Carbon Dioxide Transport Carbon dioxide is transported in
Carbon Dioxide Transport • Carbon dioxide is transported in the blood in three forms – Dissolved in plasma – 7 to 10% – Chemically bound to hemoglobin – 20% is carried in RBCs as carbaminohemoglobin – Bicarbonate ion in plasma – 70% is transported as bicarbonate (HCO 3–)

Transport and Exchange of Carbon Dioxide • Carbon dioxide diffuses into RBCs and combines with water to form carbonic acid (H 2 CO 3), which quickly dissociates into hydrogen ions and bicarbonate ions CO 2 Carbon dioxide + H 2 O Water H 2 CO 3 Carbonic acid H+ Hydrogen ion + HCO 3– Bicarbonate ion • In RBCs, carbonic anhydrase reversibly catalyzes the conversion of carbon dioxide and water to carbonic acid
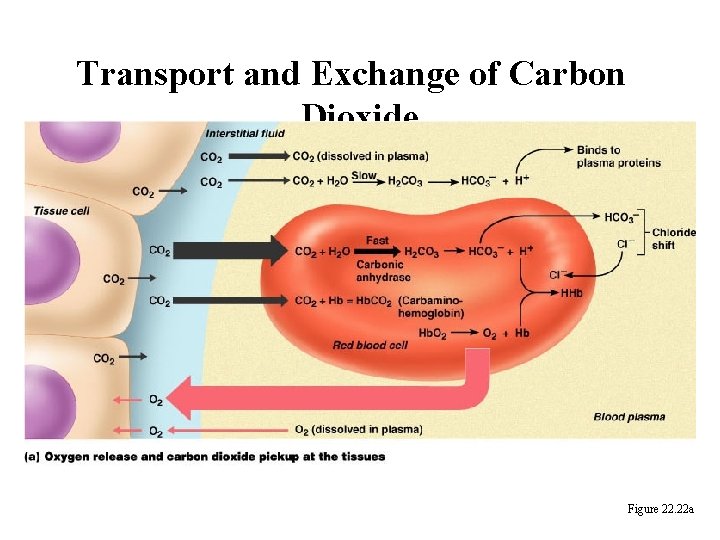
Transport and Exchange of Carbon Dioxide Figure 22. 22 a
Transport and Exchange of Carbon Dioxide • At the tissues: – Bicarbonate quickly diffuses from RBCs into the plasma – The chloride shift – to counterbalance the outrush of negative bicarbonate ions from the RBCs, chloride ions (Cl–) move from the plasma into the erythrocytes
