cardiac arrest sudden stop of circulation and breathing
cardiac arrest sudden stop of circulation and breathing with final result the inadequate oxygenated blood supply to vital organs 4 minutes brain damage 10 minutes brain death
Closed Chest Cardiac Massage Κouwenhoven WB, JAMA, 1960
cardiac arrest 1. fatal 100% (if do nothing, wait, etc) not that rare 2. (in one’s lifetime) 3. manageable (ERC ALS/BLS ie Evidence Based Medicine) 4
arrest & cathlab q cath/PCI causes in-lab arrest q 5 arrest needs cath/PCI
arrest & cathlab q cath/PCI causes in-lab arrest q 6 arrest needs cath/PCI
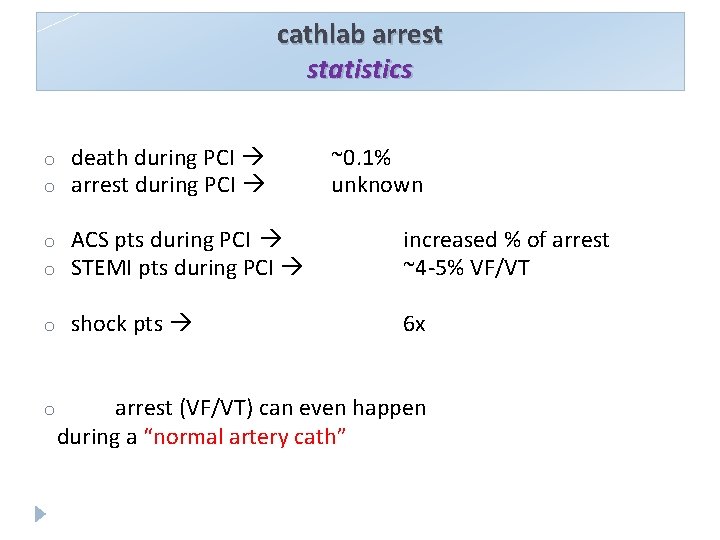
cathlab arrest statistics o o death during PCI arrest during PCI o o ACS pts during PCI STEMI pts during PCI increased % of arrest ~4 -5% VF/VT o shock pts 6 x o ~0. 1% unknown arrest (VF/VT) can even happen during a “normal artery cath”
cathlab arrest particularities 1. 2. 3. 4. 5. special causes immediate recognition (ie monitored arrest) limited space & radiation hazard no time for “expert opinion” most pts come walking and want to leave walking
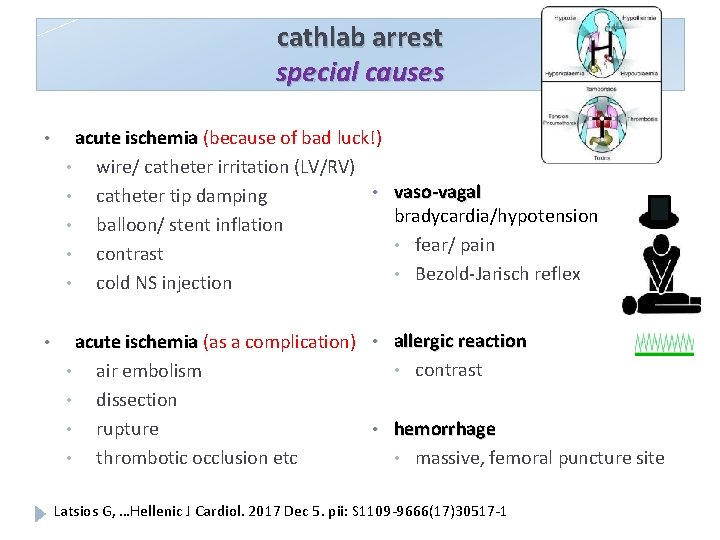
cathlab arrest special causes • acute ischemia (because of bad luck!) • wire/ catheter irritation (LV/RV) • vaso-vagal • catheter tip damping bradycardia/hypotension • balloon/ stent inflation • fear/ pain • contrast • Bezold-Jarisch reflex • cold NS injection • acute ischemia (as a complication) • air embolism • dissection • rupture • thrombotic occlusion etc • allergic reaction • contrast • hemorrhage • massive, femoral puncture site Latsios G, …Hellenic J Cardiol. 2017 Dec 5. pii: S 1109 -9666(17)30517 -1
cathlab arrest witnessed arrest many monitors that show many eyes that see many hands that act
cathlab arrest witnessed arrest many monitors that show many eyes that see many hands that act
cathlab arrest witnessed arrest many monitors that show many eyes that see many hands that act organized skilled educated

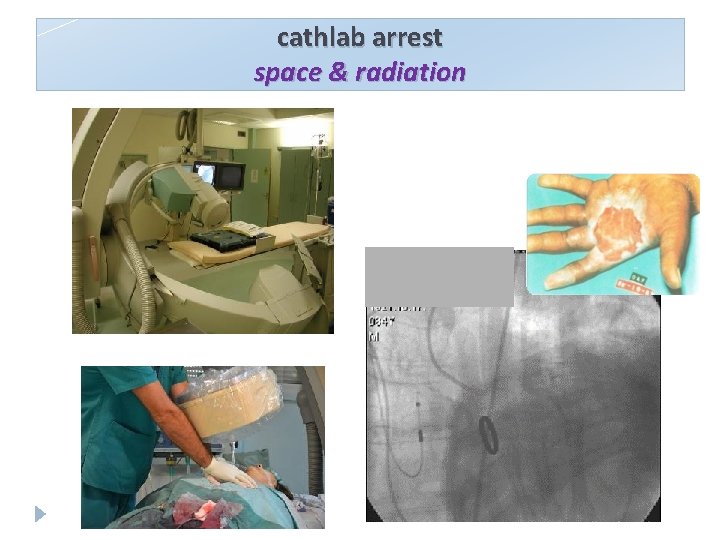
cathlab arrest space & radiation

automated chest compressions machines
AHA & ERC guidelines 2010 to support patients undergoing PCI and CT scans and also for prolonged resuscitation (Class IIa) allow defibrillation without interruption use by properly trained personnel. . (Class IIb)

SBP during C PR in femo ra ~100 mm l Hg Euro. PCR 2016, Paris 17
arrest & cathlab q cath/PCI causes in-lab arrest q arrest needs cath/PCI
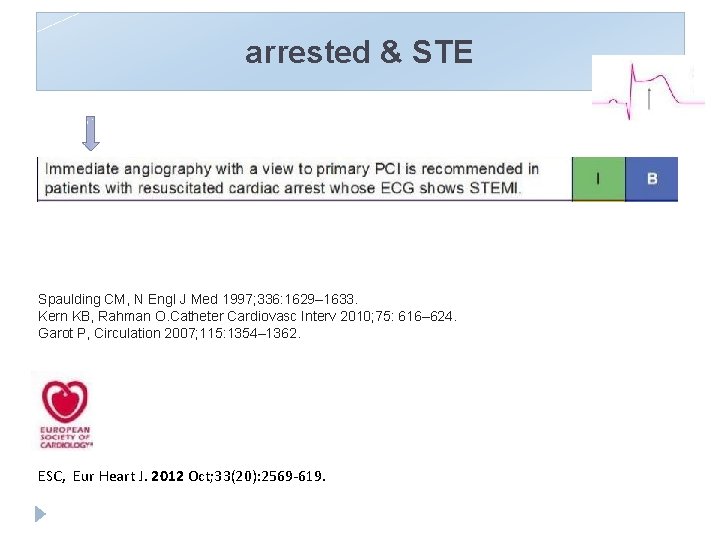
arrested & STE Spaulding CM, N Engl J Med 1997; 336: 1629– 1633. Kern KB, Rahman O. Catheter Cardiovasc Interv 2010; 75: 616– 624. Garot P, Circulation 2007; 115: 1354– 1362. ESC, Eur Heart J. 2012 Oct; 33(20): 2569 -619.
