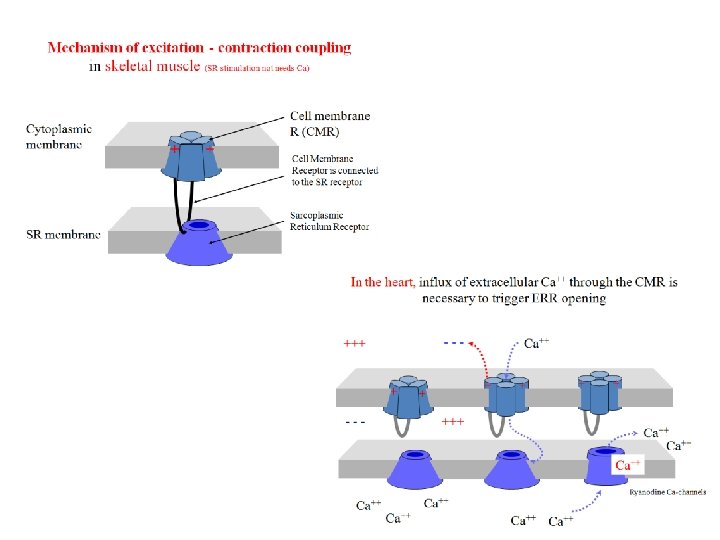
Organelles involved in Myocardial muscle contraction Once myocyte is activated by an action potential, the electrical activity transmitted to the SR leads into release of Ca **Just like the skeletal muscle contraction**(but this is not enough to cause muscle contraction). Ca also enters through the T-tubules (voltagedependent Ca channels). The entered Ca stimulates Ryanodine receptors in the SR leading to the release of SR calcium. This process is called*Calciuminduced calcium release) Striation caused by actin and myosin. The myocytes are interconnected by intercalated discs which contain the gap junctions Both (from SR + through the sarcolemma T-tubules) will give sufficient amount of intracellular Ca which is enough for contraction
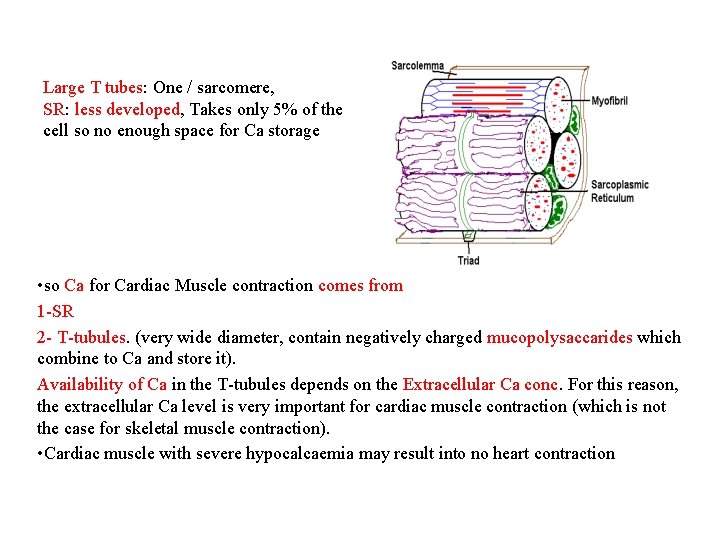
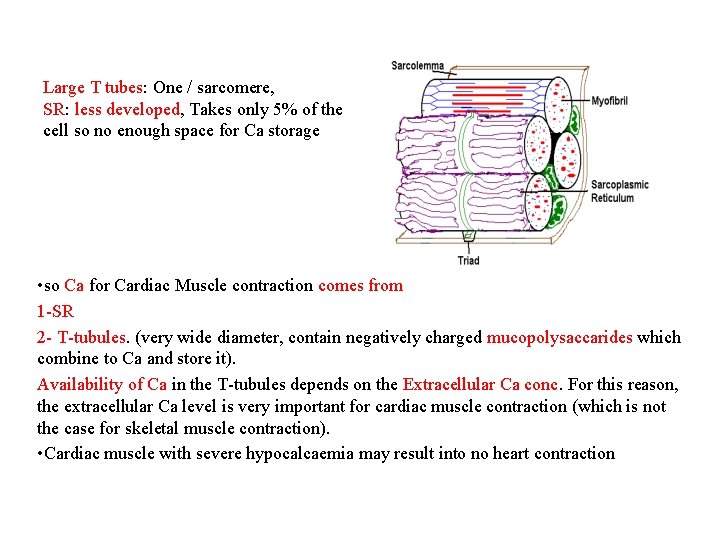
Large T tubes: One / sarcomere, SR: less developed, Takes only 5% of the cell so no enough space for Ca storage • so Ca for Cardiac Muscle contraction comes from 1 -SR 2 - T-tubules. (very wide diameter, contain negatively charged mucopolysaccarides which combine to Ca and store it). Availability of Ca in the T-tubules depends on the Extracellular Ca conc. For this reason, the extracellular Ca level is very important for cardiac muscle contraction (which is not the case for skeletal muscle contraction). • Cardiac muscle with severe hypocalcaemia may result into no heart contraction
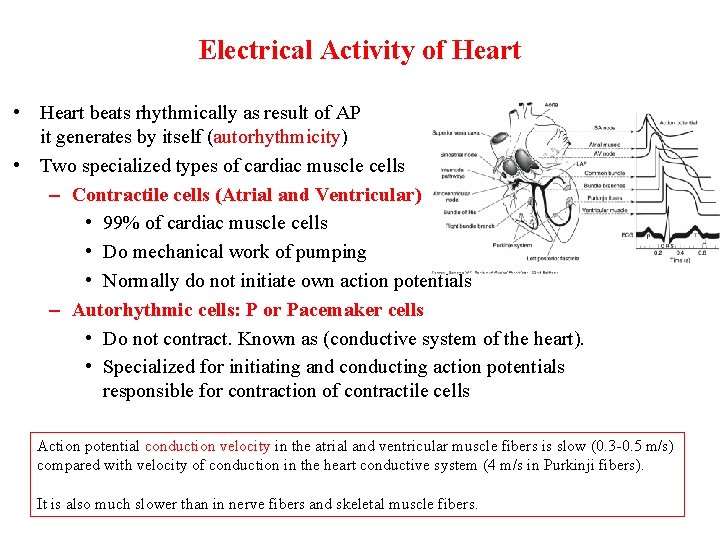
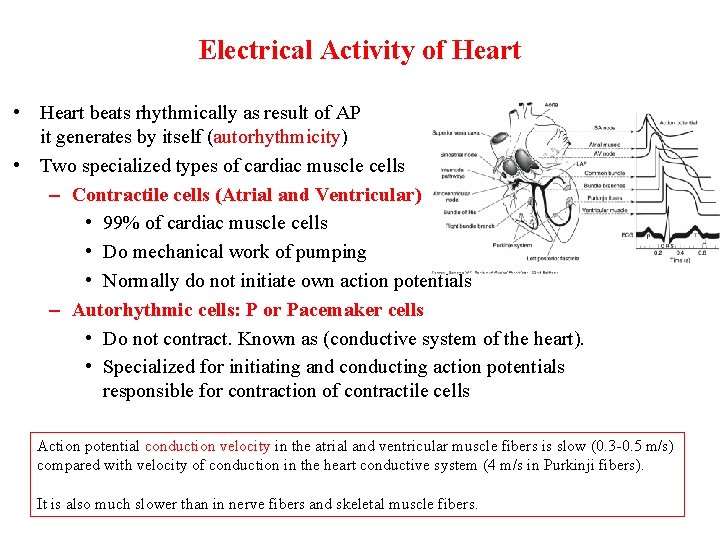
Electrical Activity of Heart • Heart beats rhythmically as result of AP it generates by itself (autorhythmicity) • Two specialized types of cardiac muscle cells – Contractile cells (Atrial and Ventricular) • 99% of cardiac muscle cells • Do mechanical work of pumping • Normally do not initiate own action potentials – Autorhythmic cells: P or Pacemaker cells • Do not contract. Known as (conductive system of the heart). • Specialized for initiating and conducting action potentials responsible for contraction of contractile cells Action potential conduction velocity in the atrial and ventricular muscle fibers is slow (0. 3 -0. 5 m/s) compared with velocity of conduction in the heart conductive system (4 m/s in Purkinji fibers). It is also much slower than in nerve fibers and skeletal muscle fibers.