Transport and Exchange of Carbon Dioxide • At the lungs, these processes are reversed – Bicarbonate ions move into the RBCs and bind with hydrogen ions to form carbonic acid – Carbonic acid is then split by carbonic anhydrase to release carbon dioxide and water – Carbon dioxide then diffuses from the blood into the alveoli
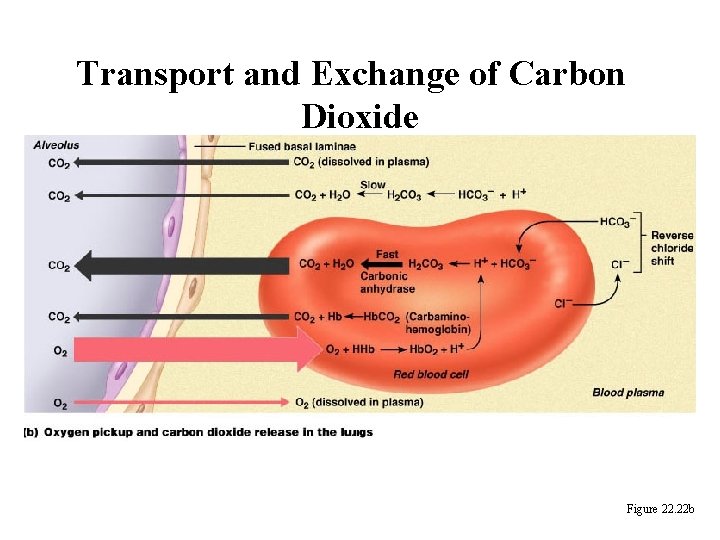
Transport and Exchange of Carbon Dioxide Figure 22. 22 b
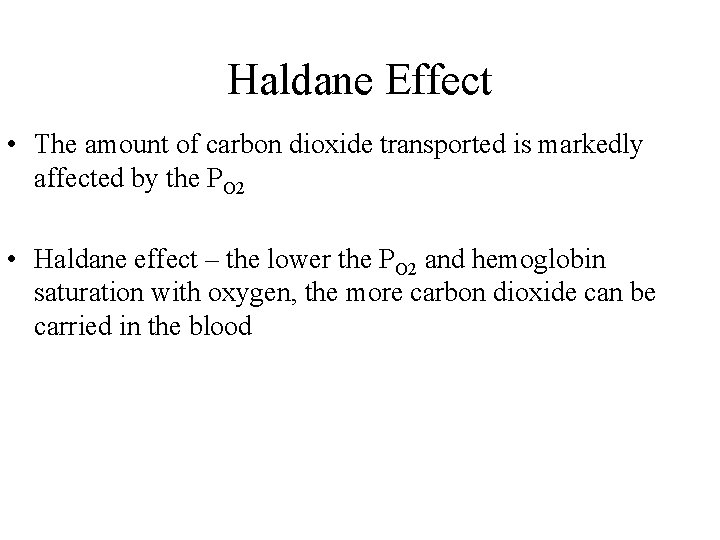
Haldane Effect • The amount of carbon dioxide transported is markedly affected by the PO 2 • Haldane effect – the lower the PO 2 and hemoglobin saturation with oxygen, the more carbon dioxide can be carried in the blood
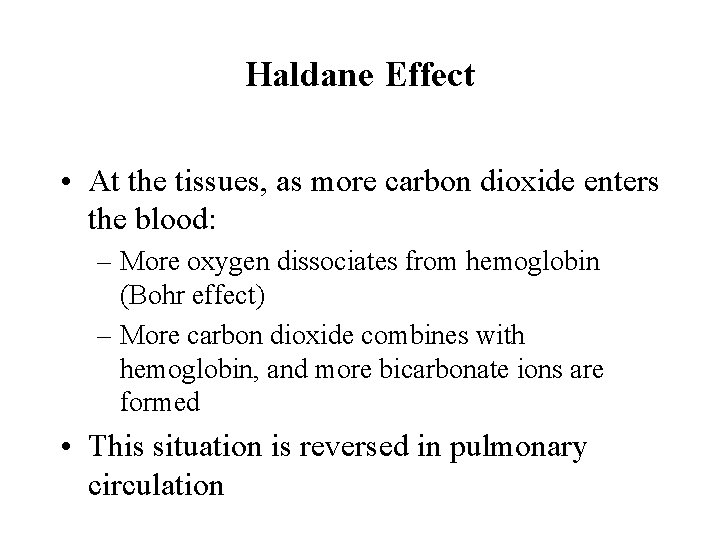
Haldane Effect • At the tissues, as more carbon dioxide enters the blood: – More oxygen dissociates from hemoglobin (Bohr effect) – More carbon dioxide combines with hemoglobin, and more bicarbonate ions are formed • This situation is reversed in pulmonary circulation
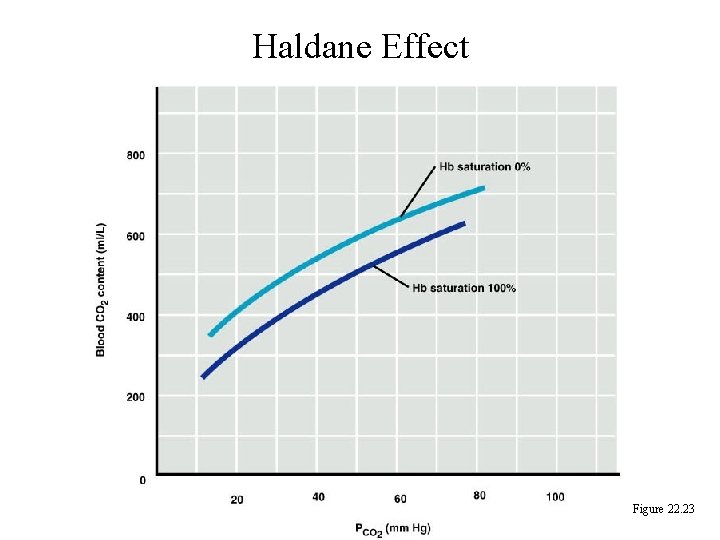
Haldane Effect Figure 22. 23
Influence of Carbon Dioxide on Blood p. H • The carbonic acid–bicarbonate buffer system resists blood p. H changes • If hydrogen ion concentrations in blood begin to rise, excess H+ is removed by combining with HCO 3– • If hydrogen ion concentrations begin to drop, carbonic acid dissociates, releasing H+