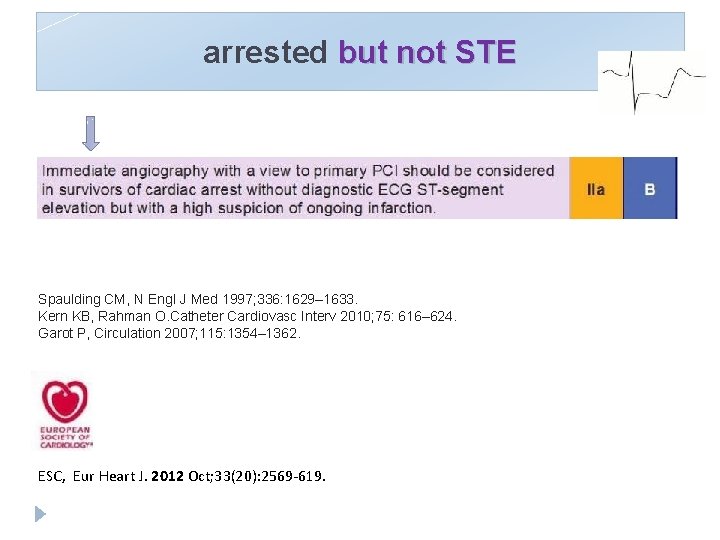
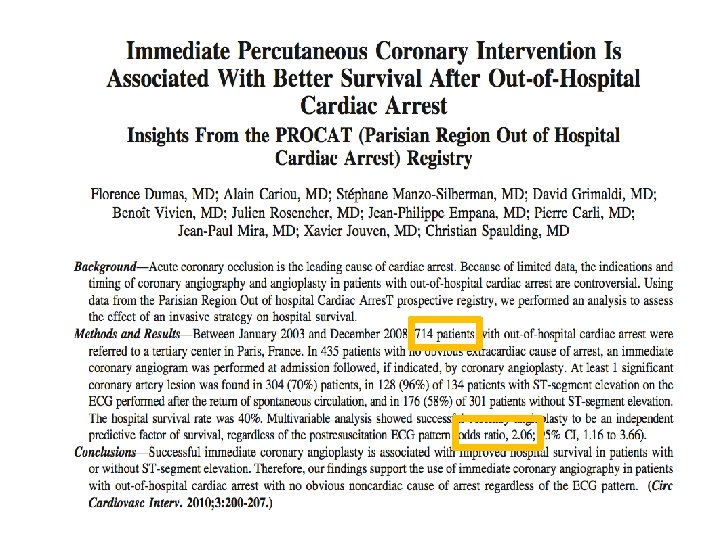
arrested but not STE Spaulding CM, N Engl J Med 1997; 336: 1629– 1633. Kern KB, Rahman O. Catheter Cardiovasc Interv 2010; 75: 616– 624. Garot P, Circulation 2007; 115: 1354– 1362. ESC, Eur Heart J. 2012 Oct; 33(20): 2569 -619.