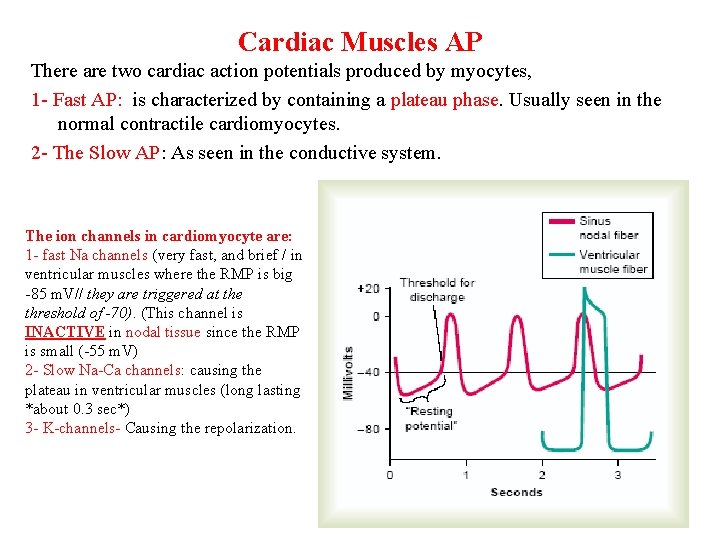
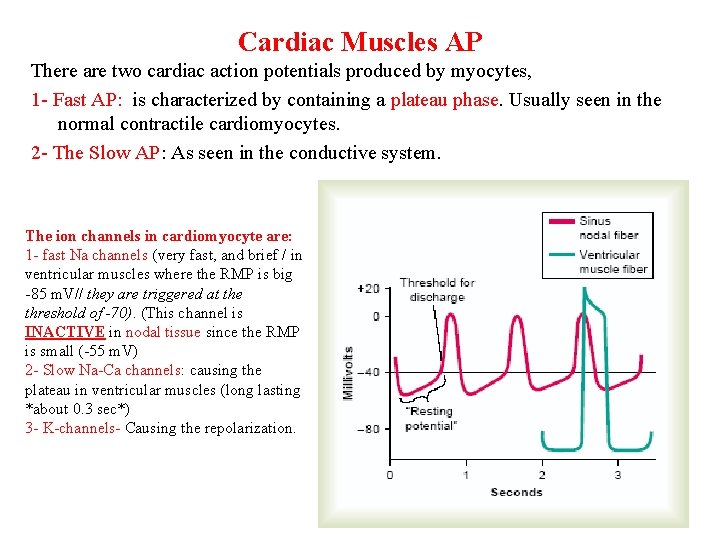
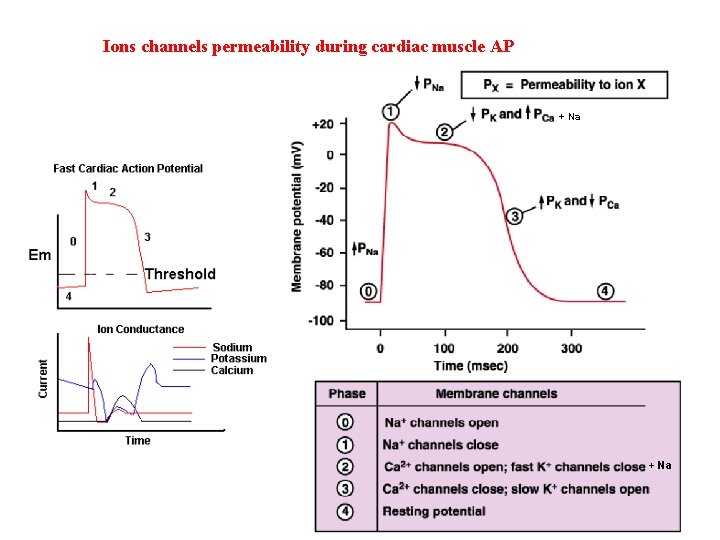
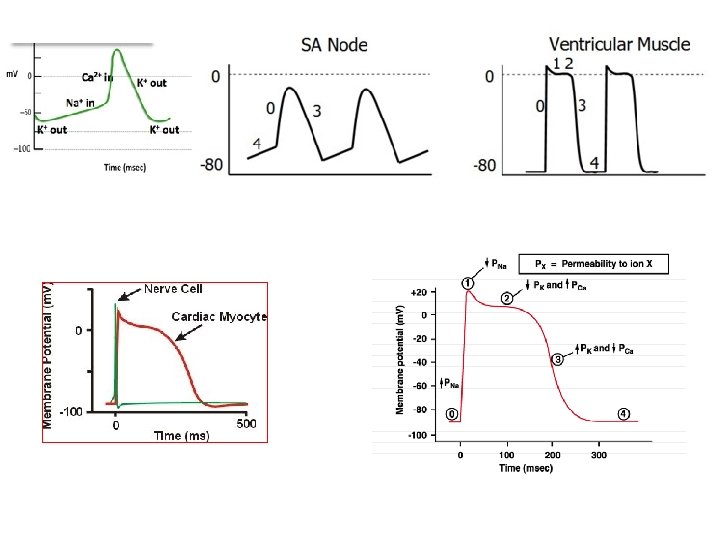
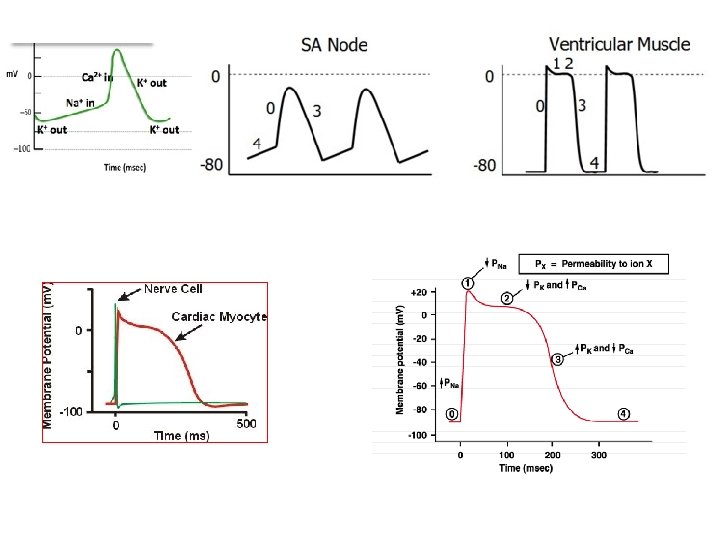
Cardiac Muscles AP There are two cardiac action potentials produced by myocytes, 1 - Fast AP: is characterized by containing a plateau phase. Usually seen in the normal contractile cardiomyocytes. 2 - The Slow AP: As seen in the conductive system. The ion channels in cardiomyocyte are: 1 - fast Na channels (very fast, and brief / in ventricular muscles where the RMP is big -85 m. V// they are triggered at the threshold of -70). (This channel is INACTIVE in nodal tissue since the RMP is small (-55 m. V) 2 - Slow Na-Ca channels: causing the plateau in ventricular muscles (long lasting *about 0. 3 sec*) 3 - K-channels- Causing the repolarization.