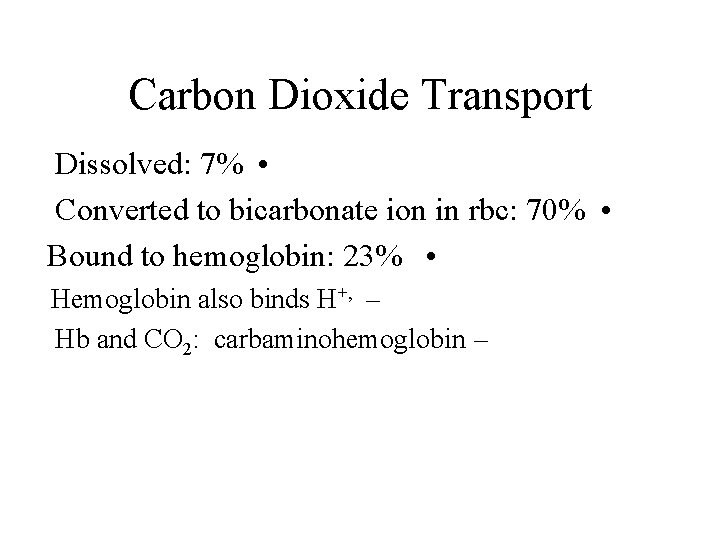
Carbon Dioxide Transport Dissolved: 7% • Converted to bicarbonate ion in rbc: 70% • Bound to hemoglobin: 23% • Hemoglobin also binds H+, – Hb and CO 2: carbaminohemoglobin –
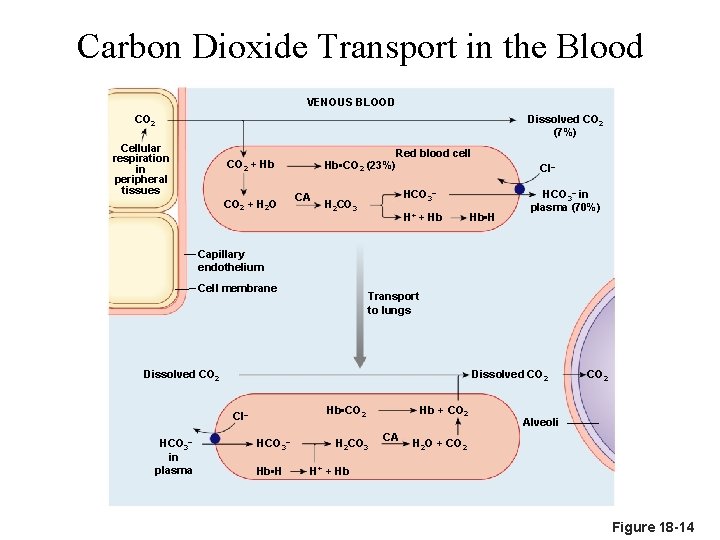
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA Cl– HCO 3– H 2 CO 3 H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 HCO 3– in plasma Hb + CO 2 Hb • CO 2 Cl– HCO 3– Hb • H H 2 CO 3 CA CO 2 Alveoli H 2 O + CO 2 H+ + Hb Figure 18 -14
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Capillary endothelium Cell membrane Alveoli Figure 18 -14 (1 of 17)
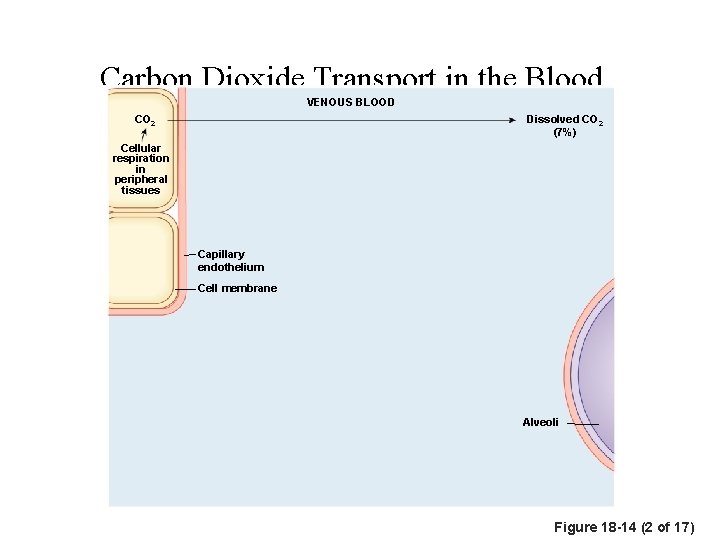
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Capillary endothelium Cell membrane Alveoli Figure 18 -14 (2 of 17)

Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Dissolved CO 2 (7%) CO 2 Red blood cell Capillary endothelium Cell membrane Alveoli Figure 18 -14 (3 of 17)

Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Dissolved CO 2 (7%) CO 2 + Hb Red blood cell Hb • CO 2 (23%) Capillary endothelium Cell membrane Alveoli Figure 18 -14 (4 of 17)
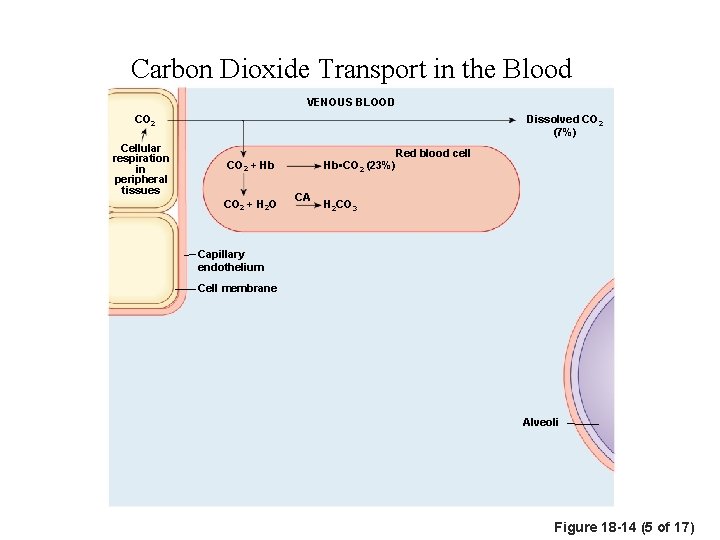