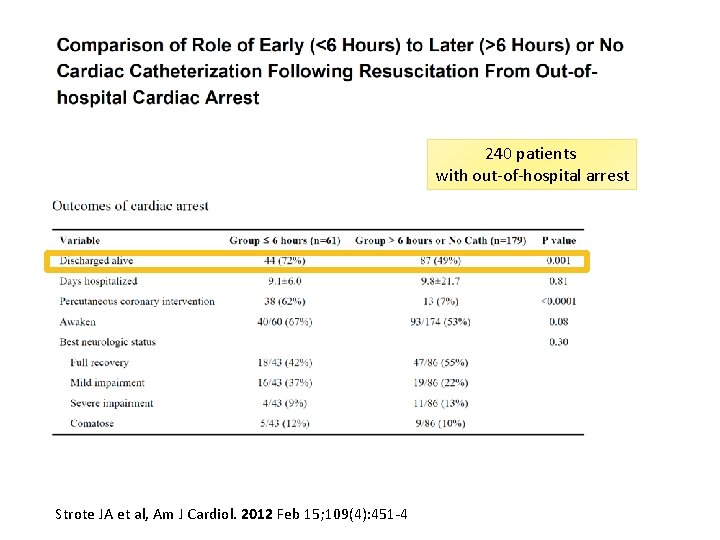
240 patients with out-of-hospital arrest Strote JA et al, Am J Cardiol. 2012 Feb 15; 109(4): 451 -4
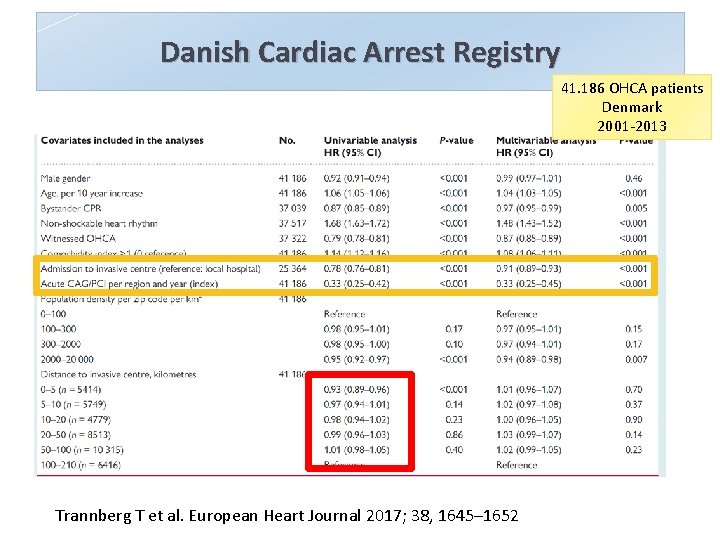
Danish Cardiac Arrest Registry 41. 186 OHCA patients Denmark 2001 -2013 Trannberg T et al. European Heart Journal 2017; 38, 1645– 1652
Urban Myth But we should make sure that the non. STEMI arrested patient wakes up or does not have severe neurological damage before we proceed to the cath lab!!!
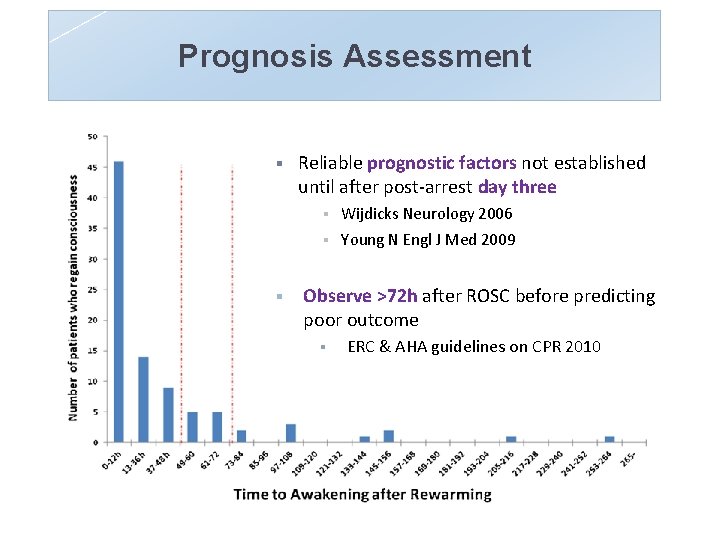
Prognosis Assessment § Reliable prognostic factors not established until after post-arrest day three § § § Wijdicks Neurology 2006 Young N Engl J Med 2009 Observe >72 h after ROSC before predicting poor outcome § ERC & AHA guidelines on CPR 2010
arrested without ROSC “refractory” VF arrest death
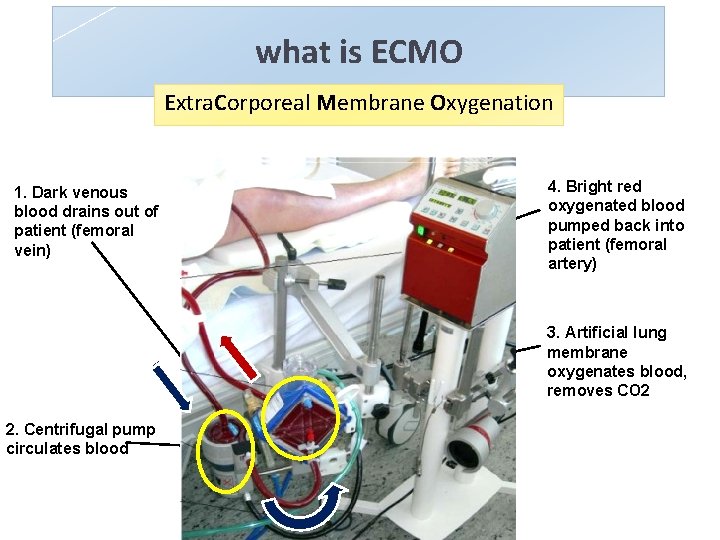