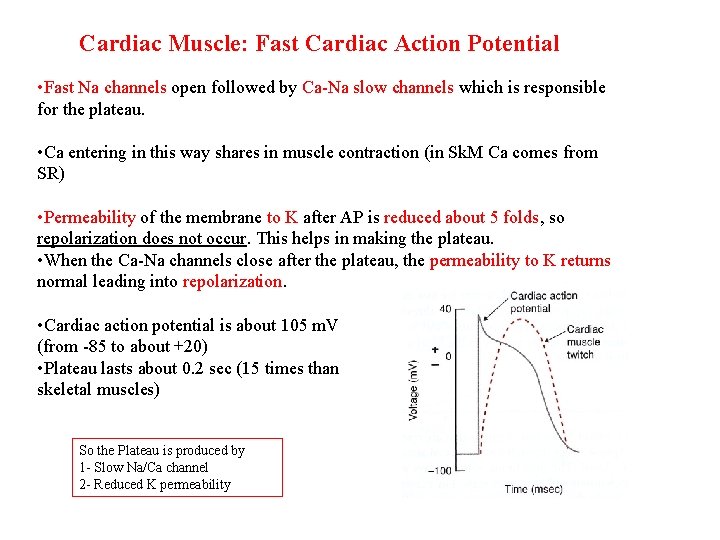
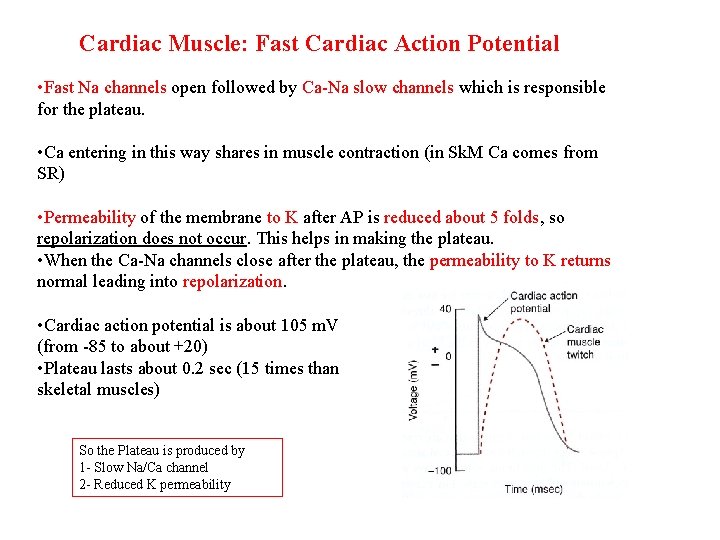
Cardiac Muscle: Fast Cardiac Action Potential • Fast Na channels open followed by Ca-Na slow channels which is responsible for the plateau. • Ca entering in this way shares in muscle contraction (in Sk. M Ca comes from SR) • Permeability of the membrane to K after AP is reduced about 5 folds, so repolarization does not occur. This helps in making the plateau. • When the Ca-Na channels close after the plateau, the permeability to K returns normal leading into repolarization. • Cardiac action potential is about 105 m. V (from -85 to about +20) • Plateau lasts about 0. 2 sec (15 times than skeletal muscles) So the Plateau is produced by 1 - Slow Na/Ca channel 2 - Reduced K permeability
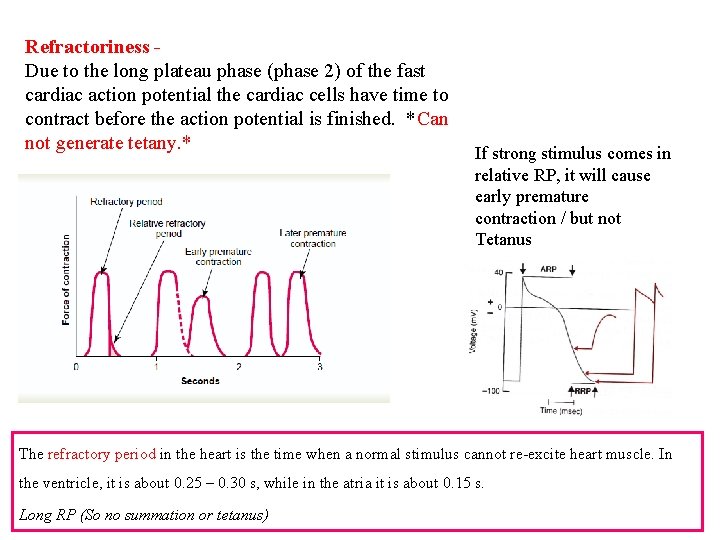
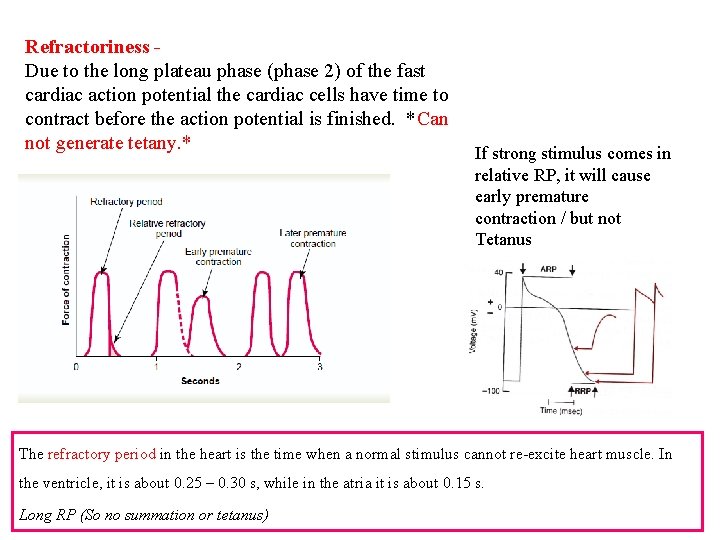
Refractoriness Due to the long plateau phase (phase 2) of the fast cardiac action potential the cardiac cells have time to contract before the action potential is finished. *Can not generate tetany. * If strong stimulus comes in relative RP, it will cause early premature contraction / but not Tetanus The refractory period in the heart is the time when a normal stimulus cannot re-excite heart muscle. In the ventricle, it is about 0. 25 – 0. 30 s, while in the atria it is about 0. 15 s. Long RP (So no summation or tetanus)
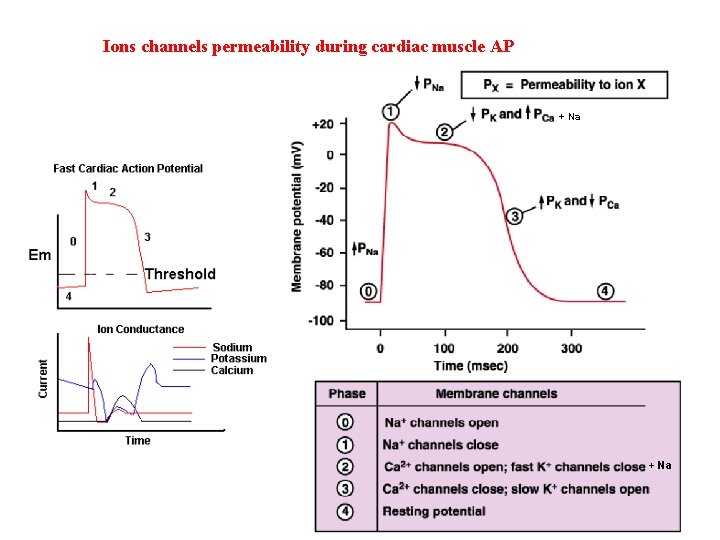
Ions channels permeability during cardiac muscle AP + Na
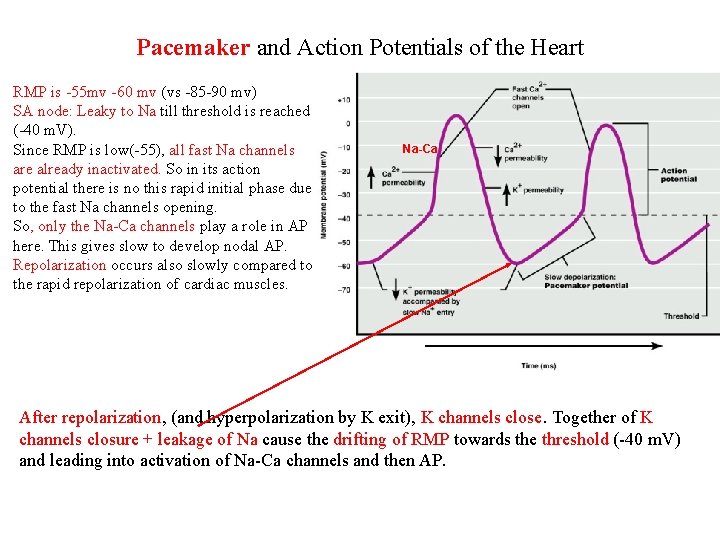
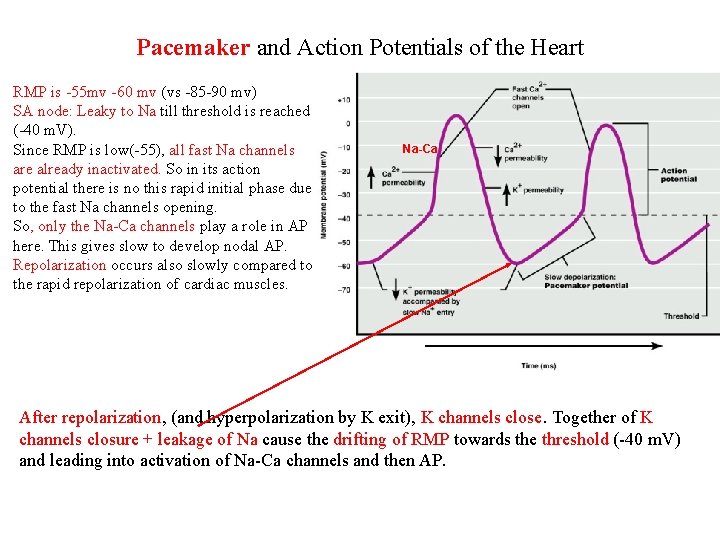
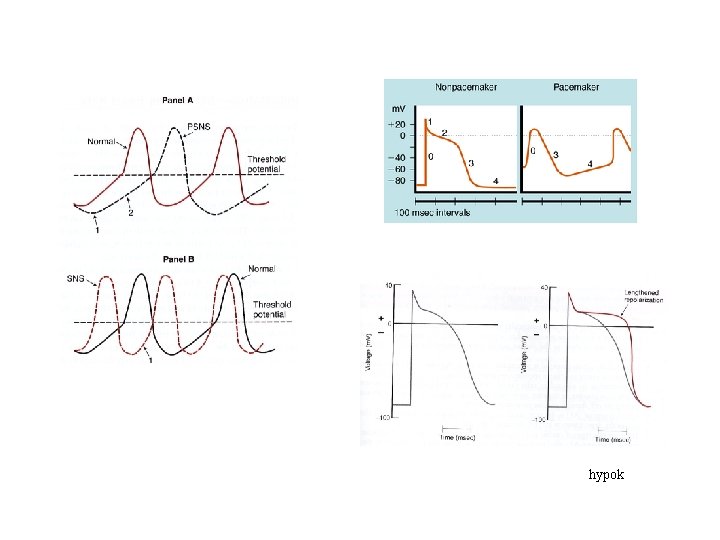
Pacemaker and Action Potentials of the Heart RMP is -55 mv -60 mv (vs -85 -90 mv) SA node: Leaky to Na till threshold is reached (-40 m. V). Since RMP is low(-55), all fast Na channels are already inactivated. So in its action potential there is no this rapid initial phase due to the fast Na channels opening. So, only the Na-Ca channels play a role in AP here. This gives slow to develop nodal AP. Repolarization occurs also slowly compared to the rapid repolarization of cardiac muscles. Na-Ca After repolarization, (and hyperpolarization by K exit), K channels close. Together of K channels closure + leakage of Na cause the drifting of RMP towards the threshold (-40 m. V) and leading into activation of Na-Ca channels and then AP.