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Dissolved CO 2 (7%) Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 Capillary endothelium Cell membrane Alveoli Figure 18 -14 (5 of 17)
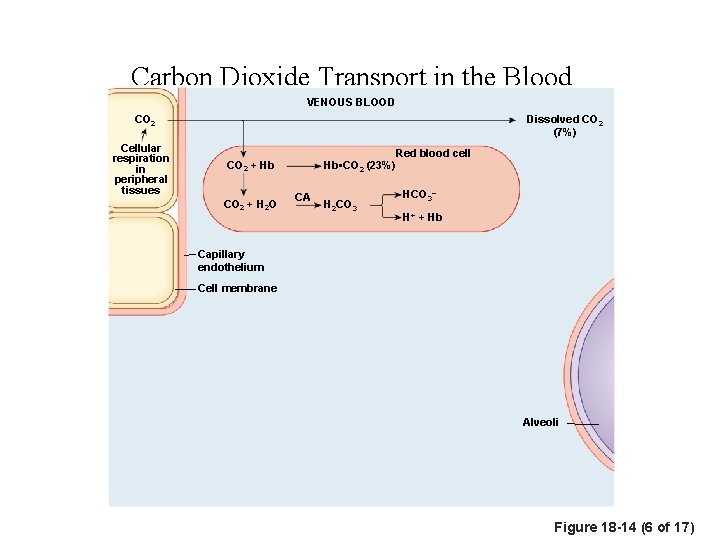
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Dissolved CO 2 (7%) Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 HCO 3– H+ + Hb Capillary endothelium Cell membrane Alveoli Figure 18 -14 (6 of 17)
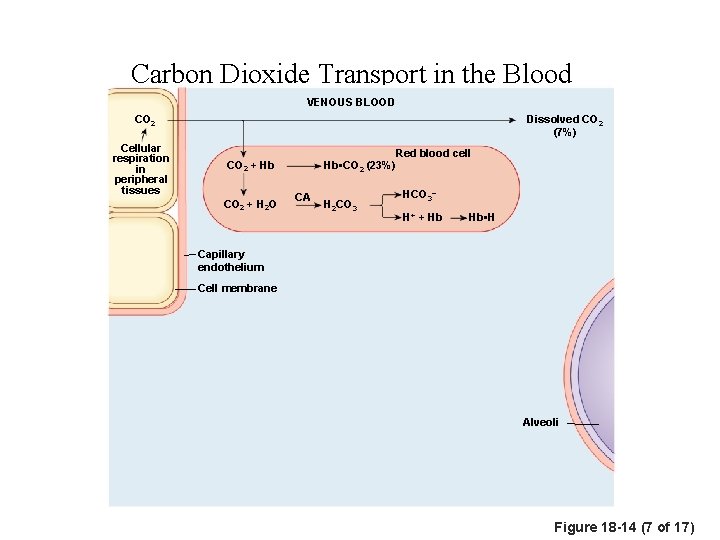
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Dissolved CO 2 (7%) Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 HCO 3– H+ + Hb Hb • H Capillary endothelium Cell membrane Alveoli Figure 18 -14 (7 of 17)
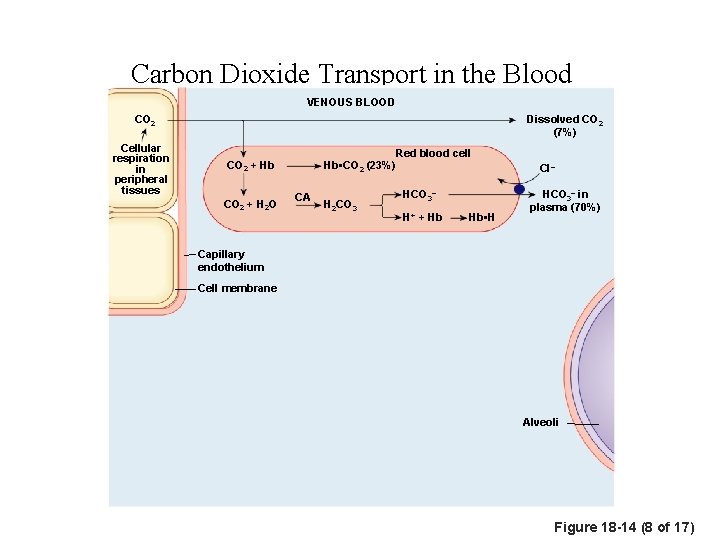
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Dissolved CO 2 (7%) Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 HCO 3– H+ + Hb Hb • H Cl– HCO 3– in plasma (70%) Capillary endothelium Cell membrane Alveoli Figure 18 -14 (8 of 17)
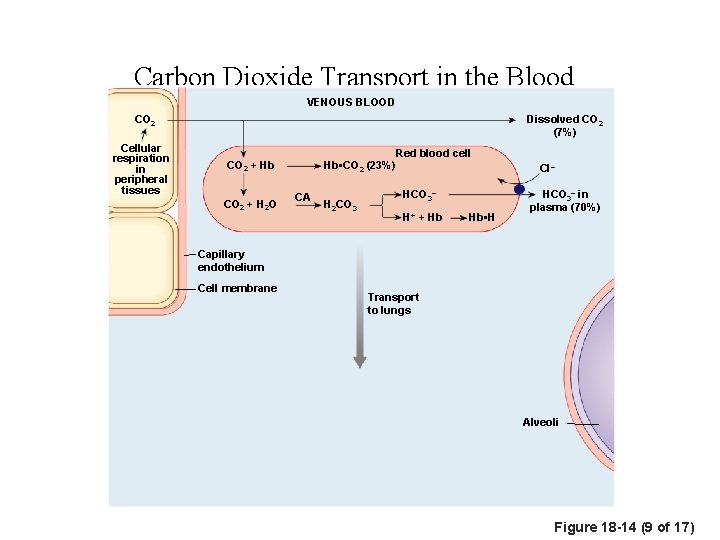
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Cellular respiration in peripheral tissues Dissolved CO 2 (7%) Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 HCO 3– H+ + Hb Hb • H Cl– HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Alveoli Figure 18 -14 (9 of 17)