what is ECMO Extra. Corporeal Membrane Oxygenation 1. Dark venous blood drains out of patient (femoral vein) 4. Bright red oxygenated blood pumped back into patient (femoral artery) 3. Artificial lung membrane oxygenates blood, removes CO 2 2. Centrifugal pump circulates blood
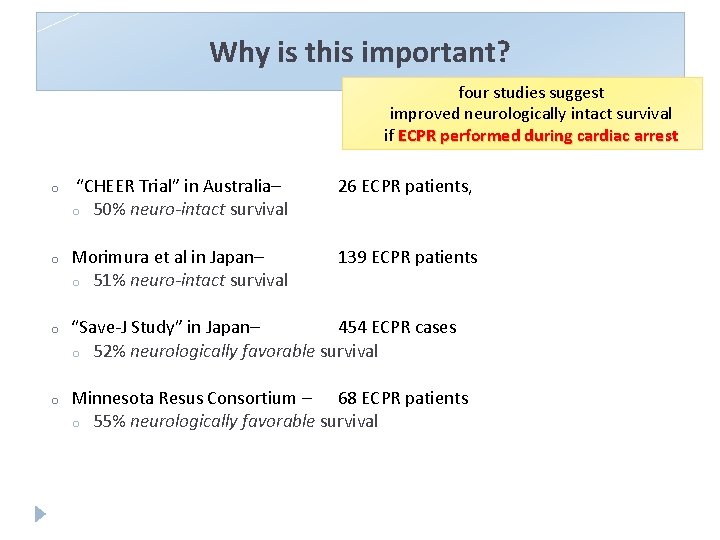
Why is this important? four studies suggest improved neurologically intact survival if ECPR performed during cardiac arrest o “CHEER Trial” in Australia– o 50% neuro-intact survival 26 ECPR patients, o Morimura et al in Japan– o 51% neuro-intact survival 139 ECPR patients o “Save-J Study” in Japan– 454 ECPR cases o 52% neurologically favorable survival o Minnesota Resus Consortium – 68 ECPR patients o 55% neurologically favorable survival

AHA ECPR guidelines 2015 There is insufficient evidence to recommend the routine use of ECPR for patients with cardiac arrest. In settings where it can be rapidly implemented, implemented ECPR may be considered for select patients for whom the suspected etiology of the cardiac arrest is potentially reversible during a limited period of mechanical cardiorespiratory support (class IIb, LOE C)