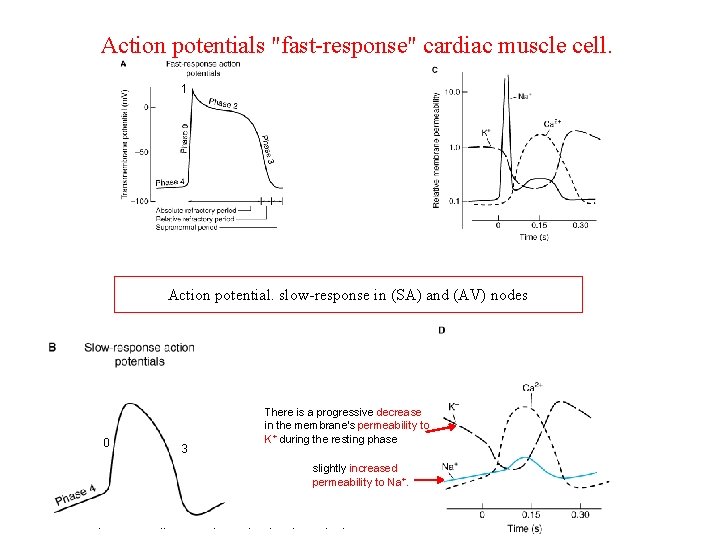
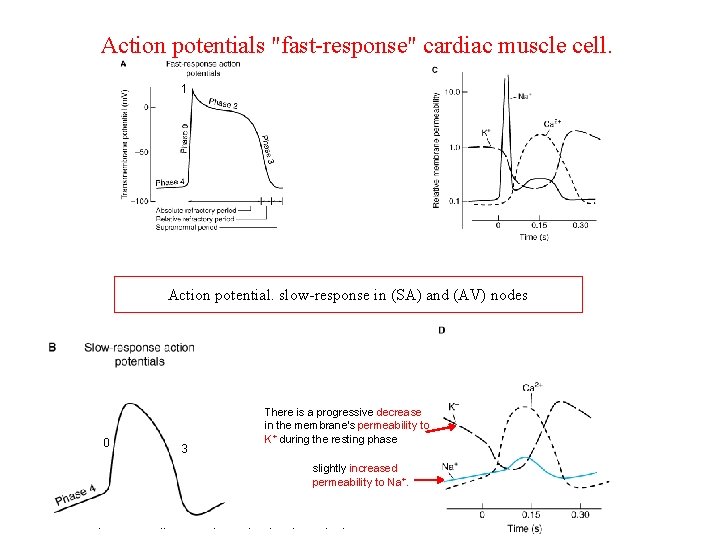
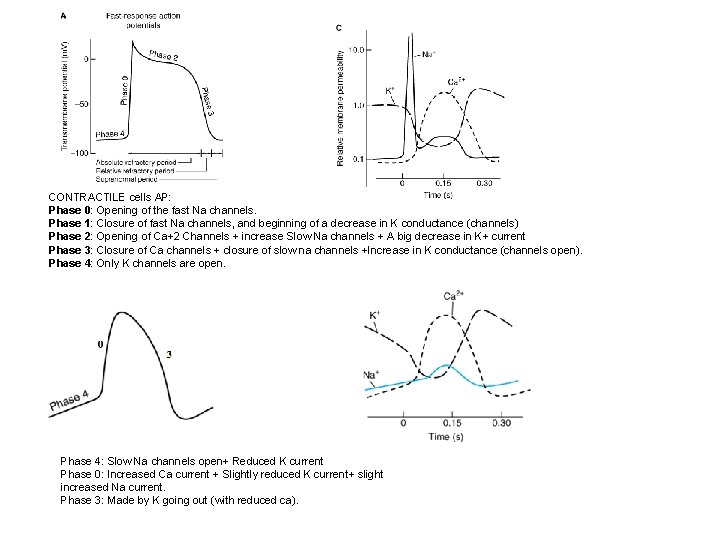
Action potentials "fast-response" cardiac muscle cell. 1 Action potential. slow-response in (SA) and (AV) nodes 0 3 There is a progressive decrease in the membrane's permeability to K+ during the resting phase slightly increased permeability to Na+.
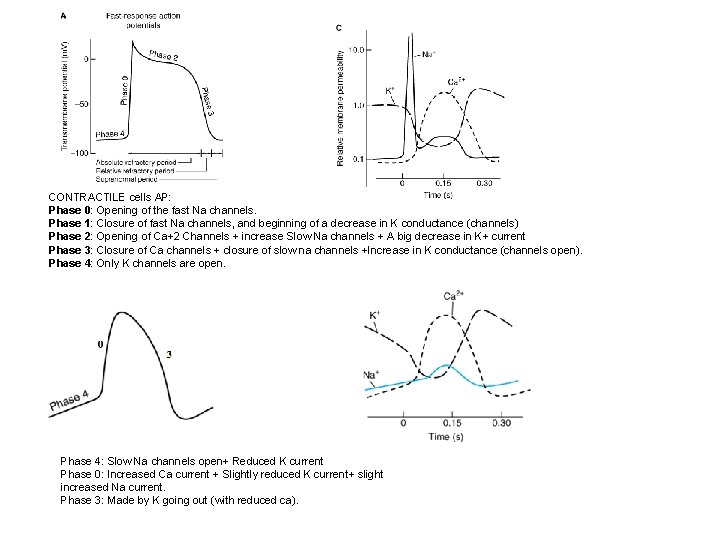
CONTRACTILE cells AP: Phase 0: Opening of the fast Na channels. Phase 1: Closure of fast Na channels, and beginning of a decrease in K conductance (channels) Phase 2: Opening of Ca+2 Channels + increase Slow Na channels + A big decrease in K+ current Phase 3: Closure of Ca channels + closure of slow na channels +Increase in K conductance (channels open). Phase 4: Only K channels are open. Phase 4: Slow Na channels open+ Reduced K current Phase 0: Increased Ca current + Slightly reduced K current+ slight increased Na current. Phase 3: Made by K going out (with reduced ca).