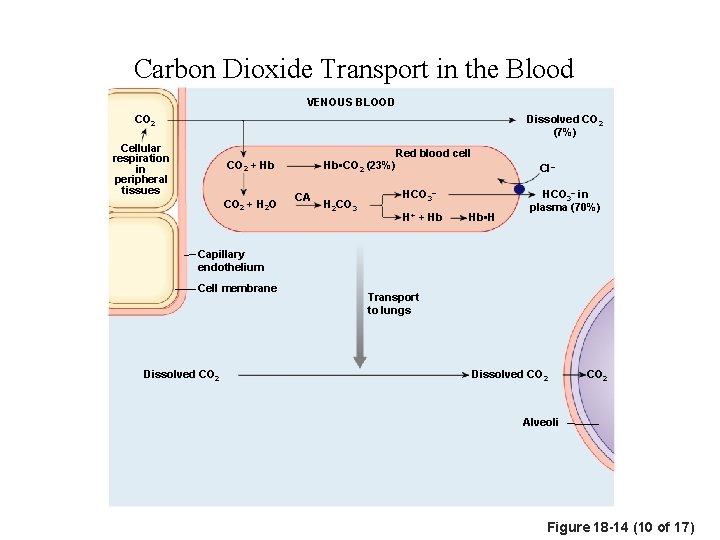
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 Cl– HCO 3– H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Dissolved CO 2 Transport to lungs Dissolved CO 2 Alveoli Figure 18 -14 (10 of 17)

Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 Cl– HCO 3– H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 Hb • CO 2 Hb + CO 2 Alveoli Figure 18 -14 (11 of 17)
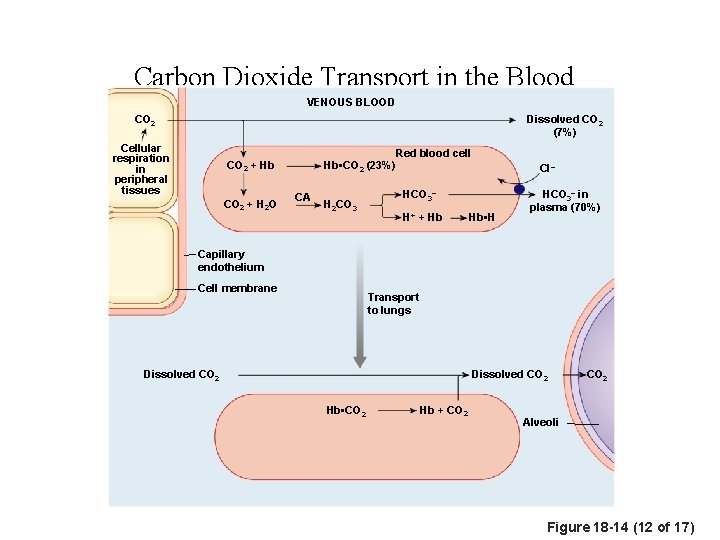
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 Cl– HCO 3– H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 Hb • CO 2 Hb + CO 2 Alveoli Figure 18 -14 (12 of 17)
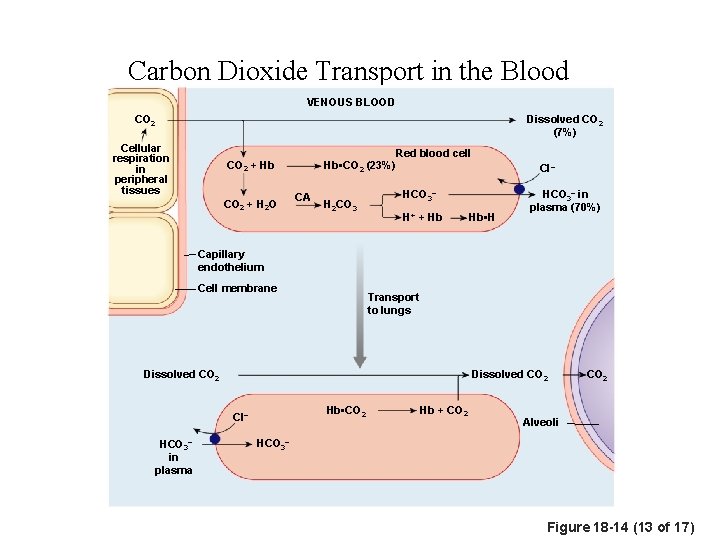
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 Cl– HCO 3– H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 Hb • CO 2 Cl– HCO 3– in plasma Hb + CO 2 Alveoli HCO 3– Figure 18 -14 (13 of 17)
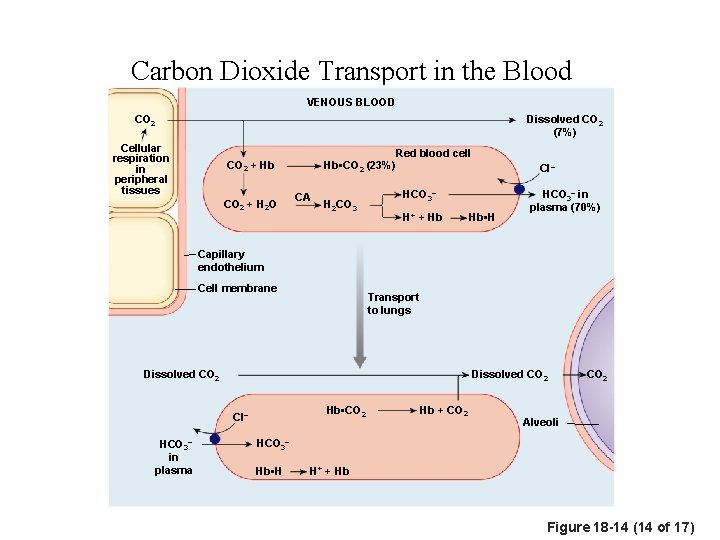
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA H 2 CO 3 Cl– HCO 3– H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 Hb • CO 2 Cl– HCO 3– in plasma Hb + CO 2 Alveoli HCO 3– Hb • H H+ + Hb Figure 18 -14 (14 of 17)