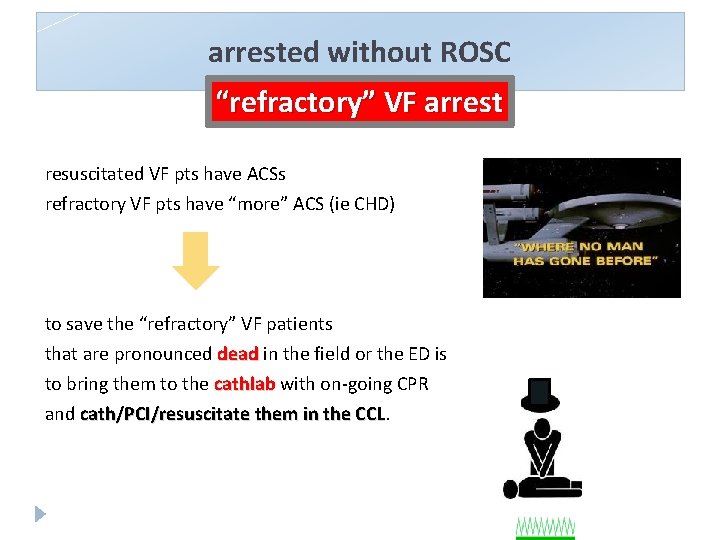
arrested without ROSC “refractory” VF arrest resuscitated VF pts have ACSs refractory VF pts have “more” ACS (ie CHD) to save the “refractory” VF patients that are pronounced dead in the field or the ED is to bring them to the cathlab with on-going CPR and cath/PCI/resuscitate them in the CCL
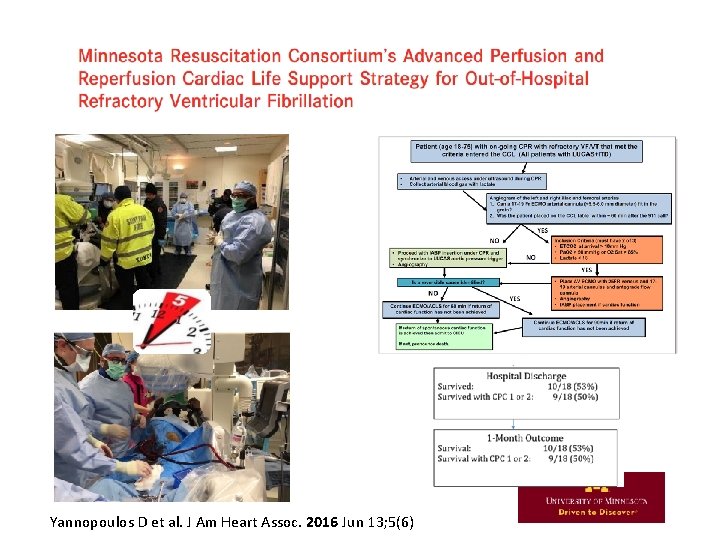
Yannopoulos D et al. J Am Heart Assoc. 2016 Jun 13; 5(6)
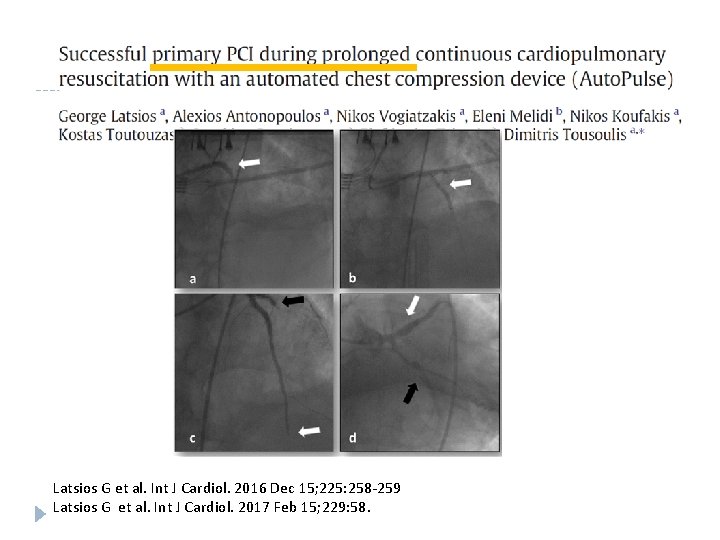
Latsios G et al. Int J Cardiol. 2016 Dec 15; 225: 258 -259 Latsios G et al. Int J Cardiol. 2017 Feb 15; 229: 58.
arrest & cathlab conclusions cath/PCI causes in-lab arrest : the best place for an arrest to happen q arrest needs cath/PCI : the best place to bring a cardiac arrested pt q q BLS/ALS trained people resuscitate pts
Latsios G, …Hellenic J Cardiol. 2017 Dec 5.
- Slides: 34