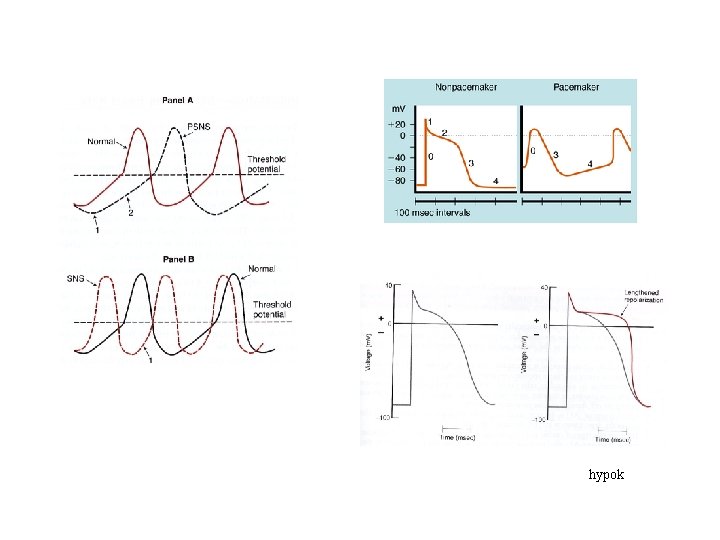
hypok
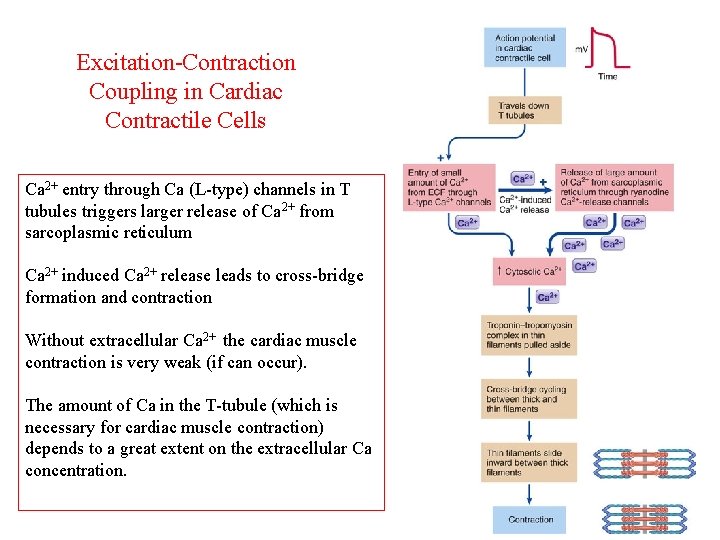
Excitation-Contraction Coupling in Cardiac Contractile Cells Ca 2+ entry through Ca (L-type) channels in T tubules triggers larger release of Ca 2+ from sarcoplasmic reticulum Ca 2+ induced Ca 2+ release leads to cross-bridge formation and contraction Without extracellular Ca 2+ the cardiac muscle contraction is very weak (if can occur). The amount of Ca in the T-tubule (which is necessary for cardiac muscle contraction) depends to a great extent on the extracellular Ca concentration.
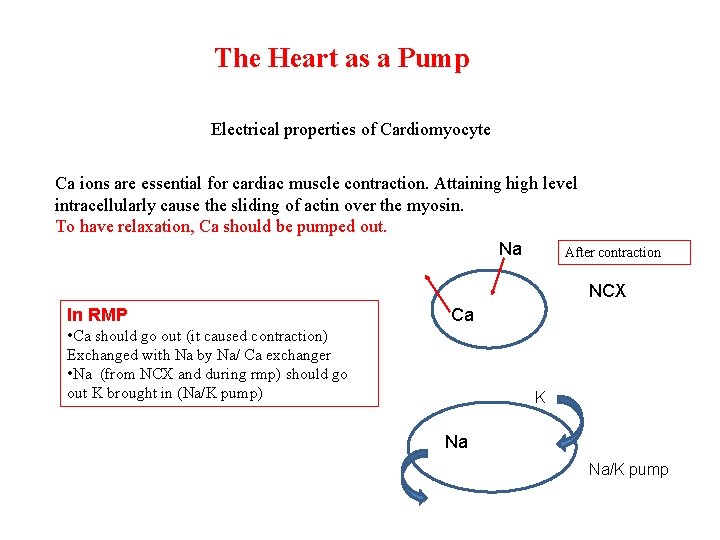
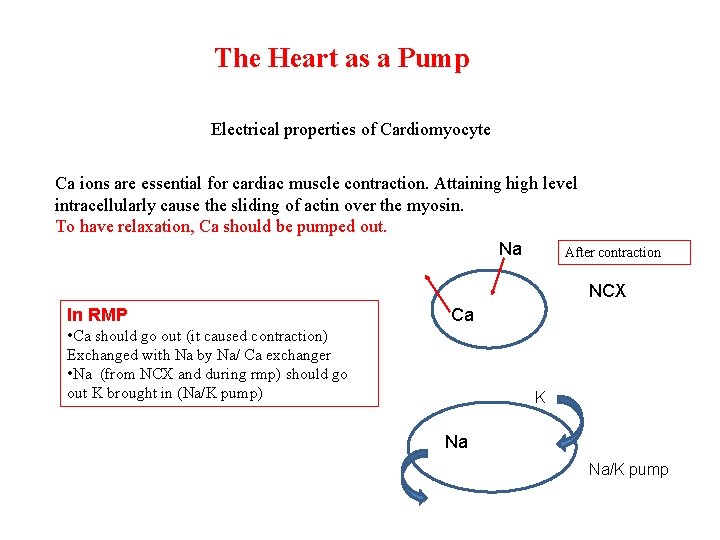
The Heart as a Pump Electrical properties of Cardiomyocyte Ca ions are essential for cardiac muscle contraction. Attaining high level intracellularly cause the sliding of actin over the myosin. To have relaxation, Ca should be pumped out. Na After contraction NCX In RMP Ca • Ca should go out (it caused contraction) Exchanged with Na by Na/ Ca exchanger • Na (from NCX and during rmp) should go out K brought in (Na/K pump) K Na Na/K pump
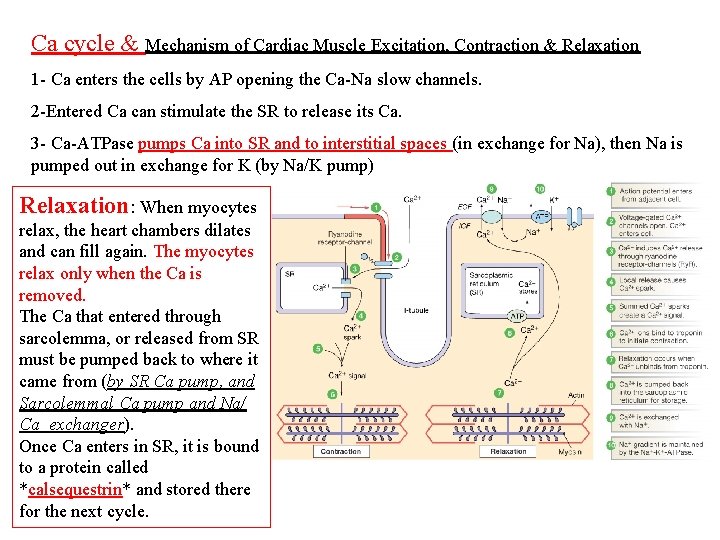
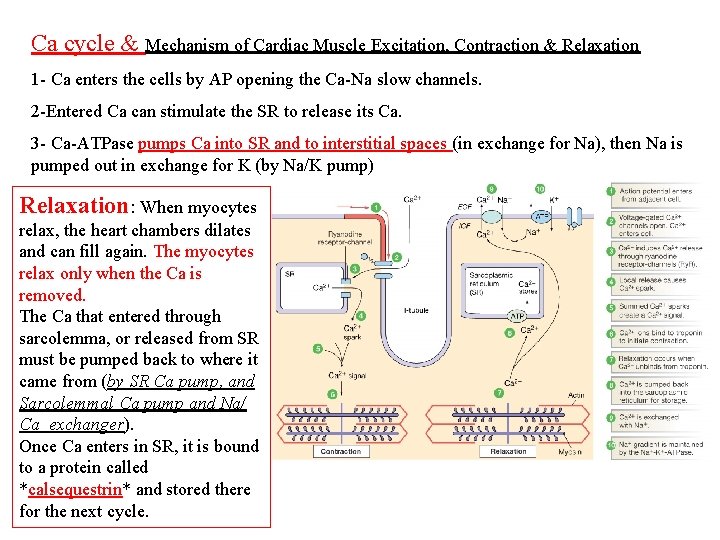
Ca cycle & Mechanism of Cardiac Muscle Excitation, Contraction & Relaxation 1 - Ca enters the cells by AP opening the Ca-Na slow channels. 2 -Entered Ca can stimulate the SR to release its Ca. 3 - Ca-ATPase pumps Ca into SR and to interstitial spaces (in exchange for Na), then Na is pumped out in exchange for K (by Na/K pump) Relaxation: When myocytes relax, the heart chambers dilates and can fill again. The myocytes relax only when the Ca is removed. The Ca that entered through sarcolemma, or released from SR must be pumped back to where it came from (by SR Ca pump, and Sarcolemmal Ca pump and Na/ Ca exchanger). Once Ca enters in SR, it is bound to a protein called *calsequestrin* and stored there for the next cycle.