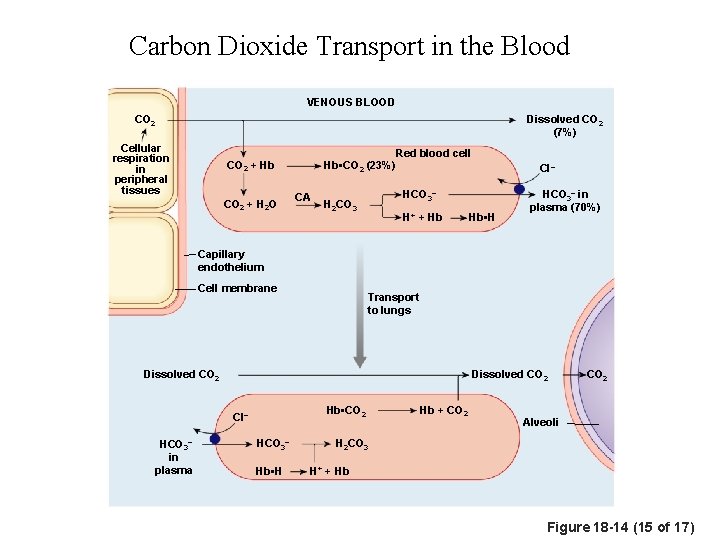
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA Cl– HCO 3– H 2 CO 3 H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 Hb • CO 2 Cl– HCO 3– in plasma HCO 3– Hb • H Hb + CO 2 Alveoli H 2 CO 3 H+ + Hb Figure 18 -14 (15 of 17)
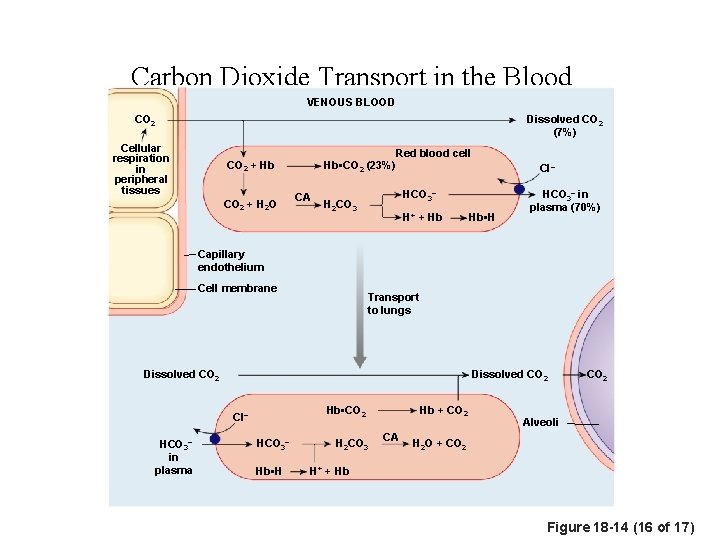
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA Cl– HCO 3– H 2 CO 3 H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 HCO 3– in plasma Hb + CO 2 Hb • CO 2 Cl– HCO 3– Hb • H H 2 CO 3 CA CO 2 Alveoli H 2 O + CO 2 H+ + Hb Figure 18 -14 (16 of 17)
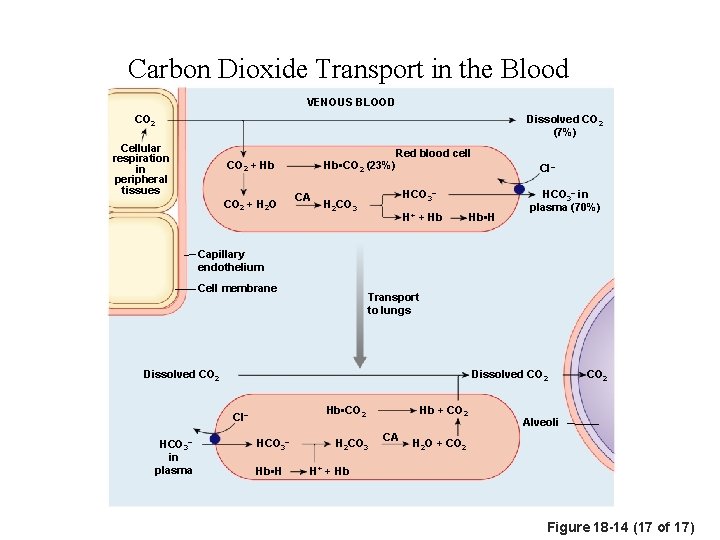
Carbon Dioxide Transport in the Blood VENOUS BLOOD CO 2 Dissolved CO 2 (7%) Cellular respiration in peripheral tissues Red blood cell Hb • CO 2 (23%) CO 2 + Hb CO 2 + H 2 O CA Cl– HCO 3– H 2 CO 3 H+ + Hb Hb • H HCO 3– in plasma (70%) Capillary endothelium Cell membrane Transport to lungs Dissolved CO 2 HCO 3– in plasma Hb + CO 2 Hb • CO 2 Cl– HCO 3– Hb • H H 2 CO 3 CA CO 2 Alveoli H 2 O + CO 2 H+ + Hb Figure 18 -14 (17 of 17)
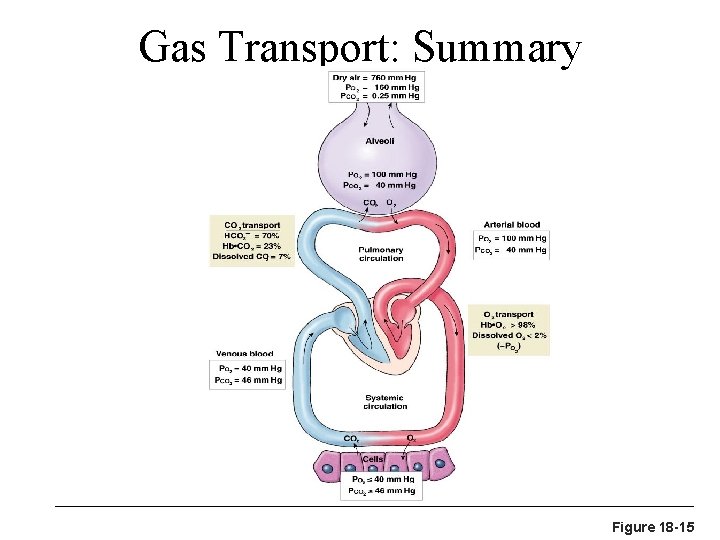
Gas Transport: Summary Figure 18 -15