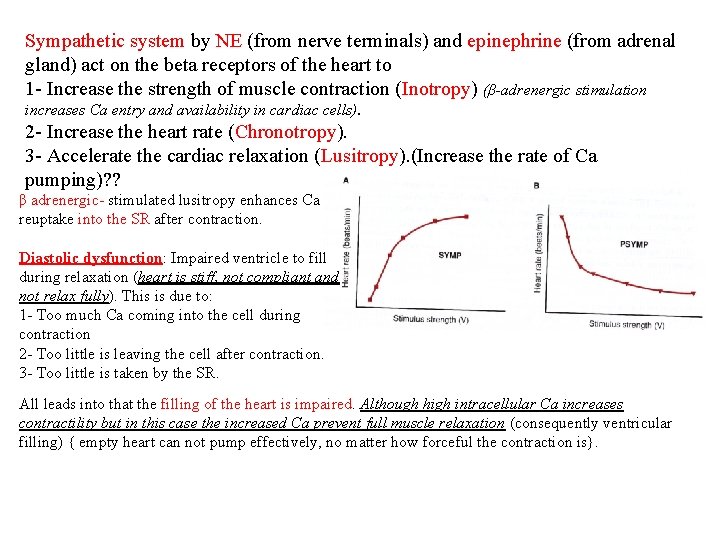
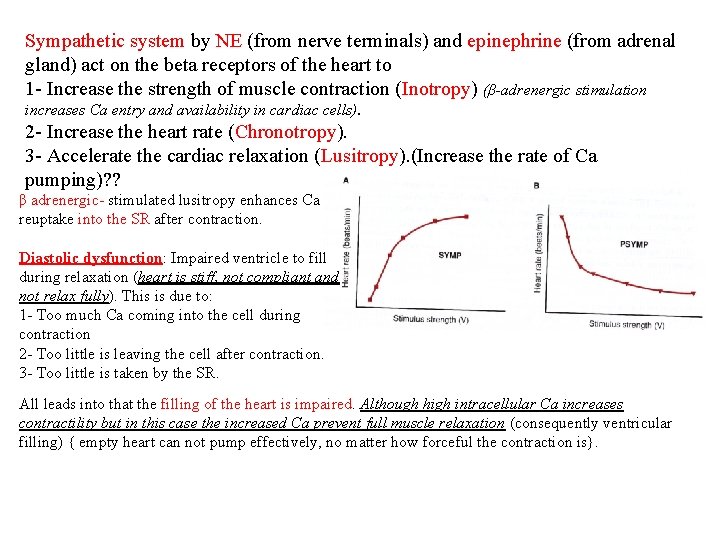
Sympathetic system by NE (from nerve terminals) and epinephrine (from adrenal gland) act on the beta receptors of the heart to 1 - Increase the strength of muscle contraction (Inotropy) (β-adrenergic stimulation increases Ca entry and availability in cardiac cells). 2 - Increase the heart rate (Chronotropy). 3 - Accelerate the cardiac relaxation (Lusitropy). (Increase the rate of Ca pumping)? ? β adrenergic- stimulated lusitropy enhances Ca reuptake into the SR after contraction. Diastolic dysfunction: Impaired ventricle to fill during relaxation (heart is stiff, not compliant and not relax fully). This is due to: 1 - Too much Ca coming into the cell during contraction 2 - Too little is leaving the cell after contraction. 3 - Too little is taken by the SR. All leads into that the filling of the heart is impaired. Although high intracellular Ca increases contractility but in this case the increased Ca prevent full muscle relaxation (consequently ventricular filling) { empty heart can not pump effectively, no matter how forceful the contraction is}.
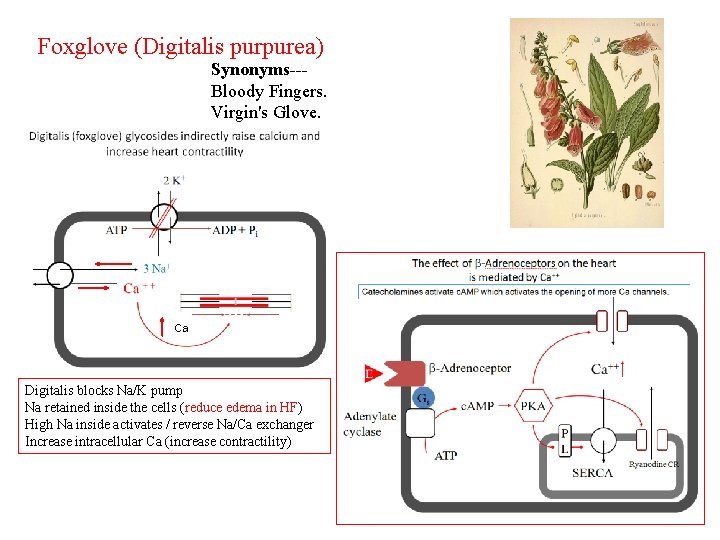
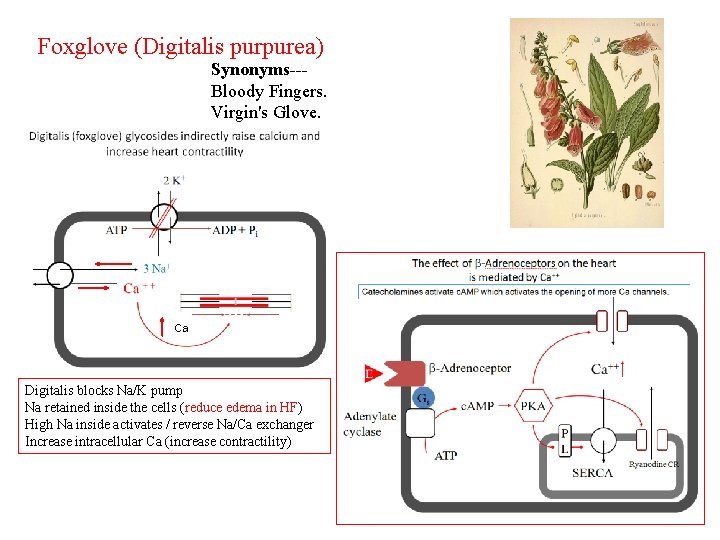