Influence of Carbon Dioxide on Blood p. H Changes in respiratory rate can also: • Alter blood p. H – Provide a fast-acting system to adjust p. H when it is – disturbed by metabolic factors
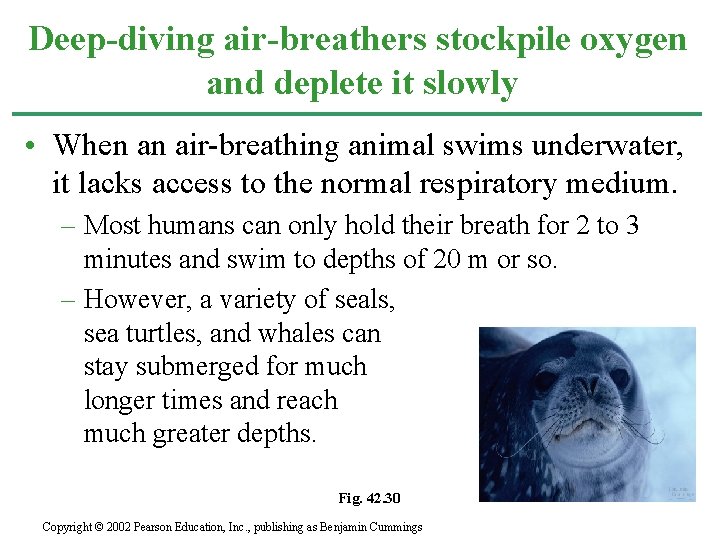
Deep-diving air-breathers stockpile oxygen and deplete it slowly • When an air-breathing animal swims underwater, it lacks access to the normal respiratory medium. – Most humans can only hold their breath for 2 to 3 minutes and swim to depths of 20 m or so. – However, a variety of seals, sea turtles, and whales can stay submerged for much longer times and reach much greater depths. Fig. 42. 30 Copyright © 2002 Pearson Education, Inc. , publishing as Benjamin Cummings
• One adaptation of these deep-divers, such as the Weddell seal, is an ability to store large amounts of O 2 in the tissues. – Compared to a human, a seal can store about twice as much O 2 per kilogram of body weight, mostly in the blood and muscles. – About 36% of our total O 2 is in our lungs and 51% in our blood. – In contrast, the Weddell seal holds only about 5% of its O 2 in its small lungs and stockpiles 70% in the blood. Copyright © 2002 Pearson Education, Inc. , publishing as Benjamin Cummings
• Several adaptations create these physiological differences between the seal and other deepdivers in comparison to humans. – First, the seal has about twice the volume of blood per kilogram of body weight as a human. – Second, the seal can store a large quantity of oxygenated blood in its huge spleen, releasing this blood after the dive begins. – Third, diving mammals have a high concentration of an oxygen-storing protein called myoglobin in their muscles. • This enables a Weddell seal to store about 25% of its O 2 in muscle, compared to only 13% in humans. Copyright © 2002 Pearson Education, Inc. , publishing as Benjamin Cummings
• Diving vertebrates not only start a dive with a relatively large O 2 stockpile, but they also have adaptations that conserve O 2. – They swim with little muscular effort and often use buoyancy changes to glide passively upward or downward. – Their heart rate and O 2 consumption rate decreases during the dive and most blood is routed to the brain, spinal cord, eyes, adrenal glands, and placenta (in pregnant seals). – Blood supply is restricted or even shut off to the muscles, and the muscles can continue to derive ATP from fermentation after their internal O 2 stores are depleted. Copyright © 2002 Pearson Education, Inc. , publishing as Benjamin Cummings
- Slides: 35