Foxglove (Digitalis purpurea) Synonyms--Bloody Fingers. Virgin's Glove. Ca Digitalis blocks Na/K pump Na retained inside the cells (reduce edema in HF) High Na inside activates / reverse Na/Ca exchanger Increase intracellular Ca (increase contractility)
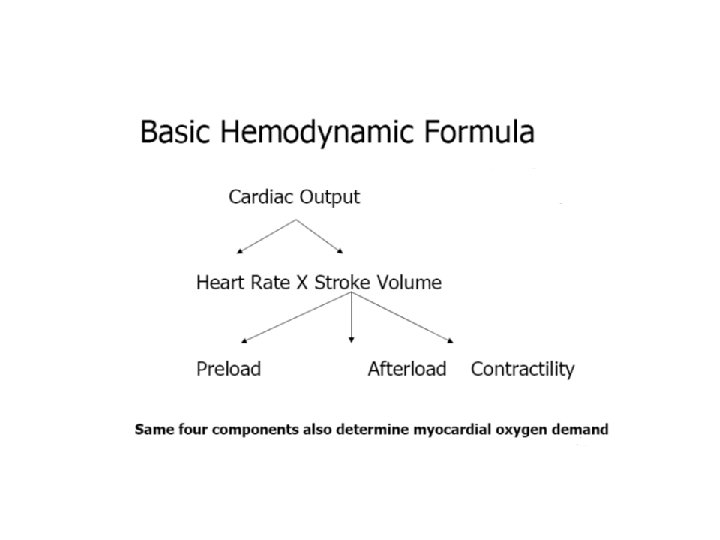
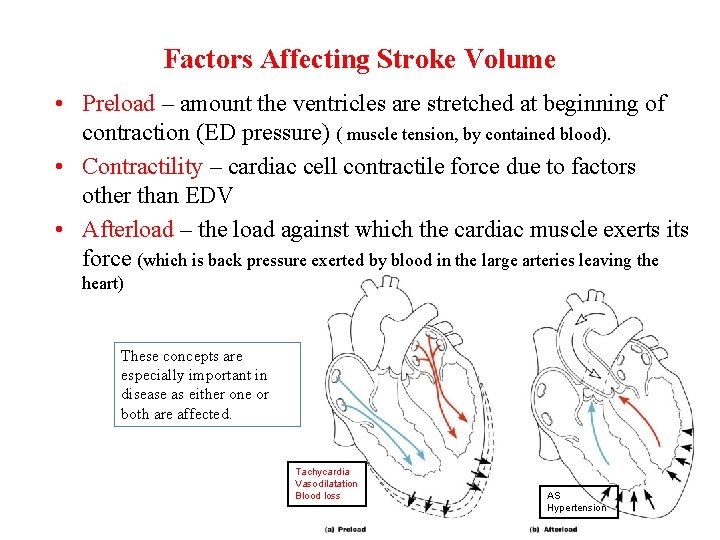
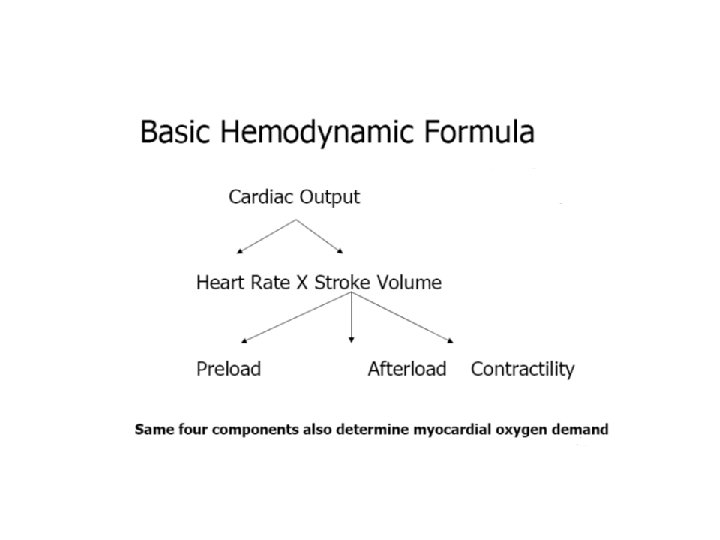
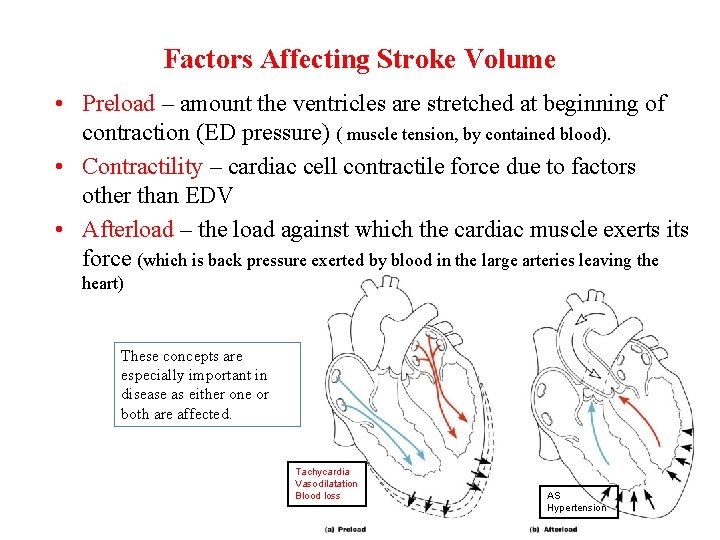
Factors Affecting Stroke Volume • Preload – amount the ventricles are stretched at beginning of contraction (ED pressure) ( muscle tension, by contained blood). • Contractility – cardiac cell contractile force due to factors other than EDV • Afterload – the load against which the cardiac muscle exerts its force (which is back pressure exerted by blood in the large arteries leaving the heart) These concepts are especially important in disease as either one or both are affected. Tachycardia Vasodilatation Blood loss AS Hypertension
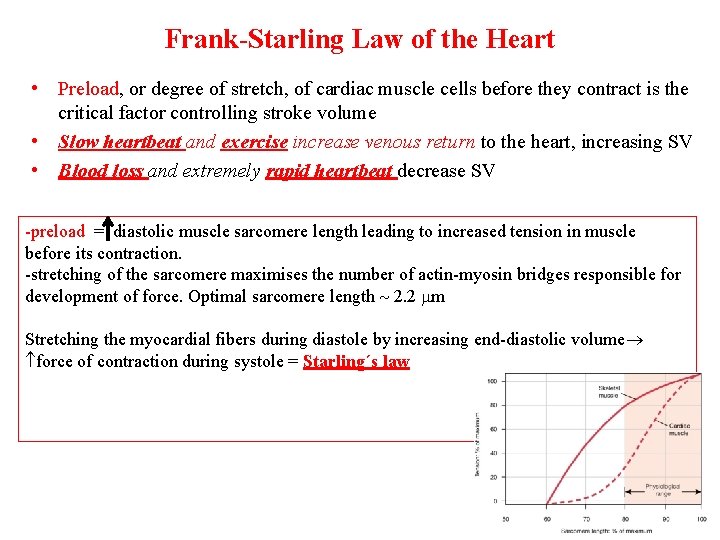
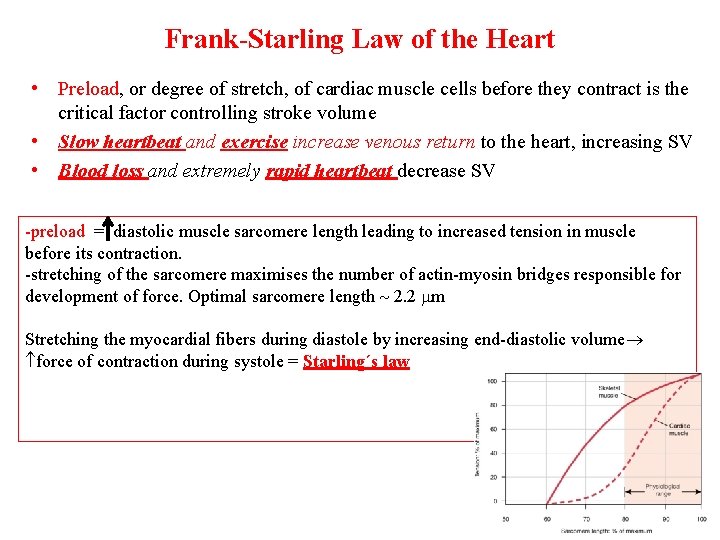
Frank-Starling Law of the Heart • Preload, or degree of stretch, of cardiac muscle cells before they contract is the critical factor controlling stroke volume • Slow heartbeat and exercise increase venous return to the heart, increasing SV • Blood loss and extremely rapid heartbeat decrease SV -preload = diastolic muscle sarcomere length leading to increased tension in muscle before its contraction. -stretching of the sarcomere maximises the number of actin-myosin bridges responsible for development of force. Optimal sarcomere length 2. 2 m Stretching the myocardial fibers during diastole by increasing end-diastolic volume force of contraction during systole = Starling´s law
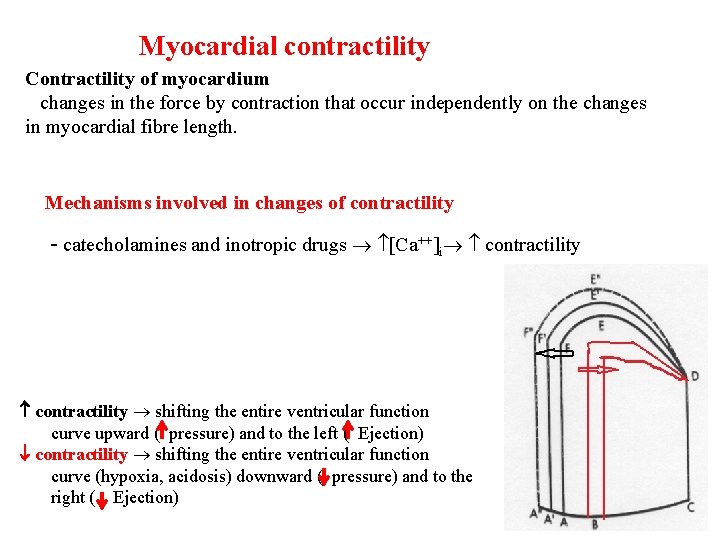
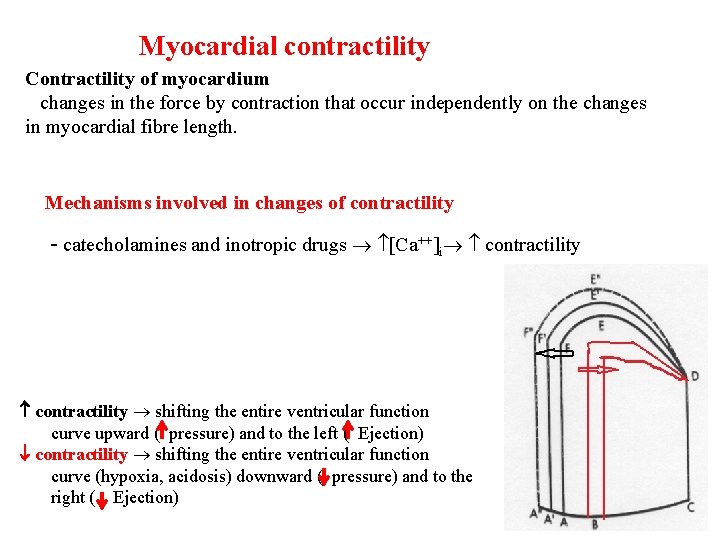
Myocardial contractility Contractility of myocardium changes in the force by contraction that occur independently on the changes in myocardial fibre length. Mechanisms involved in changes of contractility - catecholamines and inotropic drugs Ca++ i contractility shifting the entire ventricular function curve upward ( pressure) and to the left ( Ejection) contractility shifting the entire ventricular function curve (hypoxia, acidosis) downward ( pressure) and to the right ( Ejection)
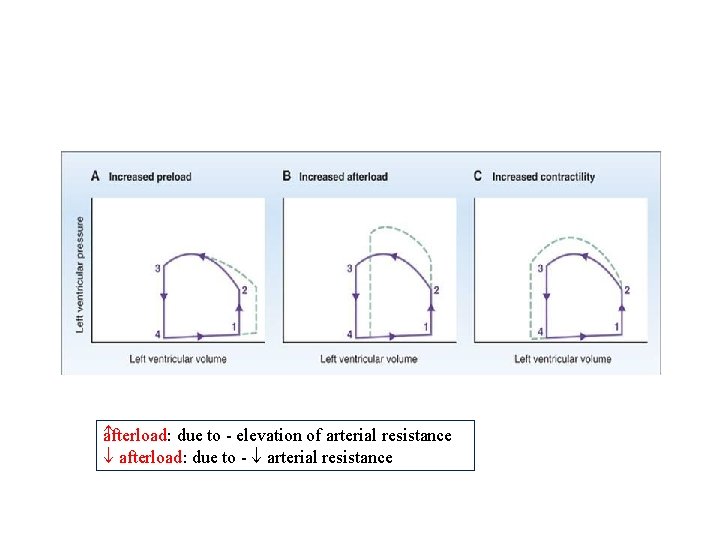
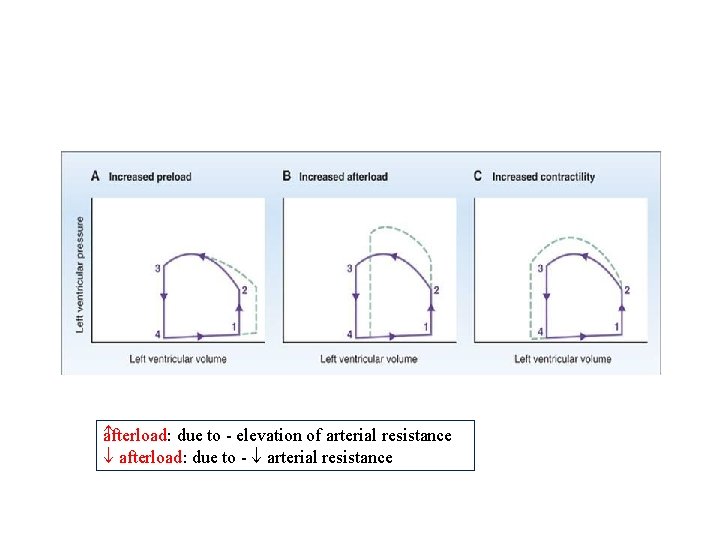
a fterload: due to - elevation of arterial resistance afterload: due to - arterial resistance
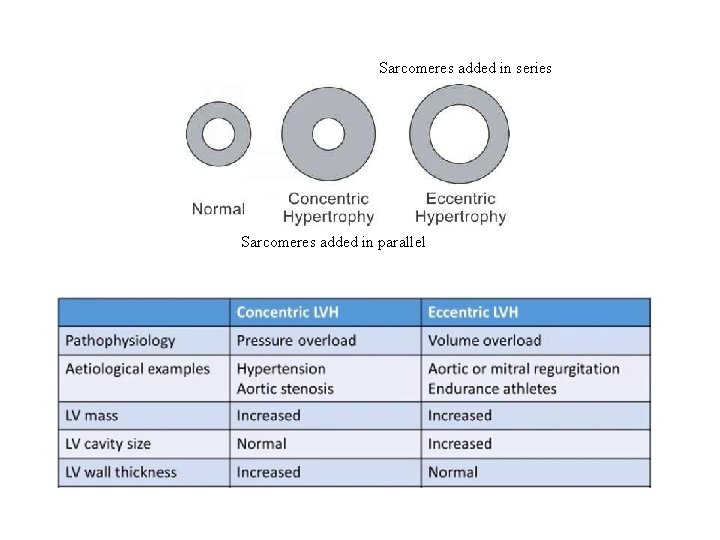
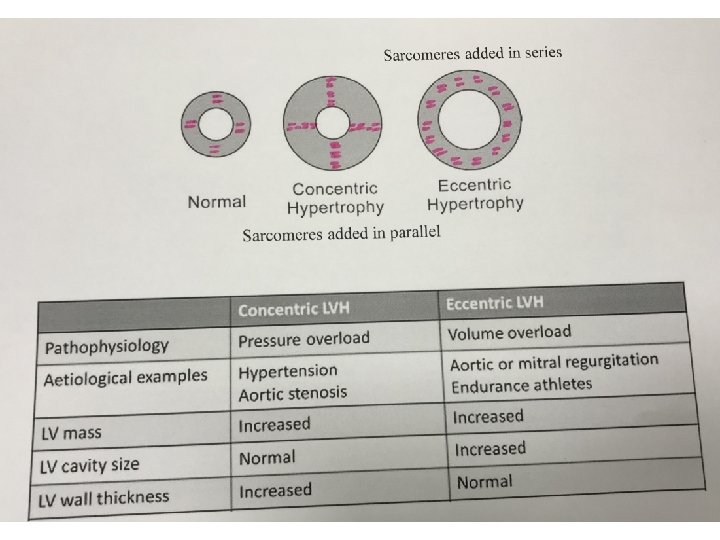
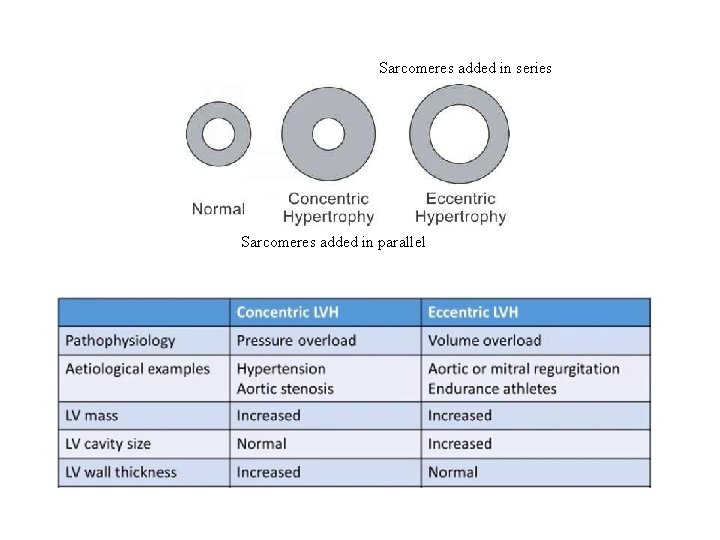
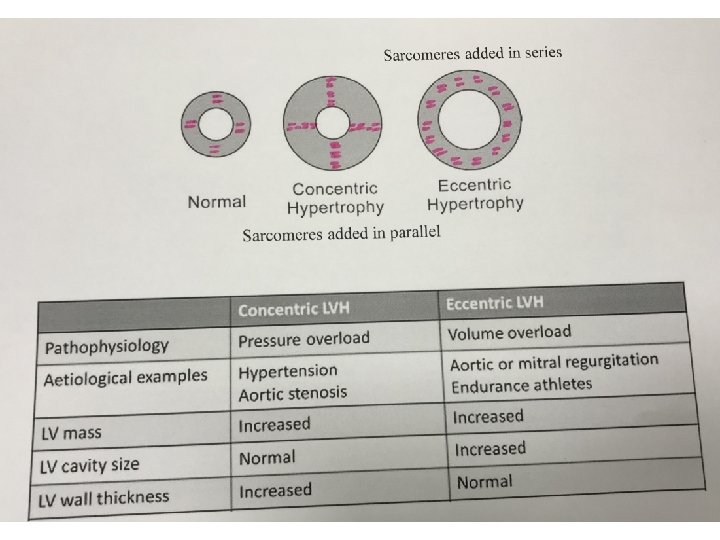
Sarcomeres added in series Sarcomeres added in parallel